Abstract
Background
Improved treatment options of HIV have resulted in regular physical activities of many HIV-infected patients. However, data on effects of sports in HIV-patients are scarce.
Methods
21 HIV-infected persons were monitored prospectively while preparing for a marathon run. Multiple parameters with regard to immunology, quality of life and metabolism were measured at 4 time points (at baseline 1 year before the marathon run, 3 and 6 months after beginning of training, and immediately before marathon).
Results
13 out of 21 participants completed the marathon (12 male, 1 female; median age 42 years [27–50]; CD4 = 620/μl [146–1268]; 11 were on ART since 3.5 years [1–7]). 8 participants ceased training early. All reasons for stopping (besides one pre-existing metatarsal fracture) were not regarded as training-related (e.g. time limitation n = 3; newly diagnosed anal cancer n = 1; personal reasons/unknown n = 3).
We observed a significant increase in absolute CD4-T-cells (620/μl [146–1268] vs. 745 [207–1647]; p = 0.001) with simultaneous decrease of CD4-T-cell apoptosis (53% [47–64] vs. 32% [14–42]); p < 0.01). No effects on viral load independent of ART occurred. Systolic blood pressure and cholesterol improved significantly, although moderate and normal at baseline (cholesterol 185 mg/dl [98–250] vs. 167 [106–222], p = 0.02; RRsys 125 mmHg [100–145] vs. 120 [100–140], p = 0.01). Blood count, liver enzymes, creatinine and CK remained unchanged.
Conclusions
The results of this pilot study indicated improved metabolic and immunologic parameters in HIV-infected patients undergoing moderate endurance training. Although training effects or ART cannot be ultimately separated as underlying mechanisms, we conclude that marathon training is safe for HIV-infected patients and potentially improves general health.
Trial registration
DRKS00011592 (retrospectively registered on February 9th 2017).
Keywords: Endurance training, Marathon, HIV-infection
Background
The face of HIV infection has changed dramatically over the past decade. Due to continuous improvements in ART life expectancy approaches to that of the general population in most developed countries [1]. Quality of life has also improved for most treated patients, who are able to participate in daily activities without restrictions. Amongst other activities, strenuous exercise is undertaken by an increasing proportion of patients. However, HIV research has focused mainly on ART and associated problems such as efficacy, safety and tolerability, long term toxicities [2] and since recently prophylaxis [3]. Little is known about effects of usual activities such as exercise on HIV-associated clinical parameters and health state.
Effects of physical exercise on health have been discussed for decades. Most studies performed have focussed on cardiovascular disease. Impact of physical activities has been studied in other chronic diseases such as chronic obstructive pulmonary disease, chronic kidney disease, asthma and osteoporosis [4], diabetes type 2 [5], colon cancer [6] and dementia [7]. Studies in HIV-infected patients were conducted in the pre-ART era [8, 9] or addressed typical complications of HIV-infected patients such as wasting [10], lipodystrophy [11, 12], anxiety, depression or HIV-associated neurocognitive disorder (HAND) [13, 14]. However, studies on effects of physical exercise beyond the treatment of HIV-associated complications are scarce.
This is of particular interest as there is increasing evidence that immunologic functions and lymphocyte responses and proliferation are affected by exercise [15, 16]. It is the hypothesis that acute effects may be rather immunosuppressive whereas in the long-term fewer infections and better immune function are observed. Immunosuppression following exhaustive, acute activities might be due to numeric changes in peripheral white blood cells [17, 18] and functional changes such as reduced neutrophil function (chemotaxis, polarization) [19], IgA-secretion [20] and NK-cell activity [21]. Accordingly, the risk of upper respiratory tract infections (URTI) is increased in athletes by up to 2–6 times compared to the general population [22, 23], especially following a long-term period of heavy training and 1–2 weeks after a competition [22, 23]. In contrast, moderate exercise has a favourable long-term effect on the overall incidence of self-reported URTI. Studies showed up to 43% annual risk reduction [24] as well as a positive effect on severity and duration of URTIs [24]. Hence, the interplay between physical activities and immune function is of special interest in the HIV-infected population.
In the present study, we assessed the effects of moderate endurance training on HIV-infected persons. We analysed immunological and metabolic data of HIV-infected subjects performing regular moderate aerobic exercise over a period of one year their aim of running a marathon.
Methods
Participants
A total of 21 HIV-infected subjects starting moderate endurance training in order to participate in a marathon run (VIII Gay Games in Cologne, Germany) were followed prospectively for one year. Participants could apply nationwide via an internet-based procedure. Volunteers had to be at least 18 years and were required to have no restriction for running (e.g. heart insufficiency) certified by their treating physician. There was no restriction with respect to HIV-infection, i.e. AIDS present or not, on ART or not. Selection process took place centrally in a randomized and anonymous manner.
Study participants were provided an intensive program: individual training plans were established by supervising exercise scientists (iQathletik GmbH, Frankfurt, Germany). Psychological support, information on equipment and nutritional facts were provided.
Participants were monitored within the study. There was no influence on medical decisions of the treating HIV-specialists. Safety parameters were revealed after every visit and communicated to the patient only in case of immediate need for reaction (this was not the case).
Persons for a reference group were chosen as age-matched HIV-positive volunteers from the infectious diseases clinic of the university clinic of Bonn, Germany.
Training
After pre training examination, participants trained three to four times per week following the individual training plans provided. Duration of training was about 3 to 4 h per week in the first training period.
Participants trained at 60–70% of maximum heart rate. Support was given directly by the exercise scientists. In the first twelve weeks the subjects’ endurance was gradually built up. Main goal of this training was to improve aerobic metabolism capacity.
After post training examination, weekly training hours were increased up to 6 h per week with the aim of economization of metabolism and cardiovascular system. Intensity of training was increased up to 70–80% of maximum heart rate.
Seven months after pre training examination, training duration increased up to 7 to 10 h per week of moderate endurance runs. For improvements of threshold performance and enzyme systems of anaerobic glycolysis, the participants had to also practice extensive sprints (e.g. 3*2 km with 800 m relaxed pace in between).
2 weeks before the marathon, participants trained only basic endurance at 60–70% of maximal heart rate.
Parameters assessed
All Participants were monitored at central meetings, which took place at 4 time points – at 12 months before the marathon run, 9 months, 6 months and right before the run. At each time point following parameters were assessed: systolic and diastolic blood pressure, pulse, weight, CD4-T-cell count and viral load, fasting lipids and glucose, liver transaminases, creatine kinase, phosphate, differential blood count. In addition, CD4T-cell apoptosis was measured. Venous blood samples were taken in the early morning hours after overnight fasting before physical activity on the respective day. Participants reported adverse events such as infections via a self-reporting diary. They were observed for infectious complications four weeks after finishing the marathon.
Routine laboratory parameters were assessed in the central clinical laboratory of the University of Bonn.
Assessment of absolute numbers of CD4+, CD8+ T cells, B cells and NK cells was conducted by multi-parameter flow cytometry using BD Trucount tubes (Becton Dickinson, Heidelberg, Germany). Briefly, 50 μl of fresh whole blood was stained with BD Multitests comprising the following fluorochrome-labelled monoclonal antibodies (mAb); Panel 1: CD3-fluoresceinisothiocyanate (FITC), CD4-Allophycocyanin (APC), CD8-phycoerythrin (PE), CD45 peridinin chlorophyll protein (PerCP); Panel 2: CD3-FITC, CD16/CD56-PE, CD45-PerCP, CD19-APC. Following red blood cell lysis and fixation, cells (FACS lysing solution, Becton Dickinson) were analysed on a FACSCalibur and absolute cell numbers were calculated by BD MultiSet software (Becton Dickinson).
Levels of CD4-T-cells apoptosis were determined by Annexin V assay (Becton Dickinson). 100 μl of fresh whole blood was stained with CD3-PerCP and CD4-APC, washed and subsequently treated with BD Pharm Lysis buffer to remove red blood cells. After additional washing cells were stained with FITC-labelled annexin V and propidium iodide according to the manufacturer’s instructions. Cells were acquired on a FACSCalibur within 30 min post staining and subsequently analysed using FlowJo software.
Quality of life was assessed using the Medical Outcomes Study HIV Health Survey (MOS-HIV). The MOS-HIV is composed of 35 items investigating 11 dimensions and recalls the last 4 weeks. These are described in detail in [25]. Questionnaires were handed to the participants in the German translation of the MOS-HIV (German MOS-HIV Questionnaire, Version 2.1). It was provided by MAPI Research Trust, Lyon, France (MOS-HIV contact information and permission to use: MAPI Research Trust, Lyon, France. E-mail: contact@mapi-trust.org). Scaling and Scoring was performed according to the instructions provided.
Statistical analysis
For statistical analysis GraphPad Prism (Version 3.0.3, GraphPad Software, La Jolla, USA) was used. Standard methods of descriptive statistics were applied (Student t-test for paired samples).
For calculation of the Homeostasis Model Assessment (HOMA) index the HOMA2 Calculator v2.2 (Diabetes Trials Unit, University of Oxford, http://www.dtu.ox.ac.uk/homacalculator/).
Availability of data and materials
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
The project was initiated, organized and sponsored by Abbott Pharmaceuticals (Wiesbaden, Germany; now Abbvie). However, the sponsor had no influence on scientific design and no access to results until completion of the project.
The study was approved by the Ethics committee of the University of Bonn (sequential number 138/09), which is in accordance with the provisions of the Declaration of Helsinki. Informed consent was given by all participants.
Results
Participant characteristics
21 HIV-positive persons were enrolled to participate in the project. 8 participants did not finish the training period. Characteristics and reasons for training interruption are summarized in Fig. 1. Besides orthopedic problems in one person, all other reasons were regarded not to be related to the training.
Fig. 1.
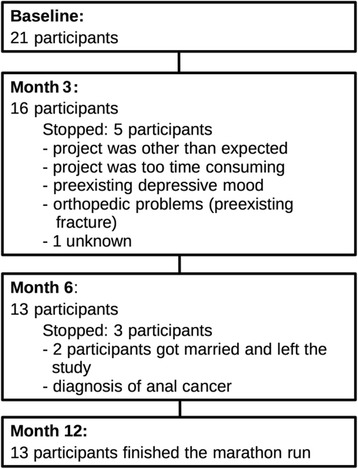
Characteristics of participants and reasons for training interruption
The remaining 13 participants competed in the marathon run. All following data refer to these 13 participants with complete follow-up available.
Baseline characteristics
Baseline characteristics of the 13 participants before training initiation are summarized in Table 1 (HIV-characteristics) and Table 2 (vital parameters and laboratory results).
Table 1.
Baseline HIV-associated characteristics of 13 HIV-positive participants and 12 HIV-positive persons of the reference group
| Parameter | Participants (n = 13) |
Reference group (n = 12) |
|---|---|---|
| Sex | Male = 12 Female = 1 |
Male = 11 Female = 1 |
| Age (years) | 42 [27–50] | 46.5 [26–57] |
| CD4 (/μl) | 620 [146–1268] | 571 [230–955] |
| CD4-Nadir (/μl) | 230 [23–732] | 315 [120–612] |
| AIDS diagnosis in history? | In 3 patients | In 1 patient |
| On ART? | Yes = 11 (6 NNRTI-based, 5 PI-based)No = 2 | Yes = 6 (2 NNRTI-based, 4 PI-based)No = 6 |
| In those on ART: Duration of ART (years) | 3.5 [1–7] | 4 [2–7] |
| HIV-RNA < 40 cop/ml | 9/11One participant had a blip at baselineOne participant most likely had compliance problems | 6/6 |
| Comorbidity | 2 chronic hepatitis 2 depression 1 psoriasis (dermal; no arthritis) |
1 chronic hepatitis 2 depression |
Table 2.
Baseline vital parameters and laboratory results of 13 HIV-positive participants and 12 HIV-positive persons of the Reference group
| Parameter | Participants (Baseline) | Reference Group | p (Participants vs. Reference group) |
|---|---|---|---|
| CD4-count (/μl) | 620 [146–1268] | 571 [230–955] | 0.81 |
| Annexin-binding (% of CD4+ cells) | 53 [47–64] | 51 [46–52] | 0.12 |
| Sodium (mmol/l) | 139 [136–142] | 139 [132–141] | 0.58 |
| Phosphate (mmol/l) | 1.06 [0.86–1.20] | 0.91 [0.66–1.19] | 0.03 |
| Weight (kg) | 78 [58–100] | 77 [59–88] | 0.44 |
| Height (cm) | 174 [158–182] | 179 [168–185] | |
| RRsys (mmHg) | 125 [100–145] | 115 [100–130] | 0.06 |
| RRdia (mmHg) | 80 [70–90] | 70 [60–90] | 0.08 |
| Leukocytes (G/l) | 6.1 [4.1–9.5] | 6.3 [3.8–10.6] | 0.80 |
| Hemoglobin (g/dl) | 15.9 [11.3–17.3] | 14.6 [12.9–16.2] | 0.38 |
| Thrombocytes (G/l) | 225 [171–294] | 255 [147–342] | 0.50 |
| INR | 1 [0.9–1.2] | 1 [0.9–1.1] | 0.06 |
| Potassium (mmol/l) | 3.9 [3.6–4.5] | 4.3 [4.0–4.9] | 0.001 |
| Creatinine (mg/dl) | 1.05 [0.8–1.17] | 0.96 [0.74–1.16] | 0.31 |
| Triglycerides (mg/dl) | 156 [85–328] | 141 [67–326] | 0.95 |
| Cholesterol (mg/dl) | 185 [98–250] | 177 [111–302] | 0.98 |
| HDL-cholesterol (mg/dl) | 48 [31–60] | 40 [28–54] | 0.28 |
| LDL-cholesterol (mg/dl) | 115 [45–161] | 111 [61–198] | 0.81 |
| Insulin (mIU/l) | 4.4 [2.1–9.5] | 6 [2–35] | 0.15 |
| Glucose (mg/dl) | 86 [78–107] | 91 [83–100] | 0.17 |
| Bilirubin (mg/dl) | 0.56 [0.28–2.90] | 0.47 [0.26–2.90] | 0.70 |
| ALT (U/l) | 25 [10–126] | 23 [10–53] | 0.42 |
| Creatine kinase (U/l) | 105 [66–145] | 86 [55–155] | 0.64 |
The following parameters were in the normal range at baseline: leukocytes, hemoglobin, thrombocytes, international-normalized-ratio (INR), sodium, potassium, phosphate, creatinine, triglycerides, cholesterol, HDL-cholesterol, LDL-cholesterol, glucose, insulin, bilirubin, ALT, creatine kinase. No abnormalities were found in the urine dipstick analysis. Blood pressure was normal in all subjects (125 over 80). One patient was treated with an ACE-inhibitor due to moderate hypertension that was controlled under treatment. 11 participants were on ART while training period. 6 took a NNRTI-based therapy and 5 a PI-based regimen.
Reference group
Laboratory parameters and vital parameters of the Reference group were assessed only at baseline to confirm, that the training group represents a representative sample of HIV-infected persons (Table 1). Longitudinal data were only assessed in the training group. At baseline, the following parameters showed no pathologic abnormalities: leukocytes, hemoglobin, thrombocytes, international-normalized-ratio (INR), sodium, potassium, phosphate, creatinine, triglycerides, cholesterol, HDL-cholesterol, LDL-cholesterol, glucose, insulin, bilirubin, ALT, creatine kinase. The average blood pressure was 115 over 70. One patient, suffering from hypertension, was treated with bisoprolol. As expected, there were no significant differences of the participants to the Reference group beside phosphate and potassium, which were in the normal range (Table 2).
6 persons of the Reference group did not take ART during the observation period. 4 were treatment naive, as they did not fulfill criteria for ART-initiation according to former treatment guidelines. However, all 4 started treatment in the longer follow-up. 1 patient had stopped ART due to toxicity and resumed ART 5 months after the study. 1 patient was regarded long-term non-progressor. He was lost to follow up thereafter.
Effects of training
In general, training in the finisher group was tolerated without major complications. During the first few months during the winter period there were few infections of the upper airways. One patient was treated for kidney stones in month 10 of the training. However, he could resume the training and finish the marathon run. This patient was on atazanavir. No other adverse events were observed during the exercise period.
Investigating the potential effects of endurance training on key parameters of HIV infection we observed a significant increase in CD4-T cell counts following training initiation, while viral loads remained undetectable in fully suppressed individuals (Table 3). Interestingly, increasing CD4-T cell numbers were associated with a decline in the frequency of Annexin V+ CD4-T-cells, indicating reduced apoptosis-associated cell death as an underlying mechanism for the improved CD4-T-cell numbers.
Table 3.
Changes in clinical and laboratory parameters throughout the training period
| Parameter | Baseline | Month 3 | Month 6 | Month 12 | p (Baseline vs. Month 12) |
|---|---|---|---|---|---|
| CD4-count (/μl) | 620 [146–1268] | 649 [198–1429] | 791 [192–1419] | 745 [207–1647] | 0.001 |
| Annexin-binding (% of CD4+ cells) | 53 [47–64] | 50 [37–60] | 48 [25–57] | 32 [14–42] | 0.001 |
| HIV-RNA (below <40 cop/ml) | 10/11 | 10/11 | 10/11 | 10/11 | |
| Sodium (mmol/l) | 139 [136–142] | 139 [137–141] | 139 [136–142] | 137 [135–139] | 0.003 |
| Phosphate (mmol/l) | 1.06 [0.86–1.20] | 1.13 [0.67–1.37] | 1.12 [0.87–1.53] | 1.19 [0.99–1.44] | 0.02 |
| Weight (kg) | 78 [58–100] | 77 [58–99] | 78 [58–97] | 77 [58–91.9] | 0.01 |
| RRsys (mmHg) | 125 [100–145] | 110 [110–140] | 120 [110–140] | 120 [100–140] | 0.02 |
| RRdia (mmHg) | 80 [70–90] | 80 [70–90] | 80 [60–90] | 80 [60–90] | 0.04 |
| Leukocytes (G/l) | 6.1 [4.1–9.5] | 5.0 [3.3–8.8] | 5.7 [3.9–13.3] | 5.5 [4.3–8.5] | 0.37 |
| Hemoglobin (g/dl) | 15.9 [11.3–17.3] | 15.4 [10.2–16.8] | 15.6 [9.7–17.5] | 14.8 [12.4–17.2] | 0.15 |
| Thrombocytes (G/l) | 225 [171–294] | 224 [164–325] | 222 [134–338] | 208 [160–316] | 0.13 |
| INR | 1 [0.9–1.2] | 1 [0.9–1.1] | 1 [0.9–1.2] | 1 [1–1.2] | 0.27 |
| Potassium (mmol/l) | 3.9 [3.6–4.5] | 4.4 [4.1–5.2] | 4.0 [3.5–4.8] | 3.9 [3.6–4.5] | 0.31 |
| Creatinine (mg/dl) | 1.05 [0.8–1.17] | 0.95 [0.66–1.17] | 1.06 [0.68–1.23] | 1.03 [0.79–1.16] | 0.47 |
| Triglycerides (mg/dl) | 156 [85–328] | 111 [84–224] | 167 [83–306] | 140 [82–262] | 0.52 |
| Cholesterol (mg/dl) | 185 [98–250] | 174 [131–227] | 179 [117–214] | 167 [106–222] | 0.02 |
| HDL-cholesterol (mg/dl) | 48 [31–60] | 42 [30–63] | 39 [24–65] | 39 [30–66] | 0.41 |
| LDL-cholesterol (mg/dl) | 115 [45–161] | 111 [73–160] | 114 [61–154] | 111 [55–141] | 0.34 |
| Insulin (mIU/l) | 4.4 [2.1–9.5] | 3.8 [2–15.7] | 5.4 [2–16.8] | 10 [2–18.8] | 0.006 |
| Glucose (mg/dl) | 86 [78–107] | 90 [79–109] | 88 [62–114] | 89 [70–109] | 0.88 |
| Bilirubin (mg/dl) | 0.56 [0.28–2.90] | 0.44 [0.24–2.94] | 0.40 [0.19–2.23] | 0.35 [0.20–1.63] | 0.10 |
| ALT (U/l) | 25 [10–126] | 25 [10–70] | 23 [7–57] | 21 [10–40] | 0.11 |
| Creatine kinase (U/l) | 105 [66–145] | 117 [84–192] | 116 [50–240] | 96 [62–226] | 0.90 |
To convert to SI-units: bilirubin mg/dl × 17.104 = μmol/l; cholesterol mg/dl × 0.0259 = mmol/l; creatinine mg/dl × 88.4 = μmol/l; glucose mg/dl × 0.05551 = mmol/l; hemoglobin g/dl × 0.6206 = mmol/l; insulin mIU/l × 7.2141 pmol/l; phosphate mmol/l × 3.0974 = mg/dl; triglycerides mg/dl × 0.0114 = mmol/l
A significant decrease in fasting cholesterol as well as systolic and diastolic blood pressure was observed. However, it has to be emphasized that all parameters were already in the normal range at baseline.
Overall, no significant change in quality of life was observed. All scales analyzed of the MOS-HIV showed no significant change (Table 4).
Table 4.
Changes in parameters of the MOS-HIV
| Parameter | Baseline | Month 3 | Month 6 | Month 12 | p (Baseline vs. Month 12) |
|---|---|---|---|---|---|
| Physical Health Summary Score | 58 [44–62] | 59 [32–62] | 59 [38–63] | 56 [21–73] | 0.26 |
| Mental Health Summary Score | 53 [38–61] | 55 [35–66] | 57 [29–64] | 56 [23–68] | 0.99 |
| General Health Perception | 70 [15–100] | 70 [15–100] | 80 [15–100] | 75 [15–100] | 0.94 |
| Physical Functioning | 100 [83–100] | 100 [83–100] | 100 [58–100] | 100 [17–100] | 0.21 |
For calculation and interpretation of scores please refer to [25].
There were no differences in the other scores provided by the MOS-HIV: pain, role functioning, social functioning, energy/fatigue, mental health, health distress, cognitive functioning, quality of life, health transition (data not shown).
Discussion
Regular physical activity is beneficial for HIV-infected patients, as for any human being. The intensity, frequency, and parameters of exercise for the population with HIV/AIDS have yet to be determined.
The main finding of our study was that regular aerobic activity resulting in performing a marathon was safe for people living with HIV. We could not show any potential harm, or increase of infections such as URTIs. Withdrawals from the study did not occur due to major health issues. There were no unfavorable effects on immunological and virological parameters.
In contrast we observed a significant increase in CD4 cell count by 20% (p = 0.001). Comparison to other studies is limited due to a vast variety of training schedules, duration and intensity. There might be an effect of the intensity of exercise: a meta-analysis of 14 studies in HIV-infected patients from 1990 to 2008 showed no difference in the CD4 cell count in the constant aerobic exercise group as well as in the moderate exercise group [26]. But there was a significant trend towards increase in CD4 cell count in the interval aerobic group, consisting of the data of two studies [9, 13].
Besides intensity another explanation of the differing results may be the compliance to training schedules, which is directly related to training frequency. This issue was further investigated by a study with evaluation of the compliance during training period [9]. A significant increase in CD4 cell count was shown in the compliant exercise group only while in the non-compliant exercise group a decrease was found. A more recent study on 10 participants with a combined training (resistance exercises plus aerobic training) over a period of 20 weeks showed an increase in CD4 cell count by 31%, but limitation of this study was the lack of a control group [27]. It is extremely difficult to adequately measure training-intensity of the participants. We tried to assess training intensity via self-reported diaries and log-files of GPS-watches in this study. However, data were not complete (mostly for technical reasons such as not activating log-files) and accurate enough to perform further detailed analyses.
The increase in CD4 counts in our study may be an effect of the longer training period compared to most studies also. We did not see a significant change in CD4 cell count after 3 months, but after 6 and 12 months. The training period of our project over one year is one of the longest being published so far. Most of the studies performed supervised exercise over a period of 12 weeks (7 of 10 studies in a recent meta-analysis [26]). Studies beyond this training period lasted for up to 24 weeks [8, 28, 29]. However, the studies with longest observation periods published by [8, 29] showed no effect on CD4 cell count. Studies on the immunological effects of aerobic training on the CD4/CD8 ratio in HIV-negative people showed conflicting results as well. Several studies observed no change [30, 31], while others found a positive alteration of CD4/CD8 ratio [32].
Interestingly, we observed a decrease of Annexin-V-binding lymphocytes in parallel to the increase in CD4 counts. A possible interplay between apoptosis and CD4+ cells was observed in numerous studies in non-HIV-infected athletes. During strenuous activities there may be changes in numbers of CD4+ cells (e.g. decrease of mainly Th1 cells but not Th2 cells) [15, 33], proliferation (decreased lymphocyte proliferation during and after exercise), probably due to an increase in apoptotic cells [34], and function of T-cells [35].
In our study the percentage of apoptotic cells was decreased after this long-term exercise. It is well-known, that following acute bouts of exhaustive exercise (> 75% VO2max) numbers of lymphocytes decrease and apoptotic cells increase [36–38]. However, long-term effects on apoptosis have not been reported. In addition, it remains unclear whether apoptosis is the main cause of lymphocyte dynamics related to exercise. It appears to be too small in number to be completely responsible for lymphocytopenia after exercise [18, 39, 40].
Going further, the effect of ART has to be considered. Some of the participants were on ART for just one year, therefore improvement of immunological status during the study period of one year is reasonable. Interestingly, few of the first studies on the effect of exercise in HIV-infection were performed before introduction of effective ART. Some studies showed an increase in CD4 cell count [41], whereas others did not [42, 43].
In summary, our data support a beneficial effect on the CD4 cell count, but study design and number of participants do not allow quantifying the direct effect of exercise on the lymphocytes and the underlying mechanism.
In general, moderate aerobic exercise has beneficial effects on metabolic parameters such as lipid profile and insulin. We found total cholesterol reduced at the end of the training period. It has to be emphasized, that cholesterol levels were already in the normal range in most patients at the beginning of the training period. Therefore, further considerations on effects have to be interpreted with caution. Nevertheless, positive results are in line with several studies on blood pressure, body fat mass and lipid profile of people living with HIV/AIDS [44, 45], where several beneficial effects such as an increase in HDL [27], a significant reduction in total adipose tissue (TAT), in cholesterol and triglycerides and an increase in HDL could be documented [46].
Noteworthy we found a significant increase in insulin-levels, while glucose levels were not changed significantly. Homeostasis Model Assessment of insulin resistance (HOMA-IR) index, calculated according to [47] increased within the training period from normal range to approximately >2 in some patients. This is surprising since moderate exercise has a beneficial effect on insulin resistance and glucose homeostasis control in diabetes patients [48] and HIV patients also [46]. The explanation for this finding remains unclear: Nine of those who finished marathon showed increasing insulinemia during the study period. Yet, none of the participants in our study had a history of diabetes or developed diabetes. 5 patients were on a PI-based regimen, and 3 of these patients had the greatest increase in insulin resistance of all patients on ART. The average increase in HOMA-index was two times higher compared to the patients on a NNRTI-based regimen. PI-based regimen have been shown to increase the risk of hyperglycemia by fivefold [49]. Two participants with decreasing dynamic of the HOMA-index (one over the complete study period) took a nevirapine containing regimen, that might have a favourable effect on insulin resistance [50]. One patient on a NNRTI based regimen remained stable with insulin resistance. The two HIV-positive patients without ART showed the greatest increase in insulin resistance.
Another finding was a significant increase in phosphate concentration. Tenofovir as part of many ART-combinations enhances phosphate excretion and has been associated with reduced serum phosphate levels [51, 52], but hypophosphatemia has a multifactorial genesis in HIV-positive patients and several analysis did not find a significant effect of tenofovir on the phosphate level [53, 54]. An increase of phosphate levels might indicate a partial reversal of this phenomenon. On the other hand, it might reflect increased cell turn-over due to exercise. It is not possible to conclude on any clinical significant effect.
Nevertheless, all changes in biological and metabolic parameters observed show – if relevant at all - an assumably positive effect.
We found no effect on the quality of life or mental health tests as assessed by MOS-HIV. Beneficial effects of exercise on these parameters have been described widely, but we have to assume that our quite small number of participants started training in a stable state of HIV-disease and state of quality of life. Possibly due to this fact, we could not document any relevant effect. However, we did not see any worsening of life quality of life in the MOS-HIV.
Limitations of our study are the lack of complete acquisition of cardiovascular parameters and training intensity, small number of participants, lack of control group, high drop out rate and difficulties in assessing outcome parameters as infections. It has to be emphasized that all HIV-infected participants were non-professionals, who lived their normal lives and contributed to this study in leisure time. Therefore, assessment could take place only during four time points, when participants met. In between, no reliable documentation other than self-reporting was possible. This is known to be highly variable. Especially severity and frequency of infections may be subject to personal variations. The overall drop out rate in our study was high with 38%. However, in most cases reasons were not related to illness but rather lack of time, marriage or feeling contrary to expectations of the project. Medical reasons for dropping out included pre-existing depression, an undiagnosed, most likely pre-existing metatarsal fracture and diagnosis of anal cancer and therefore probably only one health issue related to HIV. Noteworthy, all withdrawals took place in the first 6 months. Such a high drop out rate is a constant problem. It was estimated at the range from 3% [29] to 76% [8]. Nearly half of studies reviewed in a meta-analysis lost one third of participants [26]. However, high drop out rates in other study populations, such as non-HIV populations, are not unusual, especially in long-term studies (e.g. [55, 56]). This does not reduce the results of the study. Before the study we had a substantial discussion about the study design and about a control group. As the study mainly was designed to rule out negative effects of exercise rather than to detect CD4 dynamics, we decided to perform the study without a control group for two main reasons. Firstly, we would have needed a control group with a sedentary behaviour, which remained stable over the study period. Experience shows that the members of such a control group change behavior also, as they are enrolled in a study. Therefore, the reliability of such a study would have been substantially limited. Secondly, studies comparing of small-scale effects on lymphocyte dynamics would have required a much greater number of participants to adequately power the study. However, studies on effects of exercise on CD4 cell count have been carried out in pre-ART-era with varying results. Therefore we only expected small effects, if any. In the era of ART we had to rule out effects of a particular ART between the groups, which would have been impossible in such a setting with small numbers of participants. As efforts and costs for realization of this pilot-project were enormous and exceeded common clinical settings by far, the project targeted at 20 participants. More participants would have made this kind of project very difficult.
Conclusions
In summary, HIV-infected persons can perform moderate endurance training. No clear safety issues were found in this “healthy” study population. These data pushed the safety limit of exercise in a specific group of people living with HIV/AIDS to the distance of a marathon run. In this small pilot study an increase in CD4-T-cells was observed, although it is not possible to conclude, whether this is a direct effect of training or due to ART. In a long-term perspective effects of endurance training on typical HIV-associated risks such as cardiovascular diseases would be desirable.
Acknowledgements
The authors thank all participants who contributed to this unusual project with unrestricted motivation. This work would have not been possible by the help of study nurses Angelika Engelhardt, Karina Mohrmann, Brigitta Späth, and colleagues who contributed to drawing the blood samples Jetske Emmelkamp.
The marathon-project was initiated and financed by Abbott Pharmaceuticals, Wiesbaden (now Abbvie). As mentioned in the manuscript, there was no influence on the design, collection and analysis of the scientific part at all.
Christian Körner was funded by the German Federal Ministry of Education and Research (BMBF) [grant number 01KI0792].
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. It was approved by the Ethical Comittee of the University of Bonn.
Informed consent and consent to publish was obtained from all individual participants included in the study.
Trial registration: DRKS00011592 (retrospectively registered on February 9th 2017).
Funding
Costs of laboratory analyses were funded by Abbvie.
C.K. was funded by the German Federal Ministry of Education and Research (BMBF) [grant number 01KI0792].
Availability of data and materials
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ART
anti-retroviral therapy
- HIV
human immunodeficiency virus
- HOMA-IR
Homeostasis Model Assessment of insulin resistance
- MOS-HIV
Medical Outcomes Study HIV Health Survey
- NNRTI
non-nucleoside reverse transferase inhibitor
- PI
protease inhibitor
- URTI
upper respiratory tract infections
Authors’ contributions
JKR and JCW. initiated the study and supervised the data collection. MV, KB and JCW were responsible for study design and organization. MV, CK, CB, CSZ and JCW. were involved in the sample collection and examination of the participants. Primary data were compiled and processed by CB and CSZ The analysis of the MOS-HIV data was done by CB and CSZ Flow cytometry was done by CK, CSZ, CB, SS, JCW, KB and JKR made the analysis and interpretation of the data. The draft was written by JCW and SS and it was critically revised by all co-authors. All authors read and approved the final manuscript.
Consent for publication
Consent for publication of collected data was obtained during inclusion of study participants. Informed consent included data analysis and publication in anonymous manner.
Informed Consent for publication of individual information, videos and images enabling identifying these individuals: not applicable.
Competing interests
J.K.R. has received honoraria for consulting or speaking at educational events from Abbott, Abbvie, BMS, Bionor, Cipla, Gilead, Janssen, Merck and ViiV. J.C.W received honoraria for speaking at symposia and advisory boards from Abbvie, MSD and Janssen. C.S.Z. received honoraria for lectures and advisory boards from Abbvie, MSD, Janssen, BMS, Hexal and ViiV. C.K. was funded by the German Federal Ministry of Education and Research (BMBF) [grant number 01KI0792]. M.V. is employee of Janssen-Cilag GmbH, pharmaceutical company of Johnson & Johnson. C.B., K.B. and S.S. declare that they have no potential conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nakagawa F, May M, Phillips A. Life expectancy living with HIV: recent estimates and future implications. Curr Opin Infect Dis. 2013;26:17–25. doi: 10.1097/QCO.0b013e32835ba6b1. [DOI] [PubMed] [Google Scholar]
- 2.Tseng A, Seet J, Phillips EJ. The evolution of three decades of antiretroviral therapy: challenges, triumphs and the promise of the future. Br J Clin Pharmacol. 2015;79:182–194. doi: 10.1111/bcp.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castel AD, Magnus M, Greenberg AE. Pre-exposure prophylaxis for human immunodeficiency virus: the past, present, and future. Infect Dis Clin N Am. 2014;28:563–583. doi: 10.1016/j.idc.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports. 2006;16(Suppl 1):3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 5.Gill JM, Cooper AR. Physical activity and prevention of type 2 diabetes mellitus. Sports Med. 2008;38:807–824. doi: 10.2165/00007256-200838100-00002. [DOI] [PubMed] [Google Scholar]
- 6.Wolin KY, Yan Y, Colditz GA. Physical activity and risk of colon adenoma: a meta-analysis. Br J Cancer. 2011;104:882–885. doi: 10.1038/sj.bjc.6606045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovitch H. Walking and dementia in physically capable elderly men. JAMA. 2004;292:1447–1453. doi: 10.1001/jama.292.12.1447. [DOI] [PubMed] [Google Scholar]
- 8.MacArthur RD, Levine SD, Birk TJ. Supervised exercise training improves cardiopulmonary fitness in HIV-infected persons. Med Sci Sports Exerc. 1993;25:684–688. doi: 10.1249/00005768-199306000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Perna FM, LaPerriere A, Klimas N, Ironson G, Perry A, Pavone J, Goldstein A, Majors P, Makemson D, Talutto C, et al. Cardiopulmonary and CD4 cell changes in response to exercise training in early symptomatic HIV infection. Med Sci Sports Exerc. 1999;31:973–979. doi: 10.1097/00005768-199907000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Arey BD, Beal MW. The role of exercise in the prevention and treatment of wasting in acquired immune deficiency syndrome. J Assoc Nurses AIDS Care. 2002;13:29–49. doi: 10.1016/S1055-3290(06)60239-2. [DOI] [PubMed] [Google Scholar]
- 11.Terry L, Sprinz E, Stein R, Medeiros NB, Oliveira J, Ribeiro JP. Exercise training in HIV-1-infected individuals with dyslipidemia and lipodystrophy. Med Sci Sports Exerc. 2006;38:411–417. doi: 10.1249/01.mss.0000191347.73848.80. [DOI] [PubMed] [Google Scholar]
- 12.Lindegaard B, Hansen T, Hvid T, van Hall G, Plomgaard P, Ditlevsen S, Gerstoft J, Pedersen BK. The effect of strength and endurance training on insulin sensitivity and fat distribution in human immunodeficiency virus-infected patients with lipodystrophy. J Clin Endocrinol Metab. 2008;93:3860–3869. doi: 10.1210/jc.2007-2733. [DOI] [PubMed] [Google Scholar]
- 13.LaPerriere AR, Antoni MH, Schneiderman N, Ironson G, Klimas N, Caralis P, Fletcher MA. Exercise intervention attenuates emotional distress and natural killer cell decrements following notification of positive serologic status for HIV-1. Biofeedback Self Regul. 1990;15:229–242. doi: 10.1007/BF01011107. [DOI] [PubMed] [Google Scholar]
- 14.Fazeli PL, Woods SP, Heaton RK, Umlauf A, Gouaux B, Rosario D, Moore RC, Grant I, Moore DJ. An active lifestyle is associated with better neurocognitive functioning in adults living with HIV infection. J Neuro-Oncol. 2014;20:233–242. doi: 10.1007/s13365-014-0240-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tvede N, Kappel M, Halkjaer-Kristensen J, Galbo H, Pedersen BK. The effect of light, moderate and severe bicycle exercise on lymphocyte subsets, natural and lymphokine activated killer cells, lymphocyte proliferative response and interleukin 2 production. Int J Sports Med. 1993;14:275–282. doi: 10.1055/s-2007-1021177. [DOI] [PubMed] [Google Scholar]
- 16.Moyna NM, Acker GR, Fulton JR, Weber K, Goss FL, Robertson RJ, Tollerud DJ, Rabin BS. Lymphocyte function and cytokine production during incremental exercise in active and sedentary males and females. Int J Sports Med. 1996;17:585–591. doi: 10.1055/s-2007-972899. [DOI] [PubMed] [Google Scholar]
- 17.Robson PJ, Blannin AK, Walsh NP, Castell LM, Gleeson M. Effects of exercise intensity, duration and recovery on in vitro neutrophil function in male athletes. Int J Sports Med. 1999;20:128–135. doi: 10.1055/s-2007-971106. [DOI] [PubMed] [Google Scholar]
- 18.Simpson RJ, Florida-James GD, Cosgrove C, Whyte GP, Macrae S, Pircher H, Guy K. High-intensity exercise elicits the mobilization of senescent T lymphocytes into the peripheral blood compartment in human subjects. J Appl Physiol (1985) 2007;103:396–401. doi: 10.1152/japplphysiol.00007.2007. [DOI] [PubMed] [Google Scholar]
- 19.Gavrieli R, Ashlagi-Amiri T, Eliakim A, Nemet D, Zigel L, Berger-Achituv S, Falk B, Wolach B. The effect of aerobic exercise on neutrophil functions. Med Sci Sports Exerc. 2008;40:1623–1628. doi: 10.1249/MSS.0b013e318176b963. [DOI] [PubMed] [Google Scholar]
- 20.Bishop NC, Gleeson M. Acute and chronic effects of exercise on markers of mucosal immunity. Front Biosci (Landmark Ed) 2009;14:4444–4456. doi: 10.2741/3540. [DOI] [PubMed] [Google Scholar]
- 21.Kappel M, Tvede N, Galbo H, Haahr PM, Kjaer M, Linstow M, Klarlund K, Pedersen BK. Evidence that the effect of physical exercise on NK cell activity is mediated by epinephrine. J Appl Physiol (1985) 1991;70:2530–2534. doi: 10.1152/jappl.1991.70.6.2530. [DOI] [PubMed] [Google Scholar]
- 22.Peters EM, Bateman ED. Ultramarathon running and upper respiratory tract infections. An epidemiological survey. S Afr Med J. 1983;64:582–584. [PubMed] [Google Scholar]
- 23.Nieman DC, Johanssen LM, Lee JW, Arabatzis K. Infectious episodes in runners before and after the Los Angeles Marathon. J Sports Med Phys Fitness. 1990;30:316–328. [PubMed] [Google Scholar]
- 24.Nieman DC, Henson DA, Austin MD, Sha W. Upper respiratory tract infection is reduced in physically fit and active adults. Br J Sports Med. 2011;45:987–992. doi: 10.1136/bjsm.2010.077875. [DOI] [PubMed] [Google Scholar]
- 25.Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the medical outcomes study HIV health survey (MOS-HIV) Qual Life Res. 1997;6:481–493. doi: 10.1023/A:1018451930750. [DOI] [PubMed] [Google Scholar]
- 26.O'Brien K, Nixon S, Tynan AM, Glazier R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010:s. [DOI] [PMC free article] [PubMed]
- 27.Garcia A, Fraga GA, Vieira RC, Jr, Silva CM, Trombeta JC, Navalta JW, Prestes J, Voltarelli FA. Effects of combined exercise training on immunological, physical and biochemical parameters in individuals with HIV/AIDS. J Sports Sci. 2014;32:785–792. doi: 10.1080/02640414.2013.858177. [DOI] [PubMed] [Google Scholar]
- 28.Baigis J, Korniewicz DM, Chase G, Butz A, Jacobson D, Wu AW. Effectiveness of a home-based exercise intervention for HIV-infected adults: a randomized trial. J Assoc Nurses AIDS Care. 2002;13:33–45. doi: 10.1016/S1055-3290(06)60199-4. [DOI] [PubMed] [Google Scholar]
- 29.Mutimura E, Crowther NJ, Cade TW, Yarasheski KE, Stewart A. Exercise training reduces central adiposity and improves metabolic indices in HAART-treated HIV-positive subjects in Rwanda: a randomized controlled trial. AIDS Res Hum Retrovir. 2008;24:15–23. doi: 10.1089/aid.2007.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapasi ZF, Ouslander JG, Schnelle JF, Kutner M, Fahey JL. Effects of an exercise intervention on immunologic parameters in frail elderly nursing home residents. J Gerontol A Biol Sci Med Sci. 2003;58:636–643. doi: 10.1093/gerona/58.7.M636. [DOI] [PubMed] [Google Scholar]
- 31.Raso V, Benard G, DASD AJ, Natale VM. Effect of resistance training on immunological parameters of healthy elderly women. Med Sci Sports Exerc. 2007;39:2152–2159. doi: 10.1249/mss.0b013e318156e9fa. [DOI] [PubMed] [Google Scholar]
- 32.Shimizu K, Kimura F, Akimoto T, Akama T, Tanabe K, Nishijima T, Kuno S, Kono I. Effect of moderate exercise training on T-helper cell subpopulations in elderly people. Exerc Immunol Rev. 2008;14:24–37. [PubMed] [Google Scholar]
- 33.Steensberg A, Toft AD, Bruunsgaard H, Sandmand M, Halkjaer-Kristensen J, Pedersen BK: Strenuous exercise decreases the percentage of type 1 T cells in the circulation. J Appl Physiol (1985) 2001, 91:1708–1712. [DOI] [PubMed]
- 34.Steensberg A, Morrow J, Toft AD, Bruunsgaard H, Pedersen BK. Prolonged exercise, lymphocyte apoptosis and F2-isoprostanes. Eur J Appl Physiol. 2002;87:38–42. doi: 10.1007/s00421-002-0584-6. [DOI] [PubMed] [Google Scholar]
- 35.Bishop NC, Walker GJ, Gleeson M, Wallace FA, Hewitt CR. Human T lymphocyte migration towards the supernatants of human rhinovirus infected airway epithelial cells: influence of exercise and carbohydrate intake. Exerc Immunol Rev. 2009;15:127–144. [PubMed] [Google Scholar]
- 36.Navalta JW, Sedlock DA, Park KS. Effect of exercise intensity on exercise-induced lymphocyte apoptosis. Int J Sports Med. 2007;28:539–542. doi: 10.1055/s-2006-955898. [DOI] [PubMed] [Google Scholar]
- 37.Navalta JW, Tibana RA, Fedor EA, Vieira A, Prestes J. Three consecutive days of interval runs to exhaustion affects lymphocyte subset apoptosis and migration. Biomed Res Int. 2014;2014:694801. doi: 10.1155/2014/694801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mooren FC, Bloming D, Lechtermann A, Lerch MM, Volker K: Lymphocyte apoptosis after exhaustive and moderate exercise. J Appl Physiol (1985) 2002, 93:147–153. [DOI] [PubMed]
- 39.Simpson RJ, Cosgrove C, Ingram LA, Florida-James GD, Whyte GP, Pircher H, Guy K. Senescent T-lymphocytes are mobilised into the peripheral blood compartment in young and older humans after exhaustive exercise. Brain Behav Immun. 2008;22:544–551. doi: 10.1016/j.bbi.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 40.Turner JE, Aldred S, Witard OC, Drayson MT, Moss PM, Bosch JA. Latent cytomegalovirus infection amplifies CD8 T-lymphocyte mobilisation and egress in response to exercise. Brain Behav Immun. 2010;24:1362–1370. doi: 10.1016/j.bbi.2010.07.239. [DOI] [PubMed] [Google Scholar]
- 41.LaPerriere A, Fletcher MA, Antoni MH, Klimas NG, Ironson G, Schneiderman N. Aerobic exercise training in an AIDS risk group. Int J Sports Med. 1991;12(Suppl 1):S53–S57. doi: 10.1055/s-2007-1024751. [DOI] [PubMed] [Google Scholar]
- 42.Rigsby LW, Dishman RK, Jackson AW, Maclean GS, Raven PB. Effects of exercise training on men seropositive for the human immunodeficiency virus-1. Med Sci Sports Exerc. 1992;24:6–12. [PubMed] [Google Scholar]
- 43.Ullum H, Palmo J, Halkjaer-Kristensen J, Diamant M, Klokker M, Kruuse A, LaPerriere A, Pedersen BK. The effect of acute exercise on lymphocyte subsets, natural killer cells, proliferative responses, and cytokines in HIV-seropositive persons. J Acquir Immune Defic Syndr. 1994;7:1122–1133. [PubMed] [Google Scholar]
- 44.Dolan SE, Frontera W, Librizzi J, Ljungquist K, Juan S, Dorman R, Cole ME, Kanter JR, Grinspoon S. Effects of a supervised home-based aerobic and progressive resistance training regimen in women infected with human immunodeficiency virus: a randomized trial. Arch Intern Med. 2006;166:1225–1231. doi: 10.1001/archinte.166.11.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Driscoll SD, Meininger GE, Lareau MT, Dolan SE, Killilea KM, Hadigan CM, Lloyd-Jones DM, Klibanski A, Frontera WR, Grinspoon SK. Effects of exercise training and metformin on body composition and cardiovascular indices in HIV-infected patients. AIDS. 2004;18:465–473. doi: 10.1097/00002030-200402200-00013. [DOI] [PubMed] [Google Scholar]
- 46.Thoni GJ, Fedou C, Brun JF, Fabre J, Renard E, Reynes J, Varray A, Mercier J. Reduction of fat accumulation and lipid disorders by individualized light aerobic training in human immunodeficiency virus infected patients with lipodystrophy and/or dyslipidemia. Diabetes Metab. 2002;28:397–404. [PubMed] [Google Scholar]
- 47.Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2192. doi: 10.2337/diacare.21.12.2191. [DOI] [PubMed] [Google Scholar]
- 48.Shaban N, Kenno KA, Milne KJ. The effects of a 2 week modified high intensity interval training program on the homeostatic model of insulin resistance (HOMA-IR) in adults with type 2 diabetes. J Sports Med Phys Fitness. 2014;54:203–209. [PubMed] [Google Scholar]
- 49.Tsiodras S, Mantzoros C, Hammer S, Samore M. Effects of protease inhibitors on hyperglycemia, hyperlipidemia, and lipodystrophy: a 5-year cohort study. Arch Intern Med. 2000;160:2050–2056. doi: 10.1001/archinte.160.13.2050. [DOI] [PubMed] [Google Scholar]
- 50.Martinez E, Conget I, Lozano L, Casamitjana R, Gatell JM. Reversion of metabolic abnormalities after switching from HIV-1 protease inhibitors to nevirapine. AIDS. 1999;13:805–810. doi: 10.1097/00002030-199905070-00009. [DOI] [PubMed] [Google Scholar]
- 51.Woodward CL, Hall AM, Williams IG, Madge S, Copas A, Nair D, Edwards SG, Johnson MA, Connolly JO. Tenofovir-associated renal and bone toxicity. HIV Med. 2009;10:482–487. doi: 10.1111/j.1468-1293.2009.00716.x. [DOI] [PubMed] [Google Scholar]
- 52.Cheng CY, Chang SY, Lin MH, Ku SY, Sun NL, Cheng SH. Tenofovir disoproxil fumarate-associated hypophosphatemia as determined by fractional excretion of filtered phosphate in HIV-infected patients. J Infect Chemother. 2016;22:744–747. doi: 10.1016/j.jiac.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 53.Cooper RD, Wiebe N, Smith N, Keiser P, Naicker S, Tonelli M. Systematic review and meta-analysis: renal safety of tenofovir disoproxil fumarate in HIV-infected patients. Clin Infect Dis. 2010;51:496–505. doi: 10.1086/655681. [DOI] [PubMed] [Google Scholar]
- 54.Badiou S, De Boever CM, Terrier N, Baillat V, Cristol JP, Reynes J. Is tenofovir involved in hypophosphatemia and decrease of tubular phosphate reabsorption in HIV-positive adults? J Inf Secur. 2006;52:335–338. doi: 10.1016/j.jinf.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 55.Saida T, Juul Sorensen T, Langberg H. Long-term exercise adherence after public health training in at-risk adults. Ann Phys Rehabil Med. 2017; [DOI] [PubMed]
- 56.Sponder M, Campean IA, Emich M, Fritzer-Szekeres M, Litschauer B, Bergler-Klein J, Graf S, Strametz-Juranek J. Long-term endurance training increases serum cathepsin S and decreases IL-6 and hsCRP levels. J Sports Sci. 2016:1–6. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
The project was initiated, organized and sponsored by Abbott Pharmaceuticals (Wiesbaden, Germany; now Abbvie). However, the sponsor had no influence on scientific design and no access to results until completion of the project.
The study was approved by the Ethics committee of the University of Bonn (sequential number 138/09), which is in accordance with the provisions of the Declaration of Helsinki. Informed consent was given by all participants.
The datasets used and analysed during the current study available from the corresponding author on reasonable request.


