Abstract
NONALCOHOLIC FATTY LIVER DISEASE is emerging as the most common chronic liver condition in the Western world. It is associated with insulin resistance and frequently occurs with features of the metabolic syndrome. Disease presentation ranges from asymptomatic elevated liver enzyme levels to cirrhosis with complications of liver failure and hepatocellular carcinoma. Current treatment recommendations are limited to weight loss and exercise, although several promising medications are on the horizon. In this article we discuss the etiology, pathogenesis and diagnosis of nonalcoholic fatty liver disease as well as approaches to its management.
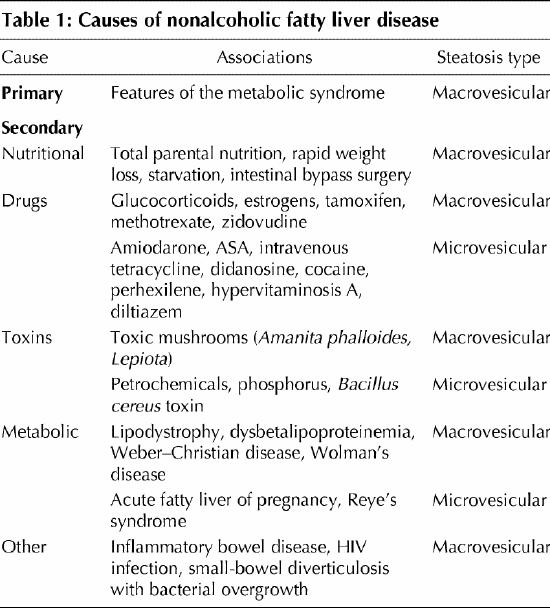
The diagnosis of nonalcoholic fatty liver disease (NAFLD) requires evidence of fatty changes in the liver in the absence of a history of excessive alcohol consumption. The histologic spectrum of NAFLD spans from generally benign, bland steatosis to steatosis with evidence of hepatocellular inflammation and damage (nonalcoholic steatohepatitis, or NASH), which may be complicated by progressive fibrosis and cirrhosis. NAFLD can be primary or secondary depending on the cause (Table 1). Secondary causes require exclusion, as these conditions have different prognoses and treatment.1 In this review we focus on primary NAFLD and discuss the current knowledge of the pathophysiology and natural history of NAFLD, appropriate management strategies and emerging treatment options.
Table 1
Epidemiology
Hepatic steatosis detected by magnetic resonance spectroscopy is found in 31% of adults in the United States2 and in 33% of potential live liver donors undergoing liver biopsy.3 Ultrasonography detects fatty changes in the liver in 12.9%–16.4% of individuals.4,5,6 The prevalence of steatosis tends to be higher among males6,7,8 and in certain ethnic groups (e.g., up to 45% of Hispanic people).2 Prevalence increases with age, from 2.6% among children to 26% among people 40–59 years old.5,9
NAFLD is more frequent among people with diabetes (50%) and obesity (76%), and it is almost universal among diabetic people who are morbidly obese.4,10,11 Obesity, diabetes and the metabolic syndrome are also risk factors for NASH and for advanced fibrosis on liver biopsy.12,13,14 NASH is present in 18.5% of obese subjects (compared with 2.7% of lean individuals) and in 50% of severely obese people with diabetes.15,16 The metabolic syndrome confers an odds ratio (OR) for NASH of 3.2 (95% confidence interval [CI] 1.2– 8.9) and an OR for advanced fibrosis of 3.5 (95% CI 1.1– 11.2).17 Among people who are not obese and do not have diabetes, risk factors for NAFLD are impaired fasting glycemia (OR 2.8, 95% CI 1.5– 5.20), hypertriglyceridemia (OR 2.8, 95% CI 2.0– 4.0), hyperuricemia (OR 2.6, 95% CI 1.6– 4.1), central obesity (OR 2.4, 95% CI 1.7– 3.4), hypertension (OR 1.7, 95% CI 1.2– 2.4) and low levels of high-density lipoprotein (HDL) cholesterol (OR 1.4, 95% CI 11.0– 2.0).18
Pathogenesis
The liver plays a central role in lipid metabolism, importing serum free fatty acids and manufacturing, storing and exporting lipids and lipoproteins. However, the pathophysiology that leads to NAFLD is not well understood; in particular, the factors that lead to progressive hepatocellular damage after triglyceride accumulation are not well elucidated. It appears that alteration of local and systemic factors (particularly insulin resistance) that control the balance between the influx or synthesis of hepatic lipids and their export or oxidation leads to hepatic triglyceride accumulation. The steatotic liver is then thought to be vulnerable to secondary insults, which lead to hepatocellular inflammation and fibrosis. A variety of factors have been implicated to produce a second “hit,” including hormones derived from adipose tissue (adipocytokines), oxidative stress and gut-derived bacterial endotoxin.19
Insulin resistance
The pathogenesis of insulin resistance is complex and is likely to involve many genetic polymorphisms that influence insulin secretion and action as well as environmental factors that promote obesity and immobility.20 Hyperinsulinemia increases serum free fatty acid levels, which are taken up by the liver and drive triglyceride production and hepatic steatosis (Fig. 1).21 In addition, chronic hyperinsulinemia promotes de novo hepatic lipogenesis through upregulation of lipogenic transcription factors21,22,23 and may activate profibrotic cytokines such as connective tissue growth factor.24
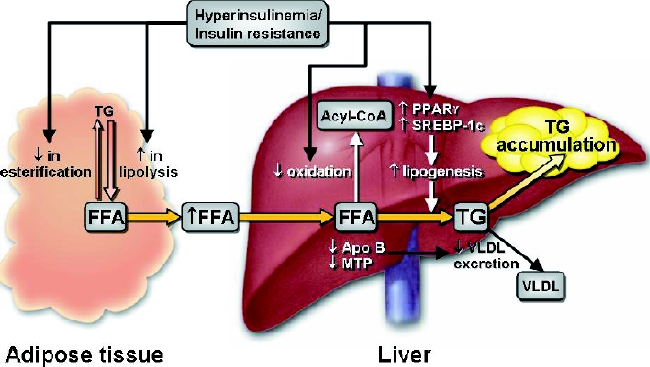
Fig. 1: Development of nonalcoholic hepatic steatosis. Insulin resistance enhances triglyceride (TG) lipolysis and inhibits esterification of free fatty acids (FFA) within adipose tissue. The result is increased serum FFA levels, which are taken up by the liver. Hepatic TG synthesis is driven by the increased influx of FFA and favoured by insulin upregulated lipogenic transcription factors, such as peroxisome proliferator-activated receptor gamma (PPARγ) and sterol regulatory element binding protein (SREBP)-1c. Alternative metabolism of FFA by oxidation is inhibited by insulin. TG export via very-low-density lipoproteins (VLDL) may be inhibited by decreased synthesis of apolipoprotein B (apo B) or reduced incorporation of TG with apo B by microsomal triglyceride transfer protein (MTP). See the animated figure at www.cmaj.ca/cgi/content/full/172/7/899/DC1. Photo: Mayo Clinic
Hepatic lipid metabolism
Lipids are normally exported from the liver in very-low-density lipoproteins (VLDL), which are formed by microsomal triglyceride transfer protein (MTP) incorporating triglyceride into apolipoprotein B (apo B). A reduction in MTP activity and apo B synthesis and secretion may impair hepatic lipid export and favour hepatic triglyceride accumulation.25,26,27,28
Inflammatory and fibrotic mediators in NAFLD
Adipocytokines (tumour necrosis factor-α [TNF-α], leptin and adiponectin), free fatty acids, mitochondrial dysfunction, bacterial endotoxin and vascular disturbance have all been implicated in the development of hepatic inflammation and fibrosis in patients with NAFLD.29,30,31,32,33 These factors may be directly hepatotoxic or generate oxygen radicals with subsequent lipid peroxidation, cytokine induction and liver damage.19
TNF-α promotes insulin resistance and liver inflammation. Levels are increased in patients with NAFLD, perhaps secondary to gut-derived endotoxin or TNF-α polymorphisms.28,31,34,35,36 Leptin and adiponectin are important regulators of adiposity and insulin resistance and have been found to promote liver fibrogenesis in animal models.30,37,38,39 Leptin and adiponectin levels are altered in patients with NASH; however, their exact pathogenic role has yet to be elucidated.31,40
As a result of insulin resistance, serum free fatty acid levels are increased in NASH patients and may be directly hepatotoxic or produce damaging reactive oxygen species.23,32,33 Oxidative stress may be exacerbated further by ultrastructural mitochondrial lesions, which impair respiratory chain function.23,33
As liver injury progresses, fat-laden hepatocytes and perisinusoidal fibrosis may impair microvascular hepatic blood flow. This effect may decrease oxygen and nutrient exchange and thus stimulate a microvascular inflammatory response and an escalating cycle of liver damage and vascular insufficiency.41,42
Natural history
The natural history of NAFLD has been examined in relatively small numbers of select patients, and thus the evolution of the disease in the general population is not well defined. However, patients who have NAFLD appear to have a higher mortality than people in the general population.43 Patients with pure steatosis have a benign prognosis: follow-up of 198 patients for up to 21 years revealed progression to cirrhosis in 3 patients and liver-related death in only 1.44,45,46 In contrast, up to 11% of NASH patients may die of liver-related causes.45 Diabetes is a risk factor for fibrosis progression and for overall and liver-related death among NAFLD patients.47,48
Many patients with cryptogenic cirrhosis have metabolic risk factors for NAFLD and are likely to represent cases of previously unrecognized NAFLD,49,50 particularly because hepatic steatosis may disappear with the development of cirrhosis.48,51 NAFLD may also present as cirrhosis complicated by hepatocellular carcinoma: at least 13% of cases of hepatocellular carcinoma were attributable to NASH in one study.52 Overall, fibrosis progression in patients with NAFLD appears to be slow: in previous studies, it took several decades for cirrhosis, hepatocellular carcinoma and liver decompensation to develop in a small proportion of patients with NASH.48,51,53
Clinical features
NAFLD is usually asymptomatic, although fatigue and discomfort in the right upper quadrant of the abdomen may be reported.51 The majority (56%–79%) of patients are overweight (body mass index [BMI] > 25 kg/m2), and one-third have the metabolic syndrome.17,54,55 Lean patients (BMI 25 kg/m2) usually have at least one metabolic risk factor.17 Hepatomegaly may be present, although signs of chronic liver disease are uncommon.51,56
Liver enzyme levels in NAFLD patients fluctuate, normal values being present in up to 78% of patients at any one time.57,58 When levels are elevated, the increase is mild and often restricted to one or both of alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The AST:ALT ratio is usually less than 1, although it may reverse in the presence of cirrhosis.59 Liver enzyme levels do not reliably correlate with liver histology, and the full range of disease may be seen in patients with NAFLD who have normal transaminase levels.12,51
Ferritin levels are increased in 20%–50% of patients, and elevated transferrin saturation (> 55%) is present in 5%– 10%.13,55,60 Autoantibodies are identified in 23%–36% of NAFLD patients and are associated with more advanced fibrosis.61,62
Diagnosis
Imaging
Ultrasonography and CT and MRI scanning are reliable for detecting moderate to severe fatty changes in the liver. Hepatic fat causes increased echogenicity on ultrasound, compared with the lower echogenicity of the spleen or renal cortex. In noncontrast CT scans, the fatty liver is hypodense and appears darker than the spleen. Hepatic vessels give the appearance of being relatively brighter and can be mistaken for contrast injection. No imaging method is able to distinguish between simple steatosis and NASH or indicate the stage of fibrosis.63 The sensitivity and specificity of ultrasonography for detecting fatty infiltration decreases as BMI increases and thus varies from 49% to 100% and from 75% to 95% respectively.63,64,65 The sensitivity of each imaging method increases with the degree of fatty infiltration, with at least 33% steatosis being optimal for detection.63
Liver biopsy
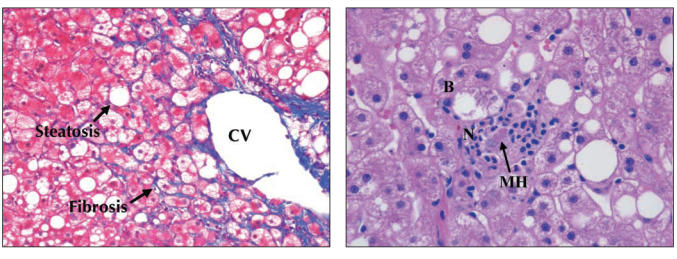
The “gold standard” for diagnosing NAFLD is clinico-pathological correlation, with confirmation of steatosis by liver biopsy and exclusion of other causes (e.g., alcohol) clinically. However, because alcoholic liver disease and NAFLD have similar histologic features (Fig. 2), they cannot be distinguished by means of liver biopsy. The cutoff limit of alcohol intake that distinguishes between alcoholic and nonalcoholic fatty liver disease is not known, although 20 g/d for women and 30 g/d for men is commonly used.66 One standard drink typically contains 10–20 g of alcohol.
Fig. 2: Left: Histologic features of fibrosis in nonalcoholic steatohepatitis (NASH). Trichrome stain of liver (magnification х 200) demonstrating macrovesicular steatosis and fibrosis, most prominent in zone 3 near the central vein (CV) of the hepatic lobule. Typically early fibrosis is pericellular and perisinusoidal, giving the appearance of “chickenwire.” Right: Histologic features of necrotic inflammation in NASH. Hematoxylin and eosin stain of liver (magnification х 400) with injured ballooned hepatocytes (B) and a mild neutrophilic infiltrate (N). Aggregations of Mallory's hyaline (MH) comprised of eosinophilic cytoskeleton filaments are also observed.
A minimum of 5%–10% steatosis by weight is considered a requirement for the diagnosis of NAFLD.66 Steatosis is generally macrovesicular, although it may be mixed with microvesicular droplets, which are seen with defective mitochondrial oxidation of free fatty acids.
Histologic features used to distinguish NASH from simple steatosis are controversial and vary in the literature. A recent conference defined NASH as zone 3 predominate macrovesicular steatosis in combination with hepatocyte ballooning and a mixed inflammatory infiltrate,66,67 often with characteristic perisinusoidal and pericellular fibrosis.
Liver biopsy performed on patients who have persistently elevated liver enzyme levels and no viral serologic markers of chronic liver disease will reveal NAFLD 66%–90% of the time.68,69,70 The positive predictive value of fatty changes on ultrasound in this setting is estimated to be 92%– 96%, whereas the negative predictive value of a normal scan is estimated to be 55%– 87%.64 Despite this, a clinical diagnosis of NAFLD before biopsy based on serologic test results and findings from imaging studies is correct in only 53%–83% of cases.68,71 However, in primary care settings where NAFLD is common, a positive ultrasound result in association with metabolic risk factors in the absence of viral serologic evidence of chronic liver disease is likely to be adequate for diagnosis.
In addition to confirming the clinical diagnosis, liver biopsy is valuable for excluding other liver disease and for monitoring disease progression.71 It provides prognostic information by distinguishing steatosis from NASH and by determining the stage of fibrosis. However, sampling error may lead to variation of one fibrosis stage in 24%– 37% of biopsies.72 Liver biopsy may also be useful when the diagnosis is uncertain (e.g., in the presence of autoantibodies62 or elevated iron indices), before participation in a clinical trial or when there is concern of advanced fibrosis, which may alter patient screening and surveillance.73 The decision to perform a biopsy should be made on an individual basis and discussed with the patient, with the benefits weighed against the small but definite risks of harm.
Serologic testing
Other causes of liver disease can usually be excluded through history taking, examination and serologic testing. In the presence of elevated liver aminotransaminase levels, it may be possible to exclude viral hepatitis, hemochromatosis, autoimmune hepatitis, chronic cholestatic disease, α1-antitrypsin deficiency and Wilson's disease through appropriate serologic testing.
Management
Weight loss and pharmacotherapy
The aim of treatment is to slow the progression of NAFLD and to prevent liver-related illness and death. However, because disease progression is slow and the magnitude of disease-related morbidity and mortality is uncertain, it is unclear which patients will benefit most from treatment. In addition, most therapeutic trials to date have been uncontrolled, of short duration and lacking histologic end points, which has led to limited treatment recommendations.74 Studies involving more than 10 participants, lasting longer than 6 months and having histologic end points are reported in Table 2.14,15,75,76,77,78,79,80,81,82,83,84,85,86
Table 2
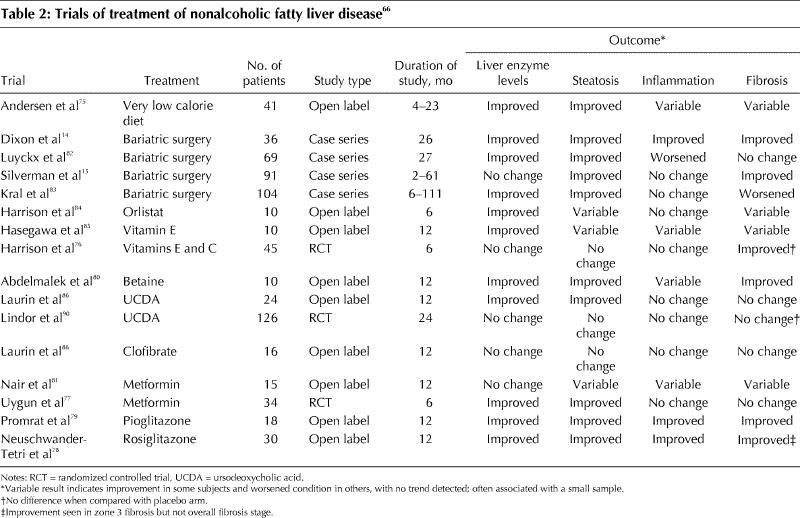
Both weight loss and exercise improve insulin resistance87 and are recommended in conjunction with the treatment of associated metabolic abnormalities. In one study, patients following a restricted diet (25 calories [105 kJ] per kilogram ideal body weight) and exercise regimen over 3 months had reduced liver enzyme levels and hepatic steatosis compared with control subjects, although it is unknown whether hepatic inflammation and fibrosis improved in the longer term.88 Rapid weight loss due to a very low energy diet (500 kcal [< 2090 kJ] daily) or jejunoileal bypass should be avoided because of the risk of worsening inflammation and fibrosis.75,89 A reasonable target is the loss of 10% of body weight over 6 months.74
Of the only 3 randomized placebo-controlled trials reported to date, none showed convincing histologic evidence of improvement with any of the investigated medications (antioxidants [vitamins E and C], hepatoprotective agents [ursodeoxycholic acid] or metformin) compared with placebo.76,77,90 Thiazolidinediones improve insulin sensitivity by activating the peroxisome proliferator-activated receptor gamma (PPARγ) and have shown promise in pilot trials involving patients with NASH, although weight gain has been a troublesome side effect.78,79 In addition, the initial PPARγ agonist troglitazone was withdrawn because of its hepatotoxic effects.91 The second-generation thioglitazones rosiglitazone and pioglitazone appear to be safer, although their use is currently contraindicated in the presence of active liver disease. Both pentoxifylline (a TNF-α inhibitor) and atorvastatin (used in NASH patients who have hyperlipidemia) improved aminotransaminase levels in uncontrolled trials, although histologic evidence of their benefit is unknown.92,93,94,95 The risk of statin-induced hepatotoxic effects does not appear to be increased among patients with unexplained elevation of liver enzyme levels presumably due to NAFLD.96 In a randomized controlled trial of probucol, an antioxidant and lipid-lowering agent, aminotransferase levels were significantly improved in the treatment group compared with the placebo group.97 Pilot studies of betaine and losartan revealed histologic and biochemical evidence of improvement, although the samples were small (fewer than 10 participants).80,98 Metformin has shown promise in small trials, and larger, randomized trials are in progress.81 However, because of the lack of evidence at this time, pharmacotherapy for NAFLD cannot be recommended outside of clinical trials.
Follow-up
Monitoring patients with NAFLD is difficult because liver enzyme levels tend to improve regardless of whether liver fibrosis worsens or improves.48 In addition, it may take several decades of monitoring before the development of complications is observed. Therefore, follow-up should be focused on patients who have risk factors for advanced disease.
Liver transplantation
Liver transplantation may be required if cirrhosis develops and is complicated by liver failure or hepatocellular carcinoma. Currently, about 3% of all transplants in North America are performed because of end-stage NAFLD,53 although this figure does not include patients with cryptogenic cirrhosis or those precluded from undergoing liver transplantation because of comorbidities related to insulin resistance. Recurrence of steatosis after transplantation is common (in 60%–100% of transplant recipients),53,99 with progression to steatohepatitis reported in one-third of cases.53
Conclusions
NAFLD is common, and its prevalence is likely to increase with the rising incidence of obesity and diabetes. A minority of patients with NAFLD, particularly those with NASH and diabetes, are at risk of liver-related complications such as cirrhosis and hepatocellular carcinoma. In addition, the overall mortality appears to be higher among NAFLD patients than among people in the general population, probably because of underlying pathogenic factors such as insulin resistance. Currently, treatment is limited to weight loss, exercise and the control of metabolic risk factors. Effective pharmacotherapies are awaited, and several promising agents are on the horizon.
Acknowledgments
Leon Adams is sponsored by an Overseas Medical Fellowship by the University of Western Australia.
Footnotes
This article has been peer reviewed.
Contributors: Leon Adams was the primary author, Paul Angulo provided scientific input, and Keith Lindor was responsible for oversight, editing and scientific content. All of the authors gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Keith D. Lindor, Division of Gastroenterology and Hepatology, Mayo Clinic and College of Medicine, 200 First St. SW, Rochester MN 55905, USA
References
- 1.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 2002;346:1221-31. [DOI] [PubMed]
- 2.Browning J, Szczepaniak L, Dobbins R, Nuremberg P, Horton J, Cohen J, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 2004;40:1387-95. [DOI] [PubMed]
- 3.Ryan CK, Johnson LA, Germin BI, Marcos A. One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transpl 2002;8:1114-22. [DOI] [PubMed]
- 4.Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann Intern Med 2000;132:112-7. [DOI] [PubMed]
- 5.Nomura H, Kashiwagi S, Hayashi J, Kajiyama W, Tani S, Goto M. Prevalence of fatty liver in a general population of Okinawa, Japan. Jpn J Med 1988;27:142-9. [DOI] [PubMed]
- 6.Shen L, Fan JG, Shao Y, Zeng MD, Wang JR, Luo GH, et al. Prevalence of nonalcoholic fatty liver among administrative officers in Shanghai: an epidemiological survey. World J Gastroenterol 2003;9:1106-10. [DOI] [PMC free article] [PubMed]
- 7.Ruhl CE, Everhart JE. Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology 2003;124:71-9. [DOI] [PubMed]
- 8.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol 2003;98:960-7. [DOI] [PubMed]
- 9.Tominaga K, Kurata JH, Chen YK, Fujimoto E, Miyagawa S, Abe I, et al. Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci 1995;40:2002-9. [DOI] [PubMed]
- 10.Gupte P, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, et al. Non-alcoholic steatohepatitis in type 2 diabetes mellitus. J Gastroenterol Hepatol 2004;19:854-8. [DOI] [PubMed]
- 11.Del Gaudio A, Boschi L, Del Gaudio GA, Mastrangelo L, Munari D. Liver damage in obese patients. Obes Surg 2002;12:802-4. [DOI] [PubMed]
- 12.Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology 2003;37:1286-92. [DOI] [PubMed]
- 13.Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology 1999;30:1356-62. [DOI] [PubMed]
- 14.Dixon JB, Bhathal PS, O'Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 2001;121:91-100. [DOI] [PubMed]
- 15.Silverman JF, Pories WJ, Caro JF. Liver pathology in diabetes mellitus and morbid obesity. Clinical, pathological, and biochemical considerations. Pathol Annu 1989;24 Pt 1:275-302. [PubMed]
- 16.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology 1990;12:1106-10. [DOI] [PubMed]
- 17.Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003;37:917-23. [DOI] [PubMed]
- 18.Kim HJ, Lee KE, Kim DJ, Kim SK, Ahn CW, Lim SK, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med 2004;164:2169-75. [DOI] [PubMed]
- 19.Day CP, James OF. Steatohepatitis: A tale of two “hits”? Gastroenterology 1998; 114:842-5. [DOI] [PubMed]
- 20.Choudhury J, Sanyal AJ. Insulin resistance and the pathogenesis of nonalcoholic fatty liver disease. Clin Liver Dis 2004;8:575-94, ix. [DOI] [PubMed]
- 21.Lewis GF, Carpentier A, Adeli K, Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr Rev 2002;23:201-29. [DOI] [PubMed]
- 22.Azzout-Marniche D, Becard D, Guichard C, Foretz M, Ferre P, Foufelle F. Insulin effects on sterol regulatory-element-binding protein-1c (SREBP-1c) transcriptional activity in rat hepatocytes. Biochem J 2000;350(Pt 2):389-93. [PMC free article] [PubMed]
- 23.Fromenty B, Robin MA, Igoudjil A, Mansouri A, Pessayre D. The ins and outs of mitochondrial dysfunction in NASH. Diabetes Metab 2004;30:121-38. [DOI] [PubMed]
- 24.Paradis V, Perlemuter G, Bonvoust F, Dargere D, Parfait B, Vidaud M, et al. High glucose and hyperinsulinemia stimulate connective tissue growth factor expression: a potential mechanism involved in progression to fibrosis in nonalcoholic steatohepatitis. Hepatology 2001;34:738-44. [DOI] [PubMed]
- 25.Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology 2003;37:909-16. [DOI] [PubMed]
- 26.Charlton M, Sreekumar R, Rasmussen D, Lindor K, Nair KS. Apolipoprotein synthesis in nonalcoholic steatohepatitis. Hepatology 2002;35:898-904. [DOI] [PubMed]
- 27.Letteron P, Sutton A, Abdellah M, Fromenty B, Pessayre D. Inhibition of microsomal triglyceride transfer protein: another mechanism of drug-induced steatosis in mice. Hepatology 2003;38:133-40. [DOI] [PubMed]
- 28.Namikawa C, Shu-Ping Z, Vyselaar JR, Nozaki Y, Nemoto Y, Ono M, et al. Polymorphisms of microsomal triglyceride transfer protein gene and manganese superoxide dismutase gene in non-alcoholic steatohepatitis. J Hepatol 2004;40:781-6. [DOI] [PubMed]
- 29.Tilg H, Diehl AM. Cytokines in alcoholic and nonalcoholic steatohepatitis. N Engl J Med 2000;343:1467-76. [DOI] [PubMed]
- 30.Leclercq IA, Farrell GC, Schriemer R, Robertson GR. Leptin is essential for the hepatic fibrogenic response to chronic liver injury. J Hepatol 2002;37:206-13. [DOI] [PubMed]
- 31.Hui JM, Hodge A, Farrell GC, Kench JG, Kriketos A, George J. Beyond insulin resistance in NASH: TNF-alpha or adiponectin? Hepatology 2004;40:46-54. [DOI] [PubMed]
- 32.Feldstein AE, Werneburg NW, Canbay A, Guicciardi ME, Bronk SF, Rydzewski R, et al. Free fatty acids promote hepatic lipotoxicity by stimulating TNF-alpha expression via a lysosomal pathway. Hepatology 2004;40:185-94. [DOI] [PubMed]
- 33.Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology 2001;120:1183-92. [DOI] [PubMed]
- 34.Crespo J, Cayon A, Fernandez-Gil P, Hernandez-Guerra M, Mayorga M, Dominguez-Diez A, et al. Gene expression of tumor necrosis factor alpha and TNF-receptors, p55 and p75, in nonalcoholic steatohepatitis patients. Hepatology 2001;34:1158-63. [DOI] [PubMed]
- 35.Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarthy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut 2001;48:206-11. [DOI] [PMC free article] [PubMed]
- 36.Valenti L, Fracanzani AL, Dongiovanni P, Santorelli G, Branchi A, Taioli E, et al. Tumor necrosis factor alpha promoter polymorphisms and insulin resistance in nonalcoholic fatty liver disease. Gastroenterology 2002;122:274-80. [DOI] [PubMed]
- 37.Honda H, Ikejima K, Hirose M, Yoshikawa M, Lang T, Enomoto N, et al. Leptin is required for fibrogenic responses induced by thioacetamide in the murine liver. Hepatology 2002;36:12-21. [DOI] [PubMed]
- 38.Masaki T, Chiba S, Tatsukawa H, Yasuda T, Noguchi H, Seike M, et al. Adiponectin protects LPS-induced liver injury through modulation of TNF-alpha in KK-Ay obese mice. Hepatology 2004;40:177-84. [DOI] [PubMed]
- 39.Kamada Y, Tamura S, Kiso S, Matsumoto H, Saji Y, Yoshida Y, et al. Enhanced carbon tetrachloride-induced liver fibrosis in mice lacking adiponectin. Gastroenterology 2003;125:1796-807. [DOI] [PubMed]
- 40.Chitturi S, Farrell G, Frost L, Kriketos A, Lin R, Fung C, et al. Serum leptin in NASH correlates with hepatic steatosis but not fibrosis: a manifestation of lipotoxicity? Hepatology 2002;36:403-9. [DOI] [PubMed]
- 41.Magalotti D, Marchesini G, Ramilli S, Berzigotti A, Bianchi G, Zoli M. Splanchnic haemodynamics in non-alcoholic fatty liver disease: effect of a dietary/pharmacological treatment. A pilot study. Dig Liver Dis 2004;36:406-11. [DOI] [PubMed]
- 42.McCuskey RS, Ito Y, Robertson GR, McCuskey MK, Perry M, Farrell GC. Hepatic microvascular dysfunction during evolution of dietary steatohepatitis in mice. Hepatology 2004;40:386-93. [DOI] [PubMed]
- 43.Jepsen P, Vilstrup H, Mellemkjaer L, Thulstrup AM, Olsen JH, Baron JA, et al. Prognosis of patients with a diagnosis of fatty liver — a registry-based cohort study. Hepatogastroenterology 2003;50:2101-4. [PubMed]
- 44.Teli MR, James OF, Burt AD, Bennett MK, Day CP. The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology 1995;22:1714-9. [PubMed]
- 45.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 1999;116:1413-9. [DOI] [PubMed]
- 46.Dam-Larsen S, Franzmann M, Andersen IB, Christoffersen P, Jensen LB, Sorensen TI, et al. Long term prognosis of fatty liver: risk of chronic liver disease and death. Gut 2004;53:750-5. [DOI] [PMC free article] [PubMed]
- 47.Younossi ZM, Gramlich T, Matteoni CA, Boparai N, McCullough AJ. Nonalcoholic fatty liver disease in patients with type 2 diabetes. Clin Gastroenterol Hepatol 2004;2:262-5. [DOI] [PubMed]
- 48.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol 2005;42:132-8. [DOI] [PubMed]
- 49.Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology 2000;32:689-92. [DOI] [PubMed]
- 50.Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology 1999;29:664-9. [DOI] [PubMed]
- 51.Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology 1990;11:74-80. [DOI] [PubMed]
- 52.Marrero JA, Fontana RJ, Su GL, Conjeevaram HS, Emick DM, Lok AS. NAFLD may be a common underlying liver disease in patients with hepatocellular carcinoma in the United States. Hepatology 2002;36:1349-54. [DOI] [PubMed]
- 53.Charlton M, Kasparova P, Weston S, Lindor K, Maor-Kendler Y, Wiesner RH, et al. Frequency of nonalcoholic steatohepatitis as a cause of advanced liver disease. Liver Transpl 2001;7:608-14. [DOI] [PubMed]
- 54.Omagari K, Kadokawa Y, Masuda J, Egawa I, Sawa T, Hazama H, et al. Fatty liver in non-alcoholic non-overweight Japanese adults: incidence and clinical characteristics. J Gastroenterol Hepatol 2002;17:1098-105. [DOI] [PubMed]
- 55.Bugianesi E, Manzini P, D'Antico S, Vanni E, Longo F, Leone N, et al. Relative contribution of iron burden, HFE mutations, and insulin resistance to fibrosis in nonalcoholic fatty liver. Hepatology 2004;39:179-87. [DOI] [PubMed]
- 56.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 1980;55:434-8. [PubMed]
- 57.Ipekci SH, Basaranoglu M, Sonsuz A. The fluctuation of serum levels of aminotransferase in patients with nonalcoholic steatohepatitis. J Clin Gastroenterol 2003;36:371. [DOI] [PubMed]
- 58.Yano E, Tagawa K, Yamaoka K, Mori M. Test validity of periodic liver function tests in a population of Japanese male bank employees. J Clin Epidemiol 2001;54:945-51. [DOI] [PubMed]
- 59.Sorbi D, Boynton J, Lindor KD. The ratio of aspartate aminotransferase to alanine aminotransferase: potential value in differentiating nonalcoholic steatohepatitis from alcoholic liver disease. Am J Gastroenterol 1999;94:1018-22. [DOI] [PubMed]
- 60.Chitturi S, Weltman M, Farrell GC, McDonald D, Kench J, Liddle C, et al. HFE mutations, hepatic iron, and fibrosis: ethnic-specific association of NASH with C282Y but not with fibrotic severity. Hepatology 2002;36:142-9. [DOI] [PubMed]
- 61.Loria P, Lonardo A, Leonardi F, Fontana C, Carulli L, Verrone AM, et al. Non-organ-specific autoantibodies in nonalcoholic fatty liver disease: prevalence and correlates. Dig Dis Sci 2003;48:2173-81. [DOI] [PubMed]
- 62.Adams LA, Lindor KD, Angulo P. The prevalence of autoantibodies and autoimmune hepatitis in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 2004;99:1316-20. [DOI] [PubMed]
- 63.Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology 2002;123:745-50. [DOI] [PubMed]
- 64.Joy D, Thava VR, Scott BB. Diagnosis of fatty liver disease: is biopsy necessary? Eur J Gastroenterol Hepatol 2003;15:539-43. [DOI] [PubMed]
- 65.Mottin CC, Moretto M, Padoin AV, Swarowsky AM, Toneto MG, Glock L, et al. The role of ultrasound in the diagnosis of hepatic steatosis in morbidly obese patients. Obes Surg 2004;14:635-7. [DOI] [PubMed]
- 66.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology 2003;37:1202-19. [DOI] [PubMed]
- 67.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 1999;94:2467-74. [DOI] [PubMed]
- 68.Sorbi D, McGill DB, Thistle JL, Therneau TM, Henry J, Lindor KD. An assessment of the role of liver biopsies in asymptomatic patients with chronic liver test abnormalities. Am J Gastroenterol 2000;95:3206-10. [DOI] [PubMed]
- 69.Skelly MM, James PD, Ryder SD. Findings on liver biopsy to investigate abnormal liver function tests in the absence of diagnostic serology. J Hepatol 2001;35:195-9. [DOI] [PubMed]
- 70.Daniel S, Ben-Menachem T, Vasudevan G, Ma CK, Blumenkehl M. Prospective evaluation of unexplained chronic liver transaminase abnormalities in asymptomatic and symptomatic patients. Am J Gastroenterol 1999;94:3010-4. [DOI] [PubMed]
- 71.Van Ness MM, Diehl AM. Is liver biopsy useful in the evaluation of patients with chronically elevated liver enzymes? Ann Intern Med 1989;111:473-8. [DOI] [PubMed]
- 72.Mendez P, Regev A, Molina E, Berho M, Bejarano P, Ladino M, et al. Sampling error and reliability of liver biopsy in patients with nonalcoholic fatty liver disease (NAFLD) [abstract]. Hepatology 2003;38(Suppl 1):673A.
- 73.Adams PC, Arthur MJ, Boyer TD, DeLeve LD, Di Bisceglie AM, Hall M, et al. Screening in liver disease: report of an AASLD clinical workshop. Hepatology 2004;39:1204-12. [DOI] [PubMed]
- 74.Angulo P. Current best treatment for non-alcoholic fatty liver disease. Expert Opin Pharmacother 2003;4:611-23. [DOI] [PubMed]
- 75.Andersen T, Gluud C, Franzmann MB, Christoffersen P. Hepatic effects of dietary weight loss in morbidly obese subjects. J Hepatol 1991;12:224-9. [DOI] [PubMed]
- 76.Harrison SA, Torgerson S, Hayashi P, Ward J, Schenker S. Vitamin E and vitamin C treatment improves fibrosis in patients with nonalcoholic steatohepatitis. Am J Gastroenterol 2003;98:2485-90. [DOI] [PubMed]
- 77.Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A, et al. Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2004;19:537-44. [DOI] [PubMed]
- 78.Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR. Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology 2003;38:1008-17. [DOI] [PubMed]
- 79.Promrat K, Lutchman G, Uwaifo GI, Freedman RJ, Soza A, Heller T, et al. A pilot study of pioglitazone treatment for nonalcoholic steatohepatitis. Hepatology 2004;39:188-96. [DOI] [PubMed]
- 80.Abdelmalek MF, Angulo P, Jorgensen RA, Sylvestre PB, Lindor KD. Betaine, a promising new agent for patients with nonalcoholic steatohepatitis: results of a pilot study. Am J Gastroenterol 2001;96:2711-7. [DOI] [PubMed]
- 81.Nair S, Diehl AM, Wiseman M, Farr GH Jr, Perrillo RP. Metformin in the treatment of non-alcoholic steatohepatitis: a pilot open label trial. Aliment Pharmacol Ther 2004;20:23-8. [DOI] [PubMed]
- 82.Luyckx FH, Desaive C, Thiry A, Dewe W, Scheen AJ, Gielen JE, et al. Liver abnormalities in severely obese subjects: effect of drastic weight loss after gas/troplasty. Int J Obes Relat Metab Disord 1998;22(3):222-6. [DOI] [PubMed]
- 83.Kral JG, Thung SN, Biron S, Hould FS, Lebel S, Marceau S, et al. Effects of surgical treatment of the metabolic syndrome on liver fibrosis and cirrhosis. Surgery 2004;135:48-58. [DOI] [PubMed]
- 84.Harrison SA, Fincke C, Helinski D, Torgerson S, Hayashi P. A pilot study of orlistat treatment in obese, non-alcoholic steatohepatitis patients. Aliment Pharmacol Ther 2004;20(6):623-8. [DOI] [PubMed]
- 85.Hasegawa T, Yoneda M, Nakamura K, Makino I, Terano A. Plasma transforming growth factor-beta1 level and efficacy of alpha-tocopherol in patients with non-alcoholic steatohepatitis: a pilot study. Aliment Pharmacol Ther 2001;15 (10):1667-72. [DOI] [PubMed]
- 86.Laurin J, Lindor KD, Crippin JS, Gossard A, Gores GJ, Ludwig J, et al. Ursodeoxycholic acid or clofibrate in the treatment of non-alcohol-induced steatohepatitis: a pilot study. Hepatology 1996;23(6):1464-7. [DOI] [PubMed]
- 87.Cox KL, Burke V, Morton AR, Beilin LJ, Puddey IB. Independent and additive effects of energy restriction and exercise on glucose and insulin concentrations in sedentary overweight men. Am J Clin Nutr 2004;80:308-16. [DOI] [PubMed]
- 88.Ueno T, Sugawara H, Sujaku K, Hashimoto O, Tsuji R, Tamaki S, et al. Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol 1997;27:103-7. [DOI] [PubMed]
- 89.Drenick EJ, Simmons F, Murphy JF. Effect on hepatic morphology of treatment of obesity by fasting, reducing diets and small-bowel bypass. N Engl J Med 1970;282:829-34. [DOI] [PubMed]
- 90.Lindor KD, Kowdley KV, Heathcote EJ, Harrison ME, Jorgensen R, Angulo P, et al. Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis: results of a randomized trial. Hepatology 2004;39:770-8. [DOI] [PubMed]
- 91.Menon KVN, Angulo P, Lindor KD. Severe cholestatic hepatitis from troglitazone in a patient with nonalcoholic steatohepatitis and diabetes mellitus. Am J Gastroenterol 2001;96:1631-4. [DOI] [PubMed]
- 92.Kiyici M, Gulten M, Gurel S, Nak SG, Dolar E, Savci G, et al. Ursodeoxycholic acid and atorvastatin in the treatment of nonalcoholic steatohepatitis. Can J Gastroenterol 2003;17:713-8. [DOI] [PubMed]
- 93.Satapathy SK, Garg S, Chauhan R, Sakhuja P, Malhotra V, Sharma BC, et al. Beneficial effects of tumor necrosis factor-alpha inhibition by pentoxifylline on clinical, biochemical, and metabolic parameters of patients with nonalcoholic steatohepatitis. Am J Gastroenterol 2004;99:1946-52. [DOI] [PubMed]
- 94.Adams LA, Zein CO, Angulo P, Lindor KD. A pilot trial of pentoxifylline in nonalcoholic steatohepatitis. Am J Gastroenterol 2004;99:2365-8. [DOI] [PubMed]
- 95.Hatzitolios A, Savopoulos C, Lazaraki G, Sidiropoulos I, Haritanti P, Lefkopoulos A, et al. Efficacy of omega-3 fatty acids, atorvastatin and orlistat in non-alcoholic fatty liver disease with dyslipidemia. Indian J Gastroenterol 2004;23:131-4. [PubMed]
- 96.Chalasani N, Aljadhey H, Kesterson J, Murray MD, Hall SD. Patients with elevated liver enzymes are not at higher risk for statin hepatotoxicity. Gastroenterology 2004;126:1287-92. [DOI] [PubMed]
- 97.Merat S, Malekzadeh R, Sohrabi MR, Sotoudeh M, Rakhshani N, Sohrabpour AA, et al. Probucol in the treatment of non-alcoholic steatohepatitis: a double-blind randomized controlled study. J Hepatol 2003;38:414-8. [DOI] [PubMed]
- 98.Yokohama S, Yoneda M, Haneda M, Okamoto S, Okada M, Aso K, et al. Therapeutic efficacy of an angiotensin II receptor antagonist in patients with nonalcoholic steatohepatitis. Hepatology 2004;40:1222-5. [DOI] [PubMed]
- 99.Contos MJ, Cales W, Sterling RK, Luketic VA, Shiffman ML, Mills AS, et al. Development of nonalcoholic fatty liver disease after orthotopic liver transplantation for cryptogenic cirrhosis. Liver Transpl 2001;7:363-73. [DOI] [PubMed]