Abstract
This review highlights recent advances in research addressing intimate partner relationships and health. Consideration of the strong mutual influences that the members of a couple have on each other's mental and physical health trajectories provides a new way to view the health implications of couples’ convergence or interdependence; marital closeness can have a clear downside when one partner has mental or physical health problems. Couples’ interconnectedness can also be leveraged to promote better treatment outcomes. Major themes addressed include the pivotal role of depression, as well as the importance of gender differences in the pathways from the marital relationship to physiological functioning and health. The health risks and benefits of support are weighed. Additionally, two prominent emerging paths from marital distress to poor health are emphasized: sleep problems, and metabolic alterations that promote obesity and its comorbidities.
Keywords: marriage, depression, convergence, interdependence, sleep, metabolism
Introduction
Married people have better mental and physical health than unmarried people, on average (Kiecolt-Glaser and Newton, 2001, Robles et al., 2014). Morbidity and mortality are reliably lower for the married than the unmarried across a variety of acute and chronic conditions, including such diverse health threats as cancer, heart attacks, and surgery (Aizer et al., 2013, Neuman and Werner, 2015, Engstrom et al., 2006).
However, the simple presence of a spouse is not necessarily protective; a troubled marriage is itself a prime source of stress, and simultaneously limits the partner's ability to seek support in other relationships (Coyne and DeLongis, 1986). Indeed, the relationship between life satisfaction and marital quality is stronger than life satisfaction’s ties to either one's job or one’s health (Heller et al., 2004). Marital quality clearly colors one’s overall sense of well-being, and marital distress elevates health risks (Kiecolt-Glaser and Newton, 2001, Robles et al., 2014).
A recent meta-analysis reported that the relationships between marital quality and various health outcomes had effect sizes similar in magnitude to the reported effects of diet and exercise on clinical health endpoints (Robles et al., 2014). Although the number of studies for specific health problems limited the conclusions that could be drawn, a notable finding was the lower risk for mortality associated with better marital quality, with the largest relationships found in studies addressing chronic illnesses (Robles et al., 2014).
In this paper we highlight advances in research addressing intimate partner relationships and health. To complement and extend the extensive reviews that have documented marital discord's negative health consequences (Kiecolt-Glaser and Newton, 2001, Robles et al., 2014), we discuss how couples mutually influence each other's mental and physical health trajectories; we consider the health and treatment implications of couples’ convergence or interdependence in health behaviors as well as in their mental and physical health. We address marital functioning’s indirect influences on health outcomes through depression and health behaviors. Following up on major themes that we have addressed previously, we emphasize the importance of differentiating positive and negative dimensions of marital functioning, specifically examining the health risks and benefits of support, as well as gender differences in the pathways from the marital relationship to physiological functioning and health (Kiecolt-Glaser and Newton, 2001). We highlight two prominent emerging paths from marital distress to poor health: sleep problems, and metabolic alterations that promote obesity, metabolic syndrome, and diabetes. Additionally, we focus on evidence that more satisfying or closer marital relationships also increase health risks; marital closeness can have a clear downside when one spouse has mental or physical health problems.
Depression, a foundational risk factor
Distressed marital relationships and depression often travel in tandem. Both syndromal depression and depressive symptoms are strongly associated with marital distress (Beach, 2014). The strength of the tie is sizable, e.g., one study found a 10-fold increase in risk for depressive symptomatology associated with marital discord (O'Leary et al., 1994); similarly, data from a large epidemiological study demonstrated that unhappy marriages were a potent risk factor for major depressive disorder for both men and women, associated with a 25-fold increase over untroubled marriages (Weissman, 1987). The relationship is bidirectional: distressed marriages enhance depressive symptoms, and depression promotes poorer marital quality (Beach, 2014). The stress generation model illustrates how this association emerges: depression contributes to marital discord, which enhances other stressors and serves to maintain or exacerbate symptoms (Foran et al., 2015).
The association of marital distress with depression has important implications for physical functioning. Depression alters multiple biological systems (e.g., endocrine, immune, cardiovascular, metabolic, neurocognitive), and these alterations are sufficient to enhance a variety of health threats, including premature mortality (Hughes et al., 2016, Jaremka et al., 2013). Depression promotes inflammation, one central pathway to poor health (Kiecolt-Glaser et al., 2015a). Heightened inflammation characterizes a number of disorders and systemic diseases including cardiovascular disease, diabetes, metabolic syndrome, rheumatoid arthritis, asthma, multiple sclerosis, chronic pain, and psoriasis; each of these also features an elevated risk for depression (Shelton and Miller, 2010, Slavich and Irwin, 2014). In addition to physiological alterations, depressed individuals are also more likely to have poorer health habits including a greater propensity for alcohol and drug abuse, inadequate sleep and nutrition, and less exercise, all of which have negative health influences in their own right (Kiecolt-Glaser et al., 2010).
Furthermore, depression can sensitize the inflammatory response, thus effectively promoting larger cytokine increases in response to stressors or pathogens (Glaser et al., 2003, Fagundes et al., 2013). Together, depression and stress contribute to a greater risk for infection, prolonged infectious episodes, and delayed wound healing; all processes that can fuel sustained proinflammatory cytokine production (Glaser and Kiecolt-Glaser, 2005).
By promoting depression and emotional stress responses, marital distress can effectively modulate secretion of proinflammatory cytokines both directly (via CNS/neural/endocrine/immune biobehavioral pathways), and indirectly, through behavioral changes. Through these pathways, depression and stressful marital experiences contribute to both acute and chronic proinflammatory cytokine production (Kiecolt-Glaser et al., 2005, Kiecolt-Glaser et al., 2003).
Couples’ health concordance, for good or ill
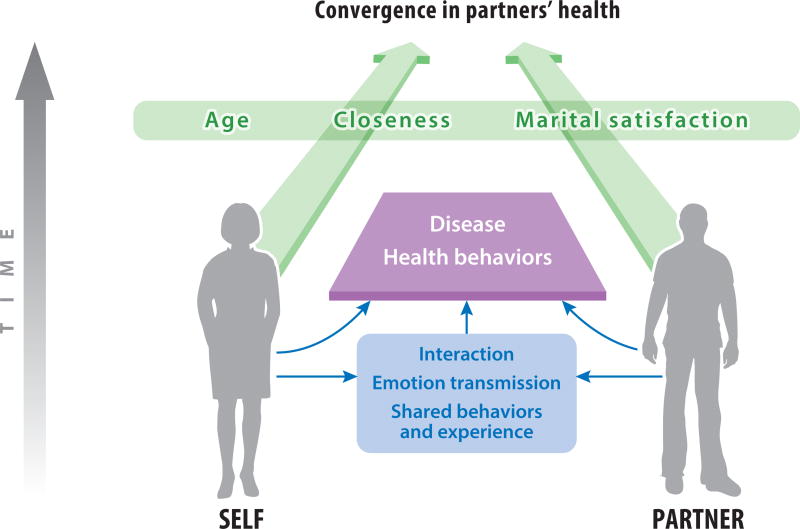
A growing literature addresses how couples mutually influence each other’s mental and physical health trajectories (Hoppmann et al., 2011a). As depicted in Figure 1, couples' health and health behaviors are often similar and tend to converge over time (Leong et al., 2014). This occurs in part because of assortative mating: people typically choose a partner who is similar in terms of attitudes and demographics, as well as health-related behaviors like diet, physical activity, smoking, alcohol consumption, and BMI (Leong et al., 2014, Jackson et al., 2015). The shared resources hypothesis speculates that concordance may be a function of the fact that couples share a lifestyle as well as common stressors; spouses typically have a common living environment, they pool resources, they eat together, and they share a social network. Shared major and minor life events contribute to behavioral convergence. Spouses’ daily life activities are intertwined, and each partner's personal attributes--mood, attitudes, behavior, health, stresses, and lifestyle--affect both spouses. Thus, couples’ mutual influence can be beneficial or harmful to health behaviors and health (Meyler et al., 2007).
Figure 1.
Conceptual framework summarizing the pathways by which partners’ health may converge over time. Partners influence each other’s health behaviors and eventual development of disease directly through interaction, emotion transmission, and shared behavior and experience. Partners’ level of closeness, their marital satisfaction, and age may modify their degree of convergence.
In accord with lifespan theories, the links between partners’ happiness trajectories across 35 years were substantially stronger than those observed in random pairs of women and men (Hoppmann et al., 2011b). Furthermore, spouses’ joint happiness explained much of the inter-individual differences in happiness.
Survey data from aging adults showed that wives’ and husbands’ quality of life traveled together over time; furthermore, each partner’s self-reported physical health and cognition predicted their spouses’ baseline quality of life, even after controlling for their own health and cognition (Bourassa et al., 2015b). In turn, better quality of life scores were related to longer-term health outcomes including better cardiovascular health, better sleep, and lower all-cause mortality (Bourassa et al., 2015b). Indeed, interdependence in couples' quality of life can persist even after a partner's death; among couples in which one spouse had died, the surviving partner’s later quality of life was associated with the deceased’s prior life quality (Bourassa et al., 2015a).
Researchers have documented strong spousal associations in exercise, smoking, alcohol consumption, and diet (Jackson et al., 2015). For example, a diary study showed that on days when spouses took more steps, osteoarthritis patients were more physically active as well (Martire et al., 2013b). Convergence on such key health behaviors has implications for other health indices; a systematic review reported positive spousal concordance for major coronary risk factors including diastolic blood pressure, triglycerides, total and low-density lipoprotein cholesterol, smoking, body mass index, and waist/hip ratio (Di Castelnuovo et al., 2009).
In addition, changes in one spouse’s behavior can prompt change in their partner. Couples in the English Longitudinal Study of Ageing, a population-based study of middle-aged and older adults in the United Kingdom, were more likely to stop smoking, increase physical activity, and lose 5% or more of their weight if their partner made the same positive change (Jackson et al., 2015). The impact on health behaviors can be substantial; longitudinal data show that when one spouse becomes obese, their partner’s risk for obesity almost doubles (Cobb et al., 2015). In fact, couples who live together for longer time periods become more similar in obesity-related behaviors, including low levels of physical activity and high rates of sedentary behavior (The and Gordon-Larsen, 2009).
Moreover, one spouse can benefit from an intervention delivered to their partner, a “ripple effect” (Gorin et al., 2008). For example, in a trial that evaluated how intentional weight loss affected cardiovascular outcomes in overweight people with type 2 diabetes, spouses of intervention group participants lost more weight than the partners of usual care condition participants, and the spouses’ weight loss was significantly correlated (Gorin et al., 2008). Similarly, husbands of women in the low-fat intervention arm of the Women’s Health Trial reduced their body fat and weight more than the husbands of control arm women (White et al., 1991).
Not surprisingly, spouses’ health behavior concordance can translate into disease risks (Monserud and Peek, 2014, Hoppmann et al., 2011a, Gerstorf et al., 2009). When one partner has a history of diabetes, spousal risk for diabetes is increased 26%; a spousal history of either diabetes or prediabetes confers a two-fold risk for the partner (Leong et al., 2014). When one spouse has metabolic syndrome, his or her spouse has roughly a 30% greater chance of also having metabolic syndrome (Kim et al., 2006). Among older Mexican American couples, a history of hypertension, arthritis, or cancer was associated with higher odds that the spouse would have the same condition. For example, having a partner with arthritis almost tripled the spouse's odds for arthritis (Stimpson and Peek, 2005). People whose partners have asthma, peptic ulcer disease, or depression have a 70% or greater increased risk themselves for these conditions, even after controlling for partners’ age, smoking, and obesity (Hippisley-Cox et al., 2002). Spouses of hypertensive patients have a two-fold increased risk of hypertension even when age, BMI, and diabetes are controlled (Hippisley-Cox and Pringle, 1998).
A large population-based, nested case-control study showed that the risk for developing physician-diagnosed hay fever was more than twice as great in people who lived with a partner with hay fever compared to people living with an unaffected partner. Furthermore, the longer the partners lived together, the greater the risk: compared to couples who had lived together for 1–11 years, the odds ratio for those who were together 12–23 years rose to 1.8, increasing to 7.4 for 24–35 years, and then rapidly escalating to 13.7 for those in the longest term relationships, 36–54 years (Schafer et al., 2004).
Married couples’ behavior patterns influence both spouses, a key assumption of interdependence theory, and one partner’s functioning can influence both spouses (Kelly and Thibaut, 1978). Crossover or spillover effects can arise in one partner following a spouse’s negative experience, particularly when one member of the couple is experiencing health problems (Bourassa et al., 2015b). In a diary study, patients diagnosed with both diabetes and osteoarthritis had heightened blood glucose problems and arthritis severity on days when their disease-free spouses reported worse physical symptoms (Yorgason et al., 2012). Relatedly, emotional transmission happens when a partner’s own personal experiences provoke emotional responses and behaviors, which, in turn, affect the spouse (Larson and Almeida, 1999). Indeed, both mood convergence and emotional contagion hypotheses suggest that the interdependence of life with a partner promotes shared emotions.
Marital contagion of depressive symptoms and distress has been extensively documented. Living with a depressed spouse clearly alters the partner's mood. Higher levels of depressive symptoms in one spouse are associated with higher levels of depressive symptoms in his or her partner; this reciprocal relationship has been a consistent theme throughout a number of studies. Furthermore, longitudinal studies suggest that increases in one partner's depressive symptoms over time are associated with increments in the spouse's symptoms (Pruchno et al., 2009, Monin et al., 2016). Diary studies suggest that negative and high-arousal emotions are particularly contagious between partners (Schoebi, 2008, Saxbe and Repetti, 2010).
Major and minor life events that happen to one spouse can influence the mental health of both partners; for example, research has confirmed convergence following such health events as a cancer diagnosis and treatment, cardiomyopathy, heart failure, coronary heart disease, erectile dysfunction, and infertility, as well as nonhealth events like job loss (Meyler et al., 2007). Data from both cross-sectional and longitudinal studies show that depressive symptoms among older adults experiencing vision loss (Strawbridge et al., 2007), prostate cancer (Berg et al., 2011), and arthritis (Stephenson et al., 2014) are also experienced by their spouse. Lung cancer patients’ declining physical function predicted increases in spouse depressive symptoms over one year (Lyons et al., 2014). Similarly, longitudinal data from the National Survey of Families and Households addressed the effects of a spouse's illness on depressive symptoms in middle-aged and older married adults. People whose spouse had become ill or stayed ill because of a chronic disease or physical disability reported higher levels of depressive symptoms at the 10 year follow-up; in contrast, depressive symptoms were lower at follow-up than at baseline among those whose spouses’ health improved (Bookwala, 2014).
Depressive symptoms and the ability to perform activities of daily living have reciprocal influences on each other among older adults; functional limitations increase risk for depression, and depression increases the risk for functional limitations (Hoppmann et al., 2011a). For example, frailty, characterized by weakness, slowness, and exhaustion, presages elevated risks for depression, disability, falls, hospitalization, and early mortality (Monin et al., 2016). Over time, people’s depression predicted their own later frailty, and frailty predicted subsequent depression (Monin et al., 2016). In couples, frailty in one spouse predicted frailty in their partner; moreover, higher levels of depressive symptoms in one spouse predicted greater depressive symptoms in the partner (Monin et al., 2016). Similarly, longitudinal data from older Mexican American couples showed that functional limitations in one spouse were linked with higher levels of depressive symptoms in their partner (Monserud and Peek, 2014). Mechanistically, both depression and frailty have inflammatory correlates, and chronic inflammation has been suggested as one key biological mechanism that may fuel declines in physical function that lead to frailty, disability, and, ultimately, death (Ershler and Keller, 2000).
Self-rated health -- how healthy one feels -- predicts physical disability, inflammation, and mortality (Pruchno et al., 2009, Christian et al., 2011). In a longitudinal study of self-rated health and depressive symptoms in patients with end-stage renal disease, changes in the patient's self-rated health increased the spouse's depressive symptoms, and these effects were greater for the spouse than changes in his or her own self-rated health (Pruchno et al., 2009).
Marital Satisfaction, Relationship Closeness, and Age Influence Convergence-Related Risk
Surprisingly, little of the research has addressed how either marital satisfaction or relationship closeness impacts convergence-related risk. The limited data described below speak to their importance.
Marital satisfaction moderates the dynamic links between partners’ health. The health of people in higher-quality marriages may be at greater risk when their partner is suffering (Hoppmann and Gerstorf, 2009). In longitudinal data from community-dwelling older couples, husbands’ cognitive impairment was associated with subsequent poorer health and well-being among their wives, but only for the 52% of wives who reported few or no marital problems (Strawbridge et al., 2009). Global marital satisfaction may serve as an interpretive backdrop, altering the partner’s appraisals of the impaired spouse’s behaviors, and thereby their functional significance for the partner’s health (Turk et al., 1992).
Marital satisfaction is moderately correlated with relationship closeness (Aron et al., 1992), another important relational dimension that may alter spillover and health convergence. Closer relationships may involve greater involvement in the spouse's daily activities compared to relationships that are not as close. Also, feeling close to one’s partner can promote more empathic responding as well as greater contagion of negative affect (Berg et al., 2008, Cialdini et al., 1997); consequently, adverse health changes in one spouse may have a particularly strong impact on close partners. For example, in a sample of osteoarthritis patients and their spouses, greater knee pain during the day predicted partner’s poorer sleep quality that night, and these effects were strongest among couples in closer relationships (Martire et al., 2013a). Other data from this cohort showed that greater relationship closeness exacerbated the impact of increased patient illness severity on their partner’s positive affect and depressive symptoms over six months (Polenick et al., 2015), consistent with previous studies that showed stronger transmission of depressive symptoms in closer couples (Tower and Kasl, 1995, Tower and Kasl, 1996).
Exposure to a partner’s disease-related pain can function as a potent stressor, influencing the spouse’s physical and psychological health (Schulz et al., 2009). For example, spouses were adversely affected by witnessing their partner’s pain; the spouse’s blood pressure increased more in response to arthritis patient’s suffering than to a stranger’s pain (Monin et al., 2010).
These studies illustrate how even close and satisfying relationships can have a clear downside, because the very fact that spouses are close and happy means that one spouse's mental or physical health problems are more likely to impact their partner, perhaps through more time spent together, greater willingness to engage the ill spouse despite stressors, and more intimate emotional connection to the ill spouse’s suffering. Among prostate cancer patients and their wives, negative affect was heightened when couples had managed daily stressors together, which underscores the risk of negative emotion transmission when both partners are closely involved (Berg et al., 2011). The closer the relationship, the greater the potential loss, and the greater the risk for the unimpaired partner’s mental and physical health.
Older adults are at greatest risk when a spouse is ill for several reasons. Older adults typically put more time and energy into close personal relationships rather than broader social networks (Charles and Carstensen, 2010), and thus partner functioning would have a greater impact than among younger people. Among older couples, social-activity trajectories are interrelated, strengthened by the partner's cognitive, physical, and affective resources (Hoppmann et al., 2008). Concordance is likely to be greater in longer-term marriages; couples have learned to function as a team throughout their history of joint experiences (Gerstorf et al., 2009). Compared to younger adults, older adults' marriages are typically closer (Hoppmann and Gerstorf, 2009). Older couples in longer-term marriages have survived many challenges, they have a long history of shared experiences and joint roles such as parenthood through their decades together (Hoppmann and Gerstorf, 2009). This interdependence can be problematic when adverse changes arise for one partner (Gerstorf et al., 2009). Greater spousal closeness in the face of one partner’s health crisis may thus spread poorer health, particularly among older couples.
Marital Support and Capitalization
Certainly, the pathways linking marital processes to health are complex. While partners may expose each other to health risks via shared health behaviors and emotion transmission, they may also influence health outcomes by exchanging support.
Supportive behaviors of one spouse may lessen symptoms in their partner; for example, greater satisfaction with the partner's behavior was related to lower pain ratings in arthritis patients (Holtzman and Delongis, 2007). Arthritis patients whose partners had more confidence in their illness management improved more in their physical function, disease severity, and activity levels compared to those with less confident spouses, in part through changes in partner responses to patient pain (Hemphill et al., 2016, Gere et al., 2014).
On the other hand, support that inadvertently undermines independence and self-efficacy to maintain healthy behaviors can have poor health consequences. For example, male osteoarthritis patients reduced their physical activity on days when wives pressured them to be more active (Martire et al., 2013b). Also, patients who received more unwanted spouse support reported worse arthritis management (Martire et al., 2002). Support delivered in a critical, controlling, or coercive way can also have negative results: a diary study found that on days when spouses used coercion in the absence of encouragement Type 2 diabetes patients were less physically active (Khan et al., 2013).
In addition to influencing health behaviors, partner support may directly alter physiological reactivity to stressors. For instance, people who received more encouragement and validation from their partner after a stressor experienced faster reductions in cortisol levels than those who were met with less sensitive and more hostile responses (Meuwly et al., 2012). In a neuroimaging study, neural reactions to a painful stimulus were less pronounced when participants held their spouse’s hand instead of a stranger’s, and maritally satisfied people reacted even less than dissatisfied participants (Coan et al., 2006).
Beyond the effects of discrete support behaviors, perceiving one’s spouse as generally responsive may confer health benefits. Perceived partner responsiveness--the extent to which people feel that their partner understands, cares for, and validates them—has emerged as a predictor of health in recent studies. For example, higher mortality rates were associated with more received partner emotional support among those who described their partner as low on responsiveness (Selcuk and Ong, 2013). However, having a partner described as very responsive protected people from the mortality risk associated with higher received partner support. Likewise, in a representative sample of 1078 married or cohabiting adults, greater perceived partner responsiveness at baseline was related to higher awakening cortisol and steeper diurnal cortisol slopes 10 years later, but not total cortisol production (Slatcher et al., 2015). However, a prospective study of osteoarthritis patients found that perceived partner responsiveness did not explain improvements in post-surgical knee recovery associated with partner support (Khan et al., 2009). Understanding the interplay of support behaviors and the general impressions that shape their interpretation represents a promising avenue for future work.
Spouses’ response to positive events, or capitalization support, should also be further examined as a candidate mechanism of marriage’s health effects. Among romantic partners in a lab study, partners’ supportive responses increased positive emotions and facial expressions but not skin conductance responses (Monfort et al., 2014). Future studies might expand the range of physiological outcomes to determine the scope of capitalization’s effects.
Gender Influences
We have focused on depression as a key pathway between marital distress and health. In this context, the consistent finding that women have higher rates of depression than men has multiple implications for marriage-related health outcomes. As described earlier, depression has close ties to inflammation (Kiecolt-Glaser et al., 2015a); this link may be particularly relevant for women for several reasons. First, inflammation-induced mood and behavior changes appear to be more prominent among women than men. For example, women respond to transient elevations in inflammation with stronger feelings of loneliness and social disconnection than men, a characteristic that likely contributes to the 2:1 ratio of women to men in depressive disorders (Moieni et al., 2015). Additionally, prior depression, somatic symptomatology, interpersonal stressors, childhood adversity, obesity, and physical inactivity are all factors that elevate inflammation, and women have disproportionately higher representation than men in each of these domains (Derry et al., 2015). Relationship-related distress has stronger ties to inflammation among women than men (Derry et al., 2015), and the relationship between depression and marital quality is stronger among women than men (Whisman, 2001). Accordingly, there are multiple reasons to believe that these gender-related differences in depression lead to greater health risks for women than for men in marriage.
Some evidence suggests that husbands' cognitive functioning can predict changes in wives' cognition, but not the reverse (Gerstorf et al., 2009, Strawbridge et al., 2009). One hypothesis used to explain this unidirectional effect suggests that the increasing time demands that would lead the wife to curtail social and other activities that provide cognitive stimulation in favor of more time at home (Gerstorf et al., 2009).
Auditory and visual impairments become increasingly prevalent with age. Hearing impairments in one spouse also affect the partner's health and well-being. As with cognitive functioning, wives were more negatively affected by their husbands' hearing loss than vice versa (Wallhagen et al., 2004).
Vision impairments can lead to poor problems in communication, as well as broader difficulties with psychosocial functioning (Strawbridge et al., 2007). In longitudinal data with older adults from the Alameda County Study, impaired vision in one spouse adversely impacted his or her own depression, physical functioning, and well-being, and the partner’s data showed negative changes on these same dimensions. After adjusting for the impact of one's own visual impairment, the spousal consequences for physical functioning, depression, and well-being were greater among wives than husbands (Strawbridge et al., 2007).
Within the dementia caregiving literature, spousal caregivers’ stress has been well-documented. Women suffer greater adverse effects when caregiving for a husband with dementia than men experience when they become caregivers (Hagedoorn et al., 2001). Although such intensive caregiving substantially increases health risks (Glaser and Kiecolt-Glaser, 2005), the data reviewed above suggest that even nondisabling conditions can raise the stakes.
A meta-analysis of distress in couples coping with cancer reported a moderate correlation of .29 between patients and partners. Nonetheless, regardless of whether they were the person with cancer or the person’s partner, women consistently reported greater distress than men (Hagedoorn et al., 2008).
Husbands' high blood pressure and stroke history were related to higher levels of depressive symptoms among their wives; however wives' health problems were not related to husbands' depressive symptoms (Ayotte et al., 2010).
Similarly, among a community-based sample of 995 older couples in which neither, one, or both partners had a chronic disease, women’s psychological distress was linked with both her own and her husband’s condition, whereas men’s distress was only related to his own health (Hagedoorn et al., 2001). Moreover, despite the fact that male patients reported fewer physical problems than female patients, the husband’s health status augmented wives’ distress, but wives’ health problems did not increase husbands’ distress.
Individuals with chronic pain often rate their pain and disability differently than their partner. Women’s perceptions of their husbands' thoughts and feelings better matched husbands’ responses compared to husbands' ratings of wives' thoughts and feelings (Cano et al., 2005).
These findings echo the gender differences we have highlighted previously (Kiecolt-Glaser and Newton, 2001). As discussed elsewhere, past studies show that wives respond more to the husband’s chronic illness than vice versa, and this greater influence means that wives are also more likely to be affected (Berg and Upchurch, 2007). However, the origin of this gender-based vulnerability is unclear; this area of research must continue to be reevaluated as new cohorts of couples marry and divorce, and as the demographic face of marriage evolves (Amato et al., 2007, Cherlin, 2010).
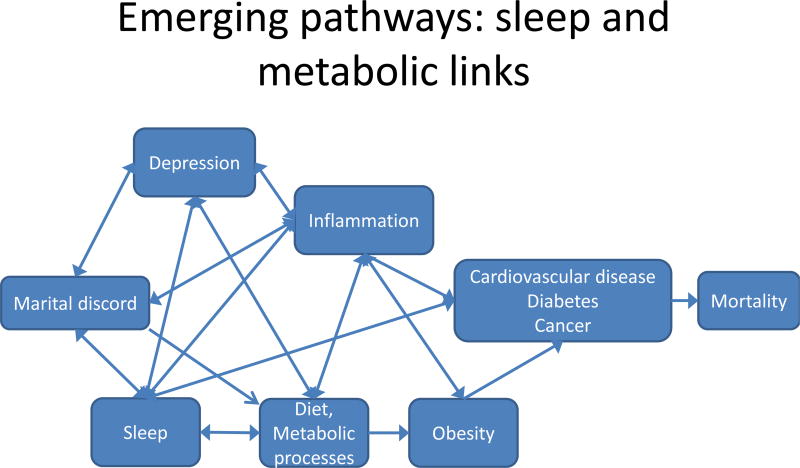
Emerging paths from marital distress to health: Sleep and metabolic changes (Figure 2)
Figure 2.
Model that links marital discord to chronic illness and mortality through emerging mechanisms, including sleep, diet, metabolic processes, and obesity.
Marital discord and sleep
Poor sleep contributes to cardiovascular disease, cancer, obesity, diabetes, and premature death (Cappuccio et al., 2010, Consensus Conference et al., 2015). Though married people sleep better than singles on average (Chen et al., 2015), marital discord jeopardizes sleep quality and quantity (Chen et al., 2015, Troxel et al., 2009). Those in more strained marriages report greater insomnia than their happily married counterparts (Chen et al., 2015, Troxel et al., 2009) and experience increased sleep disturbance over time. For instance, unhappily married older adults’ sleep problems worsened across four years (Yang et al., 2013). More destructive and less constructive conflict spurred declines in actigraphy-assessed sleep quality and duration over one year (El-Sheikh et al., 2015). Marital discord also disturbs day-to-day sleep: on days when couple interactions were more negative, women experienced worse actigraphy-assessed sleep that night (Hasler and Troxel, 2010). Moreover, the sleep-insulting effects of marital discord are contagious; wives’ report of more negative interaction quality also led to husbands’ worse sleep at night (Hasler and Troxel, 2010).
The link between marital discord and sleep exhibits a dose-response relationship: more pernicious conflict elevates the risk for sleep disturbance. Divorced victims of intimate partner violence suffered worse lingering sleep problems than did unvictimized divorcees, and those who experienced prolonged aggression slept even worse than women subjected to less frequent violence (Newton et al., 2016).
A marital therapy intervention produced mixed effects for couples’ insomnia symptoms (Troxel et al., 2016). Though therapy improved marital satisfaction in both partners compared to no-treatment controls, only husbands’ risk for insomnia lessened three months later, and this satisfaction-related sleep benefit arose irrespective of treatment. Thus, marital discord is strongly established as a predictor of sleep, but there is not clear evidence that relieving discord resolves sleep problems.
Beyond direct conflict and discord, exposure to one’s partner’s stressors impacts sleep. As described earlier, partners slept worse on days when osteoarthritis patients had more severe pain, particularly those who felt close in the relationship (Martire et al., 2013a). For patients, negative mood led to worse sleep when partners responded to pain in hostile or overzealous ways (Song et al., 2015). On the other hand, leveraging relationship resources may protect against stress-related sleep problems. For instance, on days when couples disclosed their feelings they enjoyed better sleep and fewer negative-mood-related sleep disruptions at night (Kane et al., 2014).
Bidirectional exacerbation: Sleep induces conflict
Sleep loss and poor sleep intensify conflict. In a diary study, when men slept more poorly they reported more negative partner interactions the next day (Hasler and Troxel, 2010). Likewise, couples who slept poorly over 14 nights reported more daily conflict with their partners than those with better sleep quality (Gordon and Chen, 2014). Worse sleep also translated into more negative affect and less positive affect during a marital problem discussion; moreover, partners were less able to accurately assess either their emotions or those of their partner. These data show that just one partner’s poor sleep affects not only his or her mood and empathic accuracy but also the partner’s affect and accuracy. Yang and colleagues found that more sleep problems related to lower marital quality four years later (Yang et al., 2013). Thus, the bidirectional links between marital discord and sleep disturbance foster a positive feedback loop wherein discord-induced sleep problems exacerbate conflict that can lead to longer-term marital dysfunction.
Depression as a key sleep pathway
Marital distress elevates risk for depression (Whisman, 1999) and predicts increased symptomatology over time (Whisman and Uebelacker, 2009). Accordingly, depression represents a key pathway from marital conflict and distress to disturbed sleep, a cardinal symptom of depression. In a longitudinal study, depressive symptoms explained conflict-related declines in sleep quality and duration (El-Sheikh et al., 2015). A known risk to partner well-being (Benazon and Coyne, 2000), depression also predicted worse sleep problems for partners one year later (Revenson et al., 2016, El-Sheikh et al., 2015).
In turn, sleep loss stimulates production of proinflammatory cytokines and cellular inflammatory signaling, thus facilitating depression (Irwin, 2015). Heightened inflammation feeds back to dysregulate sleep (Lopresti et al., 2013). In this way, marital discord activates a synergistic cascade of depression, sleep disturbance, and inflammation that heightens risk for comorbidities and death.
In addition to its important inflammatory consequences, insufficient sleep also alters appetite regulation and food choice (Bayon et al., 2014). Thus it is not surprising that poor sleep has also been associated with obesity and the metabolic syndrome (Bayon et al., 2014).
Marital Paths to Obesity and Its Comorbidities
Depression and stress promote obesity (Luppino et al., 2010, Raikkonen et al., 2007, Williams et al., 2009). Depressed people have a 58% increased risk of becoming obese (Luppino et al., 2010). In addition, a large prospective study showed that older depressed adults gained visceral fat over five years, while non–depressed adults lost visceral fat (Vogelzangs et al., 2008). Stressful events have also been associated with weight gain and adiposity (Block et al., 2009, Sinha and Jastreboff, 2013); longitudinal studies suggest that chronic stress and stressful life events enhance the development of the metabolic syndrome, which has central obesity as its cornerstone (Kyrou et al., 2006, Raikkonen et al., 2007, Chandola et al., 2006, Troxel et al., 2005). These data have clear implications for people in troubled marriages because of the strong ties between marital discord and depression (Beach, 2014).
Marital distress and depression can alter neurochemistry, neurobiology, and behavior, providing multiple pathways for obesity-related metabolic alterations. For example, both depression and marital distress can elevate cortisol production (Kiecolt-Glaser et al., 1996); higher cortisol fosters increased intake of calorie-dense “comfort” foods, and insulin secretion rises as cortisol increases (Dallman, 2010). Persistent hypercortisolemia and higher insulin enhance visceral fat accumulation (Vogelzangs et al., 2008, Dallman, 2010). Furthermore, marital distress can alter production of ghrelin, an appetite-stimulating hormone that promotes food intake (Jaremka et al., 2015).
A recent study from our lab examined the impact of marital conflict on couples’ metabolic responses to high-fat meals (Kiecolt-Glaser et al., 2015c). Metabolic processes that influence weight regulation and fat storage were a central focus. Resting energy expenditure plays a key role in energy balance and weight control, accounting for 65% to 75% of the total daily energy expenditure; lower daily energy expenditure increases risk for weight gain (Lara et al., 2010). Higher levels of insulin stimulate food intake and visceral fat accumulation (Dallman, 2010).
Our double-blind, randomized crossover study included serial assessments of resting energy expenditure, insulin and glucose before and after two high-fat meals during two separate 9.5 hour visits. Couples discussed a marital disagreement during both visits; behavioral coding of these interactions provided data on hostile marital behaviors.
When combined with a mood disorder history, men and women who had more hostile marital interactions had lower post-meal energy expenditure, and this disparity was clinically meaningful: the cumulative 6.75-hour total translates into 128 kcal, a difference that could add 7.6 pounds/year for women and 7.7 for men, based on weight change prediction models that incorporate metabolic adaptation. In addition to energy expenditure, higher levels of hostile behaviors among those who had a mood disorder history were also associated with higher post-meal insulin compared with other participants. Higher insulin levels stimulate food intake and visceral fat accumulation (Dallman, 2010), and thus would act in tandem with lower energy expenditure to promote obesity. These data complemented and extended an earlier study in which women who reported more recent stressors had lower energy expenditure and fat metabolism following the same high-fat, fast-food-type meals, as well as greater insulin production (Kiecolt-Glaser et al., 2015b). Our data also dovetail with a recent paper showing that chronic stress was associated with diet-related abdominal fat and insulin resistance in postmenopausal women (Aschbacher et al., 2014).
Dining with one’s partner is a common daily event, and marital discord and other stressors contribute to poorer diet quality because they enhance the likelihood that people will turn to calorie-dense high-fat “comfort” food (Tomiyama et al., 2011, Kiecolt-Glaser, 2010, Jaremka et al., 2015). Prospective studies have linked healthier diets (typically Mediterranean-style) with a lower risk for depression as well as lower inflammation, compared to less healthy, “Western” diets (Kiecolt-Glaser et al., 2015a). Both of our study meals had 930 kcal and 60 g fat as they were designed to mimic common fast food options. For example, a Burger King Double Whopper with cheese has 990 kcal and 64 g fat, while a Big Mac cheeseburger and medium French fries contain 930 kcals and 58 g fat. Thus the metabolic changes that we observed likely occur with high frequency in response to common meal choices.
The marital relationship is typically people’s most significant adult relationship and thus a troubled marriage is uniquely stressful, providing regular acute stressors, e.g. disagreements, that heighten chronic relationship stress. Distressed families experience roughly twice as many tensions per day as nondistressed families (Margolin et al., 1996). Moreover, distressed couples are more likely to have continuing conflicts that recur in well-established patterns at the same time on subsequent days – and meals provide prime opportunities for these ongoing disagreements (Margolin et al., 1996).
Metabolic syndrome
Metabolic syndrome, diagnosed using the National Cholesterol Education Program criteria, includes mild dyslipidemia, central adiposity, hypertension, and insulin resistance/hyperglycemia (Troxel et al., 2005). This cluster represents characteristics that all have individual associations with increased cardiovascular disease and diabetes risk (Whisman and Uebelacker, 2012).
Women who reported greater marital satisfaction were at significantly lower risk for developing the metabolic syndrome over a period of 11.5 years, compared to women who were maritally dissatisfied or those who were unpartnered (single, widowed, or divorced) (Troxel et al., 2005). Indeed, maritally dissatisfied women were more than three times as likely to develop the metabolic syndrome compared to those who were in higher-quality marriages, even after controlling for age, demographic characteristics, and psychosocial and behavioral risk factors.
Subsequent work in a cross-sectional sample confirmed that marital distress was associated with a greater likelihood for meeting criteria for the metabolic syndrome for women, but not men (Whisman et al., 2010). When these authors examined four-year follow-up data, they found that the magnitude of the association between marital distress and a metabolic syndrome diagnosis was substantially greater for women than men; additionally, when husbands reported marital distress at baseline, wives were more likely to meet criteria for metabolic syndrome four years later (Whisman and Uebelacker, 2012).
Further work that used a couples structural equation model with metabolic syndrome components concluded that marital quality for both husbands and wives was associated with metabolic syndrome only through depressive symptoms, not directly by itself (Henry et al., 2015). These data contrast with the earlier work showing that marital distress independently predicted metabolic syndrome in women but not men (Troxel et al., 2005, Whisman et al., 2010, Whisman and Uebelacker, 2012). However, the prior studies used a dichotomous metabolic syndrome classification, as well as different measures for depressive symptoms, and these factors could have accounted for the differences in the findings.
Diabetes
Diabetes is the fastest growing chronic health problem in the United States, and the seventh leading cause of death (Liu et al., in press, 2016). Diabetes care requires daily management, and thus adherence may be affected by the spouse’s behavior, either directly, through encouragement of a healthier diet and exercise, or indirectly, through interdependent couple behaviors, such as shared meals. Marital discord can heighten important risk factors for diabetes, including metabolic syndrome and inflammation.
Two studies have addressed marital quality and diabetes prevalence in population-based samples, and they arrived at divergent conclusions. Using data from the Health and Retirement Study, Whisman and colleagues (Whisman et al., 2014) reported that husbands’ decreased frequency of positive marital interactions and increased frequency of negative exchanges were linked with a higher prevalence of diabetes, but no effects were found for wives. In contrast, Liu et al. (Liu et al., in press, 2016) found that women who reported increased positive marital quality over time had a reduced risk for diabetes; however, men who reported increased negative marital quality over time had better outcomes. For the latter study, which used two waves of data from the National Social Life, Health, and Aging Project, the authors suggested that the somewhat counterintuitive data from men might reflect wives’ attempts to regulate husbands’ health behaviors.
As described earlier, when one spouse has metabolic syndrome, his or her spouse has roughly a 30% greater chance of also having metabolic syndrome (Kim et al., 2006). When one partner has a history of diabetes, spousal risk for diabetes is increased 26%; a spousal history of either diabetes or prediabetes confers a two-fold risk for the partner (Leong et al., 2014). Future work that addresses marital quality and marital closeness could provide more nuanced information about convergence that would enhance treatment recommendations.
Treatment Implications
Just as one partner’s health problems risk the other’s health and well-being, leveraging couples’ interconnectedness stands to promote both partners’ health. This so-called relative benefit (Martire, 2005) has been demonstrated for psychological and medical diagnoses and across intervention techniques.
As noted earlier, marital distress has strong ties with depression, both cross-sectionally and longitudinally. An excellent literature review (Whisman and Baucom, 2012) described how depressed people in distressed relationships have poorer outcomes following both psychopharmacological and individual-based treatments than those in nondistressed marriages, and relationship distress predicts depression relapse. Additionally, individual-based treatments typically do not lessen marital distress, leading to poorer outcomes than couple-based treatments.
Precisely because marital distress appears to be a potent correlate of health risk factors, the couples who do benefit substantially from marital therapy might also experience notable reductions in health risks. Importantly, treating marital distress can lower healthcare service utilization and associated costs. A comparison of healthcare utilization patterns before and after marital/family therapy showed a 21.5% reduction in medical visits; in contrast, people who received individual therapy had a 10% decrease, while comparison group participants who received no therapy increased utilization by 12.2% (Law and Crane, 2000). Diminished reactivity to couple conflict may be one biological mechanism that leads to reduced need for medical services. For example, two effective couple therapies downregulated arousal to couple conflict via vocal stress (Baucom et al., 2015). Also, enhancing positive communication through preventive couple relationship education reduced cortisol reactivity to couple conflict but not to an individual stress task (Ditzen et al., 2011).
A meta-analysis of couple-based interventions for chronic illness concluded that couple interventions improved marital functioning and reduced patient depressive symptoms and pain to a greater extent than either patient-based psychosocial interventions or usual care (Martire et al., 2010). Although all effect sizes were small, none of the reviewed studies used spouse support or distress as a criterion for treatment, and this likely attenuated the effect sizes.
Conclusions and Recommendations for Future Work
Intimate relationships play a central role in most people’s lives. Spouses influence each other's developmental trajectories and outcomes. As a consequence, health-related marital processes can be conceptualized as mutual influences on health behaviors, stress reactivity, happiness and depression, and shared life events. Future research that addresses links between spouses' well-being and morbidity and mortality would profit from a greater emphasis on partner associations (Hoppmann et al., 2011a).
The greater risk associated with marital distress among women compared to men is a clear and compelling theme in concordance studies, just as it is in marital interaction studies (Kiecolt-Glaser and Newton, 2001), but a meta-analysis did not find gender differences (Robles et al., 2014). At a demographic level, cohabiting same-sex couples have reported poorer health than their different-sex married counterparts and, after adjusting for SES, also fared worse than different-sex cohabitors (Liu et al., 2013). It remains unknown whether marital processes for same-sex couples are similar and if they confer similar health risks and benefits. Studies of men and women in same-sex and different-sex couples will help to untangle the roles of gender and sexual orientation in relationships’ health effects (Umberson and Kroeger, 2016).
One partner's distress or depression can provoke similar emotional responses in their partner as a function of their shared environment and history, interaction patterns, and emotional contagion (Schulz et al., 2009). People with a history of depression experience more major and minor stressors than those without a similar history, and past depression can also boost emotional reactivity to stressors, including relationship stressors (Hammen, 1991, Husky et al., 2009). Both currently and formerly depressed men and women had poorer family functioning than those who had no depression history, even years after their depression had remitted (Herr et al., 2007). A history of depression may index a high-risk phenotype, while marital conflict is a stressful context that provokes a coordinated physiological response. Accordingly, a past or current mood disorder could act synergistically with marital stress through multiple pathways. Indeed, depression alters inflammation-relevant health behaviors including sleep, physical activity, alcohol and drug use, smoking and diet (Kiecolt-Glaser et al., 2015a).
In addition to mood contagion, couples also transmit health behaviors including sleep, exercise, and diet quality to one another, and these can converge in a common path to promote shared risks for obesity, metabolic syndrome, and diabetes (Meyler et al., 2007, Franks et al., 2002). When marital stressors worsen sleep, they also dysregulate leptin and ghrelin, key appetite hormones that regulate energy balance and food intake (Spiegel et al., 2004). In turn, alterations in leptin and ghrelin stimulate interest in unhealthy foods, and they can induce overeating (Spiegel et al., 2004). Poor sleep has also been associated with obesity and the metabolic syndrome (Bayon et al., 2014). Thus, how couples’ mutual influences spur synergistic relationships between sleep and metabolic processes warrants further study.
Obesity has been characterized as a state of chronic inflammation. What is more, the pathways are bidirectional; visceral adipose tissue’s secretion of proinflammatory cytokines can function as a stimulus for HPA axis activation, such that hypercortisolemia enhances adipocyte accumulation, and vice versa (Kyrou et al., 2006). Inflammation is a robust and reliable predictor of all-cause mortality in older adults, in addition to its association with multiple diseases of aging (Kiecolt-Glaser et al., 2002, Ershler and Keller, 2000).
Stronger parasympathetic function has been linked with lower inflammation, and one novel study showed that more satisfied couples had stronger parasympathetic coregulation during structured lab tasks than less satisfied couples; this intriguing study suggests another potential route to marriage-related health benefits (Helm et al., 2014). Marital interaction studies with physiological assessments have provided solid, mechanistic evidence of how marital functioning can have direct consequences for cardiovascular, metabolic, endocrine, and immune function, but few have looked at coregulation across various physiological indices, a promising future direction.
Considerable evidence has linked the quality of the marital relationship to health outcomes ranging from intracellular signaling to mortality (Kiecolt-Glaser et al., 2010). Marriage can protect and promote health by buffering stress reactivity and encouraging healthy behavior. However, closer relationships also facilitate stress transmission (Larson and Almeida, 1999), and thus marital satisfaction and closeness can have a clear downside when one partner has mental or physical health problems. In higher-quality marriages, a partner's illness may put the spouse at risk for accelerated aging (Hoppmann and Gerstorf, 2009). A better understanding of how interdependent development provides both gains and losses will help illuminate the risks and benefits of couples’ relationships.
Central points
There is considerable interdependence between partners' health.
Partners’ mutual influences may introduce health risks or benefits.
The physiological cascade from marriage to health consists of bidirectional mechanisms; therefore, couples’ health risks can be synergistic.
Unresolved issues
The roles of gender and sexual orientation in relationship processes and health convergence
How to reconcile the risks of convergence with health benefits of a good relationship
The processes by which couples are buffered from convergence-related decline
The relative magnitude of marriage’s health benefits and risks across adulthood
Best methodological practices for estimating partners’ trajectories of interdependence over time
Acknowledgments
Work on this paper was supported in part by NIH grants K05 CA172296, R01 CA186720, R01 CA186251, and T32 DE014320, as well as a Pelotonia Postdoctoral Fellowship from the Ohio State University Comprehensive Cancer Center.
Contributor Information
Janice K. Kiecolt-Glaser, Institute for Behavioral Medicine Research, Department of Psychiatry and Behavioral Health, The Ohio State University College of Medicine, Columbus, OH, USA, Janice.Kiecolt-Glaser@osumc.edu.
Stephanie J. Wilson, Institute for Behavioral Medicine Research, The Ohio State University College of Medicine, Columbus, OH, USA, Stephanie.Wilson2@osumc.edu.
Literature Cited
- Aizer AA, Chen MH, Mccarthy EP, Mendu ML, Koo S, Wilhite TJ, Graham PL, Choueiri TK, Hoffman KE, Martin NE, Hu JC, Nguyen PL. Marital Status and Survival in Patients With Cancer. Journal of Clinical Oncology. 2013 doi: 10.1200/JCO.2013.49.6489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato PR, Booth A, Johnson DR, Rogers SJ. Alone Together: How Marriage in America is Changing. Cambridge, MA: Harvard University Press; 2007. [Google Scholar]
- Aron A, Aron EN, Smollan D. Inclusion of other in the self scale and the structure of interpersonal closeness. Journal of Personality and Social Psychology. 1992;63:596–612. [Google Scholar]
- Aschbacher K, Kornfeld S, Picard M, Puterman E, Havel PJ, Stanhope K, Lustig RH, Epel E. Chronic stress increases vulnerability to diet-related abdominal fat, oxidative stress, and metabolic risk. Psychoneuroendocrinology. 2014;46:14–22. doi: 10.1016/j.psyneuen.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayotte BJ, Yang FM, Jones RN. Physical health and depression: a dyadic study of chronic health conditions and depressive symptomatology in older adult couples. J Gerontol B Psychol Sci Soc Sci. 2010;65:438–48. doi: 10.1093/geronb/gbq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baucom BR, Sheng E, Christensen A, Georgiou PG, Narayanan SS, Atkins DC. Behaviorally-based couple therapies reduce emotional arousal during couple conflict. Behav Res Ther. 2015;72:49–55. doi: 10.1016/j.brat.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayon V, Leger D, Gomez-merino D, Vecchierini MF, Chennaoui M. Sleep debt and obesity. Ann Med. 2014:1–9. doi: 10.3109/07853890.2014.931103. [DOI] [PubMed] [Google Scholar]
- Beach SRH. The couple and family discord model of depression: Updates and future directions. In: South CRASC, editor. Interpersonal relationships and health: Social and clinical psychological mechanisms. New York, NY, US: Oxford University Press; 2014. [Google Scholar]
- Benazon NR, Coyne JC. Living with a depressed spouse. J Fam Psychol. 2000;14:71–9. [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J. Affect covariation in marital couples dealing with stressors surrounding prostate cancer. Gerontology. 2011;57:167–72. doi: 10.1159/000318642. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J, Bloor L, Bradstreet C, Upchurch R, Hayes J, Stephenson R, Nail L, Patton G. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychol Aging. 2008;23:505–16. doi: 10.1037/a0012687. [DOI] [PubMed] [Google Scholar]
- Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. American Journal of Epidemiology. 2009;170:181–92. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala J. Spouse health status, depressed affect, and resilience in mid and late life: a longitudinal study. Dev Psychol. 2014;50:1241–9. doi: 10.1037/a0035124. [DOI] [PubMed] [Google Scholar]
- Bourassa KJ, Knowles LM, Sbarra DA, O’connor M-F. Absent but Not Gone: Interdependence in Couples’ Quality of Life Persists After a Partner’s Death. Psychological Science. 2015a doi: 10.1177/0956797615618968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourassa KJ, Memel M, Woolverton C, Sbarra DA. A dyadic approach to health, cognition, and quality of life in aging adults. Psychol Aging. 2015b;30:449–61. doi: 10.1037/pag0000025. [DOI] [PubMed] [Google Scholar]
- Cano A, Johansen AB, Franz A. Multilevel analysis of couple congruence on pain, interference, and disability. Pain. 2005;118:369–379. doi: 10.1016/j.pain.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, D'elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. British Medical Journal. 2006;332:521–524A. doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Carstensen LL. Annual Review of Psychology. Palo Alto: Annual Reviews; 2010. Social and Emotional Aging. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JH, Waite LJ, Lauderdale DS. Marriage, Relationship Quality, and Sleep among U.S. Older Adults. Journal of Health and Social Behavior. 2015;56:356–377. doi: 10.1177/0022146515594631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherlin A. Demographic Trends in the United States: A Review of Research in the 2000s. J Marriage Fam. 2010;72:403–419. doi: 10.1111/j.1741-3737.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian LM, Glaser R, Porter K, Malarkey WB, Beversdorf D, Kiecolt-glaser JK. Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology. 2011;36:1495–1504. doi: 10.1016/j.psyneuen.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cialdini RB, Brown SL, Lewis BP, Luce C, Neuberg SL. Reinterpreting the empathy-altruism relationship: When one into one equals oneness. Journal of Personality and Social Psychology. 1997;73:481–494. [PubMed] [Google Scholar]
- Coan JA, Schaefer HS, Davidson RJ. Lending a hand: Social regulation of the neural response to threat. Psychological Science. 2006;17:1032–1039. doi: 10.1111/j.1467-9280.2006.01832.x. [DOI] [PubMed] [Google Scholar]
- Cobb LK, Mcadams-demarco MA, Gudzune KA, Anderson CAM, Demerath E, Woodward M, Selvin E, Coresh J. Changes in Body Mass Index and Obesity Risk in Married Couples Over 25 Years: The ARIC Cohort Study. American Journal of Epidemiology. 2015 doi: 10.1093/aje/kwv112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consensus conference P, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J Clin Sleep Med. 2015;11:931–52. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC, Delongis A. Going beyond social support: The role of social relationships in adaptation. Journal of Consulting and Clinical Psychology. 1986;54:454–460. doi: 10.1037//0022-006x.54.4.454. [DOI] [PubMed] [Google Scholar]
- Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21:159–65. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derry HM, Padin AC, Kuo JL, Hughes S, Kiecolt-glaser JK. Sex Differences in Depression: Does Inflammation Play a Role? Current Psychiatry Reports. 2015;17 doi: 10.1007/s11920-015-0618-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di castelnuovo A, Quacquaruccio G, Donati MB, De gaetano G, Iacoviello L. Spousal Concordance for Major Coronary Risk Factors: A Systematic Review and Meta-Analysis. American Journal of Epidemiology. 2009;169:1–8. doi: 10.1093/aje/kwn234. [DOI] [PubMed] [Google Scholar]
- Ditzen B, Hahlweg K, Fehm-wolfsdorf G, Baucom D. Assisting couples to develop healthy relationships: effects of couples relationship education on cortisol. Psychoneuroendocrinology. 2011;36:597–607. doi: 10.1016/j.psyneuen.2010.07.019. [DOI] [PubMed] [Google Scholar]
- El-sheikh M, Kelly RJ, Koss KJ, Rauer AJ. Longitudinal relations between constructive and destructive conflict and couples' sleep. J Fam Psychol. 2015;29:349–59. doi: 10.1037/fam0000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom G, Hedblad B, Rosvall M, Janzon L, Lindgarde F. Occupation, marital status, and low-grade inflammation: mutual confounding or independent cardiovascular risk factors? Arteriosclerosis, Thrombosis, and Vascular Biology. 2006;26:643–648. doi: 10.1161/01.ATV.0000200100.14612.bb. [DOI] [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annual Review of Medicine. 2000;51:245–70. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- Fagundes CP, Glaser R, Hwang BS, Malarkey WB, Kiecolt-glaser JK. Depressive symptoms enhance stress-induced inflammatory responses. Brain, Behavior, and Immunity. 2013;31:172–176. doi: 10.1016/j.bbi.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foran HM, Whisman MA, Beach SRH. Intimate Partner Relationship Distress in the DSM-5. Family Process. 2015;54:48–63. doi: 10.1111/famp.12122. [DOI] [PubMed] [Google Scholar]
- Franks MM, Pienta AM, Wray LA. It takes two: marriage and smoking cessation in the middle years. J Aging Health. 2002;14:336–54. doi: 10.1177/08964302014003002. [DOI] [PubMed] [Google Scholar]
- Gere J, Martire LM, Keefe FJ, Stephens MA, Schulz R. Spouse confidence in self-efficacy for arthritis management predicts improved patient health. Ann Behav Med. 2014;48:337–46. doi: 10.1007/s12160-014-9608-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Hoppmann CA, Kadlec KM, Mcardle JJ. Memory and Depressive Symptoms Are Dynamically Linked Among Married Couples: Longitudinal Evidence From the AHEAD Study. Developmental Psychology. 2009;45:1595–1610. doi: 10.1037/a0016346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser R, Kiecolt-glaser JK. Stress-induced immune dysfunction: Implications for health. Nature Reviews Immunology. 2005;5:243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- Glaser R, Robles T, Sheridan J, Malarkey WB, Kiecolt-glaser JK. Mild depressive symptoms are associated with amplified and prolonged inflammatory responses following influenza vaccination in older adults. Archives of General Psychiatry. 2003;60:1009–1014. doi: 10.1001/archpsyc.60.10.1009. [DOI] [PubMed] [Google Scholar]
- Gordon AM, Chen S. The Role of Sleep in Interpersonal Conflict: Do Sleepless Nights Mean Worse Fights? Social Psychological and Personality Science 2014 [Google Scholar]
- Gorin AA, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, Brelje K, Dilillo VG, Look AHERG. Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. International Journal of Obesity. 2008;32:1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Ranchor AV, Brilman EI, Kempen GI, Ormel J. Chronic disease in elderly couples: are women more responsive to their spouses' health condition than men? J Psychosom Res. 2001;51:693–6. doi: 10.1016/s0022-3999(01)00279-3. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hasler BP, Troxel WM. Couples' nighttime sleep efficiency and concordance: evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine. 2010;72:794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller D, Watson D, Ilies R. The role of person versus situation in life satisfaction: A critical examination. Psychological Bulletin. 2004;130:574–600. doi: 10.1037/0033-2909.130.4.574. [DOI] [PubMed] [Google Scholar]
- Helm JL, Sbarra DA, Ferrer E. Coregulation of respiratory sinus arrhythmia in adult romantic partners. Emotion. 2014;14:522–31. doi: 10.1037/a0035960. [DOI] [PubMed] [Google Scholar]
- Hemphill RC, Martire LM, Polenick CA, Stephens MA. Spouse Confidence and Physical Function Among Adults With Osteoarthritis: The Mediating Role of Spouse Responses to Pain. Health Psychol. 2016 doi: 10.1037/hea0000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry NJM, Smith TW, Butner J, Berg CA, Sewell KK, Uchino BN. Marital quality, depressive symptoms, and the metabolic syndrome: a couples structural model. Journal of Behavioral Medicine. 2015;38:497–506. doi: 10.1007/s10865-015-9619-4. [DOI] [PubMed] [Google Scholar]
- Herr NR, Hammen C, Brennan PA. Current and past depression as predictors of family functioning: A comparison of men and women in a community sample. Journal of Family Psychology. 2007;21:694–702. doi: 10.1037/0893-3200.21.4.694. [DOI] [PubMed] [Google Scholar]
- Hippisley-cox J, Coupland C, Pringle M, Crown N, Hammersley V. Married couples' risk of same disease: cross sectional study. British Medical Journal. 2002;325:636–638A. doi: 10.1136/bmj.325.7365.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hippisley-cox J, Pringle M. Are spouses of patients with hypertension at increased risk of having hypertension? A population-based case-control study. British Journal of General Practice. 1998;48:1580–1583. [PMC free article] [PubMed] [Google Scholar]
- Holtzman S, Delongis A. One day at a time: The impact of daily satisfaction with spouse responses on pain, negative affect and catastrophizing among individuals with rheumatoid arthritis. Pain. 2007;131:202–13. doi: 10.1016/j.pain.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D. Spousal interrelations in old age--a mini-review. Gerontology. 2009;55:449–59. doi: 10.1159/000211948. [DOI] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D, Hibbert A. Spousal Associations Between Functional Limitation and Depressive Symptom Trajectories: Longitudinal Findings From the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD) Health Psychology. 2011a;30:153–162. doi: 10.1037/a0022094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D, Luszcz M. Spousal social activity trajectories in the Australian longitudinal study of ageing in the context of cognitive, physical, and affective resources. J Gerontol B Psychol Sci Soc Sci. 2008;63:P41–50. doi: 10.1093/geronb/63.1.p41. [DOI] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D, Willis SL, Schaie KW. Spousal interrelations in happiness in the Seattle Longitudinal Study: considerable similarities in levels and change over time. Dev Psychol. 2011b;47:1–8. doi: 10.1037/a0020788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes MF, Patterson CC, Appleton KM, Blankenberg S, Woodside JV, Donnelly MB, Linden G, Zeller T, Esquirol Y, Kee F. The Predictive Value of Depressive Symptoms for All-Cause Mortality: Findings From the PRIME Belfast Study Examining the Role of Inflammation and Cardiovascular Risk Markers. Psychosomatic Medicine. 2016;78:401–411. doi: 10.1097/PSY.0000000000000289. [DOI] [PubMed] [Google Scholar]
- Husky M, Mazure C, Maciejewski P, Swendsen J. Past Depression and Gender Interact to Influence Emotional Reactivity to Daily Life Stress. Cognitive Therapy and Research. 2009;33:264–271. [Google Scholar]
- Irwin MR. Why Sleep Is Important for Health: A Psychoneuroimmunology Perspective. Annu Rev Psychol. 2015;66:143–172. doi: 10.1146/annurev-psych-010213-115205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SE, Steptoe A, Wardle J. The Influence of Partner's Behavior on Health Behavior Change The English Longitudinal Study of Ageing. Jama Internal Medicine. 2015;175:385–392. doi: 10.1001/jamainternmed.2014.7554. [DOI] [PubMed] [Google Scholar]
- Jaremka LM, Belury MA, Andridge RR, Lindgren ME, Habash D, Malarkey WB, Kiecolt-glaser JK. Novel Links Between Troubled Marriages and Appetite Regulation: Marital Distress, Ghrelin, and Diet Quality. Clinical Psychological Science. 2015;3:1–13. doi: 10.1177/2167702615593714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Lindgren ME, Kiecolt-glaser JK. Synergistic relationships among stress, depression, and distressing relationships: Insights from psychoneuroimmunology. Depression and Anxiety. 2013;30:288–296. doi: 10.1002/da.22078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane HS, Slatcher RB, Reynolds BM, Repetti RL, Robles TF. Daily Self-Disclosure and Sleep in Couples. Health Psychology. 2014;33:813–822. doi: 10.1037/hea0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly HH, Thibaut JW. Interpersonal relations: A theory of interdependence. New York, NY: Wiley; 1978. [Google Scholar]
- Khan CM, Iida M, Stephens MA, Fekete EM, Druley JA, Greene KA. Spousal support following knee surgery: roles of self-efficacy and perceived emotional responsiveness. Rehabil Psychol. 2009;54:28–32. doi: 10.1037/a0014753. [DOI] [PubMed] [Google Scholar]
- Khan CM, Stephens MA, Franks MM, Rook KS, Salem JK. Influences of spousal support and control on diabetes management through physical activity. Health Psychol. 2013;32:739–47. doi: 10.1037/a0028609. [DOI] [PubMed] [Google Scholar]
- Kiecolt-glaser JK. Stress, food, and inflammation: Psychoneuroimmunology and nutrition at the cutting edge. Psychosomatic Medicine. 2010;72:365–369. doi: 10.1097/PSY.0b013e3181dbf489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Derry HM, Fagundes CP. Inflammation: Depression Fans the Flames and Feasts on the Heat. American Journal of Psychiatry. 2015a;172:1075–1091. doi: 10.1176/appi.ajp.2015.15020152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neuroscience and Biobehavioral Reviews. 2010;35:33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Habash DL, Fagundes CP, Andridge R, Peng J, Malarkey WB, Belury MA. Daily stressors, past depression, and metabolic responses to high-fat meals: a novel path to obesity. Biol Psychiatry. 2015b;77:653–60. doi: 10.1016/j.biopsych.2014.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Jaremka L, Andridge R, Peng J, Habash D, Fagundes CP, Glaser R, Malarkey WB, Belury MA. Marital discord, past depression, and metabolic responses to high-fat meals: Interpersonal pathways to obesity. Psychoneuroendocrinology. 2015c;52:239–50. doi: 10.1016/j.psyneuen.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, Glaser R. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry. 2005;62:1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Mcguire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Newton T. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Newton T, Cacioppo JT, Maccallum RC, Glaser R, Malarkey WB. Marital conflict and endocrine function: Are men really more physiologically affected than women? Journal of Consulting and Clinical Psychology. 1996;64:324–332. doi: 10.1037//0022-006x.64.2.324. [DOI] [PubMed] [Google Scholar]
- Kiecolt-glaser JK, Preacher KJ, Maccallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:9090–9095. doi: 10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HC, Kang DR, Choi KS, Nam CM, Thomas GN, Suh I. Spousal concordance of metabolic syndrome in 3141 Korean couples: a nationwide survey. Ann Epidemiol. 2006;16 doi: 10.1016/j.annepidem.2005.07.052. [DOI] [PubMed] [Google Scholar]
- Kyrou I, Chrousos GP, Tsigos C. Stress, visceral obesity, and metabolic complications. Ann N Y Acad Sci. 2006;1083:77–110. doi: 10.1196/annals.1367.008. [DOI] [PubMed] [Google Scholar]
- Lara J, Taylor MA, Macdonald IA. Clinical Obesity in Adults and Children. Third. Wiley-Blackwell; 2010. Energy Expenditure in Humans: The Influence of Activity, Diet and the Sympathetic Nervous System. [Google Scholar]
- Larson RW, Almeida DM. Emotional transmission in the daily lives of families: A new paradigm for studying family process. Journal of Marriage and the Family. 1999;61:5–20. [Google Scholar]
- Law DD, Crane DR. The influence of marital and family therapy on health care utilization in a health-maintenance organization. J Marital Fam Ther. 2000;26:281–91. doi: 10.1111/j.1752-0606.2000.tb00298.x. [DOI] [PubMed] [Google Scholar]
- Leong A, Rahme E, Dasgupta K. Spousal diabetes as a diabetes risk factor: A systematic review and meta-analysis. BMC Medicine. 2014;12:1–12. doi: 10.1186/1741-7015-12-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Reczek C, Brown D. Same-sex cohabitors and health: the role of race-ethnicity, gender, and socioeconomic status. J Health Soc Behav. 2013;54:25–45. doi: 10.1177/0022146512468280. [DOI] [PubMed] [Google Scholar]
- Liu H, Waite L, Shen S. Diabetes risk and disease management in later life: A national longitudinal study of the role of marital quality. J Gerontol B Psychol Sci Soci Sci. 2016 doi: 10.1093/geronb/gbw061. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J Affect Disord. 2013;148:12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Luppino FS, De wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, Obesity, and Depression: A Systematic Review and Meta-analysis of Longitudinal Studies. Archives of General Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Lyons KS, Bennett JA, Nail LM, Fromme EK, Dieckmann N, Sayer AG. The role of patient pain and physical function on depressive symptoms in couples with lung cancer: a longitudinal dyadic analysis. J Fam Psychol. 2014;28:692–700. doi: 10.1037/fam0000017. [DOI] [PubMed] [Google Scholar]
- Margolin G, Christensen A, John RS. The continuance and spillover of everyday tensions in distressed and nondistressed families. Journal of Family Psychology. 1996;10:304–321. [Google Scholar]
- Martire LM. The "Relative" Efficacy of Involving Family in Psychosocial Interventions for Chronic Illness: Are There Added Benefits to Patients and Family Members? Families, Systems, & Health. 2005;23:312–328. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Parris stephens MA, Mogle JA. The impact of daily arthritis pain on spouse sleep. Pain. 2013a154:1725–31. doi: 10.1016/j.pain.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and Meta-analysis of Couple-Oriented Interventions for Chronic Illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Stephens MA, Druley JA, Wojno WC. Negative reactions to received spousal care: predictors and consequences of miscarried support. Health Psychol. 2002;21:167–76. [PubMed] [Google Scholar]
- Martire LM, Stephens MA, Mogle J, Schulz R, Brach J, Keefe FJ. Daily spousal influence on physical activity in knee osteoarthritis. Ann Behav Med. 2013b;45:213–23. doi: 10.1007/s12160-012-9442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuwly N, Bodenmann G, Germann J, Bradbury TN, Ditzen B, Heinrichs M. Dyadic coping, insecure attachment, and cortisol stress recovery following experimentally induced stress. J Fam Psychol. 2012;26:937–47. doi: 10.1037/a0030356. [DOI] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science & Medicine. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Moieni M, Irwin MR, Jevtic I, Olmstead R, Breen EC, Eisenberger NI. Sex Differences in Depressive and Socioemotional Responses to an Inflammatory Challenge: Implications for Sex Differences in Depression. Neuropsychopharmacology. 2015 doi: 10.1038/npp.2015.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monfort SS, Kaczmarek LD, Kashdan TB, Drazkowski D, Kosakowski M, Guzik P, Krauze T, Gracanin A. Capitalizing on the success of romantic partners: A laboratory investigation on subjective, facial, and physiological emotional processing. Personality and Individual Differences. 2014;68:149–153. [Google Scholar]
- Monin JK, Doyle M, Levy B, Schulz R, Fried T, Kershaw T. Spousal Associations Between Frailty and Depressive Symptoms: Longitudinal Findings from the Cardiovascular Health Study. Journal of the American Geriatrics Society. 2016;64:824–830. doi: 10.1111/jgs.14023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, Greenberg MS. Spouses' cardiovascular reactivity to their partners' suffering. Journals of Gerontology: Series B, Psychological Sciences and Social Sciences. 2010;65B:195–201. doi: 10.1093/geronb/gbp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monserud MA, Peek MK. Functional Limitations and Depressive Symptoms: A Longitudinal Analysis of Older Mexican American Couples. J Gerontol B Psychol Sci Soc Sci. 2014;69:743–762. doi: 10.1093/geronb/gbu039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman MD, Werner RM. MArital status and postoperative functional recovery. JAMA Surgery. 2015:1–3. doi: 10.1001/jamasurg.2015.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton TL, Burns VE, Miller JJ, Fernandez-botran GR. Subjective Sleep Quality in Women With Divorce Histories: The Role of Intimate Partner Victimization. J Interpers Violence. 2016;31:1430–52. doi: 10.1177/0886260514567961. [DOI] [PubMed] [Google Scholar]
- O'leary KD, Christian JL, Mendell NR. A closer look at the link between marital discord and depressive symptomatology. J Soc Clini Psychol. 1994;13:33–41. [Google Scholar]
- Polenick CA, Martire LM, Hemphill RC, Stephens MAP. Effects of Change in Arthritis Severity on Spouse Well-Being: The Moderating Role of Relationship Closeness. Journal of Family Psychology. 2015;29:331–338. doi: 10.1037/fam0000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruchno R, Wilson-genderson M, Cartwright F. Self-rated health and depressive symptoms in patients with end-stage renal disease and their spouses: a longitudinal dyadic analysis of late-life marriages. J Gerontol B Psychol Sci Soc Sci. 2009;64:212–21. doi: 10.1093/geronb/gbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raikkonen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women - A comparison of World Health Organization, Adult Treatment Panel III, and International Diabetes Foundation Definitions. Diabetes Care. 2007;30:872–877. doi: 10.2337/dc06-1857. [DOI] [PubMed] [Google Scholar]
- Revenson TA, Marin-chollom AM, Rundle AG, Wisnivesky J, Neugut AI. Hey Mr. Sandman: dyadic effects of anxiety, depressive symptoms and sleep among married couples. J Behav Med. 2016;39:225–32. doi: 10.1007/s10865-015-9693-7. [DOI] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, Mcginn MM. Marital quality and health: a meta-analytic review. Psychol Bull. 2014;140:140–87. doi: 10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxbe D, Repetti RL. For better or worse? Coregulation of couples' cortisol levels and mood states. J Pers Soc Psychol. 2010;98:92–103. doi: 10.1037/a0016959. [DOI] [PubMed] [Google Scholar]
- Schafer T, Merkl J, Klemm E, Wichmann HE, Ring J, Group KS. Does my partner cause my allergy? Allergy. 2004;59:781–5. doi: 10.1111/j.1398-9995.2004.00417.x. [DOI] [PubMed] [Google Scholar]
- Schoebi D. The coregulation of daily affect in marital relationships. J Fam Psychol. 2008;22:595–604. doi: 10.1037/0893-3200.22.3.595. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Hebert RS, Martire LM, Monin JK, Tompkins CA, Albert SM. Spousal suffering and partner's depression and cardiovascular disease: the Cardiovascular Health Study. Am J Geriatr Psychiatry. 2009;17:246–54. doi: 10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selcuk E, Ong AD. Perceived partner responsiveness moderates the association between received emotional support and all-cause mortality. Health Psychol. 2013;32:231–5. doi: 10.1037/a0028276. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Miller AH. Eating ourselves to death (and despair): the contribution of adiposity and inflammation to depression. Progress in Neurobiology. 2010;91:275–99. doi: 10.1016/j.pneurobio.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Jastreboff AM. Stress as a Common Risk Factor for Obesity and Addiction. Biological Psychiatry. 2013;73:827–835. doi: 10.1016/j.biopsych.2013.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher RB, Selcuk E, Ong AD. Perceived Partner Responsiveness Predicts Diurnal Cortisol Profiles 10 Years Later. Psychological Science. 2015;26:972–982. doi: 10.1177/0956797615575022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140:774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song S, Graham-engeland JE, Mogle J, Martire LM. The effects of daily mood and couple interactions on the sleep quality of older adults with chronic pain. J Behav Med. 2015;38:944–55. doi: 10.1007/s10865-015-9651-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, L'hermite-baleriaux M, Copinschi G, Penev PD, Van cauter E. Leptin levels are dependent on sleep duration: Relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. Journal of Clinical Endocrinology and Metabolism. 2004;89:5762–5771. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- Stephenson E, Delongis A, Esdaile JM, Lehman AJ. Depressive Symptoms and Rheumatoid Arthritis: Spouse Empathic Responding as a Buffer. Arthritis Care & Research. 2014;66:532–541. doi: 10.1002/acr.22161. [DOI] [PubMed] [Google Scholar]
- Stimpson JP, Peek MK. Concordance of chronic conditions in older Mexican American couples. Prev Chronic Dis. 2005;2:A07. [PMC free article] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Shema SJ. Impact of spouse vision impairment on partner health and well-being: A longitudinal analysis of couples. J Gerontol B Psychol Sci Soc Sci. 2007;62:S315–S322. doi: 10.1093/geronb/62.5.s315. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Thai JN, Shema S. The influence of spouse lower cognitive function on partner health and well-being among community-dwelling older couples: Moderating roles of gender and marital problems. Aging & Mental Health. 2009;13:530–536. doi: 10.1080/13607860802607330. [DOI] [PubMed] [Google Scholar]
- The NS, Gordon-larsen P. Entry into romantic partnership is associated with obesity. Obesity (Silver Spring) 2009;17:1441–7. doi: 10.1038/oby.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama AJ, Dallman MF, Epel ES. Comfort food is comforting to those most stressed: evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36:1513–9. doi: 10.1016/j.psyneuen.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses and the moderating effect of marital closeness. Psychology and Aging. 1995;10:625–638. doi: 10.1037//0882-7974.10.4.625. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996;11:683–697. doi: 10.1037//0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Braithwaite SR, Sandberg JG, Holt-lunstad J. Does Improving Marital Quality Improve Sleep? Results from a Marital Therapy Trial. Behav Sleep Med. 2016:1–14. doi: 10.1080/15402002.2015.1133420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Hall M, Matthews KA. Marital happiness and sleep disturbances in a multi-ethnic sample of middle-aged women. Behav Sleep Med. 2009;7:2–19. doi: 10.1080/15402000802577736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Gallo LC, Kuller LH. Marital quality and occurrence of the metabolic syndrome in women. Archives of Internal Medicine. 2005;165:1022–1027. doi: 10.1001/archinte.165.9.1022. [DOI] [PubMed] [Google Scholar]
- Turk DC, Kerns RD, Rosenberg R. Effects of marital interaction on chronic pain and disability: Examining the down side of social support. Rehabilitation Psychology. 1992;37:259–274. [Google Scholar]
- Umberson D, Kroeger AR. Gender, Marriage, and Health for Same-Sex and Different-Sex Couples: The Future Keeps Arriving. In: Mchale MS, King V, Van hook J, Booth A, editors. Gender and Couple Relationships. Cham: Springer International Publishing; 2016. [Google Scholar]
- Vogelzangs N, Kritchevsky SB, Beekman ATF, Newman AB, Satterfield S, Simonsick EM, Yaffe K, Harris TB, Penninx BWJH. Depressive symptoms and change in abdominal obesity in older persons. Archives of General Psychiatry. 2008;65:1386–1393. doi: 10.1001/archpsyc.65.12.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallhagen MI, Strawbridge WJ, Shema SJ, Kaplan GA. Impact of self-assessed hearing loss on a spouse: A longitudinal analysis of couples. J Gerontol B Psychol Sci Soc Sci. 2004;59:S190–S196. doi: 10.1093/geronb/59.3.s190. [DOI] [PubMed] [Google Scholar]
- Weissman MM. Advances in psychiatric epidemiology: Rates and risks for major depression. American Journal of Public Health. 1987;77:445–451. doi: 10.2105/ajph.77.4.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA. Marital dissatisfaction and psychiatric disorders: Results from the National Comorbidity Survey. Journal of Abnormal Psychology. 1999;108:701–706. doi: 10.1037//0021-843x.108.4.701. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and Family Processes in Depression: A Scientific Foundation for Clinical Practice. Washington: American Psychological Association; 2001. [Google Scholar]
- Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clin Child Fam Psychol Rev. 2012;15:4–13. doi: 10.1007/s10567-011-0107-2. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Li A, Sbarra DA, Raison CL. Marital quality and diabetes: Results from the Health and Retirement Study. Health Psychol. 2014;33:832–40. doi: 10.1037/hea0000064. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychol Aging. 2009;24:184–9. doi: 10.1037/a0014759. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. A longitudinal investigation of marital adjustment as a risk factor for metabolic syndrome. Health Psychology. 2012;31:80–86. doi: 10.1037/a0025671. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA, Settles TD. Marital Distress and the Metabolic Syndrome: Linking Social Functioning With Physical Health. Journal of Family Psychology. 2010;24:367–370. doi: 10.1037/a0019547. [DOI] [PubMed] [Google Scholar]
- White E, Hurlich M, Thompson RS, Woods MN, Henderson MM, Urban N, Kristal A. Dietary-changes among husbands of participants in a low-fat dietary intervention. American Journal of Preventive Medicine. 1991;7:319–325. [PubMed] [Google Scholar]
- Williams LJ, Pasco JA, Henry MJ, Jacka FN, Dodd S, Nicholson GC, Kotowicz MA, Berk M. Lifetime psychiatric disorders and body composition: a population-based study. Journal of Affective Disorders. 2009;118:173–9. doi: 10.1016/j.jad.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Yang HC, Suh S, Kim H, Cho ER, Lee SK, Shin C. Testing bidirectional relationships between marital quality and sleep disturbances: a 4-year follow-up study in a Korean cohort. J Psychosom Res. 2013;74:401–6. doi: 10.1016/j.jpsychores.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Yorgason JB, Roper SO, Sandberg JG, Berg CA. Stress spillover of health symptoms from healthy spouses to patient spouses in older married couples managing both diabetes and osteoarthritis. Fam Syst Health. 2012;30:330–43. doi: 10.1037/a0030670. [DOI] [PubMed] [Google Scholar]