Abstract
Background
Acute myocardial infarction (AMI) patients with type 2 diabetes mellitus are known to present with multiple vessel lesions during coronary angiography. The underlying mechanism remains elusive and there is a shortage of serum prediction markers. In this study, we investigate the relationship between admission HbA1c and severity of coronary artery stenosis and subsequent prognosis in AMI patients with or without diabetes.
Research design and methods
We measured admission HbA1c, and vessel scores based on the number of diseased coronary vessels with significant stenosis in 628 patients diagnosed with AMI. Simple and multi-regression analysis were performed to investigate the correlation between HbA1c and the severity of coronary artery stenosis. Major adverse cardiovascular events (MACE), including new-onset myocardial infarction, acute heart failure and cardiac death, were documented during the follow-up. 272 non-DM participants and 137 DM participants were separated into two groups based on HbA1c levels for survival analysis during a 2-year follow up.
Results
448 non-DM patients and 180 DM patients were included in the initial observational analysis. 272 non-DM patients and 137 DM patients were included in the follow-up survival analysis. The admission HbA1c level was found to be significantly positively correlated to the number of affected vessels suffering from significant coronary artery stenosis both in DM (R square = 0.012; 95% CI 0.002 to 0.623, P = 0.049) and non DM patients (R square = 0.025; 95% CI 0.009 to 0.289, P = 0.037). Kaplan–Meier survival analysis revealed no significant difference with regard to different HbA1c levels either in DM or non-DM patients at the end of follow-up.
Conclusions
In patients with AMI, admission HbA1c is an important predictor for the severity of coronary artery stenosis in non-DM and DM patients. Further studies are needed to determine whether longer term follow-up could further identify the prognosis effect of HbA1c on MACE.
Keywords: HbA1c, Type 2 diabetes, Acute myocardial infarction, Coronary artery stenosis
Introduction
Acute myocardial infarction (AMI) is one of the leading health threatening diseases in the world [1, 2] and it remains the most common cause for morbidity and mortality in patients with type 2 diabetes disease (T2DM) [3]. On the one hand, although AMI patients with T2DM are known to present with multiple vessel lesion during coronary angiography, the underlying mechanism remains elusive and there is a shortage of serum prediction markers [4, 5]. On the other hand, glucometabolic disturbance is common in AMI and is found to be associated with significantly increased rate of all-cause mortality, congestive heart failure and shock [6]. However, due to stress hyperglycemia, which commonly occurs secondary to increased catecholamine levels in AMI, plasma glucose level at the onset of AMI is considered not a good morbidity and mortality predictor [7, 8].
Glycated hemoglobin A1c (HbA1c), measured primarily to identify 3-month average plasma glucose concentration, is accepted as a marker for long term glucose control in diabetes management [9]. Recent studies have revealed an association between chronic glucose dysregulation, assessed by HbA1c levels, and prognosis of AMI [10]. However, although lowering HbA1c levels is proven to have beneficial effects on microvascular complications [11, 12], the effects on macrovascular complications including AMI remain under explored.
It is reported that admission HbA1c level is a prognostic factor associated with mortality after acute myocardial infarction [13]. Moreover, quantitative relationship between HbA1c and atherosclerosis plaque textures is reported among diabetes mellitus (DM) patients with cardiovascular disease [14]. It is noteworthy that patients suffering from diabetes exhibit higher incidence of multi-vessel lesions during coronary artery angiography. However, it still remains unclear whether HbA1c level correlates to the severity of coronary artery stenosis. Besides, although some studies identify HbA1c as an effective marker in predicting major adverse cardiac events (MACE) in AMI patients with or without DM [15], others show no prognostic value or different results between diabetic and nondiabetic patients [16].
In this prospective cohort study, we investigate the relationship between admission HbA1c and the severity of coronary artery stenosis in AMI patients with or without diabetes. We subsequently carry survival analysis to investigate the effects of admission HbA1c levels on long term mortality and morbidity in AMI patients.
Research design and methods
Study design and participants
This was a single-center, prospective cohort study. Consecutive patients admitted to the cardiology department of the First Affiliated Hospital of Xi’an Jiaotong University for AMI between January 2013 and December 2016 were selected. The inclusion criteria were: (1) confirmed admission diagnosis of AMI, (2) successful treatment by angioplasty, (3) without diabetic ketosis or nonketotic hyperosmolar coma. The exclusion criteria were: (1) severe noncardiac disease with expected survival of less than 1 year and unwillingness to participation, (2) patients refusing angioplasty, (3) patients over the age of 80 years or living far away from the hospital’s catchment area. A patient could only be included once. Information about patients’ present medication, vascular risk factors and detailed medical history were obtained via questionnaires. Follow-up information was obtained via telephone questionnaires by the general practitioner (GP). AMI and DM were defined based on the universal definition criteria by the American Cardiology College and the American Diabetes Association criteria, respectively [17, 18]. Patients’ MACE, including new-onset myocardial infarction, acute heart failure and cardiac death, were documented during follow-up. Written informed consent was obtained from all study participants, with ethnic committee approval at the First Affiliated Hospital of Xi’an Jiaotong University.
Assessment of HbA1c and coronary artery stenosis
Blood HbA1c levels of all patients were measured within 3 h of admission, regardless of whether they had been fasting, using Siemens DCA analyzer for quantitative assay of HbA1c in blood. Both the concentrations of specific HbA1c and the concentration of total hemoglobin were measured. The ratio was reported as percent HbA1c. The HbA1c was studied as a continuous variable.
Selective coronary angiography was performed in multiple views. Coronary angiograms were analyzed by two experienced observers who were blinded to the identities and clinical information of the patients. Vessel scores were assessed based on the number of diseased coronary vessels with significant stenosis (greater than 50% stenosis of the lumen diameter). Next, the relationships between admission HbA1c and the results of coronary angiography were statistically evaluated.
Statistical analysis
All statistical analyses were performed by using SPSS for Windows 17.0 (SPSS Inc, Chicago, IL). Data were presented as frequencies and percentages for categorical variables and mean ± SD for continuous variables, unless otherwise indicated. One-way ANOVA was used to compare continuous variables. Simple linear analysis was used for calculating correlation between HbA1c and the severity of coronary artery stenosis. To ascertain the independent contribution to coronary artery stenosis, multivariate regression analysis was conducted. Kaplan–Meier survival curve analysis was used to represent the proportional risk of all-cause mortality and MACE for the admission HbA1c values in patients with or without DM. Patients were divided into two groups based on medians of HbA1c levels in DM and non-DM groups separately. A value of P < 0.05 was considered statistically significant.
Results
Study population
From January 2013 till December 2016, a total of 2054 patients were enrolled in the study; 448 non-DM patients and 180 DM patients were included in the initial observational analysis, while 272 non-DM patients and 137 DM patients were included in the follow-up survival analysis (Fig. 1). The main reason for exclusion were that patients refused consent for full screen (53.2%), that they were over the age of 80 (16.5%), and that they refused angioplasty (5.9%). Baseline patients’ characteristics are shown in Table 1a for patients without DM and in Table 1b for patients with DM in whole and divided based on medians of HbA1c. The mean age was 59.84 ± 10.71 years in non-DM and 61.00 ± 10.41 years in DM patients. The mean HbA1c was 5.73 ± 0.76% in non-DM and 7.86 ± 1.56% in DM patients. The median points of HbA1c were 5.7% in non-DM and 7.1% in DM patients. No significant difference in risk factors at baseline were seen in different HbA1c groups in either non-DM or DM patients.
Fig. 1.
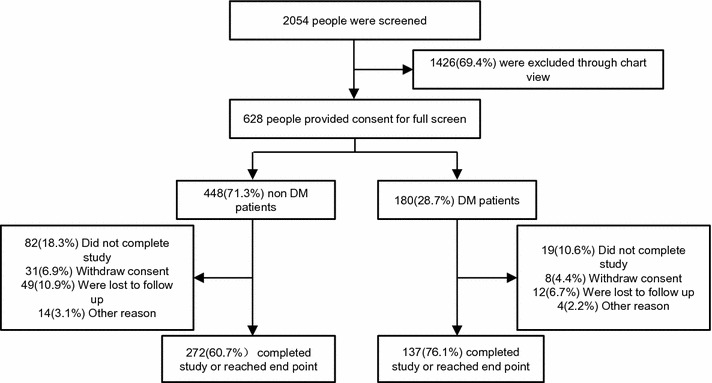
Enrollment an outcomes
Table 1.
Basic characteristics for patients (a) without DM and (b) with DM
| Whole | HbA1c (%) | P value | ||
|---|---|---|---|---|
| ≤5.7 | >5.7 | |||
| (a) | ||||
| Patient number | 272 | 142 | 130 | |
| Average HbA1c (%) | 5.73 ± 0.76 | 5.46 ± 0.21 | 6.05 ± 0.18 | <0.001 |
| Age (years) | 59.84 ± 10.71 | 59.79 ± 10.44 | 59.90 ± 11.03 | 0.93 |
| Female (%) | 20.96% | 20.28% | 26.15% | |
| BMI (kg/m2) | 24.81 ± 3.15 | 24.96 ± 3.25 | 24.54 ± 3.02 | 0.4 |
| Current/exsmoker (%) | 57.72% | 60.84% | 56.77% | |
| Systolic BP (mmHg) | 124.25 ± 20.07 | 124.49 ± 19.19 | 123.78 ± 17.83 | 0.75 |
| DiastolicBP (mmHg) | 77.44 ± 12.56 | 77.36 ± 11.26 | 77.45 ± 10.87 | 0.95 |
| FBG (mg/dL) | 6.05 ± 2.07 | 5.82 ± 1.61 | 6.15 ± 2.24 | 0.23 |
| Ejection fraction (%) | 59.25 ± 19.47 | 59.21 ± 13.01 | 59.12 ± 12.19 | 0.95 |
| LDL-C (mmol/L) | 2.28 ± 0.83 | 2.36 ± 0.72 | 2.19 ± 0.79 | 0.07 |
| Creatine (µmol/L) | 68.54 ± 15.72 | 68.75 ± 16.11 | 68.17 ± 15.19 | 0.76 |
| Previous history of hypertension (%) | 49.63% | 51.05% | 55.20% | |
| CHF (%) | 6.99% | 7.69% | 6.27% | |
| Myocardial infarction (%) | 16.18% | 22.38% | 24.74% | |
| PCI or CABG (%) | 19.49% | 18.88% | 16.64% | |
| In hospital treatment aspirin (%) | 95.96% | 96.50% | 95.67% | |
| β-Blocker (%) | 82.72% | 80.42% | 78.66% | |
| Statin (%) | 93.75% | 97.20% | 97.23% | |
| CCB (%) | 30.88% | 20.28% | 15.44% | |
| Whole | HbA1c (%) | P value | ||
|---|---|---|---|---|
| ≤7.1 | >7.1 | |||
| (b) | ||||
| Patient number | 137 | 60 | 77 | |
| Average HbA1c (%) | 7.86 ± 1.56 | 6.53 ± 0.36 | 6.53 ± 0.36 | <0.001 |
| Age (years) | 61.00 ± 10.41 | 57.52 ± 10.15 | 64.05 ± 10.17 | 0.003 |
| DM duration (years) | 4.33 ± 5.91 | 2.83 ± 4.52 | 5.71 ± 6.67 | <0.001 |
| Female (%) | 20.44% | 16.70% | 25.12% | |
| BMI (kg/m2) | 25.80 ± 2.76 | 25.84 ± 2.57 | 25.78 ± 2.92 | 0.95 |
| Current/exsmoker (%) | 56.20% | 73.29% | 49.73% | |
| Systolic BP (mmHg) | 127.99 ± 20.45 | 126.18 ± 22.40 | 129.40 ± 18.82 | 0.36 |
| DiastolicBP (mmHg) | 79.47 ± 11.80 | 79.61 ± 12.76 | 79.36 ± 11.07 | 0.9 |
| Fasting plasma glucose | 7.39 ± 2.95 | 7.22 ± 3.08 | 7.54 ± 2.82 | 0.47 |
| Ejection fraction (%) | 56.61 ± 18.07 | 56.73 ± 11.70 | 56.51 ± 11.84 | 0.92 |
| LDL-C (mmol/L) | 2.20 ± 0.93 | 2.35 ± 0.95 | 2.08 ± 0.84 | 0.08 |
| Creatine (µmol/L) | 71.68 ± 28.41 | 69.88 ± 21.91 | 73.08 ± 32.66 | 0.52 |
| Previous history of hypertension (%) | 59.85% | 54.97% | 55.83% | |
| CHF (%) | 8.03% | 6.69% | 8.36% | |
| Myocardial infarction (%) | 19.71% | 20.02% | 26.52% | |
| PCI or CABG (%) | 24.82% | 26.73% | 35.80% | |
| In hospital treatment aspirin (%) | 98.54% | 40.28% | 97.68% | |
| β-Blocker (%) | 89.05% | 96.64% | 89.76% | |
| Statin (%) | 99.27% | 100.00% | 100.00% | |
| CCB (%) | 27.74% | 21.68% | 27.92% | |
| Insulin (%) | 17.78% | 13.64% | 21.74% | |
| Metformin (%) | 0.00% | 0.00% | 0.00% | |
| Acarbose (%) | 35.56% | 27.27% | 43.48% | |
| Sulfonylureas (%) | 13.33% | 9.09% | 17.39% | |
Data are mean ± SD and number (%)
DM diabetes mellitus, HbA 1c, hemoglobin A1c, BMI body mass index, BP blood pressure, FBG fasting blood glucose, CHF chronic heart failure, PCI percutaneous coronary intervention, CABG coronary artery bypass graft, LDL-C low density lipoprotein-cholesterol, CCB calcium channel blocker
Association between HbA1c and severity of coronary artery stenosis
To investigate the relationship between HbA1c and the severity of coronary artery stenosis, we utilized simple linear regression analysis. The admission HbA1c levels were found to be significantly positively correlated with the numbers of affected vessels suffering from significant coronary artery stenosis both in DM (R square = 0.012; 95% CI 0.002 to 0.623, P = 0.049) and non-DM patients (R square = 0.025; 95% CI 0.009 to 0.289, P = 0.037) (Fig. 2; Table 2).
Fig. 2.
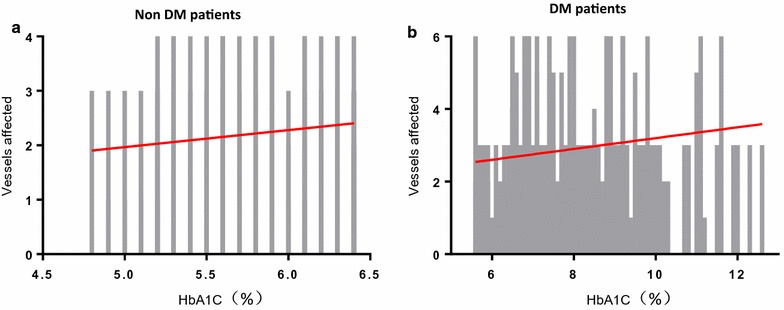
Simple linear analysis between HbA1c and number of stenosis coronary arteries in non-DM and DM groups. a Simple linear regression model with HbA1c level in relation to the number of stenosis coronary vessels in non-DM patients with AMI. b Simple linear regression model with HbA1c level in relation to number of stenosis coronary vessels in DM patients with AMI
Table 2.
Linear regression analysis of HbA1c and coronary artery stenosis in patients with or without DM
| Group | R square | Coefficient | 95% CI | SEM | P value |
|---|---|---|---|---|---|
| Non DM | 0.012 | 0.313 | 0.002 to 0.623 | 0.158 | 0.049 |
| DM | 0.025 | 0.149 | 0.009 to 0.289 | 0.071 | 0.037 |
HbA 1c hemoglobin A1c, DM diabetes mellitus, CI confidence interval, SEM standard error of measurement
Multi-regression analysis was then utilized to further determine the association of severity of coronary artery lesions and baseline characteristics including admission HbA1c. Interestingly, although HbA1c level was found to be significantly positively correlated to the severity of coronary artery stenosis in DM patients (95% CI 0.040 to 0.312, P = 0.011), the P value was yet close to significance in non-DM patients (95% CI −0.648 to 0.032, P = 0.076) (Table 3a, b).
Table 3.
Multi regression analysis of coronary artery stenosis in patients (a) without DM and (b) with DM
| Factors | Coefficient | 95% CI | SEM | P value |
|---|---|---|---|---|
| (a) | ||||
| Average HbA1c (%) | −0.308 | −0.648 to 0.032 | 0.173 | 0.076 |
| Age (years) | 0.003 | −0.009 to 0.015 | 0.006 | 0.630 |
| GRACE score | 0.000 | −0.003 to 0.003 | 0.002 | 0.744 |
| HR (bpm) | 0.001 | −0.006 to 0.008 | 0.003 | 0.755 |
| Systolic BP (mmHg) | 0.003 | −0.007 to 0.013 | 0.005 | 0.573 |
| DiastolicBP (mmHg) | −0.008 | −0.023 to 0.007 | 0.008 | 0.282 |
| FBG (mg/dL) | 0.024 | −0.032 to 0.081 | 0.029 | 0.397 |
| CKMB (U/L) | −0.001 | −0.004 to 0.001 | 0.001 | 0.185 |
| LDL-C (mmol/L) | 0.092 | −0.060 to 0.245 | 0.078 | 0.234 |
| Creatine (µmol/L) | 0.005 | −0.003 to 0.012 | 0.004 | 0.225 |
| (b) | ||||
| Average HbA1c (%) | 0.176 | 0.040 to 0.312 | 0.069 | 0.011 |
| Age (years) | 0.008 | −0.013 to 0.030 | 0.011 | 0.454 |
| DM duration (years) | −0.001 | −0.037 to 0.035 | 0.018 | 0.954 |
| GRACE score | 0.004 | −0.002 to 0.010 | 0.003 | 0.169 |
| HR (bpm) | 0.019 | 0.004 to 0.035 | 0.008 | 0.016 |
| Systolic BP (mmHg) | 0.000 | −0.001 to 0.000 | 0.000 | 0.202 |
| DiastolicBP (mmHg) | −0.011 | −0.021 to −0.001 | 0.005 | 0.038 |
| FBG (mg/dL) | 0.183 | 0.115 to 0.251 | 0.034 | 0.000 |
| CKMB (U/L) | −0.003 | −0.007 to 0.001 | 0.002 | 0.160 |
| LDL-C (mmol/L) | 0.501 | −0.465 to 1.468 | 0.489 | 0.307 |
| Creatine (µmol/L) | 0.027 | −0.099 to 0.153 | 0.064 | 0.678 |
HbA 1c hemoglobin A1c, DM diabetes mellitus, CI confidence interval, SEM standard error of measurement, GRACE the global registry of acute coronary events, HR heart rate, BP blood pressure, FBG fasting blood glucose, CKMB MB isoenzyme of creatine kinase, LDL-C low density lipoprotein-cholesterol
All cause mortality and MACE
At the end of the follow-up, within non-DM patients 14 (5.1%) patients died for all cause, 11 (4.0%) for cardiac cause, 30 (11.0%) for acute heart failure, and 12 (4.4%) had new-onset myocardial infarction. Within DM patients, 5 (3.6%) died for all cause, 2 (1.5%) for cardiac cause, 13 (9.5%) for acute heart failure, and 9 (6.5%) had new-onset myocardial infarction.
Kaplan–Meier survival analysis was utilized to evaluate the survival curve in different HbA1c groups in non-DM and DM patients. The analysis revealed no significant difference with regard to different HbA1c levels both in DM and non-DM patients, shown in Fig. 3.
Fig. 3.
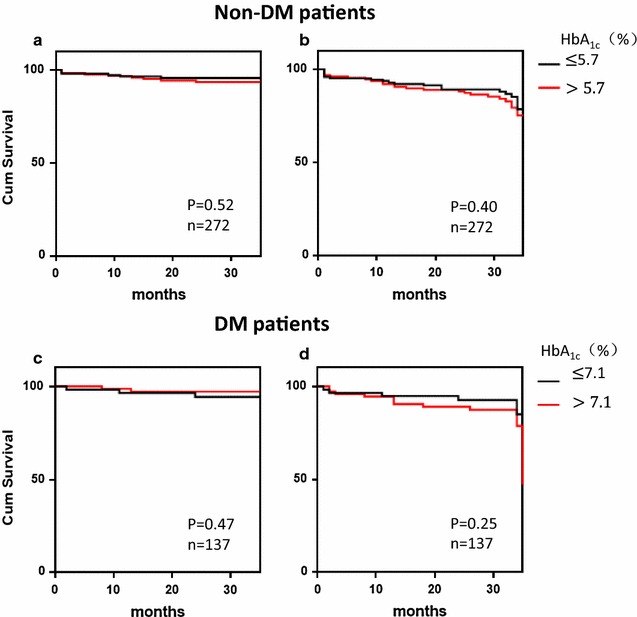
Kaplan–Meier survival curves for freedom from all cause mortality and MACE in non-DM and DM patient groups. a Kaplan–Meier survival curves for freedom from all cause mortality in non-DM by HbA1c levels. P = 0.86. b Kaplan–Meier survival curves for freedom from MACE in non-DM by HbA1c levels. P = 0.84. c Kaplan–Meier survival curves for freedom from all cause mortality in DM by HbA1c levels. P = 0.62. d Kaplan–Meier survival curves for freedom from MACE in DM by HbA1c levels. P = 0.34. There is not significant higher event-free survival rate in high HbA1c level patients in two groups
Discussion
In this study, serum HbA1c is found to be associated with the severity of coronary artery stenosis in diabetic and nondiabetic patients with acute myocardial infarction undergoing primary angioplasty. Moreover, admission serum HbA1c level exhibits no effect on all cause mortality rate and MACE rate either in non-DM or DM patients in 2-year follow-up.
The important implication of the present study is that HbA1c is identified as a serum predictor for severity of cardiovascular lesions in non-DM and DM patients. Previous study indicates a non-linear relationship between HbA1c and major vascular outcomes and mortality [16]. It is also known that poor glycemic control is associated with multiple vessel lesions in coronary artery disease [19, 20]. However, few studies have addressed the question whether HbA1c is related to the severity of coronary artery stenosis under non-DM and DM background. The major outcome of this study shows a positive correlation between admission HbA1c concentrations and the number of stenosis coronary arteries in patients with acute myocardial infarction, indicating that HbA1c level is a potential indicator for multiple coronary vessel lesions. Moreover, the significant correlation between HbA1c and coronary artery stenosis is identified both in non-DM and DM population, implying that HbA1c level monitoring might be beneficial even for patients without diabetes.
Acute hyperglycemia has been reported to be associated with acute adrenergic signal of stress [16, 21] and endothelial cell dysfunction in acute myocardial infarction, which is partially attributed to endothelial cell apoptosis [22, 23], reactive oxygen species (ROS) over production [24], and inflammation [25]. However, the effect of chronic hyperglycemia on vascular function and coronary artery complications has been less reported. It is shown before that long-term glucose dysregulation is associated with increased cell death signaling [26], inflammatory changes and fibrosis [27], and subsequent cardiomyopathy [28]. In this study, long term uncontrolled glucose level, indicated by HbA1c is shown to be correlated with the severity of coronary artery complications. Besides, this correlation could be further identified in patients without diabetes but with relatively higher level of HbA1c.
There is conflicting evidence regarding HbA1c level and major cardiovascular outcomes [13, 16, 29, 30]. In this study, HbA1c is not associated with all cause mortality and MACE in both non-DM and DM group over a 2-year follow up. The less clear association between HbA1c and cardiovascular outcomes could be due to a limited number of patients with a relatively short follow-up in the present study [16]. It is speculated that HbA1c may have limited predictive power for short-term prognosis in patients with AMI, but its association with long-term prognosis may be stronger [31]. As a result, more well-designed and long-term studies as well as systemic analysis are needed to investigate whether HbA1c will play an important role in the prognosis of AMI.
Study limitations
This is a single centre based observational cohort study. The sample size in this study is relatively small, especially in patients with T2DM, therefore, comparisons of some subgroups may lack power to detect significant differences for selected variables. Although HbA1c level is associated with the number of the stenosis coronary arteries, a complex and systemic score, i.e. SYNTAX score, could be further recorded to predict the severity of coronary artery stenosis more accurately.
Conclusions
In patients with AMI, admission HbA1c may be an important predictor for severity of coronary artery stenosis in non-DM and DM patients. The results of this study further support the view that chronic glycemic control should be one of the treatment targets for AMI patients. Further studies are needed to determine whether longer term follow-up would further identify the prognosis effect of HbA1c on MACE.
Authors’ contributions
JS, YW and ZY participated in the design of the study. HL and YX collected the written informed consent and patients’ data. XL, RS performed the statistical analysis. JS and YD drafted the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge support of China Scholarship Council (CSC) and Deutscher Akademischer Austauschdienst (DAAD).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
We acknowledge the availability of the data in the paper.
Consent for publication
All authors have reviewed the final version of the manuscript and approve it for publication.
Ethics approval and consent to participate
Written informed consent was obtained from all study participants, with ethnic committee approval at the First Affiliated Hospital of Xi’an Jiaotong University.
Funding
This study was supported by Central University Basic Science Foundation of China (1191329724) and by National Natural Science Foundation of China (81570406).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- HbA1c
hemoglobin A1c
- AMI
acute myocardial infarction
- T2DM
type 2 diabetes mellitus
- MACE
major adverse cardiovascular events
- GP
general practitioner
- BMI
body mass index
- BP
blood pressure
- HR
heart rate
- FBG
fasting blood glucose
- CKMB
MB isoenzyme of creatine kinase
- LDL-C
low density lipoprotein-cholesterol
- CHF
chronic heart failure
- PCI
percutaneous coronary intervention
- CABG
coronary artery bypass graft
- CCB
calcium channel blocker
- GRACE
the global registry of acute coronary events
Contributor Information
Jianqing She, Email: jianqingshe@xjtu.edu.cn.
Yangyang Deng, Email: yangyangdeng@126.com.
Yue Wu, Email: imwuyue@qq.com.
Yulong Xia, Email: yulongxia@126.com.
Hongbing Li, Email: lihongbing@126.com.
Xiao Liang, Email: liangxiao@126.com.
Rui Shi, Email: shirui@xjtu.edu.cn.
Zuyi Yuan, Email: zuyiyuan@mail.xjtu.edu.cn.
References
- 1.Hollander JE, Than M, Mueller C. State-of-the-art evaluation of emergency department patients presenting with potential acute coronary syndromes. Circulation. 2016;134:547–564. doi: 10.1161/CIRCULATIONAHA.116.021886. [DOI] [PubMed] [Google Scholar]
- 2.She J, Hu Z, Deng Y, Liu F, Yuan Z. Chest pain after aortic valve replacement: rupture of right sinus of valsalva presenting as myocardial infarction. Cardiology. 2016;134:22–25. doi: 10.1159/000443266. [DOI] [PubMed] [Google Scholar]
- 3.Bohn B, et al. Achievement of treatment goals for secondary prevention of myocardial infarction or stroke in 29,325 patients with type 2 diabetes: a German/Austrian DPV-multicenter analysis. Cardiovasc Diabetol. 2016;15:72. doi: 10.1186/s12933-016-0391-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnold SV, et al. Predicting adverse outcomes after myocardial infarction among patients with diabetes mellitus. Circ Cardiovasc Qual Outcomes. 2016;9:372–379. doi: 10.1161/CIRCOUTCOMES.115.002365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold LW, Hoy WE, Sharma SK, Wang Z. The Association between HbA1c and cardiovascular disease markers in a remote indigenous Australian community with and without diagnosed diabetes. J Diabetes Res. 2016;2016:5342304. doi: 10.1155/2016/5342304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mellbin LG, Bjerre M, Thiel S, Hansen TK. Complement activation and prognosis in patients with type 2 diabetes and myocardial infarction: a report from the DIGAMI 2 trial. Diabetes Care. 2012;35:911–917. doi: 10.2337/dc11-1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Won KB, et al. Comparison of 2-year mortality according to obesity in stabilized patients with type 2 diabetes mellitus after acute myocardial infarction: results from the DIAMOND prospective cohort registry. Cardiovasc Diabetol. 2015;14:141. doi: 10.1186/s12933-015-0305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arnold SV, et al. Recognition of incident diabetes mellitus during an acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2015;8:260–267. doi: 10.1161/CIRCOUTCOMES.114.001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skriver MV, Stovring H, Kristensen JK, Charles M, Sandbaek A. Short-term impact of HbA1c on morbidity and all-cause mortality in people with type 2 diabetes: a Danish population-based observational study. Diabetologia. 2012;55:2361–2370. doi: 10.1007/s00125-012-2614-1. [DOI] [PubMed] [Google Scholar]
- 10.Olsson M, Schnecke V, Cabrera C, Skrtic S, Lind M. Contemporary risk estimates of three HbA1c variables for myocardial infarction in 101,799 patients following diagnosis of type 2 diabetes. Diabetes Care. 2015;38:1481–1486. doi: 10.2337/dc14-2351. [DOI] [PubMed] [Google Scholar]
- 11.Umayahara Y, et al. Association of glycated albumin to HbA1c ratio with diabetic retinopathy but not diabetic nephropathy in patients with type 2 diabetes. Clin Biochem. 2017;50:270–273. doi: 10.1016/j.clinbiochem.2016.11.032. [DOI] [PubMed] [Google Scholar]
- 12.Liu F, et al. Influence of HbA1c on short-term blood pressure variability in type 2 diabetic patients with diabetic nephropathy. J Zhejiang Univ Sci B. 2013;14:1033–1040. doi: 10.1631/jzus.B1300030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu XJ, et al. Adjustment of the GRACE score by Hemoglobin A1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2015;14:110. doi: 10.1186/s12933-015-0274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SW, et al. Association between HbA1c and carotid atherosclerosis among elderly Koreans with normal fasting glucose. PLoS ONE. 2017;12:e0171761. doi: 10.1371/journal.pone.0171761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis TM, Coleman RL, Holman RR. Prognostic significance of silent myocardial infarction in newly diagnosed type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS) 79. Circulation. 2013;127:980–987. doi: 10.1161/CIRCULATIONAHA.112.000908. [DOI] [PubMed] [Google Scholar]
- 16.Su G, et al. Prognostic value of early in-hospital glycemic excursion in elderly patients with acute myocardial infarction. Cardiovasc Diabetol. 2013;12:33. doi: 10.1186/1475-2840-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Handelsman Y, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011;17(Suppl 2):1–53. doi: 10.4158/EP.17.S2.1. [DOI] [PubMed] [Google Scholar]
- 18.Levine GN, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2016;152:1243–1275. doi: 10.1016/j.jtcvs.2016.07.044. [DOI] [PubMed] [Google Scholar]
- 19.Chi C, Snaith J, Gunton JE. Diabetes medications and cardiovascular outcomes in type 2 diabetes. Heart Lung Circ. 2017 doi: 10.1016/j.hlc.2017.02.030. [DOI] [PubMed] [Google Scholar]
- 20.Joffe HV, Parks MH, Temple R. Impact of cardiovascular outcomes on the development and approval of medications for the treatment of diabetes mellitus. Rev Endocr Metab Disord. 2010;11:21–30. doi: 10.1007/s11154-010-9130-8. [DOI] [PubMed] [Google Scholar]
- 21.Ye Y, Xie H, Zhao X, Zhang S. The oral glucose tolerance test for the diagnosis of diabetes mellitus in patients during acute coronary syndrome hospitalization: a meta-analysis of diagnostic test accuracy. Cardiovasc Diabetol. 2012;11:155. doi: 10.1186/1475-2840-11-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mourino-Alvarez L, et al. Proteomic characterization of EPCs and CECs “in vivo” from acute coronary syndrome patients and control subjects. Biochim Biophys Acta. 1830;3030–3053:2013. doi: 10.1016/j.bbagen.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 23.Hyseni A, et al. Chronic dysfunction of the endothelium is associated with mortality in acute coronary syndrome patients. Thromb Res. 2013;131:198–203. doi: 10.1016/j.thromres.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Quagliaro L, et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes. 2003;52:2795–2804. doi: 10.2337/diabetes.52.11.2795. [DOI] [PubMed] [Google Scholar]
- 25.Wu Y, et al. Activation of AMPKalpha2 in adipocytes is essential for nicotine-induced insulin resistance in vivo. Nat Med. 2015;21:373–382. doi: 10.1038/nm.3826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lal N, et al. Loss of VEGFB and its signaling in the diabetic heart is associated with increased cell death signaling. Am J Physiol. Heart and circulatory physiology, ajpheart 00659 02016, doi:10.1152/ajpheart.00659.2016 (2017). [DOI] [PubMed]
- 27.Feng B, Chen S, Gordon AD, Chakrabarti S. miR-146a mediates inflammatory changes and fibrosis in the heart in diabetes. J Mol Cell Cardiol. 2017;105:70–76. doi: 10.1016/j.yjmcc.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Lorenzo-Almoros A, et al. Diagnostic approaches for diabetic cardiomyopathy. Cardiovasc Diabetol. 2017;16:28. doi: 10.1186/s12933-017-0506-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hadjadj S, et al. Determination of HbA1c concentrations in patients with acute myocardial infarction: comparison of the DCA 2000 device with the HPLC method. Diabetes Metab. 2005;31:290–294. doi: 10.1016/S1262-3636(07)70196-9. [DOI] [PubMed] [Google Scholar]
- 30.Ghaffari S, et al. Association between HbA1c levels with severity of coronary artery disease and short-term outcomes of acute ST-elevation myocardial infarction in nondiabetic patients. Ther Adv Cardiovasc Dis. 2015;9:305–313. doi: 10.1177/1753944715585500. [DOI] [PubMed] [Google Scholar]
- 31.Gupta V, Singh S, Maheshwari PK, Gupta AK, Chaturvedi M. Prognostic significance of HbA1C in non-diabetic patients in acute coronary syndrome. J Assoc Physicians India. 2016;64:76. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We acknowledge the availability of the data in the paper.


