Abstract
Objective
Miniscrew-assisted rapid palatal expansion (MARPE) is a means for expanding the basal bone without surgical intervention in young adults. Here, we assessed the differences in dental, alveolar, and skeletal measurements taken before (T0), immediately after (T1), and 1 year after (T2) MARPE.
Methods
Twenty-four patients (mean age, 21.6 years) who had undergone MARPE and cone-beam computed tomography at T0, T1, and T2 were included. Changes in the following parameters were compared using paired t-tests: intercusp, interapex, alveolar, nasal floor, and nasal cavity widths; inclination of the first molar (M1) and its alveolus; and thickness and height of the alveolar bone. A linear mixed-effects model was used to determine variables that affected periodontal changes in the M1.
Results
MARPE produced significant increases in most measurements during T0–T2, despite relapse of some measurements during T1–T2. The alveolar thickness decreased on the buccal side, but increased on the palatal side. The alveolar crest level at the first premolar moved apically. Changes in the thickness and height of the alveolar bone were affected by the corresponding initial values.
Conclusions
MARPE can be used as an effective tool for correcting maxillomandibular transverse discrepancy, showing stable outcomes 1 year after expansion.
Keywords: Cone-beam computed tomography, Miniscrew-assisted rapid palatal expansion, Stability, Expansion
INTRODUCTION
Age is considered an important factor in rapid palatal expansion (RPE), which is used to obtain orthopedic expansion.1,2,3 Orthopedic expansion through RPE is achieved not only by the separation of the midpalatal suture, but also by its effects on the circummaxillary sutures.4 These structures show greater resistance to expansion with age; thus, RPE produces predominantly dentoalveolar effects5 and may cause detrimental periodontal effects in adults. Therefore, the optimal age for RPE would be below 13 to 15 years of age,6 when growth at the midpalatal suture would have ceased.7 In adults, surgically assisted RPE (SARPE) has been the treatment of choice.8
Periodontal recession is considered inevitable even after SARPE, despite the surgical separation of the suture,9 which may be because of the tooth-borne design of the appliance. Additionally, the surgical intervention required for SARPE creates a burden on the patient and practitioner. Therefore, miniscrew-assisted RPE (MARPE), which is a tooth-and-bone-borne appliance, can offer an alternative approach for expanding the basal bone without surgical intervention in young adults.10,11,12 This appliance has a rigid element that connects to four miniscrews, which are inserted into the para-midsagittal area, delivering the expansion force directly to the basal bone and maximizing the skeletal effect.
In previous studies of periodontal changes after RPE, the thickness of the buccal bone of the supporting teeth was reduced by 0.6–0.9 mm, and the buccal alveolar crest level was lowered.13,14 However, in non-growing patients, the periodontal effects remain unclear, because the measurements have been performed in growing patients immediately after expansion. Increased interdigitation of the midpalatal suture with age may result in more dentoalveolar effects after maxillary expansion in adults,1 resulting in greater detrimental periodontal changes. Although buccal dehiscence has been reported immediately after maxillary expansion in late adolescent individuals,15 changes in the alveolar bone should be monitored over an extended period, because its remodeling continues even after the removal of the appliance.16
Immediately after MARPE in young adults, the buccal alveolar bone thickness is decreased and the alveolar crest is lowered.12 Because the alveolar bone remodels according to tooth position,17,18 changes in the alveolar bone may differ thereafter, which indicates the necessity of long-term evaluation. Even though the long-term stability of skeletal and dental expansion has already been confirmed by means of posteroanterior cephalograms,11 various aspects of dental and alveolar evaluation have been limited by the two-dimensional nature of these scans. Thus, this study aimed to evaluate the following null hypothesis: there are no differences in dental, alveolar, and skeletal measurements derived from cone-beam computed tomography (CBCT) images acquired before (T0), immediately after (T1), and 1 year after (T2) MARPE. This study further investigated factors affecting alveolar changes.
MATERIALS AND METHODS
Subjects
This retrospective study included 24 patients (8 men and 16 women; mean age, 21.6 ± 3.1 years; range, 18.25–26.75 years; Table 1). The subjects were selected among 38 patients who had been diagnosed with maxillary constriction19 and were treated with MARPE at the study hospital since January 2012. The inclusion criteria were as follows: successful opening of the midpalatal suture; availability of serial CBCT images acquired at T0, T1, and T2; non-extraction treatment; less than 2-mm anteroposterior movement of the maxillary first molar during treatment; cervical vertebrae maturity indicator at stage 620; less than 1-mm gingival recession before treatment; and absence of systemic diseases and craniofacial syndrome. Fourteen patients were excluded for the following reasons: failure of opening of the midpalatal suture (n = 5); extraction treatment (n = 7); and molar distalization > 2 mm (n = 2). Based on the findings of a previous study,11 the minimum sample size for revealing significant changes after MARPE for this study was calculated as 9; thus, the 24 subjects included in this study were considered adequate.
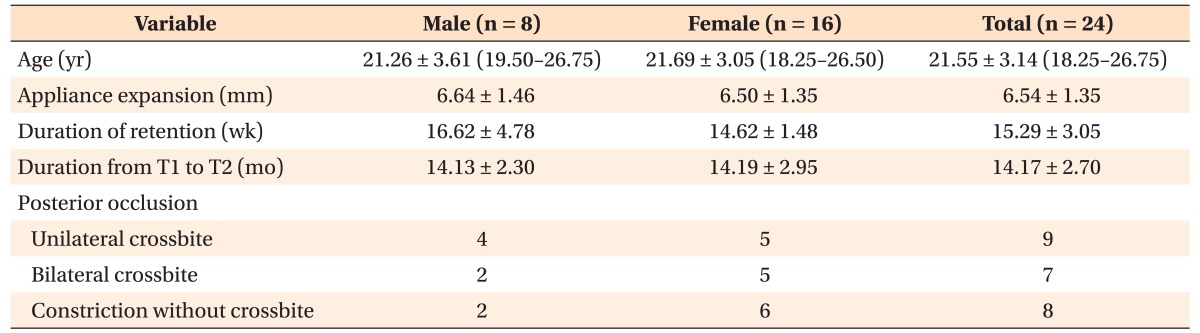
Table 1. Demographic features of the study subjects.
Values are presented as number or mean ± standard deviation (range) or number only.
T1, Immediately after expansion; T2, approximately 1 year after expansion.
MARPE is a modified Hyrax-type expander (Hyrax II; Dentaurum, Ispringen, Germany), which is connected to the palate at the para-midsagittal area by means of four miniscrews (collar diameter, 1.8 mm; length, 7 mm; Orlus, Ortholution, Seoul, Korea) (Figure 1).10 Four hooks soldered onto the screw body delivered the expansion force to the bone through each miniscrew: two anterior miniscrews were implanted in the rugae area and two posterior miniscrews in the para-midsagittal area. The jackscrew was turned once a day (0.2 mm per turn) until the required expansion had been achieved. Separation of the midpalatal suture was confirmed on a periapical radiograph. The mean (± standard deviation) appliance expansion was 6.54 (± 1.35) mm, and the duration of expansion was approximately 5 weeks. The second CBCT image was taken within 1 month (mean, 9.5 days; range, 0–28 days) after the completion of expansion to confirm alveolar dehiscence. After approximately 4 months (15.29 ± 3.05 weeks) of retention, the appliance was removed, and the maxillary first premolars and first molars were included for leveling and alignment. The third CBCT image was taken approximately 1 year after the completion of expansion (mean duration, 14.17 months; range, 12.0–16.5 months) either for presurgical planning for orthognathic surgery (n = 13) or as a posttreatment record after orthodontic treatment (n = 11). This study was approved by the institutional review board of Yonsei University Dental Hospital (IRB No. 2-2015-0020).
Figure 1. Miniscrew-assisted rapid palatal expander. Left, before expansion; right, after expansion.
Measurements
A CBCT apparatus (Alphard VEGA; ASAHI Roentgen IND, Kyoto, Japan) was set at 80 kV and 5.0 mA, and images were captured for 17 seconds with a 0.3-mm voxel size. CBCT images were acquired with each patient seated in an upright position and with the Frankfort horizontal and Camper's planes parallel to the floor in the lateral and frontal planes, respectively. To prevent the overlapping of teeth, the patients were asked to bite onto a cotton roll with their posterior teeth during image acquisition.
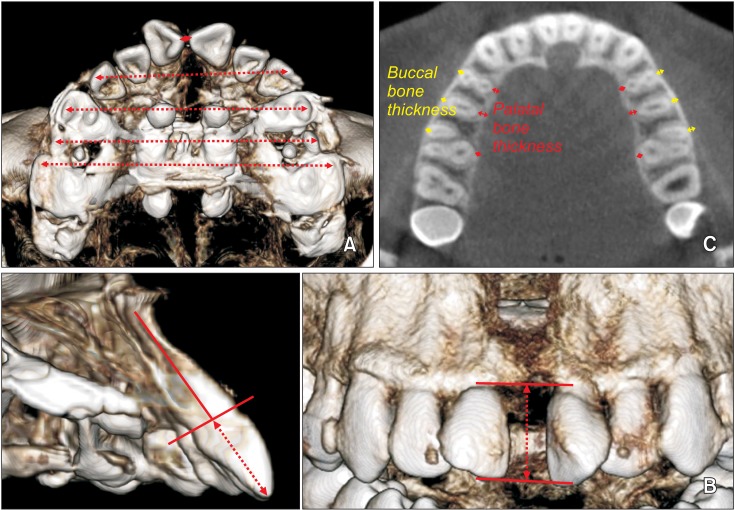
The images were imported as DICOM files using InVivo5® software (Anatomage, San Jose, CA, USA) and were reoriented with the palatal plane parallel to the floor in the sagittal and coronal planes. The following measurements were recorded (Table 2; Figures 2 and 3): appliance expansion (Figure 2A); intercusp (Figure 3A), interapex (Figure 2B), nasal cavity (Figure 2C), nasal floor (Figure 2C), and alveolar (Figure 2C) widths; changes in the inclination of the first molar (M1) and its surrounding alveolar bone (Figure 2D)15,21; interproximal (Figure 3B) and buccal (Figure 2E) alveolar crest levels (interproximal and buccal level, respectively); and buccal and palatal bone thicknesses (buccal/palatal thickness, Figure 3C). Intercusp and interapex widths were measured for the central incisor (I1), canine (C), first premolar (PM1), second premolar (PM2), and M1. The interproximal level was measured between the I1, while the buccal level and buccal/palatal thickness were measured at the PM1, PM2, and M1. For measurement of buccal thickness at the M1, the mesiobuccal root was selected because it was more prominent, and was, therefore, more likely to exhibit greater changes than did the distobuccal root.13 For evaluation of changes in inclination, buccal level, and buccal/palatal thickness, measurements were acquired on both sides, and the mean values were used for analysis.
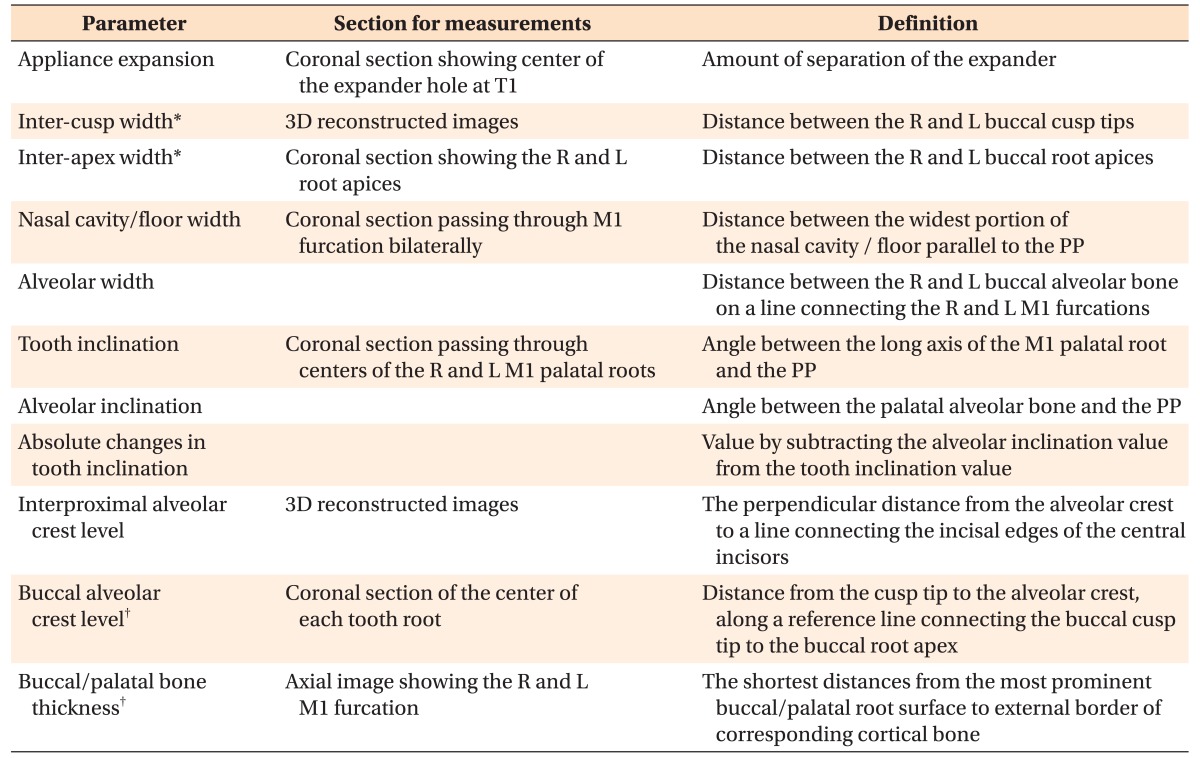
Table 2. Definitions of the parameters used in this study.
T1, Immediately after expansion; 3D, three-dimensional; R, right; L, left; M1, the maxillary first molar; PP, palatal plane.
*Intercusp and interapex widths were measured for the central incisors, canines, first and second premolars, and M1. In case of the central incisors, the most mesial point of the incisal edge was used for measurement; and in case of the M1, the mesiobuccal cusp was used.
†Buccal alveolar crest level and buccal/palatal bone thickness were measured for the first and second premolars and M1. For the M1, the mesiobuccal root was used for the measurements.
Figure 2. Measurements on the coronal images. A, Appliance expansion; B, interapex width; C, nasal cavity width (top), nasal floor width (middle), and alveolar width (bottom); D, alveolar inclination (left) and tooth inclination (right); E, buccal alveolar crest level.
Figure 3. Measurements on three-dimensional and axial images. A, Intercusp width. From top to bottom, intercusp widths of the central incisors, canines, first premolars, second premolars, and first molars. B, Interproximal alveolar crest level (dashed arrow) between the central incisors; C, buccal and palatal bone thicknesses.
Statistical analyses
Normal distribution of data was confirmed using the Shapiro–Wilk test. Paired t-tests were used to investigate changes between T0 and T1, T1 and T2, and T0 and T2. Changes in the buccal thickness and buccal level at the M1 were evaluated using a linear mixed-effects model, which included age, amount of expansion, duration of expansion, duration of retention, initial buccal thickness, and initial buccal level as covariates. The variance inflation factor revealed no multicollinearity among the covariates. Participants were treated as a random effect, and all other effects were considered fixed. We assumed that the model had a compound-symmetry variance–covariance structure.
One examiner performed all measurements. To determine intraexaminer reliability, 10 patients were randomly selected and the measurements were repeated 2 weeks apart. Intraclass correlation coefficients were determined to range from 0.966 to 0.976. All statistical analyses were performed using IBM SPSS Statistics ver. 20.0 software (IBM Co., Armonk, NY, USA), with the significance level set at p < 0.05.
RESULTS
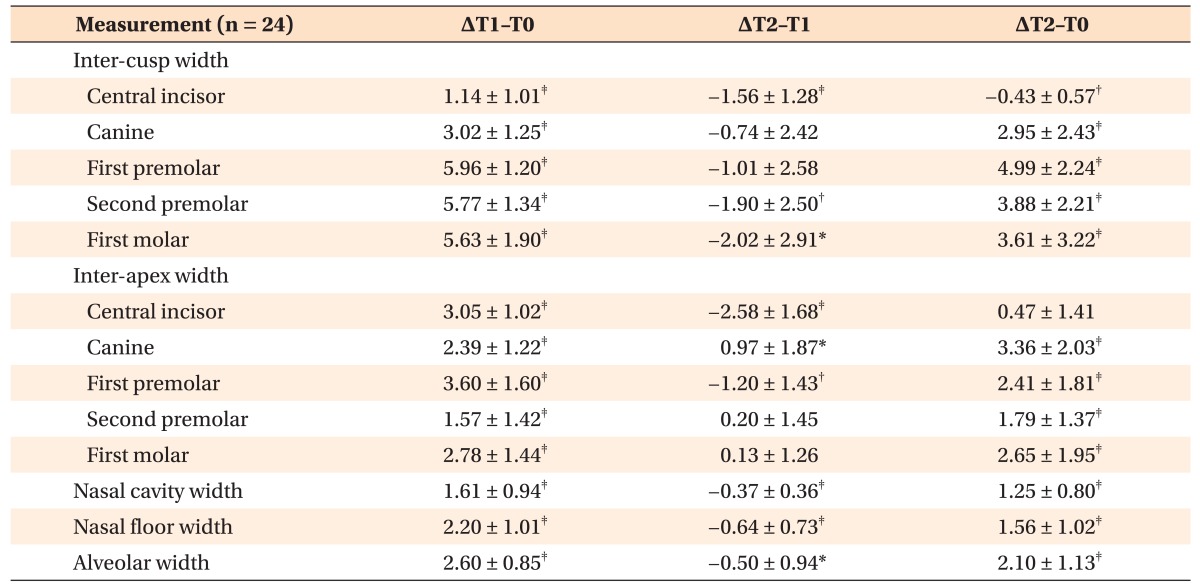
Intercusp, interapex, alveolar, nasal floor, and nasal cavity widths showed significant increases during T0–T1 (p < 0.001), and most of the measurements decreased slightly during T1–T2 (p < 0.05). All parameters of the transverse dimension, except the interapex width at I1, showed significant increases during T0–T2 (p < 0.01; Table 3).
Table 3. Changes in intercusp width, interapex width, and skeletal widths before (T0), immediately after (T1), and 1 year after (T2) expansion (unit: mm).
Values are presented as the mean ± standard deviation.
Paired t-tests were performed; *p < 0.05, †p < 0.01, ‡p < 0.001.
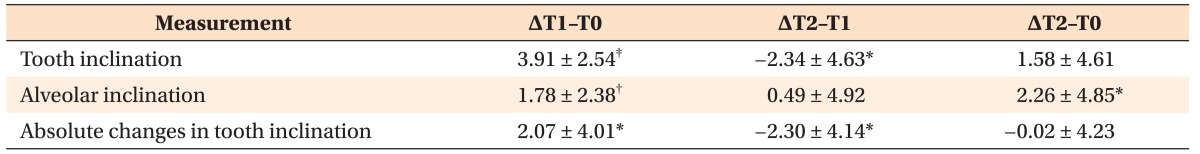
During T0–T1, the M1 and its corresponding alveolar bone showed buccal tipping of 3.91° and 1.78°, respectively (p < 0.01), indicating a 2.07° buccal tipping of the tooth itself (p < 0.05). During T1–T2, the tooth axis decreased by 2.34°, while the alveolar axis increased further by 0.49°, indicating that the tooth itself became more upright by 2.30° (p < 0.05). Consequently, during T0–T2, the alveolar bone showed a 2.26° buccal tipping (p < 0.01), but the tooth, per se, did not show significant changes in inclination (p > 0.05; Table 4).
Table 4. Changes in the axis of the first molar and alveolar bone before (T0), immediately after (T1), and 1 year after (T2) expansion (unit: degrees).
Measurements were conducted on both the right and left sides for the 21 subjects, and the mean values were used.
Values are presented as the mean ± standard deviation.
Paired t-tests were performed; *p < 0.05, †p < 0.01, ‡p < 0.001.
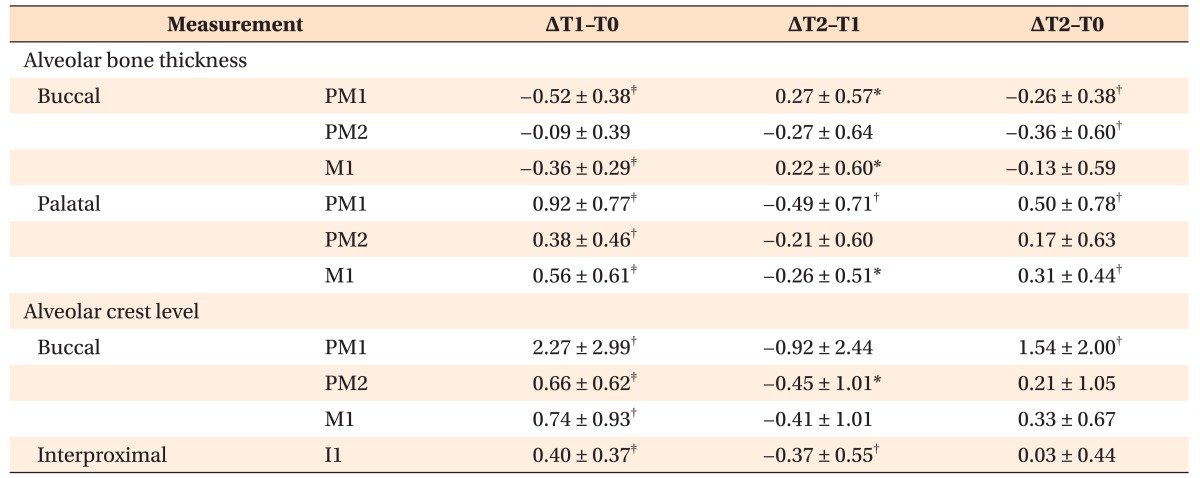
During T0–T1, the thickness of the alveolar bone at the PM1 and M1 decreased on the buccal side, while it increased on the palatal side (p < 0.001). For the buccal bone, as the thickness increased during T1–T2 (p < 0.05), it exhibited a 0.26-mm decrease at the PM1 during T0–T2 (p < 0.01), but no significant differences were observed at the M1 during T0–T2 (p > 0.05). Although the thickness of the palatal bone decreased during T1–T2 (p < 0.05), it showed an increase of 0.31–0.50 mm during T0–T2 (p < 0.01). The alveolar crest levels at the I1, PM1, PM2, and M1 moved significantly apically during T0–T1 (p < 0.01), but moved coronally during T1–T2 (p < 0.05). One year after expansion, the buccal alveolar crest level at the PM1 had moved 1.54-mm apically (p < 0.01), while that at the other teeth showed no significant movement (p > 0.05; Table 5).
Table 5. Changes in the alveolar variables before (T0), immediately after (T1), and 1 year after (T2) expansion (unit: mm).
Measurements for the alveolar bone thickness and buccal alveolar crest level were conducted on both the right and left sides for the 21 subjects, and the mean values were used.
Values are presented as the mean ± standard deviation.
I1, The central incisor; PM1 and PM2, the maxillary first and second premolars, respectively; M1, the maxillary first molar.
Paired t-tests were performed; *p < 0.05, †p < 0.01, ‡p < 0.001.
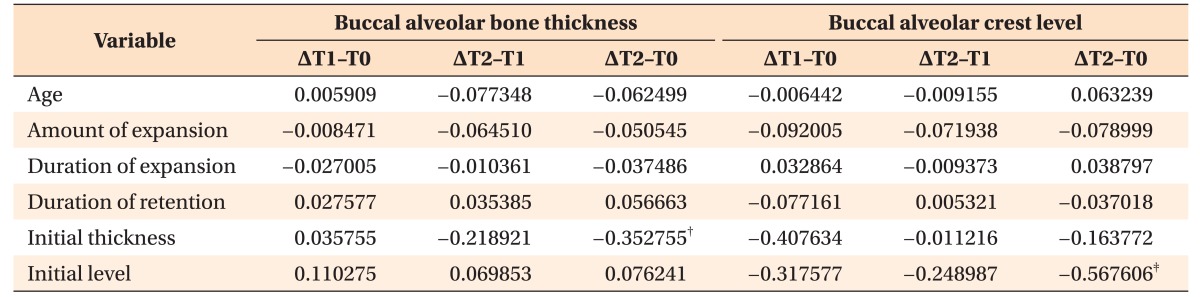
The linear mixed-effects models revealed that the changes in buccal thickness during T0–T2 were negatively affected by the initial buccal thickness (p < 0.01). The changes in buccal level during T0–T2 were negatively affected by the initial buccal level (p < 0.001; Table 6).
Table 6. Correlation coefficients using linear mixed-effects models showing factors affecting changes in the alveolar bone.
Initial thickness, Initial buccal alveolar bone thickness; initial level, initial buccal alveolar crest level.
*p < 0.05, †p < 0.01, ‡p < 0.001.
DISCUSSION
This study investigated transverse changes in various aspects of anatomical structures after MARPE and their 1-year stability in young adults. Expansion at T1 included 39.1% skeletal (nasal floor), 7.1% alveolar, and 53.8% dental expansion, while that at T2 included 43.2% skeletal, 15.0% alveolar, and 41.8% dental expansion. These percentages differed because the dental parameters exhibited a greater tendency for relapse than did the alveolar and skeletal measurements. The expansion percentages after MARPE at T2 were comparable to those previously reported after RPE (40% skeletal, 11% alveolar, and 49% dental expansion)21 but were different from those reported after SARPE (46.3% skeletal, 33.3% alveolar, and 20.4% dental expansion).22 While the M1 initially showed buccal crown tipping, followed by uprighting of the root, the alveolar bone showed buccal tipping during expansion and retention. The decrease in buccal thickness and increase in palatal thickness were 0.13–0.36 mm and 0.17–0.50 mm, respectively, which may be clinically insignificant. However, the alveolar crest at the PM1 was reduced by 1.54 mm at 1 year after the expansion, and the changes in the alveolar bone were negatively affected by the initial bone level.
Separation of the midpalatal suture was observed in subjects of the present study, who—at a mean age of 21.6 years (range, 18.25–26.75 years)—were older than those enrolled in previous tooth-borne or bone-borne RME studies.15,23 Of the 38 patients who had initially been enrolled, 5 patients (4 men and 1 woman; age range, 20.1–24.3 years) failed to exhibit opening of the midpalatal suture; this amounted to an 86.8% success rate in suture opening, similar to that reported in previous studies.11,12 A study on cadavers reported only 5% of the suture to be invisible by the age of 25 years.24 Histological and radiographic findings have revealed that the midpalatal suture begins to close in the late twenties,25 which possibly supports the data on suture opening. Moreover, the proportion of skeletal expansion at T1 (39.1%) was comparable to that previously reported in adolescents (35–40%)19,21 and after SARPE (21.5–46.3%).22,26,27 However, because of the resistance of the midpalatal and circummaxillary structures to expansion, stress would continue to accumulate until the separation of the maxillary bone, which might result in dental tipping, alveolar bending, and deformation of the appliance.19,28 Relative to the extent of appliance expansion, the lower extent of expansion of the intercusp width could be explained by the stress-induced deformation of the appliance.
The effects of MARPE were not only limited to the maxilla, but also extended to the circummaxillary structures. The maxillary halves showed buccal rotation, with the rotational center located near the frontonasal suture.15,21 The pyramidal pattern of expansion indicates buccal tipping not only of the teeth but also of the alveolar bone. On the axial plane, similar degrees of expansion were noticed at the premolars and M1, which might be due to the even distribution of the resistance from the maxilla.1 After expansion, the skeletal measurements (nasal cavity width and nasal floor width) had decreased by 23.0–29.1% (0.37–0.64 mm), which could be considered clinically insignificant, while dental measurements showed various ranges of change. During T1–T2, the intercusp widths of all the examined teeth except the canines and first premolars showed significant decreases. Several variables, such as overexpansion and subsequent alignment by comprehensive orthodontic treatment, could have affected relapse. Although the central incisors were not included in the appliance, they showed a decrease in dental measurements during T1–T2, similar to the other teeth. Bioelastic activity on the palatal soft tissue and stretching of the transseptal fibers between the teeth might have affected the decrease.29
Buccal tipping of the M1 was noticed during T0–T1, while that of the alveolar bone was noticed during T0–T2. The greater extent of buccal tipping of the tooth during T0–T1, relative to that of the alveolar bone, could explain the decrease in buccal thickness and increase in palatal thickness, as reported in previous studies.13,15 Thereafter, the tooth adopted an upright position, and the alveolar bone appeared to remodel according to the tooth position, as evident from the increase in buccal thickness, decrease in palatal thickness, and subsequent additional buccal tipping of the alveolar bone. Even though the timing of the alveolar changes is unclear, the alveolar bone seemed to change more slowly than did the tooth, which suggests that the alveolar bone underwent remodeling.17,18,30 The increase in buccal thickness and decrease in palatal thickness might be a homeostatic mechanism,31 or it might indicate the potential of bone apposition due to uncontaminated periodontal attachment to the oral cavity.32
A decrease in interproximal level was observed after not only MARPE but also SARPE.9 This might have been caused by the stretching of the transseptal fibers during expansion and their subsequent recovery to their original positions over time after the disappearance of tension.33 The decrease in buccal level after expansion might have been due to the decrease in buccal thickness.13,15 The PM1, unlike other teeth, showed a 1.5-mm vertical bone loss at 1 year after expansion, although the bone loss had been partially recovered during T1–T2. The differences in anatomical characteristics between the PM1 and M1 might underlie this change: the contour of the buccal alveolus shows superior narrowing in the PM1 area but superior widening in the M1 area.13 The findings of regression analysis revealed that the quantity of the initial alveolar bone in terms of thickness and height would influence the changes in buccal thickness and buccal level, respectively, although this analysis was performed only for the M1. Thus, the greater the initial quantity of bone present, the lesser would be the extent of alveolar bone loss.13,14
The present findings on the stability and periodontal changes after MARPE demonstrate that MARPE is an alternative to RPE or SARPE in young adults. Because bone regeneration was not observed in a previous study even at 7 months after SARPE,34 we collected the final CBCT images that were acquired at least 1 year after expansion. However, in the present study, orthodontic treatment administered during T1–T2 might have obscured the changes solely due to MARPE. In addition, 1 year might not be an adequate time period for estimation of stability. Even though gingival recession was not observed clinically, further changes should be monitored since gingival recession could occur in the presence of gingival inflammation.35 With limited numbers of patients exhibiting maxillary constriction, we could not address conventional RPE and SARPE. Future randomized clinical trials may need to comparatively evaluate the clinical efficacies of MARPE and conventional RPE or SARPE.
CONCLUSION
The null hypothesis was rejected: there were significant increases in dentoalveolar and skeletal measurements 1 year after MARPE, while buccal alveolar bone thickness and height at the first premolar decreased 1 year after MARPE. Within the limitations of this study, our results suggest that MARPE can be used as an effective tool for correcting maxillomandibular transverse discrepancies in young adults, showing stable outcomes by 1 year after expansion. However, in patients whose buccal alveolar bone in the first premolar area is thin and the alveolar crest is low before expansion, the possibility of alveolar dehiscence should be carefully monitored.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Melsen B. Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 1975;68:42–54. doi: 10.1016/0002-9416(75)90158-x. [DOI] [PubMed] [Google Scholar]
- 2.Kwak KH, Kim SS, Kim YI, Kim YD. Quantitative evaluation of midpalatal suture maturation via fractal analysis. Korean J Orthod. 2016;46:323–330. doi: 10.4041/kjod.2016.46.5.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jang HI, Kim SC, Chae JM, Kang KH, Cho JW, Chang NY, et al. Relationship between maturation indices and morphology of the midpalatal suture obtained using cone-beam computed tomography images. Korean J Orthod. 2016;46:345–355. doi: 10.4041/kjod.2016.46.6.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starnbach H, Bayne D, Cleall J, Subtelny JD. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152–164. doi: 10.1043/0003-3219(1966)036<0152:FADCRF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41–66. doi: 10.1016/0002-9416(70)90127-2. [DOI] [PubMed] [Google Scholar]
- 6.Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop. 1987;91:3–14. doi: 10.1016/0889-5406(87)90202-2. [DOI] [PubMed] [Google Scholar]
- 7.Björk A, Skieller V. Growth in width of the maxilla studied by the implant method. Scand J Plast Reconstr Surg. 1974;8:26–33. doi: 10.3109/02844317409084367. [DOI] [PubMed] [Google Scholar]
- 8.Suri L, Taneja P. Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofacial Orthop. 2008;133:290–302. doi: 10.1016/j.ajodo.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Gauthier C, Voyer R, Paquette M, Rompré P, Papadakis A. Periodontal effects of surgically assisted rapid palatal expansion evaluated clinically and with cone-beam computerized tomography: 6-month preliminary results. Am J Orthod Dentofacial Orthop. 2011;139(4 Suppl):S117–S128. doi: 10.1016/j.ajodo.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 10.Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew+assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137:830–839. doi: 10.1016/j.ajodo.2007.10.065. [DOI] [PubMed] [Google Scholar]
- 11.Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016;86:713–720. doi: 10.2319/101415-689.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park JJ, Park YC, Lee KJ, Cha JY, Tahk JH, Choi YJ. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: a cone-beam computed tomography study. Korean J Orthod. 2017;47:77–86. doi: 10.4041/kjod.2017.47.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garib DG, Henriques JF, Janson G, de Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749–758. doi: 10.1016/j.ajodo.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 14.Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–428.e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 15.Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253–262. doi: 10.2319/030514-156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenbaum KR, Zachrisson BU. The effect of palatal expansion therapy on the periodontal supporting tissues. Am J Orthod. 1982;81:12–21. doi: 10.1016/0002-9416(82)90283-4. [DOI] [PubMed] [Google Scholar]
- 17.Sarikaya S, Haydar B, Ciğer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 18.Choi YJ, Kim KH, Lee KJ, Chung CJ, Park YC. Radiographic evaluations of molar intrusion and changes with or without retention in rats. Angle Orthod. 2011;81:389–396. doi: 10.2319/060510-307.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanarsdall RL., Jr Transverse dimension and long-term stability. Semin Orthod. 1999;5:171–180. doi: 10.1016/s1073-8746(99)80008-5. [DOI] [PubMed] [Google Scholar]
- 20.Baccetti T, Franchi L, Toth LR, McNamara JA., Jr Treatment timing for Twin-block therapy. Am J Orthod Dentofacial Orthop. 2000;118:159–170. doi: 10.1067/mod.2000.105571. [DOI] [PubMed] [Google Scholar]
- 21.Kartalian A, Gohl E, Adamian M, Enciso R. Cone-beam computerized tomography evaluation of the maxillary dentoskeletal complex after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2010;138:486–492. doi: 10.1016/j.ajodo.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 22.Asscherickx K, Govaerts E, Aerts J, Vande Vannet B. Maxillary changes with bone-borne surgically assisted rapid palatal expansion: a prospective study. Am J Orthod Dentofacial Orthop. 2016;149:374–383. doi: 10.1016/j.ajodo.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 23.Gunyuz Toklu M, Germec-Cakan D, Tozlu M. Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am J Orthod Dentofacial Orthop. 2015;148:97–109. doi: 10.1016/j.ajodo.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 24.Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977;72:42–52. doi: 10.1016/0002-9416(77)90123-3. [DOI] [PubMed] [Google Scholar]
- 25.Wehrbein H, Yildizhan F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod. 2001;23:105–114. doi: 10.1093/ejo/23.2.105. [DOI] [PubMed] [Google Scholar]
- 26.Goldenberg DC, Goldenberg FC, Alonso N, Gebrin ES, Amaral TS, Scanavini MA, et al. Hyrax appliance opening and pattern of skeletal maxillary expansion after surgically assisted rapid palatal expansion: a computed tomography evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:812–819. doi: 10.1016/j.tripleo.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 27.Zandi M, Miresmaeili A, Heidari A. Short-term skeletal and dental changes following bone-borne versus tooth-borne surgically assisted rapid maxillary expansion: a randomized clinical trial study. J Craniomaxillofac Surg. 2014;42:1190–1195. doi: 10.1016/j.jcms.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 28.Isaacson RJ, Ingram AH. Forces produced by rapid maxillary expansion. II. Forces present during treatment. Angle Orthod. 1964;34:261–270. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Storey E. Tissue response to the movement of bones. Am J Orthod. 1973;64:229–247. doi: 10.1016/0002-9416(73)90017-1. [DOI] [PubMed] [Google Scholar]
- 30.Choi YJ, Kim KH, Lee KJ, Chung CJ, Park YC. Histomorphometric evaluation of maxillary molar roots and surrounding periodontium following molar intrusion in rats. Orthod Craniofac Res. 2015;18:12–20. doi: 10.1111/ocr.12054. [DOI] [PubMed] [Google Scholar]
- 31.Wehrbein H, Fuhrmann RA, Diedrich PR. Periodontal conditions after facial root tipping and palatal root torque of incisors. Am J Orthod Dentofacial Orthop. 1994;106:455–462. doi: 10.1016/S0889-5406(94)70067-2. [DOI] [PubMed] [Google Scholar]
- 32.Grzesik WJ, Narayanan AS. Cementum and periodontal wound healing and regeneration. Crit Rev Oral Biol Med. 2002;13:474–484. doi: 10.1177/154411130201300605. [DOI] [PubMed] [Google Scholar]
- 33.Kanzaki R, Daimaruya T, Takahashi I, Mitani H, Sugawara J. Remodeling of alveolar bone crest after molar intrusion with skeletal anchorage system in dogs. Am J Orthod Dentofacial Orthop. 2007;131:343–351. doi: 10.1016/j.ajodo.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 34.Angeletti P, Pereira MD, Gomes HC, Hino CT, Ferreira LM. Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e38–e46. doi: 10.1016/j.tripleo.2009.10.043. [DOI] [PubMed] [Google Scholar]
- 35.Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14:121–129. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]