Abstract
Background
The independent prognostic role of squamous differentiation in pT1 bladder urothelial carcinoma has not been reported in previous studies. This article describes the impact of squamous differentiation on tumor recurrence and survival, and whether this histologic variant could indeed alter definitive treatment, based on single center-based retrospective data.
Methods
Totally, we retrieved (1)1449 histologically confirmed pT1 bladder urothelial carcinoma patients without histologic variants; (2)227 pT1 bladder urothelial carcinoma patients with squamous differentiation in our institution, from May 2004 to Oct 2015. The total amount of high/low grade urothelial carcinoma patients was 991/685 respectively. Transurethral resection of bladder tumor (TURBT) and intravesical chemotherapy were performed as initial treatments for all the patients. The clinical and pathological characteristics, treatment and survival outcomes were compared between squamous differentiation-positive and squamous differentiation-negative patients.
Results
In our study, 14% urothelial carcinoma patients were detected with squamous differentiation. The mean age of all the patients examined was 66.4, of whom 82% were males. The 5-year cancer specific survival rates were 69% for squamous differentiation-positive patients and 91% for squamous differentiation-negative patients (p < 0.001). Recurrence proved to be more common in squamous differentiation-positive patients than in negative patients. In the results of the univariate and multivariate Cox proportional hazard analysis, tumor size, lymphovascular invasion, recurrence and squamous differentiation were confirmed to be the prognostic factors associated with patients’ survival.
Conclusions
Squamous differentiation in pT1 bladder urothelial carcinoma is correlated to high risk of recurrence and poor prognosis as an independent prognostic factor. Radical cystectomy is essential for recurred high grade pT1 bladder urothelial carcinoma with squamous differentiation accompanied by lymphovascular invasion.
Keywords: Squamous differentiation, Urothelial carcinoma, Transurethral resection of bladder tumor, Radical cystectomy, Recurrence, Bladder cancer
Background
Approximately 380,000 bladder cancer patients are diagnosed and 150,000 patients die annually worldwide [1]. Urothelial carcinoma accounts for the majority of bladder cancers and has a substantial public health impact [2–4]. The morphological diversity of urothelial carcinoma is quite common. Squamous differentiation represents the most common form of mixed differentiation in invasive urothelial carcinoma and tremendous studies reveal that squamous differentiation may represent a precursor to invasive bladder cancer [5]. Squamous differentiation warrants aggressive therapy and may be beneficial for close monitoring [6]. Much attention has been paid to squamous differentiation in invasive bladder cancer [5, 7, 8], however, its significance on pT1 bladder tumor was ignored. Urothelial carcinoma with squamous differentiation is expected to be more aggressive, compared with pure bladder urothelial carcinoma without squamous differentiation. It is hypothesized that similar pathological stage pT1 urothelial carcinoma with squamous differentiation is more aggressive and greatly related to poor prognosis.
Methods
We retrospectively analyzed 1676 bladder urothelial carcinoma patients between May 2004 and Oct 2015 in our institution. The pathologic stage was determined according to the 2009 Union for International Cancer Control (UICC) TNM staging system [9]. Pathologic grading of each tumor was based on the 2004 World Health Organization (WHO) classified system for non-invasive urothelial neoplasia [10]. The medical records and clinical data of the 1676 enrolled patients were reviewed. Patients with a history of previous urothelial carcinoma, other variant morphology, or concomitant upper tract urothelial carcinoma were excluded. TURBT and intravesical chemotherapy with Pirarubicin or camptothecin were performed as initial treatments for all the patients. Subsequent cystoscopy has been suggested to be performed during the postoperative follow-up period based on the European and US guidelines [11]. According to individual histological grade and stage, all recurrent tumors received re-TURBT or radical cystectomy. High grade recurrent tumors were suggested RC and low grade were proposed re-TURBT, however, the choices were based on the patients’ decisions. All of the enrolled patients were divided into two cohorts by squamous differentiation or not, and all patients with tumor recurrence were divided into two cohorts by TURBT and radical cystectomy. Age, gender, tumor grade, tumor multiplicity, tumor size, lymphovascular invasion, recurrence and squamous differentiation were assessed as prognostic factors. To avoid the influence of bladder tumor grade, analyses were also performed in low-grade and high-grade tumors with or without squamous differentiation respectively. Analyses of the prognostic implications of these factors were performed with the cancer specific survival rates. All demographic and pathological variables were queried. Variables were evaluated for inconsistencies and data integrity.
Pathology
All surgical specimens determined by pathologists were submitted en bloc. Each of the pathology slides was evaluated case by case and assembled methodically for the adequate determination of grade and stage. Three representative slides of all the sections from each patient were assigned and re-reviewed independently by at least two pathologists in our institute to identify reported pathologic findings and squamous differentiation status. Presence of squamous differentiation, indicated by keratinization or intercellular bridges, was systematically assessed by hematoxylin and eosin (H&E) staining. The presence of lymphovascular invasion was also recorded using H&E staining. The criteria for confirming characterization of squamous differentiation did not change over the study period.
Statistical methods
The period between the day of surgery and the day of bladder cancer specific death was considered as cancer specific survival. The independent-sample Student’s t-test and chi-square test were used to assess continuous variables and categorical variables, respectively. Overall survival trends and curves were calculated by the Kaplan–Meier method and differences were evaluated using the log-rank test. Univariate and multivariate analyses using the Cox regression models were performed to examine overall survival after operation. A p value of ≤0.05 (two-sided) was considered to indicate a statistically significant difference. All statistical analysis was performed with SPSS 22 statistical software (SPSS, IBM Corporation, Armonk, NY, USA).
Results
Clinical characteristics
Clinical and pathological characteristics were shown in Table 1. Average patient age was 66 years old. In this study, 1376 patients were males and 300 patients were females with a 5:1 male-to-female ratio. Of the 1676 patients, squamous differentiation was determined in 227 (14%) patients. Squamous differentiation was not significantly associated with age (p = 0.150), gender (p = 0.499) and tumor size (p = 0.708). However, high grade tumors with squamous differentiation were more common than high grade tumors without squamous differentiation (66% versus 58%, p = 0.022). The tumor multiplicity rate was significantly different between squamous differentiation-positive patients (115 patients, 51%) and squamous differentiation-negative patients (615 patients, 42%) (p = 0.02). Lymphovascular invasion rate showed a significant difference between the two cohorts, urothelial carcinoma with squamous differentiation revealed an increased occurrence of lymphovascular invasion (67 squamous differentiation-positive patients (30%) versus 121 squamous differentiation-negative patients (8%)) (p < 0.001). Recurrent patients with squamous differentiation was 72 (32%) and recurrent patients without squamous differentiation was 359 (25%) (p = 0.026). As data shown in Table 2, all recurrent patients underwent re-TURBT or radical cystectomy. According to decision of patients and our suggestions, 139 (61%) high grade recurrent patients were received radical cystectomy and 118 (58%) low grade recurrent patients underwent radical cystectomy.
Table 1.
Association of squamous differentiation with clinical and pathological characteristics
| Characteristic | Total | Squamous differentiation-negative | Squamous differentiation-positive | p value | |
|---|---|---|---|---|---|
| Cases, n (%) | 1676 (100) | 1449 (86) | 227 (14) | ||
| Mean age (range),years | 66.4 (24–92) | 66.5 (26–92) | 65.4 (24–90) | 0.150 | |
| Gender, n (%) | M | 1376 (82) | 1186 (82) | 190 (84) | 0.499 |
| F | 300 (18) | 263 (18) | 37 (16) | ||
| M:F | 5:1 | 5:1 | 5:1 | ||
| Tumor grade, n (%) | Low | 685 (41) | 608 (42) | 77 (34) | 0.022 |
| High | 991 (59) | 841 (58) | 150 (66) | ||
| Tumor multiplicity, n (%) | No | 946 (56) | 834 (58) | 112 (49) | 0.02 |
| Yes | 730 (44) | 615 (42) | 115 (51) | ||
| Tumor size (cm), n (%) | <3 | 1089 (65) | 939 (65) | 150 (66) | 0.708 |
| ≥3 | 587 (35) | 510 (35) | 77 (34) | ||
| Lymphovascular invasion, n (%) | No | 1488 (89) | 1328 (92) | 160 (70) | <0.001 |
| Yes | 188 (11) | 121 (8) | 67 (30) | ||
| Recurrence, n (%) | No | 1245 (74) | 1090 (75) | 155 (68) | 0.026 |
| Yes | 431 (26) | 359 (25) | 72 (32) |
M male; F female
Table 2.
The patients of recurrence underwent re-transurethral resection of bladder tumor or radical cystectomy
| Tumor grade | Squamous differentiation-negative | Squamous differentiation-positive | Total | |
|---|---|---|---|---|
| re-TURBT | Low | 75 (21%) | 9 (12%) | 84 (20%) |
| High | 68 (19%) | 22 (31%) | 90 (21%) | |
| Radical cystectomy | Low | 113 (31%) | 5 (7%) | 118 (27%) |
| High | 103 (29%) | 36 (50%) | 139 (32%) | |
| Total | 359 | 72 | 431 | |
TURBT transurethral resection of bladder tumor
Oncological outcome
In this retrospective study, the median follow-up was 78 months (range 4 to 138). Because of cancer metastasis, 601 patients (36%) died during this follow-up period. The overall 5 year cancer specific survival rate was 88%. Furthermore, the 5 year cancer specific survival rates were 69% for squamous differentiation-positive patients and 91% for squamous differentiation-negative patients (p < 0.001, Fig. 1). In subgroup of low-grade, the 5 year cancer specific survival rates were 84% in squamous differentiation-negative patients and 73% in squamous differentiation-positive patients (p < 0.001, Fig. 2). In subgroup of high-grade, the 5 year cancer specific survival rates were 96% in squamous differentiation-negative patients and 67% in squamous differentiation-positive patients (p < 0.001, Fig. 3). Because the high grade recurrent patients received radical cystectomy were more than low grade recurrent patients, compared with low-grade squamous differentiation-negative patients, the 5 year cancer specific survival rate was a little higher in subgroup of high-grade squamous differentiation-negative patients (96% versus 84%). Recurrence was observed in 431 (26%) patients. However, recurrence was more common in squamous differentiation-positive patients than squamous differentiation-negative patients (32% versus 25%, p = 0.026). Cox proportional hazard analysis was used for further analysis (Table 3). In the results of univariate analysis, tumor size (HR 1.397, 95% CI 1.052–1.856, p = 0.021), lymphovascular invasion (HR 1.272, 95% CI 1.002–1.614, p = 0.048), recurrence (HR 5.726, 95% CI 4.707–6.965, p < 0.001), and squamous differentiation (HR 2.091, 95% CI 1.709–2.557, p < 0.001) were found to be the prognostic factors associated with cancer specific survival rates. Moreover, according to the results of the multivariate Cox proportional hazard analysis, tumor size (HR 1.312, 95% CI 1.107–1.556, p = 0.002), lymphovascular invasion (HR 1.291, 95% CI 1.021–1.631, p = 0.033), recurrence (HR 5.610, 95% CI 4.633–6.793, p < 0.001) and squamous differentiation (HR 2.068, 95% CI 1.693–2.526, p < 0.001) significantly influenced the cancer specific survival rates.
Fig. 1.
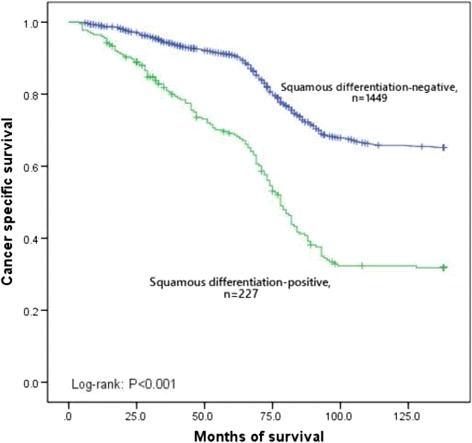
Kaplan–Meier curve of the cancer specific survival rates for the squamous differentiation-negative and squamous differentiation-positive (p < 0.001)
Fig. 2.
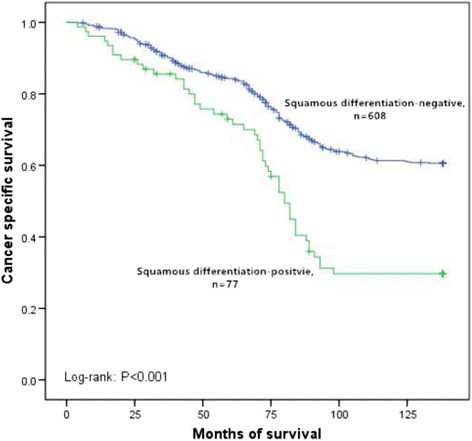
Kaplan–Meier curve of the cancer specific survival rates for the squamous differentiation-negative and squamous differentiation-positive in subgroup of low-grade (p < 0.001)
Fig. 3.
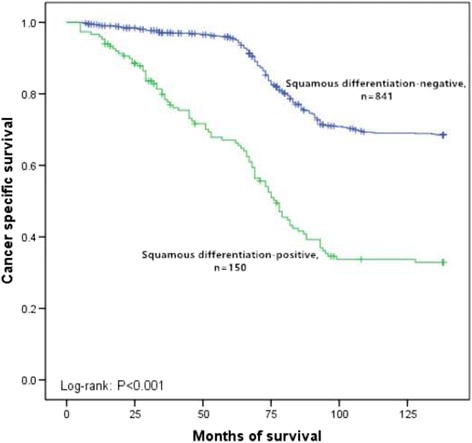
Kaplan–Meier curve of the cancer specific survival rates for the squamous differentiation-negative and squamous differentiation-positive in subgroup of high-grade (p < 0.001)
Table 3.
Univariate and multivariate Cox regression analyses predicting cancer specific survival
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| Age | 1.003 | 0.997–1.010 | 0.339 | —— | —— | —— |
| Gender | 1.039 | 0.847–1.275 | 0.714 | —— | —— | —— |
| Tumor grade | 0.944 | 0.722–1.234 | 0.674 | —— | —— | —— |
| Tumor multiplicity | 0. 900 | 0.688–1.178 | 0.444 | —— | —— | —— |
| Tumor size | 1.397 | 1.052–1.856 | 0.021 | 1.312 | 1.107–1.556 | 0.002 |
| Lymphovascular invasion | 1.272 | 1.002–1.614 | 0.048 | 1.291 | 1.021–1.631 | 0.033 |
| Recurrence | 5.726 | 4.707–6.965 | <0.001 | 5.610 | 4.633–6.793 | <0.001 |
| Squamous differentiation | 2.091 | 1.709–2.557 | <0.001 | 2.068 | 1.693–2.526 | <0.001 |
HR hazard ratio; CI confidence interval
After recurrence stratified by re-TURBT and radical cystectomy in squamous differentiation-positive group and squamous differentiation-negative group, cancer specific survival rates were estimated by the Kaplan–Meier analysis. Patients after re-TURBT had shorter median cancer specific survival than those underwent radical cystectomy in squamous differentiation-positive patients (33 versus 67 months, p = 0.009, Fig. 4). Nevertheless, no significant imbalance was found between re-TURBT and radical cystectomy groups in squamous differentiation-negative patients (66 versus 70 months, p = 0.418, Fig. 5).
Fig. 4.
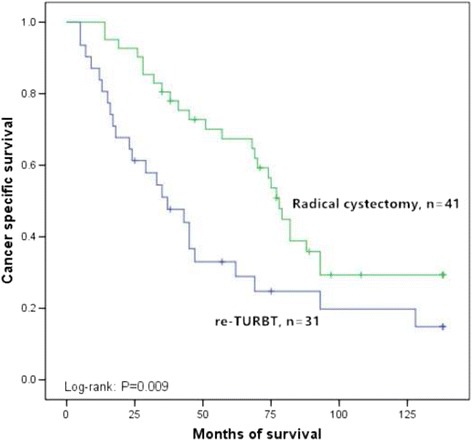
Kaplan–Meier curve of the cancer specific survival rates for re-transurethral resection of bladder tumor and radical cystectomy in the squamous differentiation-positive (p = 0.009). TURBT: Transurethral resection of bladder tumor
Fig. 5.
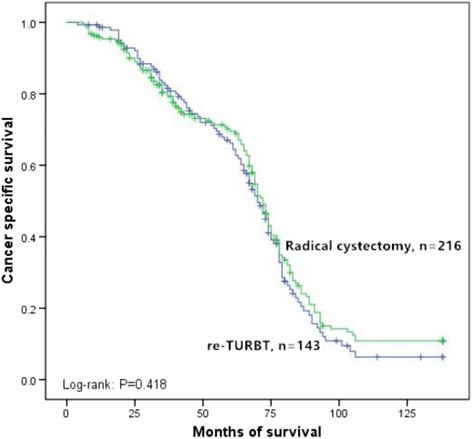
Kaplan–Meier curve of the cancer specific survival rates for re-transurethral resection of bladder tumor and radical cystectomy in the squamous differentiation-negative (p = 0.418). TURBT: Transurethral resection of bladder tumor
Pathology
Pathologists determined and confirmed 227 squamous differentiation patients. Evident intercellular bridges and/or keratinization indicated the presence of squamous differentiation (Fig. 6). The main histological characteristic is: 1. Presence of large and medium sized nucleolus in strands or nests of infiltrating tumor cells; 2. without clearly separated amphophilic or eosinophilic cytoplasmic background. The presence of lymphovascular invasion was determined by the stained sections in H&E (Fig. 7).
Fig. 6.
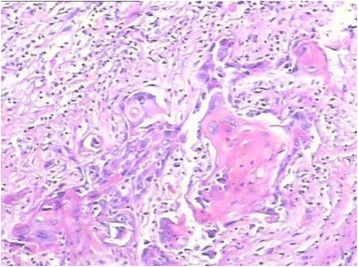
The component of tumor was considered to be squamous when intercellular bridges and/or keratinization were evident
Fig. 7.
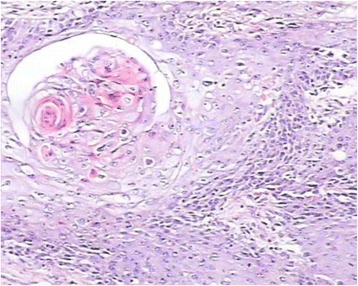
Stained sections in hematoxylin and eosin were used to evaluate the presence of lymphovascular invasion. H&E: hematoxylin and eosin
Discussion
Prior studies well established that urothelial carcinoma harbors remarkable propensity for divergent differentiation [12–14]. Squamous differentiation has been suggested to be the most common histological variation in bladder urothelial carcinoma and it may present basaloid or clear cell features [15]. However, mechanisms of squamous differentiation in urothelial carcinoma is not very clear. In 1925, Wolbach and Howe found that long time vitamin A deficiency treatment could lead to bladder squamous differentiation in rats [16]. More recently, several findings together with previous studies on the development of squamous differentiation under condition of retinoid deficiency, strongly recommend that retinoid signaling pathways and related networks are significant in the development of squamous lesions in the urinary bladder [17–20]. Maraver et al. showed that downregulation of NOTCH signaling contributed to occurrence of aggression in squamous lesions [21, 22]. Some transcriptional regulators (like forkhead boxA1) and activation of epidermal growth factor receptor (EGFR) pathway also play key roles in squamous differentiation in urothelial carcinoma. Moreover, Guma et al. found that HPV infection was associated with urothelial carcinoma with squamous differentiation [23]. Fujii et al. proposed that miR-145 may promote stem cell-like transformation in urothelial carcinoma cells and lead to differentiation into multiple cell types [24]. Therefore, it still requires a concerted effort by the research communities to differentiate “drivers” from “passengers” in the mechanisms of squamous differentiation.
Although thorough and careful light microscopic assessment is the best way to determine squamous lesions, it could be sometimes difficult to differentiate squamous differentiation from conventional urothelial carcinoma or squamous cell carcinoma, particularly in patients with borderline features. In such situation, the use of immunohistochemical technique, in addition to light microscopy, may be helpful. Huang et al. recently reported that MAC387, desmoglein-3 and TRIM29 could be a novel panel of specific markers for squamous differentiation in a series of bladder cancer [25]. In our study, the tumors showed a not clearly separated eosinophilic or amphophilic cytoplasmic background and strands or nests of infiltrating tumor cells with large and medium sized nuclei, often with nucleolus. Stained sections in H&E were used to evaluate the presence of squamous differentiation.
Many of recent studies have suggested the clinical significance of squamous differentiation in urothelial carcinoma. Fikret et al. evaluated the data from 223 patients treated with transurethral resection for bladder cancer and found squamous differentiation type of bladder urothelial carcinoma was more aggressive than conventional urothelial carcinoma and squamous differentiation may lead to poor prognosis [15]. Gluck et al., who analyzed 361 patients with invasive bladder carcinoma, concluded that squamous differentiation carcinomas were more aggressive with worse prognosis than pure urothelial carcinoma [5]. Alberto et al. retrospectively selected 113 patients with transitional cell carcinoma and suggested that squamous differentiation was an independent prognostic factor for cancer specific survival in patients treated with radical cystectomy [9]. However, there is short of data on the significance of squamous differentiation in 1676 patients with pT1 bladder urothelial carcinoma. Our study showed further evidence suggesting that squamous differentiation, a pathological variant, was an independent prognostic indicator for pT1 urothelial carcinoma in bladder cancer. Although survival of recurred patients with invasive bladder cancer has been reported, there is little data on the survival of the recurred pT1 bladder cancer patients after re-TURBT or radical cystectomy. Our series found that patients after re-TURBT had shorter median cancer specific survival than those underwent radical cystectomy in squamous differentiation-positive group (33 versus 67 months, p = 0.009). Nevertheless, no significant difference was found between the two operations in squamous differentiation-negative recurred patients (66 versus 70 months, p = 0.418). We suggested surgeons should operate radical cystectomy routinely in recurred pT1 urothelial carcinoma with squamous differentiation.
Tang et al. retrospectively analyzed the data of 687 upper tract urothelial carcinoma patients and found that patients with squamous and/or glandular differentiation were more likely to receive aggressive tumor biological characteristics and tend to have worse postoperative outcomes [26]. Our series found that squamous differentiation (HR 2.091, 95% CI 1.709–2.557, p < 0.001) was an independent prognostic factor associated with cancer specific survival in both univariate analysis and multivariate analyses. Tumor size (HR 1.397, 95% CI 1.052–1.856, p = 0.021), lymphovascular invasion (HR 1.272, 95% CI 1.002–1.614, p = 0.048) and recurrence (HR 5.726, 95% CI 4.707–6.965, P < 0.001) were also found to be the prognostic factors associated with cancer specific survival. In addition, in the results of the multivariate Cox proportional hazard analysis, tumor size (HR 1.312, 95% CI 1.107–1.556, p = 0.002), lymphovascular invasion (HR 1.291, 95% CI 1.021–1.631, p = 0.033), recurrence (HR 5.610, 95% CI 4.633–6.793, p < 0.001) and squamous differentiation (HR 2.068, 95% CI 1.693–2.526, p < 0.001) significantly influenced the cancer specific survival too.
It is routine to perform radical surgery on muscle-invasive tumor with urothelial carcinoma with squamous differentiation. However,if the patient is a non-muscle invasive case, it will be a dilemma in treatment option. Immunotherapy with bacillus Calmette–Guerin (BCG) on patients with variant tumors has been reported rarely [27]. Gofrit et al., who focused on 41 Ta or T1 patients diagnosed by second biopsy and received immunotherapy with BCG, found that BCG treatment was risky for patients with non-muscle invasive variant bladder tumors and these patients were more liable to worsen [28]. Furthermore, compared with conventional high-grade tumors, successful salvage may be a big challenge for these patients [28]. In this study, TURBT and intravesical chemotherapy with Pirarubicin or camptothecin were performed as initial treatments for all the patients to avoid adverse clinical course. Previous studies reported that intravesical BCG had worse prognosis, which was consistent with our study. According to previous results and our series, it is suggested that radical cystectomy is necessary for recurred pT1 urothelial carcinoma with squamous differentiation patients.
Conclusion
As it is concerned, the study is the first to concentrate on clinical significance of squamous differentiation on pT1 bladder urothelial carcinoma. When treated as an independent prognostic factor, squamous differentiation is related to higher risk of recurrence and poorer prognosis on patients: Suggesting its unique clinically-related nature. Based on the results mentioned above, radical cystectomy is of huge essence to deal with recurred patients suffering from high grade urothelial carcinoma with squamous differentiation, especially with lymphovascular invasion.
Acknowledgements
Medbanks (Beijing) Network Technology Co., Ltd. was thanked for data collection from patients’ charts and electronic medical records.
Funding
This study was supported by Tianjin Research Program of Application Foundation and Advanced Technology (number, 14CYBJC29800), Tianjin Municipal Natural Science Foundation (Grant 17JCYBJC26000) and Science and technology innovation fund projects of Tianjin Institute of Urology (number, MNYB201503). The funding bodies played no role in the design of the study, data collection, analysis, or interpretation of data.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CI
confidence interval
- EGFR
epidermal growth factor receptor
- H&E
hematoxylin and eosin
- HR
hazard ratio
- TURBT
Transurethral resection of bladder tumor
- UICC
Union for International Cancer Control
- WHO
World Health Organization
Authors’ contributions
YJN, GL and JPY conceived and designed the study. JPY and GL contributed to the writing of the manuscript. GL, JPY, HLS, SMZ, LBS, ZQS analyzed the data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Our study was approved by an independent ethical committee/institutional review board of the Second Hospital of Tianjin Medical University, Tianjin, China. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Gang Li, Email: 797980@sina.com.
Jianpeng Yu, Email: yjpgogogo@sina.com.
Hualin Song, Email: Fufengkui77@sina.com.
Shimiao Zhu, Email: Pengge122@sina.com.
Libin Sun, Email: fufengkui@126.com.
Zhiqun Shang, Email: xijuncui@163.com.
Yuanjie Niu, Email: inkexist@tmu.edu.cn.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 3.Moschini M, Karnes RJ, Sharma V, Gandaglia G, Fossati N, Dell’Oglio P, et al. Patterns and prognostic significance of clinical recurrences after radical cystectomy for bladder cancer: a 20-year single center experience. European J Surg Oncol: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2016;42(5):735–743. doi: 10.1016/j.ejso.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Shariat SF, Karakiewicz PI, Palapattu GS, Amiel GE, Lotan Y, Rogers CG, et al. Nomograms provide improved accuracy for predicting survival after radical cystectomy. Clin Cancer Res: an official journal of the American Association for Cancer Research. 2006;12(22):6663–6676. doi: 10.1158/1078-0432.CCR-06-0372. [DOI] [PubMed] [Google Scholar]
- 5.Gluck G, Hortopan M, Stanculeanu D, Chirita M, Stoica R, Sinescu I. Comparative study of conventional urothelial carcinoma, squamous differentiation carcinoma and pure squamous carcinoma in patients with invasive bladder tumors. J Med Life. 2014;7(2):211–214. [PMC free article] [PubMed] [Google Scholar]
- 6.Rausch S, Lotan Y, Youssef RF. Squamous cell carcinogenesis and squamous cell carcinoma of the urinary bladder: a contemporary review with focus on nonbilharzial squamous cell carcinoma. Urologic oncology. 2014;32(1):32.e11–6. doi:10.1016/j.urolonc.2012.11.020. [DOI] [PubMed]
- 7.Wishahi M, Elganzoury H, Elhouly A, Badawi M. Urothelial carcinoma of the urinary bladder mixed with squamous differentiation or squamous cell carcinoma in areas with schistosomiasis is showing high risk of recurrence and poor survival. J Egypt Soc Parasitol. 2014;44(2):467–473. doi: 10.12816/0006485. [DOI] [PubMed] [Google Scholar]
- 8.Raman JD, Jafri SM. Surgical management of bladder urothelial carcinoma with squamous differentiation. Urol Oncol. 2015;33(10):429–433. doi: 10.1016/j.urolonc.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Antunes AA, Nesrallah LJ, Dall’Oglio MF, Maluf CE, Camara C, Leite KR, et al. The role of squamous differentiation in patients with transitional cell carcinoma of the bladder treated with radical cystectomy. Intern Braz J Urol : official journal of the Brazilian Society of Urology. 2007;33(3):339–345. doi: 10.1590/S1677-55382007000300006. [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Beltran A, Cheng L. Histologic variants of urothelial carcinoma: differential diagnosis and clinical implications. Hum Pathol. 2006;37(11):1371–1388. doi: 10.1016/j.humpath.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 11.Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol. 2016; doi:10.1016/j.eururo.2016.05.041. [DOI] [PubMed]
- 12.Jozwicki W, Domaniewski J, Skok Z, Wolski Z, Domanowska E, Jozwicka G. Usefulness of histologic homogeneity estimation of muscle-invasive urinary bladder cancer in an individual prognosis: a mapping study. Urology. 2005;66(5):1122–1126. doi: 10.1016/j.urology.2005.06.134. [DOI] [PubMed] [Google Scholar]
- 13.Billis A, Schenka AA, Ramos CC, Carneiro LT, Araujo V. Squamous and/or glandular differentiation in urothelial carcinoma: prevalence and significance in transurethral resections of the bladder. Int Urol Nephrol. 2001;33(4):631–633. doi: 10.1023/A:1020597611645. [DOI] [PubMed] [Google Scholar]
- 14.Amin MB. Histological variants of urothelial carcinoma: diagnostic, therapeutic and prognostic implications. Modern Pathol : an official journal of the United States and Canadian Academy of Pathology, Inc. 2009;22(Suppl 2):S96–s118. doi: 10.1038/modpathol.2009.26. [DOI] [PubMed] [Google Scholar]
- 15.Erdemir F, Tunc M, Ozcan F, Parlaktas BS, Uluocak N, Kilicaslan I, et al. The effect of squamous and/or glandular differentiation on recurrence, progression and survival in urothelial carcinoma of bladder. Int Urol Nephrol. 2007;39(3):803–807. doi: 10.1007/s11255-006-9151-0. [DOI] [PubMed] [Google Scholar]
- 16.Wolbach SB, Howe PR. Tissue changes following deprivation of fat-soluble a vitamin. J Exp Med. 1925;42(6):753–777. doi: 10.1084/jem.42.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandhi D, Molotkov A, Batourina E, Schneider K, Dan H, Reiley M, et al. Retinoid signaling in progenitors controls specification and regeneration of the urothelium. Dev Cell. 2013;26(5):469–482. doi: 10.1016/j.devcel.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mauney JR, Ramachandran A, Yu RN, Daley GQ, Adam RM, Estrada CR. All-trans retinoic acid directs urothelial specification of murine embryonic stem cells via GATA4/6 signaling mechanisms. PLoS One. 2010;5(7) doi: 10.1371/journal.pone.0011513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang FX, Bosland MC, Huang H, Romih R, Baptiste S, Deng FM, et al. Cellular basis of urothelial squamous metaplasia: roles of lineage heterogeneity and cell replacement. J Cell Biol. 2005;171(5):835–844. doi: 10.1083/jcb.200505035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Molloy CJ, Laskin JD. Effect of retinoid deficiency on keratin expression in mouse bladder. Exp Mol Pathol. 1988;49(1):128–140. doi: 10.1016/0014-4800(88)90027-5. [DOI] [PubMed] [Google Scholar]
- 21.Maraver A, Fernandez-Marcos PJ, Cash TP, Mendez-Pertuz M, Duenas M, Maietta P, et al. NOTCH pathway inactivation promotes bladder cancer progression. J Clin Invest. 2015;125(2):824–830. doi: 10.1172/JCI78185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi W, Shah JB, Tran M, Svatek R, Marquis L, Lee IL, et al. p63 expression defines a lethal subset of muscle-invasive bladder cancers. PLoS One. 2012;7(1) doi: 10.1371/journal.pone.0030206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guma S, Maglantay R, Lau R, Wieczorek R, Melamed J, Deng FM, et al. Papillary urothelial carcinoma with squamous differentiation in association with human papilloma virus: case report and literature review. Am J Clin Exp Urol. 2016;4(1):12–16. [PMC free article] [PubMed] [Google Scholar]
- 24.Fujii T, Shimada K, Tatsumi Y, Hatakeyama K, Obayashi C, Fujimoto K et al. microRNA-145 promotes differentiation in human urothelial carcinoma through down-regulation of syndecan-1. BMC cancer. 2015;15:818. doi:10.1186/s12885-015-1846-0. [DOI] [PMC free article] [PubMed]
- 25.Huang W, Williamson SR, Rao Q, Lopez-Beltran A, Montironi R, Eble JN, et al. Novel markers of squamous differentiation in the urinary bladder. Hum Pathol. 2013;44(10):1989–1997. doi: 10.1016/j.humpath.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Tang Q, Xiong G, Li X, Fang D, Xi C, Zhang L, et al. The prognostic impact of squamous and glandular differentiation for upper tract urothelial carcinoma patients after radical nephroureterectomy. World J Urol. 2016;34(6):871–877. doi: 10.1007/s00345-015-1715-0. [DOI] [PubMed] [Google Scholar]
- 27.Shapur NK, Katz R, Pode D, Shapiro A, Yutkin V, Pizov G, et al. Is radical cystectomy mandatory in every patient with variant histology of bladder cancer. Rare Tumors. 2011;3(2) doi: 10.4081/rt.2011.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gofrit ON, Yutkin V, Shapiro A, Pizov G, Zorn KC, Hidas G, et al. The response of variant histology bladder cancer to Intravesical immunotherapy compared to conventional cancer. Front Oncol. 2016;6:43. doi: 10.3389/fonc.2016.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


