Abstract
Cumulative stresses associated with concerns about cognitive functioning and worries about developing Alzheimer’s disease (AD) have been shown to be related to poorer health and lower psychological well-being. Among older persons, AD also generates higher levels of fear than any other disease. But much remains to be learned about predictors of worries and fears, especially from a temporal perspective. Thus, the principal objective of the current research is to examine long-term effects of self-perceptions of cognitive functioning on worries about developing AD. Data for the study are drawn from the University of Michigan’s Health and Retirement Study. We use up to ten measurements of self-perceived cognitive functioning collected from 1992 to 2010 for respondents 50 years of age and older at the time of their entrance into the study. Demographics (marital status, age, education, and gender); beliefs about the role of genetics, personal knowledge of someone with AD, and their interaction; and depression and health are other variables included in the model. The data are analyzed using the full information maximum likelihood procedure and latent growth curve modeling to account for the long-term effects. The analysis shows evidence of both short-term effects of depression, age, beliefs, and the interaction of beliefs and personal familiarity and long-term effects of cognitive self-assessment on worries about getting AD. Further analyses of these relationships and inclusion of these items in other studies are recommended.
Keywords: Alzheimer’s disease, Memory functioning, Worry, Longitudinal data, Structural equation modeling
Introduction
More accurate pre-mortem diagnosis in conjunction with population aging will lead to a dramatic increase in cases of Alzheimer’s disease (AD) in the coming decades. In the absence of effective prevention measures, one study suggests that the number of persons 65 years of age and older in the U.S. with AD will climb from 4.7 million in 2010 to 13.8 million in 2050 (Hebert et al. 2013). Prevalence estimates by Prince et al. (2013) point to an increase from 10.0 million to 18.7 million between 2010 and 2050 in the number of older (60+) Europeans with AD. Worldwide predictions about the global prevalence of AD (Prince et al. 2013) estimate that 35.6 million people 60 years of age and older lived with dementia in 2010 and that these numbers are expected to more than triple to 115.4 million by 2050. Simultaneously, public awareness of AD has been growing (MetLife Foundation 2011), as has recognition of its symptoms (Harvard School of Public Health and Alzheimer Europe 2011) and acknowledgement of AD’s social, psychological, economic, and physical burdens (Takizawa et al. 2014).
Coupling growing prevalence and visibility with the fact that AD is inevitably fatal and that there are no behavioral or pharmaceutical agents known to be fully effective in slowing down, stopping, or reversing the course of the disease’s progression (Daviglus et al. 2010),1 it is understandable that AD is a particularly feared condition. Data from a five-country survey conducted by the Harvard University School of Public Health in collaboration with Alzheimer Europe (2011) show that among persons 60 years of age and older, AD is reported as the disease they most fear getting by 47 % of the respondents (Rs) in France, 35 % in Spain, 32 % in the U.S., 30 % in Germany, and 20 % in Poland. Other studies have shown that the fear of getting AD is as great if not greater than the fear of getting cancer. In 2006, 31 % of Americans ages 55 and over indicated that AD was the disease they most feared getting compared with 27 % saying that they most feared getting cancer (MetLife Foundation 2006). And recent survey data from England showed that two-thirds of respondents over 50 years of age fear they will develop AD compared with only 10 % indicating they feared getting cancer (Huffington Post UK/PA 2014).
It comes as little surprise, then, that investigators have been turning their attention to worries about getting AD. Variously known as “anticipatory dementia” (Cutler and Hodgson 1996) or “dementia worry” (Kessler et al. 2012), studies have shown that such concerns are widespread, especially among middle-aged and older people (Commisaris et al. 1996; Cutler and Hodgson 2001). This research has also provided insights into the factors that predict fear and concerns. We know, for example, that worry is greater among persons who have a first-degree relative with a diagnosis of AD. But we have also learned that concern is not confined to first-degree relatives (Cutler and Hodgson 2001; Cutler 2015). These worries exist among all segments of the older population, and they exist particularly among those who report negative changes in their cognitive functioning regardless of whether they have a first-degree relative with AD (Cutler 2015).
Results for other predictors have been less consistent. Cutler (2015) and Roberts et al. (2014) find that worries decrease with advancing age among a sample of persons 50 years of age and older. On the other hand, Werner (2002) and Zeng et al. (2015) find nonsignificant relationships between age and concerns, while Cantegreil-Kallen and Pin (2012) find personal fear to be significantly higher among persons 65+ than among persons 35–64. Inconsistent results have also been reported for the effects of gender. The recent work of Werner et al. (2013) in Israel reports significant gender differences in worry about getting AD, with women expressing greater worry, but the studies reported by Roberts and colleagues (2014) and by Cutler (2015) based on a U.S. sample find gender to be a nonsignificant predictor of worry. Such variation in results may be due to different analysis designs or perhaps to cultural differences in the respective countries from which samples have been drawn.
Other bodies of evidence are finding that having memory complaints and memory concerns appears to be associated with a higher risk of developing mild cognitive impairment and dementia (Mah et al. 2014; Kryscio et al. 2014; Abner et al. 2015; Pankratz et al. 2015) and that stress itself may impair cognitive functioning (Liao et al. 2014; Rickenbach et al. 2014). If cumulative, continuing worry about getting AD may qualify as a chronic stressor, and given the known effects of stress (George 2001; Steverink et al. 2011), it is reasonable to hypothesize that the accumulation of stressors related to worries about getting AD can have detrimental effects on physical health and psychological well-being. Tantalizing but preliminary evidence from the work of Cutler and Hodgson (2013, 2014) has, indeed, shown that the more often persons express concerns about their cognitive functioning and the more often they express worries about developing AD, the lower their scores on a variety of measures of psychological well-being and the poorer their physical health.
Based on the foregoing, it would seem to be of great importance to better understand the nature of the worries that persons have about developing AD and the factors that promote those worries. Apart from the substantive importance of learning more about constellations of factors affecting worries about developing AD, also missing from the literature is research based on large-scale, nationally representative studies conducted over multiple waves that would allow for an examination and identification of long-term predictors of worries about getting AD. Almost all of the research on worries about getting AD is cross-sectional, and a good deal of it is based on small samples of questionable representativeness. Investigations reported by Cutler and Hodgson (2013, 2014), while using three waves of data collected over an 11-year period, are based on a small sample of Rs (T 1 N = 258; T 3 N = 177) who resided in the New England area of the U.S. Werner’s (2002) earlier research, to take another example, is based on a cross-sectional convenience sample of 186 Jewish and Arab adults in Israel with no family history of the illness. Recent research by Zeng et al. (2015) in China is based on a sample of 2000, but it is drawn from just five urban areas, areas which ranged in size in 2010 from 2.8 million residents to nearly 29 million residents and which could hardly be considered as representative of the 45 %+ of the Chinese population living in rural areas (World Bank 2014). And while the work by Roberts et al. (2014) is based on a nationally representative sample of the older population of the U.S., it uses only one wave (Wave 10) of the 10 waves of data available in the Health and Retirement Study (HRS; National Institute on Aging [NIA] NIH 2014).
The purpose of the present study, then, is to address several of the gaps and needs identified above. We use an item asked in Wave 10 (2010) of HRS that measures how worried Rs are about getting AD,2 but we examine the effects of measures of self-perceived assessment of present memory functioning obtained in all waves to determine their effect on current worries.3 In so doing, we inquire into the long-term effects of self-assessments of cognitive functioning on current worries about developing AD. This extends the work of Cutler (2015) whose study looked only at contemporaneous predictors of worry about getting AD that were measured in 2010. It also extends the work of Roberts et al. (2014) whose work was restricted to the 2010 HRS data and did not include the measures of self-assessed cognitive functioning as predictors of worries about getting AD. Thus, we go beyond prior work that relied on single wave, cross-sectional, regression-based approaches by using responses from up to 10 waves of data, spanning up to 20 years, collected every two years as part of the ongoing HRS, and by analyzing the longitudinal data using latent growth curve models (McArdle 2009, pp. 592–594; see also Duncan et al. 2006 and Byrne 2010).
Finally, the present study adds to earlier work by extending the range of predictor variables. Specifically, our predictors include (1) over the entire period in which Rs have participated in the HRS, assessments of current memory functioning; (2) Wave 10 measures of personal familiarity with persons who have had AD, beliefs about whether having a first-degree relative who has had AD increases one’s own chances of developing the condition, and the interaction of these two predictors; and (3) Wave 10 demographic variables often used in prior studies (marital status, gender, educational attainment, and age); and measures of depression and health, two variables that prior studies (e.g., Grut et al. 1993; Hanninen 1994; Zandi 2004; Ownby et al. 2006; González et al. 2008; Byers and Yaffe 2011) have suggested might have an explanatory bearing on the relationship between subjective assessments of cognitive functioning and worries about getting AD.4
Methods
Data
The data used in this study are drawn from Waves 1–10 of the University of Michigan’s HRS. HRS is a representative, ongoing longitudinal panel study of older Americans over the age of 50. Supported by NIA and the Social Security Administration, HRS has followed and re-interviewed the original sample every 2 years since 1992 and has added new cohorts of the 50+ population at each wave. These new cohorts are also followed and re-interviewed at 2-year intervals. Data are routinely gathered on income and wealth, health and use of health services, employment, family relationships, biomarkers, and genetics. HRS has also served as a model for the development of longitudinal surveys in other countries [e.g., SHARE—the Survey of Health, Ageing, and Retirement in Europe (Börsch-Supan et al. 2005)], thus enabling comparative research on aging (Tesch-Römer and von Kondratowitz 2006). For additional information about the HRS, see NIA NIH (2014).
Topical modules included in the HRS allow investigators to examine sets of specific issues with a random subsample of HRS Rs. Thus, Wave 10 of HRS in 2010 had a brief module on AD that included our principal outcome variable, worries about developing AD. Items in the Wave 10 module were asked of a subsample of 1734 respondents ages 50 and older. Long-term cognitive predictors of worries for this subsample of Rs were measured in Waves 1–10.
Measures5
Worry
Our principal dependent variable, the measure of worry about developing AD, is based on a single item asking Rs in Wave 10 if they strongly disagree (scored 1); somewhat disagree (2); neither agree nor disagree (3); somewhat agree (4); or strongly agree (5) with the statement “You worry about getting Alzheimer’s someday.”6
Memory assessment
In Waves 1–10 of the HRS, Rs were asked to assess how they perceived their memory performance: “How would you rate your memory at the present time? Would you say it is excellent (scored 5), very good (4), good (3), fair (2), or poor (1)?”
Personal familiarity with AD
Rs were asked in 2010 “Do you know someone who has had Alzheimer’s disease?” and, if so, “Has your [husband/wife/partner], or a parent, sibling, or adult child of yours been diagnosed with Alzheimer’s?” A measure with two categories was constructed from the two questions: R does not know anyone who has AD and R knows someone who has AD but it is not a spouse or partner, nor is it a parent, sibling, or adult child (scored 0); or R has had a spouse or partner, a parent, a sibling, or an adult child who has been diagnosed with AD (1).
Beliefs
Numerous studies have shown that first-degree relatives of someone with AD have a higher probability of having AD themselves (Silverman et al. 1994; Green et al. 2002). Yet, worry may be conditioned upon whether persons believe this to be true or not. Hence, the analysis includes a Wave 10 variable measuring whether Rs answered true (scored 1) or false (0) to the statement “Having a parent or sibling with Alzheimer’s disease increases the chance of developing it.”
Familiarity-beliefs interaction
In the analysis, we also look at the interaction between beliefs and familiarity under the assumption that beliefs about the effects of having a first-degree relative with AD on worry are especially salient for that group of Rs with a first-degree relative with AD. Thus, an interaction variable has been constructed by multiplying the two variables (personal familiarity × beliefs). Rs with a score of 1 represent those with a first-degree relative with AD and who believe that having a first-degree relative with AD increases one’s own chances of getting AD, and those with a score of 0 represent all other Rs.
Demographics and other controls
Marital status is based on Wave 10 responses and has been dichotomized into those Rs who are married (1) and all others (0). On gender, males are scored 1 and females 0. Educational attainment is measured at Wave 10 by number of years in school, recoded to 0–8 years (scored 0), 9–11 years (1), 12 years (2), 13–15 years (3), 16 or 17 years (4), and 18 years or more (5). Rs range in age at Wave 10 from 50 to 98, and age has been included in its raw form as a continuous variable.7 Depression is measured using an 8-item abbreviated version of the CES-D (see Steffick 2000). The Cronbach’s alpha is .803 for this subsample of HRS Rs and higher scores represent higher levels of depression. Finally, health is measured using a self-rated item asking respondents “Would you say your health is excellent (scored 5), very good (4), good (3), fair (2), or poor (1)?”
Analysis
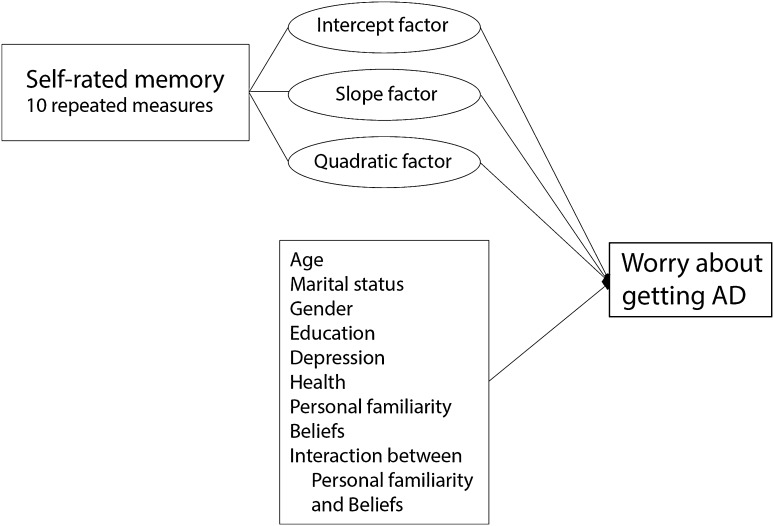
The general conceptual model we are examining in this study is presented in Fig. 1. Specifically, we are interested in knowing whether the initial level of self-assessments of memory functioning (the intercept factor), the long-term rate of change in self-assessed memory functioning (the slope factor), and the rate of acceleration of change in self-assessed memory functioning (the quadratic factor) affect worries about getting AD, net of the effects of a variety of control variables. Also of interest will be the net effects of the controls on worries about getting AD.
Fig. 1.
Conceptual diagram
In addition to descriptive and correlational8 analyses of the variables used in the study, the principal analysis approach we employed was the full information maximum likelihood procedure in a structural equation modeling framework. We also checked for goodness of fit using criteria discussed by Arbuckle (2012). Causal modeling was selected instead of linear regression because we wished to account for the temporal position of our variables, to deal with measurement errors, and to account for the 10 waves of repeated measures of self-perception of cognitive functioning (self-rated memory) by means of latent growth curve modeling (LGCM). Accordingly, the measures were incorporated into an intercept factor (measuring the situation at the beginning, the average of the concept), a slope factor (measuring the rate of change and its direction), and a quadratic factor (measuring the rate of acceleration of change and its direction). All the loadings for the intercept factor are 1, and those for the slope factor were computed on the basis of an arithmetic sequence with a difference of 2 (i.e., the number of years between the waves under analysis with the loading for the first wave being 0, the next one 2, then 4, and so on, with the last one being 18). Loadings for the quadratic factor were computed by squaring the values of the loadings of the slope factor, resulting in the following loadings: for the first wave 0, the next one 4, then 16, then 36, 64, 100, 144, 196, 256, and for the tenth wave 324. The technical procedure for LGCM is based on reflective factors, which account for measurement errors in the observed variables. A full information maximum likelihood approach was used for dealing with missing data in order to include all available respondents in the analysis, a method which is considered to be one of the most robust (Carter 2006; Ferrer et al. 2009).
Results
Descriptive statistics
The main dependent variable—worry about getting AD someday—shows that the majority of Wave 10 HRS Rs were not particularly worried about getting AD (see Table 1). Considering those who strongly (36.4 %) or somewhat (21.7 %) disagreed that they worried about getting AD someday, more than half of the Rs expressed little or no worry. However, a substantial minority of these Rs did express some level of worry, either agreeing strongly (9.5 %) with the statement about being worried or agreeing somewhat (20.6 %) that they worried about getting AD someday.
Table 1.
Descriptive statistics for variables used in the analysis
| Variable | % | Mean | SD | Min. | Max. |
|---|---|---|---|---|---|
| Worry about getting AD | |||||
| 1. Strongly disagree | 36.4 | ||||
| 2. Somewhat disagree | 21.7 | ||||
| 3. Neither agree nor disagree | 11.9 | ||||
| 4. Somewhat agree | 20.6 | ||||
| 5. Strongly agree | 9.5 | ||||
| (N) | (1708) | ||||
| Depression | 1.36 | 1.92 | 0 | 8 | |
| (N) | (1725) | ||||
| Health | |||||
| 1. Poor | 6.5 | ||||
| 2. Fair | 19.9 | ||||
| 3. Good | 31.7 | ||||
| 4. Very good | 30.8 | ||||
| 5. Excellent | 11.1 | ||||
| (N) | (1733) | ||||
| Personal familiarity with AD | |||||
| 0. Knows no one with AD or Knows someone but not 1st degree relative | 87.1 | ||||
| 1. Has 1st degree relative with AD | 12.9 | ||||
| (N) | (1733) | ||||
| 1st degree relative with AD increases chances (beliefs) | |||||
| 1. True | 65.4 | ||||
| 0. False | 34.6 | ||||
| (N) | (1671) | ||||
| Personal familiarity × beliefs | |||||
| 1. Belief = true and has 1st degree relative | 8.5 | ||||
| 0. All others | 91.5 | ||||
| (N) | (1701) | ||||
| Marital status | |||||
| 1. Married | 58.4 | ||||
| 0. All others | 41.6 | ||||
| (N) | (1734) | ||||
| Gender | |||||
| 1. Male | 43.7 | ||||
| 0. Female | 56.3 | ||||
| (N) | (1743) | ||||
| Education | |||||
| 0. 0–8 years | 8.4 | ||||
| 1. 9–11 years | 12.3 | ||||
| 2. 12 years | 32.1 | ||||
| 3. 13–15 years | 23.7 | ||||
| 4. 16 years | 12.4 | ||||
| 5. 17 years or more | 11.1 | ||||
| (N) | (1724) | ||||
| Age | 66.45 | 10.93 | 50 | 98 | |
| (N) | (1734) | ||||
The descriptive statistics show that signs of depression are not highly prevalent among the Rs in this sample (mean of 1.36), and only a minority consider themselves as being in poor (6.5 %) or fair (19.9 %) health. A clear majority of Rs either know no one with AD or know someone with AD who is not a first-degree relative (87.1 %). These Rs also seem to have a good understanding of the genetic implications of having a first-degree relative with AD: just under two-thirds of the Rs (65.4 %) correctly indicate that having a parent or sibling with AD increases one’s chances of developing it. With respect to the interaction variable, 8.5 % of our Rs have a first-degree relative with AD and believe that having a first-degree relative with AD increases one’s own chances of getting AD while 91.5 % are included in all the other types.
In terms of demographics, the majority of these Rs are married (58.4 %). Consistent with the older age distribution of the sample, 56.3 % are female. Slightly more than half (52.8 %) have 12 or fewer years of education. The sample mean age is approximately 66.5 years.
Concerning the distribution of the repeated measures of memory, most Rs place themselves toward the middle of the memory measurements, although there seems to be a general increase in the percentages of those who rate their memory as fair or poor with each successive wave (see Table 2). Sample attrition over time is also noticeable as the number of missing data cases decreases at successively recent waves.
Table 2.
Descriptive statistics for variables used in the analysis: Self-perceptions of cognitive functioning in each wave
| Self-rated memory (%) | Rs1 | Rs2 | Rs3 | Rs4 | Rs5 | Rs6 | Rs7 | Rs8 | Rs9 | Rs10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Poor | 1.4 | 1.4 | 3.1 | 3.1 | 2.3 | 3.1 | 4.0 | 4.0 | 5.0 | 5.0 |
| 2. Fair | 9.5 | 12.7 | 23.1 | 18.2 | 19.6 | 20.5 | 23.8 | 23.6 | 22.7 | 22.4 |
| 3. Good | 30.1 | 33.1 | 44.5 | 44.4 | 46.2 | 44.8 | 42.3 | 43.6 | 43.5 | 41.1 |
| 4. Very good | 40.5 | 35.6 | 22.2 | 26.4 | 26.7 | 25.8 | 23.9 | 23.2 | 24.0 | 25.1 |
| 5. Excellent | 18.5 | 17.2 | 7.2 | 8.0 | 5.2 | 5.7 | 5.9 | 5.6 | 4.9 | 6.5 |
| (N) | (578) | (646) | (650) | (914) | (904) | (925) | (1149) | (1166) | (1194) | (1734) |
Corroboration of the Table 2 results is seen in Table 3, which presents the mean levels of the self-reported memory factors. All significant at the 0.001 level, the mean of self-rated memory in Wave 1 was 3.7 (the intercept factor), self-rated memory performance decreased over the 20 years (−0.076; the slope factor), and the acceleration of change was low (but significant) over the 20-year span (−0.002; the quadratic factor). The variances are also statistically significant at the 0.001 level and show individual differences across respondents of 0.425 on the initial intercept and 0.008 on the rate of change. In terms of acceleration of change, the variance of 0.000 indicates that the pattern of variation of change was not very different across respondents in the sample under analysis, but it too is statistically significant.
Table 3.
Means and variances of the intercept, slope, and quadratic factors in the latent growth curve model
| Variable | Mean | Variance |
|---|---|---|
| Self-rated memory: intercept factor | 3.734*** | 0.425*** |
| Self-rated memory: slope factor | −0.076*** | 0.008*** |
| Self-rated memory: quadratic factor | −0.002*** | 0.000*** |
Level of significance *** p<0.001
Bolded entries are statistically significant
Multivariate results
Net of the effects of all the other variables entered in the model, the data in Table 4 show support for the importance of examining long-term precursors of current worries about getting AD. In terms of self-assessments of current levels of memory functioning over the 10 waves, both the significant intercept effect (−0.264) and the negative significant slope effect (−0.208) on worry support our hypothesis. Poorer initial assessments and trends toward more negative assessments are significantly associated with higher levels of worry. And the significant coefficient for the quadratic factor suggests that the rate of acceleration of change has a negative and statistically significant effect (−0.234) on worry. In other words, a negative history of changes in memory assessment is associated with higher levels of worry.
Table 4.
Standardized coefficients (standard errors in parentheses) in the prediction of worry about getting Alzheimer’s disease
| Variable | Worry |
|---|---|
| Self-rated memory intercept factor |
−0.264*
(0.107) |
| Self-rated memory slope factor |
−0.208***
(1.787) |
| Self-rated memory quadratic factor |
−0.234*
(32.817) |
| Personal familiarity | 0.051 (0.180) |
| Beliefs |
0.073**
(0.081) |
| Interaction between personal familiarity and beliefs | 0.083 + (0.220) |
| Age |
−0.136***
(0.003) |
| Marital status | 0.021 (0.075) |
| Gender | 0.005 (0.092) |
| Education | 0.035 (0.027) |
| Depression |
0.092**
(0.021) |
| Health | 0.001 (0.038) |
| R 2 | 0.105 |
Level of significance *** p<0.001; ** p<0.01; * p<0.05; + p<0.10
Statistically significant coefficients in bold
Net of all other variables in the model, having a first-degree relative with AD and believing that having a first-degree relative with AD increases one’s own chances of getting AD is also associated with a higher level of worry (0.083) (see Table 4). Although the effect of the interaction term is significant at the p < 0.10 level, only one of the two component variables—beliefs—is statistically significant.
The remaining effects in the model are also presented in Table 4. Of the four demographic variables, only age exerts a statistically significant effect on worry. As others using these data have found (Roberts et al. 2014; Cutler 2015), that age effect is negative: the greater the age, the less the worry (−0.136). The direct effects of marital status, education, and gender on worry are all statistically nonsignificant. Depression is a significant predictor of worry: the higher the level of depression, the greater the worry about getting AD. The effect of self-reported health is statistically nonsignificant.
With respect to the adequacy of the model, we examined the explained variance and various measures of goodness of fit. First, all of the variables in the model explain only 10.5 % of the variance in worry about getting AD. Although low, this result is similar to other findings in the literature as discussed below. Second, in regard to goodness of fit, we looked at the CFI (comparative fit index) and RMSEA (root mean square error of approximation) tests (Arbuckle 2012, pp. 599–605). The CFI is 0.978 (greater than 0.95), while the RMSEA is 0.029 (smaller than 0.05 and its associated PCLOSE is 1, greater than 0.05). These two tests show that the model is a good fit to the data. Although specific causal effects may be open to discussion, these results suggest that the conceptual model in Fig. 1 can provide a useful framework for further analyses.
Discussion
The prevalence of AD will increase dramatically in coming years. It is also likely that lay knowledge of the condition and recognition of its symptoms will increase. Accumulating evidence points to the fear that AD generates among middle-aged and older persons. And there is the beginning of a body of research suggesting that such “anticipatory dementia,” as Cutler and Hodgson (1996) call it, and “dementia worry,” as Kessler et al. (2012) have called it, if experienced long enough and seriously enough, may prove to be detrimental to physical and psychological well-being. Long ago, W. I. Thomas (Thomas and Thomas 1928) observed that if persons perceive a situation as real, it is real in its consequences. For these reasons, how AD is perceived warrants careful study.
The current research examines both long-term and short-term precursors of worries about getting AD. While this is not the first investigation to look at correlates of fear, it adds to the existing literature in three important respects. First, the analysis is based on a large-scale, nationally representative sample of older persons ages 50 and over. Although some studies of worries about getting AD are based on nationally representative data (Roberts et al. 2014), many investigations have relied upon small-scale samples of questionable representativeness (Werner 2002; Cutler and Hodgson 2013, 2014; Zeng et al. 2015). Second, to our knowledge no large-scale, nationally representative study has used multiwave data that would enable a longer-term perspective on worries about getting AD. And, third, we know of no studies that have used analytic techniques such as latent growth curve modeling to take advantage of longitudinal data to examine how worries about getting AD are affected by long-term, self-assessments of cognitive functioning as measured in a large-scale, multiwave, nationally representative survey.
The present research addresses each of these shortcomings by using the HRS, which includes up to ten waves of data collected over a 20-year period. The availability of these data enables us to examine both long-term and short-term predictors of current AD worries. Specifically, we employ measures of how Rs perceive their present memory performance, measures that were obtained at each wave in which an R participated in the survey. In addition to these long-term predictors, we examine the effects of whether the R knows someone with AD and who that person is combined with beliefs about whether having a first-degree relative with AD increases one’s chances of getting AD. Finally, we include in the analysis—both as controls and to assess their independent effects on worry about getting AD—several demographic and other variables suggested by prior work: age, education, marital status, gender, depression, and health.
The results of our analyses provide support for a hypothesis about long-term effects of memory assessments and present some additional findings. In terms of the latter, the net effects of three of the four demographic variables were weak and nonsignificant. Neither gender nor education nor marital status proved to be a significant predictor of worries about getting AD. Nor was self-reported health, although a more nuanced variable measuring worries about health may have been more appropriate for inclusion had it been available in HRS.
On the other hand, and as some have suggested (e.g., Grut et al. 1993; Zandi 2004; Byers and Yaffe 2011), depression did have a significant and independent effect on worries about getting AD. Age also had a significant but negative effect. Given that age is widely considered to be the best predictor of being diagnosed with AD (Alzheimer’s Association 2015), we would have expected increasing age to be associated with increasing worry. However, and as others who have used these data have found (Roberts et al. 2014; Cutler 2015), increasing age was associated with decreasing worry. Perhaps this reflects a perceived threshold effect such that persons 50 years of age and older become less worried about getting AD as they advance in years. Had the question on worries about getting AD been asked in every wave—rather than just in wave 10—it would have been possible to test this hypothesis more directly by following the trajectory of worries over time. Unfortunately, this is not possible with the HRS data.
Apart from the age and depression effects, several findings net of the demographic and other controls are noteworthy. Importantly, and net of all other variables, our analysis provides evidence that long-term self-assessments of memory are of consequence in predicting worries about getting AD. In terms of self-assessments of current levels of memory functioning over the 10 waves, the significant effects of the intercept, slope, and quadratic factors support the hypothesis that a long-term perspective on self-reported memory functioning is of importance in understanding current levels of worries about getting AD. Poorer initial assessments, trends toward more negative assessments, and acceleration of change of negative assessments are associated with higher levels of worry. These results suggest that a history of negative assessments of memory functioning is of significance in predicting worries about getting AD, not just contemporary assessments of memory performance (Cutler 2015). In addition, we have been able to specify the relationships between personal familiarity with someone with AD, beliefs about whether having a first-degree relative with AD confers a greater chance of getting it, and worries. Although beliefs about the role of genetics is itself significantly associated with worry, the role of beliefs in heightening worry is especially important among Rs with a first-degree relative who has or who has had AD as indicated by the interaction term.
In short, our findings reinforce the importance of examining subjective assessments of cognitive functioning as predictors of concerns about developing AD. Our results also reinforce the utility of doing so over an extended period of time and not simply relying on contemporaneous assessments of cognitive performance and memory functioning. They also indicate that the combination of having a first-degree relative with AD and believing that having a first-degree relative with AD increases one’s own chances of getting AD is an important predictor in worries. Confirming Thomas’ dictum about the definition of the situation (Thomas and Thomas 1928), these results point to how beliefs and knowledge about AD function as predictors of worries.
To conclude, we note four directions that future research should take. First, it is in the nature of secondary analysis that this study is constrained by having to use limited indicators. In particular, we have had to rely upon a single indicator of worries about getting AD. It would have been valuable to be able to draw upon a more textured and nuanced outcome variable that captures a wider range of dimensions of worries about getting AD. Further psychometric work along these lines is much needed. In addition, we have had only limited access to some important control variables. Although we have been able to control for the effects of health and depression in addition to important demographic variables, HRS does not allow us to parcel out the effects of other relevant personality controls such as neuroticism (see, for example, Pearman and Storandt 2005; Steinberg et al. 2013).
Second, as has been the case with other studies on the topic of worries about getting AD, the predictors identified in this analysis have explained only a small proportion of the variance in worries. Specifically, the R 2 of .105 is only slightly higher than what Werner et al. (2013) and Cutler (2015) found. Although this study has demonstrated the substantive and statistical significances of the variables we have examined, there is clearly much more that needs to be done to understand the sources of worries about getting AD.
Third, the work of Cutler and Hodgson (2013, 2014) has explored the connections between cognitive assessments, AD worries, and selected measures of psychological and physical well-being. Those studies suggest that negative assessments of cognitive functioning and dementia worries are detrimental to psychological and physical well-being. As noted earlier, however, the samples on which the data are based are small and from a limited geographic area. Just as the current study has looked at predictors of worries about getting AD, so too can HRS be used to look at a variety of well-being outcomes of cognitive assessments and concerns about getting AD. That HRS is both nationally representative of the older population and longitudinal in design enhances the attractiveness and potential robustness of such research.
Finally, HRS is being used as both a model and a template for studies of aging in other nations. The Survey of Health, Ageing, and Retirement in Europe (SHARE) is one such endeavor (Börsch-Supan et al. 2005). Others include the Mexican Health and Ageing Study (MHAS), the Japanese Study of Aging and Retirement (JSTAR), and the China Health, Aging, and Retirement Longitudinal Study (CHARLS).9 As the five-nation study shows (Harvard School of Public Health and Alzheimer Europe 2011), fear of getting AD crosses national borders and is widely prevalent in other countries. Including items on AD in these other surveys and replicating our analysis in other nations would allow for comparative, macrostructural studies of the prevalence, predictors, and consequences of fear (Kessler et al. 2012).
Acknowledgments
The authors wish to thank Paula Tufiş of the Faculty of Sociology and Social Work at the University of Bucharest and the two reviewers for their contributions to the analysis reported in this article.
Footnotes
This conclusion of the U.S. National Institutes of Health state-of-the-science conference on preventing AD and cognitive decline reported in Daviglus et al. (2010) represents one perspective. On the other hand, a recent report from Alzheimer’s Disease International (Prince et al. 2014) suggests that the risk of dementia may be modifiable through selected behavioral interventions. This article is not the place to reconcile these divergent conclusions, although sorting out the evidence for such conflicting positions will without doubt be a high-priority agenda item.
Although a version of data from Wave 11 (2012) has been released, it could not be used in this study because our principal dependent variable, R’s worry about getting AD, was not asked in Wave 11 nor in any wave other than Wave 10.
Another measure of cognitive assessment asked over the entire span refers to a comparison of memory functioning between the current time and 2 years earlier. For a variety of reasons, but mainly because the analytic approach we use in the study will already capture change and rate of change in self-reported memory, we have elected to exclude these measures of self-reported, two-year changes in memory functioning.
Prior work (e.g., Pearman and Storandt 2005; Steinberg et al. 2013; Johansson et al. 2014) has also concluded that selected personality variables associated with subjective memory complaints and concerns about AD may be relevant controls. We tried to represent this focus in the present study by including neuroticism as a control variable, but we were unable to do so because the split-ballot nature of HRS meant there was only minimal overlap between Rs who responded to the neuroticism items and Rs who responded to the topical module on AD concerns.
Distributional characteristics on the measures used in the analysis are presented in Tables 1, 2, and 3 and discussed in the “Results” section.
As used here, the responses to this item (as well as to the following item on memory assessment) were reverse scored compared to the original version.
We also included age2 to assess whether there is a curvilinear relationship between age and worries about getting AD, but the effect of this multiplicative term on worries proved to be nonsignificant.
To determine whether multicollinearity might be a potential problem, we examined the correlation matrix of all variables included in the study. Because only one of the coefficients exceeded .6 (.618) and because all of the remaining coefficients were below .6, with most of them being well below that level, we concluded that multicollinearity was not likely to be a problem.
For additional information on these and other investigations that are referred to as the HRS “family” of studies, see http://gateway.usc.edu/ and http://grants.nih.gov/grants/guide/rfa-files/RFA-AG-15-015.html.
The data used for this study are available from the University of Michigan at http://hrsonline.isr.umich.edu/ (Wave 10 downloaded on September 28, 2014) or from the Rand Corporation at http://www.rand.org/labor/aging/dataprod.html (version M, downloaded on September 30, 2014).
The authors wish to dedicate this article to the memory of Dr. Richard Suzman, Director of the Division of Behavioral and Social Research at the National Institute on Aging, National Institutes of Health without whose vision and support there would be no Health and Retirement Study (HRS).
An erratum to this article can be found at http://dx.doi.org/10.1007/s10433-015-0353-0.
References
- Abner EL, Kryscio RJ, Caban-Holt AM, Schmitt FA. Baseline subjective memory complaints associate with increased risk of incident dementia: the PREADVISE trial. J Prev Alzheimer’s Dis. 2015;2:11–16. doi: 10.14283/jpad.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Association Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2015;11:332–384. doi: 10.1016/j.jalz.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL (2012) IBM® SPSS® Amos™ 21 user’s guide. Amos Development Corporation
- Börsch-Supan A, Hank K, Jürges H. A new comprehensive and international view on ageing: introducing the “Survey of Health, Ageing and Retirement in Europe”. Eur J Ageing. 2005;2:245–253. doi: 10.1007/s10433-005-0014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7:323–331. doi: 10.1038/nrneurol.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM. Testing for change over time: the latent growth curve model. Structural equation modeling with AMOS: basic concepts, applications, and programming. 2. New York: Routledge (Taylor & Francis Group); 2010. pp. 303–325. [Google Scholar]
- Cantegreil-Kallen I, Pin S. Fear of Alzheimer’s disease in the French population: impact of age and proximity to the disease. Int Psychogeriatr. 2012;24:108–116. doi: 10.1017/S1041610211001529. [DOI] [PubMed] [Google Scholar]
- Carter RL. Solutions for missing data in structural equation modeling. Res Pract Assess. 2006;1:4–7. [Google Scholar]
- Commisaris CJAM, Jolles J, Verhey FRJ, et al. Forgetfulness or dementia? Who is worried and why? Eur J Public Health. 1996;6:297–299. doi: 10.1093/eurpub/6.4.297. [DOI] [Google Scholar]
- Cutler SJ. Worries about getting Alzheimer’s: who’s concerned? Am J Alzheimers Dis Other Demen. 2015;30(1):98–100. doi: 10.1177/1533317514559827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler SJ, Hodgson LG. Anticipatory dementia: a link between memory appraisals and concerns about developing Alzheimer’s disease. Gerontologist. 1996;36:657–664. doi: 10.1093/geront/36.5.657. [DOI] [PubMed] [Google Scholar]
- Cutler SJ, Hodgson LG. Correlates of personal concerns about developing Alzheimer’s disease among middle-aged persons. Am J Alzheimers Dis Other Demen. 2001;16:335–343. doi: 10.1177/153331750101600604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler SJ, Hodgson LG. Concerns about cognitive functioning, dementia worries, and psychological well-being. Rev Asistenţă Soc. 2013;XI:77–86. [Google Scholar]
- Cutler SJ, Hodgson LG. Is health affected by dementia worries and concerns about cognitive functioning? Rev Asistenţă Soc. 2014;XII:7–15. [Google Scholar]
- Daviglus ML, Bell CC, Berrettini W, et al. National Institutes of Health state-of-the-science conference statement: preventing Alzheimer disease and cognitive decline. Ann Intern Med. 2010;153:176–181. doi: 10.7326/0003-4819-153-3-201008030-00260. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling. New Jersey: Lawrence Erlbaum Associates Inc.; 2006. [Google Scholar]
- Ferrer E, Hamagami F, McArdle JJ. Modeling latent growth curves with incomplete data using different types of structural equation modeling and multilevel software. Struct Equ Model. 2009;11:452–483. doi: 10.1207/s15328007sem1103_8. [DOI] [Google Scholar]
- George L. The social psychology of health. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. 5. San Diego: Academic Press; 2001. pp. 217–237. [Google Scholar]
- González HM, Bowen ME, Fisher GG. Memory decline and depressive symptoms in a nationally representative sample of older adults: the Health and Retirement Study (1998–2004) Dement Geriatr Cogn Disord. 2008;25:266–271. doi: 10.1159/000115976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green RC, Adrienne CL, Go R, et al. Risk of dementia among white and African American relatives of patients with Alzheimer disease. J Am Med Assoc. 2002;287:329–336. doi: 10.1001/jama.287.3.329. [DOI] [PubMed] [Google Scholar]
- Grut M, Jorm AF, Fratiglioni L, et al. Memory complaints of elderly people in a population survey: variation according to dementia stage and depression. J Am Geriatr Soc. 1993;41:1295–1300. doi: 10.1111/j.1532-5415.1993.tb06478.x. [DOI] [PubMed] [Google Scholar]
- Hanninen T. Subjective memory complaints and personality traits in normal elderly subjects. J Am Geriatr Soc. 1994;42:1–4. doi: 10.1111/j.1532-5415.1994.tb06064.x. [DOI] [PubMed] [Google Scholar]
- Harvard School of Public Health and Alzheimer Europe (2011) Five-country Alzheimer’s disease survey. http://www.hsph.harvard.edu/news/press-releases/alzheimers-international-survey/. Accessed 7 June 2015
- Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778–1783. doi: 10.1212/WNL.0b013e31828726f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffington Post UK/PA (2014) Why people fear dementia more than they do cancer. In: Huffingt. Post UK. http://www.huffingtonpost.co.uk/2014/08/04/dementia-more-feared-than-cancer_n_5646872.html. Accessed 7 June 2015
- Johansson L, Guo X, Duberstein PR, et al. Midlife personality and risk of Alzheimer disease and distress: a 38-year follow-up. Neurology. 2014;83:1538–1544. doi: 10.1212/WNL.0000000000000907. [DOI] [PubMed] [Google Scholar]
- Kessler E-M, Bowen CE, Baer M, et al. Dementia worry: a psychological examination of an unexplored phenomenon. Eur J Ageing. 2012;9:275–284. doi: 10.1007/s10433-012-0242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kryscio RJ, Abner EL, Cooper GE, et al. Self-reported memory complaints: implications from a longitudinal cohort with autopsies. Neurology. 2014;83:1359–1365. doi: 10.1212/WNL.0000000000000856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao J, Head J, Kumari M, et al. Negative aspects of close relationships as risk factors for cognitive aging. Am J Epidemiol. 2014;180:1118–1125. doi: 10.1093/aje/kwu236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah L, Binns MA, Steffens DC. Anxiety symptoms in amnestic mild cognitive impairment are associated with medial temporal atrophy and predict conversion to Alzheimer’s disease. Am J Geriatr Psychiatry. 2014 doi: 10.1016/j.jagp.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annu Rev Psychol. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- MetLife Foundation (2006) MetLife Foundation Alzheimer’s survey: what America thinks. muskrat.middlebury.edu/Lt/cr/faculty/shalpern-lt/Memory/20538296421147208330V1FAlzheimersSurvey.pdf. Accessed 7 June 2015
- MetLife Foundation (2011) What America thinks: MetLife Foundation Alzheimer’s survey. https://www.metlife.com/assets/cao/foundation/alzheimers-2011.pdf. Accessed 7 June 2015
- National Institute on Aging (NIA) NIH (2014) Growing older in America: the Health and Retirement Study. http://hrsonline.isr.umich.edu/index.php?p=dbook. Accessed 7 June 2015
- Ownby RL, Crocco E, Acevedo A, et al. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530–538. doi: 10.1001/archpsyc.63.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pankratz S, Roberts RO, Mielke MM, et al. Predicting the risk of mild cognitive impairment in the Mayo Clinic study of aging. Neurology. 2015;84:1433–1442. doi: 10.1212/WNL.0000000000001437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman A, Storandt M. Self-discipline and self-consciousness predict subjective memory in older adults. J Gerontol Ser B. 2005;60:153–157. doi: 10.1093/geronb/60.3.P153. [DOI] [PubMed] [Google Scholar]
- Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer’s Dement. 2013;9:63–75. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Prince M, Albanese E, Guerchet M, Prina M (2014) World Alzheimer report 2014: dementia and risk reduction, London
- Rickenbach EH, Almeida DM, Seeman TE, Lachman ME. Daily stress magnifies the association between cognitive decline and everyday memory problems: an integration of longitudinal and diary methods. Psychol Aging. 2014;29:852–862. doi: 10.1037/a0038072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JS, McLaughlin SJ, Connell CM. Public beliefs and knowledge about risk and protective factors for Alzheimer’s disease. Alzheimer’s Dement. 2014;10:S381–S389. doi: 10.1016/j.jalz.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman JM, Li G, Zaccario ML, et al. Patterns of risk in first degree relatives of patients with Alzheimer’s disease. Arch Gen Psychiatry. 1994;51:577–586. doi: 10.1001/archpsyc.1994.03950070069012. [DOI] [PubMed] [Google Scholar]
- Steffick DE (2000) HRS/AHEAD Documentation report DR-00: documentation of affective functioning measures in the Health and Retirement Study. Ann Arbor, MI
- Steinberg SI, Negash S, Sammel M, et al. Subjective memory complaints, cognitive performance, and psychological factors in healthy older adults. Am J Alzheimers Dis Other Demen. 2013;28:776–783. doi: 10.1177/1533317513504817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steverink N, Veenstra R, Oldehinkel AJ, et al. Is social stress in the first half of life detrimental to later physical and mental health in both men and women? Eur J Ageing. 2011;8:21–30. doi: 10.1007/s10433-011-0178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takizawa C, Thompson P, van Walsen A, et al. Epidemiological and economic burden of Alzheimer’s disease: a systematic literature review of data across Europe and the United States of America. J Alzheimer’s Dis. 2014 doi: 10.3233/JAD-141134. [DOI] [PubMed] [Google Scholar]
- Tesch-Römer C, von Kondratowitz H-J. Comparative ageing research: a flourishing field in need of theoretical cultivation. Eur J Ageing. 2006;3:155–167. doi: 10.1007/s10433-006-0034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas WI, Thomas DS. The child in America: behavior problems and programs. New York: Knopf; 1928. [Google Scholar]
- Werner P. Assessing correlates of concern about developing Alzheimer’s dementia among adults with no family history of the disease. Am J Alzheimers Dis Other Demen. 2002;17:331–337. doi: 10.1177/153331750201700609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner P, Goldberg S, Mandel S, Korczyn AD. Gender differences in lay persons’ beliefs and knowledge about Alzheimer’s disease (AD): a national representative study of Israeli adults. Arch Gerontol Geriatr. 2013;56:400–404. doi: 10.1016/j.archger.2012.11.001. [DOI] [PubMed] [Google Scholar]
- World Bank (2014) Urban population (% of total). http://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS. Accessed 7 June 2015
- Zandi T. Relationship between subjective memory complaints, objective memory performance, and depression among older adults. Am J Alzheimers Dis Other Demen. 2004;19:353–360. doi: 10.1177/153331750401900610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng F, Xie W, Wang Y, et al. General public perceptions and attitudes toward Alzheimer’s disease from five cities in China. J Alzheimer’s Dis. 2015;43:511–518. doi: 10.3233/JAD-141371. [DOI] [PubMed] [Google Scholar]