Abstract
Background
Timely access to emergency contraception has the potential to reduce the number of unwanted pregnancies and subsequent abortions. A public health policy initiative in British Columbia beginning in December 2000 allowed pharmacists to provide emergency contraceptives (ECs) without a prescription. We sought to determine changes in EC use after the policy was introduced and to analyze EC use with data generated by the policy.
Methods
All Ovral, Preven and Plan B EC prescriptions from Jan. 1, 1996, to Dec. 31, 2003, were identified through the BC PharmaNet and Medical Services Plan administrative databases and the data analyzed to determine changes between 1996 and 2002. Changes over time were determined in the frequency of EC provision, choice of EC agent, frequency of EC use by age group, repeat use and geographic distribution of EC prescription for the pre- and post-policy periods. Anonymized patient-specific data from treatment consent forms were used to describe the reason for EC use, interval between unprotected intercourse and EC prescription, proportion prescribed for immediate or future use, referrals for regular birth control and STD screening and concomitant antiemetic use. Consent data also provided the time in the menstrual cycle that the EC was requested.
Results
The number of EC prescriptions increased from a pre-policy mean of 8805 (99% confidence interval 7823–9787) in the years 1996 to 2000 to a post-policy total in 2002 of 17 794. Physicians prescribed the levonorgestrel regimen (Plan B) less frequently than did pharmacists. The frequency of EC use was highest among women aged 20–24 years across all study years, and all age groups demonstrated a post-policy increase in use. On average, 2.1% of the women received an EC 3 or more times a year over the period of the study. More women in urban regions received ECs than women in more rural areas of the province. Analysis of pharmacist treatment consent forms used in 2001 and 2002 showed that 56.2% of women receiving an EC reported using a method of birth control that had failed, 55.7% of pharmacist-provided ECs were obtained within 24 hours after unprotected intercourse, 1.1% of ECs were obtained for future use, antiemetics were provided to 57.7% of women receiving the Yuzpe regimen (Ovral, Preven) and to 20.5% of women receiving levonorgestrel, and women tended to seek ECs when unprotected intercourse occurred at the time of highest risk of pregnancy in their menstrual cycle. Women in greatest financial need obtained ECs more frequently from physicians than from pharmacists.
Interpretation
The policy change that granted pharmacists authority to provide ECs to women without a physician's prescription did not simply expand EC availability but was associated with an overall increase in EC use in the province.
Unwanted pregnancy is a worldwide social and health concern that frequently results in therapeutic abortion.1 In 2001, almost 13 700 abortions were performed in British Columbia, representing more than 23% of all pregnancies and 58% of pregnancies among women aged 15–19 years.2 Postcoital hormonal emergency contraception has the potential to substantially reduce the risk of pregnancy and subsequent abortion when taken as early as possible after unprotected intercourse.3,4
Despite evidence for the effectiveness and safety of emergency contraceptives (ECs),3,5,6,7 this method of preventing pregnancy is underused.8 Barriers include lack of knowledge,9,10 reluctance of young women to request medication from their physicians,11 denial of pregnancy risk12 and lack of timely access to physicians or family planning clinics.13 As the effectiveness of emergency contraception is time-dependent, convenient prescription and dispensing mechanisms are crucial to enabling its use.
To increase access to ECs, in December 2000 British Columbia became the first province to grant independent prescriptive authority to specially trained pharmacists, enabling them to provide emergency contraception without a physician's prescription.14 Our aim was to determine whether granting prescriptive authority to pharmacists would result in women obtaining ECs from pharmacists instead of their physicians, and whether the number of overall EC prescriptions would increase.
Methods
A population-based cohort study was performed among women 10–59 years of age who received EC prescriptions from 1996 to 2002. In 2001, 1.4 million women were in this age group (total BC population 3.9 million).15 British Columbia has a universal-access, publicly funded health care system with coverage of medical and hospital services and a combination of private and third-party payment for prescription drugs.
Data were obtained from 2 linkable administrative databases maintained by the BC Ministry of Health Services, PharmaNet (retail pharmacy prescriptions) and Medical Services Plan (physician reimbursement claims). Use of a unique anonymized patient identifier allowed linkage of the health care records. Using the drug identification number, PharmaNet records were obtained for Ovral, the most commonly used agent for the Yuzpe regimen (a combination of estrogen and progestin), Preven (available from November 1999 to February 2001) and Plan B (available from December 2000). Data were collected for the period Jan. 1, 1996, to Dec. 31, 2003.
PharmaNet-derived records contained the anonymous patient identifier, year of birth, drug identification number, local health area of the person, the pharmacy, prescription date, generic and brand name of the drug, strength and dosage form, quantity and physician or pharmacist prescriber code. EC records were linked to the Medical Services Plan files to obtain ICD-10 diagnostic codes,16 year and month of birth, sex, subsidy code,17 service date, service provider, specialty code, local health area and service location code.
An algorithm was developed to exclude potential non-EC prescriptions for Ovral using patterns of physician billing codes, quantities of tablets dispensed and patterns of refills (Fig. 1). This algorithm was validated by applying the criteria to Ovral prescriptions initiated by pharmacists. Potential coding errors (steps 3, 4, 7 and 8) were infrequent (< 0.4%), as established by pharmacist exclusions for these steps. The chance occurrence of a physician visit in the 7 days before an EC prescription for an excluded Medical Services Plan code event was uncommon (step 5), as were linked prescriptions over the following 12 months (step 6). Thus, the physician and pharmacist Ovral exclusions in steps 5 and 6 would appear to be related to alternate gynecologic indications for Ovral and therefore appropriate to exclude. In step 7, multiple-month (e.g., 42s, 63s) supplies of Ovral 21s constituted almost all of the excluded physician prescriptions. In step 8, repeat prescriptions for Ovral 21s that were excluded were usually for 2 or more consecutive months, and thus non-emergency contraception indications were likely. Overall, the error rate in understating emergency contraception use of Ovral was low (< 3.7%). The algorithm was used to determine EC prescription numbers for each year of the study.
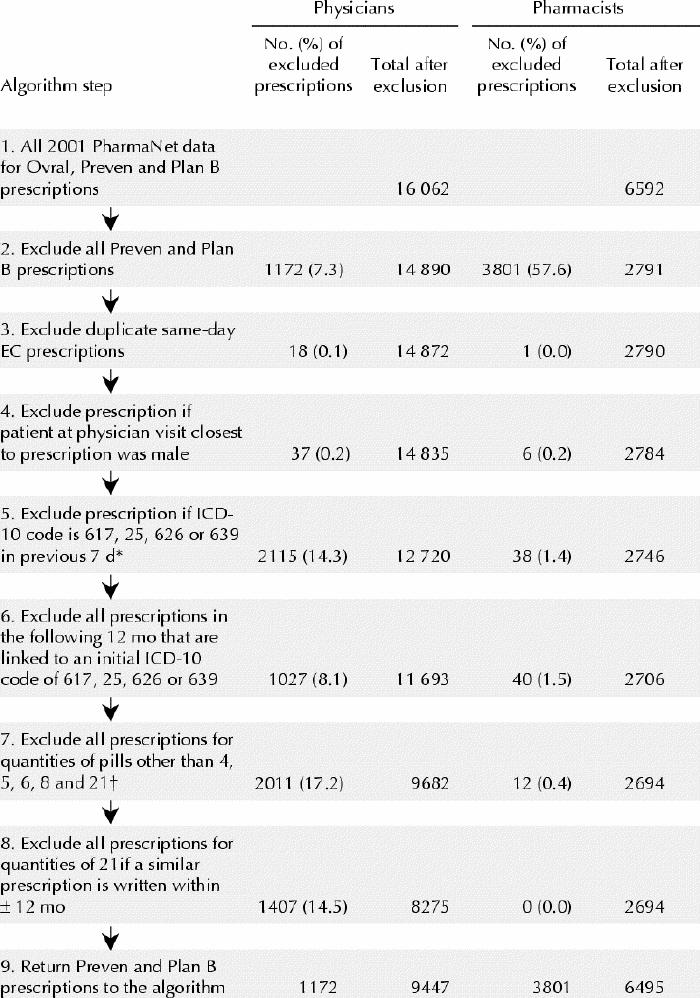
Fig. 1: Algorithm used to exclude potential non-EC prescriptions for Ovral. Data for 2001 are presented here and were used to validate the algorithm. *ICD-10 codes for which Ovral is prescribed for non-EC indications: 617 (endometriosis), 625 (pain and other symptoms associated with female genital organs), 626 (disorders of menstruation and other abnormal uterine bleeding) and 639 (complication following abortion or ectopic or molar pregnancy). †These quantities are commonly associated with EC use: 4 represents 1 treatment, 5–6 include additional pills in case of vomiting, 8 represents 2 treatments and 21 for immediate and future use.
For pharmacists to provide emergency contraception, the BC College of Pharmacists of British Columbia required completion of a standardized 4-hour emergency contraception training program.18 Pharmacists were trained to advise women on the effectiveness, side effects and costs of the Yuzpe regimen (Ovral, Preven) and levonorgestrel (Plan B) (progestin only). Emergency contraception could be provided for immediate or future use.
During 2001–2002, women of any age who met the criteria for emergency contraception completed a 10- to 15-minute confidential, standardized pharmacist–patient interview and treatment consent form. Information provided by the women included whether the emergency contraception was for immediate or future use, time since onset of the last menstrual cycle, time of unprotected intercourse and age. Pharmacists documented on the consent form the date and time of dispensing, pharmacy code, pharmacist identifier, type of EC agent and whether an antiemetic was provided. Pharmacists also noted referrals made for long-term birth control, for STD screening and to other community resources. Women were advised the prescription would be entered on their PharmaNet profile. The anonymized consent was faxed to the College of Pharmacists, and copies were subsequently provided to the investigators. Approval was granted by the University of British Columbia Clinical Research Ethics Board.
Frequency of EC use standardized per 1000 women per 5-year age group was based on BC Health Data Warehouse data.19 PharmaNet 2003 data were used in the algorithm to evaluate the 12-month period after 2002 EC prescriptions.
Results
Pre-policy, physicians prescribed an average of 8805 (99% confidence interval [CI] 7823–9787) ECs yearly; post-policy, physicians prescribed 9447 ECs in 2001 and 10 669 in 2002. In 2001 and 2002, pharmacists provided 6592 and 7125 ECs, respectively, for a combined total of 16 039 and 17 794 ECs in 2001 and 2002 respectively. Thus, by 2002, the number of ECs received by women had increased by 102% relative to the 5-year pre-policy mean. The mean age of EC users was similar across all study years: pre-policy 24.9 (standard deviation [SD] 7.2) years and post-policy 25.5 (SD 7.4) years for physician prescriptions and 26.0 (SD 7.6) years for pharmacy-provided ECs.
In 2001 pharmacists provided the levonorgestrel agent, Plan B, to a larger proportion of women than did physicians (Fig. 2). In 2002 the frequency of levonorgestrel provision had increased for both pharmacists and physicians, to 63.9% and 32.4% respectively.
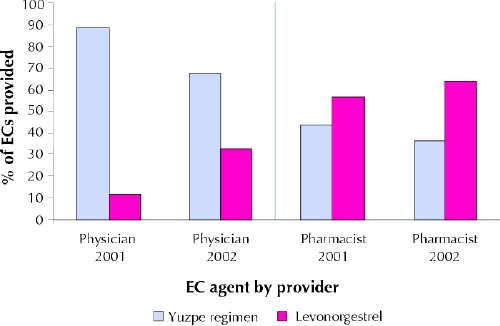
Fig. 2: Comparison of EC prescriptions for the Yuzpe regimen (Ovral or Preven) and levonorgestrel (Plan B) by type of provider in 2001–2002 in British Columbia.
Women prescribed ECs by physicians paid the drug cost and dispensing fee, and Medical Services Plan paid for physician office visits; women provided ECs by pharmacists paid the drug cost, dispensing fee and, in most cases, an additional $25 counselling fee. Women who were in greatest financial need, as indicated by eligibility for a 100% Medical Services Plan premium or 100% social services subsidy, visited physicians more frequently than pharmacists for emergency contraception (33.6% v. 21.5%). More women in urban regions received emergency contraception than women in rural areas (data not shown).
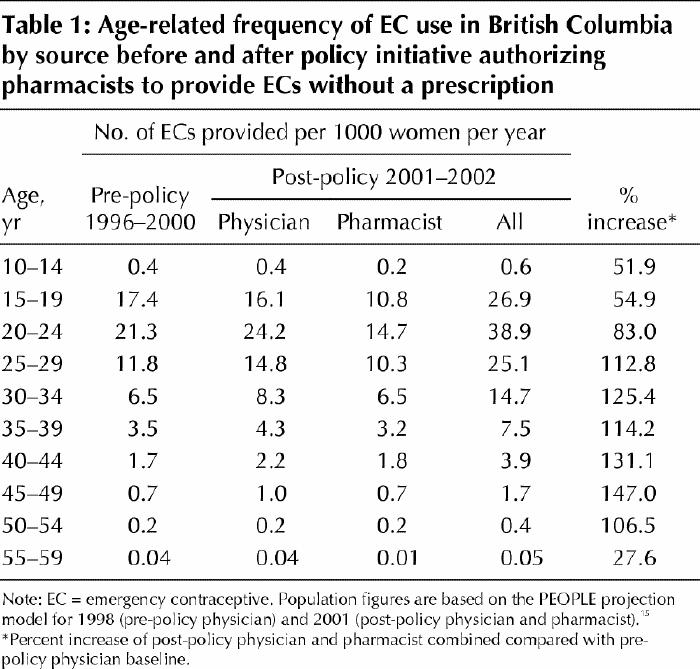
Frequency of EC use per 1000 women varied by age group, with highest rates for women aged 20–24, followed by women aged 15–19 and 25–29 years (Table 1). All groups demonstrated post-policy increases in the number of EC prescriptions, with an increase 2-fold or greater among women aged 25–54 years.
Table 1
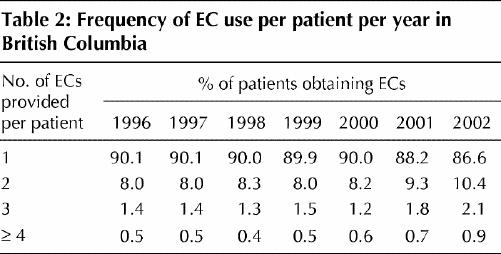
Repeat EC use was infrequent, as a mean of only 2.1% of EC users received emergency contraception 3 or more times during the study period (Table 2).
Table 2
Consent forms were available for 96.1% (13 178/13 717) of pharmacist-provided EC prescriptions in PharmaNet. According to the consent data, 56.2% of the women reported that a method of birth control had been used but had failed (90.3% reported condom failure, 7.9% erratic oral contraceptive use and 1.8% other forms of contraception failure).
In 55.7% of cases, women obtained ECs from pharmacists within 24 hours after unprotected intercourse, and 86.8% and 98.2% received ECs within 48 and 72 hours respectively. Women requesting ECs within the first 24 hours were more likely to have experienced failure of a method of birth control than women requesting ECs after 96 hours (59.0% v. 41.7%).
Pharmacists provided emergency contraception for future use to 1.1% of EC users, often with a prescription for immediate use. Pharmacists gave referrals for long-term birth control to 35.3% of EC users and for STD screening to 3.2%. Referrals to other community resources were provided to an additional 5.2%. Antiemetics were provided to 57.7% of women receiving the Yuzpe regimen and to 20.5% of women receiving levonorgestrel.
Women tended to seek emergency contraception on menstrual cycle days clustered around the time of highest risk of pregnancy, although emergency contraception was also requested both early (≤ day 5) and late (≥ day 28) in the cycle (Fig. 3) by women with erratic menstrual cycles. On the basis of time since onset of the last menstrual cycle reported by 11 830 of the women who received emergency contraception from pharmacists in 2001 and 2002, we estimated that 550 pregnancies would have been expected among the 13 717 women who received ECs from pharmacists in those 2 years.20
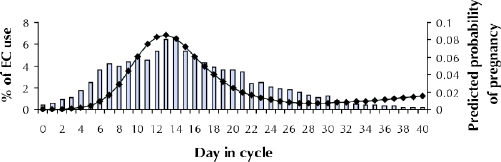
Fig. 3: Predicted probability of pregnancy (diamonds) and percent of EC use (bars) by day in menstrual cycle.
Interpretation
The emergency contraception public health initiative did not merely expand EC availability through pharmacists provision; the total yearly number of ECs received by women more than doubled by the second year of the new policy. Our findings suggest that pharmacist provision increased the number of EC prescriptions by increasing access through the extended hours of operation of pharmacies and the higher number of locations from which to obtain ECs. In light of the guideline of the Society of Obstetricians and Gynaecologists of Canada21 published in 2000 that suggests that levonorgestrel is more effective and causes fewer side effects than the Yuzpe regimen, it is of interest that physicians prescribed levonorgestrel 4 times less frequently than the Yuzpe regimen. This may reflect the lag time in disseminating information on the relative effectiveness and availability of Plan B or physicians' concern about drug costs for their patients. Women who obtained ECs from physicians were more likely to have a 100% subsidy code than women obtaining ECs from pharmacists. It is noteworthy that about 40% of women chose to receive the Yuzpe regimen from pharmacists despite being informed that it is possibly less effective than levonorgestrel and likely causes more side effects. The lower cost of the Yuzpe regimen may be partly responsible.
EC provision increased more among women aged 25–29 years than among those 15–19 years, despite similar abortion rates for the two groups.2 Lack of public awareness materials and media attention specifically tailored for teens may have hampered widespread dissemination of information about emergency contraception. Repeat use of ECs was infrequent, a finding similar to that in a British study, in which only 4% of women used ECs 3 or more times in a year.22 Improving access to reproductive choices for women in rural and remote communities was a key reason for the BC initiative, and our findings suggest that EC prescriptions increased substantially in those areas. Although 56% of women requested emergency contraception for condom or other birth control method failure, only 1% requested ECs for future use. Since women with ECs at home can use the agent as soon as they recognize the risk of pregnancy,23,24 a public health promotion regarding the benefits of having ECs for potential future use may be warranted. When providing ECs, pharmacists used the opportunity to give referrals for long-term birth control and screening for STDs when necessary. Consent data suggested that women were able to independently assess when they were likely at highest risk of unintended pregnancy. It is important for clinicians and patients to be aware that women with erratic menstrual cycles continue to be at risk of pregnancy late in their cycle.20
EC prescriptions in PharmaNet likely understated emergency contraception use for 2 reasons. First, our algorithm determining Ovral prescriptions for emergency contraception was conservative. Although some actual EC prescriptions may have been miscoded, associated by chance with an ICD-10 code suggesting non-EC use or prescribed in nonstandard quantities and excluded, the error rate in underestimating EC prescription use of Ovral was low (≤ 3.7%). Second, emergency contraception is available in British Columbia from alternate sources such as emergency departments, Options for Sexual Health Planned Parenthood, and youth and walk-in clinics, which are not recorded in the PharmaNet database. We are currently attempting to evaluate the magnitude of such EC provision in the province.
Timely access to emergency contraception has the potential to reduce unwanted pregnancies and subsequent abortions. Pharmacists are knowledgeable health care professionals who are readily accessible by patients, and these population-based data suggest that the BC public health initiative authorizing pharmacists to provide ECs was indeed associated with an overall increase in emergency contraception access among women in the province. The potential availability of behind-the-counter levonorgestrel on a nation-wide basis25 is promising, if reimbursement issues are carefully considered and proactively addressed so that cost barriers do not inadvertently reduce EC access for those who cannot afford to pay the full costs. Further research evaluating the cost-effectiveness and comparative effectiveness of the Yuzpe regimen and levonorgestrel under conditions of usual care will also be beneficial.
Acknowledgments
We would like to sincerely thank Selena Santi for her assistance with data coordination and analyses, and Pat McCrea of Bluethorn Research & Analysis for data management and analytic support with the BC administrative databases. We would also like to acknowledge the expert panel advising on non-EC indications for Ovral: Drs. Jerilynn Prior, Timothy Rowe, Barry Sanders and Petra Selke. We would like to thank our Advisory Steering Committee for ongoing advice and support, who, in addition to the authors, were: Dr. Perry Kendall, Provincial Health Officer; Ms. Tessa Graham, Executive Director, Healthy Children, Women & Seniors, BC Ministry of Health Services; Dr. Elizabeth Whynot, President, BC Women's Hospital and Health Centre; Dr. Roey Malleson, Medical Director, Youth Health Program, Head Division of Adolescent Medicine, Children's & Women's Health Centre of BC; Dr. Lorraine Greaves, Executive Director, BC Centre of Excellence for Women's Health; Greg Smith, Executive Director, Options for Sexual Health (Planned Parenthood); Barbara Hestrin, Director, CARE Program, BC Women's Hospital; Dr. Jacqueline Gardner, Professor, School of Pharmacy, University of Washington. The authors would also like to recognize all EC-trained pharmacists in British Columbia who so diligently contributed to this public health initiative.
Footnotes
This article has been peer reviewed.
Contributors: Judith Soon and Marc Levine contributed substantially to the conception and design of the study, interpretation of data, and also drafted the manuscript. Brenda Osmond was responsible for data acquisition and quality control of treatment consent data and contributed to the writing of the manuscript. Mary Ensom and David Fielding contributed to the conception and design of the study, as well as to the writing of the manuscript. All authors revised the article critically for important intellectual content and approved the version to be published.
This study was supported by grants from the British Columbia Ministry of Health Services, the British Columbia Medical Services Foundation and the Pharmacy Access Partnership funded by the David and Lucile Packard Foundation. Access to data was granted by the BC Ministry of Health Services.
Competing interests: None declared.
Correspondence to: Dr. Judith A. Soon, Collaboration for Outcomes Research and Evaluation, Faculty of Pharmaceutical Sciences, University of British Columbia, 2146 East Mall, Vancouver BC V6T 1Z3; fax 604 859-4345; jsoon@interchange.ubc.ca
References
- 1.Jones RK, Darroch JE, Henshaw SK. Contraceptive use among US women having abortions in 2000–2001. Perspect Sex Reprod Health 2002;34:294-303. [PubMed]
- 2.BC Vital Statistics Agency. Pregnancy rates by health authority: British Columbia, 1993 to 2001. Victoria, BC: British Columbia Vital Statistics Agency; 2003.
- 3.Task Force on Postovulatory Methods of Fertility Regulation. Randomised controlled trial of levonorgestrel versus the Yuzpe regimen of combined oral contraceptives for emergency contraception. Lancet 1998;352:428-33. [PubMed]
- 4.Piaggio G, von Hertzen H, Grimes DA, Van Look PFA. Timing of emergency contraception with levonorgestrel or the Yuzpe regimen. Task Force on Postovulatory Methods of Fertility Regulation. Lancet 1998;353:721. [DOI] [PubMed]
- 5.Norris Turner A, Ellertson C. How safe is emergency contraception? Drug Safety 2002;25:695-706. [DOI] [PubMed]
- 6.Vasilakis C, Jick SS, Jick H. The risk of venous thromboembolism in users of postcoital contraceptive pills. Contraception 1999;59:79-83. [DOI] [PubMed]
- 7.Glasier A. Safety of emergency contraception. J Am Med Womens Assoc 1998;53(5 Suppl 2):219-21. [PubMed]
- 8.Trussell J, Ellertson C, Stewart F, Raymond EG, Shochet T. The role of emergency contraception. Am J Obstet Gynecol 2004 Apr;190(4 Pt 2):S30-S38. [DOI] [PubMed]
- 9.Blanchard K. Improving women's access to emergency contraception: Innovative information and service delivery strategies. J Am Med Womens Assoc 1998;53(5 Suppl 2):238-41. [PubMed]
- 10.Delbanco S, Stewart F, Koenig J, Parker ML, Hoff T, McIntosh M. Are we making progress with emergency contraception? Recent findings on American adults and health professionals. J Am Med Womens Assoc 1998;53(5 Suppl 2):242-6. [PubMed]
- 11.Blanchard K, Bungay H, Furedi A, Sanders L. Evaluation of an emergency contraception advance provision service. Contraception 2003;67:343-8. [DOI] [PubMed]
- 12.Glasier A, Fairhurst K, Wyke S, Ziebland S, Seaman P, Walker J, et al. Advanced provision of emergency contraception does not reduce abortion rates. Contraception 2004;69:361-6. [DOI] [PubMed]
- 13.Webb A. Emergency contraception: Is it time to change method? BMJ 1999;318:342-3. [DOI] [PMC free article] [PubMed]
- 14.Soon JA, Levine M, Ensom MHH, Gardner JS, Edmondson HM, Fielding DW. The developing role of pharmacists in patient access to emergency contraception. Dis Manage Health Outcomes 2002;10:601-11.
- 15.BC Ministry of Management Services. Population of BC — P.E.O.P.L.E. 28: Population estimates and projections. 1998 and 2001. Victoria: BC Ministry of Health Service; 2003.
- 16.World Health Organization. International statistical classification of diseases and related health problems. 10th rev. Geneva: The Organization; 1992.
- 17.Medical Services Plan, BC Ministry of Health Services. MSP premiums. Available at: www.healthservices.gov.bc.ca/msp/infoben/premium.html (accessed 2005 Feb 8).
- 18.Soon JA, Levine M, Osmond BL, Ensom MHH, Fielding DW. Provision of emergency contraceptives by pharmacists. Can Pharm J 2004;137(6):23-9.
- 19.2001 Census statistics; semi-custom area profile. British Columbia. Victoria: BC Ministry of Health Services; 2002.
- 20.Trussell J, Ellertson C, von Hertzen H, Bigrigg A, Webb A, Evans M, et al. Estimating the effectiveness of emergency contraceptive pills. Contraception 2003;67:259-65. [DOI] [PubMed]
- 21.Davis V, Dunn S. Emergency postcoital contraception. Clinical Practice Gynaecology and Social Sexual Issues Committees. Society of Obstetricians and Gynaecologists of Canada. Emergency contraception. J Obstet Gynaecol Can 2000;92:544-8.
- 22.Rowlands S, Lawrenson R, Logie J, Ineichen B. Repeated use of hormonal emergency contraception by younger women in the UK. Br J Fam Plann 2000;26(3):138-43. [DOI] [PubMed]
- 23.Glasier A, Baird D. The effects of self-administering emergency contraception. N Engl J Med 1998;339(1):1-4. [DOI] [PubMed]
- 24.Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, et al. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs: a randomized controlled trial. JAMA 2005;293:54-62. [DOI] [PubMed]
- 25.Health Canada Therapeutics Products Directorate. Amendment—Levonorgestrel—Schedule 1272. Request for stakeholder comments. Ottawa: Health Canada; 2004 May 22. Available at: www.hc-sc.gc.ca/hpfb-dgpsa/tpd-dpt/sch-1272_e.html (accessed 2005 Feb 8).


