Abstract
Scutellaria altissima L. is a common traditional Chinese medicine used to treat inflammation in some countries. Scutellarin, an active major flavone glycoside isolated from the traditional Chinese medicine Scutellaria altissima L., has been shown to offer various beneficial biochemical effects on cerebrovascular diseases and inflammation. However, the antiproliferative effects of Scutellarin in prostate cancer and the underlying mechanism are not fully elucidated. In the present study, we aimed to ascertain whether Scutellarin inhibits cancer cell growth and to further explore the molecular mechanism. Scutellarin enhanced the sensitivity of prostate cancer cells to cisplatin. MTT assays revealed that cell viability was significantly decreased in the prostate cancer cells treated with Scutellarin. Flow cytometric analysis indicated that Scutellarin suppressed cell proliferation by promoting G2/M arrest and inducing apoptosis. We employed western blotting to delineate the underlying mechanisms involved in the G2/M arrest and apoptosis. Comet assay and γH2AX immunocytochemistry were used to detect levels of DNA damage in PC3 cells exposed to Scutellarin and/or cisplatin. Our data revealed that Scutellarin significantly induced prostate cancer cell apoptosis by activating the caspase cascade. An increase in the Bax/Bcl-2 ratio, depolarization of mitochondrial membrane potential and cell cycle arrest at G2/M phase were accompanied by the apoptosis induction. Additionally, Scutellarin altered the protein expression of cell cycle and apoptosis regulatory genes by downregulating Cdc2, cyclin B1 and Bcl-2 and upregulating caspase-3, caspase-9 and Bax in prostate cancer cells. Furthermore, Scutellarin sensitized PC3 cells to cisplastin treatment in a dose-dependent manner. Taken together, our data confirmed the cytotoxicity of Scutellarin against prostate cancer PC3 cells and provide new findings in regards to Scutellarin sensitizing prostate cancer cells to chemotherapy. Our findings suggest that Scutellarin has potential to be used as a novel antineoplastic therapeutic candidate for prostate cancer patients.
Keywords: Scutellarin, prostate cancer, apoptosis, cell cycle arrest, chemosensitizing effects
Introduction
Prostate cancer remains the second cause of cancer-related death among men (1). It is difficult to detect this tumor at an early stage, and poses a major challenge for treatment (2). Due to late diagnosis and increasing chemoresistance of prostate cancer, the five-year survival rate of patients remains <50% after chemotherapeutic regimens and cytoreductive surgery (3). Prostate cancer metastasizes and transfers easily, is recurrent and is also resistant to chemotherapy, thus resulting in a high mortality rate (4). Therefore, development of novel effective and less toxic drugs is urgent for prostate cancer patients.
Recently, many types of bioactive phytochemicals play a vital role in tumor suppression and antioxidant capacity (5,6). Many flavone glycoside bioactive phytochemicals, such as hesperidin and puerarin, have been identified to exhibit anticancer activity (7,8). Scutellarin is one of the effective bioactive phytochemicals found in the traditional Chinese herbal medicine Scutellaria altissima L. (9). It is a traditional Chinese medicinal plants commomly used for upper respiratory infection, pneumonia and high blood pressure (10,11). Scutellaria altissima L. is a plant from the family Lamiaceae found on the top of the hills and slopes, and in forest margins in China. The chemical formula of Scutellarin is C21H18O12. Scutellarin has been widely used to treat cardiovascular and cerebrovascular diseases (12). It has been revealed that Scutellarin exhibits a variety of pharmacological actions, including antioxidative, anti-inflammatory and vasodilator activity (13,14). It has been confirmed to show antitumor effects in many types of cancers, such as gastric and breast cancer, glioblastoma, prostate, lung and hepatocellular cancer by inhibiting tumor cell growth, metastasis and inducing cell cycle arrest and mitochondrial pathway-mediated apoptosis. However, there is no sufficient evidence confirming the effects of Scutellarin on prostate cancer cells and the underlying molecular mechanisms remain unclear. Thus, whether Scutellarin can sensitize cancer PC3 cells to chemotherapy has not been revealed.
In the present study, our results showed that Scutellarin exerts antitumor effects on prostate cancer cells and we furthered explored the molecular mechanism underlying this process. Data from the present study revealed that Scutellarin significantly induced dose-dependent apoptosis and sensitized PC3 cells to cisplatin through induction of DNA breaks. Our results show that Scutellarin warrants future development as an effective and novel drug for patients with prostate cancer.
Materials and methods
Materials, reagents and chemicals
Antibodies against caspase-3, caspase-9, Bcl-2, Bax, Cdc2, cyclin B1, β-actin and γH2AX were obtained from Cell Signaling Technology Inc. (Beverly, MA, USA). The enhanced chemiluminescence (ECL) kit was purchased from Amersham Life Science, Inc. (Arlington Heights, IL, USA). The Annexin V-conjugated FITC apoptosis detection kit and JC-1 mitochondrial membrane potential detection kit were purchased from NanJing KeyGen Biotech Co., Ltd. (Nanjing, China). The Comet Assay kit was from NanJing KeyGen Biotech Co., Ltd. (Nanjing, China). 3-(4,5-Dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and 46-diamidino-2-phenylindole dihydrochloride (DAPI) were obtained from Sigma Chemical Co. (St. Louis, MO, USA). Scutellarin (>98%) powder was purchased from Sichuan Best-Reagent Industry Co., Ltd. (Sichuan, China, lot no. B01146801) and dissolved in dimethyl sulfoxide (DMSO). The final concentration of DMSO was 0.1% in all groups and had no effect on cell viability. The chemical formula of Scutellarin is C21H18O12.
Cell lines and cell culture
The prostate cancer cell line PC3 was purchased from the American Type Culture Collection (ATCC; Manassas, VA, USA) and cultured in Dulbeccos modified Eagles medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 100 U/ml penicillin (all from Gibco-BRL, Grand Island, NY, USA) at 37°C with 5% CO2.
Cell viability assays
The effect of Scutellarin on the viability of cells was detected by MTT assay. The cells (1×104/well) were seeded into 96-well plate and incubated for 24 h. After treatment with Scutellarin (0, 100, 200, 300, 400, 500 or 600 µM) for 24, 48 and 72 h, the viability of the cancer cells was detected with MTT assay. Twenty microliters (20 µl) of MTT solution [5 mg/ml in phosphate-buffered saline (PBS)] was added to each well, and the mixtures were incubated for 4 h at 37°C. Then, the MTT solution was removed and 150 µl of DMSO was added to the wells. The absorbance was measured using a Multiskan Ascent plate reader at 540 nm wavelength.
Cell cycle analysis by flow cytometry
The cells were treated with Scutellarin (0, 200, 400 or 600 µM) for 24 h, washed twice with PBS and fixed with 70% ethanol overnight at 4°C. Following fixation, the DNA fragments were stained in PBS containing propidium iodide (PI) and RNase A for 1 h at 37°C. The DNA content was evaluated on a flow cytometer Accuri C6 (BD Biosciences, Franklin Lakes, NJ, USA). The data were analyzed using ModFit LT V4.1.
DAPI staining assay
Approximately 4×104 cells/well of prostate cancer cells were treated with Scutellarin at 0, 200, 400 or 600 µM for 24 h. Cells in each well were stained with DAPI before fixation with 3.7% formaldehyde. The cells were then washed with PBS and detected using fluorescence microscopy.
Cell apoptosis by flow cytometry
The extent of apopotosis was evaluated by flow cytometry using Annexin V-FITC. After treatment with 0, 200, 400 or 600 µM Scutellarin for 24 h, prostate cancer cells were harvested and washed with PBS for three times, and then incubated with Annexin V-FITC and PI for 10 min in the dark. The cells were detected by a flow cytometer Accuri C6.
Assay for mitochondrial membrane potential
Changes in mitochondrial membrane potential of prostate cancer cells were detected by flow cytometry using JC-1 detection kit. After treatment with 0, 200, 400 or 600 µM Scutellarin for 24 h, cells were harvested and incubated with JC-1 dye for 15 min at 37°C according to the manufacturer's protocol. The cells were detected by a flow cytometer Accuri C6.
Colony formation assay
Cells (500 cells per 35-mm dish) were plated before treatment. Then, 1 ml medium with or without drug was added into each well. Cells were fixed using 70% ethanol, and stained using crystal violet (Sigma, St. Louis, MO, USA) dissolved in 10% ethanol for 15 days. The number of colonies was obtained by cell counting. Colonies were defined as a minimum of 50 cells in a group.
Comet assay
DNA damage induction of Scutellarin in hepatocellular carcinoma cells was determined using the Comet assay, according to the manufacturer's protocol. Briefly, cells were treated with Scutellarin (200 µM) and/or cisplatin (6 µM) for 48 h in complete medium, and then cells were harvested and resuspended in ice-cold PBS buffer. We used the concentration of 6 µM for cisplatin and 200 µM for Scutellarin as these concentrations do not inhibit the proliferation of cells significantly, and thus it could be ascertained whether Scutellarin enhances the sensitivity of prostate cancer cells to cisplatin. Approximately 1×104 cells in a volume of 75 µl of 0.5% (w/v) low-melting-point agarose were pipetted into a frosted glass slide coated with a thin layer of 1.0% (w/v) agarose, covered with a coverslip, and allowed to set on ice for 10 min. Following removal of the coverslip, the slides were immersed in ice-cold lysis solution. After 2 h at 4°C, the slides were placed into a horizontal electrophoresis tank filled with electrophoresis buffer and subjected to electrophoresis for 30 min at 30 V at 4°C. Cells were stained with 2.5 µg/ml PI for 5 min and visualized under a microscope at a magnification of ×200. Tail length from a minimum of 10 cells was quantified as the distance from the center of the cell nucleus to the tip of the tail.
γH2AX immunocytochemistry
Cells were seeded on microscope slides and treated with Scutellarin (200 µM) and/or cisplatin (6 µM). Cells were fixed with 4% polyformaldehyde, washed with PBS and blocked with 1% bovine albumin serum with 0.1% Triton-X. Slides were washed in PBS, and then incubated with γH2AX primary antibody at a dilution of 1:800 in 1% BSA in PBS overnight at 4°C with gentle shaking. Cells were then washed three times in PBS before incubating in the dark with goat anti-rabbit IgG/FITC-conjugated secondary antibody at a dilution of 1:1,000 in 1% BSA in PBS for 2 h. Nuclei were counterstained with DAPI (1 µg/ml) in PBS for 5 min. Images were collected using a fluorescence microscope.
Western blotting
The total protein was extracted from the cell samples using lysis buffer (Beyotime, Shanghai, China) and protease inhibitor (Biocolors, Shanghai, China). Lysis buffer and protease inhibitor were used after being mixed in a proportion of 1:100. Equal amounts of protein were loaded on a 10% SDS-PAGE gel. The lysates were resolved by electrophoresis (80 V for 30 min and 120 V for 1.5 h), and transferred onto polyvinylidene difluoride (PVDF) membranes (nitrocellulose membrane; Bio-Rad, Hercules, CA, USA). After blocking in 5% nonfat milk for 1 h at room temperature, incubation was carried out with the different antibodies overnight at 4°C. This was followed by incubation with relevant secondary antibodies for 1 h at room temperature. Protein bands were visualized using the Chemiluminescent ECL assay kit for each group and the Bio-Rad ChemiDoc XRS+ image analyzer. Protein expression levels were quantitatively determined using ImageJ software (National Institutes of Health, Bethesda, MD, USA). β-actin was used as an internal reference for protein expression in the treated cells.
Statistical analysis
Data are presented as means ± SD for three independent experiments. Statistical differences between two groups were analyzed using a Student's t-test by GraphPad Prism 5.0 (GraphPad Software, San Diego, CA, USA). A significant difference was considered as P<0.05.
Results
Scutellarin inhibits prostate cancer cell proliferation
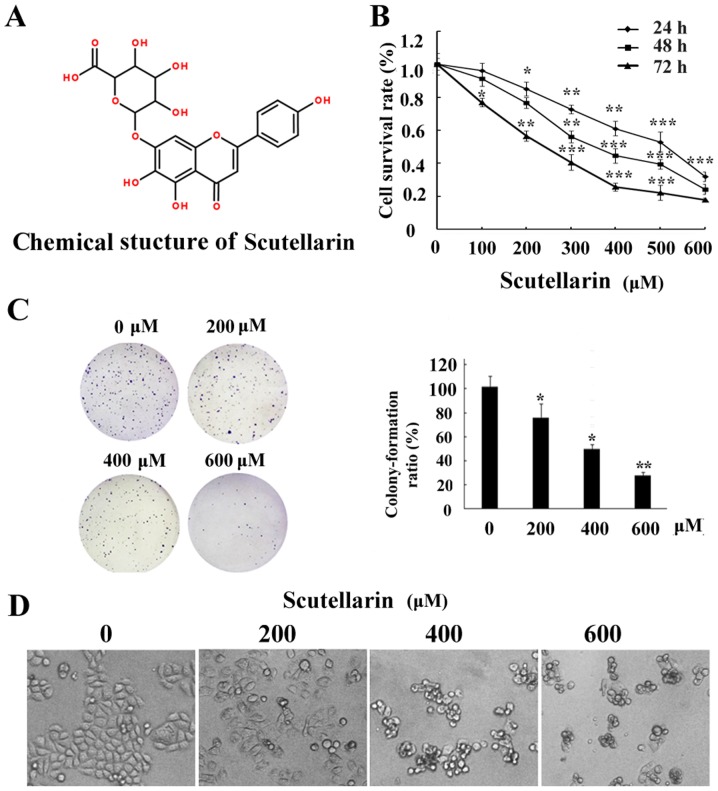
The chemical structure of Scutellarin is shown in Fig. 1A. In order to determine the cytotoxic effects of Scutellarin on prostate cancer cells, cell viability was detected by MTT assay. Prostate cancer PC3 cells were treated with different concentrations of Scutellarin (0, 100, 200, 300, 400, 500 or 600 µM) for 24, 48 or 72 h (Fig. 1B). Scutellarin exhibited cytotoxicity against the PC3 cells. The prostate cancer cells treated with Scutellarin showed a reduced proliferation capacity in a dose- and time-dependent manner (P<0.05).
Figure 1.
Effect of Scutellarin on the proliferation of prostate cancer cells. (A) Chemical structure of Scutellarin. (B) Prostate cancer PC3 cells were treated with Scutellarin (0, 100, 200, 300, 400, 500 or 600 µM) for 24, 48 and 72 h. Cell viability was determined by MTT assay. (C) The proliferative effect of Scutellarin on PC3 cells by colony formation assay. The surviving colonies were stained. (D) Cells were photographed with inverted contrast microscopy at a magnification of ×200. Data shown are representatives of three experiments; *Significant difference (P<0.05) and **/***extremely significant difference (P<0.01/P<0.001) compared to the control group.
In order to determine the long-term growth inhibitory effects, we pre-incubated PC3 cells with Scutellarin (0, 200, 400 or 600 µM) for 24 h, washed the cells, and cultured them for 7 additional days. As shown in Fig. 1C, the colony formation ability of the prostate cancer cells was significantly reduced in a dose-dependent manner.
In addition, the morphological changes in prostate cancer cells were examined under a phase contrast microscope. PC3 cells cultured with complete DMEM without Scutellarin displayed a normal shape with 60% confluency for 24 h. However, the cell confluence was markedly reduced and the morphologic changes in PC3 cells were also quite obvious after Scutellarin treatment. The cells started to shrink, lost their normal shape, became round and ultimately detached from the culture dish (Fig. 1D). All of these results indicated that Scutellarin inhibited prostate cancer cell growth and caused cell death.
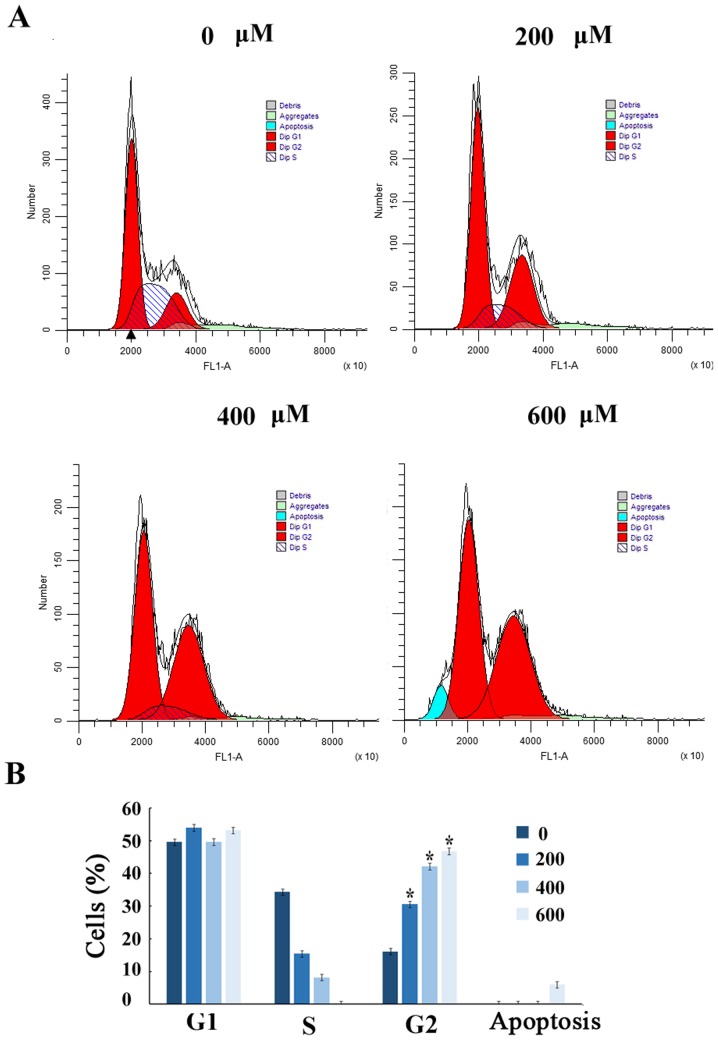
Scutellarin induces G2/M arrest
To further demonstrate that the growth inhibition of human prostate cancer cells leads to alterations in cell cycle distribution, cells were treated with Scutellarin and stained with PI. The percentage of cells in each stage of the cell cycle was evaluated by flow cytometry (Fig. 2A). Treatment of the human prostate cancer PC3 cells with Scutellarin (0, 200, 400 or 600 µM) for 24 h resulted in accumulation of cells in the G2/M phase from 16.6%±2.1 to 47.2%±2.3 (P≤0.01; Fig. 2B).
Figure 2.
Cell cycle distribution analysis by flow cytometry. (A) Cell cycle analysis of PC3 cells following Scutellarin (0, 200, 400 or 600 µM) treatment for 24 h by flow cytometry. (B) Histogram showing the percentage of cells in the G2/M phase; *Significant difference (P<0.05) compared to the control group.
Scutellarin induces prostate cancer cell apoptosis
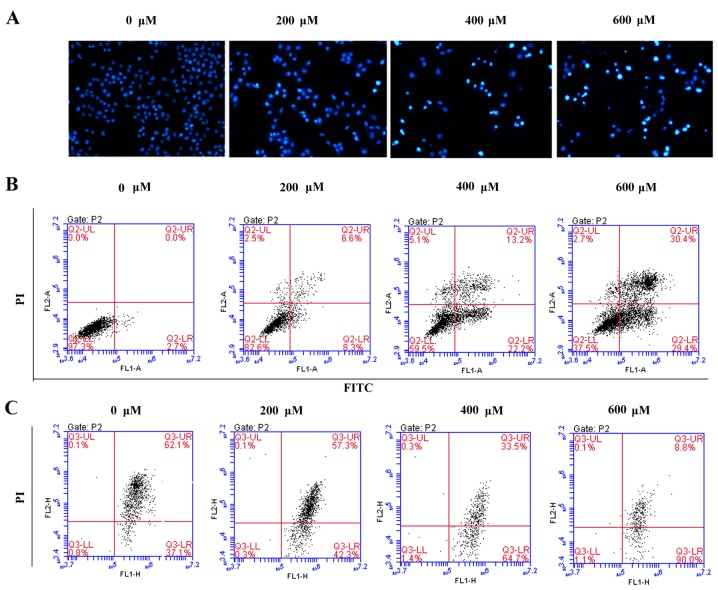
To assess whether the growth inhibitory effect of Scutellarin on PC3 cells was associated with apoptosis, the prostate cancer cells were stained with DAPI and observed under a fluorescence microscope (Fig. 3A). After treatment with different concentrations of Scutellarin (0, 200, 400 or 600 µM) for 24 h, nuclear chromatin condensation and fragmented punctuate blue nuclear fluorescence were observed in the prostate cancer cells in a dose-dependent manner, which was similar to the morphological changes in the apoptotic cells, while the control cells displayed normal and intact nuclei. This suggested that Scutellarin may induce prostate cancer cell apoptosis.
Figure 3.
Scutellarin induces the apoptosis of prostate cancer PC3 cells. (A) Morphology of cell nuclei in the PC3 cells treated with Scutellarin were observed after DAPI staining (magnification, ×100). (B) PC3 cells were treated with Scutellarin (0, 200, 400 and 600 µM) for 24 h. Annexin V/PI staining was performed to detect apoptosis. The lower right quadrant of the fluorescence activated cell sorting (FACS) histogram indicates the percentage of early apoptotic cells (Annexin V+/PI− stained cells), while the upper right quadrant indicates the percentage of late apoptotic cells (Annexin V+/PI+ stained cells). (C) The PC3 cells were treated with Scutellarin (0, 200, 400 and 600 µM) for 24 h and then harvested, stained with JC-1 dye, and finally analyzed using flow cytometry to assess changes in mitochondrial membrane potential.
To further investigate whether the antitumor effects of Scutellarin on PC3 cells are associated with apoptosis, the apoptotic cell percentages were analyzed by flow cytometry (Fig. 3B). After treatment with different concentrations of Scutellarin for 24 h, the numbers of early and late apoptotic cells were significantly increased compared to these numbers in the control group. The percentage of total apoptotic cells was 2.7% in the PC3 control cells (early-stage, 2.7%; and late-stage, 0%), 14.9% in the cells treated with 200 µM Scutellarin (early-stage, 8.3%; and late-stage, 6.6%), 35.4% in the cells treated with 400 µM Scutellarin (early-stage, 22.2%; and late-stage, 13.2%) and 59.8% in the cells treated with 600 µM Scutellarin (early-stage, 29.4%; and late-stage, 30.4%).
It is known that changes in mitochondrial membrane potential involved in apoptosis are induced by mitochondrial damage (15). To explore the effect of Scutellarin on mitochondrial membrane potential, the cells were treated with Scutellarin and mitochondrial membrane potential was detected by JC-1 dye. As shown in Fig. 3C, the average percentage of green fluorescence-positive PC3 cells was 37.1% in the control cells, 42.3% in cells treated with 200 µM Scutellarin, 64.7% in cells treated with 400 µM Scutellarin and 90.0% in cells treated with 600 µM Scutellarin. These results showed a significant dose-dependent increase in green fluorescence-positive cells, suggesting occurrence of the loss of mitochondrial membrane potential with Scutellarin treatment. Thus, the apoptosis of prostate cancer cells by Scutellarin was associated with the damage of the mitochondrial membrane.
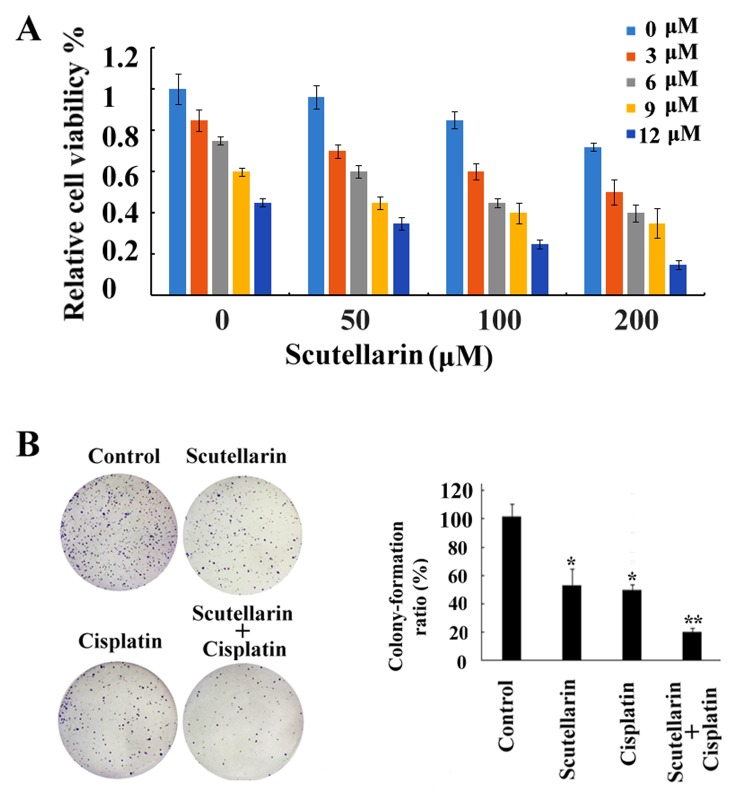
Chemosensitizing effects of Scutellarin on PC3 cells
Although research has been carried out to investigate the antitumor activities of Scutellarin (16), to date no research studies have been performed to explore the sensitizing effects of Scutellarin on tumor cells. In the present study our data showed that cell death induced by cisplatin treatment was further enhanced by combination with Scutellarin treatment in a dose-dependent manner (Fig. 4A), which proved the chemosensitizing effects of Scutellarin on PC3 cells. Scutellarin sensitized PC3 cells to cisplatin-induced cytotoxicity. PC3 cells were treated with different concentrations of cisplatin (3–12 µM) for 24 h in the presence or absence of different doses of Scutellarin (50–200 µM). Cell viability was measured using MTT assay as described in the Materials and methods section and presented as a percentage of the control. Data are presented as mean ± standard deviation (SD). The inhibition of colony ability by cisplatin treatment significantly enhanced after combination with Scutellarin treatment in the prostate cancer cells (Fig. 4B).
Figure 4.
Scutellarin enhances cisplatin-induced cell death. (A) The cell viability inhibitory effects of the single and combined treatment were analyzed using MTT assay. Cisplatin-induced cell death was further enhanced by combination with Scutellarin treatment in a dose-dependent manner. (B) Colony formation assay was performed to verify the proliferative potential of PC3 cells after cisplatin (6 µM) and/or Scutellarin (200 µM) treatment. Data shown are representatives of three experiments; *Significant difference (P<0.05) and **extremely significant difference (P<0.01) compared to the control group.
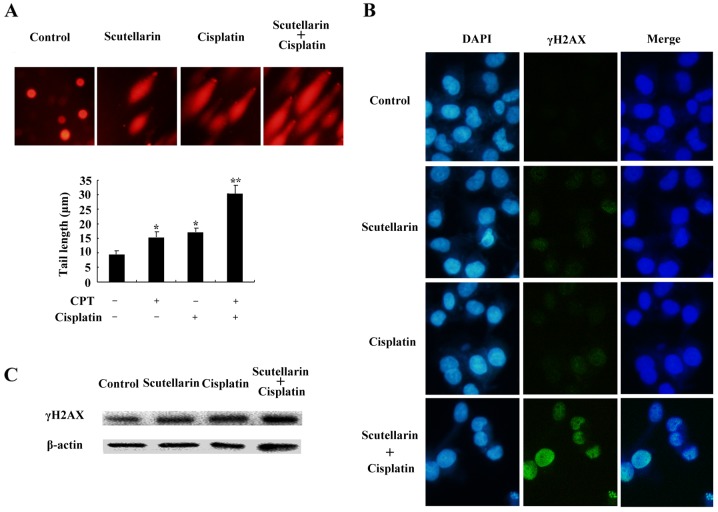
DNA damage is induced by cisplatin and/or Scutellarin in PC3 cells
Cisplatin is one of the most important chemotherapeutic agents for cancer treatment (17). To further investigate the effect of Scutellarin on cisplatin sensitivity through induction of DNA damage, cells were treated with Scutellarin and/or cisplatin, and comet assay and immunofluorescence staining was carried out 24 h later. Scutellarin combined with cisplatin induced a significant increase in the frequency of DNA damage using the comet assay (Fig. 5A).
Figure 5.
(A) DNA damage in PC3 cells was examined by comet assays. The cells were treated with cisplatin (6 µM) and/or Scutellarin (200 µM). The tail length of comets was measured in each cell and the tail length is expressed in µm as a mean ± SD from at least 10 cells in each treatment group; *Significant difference (P<0.05) and **extremely significant difference (P<0.01), compared with the negative control. (B) DNA damage in PC3 cells was examined by immunofluorescence staining. The cells were treated with cisplatin (6 µM) and/or Scutellarin (200 µM), and the cells wer examined for γ-H2AX foci formation. (C) The expression of γ-H2AX was examined by western blot analysis.
We further used the immunofluorescence focus assay to measure the levels of DNA damage in PC3 cells exposed to Scutellarin and/or cisplatin. An increase in the cellular levels of γ-H2AX foci is associated with the formation of double-strand breaks (DSBs) in DNA. γ-H2AX can therefore be considered as a marker of general DNA damage. We used specific antibodies to determine the levels of γ-H2AX foci (Fig. 5B). Scutellarin increased the sensitivity to cisplatin through induced DNA damage, as shown by the higher level of γ-H2AX expression (Fig. 5C).
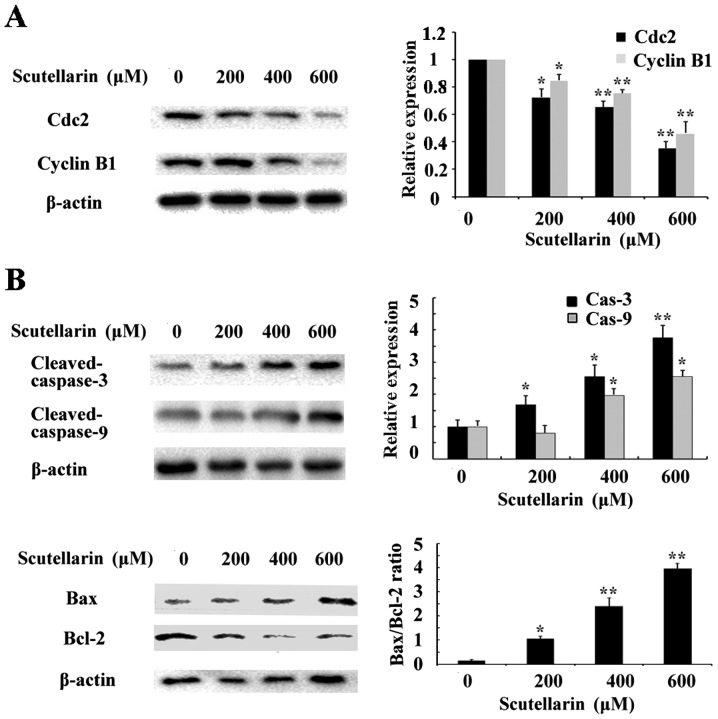
Scutellarin decreases cyclin B1 and Cdc2 expression
To investigate the mechanism underlying the cell cycle arrest induced by Scutellarin, we tested the effect of this compound on Cdc2 and cyclin B1 protein levels. As shown in Fig. 6A, western blot analysis revealed that Scutellarin decreased the protein levels of cyclin B1 and Cdc2 in a dose-dependent manner.
Figure 6.
Effects of Scutellarin on cyclin B1, Cdc2 and apoptosis-related protein expression. (A) The protein levels of cyclin B1 and Cdc2 were measured by western blotting. β-actin served as a loading control. (B) The protein levels of cleaved-caspase-3, cleaved-caspase-9, Bcl-2 and Bax were measured by western blotting. β-actin served as a loading control. All experiments were repeated three times. Data analysis was performed using ImageJ software by measuring the integrated band densities following background subtraction. Each bar represents the means ± SD calculated from three independent experiments. *Significant difference (P<0.05) and **extremely significant difference (P<0.01), compared to the control group.
Effects of Scutellarin on apoptosis-related proteins
Since Scutellarin induced apoptosis in prostate cancer cells, we further investigated the apoptosis-related proteins involved in this process by western blotting. The level of β-actin served as an internal control. We found that the expression of anti-apoptotic protein Bcl-2 inthe prostate cancer cells treated with Scutellarin was decreased in a dose-dependent manner (Fig. 6B). The expression of caspase-3 and caspase-9 were also assessed. The results showed that cleaved-caspase-3 and caspase-9 expression levels were upregulated in the Scutellarin-treated prostate cancer cells. These results suggest that Scutellarin activates the caspase-dependent pathway.
Discussion
Prostate cancer patients still face the challenging problem of chemotherapy resistance (18). Monomer compounds derived from herbal medicine have been demonstrated as therapeutic agents for current cancer treatment (19,20). Therefore, we explored the latent capability of Scutellarin on prostate cancer cells in the hope to discover new and effective drugs for prostate cancer patients. Scutellarin, a well known phytochemical composition of Scutellaria altissima L. was found to have widespread applications as an anti-inflammatory (21), anti-hepatitis (22) and antioxidation agent (23). Moreover, the anticancer effect of Scutellarin has been previously documented (16). Our results here explored the effects of Scutellarin on prostate cancer cells to develop a novel effective anticancer drug.
Monomer compounds extracted from plants have been reported to induce cell cycle arrest (24) and apoptosis (25). Proliferation inhibition and apoptosis induction can be trigger by cell cycle arrest in cancer cells (26). Cdc2 and cyclin B1 are involved in controlling the G2/M checkpoint (27), and some anticancer-drugs induce G2/M arrest by deregulating the expression of cyclin B1 and Cdc2 (28,29). The results in the present study indicated that treatment of the prostate cancer cells with Scutellarin induced G2/M arrest which was mainly due to a decrease in cyclin B1 and Cdc2 expression.
Various natural compounds have been found to prevent the growth of tumor cells by inducing apoptosis (30,31). Apoptosis is programmed cell death which plays a vital role in eliminating the mutated or increased growth of cancer cells. Therefore, induction of apoptosis has become a major target of most anticancer agents. Our data indicated that prostate cancer cells treated with Scutellarin displayed specific apoptotic morphological changes. In addition, flow cytometry data further indicated that the percentages of early and late apoptotic cells were markedly increased following treatment of Scutellarin. All these data indicated that Scutellarin induced apoptosis in prostate cancer cells.
Mitochondrial proteins directly activate cellular apoptotic programs (32). Bcl-2 protein is involved in the mitochondrial-associated apoptotic pathway (33). Downregulation of the Bcl-2 protein level leads to loss of mitochondrial membrane potential and triggers a series of apoptotic events such as activation of caspase-9 and caspase-3. In the present study, Scutellarin significantly decreased Bcl-2 protein expression accompanied by upregulation of cleaved-caspase-9 and −3 levels in prostate cancer cells. All these results indicated that Scutellarin treatment induced apoptosis through the mitochondrial-associated apoptotic pathway in prostate cancer cells.
Cisplatin [cis-diamminedichloroplatinum II (cDDP)] is one of the most effective cancer chemotherapeutic agents and is used in the treatment of many types of human malignancies. Cisplatin is considered to be a cytotoxic drug, for damaging DNA and inhibiting DNA synthesis, resulting in apoptosis via the mitochondrial death pathway or plasma membrane disruption (34). However, inherent tumor resistance is a major barrier to effective cisplatin therapy (35). Therefore, it is necessary to discover new antitumor mechanisms and enhance cisplatin sensitivity. In the present study, DNA damage was determined using comet assay and confirmed by detection of γH2AX, a biomarker for DNA double-strand breaks. We observed DNA damage after cisplatin and/or Scutellarin treatment, as indicated by an increase in tail length and accumulation of γH2AX. The results indicated that Scutellarin treatment enhanced chemosensitivity by strengthening cisplatin-induced DNA damage in prostate cancer cells.
In conclusion, we demonstrated that Scutellarin exerts an antitumor effect through inhibition of cell proliferation, induction of apoptosis and G2/M arrest, and Scutellarin also sensitized prostate cancer PC3 cells to chemotherapy. Our results suggest the potential use of Scutellarin as a new and effective antitumor treatment for prostate cancer patients.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (nos. 31572590 and 31502138) and Shandong Povince (BS2015NY001), and the Higher Educational Science and Technology Program of Shandong Province (J15LF03).
References
- 1.da Silva FC, Oliveira P. Tumor clone dynamics in lethal prostate cancer. Eur Urol. 2017;71:142–143. doi: 10.1016/j.eururo.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Jazayeri SB, Samadi DB. Prostate cancer in African Americans: Early oncological and functional outcomes after robotic prostatectomy. Int J Urol. 2017;24:236–237. doi: 10.1111/iju.13255. [DOI] [PubMed] [Google Scholar]
- 3.Zhang W, Meng Y, Liu N, Wen XF, Yang T. Insights into chemoresistance of prostate cancer. Int J Biol Sci. 2015;11:1160–1170. doi: 10.7150/ijbs.11439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keller ET. Prostate cancer cells metastasize to the hematopoietic stem cell niche in bone. Asian J Androl. 2011;13:622–623. doi: 10.1038/aja.2011.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Catalani E, Serafini F Proietti, Zecchini S, Picchietti S, Fausto AM, Marcantoni E, Buonanno F, Ortenzi C, Perrotta C, Cervia D. Natural products from aquatic eukaryotic microorganisms for cancer therapy: Perspectives on anti-tumour properties of ciliate bioactive molecules. Pharmacol Res. 2016;113:409–420. doi: 10.1016/j.phrs.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Tatullo M, Simone GM, Tarullo F, Irlandese G, Vito D, Marrelli M, Santacroce L, Cocco T, Ballini A, Scacco S. Antioxidant and antitumor activity of a bioactive polyphenolic fraction isolated from the brewing process. Sci Rep. 2016;6:36042. doi: 10.1038/srep36042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmadi A, Shadboorestan A, Nabavi SF, Setzer WN, Nabavi SM. The role of hesperidin in cell signal transduction pathway for the prevention or treatment of cancer. Curr Med Chem. 2015;22:3462–3471. doi: 10.2174/092986732230151019103810. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Ma Y, Zheng Y, Song J, Yang X, Bi C, Zhang D, Zhang Q. In vitro and in vivo anticancer activity of a novel puerarin nanosuspension against colon cancer, with high efficacy and low toxicity. Int J Pharm. 2013;441:728–735. doi: 10.1016/j.ijpharm.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Chai L, Guo H, Li H, Wang S, Wang YL, Shi F, Hu LM, Liu Y, Adah D. Scutellarin and caffeic acid ester fraction, active components of Dengzhanxixin injection, upregulate neurotrophins synthesis and release in hypoxia/reoxygenation rat astrocytes. J Ethnopharmacol. 2013;150:100–107. doi: 10.1016/j.jep.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 10.Grzegorczyk-Karolak I, Gołąb K, Gburek J, Wysokińska H, Matkowski A. Inhibition of advanced glycation end-product formation and antioxidant activity by extracts and polyphenols from Scutellaria alpina L. and S. altissima L. Molecules. 2016;21 doi: 10.3390/molecules21060739. pii: E739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bozov PI, Coll J. Neo-clerodane diterpenoids from Scutellaria altissima. Nat Prod Commun. 2015;10:13–16. [PubMed] [Google Scholar]
- 12.Zhao Q, Chen XY, Martin C. Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Sci Bull. 2016;61:1391–1398. doi: 10.1007/s11434-016-1136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi W, No RH, Kwon HS, Lee HY. Enhancement of skin anti-inflammatory activities of Scutellaria baicalensis extract using a nanoencapsulation process. J Cosmet Laser Ther. 2014;16:271–278. doi: 10.3109/14764172.2014.946051. [DOI] [PubMed] [Google Scholar]
- 14.Shang YZ, Qin BW, Cheng JJ, Miao H. Prevention of oxidative injury by flavonoids from stems and leaves of Scutellaria baicalensis Georgi in PC12 cells. Phytother Res. 2006;20:53–57. doi: 10.1002/ptr.1802. [DOI] [PubMed] [Google Scholar]
- 15.Mallick A, More P, Syed MM, Basu S. Nanoparticle-mediated mitochondrial damage induces apoptosis in cancer. ACS Appl Mater Interfaces. 2016;8:13218–13231. doi: 10.1021/acsami.6b00263. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Huang D, Gao Z, Lv Y, Zhang L, Cui H, Zheng J. Scutellarin inhibits cell migration by regulating production of αvβ6 integrin and E-cadherin in human tongue cancer cells. Oncol Rep. 2010;24:1153–1160. doi: 10.3892/or_00000967. [DOI] [PubMed] [Google Scholar]
- 17.Adam-Zahir S, Plowman PN, Bourton EC, Sharif F, Parris CN. Increased γ-H2AX and Rad51 DNA repair biomarker expression in human cell lines resistant to the chemotherapeutic agents nitrogen mustard and cisplatin. Chemotherapy. 2014;60:310–320. doi: 10.1159/000430086. [DOI] [PubMed] [Google Scholar]
- 18.Madan RA, Pal SK, Sartor O, Dahut WL. Overcoming chemotherapy resistance in prostate cancer. Clin Cancer Res. 2011;17:3892–3902. doi: 10.1158/1078-0432.CCR-10-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cao H, Mu Y, Li X, Wang Y, Chen S, Liu JP. A systematic review of randomized controlled trials on oral Chinese herbal medicine for prostate cancer. PLoS One. 2016;11:e0160253. doi: 10.1371/journal.pone.0160253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohammadi A, Mansoori B, Aghapour M, Baradaran PC, Shajari N, Davudian S, Salehi S, Baradaran B. The herbal medicine Utrica dioica inhibits proliferation of colorectal cancer cell line by inducing apoptosis and arrest at the G2/M phase. J Gastrointest Cancer. 2016;47:187–195. doi: 10.1007/s12029-016-9819-3. [DOI] [PubMed] [Google Scholar]
- 21.Yuan Y, Zha H, Rangarajan P, Ling EA, Wu C. Anti-inflammatory effects of Edaravone and Scutellarin in activated microglia in experimentally induced ischemia injury in rats and in BV-2 microglia. BMC Neurosci. 2014;15:125. doi: 10.1186/s12868-014-0125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niu C, Sheng Y, Yang R, Lu B, Bai Q, Ji L, Wang Z. Scutellarin protects against the liver injury induced by diosbulbin B in mice and its mechanism. J Ethnopharmacol. 2015;164:301–308. doi: 10.1016/j.jep.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 23.Wang Z, Yu J, Wu J, Qi F, Wang H, Wang Z, Xu Z. Scutellarin protects cardiomyocyte ischemia-reperfusion injury by reducing apoptosis and oxidative stress. Life Sci. 2016;157:200–207. doi: 10.1016/j.lfs.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 24.Cai F, Li J, Liu Y, Zhang Z, Hettiarachchi DS, Li D. Effect of ximenynic acid on cell cycle arrest and apoptosis and COX-1 in HepG2 cells. Mol Med Rep. 2016;14:5667–5676. doi: 10.3892/mmr.2016.5920. [DOI] [PubMed] [Google Scholar]
- 25.Gao Y, Wang X, He C. An isoflavonoid-enriched extract from Pueraria lobata (kudzu) root protects human umbilical vein endothelial cells against oxidative stress induced apoptosis. J Ethnopharmacol. 2016;193:524–530. doi: 10.1016/j.jep.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Forster L, Cornwall S, Finlayson J, Ghassemifar R. Cell cycle, proliferation and apoptosis in erythroblasts cultured from patients with β-thalassaemia major. Br J Haematol. 2016;175:539–542. doi: 10.1111/bjh.13875. [DOI] [PubMed] [Google Scholar]
- 27.Chang CC, Hung CM, Yang YR, Lee MJ, Hsu YC. Sulforaphane induced cell cycle arrest in the G2/M phase via the blockade of cyclin B1/CDC2 in human ovarian cancer cells. J Ovarian Res. 2013;6:41. doi: 10.1186/1757-2215-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qi LW, Zhang Z, Zhang CF, Anderson S, Liu Q, Yuan CS, Wang CZ. Anti-colon cancer effects of 6-Shogaol through G2/M cell cycle arrest by p53/p21-cdc2/cdc25A crosstalk. Am J Chin Med. 2015;43:743–756. doi: 10.1142/S0192415X15500469. [DOI] [PubMed] [Google Scholar]
- 29.Lohberger B, Leithner A, Stuendl N, Kaltenegger H, Kullich W, Steinecker-Frohnwieser B. Diacerein retards cell growth of chondrosarcoma cells at the G2/M cell cycle checkpoint via cyclin B1/CDK1 and CDK2 downregulation. BMC Cancer. 2015;15:891. doi: 10.1186/s12885-015-1915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Millimouno FM, Dong J, Yang L, Li J, Li X. Targeting apoptosis pathways in cancer and perspectives with natural compounds from mother nature. Cancer Prev Res. 2014;7:1081–1107. doi: 10.1158/1940-6207.CAPR-14-0136. [DOI] [PubMed] [Google Scholar]
- 31.Zhang A, He W, Shi H, Huang X, Ji G. Natural compound oblongifolin C inhibits autophagic flux, and induces apoptosis and mitochondrial dysfunction in human cholangiocarcinoma QBC939 cells. Mol Med Rep. 2016;14:3179–3183. doi: 10.3892/mmr.2016.5591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song XF, Tian H, Zhang P, Zhang ZX. Expression of Cyt-c-mediated mitochondrial apoptosis-related proteins in rat renal proximal tubules during development. Nephron. 2016;135:77–86. doi: 10.1159/000450585. [DOI] [PubMed] [Google Scholar]
- 33.Wang Q, Zhang L, Yuan X, Ou Y, Zhu X, Cheng Z, Zhang P, Wu X, Meng Y, Zhang L. The relationship between the Bcl-2/Bax proteins and the mitochondria-mediated apoptosis pathway in the differentiation of adipose-derived stromal cells into neurons. PLoS One. 2016;11:e0163327. doi: 10.1371/journal.pone.0163327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hardie ME, Kava HW, Murray V. Cisplatin analogues with an increased interaction with DNA: Prospects for therapy. Curr Pharm Des. 2016;22:6645–6664. doi: 10.2174/1381612822666160831101529. [DOI] [PubMed] [Google Scholar]
- 35.Kim SH, Ho JN, Jin H, Lee SC, Lee SE, Hong SK, Lee JW, Lee ES, Byun SS. Upregulated expression of BCL2, MCM7, and CCNE1 indicate cisplatin-resistance in the set of two human bladder cancer cell lines: T24 cisplatin sensitive and T24R2 cisplatin resistant bladder cancer cell lines. Investig Clin Urol. 2016;57:63–72. doi: 10.4111/icu.2016.57.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]