Abstract
Young men who have sex with men are at high risk for HIV, and most new HIV infections occur in serious relationships. This pilot study assessed the feasibility, acceptability and preliminary efficacy of the 2GETHER couples-based HIV prevention and relationship education intervention for young same-sex male couples. We enrolled 57 young male couples (N = 114) into a four-session hybrid group and individual intervention. We assessed acceptability via post-session surveys and exit interviews, and we examined preliminary efficacy at a two week posttest. The vast majority of participants (93%) reported exclusively positive impressions of 2GETHER, and all components received high mean ratings. We observed decreases in HIV risk behavior, increases in information, motivation and behavioral skills related to HIV prevention, and improvement in relationship investment between pretest and posttest. Integrating relationship education and sexual health programming may be an effective way to reduce HIV transmissions in young male couples.
Keywords: HIV/AIDS, Relationship education, Couples, Young men who have sex with men
Introduction
Men who have sex with men (MSM) accounted for 63% of new HIV infections in 2014 [1], and young MSM (YMSM) ages 13–24 and 25–34 have the highest rates of new infections (10 and 27% increased incidence from 2010 to 2014, respectively). Steady or main partner relationships account for a substantial proportion of new HIV infections in MSM (35–68%) [2, 3], and this proportion has been estimated to be 79–84% in YMSM ages 18–29 [3]. Given rising HIV incidence among YMSM and the high proportion of new infections attributable to main partnerships, there is an urgent need to establish innovative couples-based HIV prevention strategies for YMSM. Further, many adult and YMSM report increased fatigue with safer sex messages and practices but express a need for services that address health more generally [4, 5], including relationship education services [6]. Integrating relationship education with HIV prevention is an innovative approach to curbing HIV incidence amongst those at highest risk for infection.
Extant research indicates that YMSM are more likely to have condomless anal sex (CAS) with main or serious partners compared to casual sex partners [3, 7, 8]. Qualitative evidence suggests that YMSM have CAS with serious partners to express trust and intimacy, and they stop using condoms without initiating pre-exposure prophylaxis (PrEP) because they perceive their relationship to be monogamous/low-risk [9, 10]. Unfortunately, male couples also report infrequent HIV testing, even when CAS has occurred with outside partners [11, 12]. Given the high proportion of HIV-positive YMSM who are unaware they are infected [13], YMSM may unknowingly put their serious partners at risk for infection. Because most existing prevention strategies focus in large part on reducing CAS with casual partners [14], most YMSM do not have the skills to navigate the complexities of HIV prevention in romantic relationships, such as timing of HIV testing, condom use, and use of biomedical prevention strategies. Furthermore, various relationship factors and partner characteristics predict CAS in YMSM, including having older sexual partners [15, 16], intimate partner violence [7], power differentials between partners [7, 8], and alcohol and drug use before sex [17, 18]. These are all aspects of relationships that can be addressed in couples-based interventions in order to reduce their effects on HIV risk.
Many male couples use relationship agreements to reduce HIV risk in their main partnerships [19, 20], which delineate whether relationships are “closed/monogamous” or “open”, specify the conditions under which outside sexual partners are permissible, and establish rules about extradyadic sex. Studies suggest a large proportion of male couples either do not have an agreement or disagree about the agreement rules [21, 22]. Indeed, nearly 20% of couples report discrepant agreements [23], which may result in exposure to HIV/STIs. Breaks in agreements are also not uncommon in male couples (~46% report breaks) [22], and breaks are frequently undisclosed to partners. These findings highlight the need for MSM to develop skills to negotiate formal relationship agreements with their partners, as well as strategies for adhering to agreements, changing agreements over time based on needs, and disclosing breaks in agreements promptly if they occur.
Recent advances in biomedical treatment as prevention (TasP), including the use of PrEP among HIV-negative persons and viral suppression among HIV-positive persons, have drastically changed the landscape of HIV prevention [24, 25]. MSM are already making decisions to forego condom use based on their partners’ use of biomedical prevention [26], and the field is in desperate need of interventions that effectively integrate biomedical and behavioral approaches. Couples-based programs create unique opportunities for this integration because both partners are involved and an integrated strategy can be developed to reduce transmission risk within the couple (i.e., when one member is known/unknown HIV-positive) and with extradyadic partners. Furthermore, couples may be composed of individuals with the same HIV status (i.e., concordant negative or positive) or different statuses (i.e., serodiscordant). While it may be simpler from an evaluation perspective to develop separate intervention modalities for each type of couple (concordant negative, concordant positive, and serodiscordant), separating couples based on HIV status does not make practical or fiscal sense for organizations that may ultimately implement such programs.
Several domestic couples-based HIV prevention programs have been developed for heterosexual adults [27], but a recent review found that only one couples-based program has been developed for adult MSM (none for YMSM) [28]. YMSM have unique developmental needs, including experiences with stigma and delays in achieving relationship milestones due to lack of available partners [29], so content developed for heterosexuals and adult MSM may not be relevant. Couples HIV counseling and testing (CHCT), a single-session program that provides skills for reducing HIV risk in couples, is an effective HIV prevention strategy [30, 31]. Despite widespread use in Africa [32, 33], it is not widely used as a testing strategy in the United States [34]. Further, CHCT does not address relationship skills and it is not applicable to transmission risk in HIV-positive YMSM. In order to optimize the effectiveness of couples-based HIV prevention strategies for YMSM, interventions must not only address the various factors that influence HIV risk in relationships but also the overall functioning of the relationship more broadly.
Relationship education is a growing field that uses a preventive approach to promote long-term couple health by teaching skills to form and maintain healthy relationships. Because couples’ abilities to communicate constructively about relationship expectations and disagreements are well-established predictors of couple outcomes, relationship education programs heavily emphasize skill-building in communication and conflict resolution [35]. Meta-analysis indicates that these programs are effective in improving conflict-management skills, as well as global relationship satisfaction, among different-sex couples [36]. Recently, adaptations of evidence-based relationship education programs for same-sex couples have demonstrated acceptability to participants and positive effects on couple communication, conflict resolution, and relationship quality [37, 38]. Furthermore, research has detailed the various long-term mental and physical health benefits of healthy romantic relationships, including reducing depression and heavy alcohol use [39, 40]. This indicates that relationship education may also improve other important health outcomes among YMSM beyond reducing HIV transmission risk, particularly given that depression and problem alcohol use also disproportionately impact sexual minorities [41, 42].
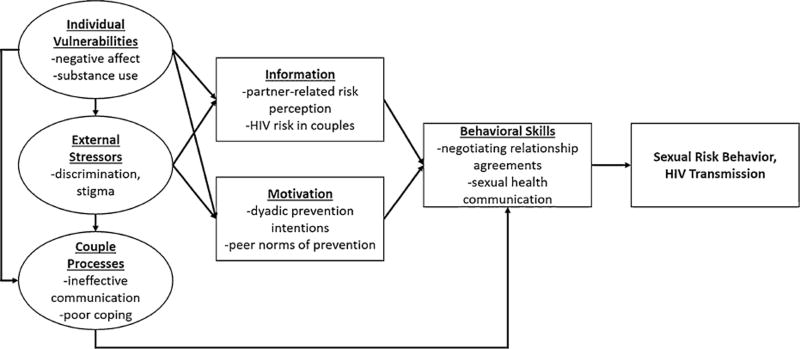
We drew upon two widely-used frameworks to integrate relationship education and HIV prevention content for coupled YMSM in developing the 2GETHER intervention (see Fig. 1). First, the Information–Motivation–Behavioral Skills (IMB) model explains how cognitive, motivational, and behavioral factors contribute to HIV risk behavior [43]. The IMB model was adapted to address HIV risk behavior in romantic relationships [44], and this Relationship-Oriented IMB model (RELO-IMB) was recently validated in a sample of YMSM [45]. In this model, “Information” addresses couples-specific HIV knowledge (e.g., risk within dyad and with outside partners), “Motivation” addresses attitudes and peer norms about prevention in relationships, and “Behavioral Skills” addresses risk reduction skills relevant to couples (e.g., discussions about safer sex and HIV testing, negotiating relationship agreements). Next, the Vulnerability–Stress–Adaptation model of relationship functioning (VSA) [46] asserts that negative relationship outcomes are explained by: (1) the individual partner’s vulnerabilities (e.g., negative affect, substance use), (2) stressors faced outside the relationship (e.g., stigma, prejudice), and (3) deficits in adaptive couple processes (e.g., communication skills). Consistent with minority stress theory [47], same-sex couples are more likely than heterosexuals to experience stress in each VSA domain due to exposure to intolerant societal conditions (e.g., stigma) that promote negative internalized beliefs, and because delays in reaching relationship milestones lead to deficits in adaptive couple processes (e.g., effective communication) [29].
Fig. 1.
Integrated vulnerability stress adaptation and relationship-oriented information, motivation, behavioral skills model. Note: The investigator-created framework was developed specifically for the development of the 2GETHER intervention, and it draws on the relationship-orientation information, motivation, behavioral skills (RELO-IMB) and vulnerbality stress adaptation (VSA) models
In addition to general relationship stress, young same-sex couples experience sexual minority-specific stressors, such as discrepancies in partner outness, comfort with public displays of affection, and family acceptance of their relationship [29]. In turn, psychological distress can impact couples’ relationship functioning [46] and their ability to consistently engage in sexual risk reduction behaviors [4]. As such, teaching coping skills in tandem with HIV prevention and relationship education for coupled YMSM could improve intervention efficacy. Cognitive-behavioral coping strategies, such as problem-solving, have been used successfully in HIV risk reduction interventions with MSM [48, 49]. Other techniques rooted in acceptance, such as acknowledging one’s internal reactions to a problem and identifying that negative situations may not be able to change, have been effective in decreasing sexual minority stress [50]. Integrating these approaches into sexual and relationship education for YMSM may reduce HIV risk through improved couple functioning and reduced psychological distress.
The goal of the current study was to conduct an initial evaluation of 2GETHER, an intervention that aims to reduce HIV transmission risk and improve relationship functioning among young same-sex male couples. Mixed methods formative work that informed the development of 2GETHER is described elsewhere [6, 10, 29]. Our aims were to (1) determine the feasibility of recruiting, enrolling and retaining coupled YMSM into a four session hybrid group and individual intervention; (2) use multiple methods to evaluate the acceptability of and engagement with the intervention; (3) and obtain initial estimates of intervention efficacy using a one-group pretest–posttest design. We hypothesized significant reductions in sexual risk behavior, improvements in RELO-IMB constructs, and improvements in relationship-orientated outcomes (i.e., investment, satisfaction, and functioning). We also examined potential changes in depressive symptoms and alcohol problems as exploratory analyses.
Method
Participants, Procedures and Design
Participants were 57 young same-sex male couples recruited in the Chicago area (total individual N = 114). Couples were eligible for participating if: (1) both members were assigned male at birth and currently identified as male; (2) both members identified as gay, bisexual or same-sex attracted; (3) both members were at least 18 years of age and one member was between ages 18 and 29; (4) the couple identified one another as primary partners and had been together for at least three months; (5) the couple had engaged in oral or anal sex with one another in the past three months; and (6) both members agreed to audio recording of intervention sessions.
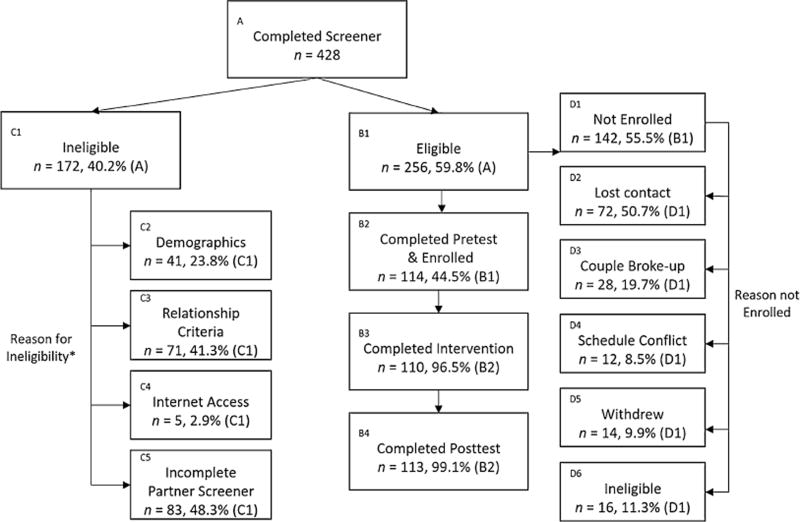
Enrollment for this pilot trial began in January 2015 and lasted for 10 months. Recruitment was conducted through targeted Facebook advertisements, venue-based recruitment (e.g., local Pride events), and recruitment from HIV testing and primary care programs at a local LGBT health care organization. One member of the dyad served as the initial recruit (either online or in-person). If this individual screened preliminarily eligible, he had the option of allowing the research team to reach out to his partner by providing his partner’s contact information (i.e., phone number and/or email) or referring his partner to the online eligibility screener himself. Once both members of the dyad screened preliminarily eligible, each couple was confirmed by study staff, which involved separate phone calls to each partner with a series of questions about their relationship to identify dyads who may be attempting to fake eligiblity (e.g., “Tell me about your first date?”). After completing relationship confirmation, couples completed a pretest assessment, four intervention sessions (two group sessions, two individualized couple sessions) over the course of four weeks, and a posttest assessment at least 2 weeks after intervention completion (i.e., 2 months after the pretest). To evaluate intervention acceptability, individuals completed brief surveys after each intervention session and a semi-structured exit interview after completing the posttest assessment. Figure 2 contains a flowchart illustrating recruitment and retention statistics. The final analytic sample was 114 participants (57 dyads) that completed the pretest and enrolled in the intervention. Participants were paid up to $75, pro-rated for participation level. This study was approved by the institutional review board at Northwestern University.
Fig. 2.
2GETHER participant recruitment process. Note: This figure illustrates the number of individuals at each step of the recruitment process, as opposed to dyads. The total number of dyads that completed pretest and enrolled was 57 (B2). Asterisk reasons for ineligibility were not mutually exclusive
Intervention Description
The primary goal of 2GETHER was to increase couples’ knowledge, motivation, and behavioral skills related to HIV risk reduction in relationships, as well as to improve relationship functioning more broadly (i.e., dyadic communication, coping, and satisfaction). The majority of content was designed through an inductive process in order to ensure its relevance and cultural sensitivity to young same-sex male couples.
2GETHER consisted of four weekly, face-to-face sessions totaling 10 h of content (see Table 1 for an overview). We utilized a hybrid group and individual format, which was specifically requested by couples during our formative research [6]. The first two sessions were psychoeducational groups led by two facilitators and attended by up to 8 couples. In addition to teaching skills, the groups aimed to foster a sense of community and to facilitate learning from other couples’ experiences. Session 1 focused on defining healthy and unhealthy relationship characteristics, teaching effective communication skills, reviewing couples-based sexual health information (including HIV/STI prevention), and discussing strategies for increasing couples’ connectedness by scheduling dates and other activities. Session 2 focused on cognitive-behavioral and acceptance-based strategies for coping with minority stress and relationship stress. Group sessions were highly interactive and content was delivered in diverse formats, including a Prezi presentation, video clips, worksheets, quizzes, facilitated discussion, and role-plays to appeal to different learning styles and to maintain participants’ engagement in the program. Wherever possible, program content depicted examples of same-sex couples, and discussions and role-plays drew from the facilitators’ and participants’ own relationship experiences.
Table 1.
Summary of 2GETHER intervention content
| Topic | Content | Model components |
|---|---|---|
| Session 1 (4 h) | ||
| Orientation | Purpose, structure, and ground rules. Discuss motivations for participation | RELO-IMB constructs |
| Healthy relationships | Discuss healthy and unhealthy relationships, identify similarities and differences between other- and same-sex couples | Information, motivation |
| Communication skills training, part 1 | Review effective/ineffective communication and how individual/couple characteristics impact communication. Communication skills role-play | VSA constructs External stressors, couple processes |
| Sexual health information overview | Discuss sexual health and satisfaction. Review HIV/STI risks for young male couples, discuss behavioral and biomedical prevention. Present decision-making tool to guide condom discontinuation decisions in serious relationships | |
| Pleasurable activities | Discuss importance of pleasurable activities to improve connectedness. Couples practice effective communication skills while planning a date | |
| Session 2 (2.5 h) | ||
| Coping skills training | Review homework (go on date, communication practice). Discuss impact of minority stress and relationship stress on couples’ relationships. Teach various coping strategies and review handling stressors as a couple | VSA constructs Individual vulnerabilities, external stressors, couple processes |
| Problem-solving | Teach couples-based framework for solving problems | |
| Social and community support | Discuss utilizing social and community support to cope with stress | |
| Acceptance | Teach acceptance skills for stressors that cannot be changed | |
| Session 3 (1.5 h) | ||
| Communication skills training, part | Review homework (going on date, communication/problem-solving practice, coping skills). Practice communication and problem-solving with 2 issues | VSA constructions Couple processes |
| Session 4 (2 h) | ||
| Healthy sexuality for couples | Review homework (going on date, communication/problem-solving practice, coping skills). Discuss sexual health in couples. Receive couples-based HIV testing (HIV-negative/unknown), or medication adherence counseling (HIV-positive). Discuss sexual satisfaction and meeting each partner’s sexual needs | RELO-IMB Motivation, behavioral skills |
| Creating a relationship agreement | Discusses relationship agreements, HIV testing and prevention in couples. Negotiate details of relationship agreement using effective communication skills. Discuss potential breaks or changes in agreement | |
| Wrap up | Couple sets goals to improve their relationship and sexual health, anticipate potential lapses in skills, and reflect on lessons learned in 2GETHER |
The final two sessions were skills coaching sessions in which each couple was paired with one facilitator in order to focus on in-depth application of the skills to the individual couple’s circumstances. Sessions also provided a space for the couples to discuss relationship details or concerns that they may have been reluctant to share in the larger group. The first couples’ session (Session 3) focused on applying effective communication and problem-solving skills to two relationship issues identified by the couple. Session 4 focused on each couple’s sexual health, including optimizing each couple’s sexual satisfaction and drafting a relationship agreement to reduce HIV transmission risk within the dyad and with outside partners. Participants who were HIV-negative or unsure of their status were also offered couples-based HIV testing, while a brief medication adherence intervention [48] was administered to participants who were HIV-positive. At the end of each of the four sessions, participants were assigned homework focused on applying the skills learned in the program to their everyday life.
All facilitators participated in a 2-day training and received biweekly group supervision throughout the project. At least one facilitator per group identified as a sexual or gender minority in order to highlight shared experience between facilitators and participants. Facilitators came from diverse educational backgrounds, including individuals with bachelor’s degrees in the social sciences, master’s level clinical trainees, and clinical psychologists. Advanced clinical training was not needed in order to facilitate this intervention.
Measures
Demographics
The demographic questionnaire assessed participants’ age, race/ethnicity, self-reported sexual orientation, self-reported HIV status, and relationship length in months (discrepancies in relationship length were resolved by using the mean response of each member of the couple).
HIV Transmission Risk Behavior
We examined two sexual risk behavior outcomes using the HIV-Risk Assessment of Sexual Partnerships (H-RASP) [51], which retrospectively assesses sexual behavior partner-by-partner during a specified reporting period. First, we calculated the total number of CAS acts in the reporting period by summing the total number of CAS acts across all partners reported in the H-RASP. Second, we calculated the proportion of partners with whom each participant had CAS during the reporting period.
Relationship-Oriented Information, Motivation and Behavioral Skills
We used a questionnaire that was recently validated to measure the Relationship-Oriented Information, Motivation and Behavioral Skills Model (RELO-IMB) among YMSM [45, 52], and we adapted and added several items to measure constructs specific to this intervention trial. The Information construct was measured by 11 items that assessed respondents’ knowledge and beliefs about HIV prevention in a relationship. Four items were taken from Misovich et al. [52] that consisted of incorrect statements followed by five Likert-type response options (1 = strongly agree, 5 = strongly disagree). Response options of “strongly agree” and “agree” were coded as 1 to indicate a correct response and all other responses were coded 0. Given that these items focused primarily on condom use, we added seven information items that assessed knowledge and beliefs about: (a) HIV testing (two items), (b) HIV transmission in couples (three items), and (c) biomedical prevention in couples (2 items). Response options for these additional items were “true,” “false,” and “I don’t know.” Correct responses were coded as 1 and incorrected responses were coded as 0 (“I don’t know” was always coded as incorrect). Consistent with prior recommendations [53], we summed all items to create an 11-item scale, with higher scores reflecting more accurate information.
The motivation construct was measured in several ways. First, we examined subjective norms regarding HIV prevention acts using 10 items that assessed perceived social support for HIV preventive behaviors (e.g., “Most people who are important to me think I should try to persuade my partner to practice only safer sex”) [52]. Items were scored on a 5-point scale (1 = very true, 5 = very untrue), and item responses were reverse-scored such that higher scores indicate more supportive social norms for safer sex. Cronbach’s alpha was 0.80 at pretest and 0.82 at posttest. Next, we created items to assess dyadic motivation to use condoms, receive couples-based HIV testing, use PrEP, and discuss relationship agreements. For each of these preventive behaviors, we administed four items assessing whether participants: (a) feared what their partner would do if they asked to engage in the behavior, (b) believed their partner would not trust the participant if the participant asked to engage in the behavior, (c) believed their partner would think the participant did not trust their partner if the participant asked to engage in the behavior, and (d) believed that asking to engage in the behavior would ruin the mood. Each item was scored on a 5-point Likert-type scale (1 = very unlikely, 5 = very likely), and item responses were reverse-scored such that higher scores indicate more motivation in each domain. Cronbach’s alpha was high across all preventive behavior domains at pretest (range 0.79–0.92) and posttest (range 0.88–0.94).
The Behavioral Skills construct was measured in two ways. First, we utilized nine items from Misovich et al. [52] Perceived Difficulty of HIV Prevention Behaviors scale. This scale assessed participants’ confidence in their ability to engage in preventive behaviors in various contexts (e.g., “How hard would it be for you to use a condom with your partner while under the influence of alcohol or drugs?”) scored on a 5-point Likert-type scale (1 = very hard, 5 = very easy). Cronbach’s alpha was 0.80 at pretest and 0.86 at posttest. Next, we assessed presence and concordance of couples’ relationship agreement, as negotiation of relationship agreements was the primary behavioral skill in this trial. We administered the following self-report item: “Which of the following scenarios best describes the relationship agreement that you and your current partner have?” Response options included: “we cannot have sex with an outside partner,” “we can have sex with outside partners but with some restrictions,” “we can have sex with outside partners without any restrictions,” “we do not have an agreement.” Couples in which both members reported the same agreement type were scored as a 1 while those who were discordant were scored as a 0. If both partners selected “we do not have an agreement,” the couple was coded as discordant because absence of an agreement indicates a lack of understanding of the monogamy or non-monogamy rules in the relationship.
Relationship Outcomes
Relationship satisfaction was measured with three investigator created items (e.g., “How satisfied are you with your partner?”). Response options were on a 7-point scale (1 = extremely dissatisfied, 7 = extremely satisfied). Cronbach’s alpha was high (α = 0.93 at pretest and posttest). Relationship investment was measured with four items from the commitment subscale of the Investment Model Scale (e.g., “Compared to other people I know, I have invested a great deal in my relationship with my partner”). Response options were on a 9-point scale (1 = do not agree at all, 9 = agree completely). Internal consistency was modest for relationship investment (α = 0.55 and 0.50 at pretest and posttest, respectively). Finally, relationship functioning was measured with the Dyadic Adjustment Scale (DAS) [54], a well-validated 32-item scale that assesses the quality of romantic relationships across four domains: satisfaction, cohesion, consensus and affectional expression. The current analyses utilized the full scale score, and Cronbach’s alpha for the full scale was high at both pretest and posttest (α = 0.90 and 0.92, respectively).
Depressive Symptoms
The Patient-Reported Outcomes Measurement Information System (PROMIS) Depression—Short Form 8b [55, 56] instrument was used to assess self-reported negative mood, views of self, and social cognition, as well as decreased positive affect and engagement. This 8-item instrument assesses depressive symptoms over the past seven days. For each symptom, participants respond on a 5-point scale ranging from never (1) to always (5). Cronbach’s alpha was high at both pretest (α = 0.94) and posttest (α = 0.96).
Alcohol Problems
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening tool that assesses consumption, behaviors, and problems related to alcohol in the past 6 months [57]. For the purposes of this study, we adapted the reporting timeframe to the past 2 months in order to align with the pretest and posttest schedule. We used the mean score of the AUDIT, which had strong reliability at pretest and posttest (Cronbach’s α = 0.83 and 0.84, respectively).
Intervention Component Ratings
After each of the four intervention sessions, participants were emailed a link to complete a brief survey assessing the acceptability of each session and intervention component. Acceptability of each session was assessed with the following item: “Overall, I found Session [1–4] useful.” Acceptability of each session component was assessed with the following item: “I found the section on [session component] to be useful.” Each item was rated on a 5-point Likert scale, ranging from strongly disagree (1) to strongly agree (5).
Exit Interview
Participants completed an exit interview via phone after completing the two-week posttest. Participants were asked open-ended questions to assess acceptability of 2GETHER and its various intervention topics. Relevant to the current analyses, participants were asked the following questions: (1) “What was your impression of the program?”; (2) “What did you think was the best part of the program and why?”; (3) “What was your least favorite part of the program and why?” The interview was completed by a member of the research team who did not facilitate any of the participants’ intervention sessions. All interviews were audio recorded and transcribed verbatim.
Analytic Plan
We calculated mean acceptability scores for each session and intervention topic using SPSS 23 software. With regard to the qualitative exit interview data, a member of the research team read all participant responses to the three questions, identified themes that were observed across participants’ answers, and developed a codebook. Another member of the team then reviewed the codebook, disagreements were resolved via consensus, and a final codebook was created. Both team members then coded a randomly selected 20% of the exit interview responses to ensure that themes could be reliably coded. Interrater reliability was high (overall kappa = 0.94; kappa for questions 1, 2, and 3 = 0.89, 0.94, and 1.00, respectively), and the original coder then coded the remaining interviews.
The differences in HIV related outcomes, relationship functioning and other health outcomes (alcohol use, depressive symptoms) from pretest to posttest were tested in SPSS 23 using multilevel repeated measures models and paired-samples t tests. The multilevel repeated measures test is used to control for the similarity between members of the same couple by modeling the variance within couples at the same time as modeling the differences between individuals. The multilevel repeated measures model is equivalent to a paired-samples t test except that it controls for the within-couple similarity. In cases where the within-couple variance is small and the within-couple parameter can be excluded from the model, the results from the repeated measures model are the same as the paired-samples t test. For outcomes where the within-couple parameter was not significant and close to zero, the paired-samples t test was considered the more appropriate test and was run instead.
Results
Feasibility
We recruited a diverse sample (see Table 2) and maintained robust intervention engagement. Mean age of the sample was 26.4 years (SD = 4.55), 14% were aged 30 or older, and about a quarter of couples had an age disparity of at least 5 years. Participants were diverse in terms of race/ethnicity; 48.2% of individuals were racial minorities and 50.9% of the couples were interracial. In terms of HIV status, 11.4% of individuals were HIV-positive. The majority of couples were seroconcordant negative (70.2%). Known serodiscordant couples were 8.8% of the sample, while unknown serodiscordant couples (i.e., at least one individual reported unknown HIV status) were 14%. Seroconcordant positive couples were 7% of the sample. Except for the unknown serodiscordant couples, all couples were mutually aware of one another’s status at baseline. Mean relationship length was 19 months (1.6 years; SD = 1.3 years) and ranged from 3 months to over 6 years. With regard to intervention engagement and study retention, 96.5% of participants completed all intervention sessions. Two couples withdrew after completing Session 1; one due to relationship conflict and one due to scheduling difficulties. All but one participant (99.1%) completed the two week posttest, and 87.7% completed the exit interview.
Table 2.
Demographic characteristics of the cohort (N = 114)
| N | % | |
|---|---|---|
| Individual-level (N = 114) | ||
| Age (M = 26.4; SD = 4.6) | ||
| 18–29 | 98 | 86.0 |
| 30+ | 16 | 14.0 |
| Race/ethnicity | ||
| White | 59 | 51.8 |
| Black/African American | 13 | 11.4 |
| Hispanic/Latino | 27 | 23.7 |
| Asian | 8 | 7.0 |
| Multiracial | 7 | 6.1 |
| Sexual orientation | ||
| Gay | 100 | 87.7 |
| Bisexual | 8 | 7.0 |
| Queer | 6 | 5.3 |
| HIV status | ||
| Negative | 92 | 80.7 |
| Positive | 13 | 11.4 |
| Don’t know | 9 | 7.9 |
| Couple-level (N = 57) | ||
| Relationship length in months (M = 19.0; SD = 16.1) | ||
| Less than 12 months | 27 | 47.4 |
| 12 months or longer | 30 | 52.6 |
| Age concordance | ||
| Less than 5 years difference between partners | 42 | 73.7 |
| 5–9 years difference between partners | 8 | 14.0 |
| 10 years or more difference between partners | 7 | 12.3 |
| Racial/ethnic concordance | ||
| Racial/ethnic concordant | 28 | 49.1 |
| Racial/ethnic discordant | 29 | 50.9 |
| HIV concordance | ||
| Concordant negative | 40 | 70.2 |
| Concordant positive | 4 | 7.0 |
| Known discordant | 5 | 8.8 |
| Unknown discordant | 8 | 12.3 |
“Unknown discordant” couples are couples in which at least one individual reported unknown HIV status
Acceptability
Mean acceptability ratings across intervention sessions ranged from 4.3 to 4.7. Session 3 (individual session, communication skills) received the highest mean score, and paired-samples t tests revealed that this session was rated significantly higher than all other sessions. Session 4 was also rated significantly higher than Sessions 1 and 2, but mean scores did not differ between Sessions 1 and 2. Mean intervention component scores ranged from 4.1 to 4.8. The communication skills and problem-solving practice components of Session 3 received the highest mean score, while the social and community support component of Session 2 received the lowest mean score.
Table 3 summarizes participant responses about acceptability of 2GETHER during the exit interview, as well as frequency of qualitative code applications across participants. Fifty couples (N = 100) completed exit interviews. The majority of participants had a positive impression of the program (93%). One participant stated: “It definitely helped [my partner] and I a lot. The main thing for us was our communication skills. It helped us develop that a bit further so that we would be able to communicate when it came down to debates or arguments or disagreements. And also…it helped us further talk about [our relationship agreement] more in depth so that we both completely understand each other and what exactly it means for us and our relationship.” Although seven participants had a neutral or mixed positive/negative impression (7%), no participants had an entirely negative impression of 2GETHER.
Table 3.
Themes of responses to exit interview questions
| Question | Response theme | Example quote | % (N) |
|---|---|---|---|
| What was your impression of the program? | Positive impression | “It was very good. I actually learned a lot. I definitely gained a lot for myself and for my relationship with my partner and I definitely took different things that I learned and I applied them daily to my relationship.” (28 years old, Black, HIV-positive) | 93.0 (93) |
| Negative impression | N/A | 0.0 (0) | |
| Neutral or mixed impression | “I think being a therapist and already knowing a lot of the material that you guys presented, I just did not fully get the opportunity to learn anything new. That said, there were aspects to the program that I did find beneficial, which were the two sessions, sessions 3 and 4, that we had with [facilitator]. I felt that it sort of allowed us, me and my partner, to talk about issues that we hadn’t previously discussed and to take us a little bit outside of our comfort level and to really have some meaningful conversations about things that needed to be discussed.” (33 years old, White, HIV-negative) | 7.0 (7) | |
| What did you think was the best part of the program? | Communication skills training | “I think communication and how we discussed talking to each other. It pointed out issues that I had with my own communication. It included really good information on how to address anyone I am in a relationship with.” (24 years old, White, HIV-negative) | 61.6 (61) |
| Coping skills training | “I think the problem solving and handling stress were the best parts of the program…there’s the widest range of possibilities. Confronting issues and problem-solving, that’s kind of a very general skill that could be applied in a lot of ways in a relationship.” (19 years old, Latino, unknown HIV-status) | 23.2 (23) | |
| Creating relationship agreement | “I think that talking about relationship agreements was the best, because I think it’s something that usually partners don’t take the time to discuss and really understand what is healthy for them and what their needs are and how those needs get met.” (27 years old, White, HIV-negative) | 20.2 (20) | |
| Individual sessions | “What I liked most about it was the individual sessions…we were really able to end up talking about things within our relationship and talk with each other and it was good to have somebody there to help monitor the way that we communicate and advise us on when we’re not communicating effectively.” (24 years old, White, HIV-negative) | 19.2 (19) | |
| Sexual health information | “Actually, I think the sexual health is because a lot of couples or a lot of people learn about sexual health in school or health class or something and they don’t really cover gay sex or gay health. I found it very informative.” (24 years old, Asian, HIV-negative) | 5.1 (5) | |
| What was your least favorite part of the program? | Nothing | “I can’t say that I have one. I pretty much liked the whole program.” (20 years old, Black, HIV-negative) | 28.3 (28) |
| Sexual health information | “ …the part about sexual health. I think it was great to hear some of the numbers and statistics, because my thoughts about some of it was different than what the actual statistics were. But for me personally it was stuff that I already knew, so it was my least favorite.” (26 years old, Latino, HIV-negative) | 16.2 (16) | |
| Coping skills training | “I would say the problem solving…the way the problem solving was presented was too structured. I don’t think every problem can be resolved in the way that it was structured and taught like that.” (26 years old, White, HIV-negative) | 11.1 (11) | |
| Program logistics | “Probably just the length of the sessions…there’s no topic or information that I didn’t like. It’s just in the group sessions it was hard to stay focused toward the end and keep participating.” (36 years old, White, HIV-negative) | 10.1 (10) | |
| Role playing exercises | “I would say maybe the role playing. It felt kind of like forced a little bit and awkward.” (19 years old, Asian, unknown HIV-status) | 8.1 (8) | |
| Group sessions | “Maybe the group sessions and those awkward moments waiting for somebody to talk.” (24 years old, White, HIV-negative) | 8.1 (8) | |
| Lecture style | “I think my least favorite part of the program was some of the lecture style stuff…” (22 years old, White, HIV-positive) | 6.1 (6) |
For question 1, N = 100 and percentages add up to 100% because participants could only be coded as one response for that question. Percentages may exceed 100% because participants could be coded as more than one response for these questions
For the next two exit interview questions, percentages may exceed 100% because participants could provide multiple responses. Participants most frequently stated that communication skills training was the “best” component of the intervention (61.6%), followed by coping skills training (23.2%), creating a relationship agreement (20.2%), and sexual health information overview (5.1%). In addition to these specific components, 19.2% stated more broadly that the two individual sessions were their favorite part of the intervention. With regard to participants’ “least favorite” parts of the program, the largest proportion (28.3%) did not list a least favorite component, noting that they liked the entire program. Sexual health information overview (16.2%) and coping skills training (11.1%) were the least favorite components. In addition to these specific components, 10.1% noted program logistics (e.g., scheduling sessions, group dynamics) as their least favorite part of the program, 8.1% noted the two group sessions more broadly, 8.1% noted the role playing exercises, and 6.1% noted the lecture style during certain portions of the group sessions. Finally, while we did not specifically ask participants about their facilitators in exit interviews, several spontaneously discussed their impressions of their facilitators. Only one individual noted a mixed impression of a facilitator. Of the several others who noted positive impressions of their facilitators, there was no observable pattern of a preference for facilitators with certain demographic characteristcs (e.g., sexual orientation or gender identity).
Preliminary Efficacy: Intervention Outcomes
First, we examined demographic differences in study variables. Compared to White participants, Latino participants had significantly higher baseline scores on Motivation–Subjective Norms (M = 4.02 vs. M = 3.73, t = 2.11, p < 0.05), and significantly lower scores on both relationship satisfaction (M = 5.79 vs. M = 6.25, t = −2.38, p < 0.05) and functioning (M = 117.44 vs. M = 124.36, t = −2.15, p < 0.05). Black participants scored significantly higher than White participants on both Motivation– Subjective Norms (M = 4.12 vs. M = 3.73, t = 2.17, p < 0.05) and relationship investment (M = 8.03 vs. M = 7.31, t = 2.66, p < 0.01), as well as significantly lower on alcohol problems (M = 3.92 vs. M = 7.12, t = −2.22, p < 0.05). Participants of other racial/ethnic backgrounds had significantly lower scores on Information (M = 66.06 vs. M = 73.65, t = −2.06, p < 0.05). With regard to HIV status, participants of unknown HIV status scored significantly higher than HIV-negative participants on dyadic motivation to use condoms (M = 4.83 vs. M = 4.12, t = 2.24, p < 0.05).
Results for multi-level mixed-effects repeated measures and paired-sample t tests are reported in Table 4. One participant was removed from outcome analyses due to extensive missing data at posttest. Participants reported a significant decrease in the percentage of CAS partners from pretest to posttest (p < 0.05, d = 0.15). Given that the majority of participants reported that they had only had sex with their primary partner at pretest and posttest, we also examined change in the percentage of CAS partners amongst those who had extradyadic partners at either timepoint. Among these participants, we observed a 43% decrease in the percentage of CAS partners from pretest (63% CAS partners) to posttest (36% CAS partners). We observed no change in total CAS acts during the two month reporting period. With regard to RELO-IMB constructs, participants scored significantly higher on Information (p < 0.001, d = 0.64) from pretest to posttest. We also observed significant increases in Motivation–Subjective Norms (p < 0.05, d = 0.23), dyadic motivation to use PrEP (p < 0.05, d = 0.17), and a marginal decrease in dyadic motivation to use condoms (p = 0.08, d = 0.17) at posttest. There were no significant changes in dyadic motivation to create a relationship agreement or receive couples-based HIV testing. In terms of Behavioral Skills, there was significant improvement in couples’ concordance in sexual agreement type from pretest to posttest (p < 0.001, d = 0.66), such that only 1.8% of individuals (one couple) were disconcordant in their report of their relationship agreement type at posttest (24.6% of individuals were discordant at pretest). We observed no change in the HIV Prevention Behaviors Perceived Difficulty scale.
Table 4.
Multi-level mixed effects repeated measures and paired-samples t tests for primary outcomes
| Pretest mean | Posttest mean | t | p-value | Effect size (d) | |
|---|---|---|---|---|---|
| HIV-related outcomes | |||||
| Sexual risk | |||||
| % Condomless anal sex partnersa | 90% | 86% | −2.18 | 0.032 | 0.15 |
| Total number of condomless anal sex actsb | 14.36 | 14.55 | 0.14 | 0.888 | 0.01 |
| Information, motivation, behavioral skills | |||||
| Informationb | 73.85 | 82.06 | 5.50 | 0.000 | 0.64 |
| Motivation | |||||
| Subjective normsb | 3.82 | 3.96 | 2.46 | 0.017 | 0.23 |
| Condom usea | 4.22 | 4.04 | 1.79 | 0.076 | 0.17 |
| Relationship agreementa | 4.40 | 4.48 | 0.83 | 0.406 | 0.09 |
| Couples-based HIV testinga | 4.70 | 4.77 | 0.97 | 0.335 | 0.12 |
| PrEP useb | 4.02 | 4.28 | 2.03 | 0.047 | 0.17 |
| Behavioral skills | |||||
| Barriers to preventionb | 3.91 | 3.98 | 1.10 | 0.276 | 0.11 |
| Relationship agreement concordanceb | 0.77 | 0.98 | 5.24 | 0.000 | 0.66 |
| Relationship-related outcomes | |||||
| Investmenta | 7.40 | 7.62 | 2.97 | 0.004 | 0.26 |
| Satisfactiona | 6.18 | 6.26 | 1.03 | 0.307 | 0.10 |
| Dyadic adjustment scaleb | 123.24 | 122.89 | −0.33 | 0.744 | 0.03 |
| Other health-related outcomes | |||||
| Depressive symptomsb | 14.27 | 14.04 | −0.47 | 0.641 | 0.04 |
| Alcohol problemsb | 6.25 | 5.73 | −1.79 | 0.078 | 0.11 |
Variability in sample size for each scale is due to missingness
Paired-samples t test
Multi-level mixed effects repeated measures
With regard to relationship outcomes, relationship investment significantly increased from pretest to posttest (p < 0.01, d = 0.27). Relationship satisfaction and relationship functioning scores did not show significant change. Finally, we measured alcohol problems and depressive symptoms as exploratory health outcomes given the demonstrated effects of relationship education on these outcomes. We observed a marginal decrease in alcohol problems (p = 0.08, d = 0.11) at posttest, but there were no differences in depressive symptoms. Of note, we re-ran all analyses while adjusting for relationship length, as it is possible that relationship length is associated with study outcomes. The pattern of findings (including p-values) remained unchanged, and changes in effect sizes were negligible.
Discussion
This pilot study found promising evidence of the feasibility, acceptability and preliminary efficacy of the 2GETHER couples-based HIV prevention and relationship education intervention. We were able to recruit a diverse sample of young same-sex male couples and maintain robust engagement in the intervention. 2GETHER also received high acceptability ratings from participants, both in quantitative post-session evaluations and in qualitative semi-structured exit interviews. Finally, we found evidence of preliminary efficacy of the intervention, including decreases in HIV risk behavior, increases in relationship-oriented information, motivation and behavioral skills related to HIV prevention, and improvement in relationship investment. We did not observe significant improvement in other indicators of relationship functioning, including satisfaction and relationship functioning (as measured by the Dyadic Adjustment Scale; [54]), but high mean scores on these constructs at baseline may have caused ceiling effects that prevented observation of change. These findings indicate that couples-based interventions may be an effective strategy for reducing new HIV infections among YMSM and improving relationship health. The next step in the evaluation of 2GETHER will be to conduct a larger randomized controlled trial to establish intervention efficacy.
With regard to feasibility, we were able to efficiently recruit a sample that was diverse in terms of race/ethnicity, HIV status, and relationship duration. First, nearly half of the sample was racial or ethnic minorities, with good representation of Hispanic/Latino (23.7%) and Black participants (11.4%). Furthermore, 11.4% of our sample was HIV-positive and an additional 7.9% were unaware of their HIV status, which led to adequate representation of seroconcordant HIV-negative couples, seroconcordant HIV-positive couples and serodiscordant couples. Couples in this sample were also diverse in terms of relationship duration. On average, couples had been together for 19 months, with a range of 3 months to more than 6 years. While it was not possible to conduct subgroup analyses in this pilot study to determine differential intervention effects, future trials should strive to recruit even larger percentages of racial minorities and HIV positive individuals in order to conduct such analyses. This may be achieved by embedding recruitment activities in local community centers, behavioral health services, and primary care facilities that serve the LGBT community, all of which we began to pilot (with limited resources) in this trial. Finally, we were able to maintain robust intervention engagement; 96.5% of participants completed all intervention sessions and 99.1% completed the two-week posttest. Together, these data indicate that diverse YMSM are interested in couples-based services and are able to maintain high engagement over an approximate two-month study period.
In addition to evidence of feasibility, our post-session evaluation and exit interview data indicate high levels of acceptability of 2GETHER to our study population. In post-session evaluations, all intervention sessions and components received mean scores above four, which indicated that the majority of participants “agreed” or “strongly agreed” that the sessions and topics were helpful. In exit interviews, 93% reported having a positive experience in the intervention (0% reported an entirely negative experience). A large majority reported that the communication skills training was their favorite topic of 2GETHER, followed by coping skills training and creating a relationship agreement, and importantly, these components map onto the hypothesized mechanisms of change in 2GETHER. In other words, the VSA model of relationship functioning hypothesizes that couples need to learn to cope with stress and communicate more effectively in order to improve relationship health. Extended to HIV transmission risk, improvements in these domains would facilitate more effective negotiation of relationship agreements, which in turn would reduce HIV transmission risk behavior.
The largest proportion of participants stated that they did not have a least favorite part of 2GETHER (28.1%). Participants’ least favorite components were sexual health information and coping skills training. Feedback during exit interviews indicated participants felt the information provided in these components was too basic and was not tailored to couples-specific information. Additionally, a minority of participants noted that the role-playing exercises and lecture style during group sessions was their least favorite. This indicates that young male couples may prefer more discussion-based and interactive activities, rather than traditional psychoeducation and role-playing activities that are common in behavioral interventions. In fact, the sexual health information and coping skills training sections were primarily lecture-based, which may explain why some participants liked these components the least. In future iterations of 2GETHER, we plan to provide more couples-specific information in these sections, as well as to incorporate more small-group discussion. Regardless, as a whole these qualitative findings indicate that integrated relationship education and HIV prevention content is appealing to YMSM in relationships and viewed as relevant to their experiences.
Our pilot trial also found strong evidence of preliminary efficacy in changing target outcomes and some hypothesized mediators of change. Our integrated IMB and VSA theoretical model hypothesized that 2GETHER would reduce HIV transmission risk behavior by nature of both: (a) improving relationship functioning; and (b) facilitating change in RELO-IMB constructs related to HIV. With regard to HIV-related outcomes, we saw significant reduction in the proportion of partners with whom participants had CAS from pretest to posttest, particularly amongst those who reported multiple sexual partners (43% decrease). We also saw significant increases in Information, Motivation (subjective norms of HIV prevention, dyadic motivation to use PrEP), and Behavioral Skills (significant increase in dyadic concordance on relationship agreement type). Interestingly, we observed a marginal decrease in motivation to use condoms, which may be explained by the significant increase in motivation to use PrEP. These findings indicate that condom use alone may not be a realistic HIV prevention approach for many couples, and couples-based interventions provide a unique opportunity to develop an integrated biomedical and behavioral HIV prevention plan for maintaining the health of the dyad.
In sum, these preliminary efficacy findings indicate that 2GETHER adequately facilitates improvement in many of the RELO-IMB constructs assessed in this trial and therefore reductions in HIV transmission risk, though we note that effect sizes were generally larger for RELO-IMB constructs than for sexual behavior change. Given that a two-month reporting window does not allow for substantial change in behaviors that may occur infrequently (e.g., sex with outside partners), future research should measure behavior change over a longer follow-up period. It may also be that certain couples benefit more from this type of intervention than others, which should be further evaluated. However, the fact that we were able to observe significant change in sexual risk in such a short period of time, particularly when we did not selectively enroll participants who had engaged in risk behavior at pretest, provides strong evidence for 2GETHER’s potential to lead to meaningful behavior change.
Our pilot trial also observed significant increases in relationship investment, but we note that internal consistency of the relationship investment scale was low, so this finding may not be reliable. We saw no change in relationship satisfaction or relationship functioning. However, we did not measure communication skills specifically in this trial, which is one of our hypothesized mediators of change. Instead, we chose to administer the Dyadic Adjustment Scale, which provides a broader assessment of general relationship functioning, and we observed no change in the total score or any of the subscales at post-test. Interestingly, pretest assessment of the constructs indicated very high mean scores on satisfaction and functioning with restricted variance across participants, so we may not have been able to observe significant change due to ceiling effects. While 2GETHER may be facilitating greater investment in relationships, future evaluations of the intervention should strive to recruit samples that are more diverse in terms of satisfaction and adjustment.
Alternatively, it is possible that young couples overestimate their satisfaction and relationship functioning in traditional self-report measures. Indeed, some evidence suggests that among heterosexual adolescent and young adult couples, the negative association between relationship conflict and satisfaction is much weaker than in adult relationships [58]. Indeed, the largest proportion of couples in this trial noted that the communication skills section was their favorite part of the program and that 2GETHER helped them to communicate more effectively and feel closer as a couple. To address these possible measurement issues, future evaluations of 2GETHER and other couples programs could utilize more nuanced approaches to assessing relationship adjustment and skills, such as observational approaches in which couples are asked to discuss an area of conflict and trained observers code their interaction.
Finally, we observed a marginal decrease in alcohol problems from pretest to posttest. While alcohol use was not specifically a target in this intervention, it was frequently endorsed as an area of conflict between partners during intervention sessions. Facilitating partner communication about alcohol and drug use could lead to significant reductions in substance use problems if more targeted intervention content is developed, and we plan to add substance use risk reduction content to future iterations of 2GETHER. This is a particularly important future avenue of intervention given that MSM use substances at higher rates than heterosexuals [41, 59], and alcohol and drug use in the context of sex have been found to predict CAS, particularly in serious relationships [17, 18].
We acknowledge certain limitations to this study. In this pilot trial, we utilized a pretest posttest design in which all participants received the intervention. Without a randomized controlled trial, it is not possible to know whether the intervention components caused the changes we observed. Future evaluations should compare 2GETHER to an attention-matched control condition to more confidently draw these conclusions. Further, we were able to recruit and engage a diverse sample in terms of race/ethnicity, HIV status, and relationship duration, but we were not powered to conduct subgroup analyses to determine differential intervention effects across groups. Finally, HIV transmission risk variables may not be directly comparable for HIV-negative and HIV-positive individuals. Larger efficacy trials of couples-based programs should enroll sufficient numbers of HIV-positive individuals to conduct analyses specific to that group.
Despite these limitations, this study demonstrates compelling evidence for the feasibility, acceptability and preliminary efficacy of the 2GETHER HIV prevention and relationship education program for young same-sex male couples. Given the large proportion of new HIV infections attributed to main partnerships among YMSM, it is critically important that we develop couples-based intervention strategies in order to curb HIV incidence. Furthermore, as biomedical approaches to prevention continue to grow in their use, prevention programs must adapt, and programs that integrate primary and secondary prevention allow for all individuals (regardless of HIV status) to learn how to prevent transmission of HIV. Finally, developing programs that focus on the broader physical and emotional health of YMSM, such as relationship education services, is an innovative strategy for reinvigorating HIV prevention, and these types of programs are appealing to community based organizations that strive to address the multiple health and wellness needs of the LGBT community.
Acknowledgments
This research was supported by a grant from the Sexualities Project at Northwestern (PI: M. Newcomb). Michael Newcomb’s time was also supported in part by a grant from the National Institute on Drug Abuse (DP2DA042417; PI: M. Newcomb). We would like to acknowledge the various individuals who served as facilitators for this project (in addition to the authors): Ryan Coventry, David Drustrup, John Frank, Kelsey Howard, Darnell Motley, Jae A. Puckett, and Tyson Reuter. We would also like to acknowledge Samuel McMillen and Brian Mustanski for their support. Finally, we would like to thank the couples that participated in this study for their time.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors do not have any conflicts of interest to report.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Participants provided their consent/assent to participate in the study.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance—Men Who Have Sex with Men. 2016 [Google Scholar]
- 2.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE. 2012;7:e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–62. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 4.Safren SA, Blashill AJ, O’Cleirigh CM. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS Behav. 2011;15(Suppl 1):S30–4. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rowniak S. Safe sex fatigue, treatment optimism, and serosorting: new challenges to HIV prevention among men who have sex with men. J Assoc Nurses AIDS Care. 2009;20:31–8. doi: 10.1016/j.jana.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Greene GJ, Fisher KA, Kuper L, Andrews R, Mustanski B. “Is this normal? Is this not normal? There’s no set example”: sexual health intervention preferences of LGBT youth in romantic relationships. Sex Res Social Policy. 2015;12:1–14. doi: 10.1007/s13178-014-0169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30:597–605. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43:61–72. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: the P18 Study. AIDS Educ Prev. 2015;27:112–25. doi: 10.1521/aeap.2015.27.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greene GJ, Andrews R, Kuper L, Mustanski B. Intimacy, monogamy, and condom problems drive unprotected sex among young men in serious relationships with other men: a mixed methods dyadic study. Arch Sex Behav. 2014;43:73–87. doi: 10.1007/s10508-013-0210-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitchell JW, Petroll AE. Patterns of HIV and sexually transmitted infection testing among men who have sex with men couples in the United States. Sex Transm Dis. 2012;39:871–6. doi: 10.1097/OLQ.0b013e3182649135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chakravarty D, Hoff CC, Neilands TB, Darbes LA. Rates of testing for HIV in the presence of serodiscordant UAI among HIV-negative gay men in committed relationships. AIDS Behav. 2012;16:1944–8. doi: 10.1007/s10461-012-0181-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. HIV among gay and bisexual men: CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of HIV/AIDS Prevention. 2015 [Google Scholar]
- 14.Mustanski B, Newcomb M, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–53. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bingham TA, Harawa NT, Johnson DF, et al. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999–2000. AIDS Educ Prev. 2003;15:39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- 16.Mustanski B, Newcomb ME. Older sexual partners may contribute to racial disparities in HIV among young men who have sex with men. J Adolesc Health. 2013;52:666–7. doi: 10.1016/j.jadohealth.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newcomb ME, Mustanski B. Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS Behav. 2014;18:1981–90. doi: 10.1007/s10461-014-0766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- 19.Grov C, Starks TJ, Rendina HJ, Parsons J. Rules about casual sex partners, relationship satisfaction, and HIV risk in partnered gay and bisexual men. J Sex Marital Ther. 2014;40:105–22. doi: 10.1080/0092623X.2012.691948. [DOI] [PubMed] [Google Scholar]
- 20.Hoff CC, Beougher SC. Sexual agreements among gay male couples. Arch Sex Behav. 2010;39:774–87. doi: 10.1007/s10508-008-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoff CC, Beougher SC, Chakravarty D, Darbes LA, Neilands TB. Relationship characteristics and motivations behind agreements among gay male couples: differences by agreement type and couple serostatus. AIDS Care. 2010;22:827–35. doi: 10.1080/09540120903443384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitchell JW. Characteristics and allowed behaviors of gay male couples’ sexual agreements. J Sex Res. 2014;51:316–28. doi: 10.1080/00224499.2012.727915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsons JT, Starks TJ. Drug use and sexual arrangements among gay couples: frequency, interdependence, and associations with sexual risk. Arch Sex Behav. 2014;43:89–98. doi: 10.1007/s10508-013-0237-3. [DOI] [PubMed] [Google Scholar]
- 24.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Curr Opin HIV AIDS. 2012;7:99–105. doi: 10.1097/COH.0b013e32834f5cf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newcomb ME, Mongrella MC, Weis B, McMillen SJ, Mustanski B. Partner disclosure of PrEP use and undetectable viral load on geosocial networking apps: frequency of disclosure and decisions about condomless sex. J Acquir Immune Defic Syndr. 2016;71:200–6. doi: 10.1097/QAI.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Bassel N, Witte SS, Gilbert L, et al. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93:963–9. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiwatram-Negron T, El-Bassel N. Systematic review of couple-based HIV intervention and prevention studies: advantages, gaps, and future directions. AIDS Behav. 2014;18:1864–87. doi: 10.1007/s10461-014-0827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macapagal K, Greene GJ, Rivera Z, Mustanski B. “The best is always yet to come”: relationship stages and processes among young LGBT couples. J Fam Psychol. 2015;29:309–20. doi: 10.1037/fam0000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagenaar BH, Christiansen-Lindquist L, Khosropour C, et al. Willingness of US men who have sex with men (MSM) to participate in Couples HIV Voluntary Counseling and Testing (CVCT) PLoS ONE. 2012;7:e42953. doi: 10.1371/journal.pone.0042953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan PS, Stephenson R, Grazter B, et al. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework. Springerplus. 2014;3:249. doi: 10.1186/2193-1801-3-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen S, Meinzen-Derr J, Kautzman M, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17:733–40. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization. Guidance on couples HIV testing and counselling including antiretroviral therapy for treatment and prevention in serodiscordant couples. Geneva: WHO; 2012. [PubMed] [Google Scholar]
- 34.Purcell DW, Mizuno Y, Smith DK, et al. Incorporating couples-based approaches into HIV prevention for gay and bisexual men: opportunities and challenges. Arch Sex Behav. 2014;43:35–46. doi: 10.1007/s10508-013-0205-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Markman HJ, Rhoades GK. Relationship education research: current status and future directions. J Marital Fam Ther. 2012;38:169–200. doi: 10.1111/j.1752-0606.2011.00247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawkins AJ, Blanchard VL, Baldwin SA, Fawcett EB. Does marriage and relationship education work? A meta-analytic study. J Consult Clin Psychol. 2008;76:723–34. doi: 10.1037/a0012584. [DOI] [PubMed] [Google Scholar]
- 37.Buzzella BA, Whitton SW, Tompson MC. The initial evaluation of a relationship education program for male same-sex couples. Couple Family Psychol. 2012;14:306–22. [Google Scholar]
- 38.Whitton SW, Weitbrecht EM, Kuryluk AD, Hutsell DW. A randomized waitlist-controlled trial of culturally sensitive relationship education for male same-sex couples. J Fam Psychol. 2016;30:763–8. doi: 10.1037/fam0000199. [DOI] [PubMed] [Google Scholar]
- 39.Lewis MA, Butterfield RM. Social control in marital relationships: effect of one’s partner on health behaviors. J Appl Soc Psychol. 2007;37:298–319. [Google Scholar]
- 40.Waite LJ, Gallagher M. The case for marriage: why married people are happier, healthier, and better off financially. New York: Doubleday; 2000. [Google Scholar]
- 41.Talley AE, Hughes TL, Aranda F, Birkett M, Marshal MP. Exploring alcohol-use behaviors among heterosexual and sexual minority adolescents: intersections with sex, age, and race/ethnicity. Am J Public Health. 2014;104:295–303. doi: 10.2105/AJPH.2013.301627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bostwick WB, Meyer I, Aranda F, et al. Mental health and suicidality among racially/ethnically diverse sexual minority youths. Am J Public Health. 2014;104:1129–36. doi: 10.2105/AJPH.2013.301749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 44.Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: evidence and possible underlying psychological processes. Rev Gen Psychol. 1997;1:72–107. [Google Scholar]
- 45.Macapagal K, Greene GJ, Andrews R, Mustanski B. Evaluating the Relationship-Oriented Information, Motivation, and Behavioral Skills Model of HIV preventive behaviors in young men who have sex with men. AIDS Educ Prev. 2016;28:165–79. doi: 10.1521/aeap.2016.28.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karney BR, Bradbury TN. The longitudinal course of marital quality and stability: a review of theory, method, and research. Psychol Bull. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- 47.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–97. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Safren S, Otto MW, Worth JL. Life-steps: applying cognitive behavioral therapy to HIV medication adherence. Cogn Behav Pract. 1999;6:332–41. [Google Scholar]
- 49.Smith NG, Hart TA, Moody C, et al. Project PRIDE: a cognitive-behavioral group intervention to reduce HIV risk behaviors among HIV-negative young gay and bisexual men. Cogn Behav Pract. 2016;23:398–411. [Google Scholar]
- 50.Yadavaia JE, Hayes SC, Vilardaga R. Using acceptance and commitment therapy to increase self-compassion: a randomized controlled trial. J Context Behav Sci. 2014;3:248–57. doi: 10.1016/j.jcbs.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mustanski B, Starks T, Newcomb ME. Methods for the design and analysis of relationship and partner effects on sexual health. Arch Sex Behav. 2014;43:21–33. doi: 10.1007/s10508-013-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Misovich SJ, Fisher WA, Fisher JD. A measure of AIDS prevention information, motivation, behavioral skills, and behavior. In: Davis C, Yarber R, Bauserman R, et al., editors. Handbook of sexuality-related measures. Thousand Oaks, CA: SAGE; 1998. pp. 328–37. [Google Scholar]
- 53.Janulis P, Newcomb ME, Sullivan P, Mustanski B. Evaluating HIV knowledge questionnaires among men who have sex with men: a multi-study item response theory analysis. Arch Sex Behav. doi: 10.1007/s10508-016-0910-4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. [Google Scholar]
- 55.Choi SW, Schalet B, Cook KF, Cella D. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess. 2014;26:513–27. doi: 10.1037/a0035768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18:263–83. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 58.Levesque RJR. The romantic experience of adolescents satisfying love relationships. J Youth Adolesc. 1992;22:219–51. [Google Scholar]
- 59.Newcomb ME, Birkett M, Corliss HL, Mustanski B. Sexual orientation, gender, and racial differences in illicit drug use in a sample of US high school students. Am J Public Health. 2014;104:304–10. doi: 10.2105/AJPH.2013.301702. [DOI] [PMC free article] [PubMed] [Google Scholar]