Abstract
We reviewed research regarding system- and visit-level strategies to enhance clinical preventive service delivery and quality for adolescents and young adults. Despite professional consensus on recommended services for adolescents, a strong evidence base for services for young adults, and improved financial access to services with the Affordable Care Act’s provisions, receipt of preventive services remains suboptimal. Further research that builds off successful models of linking traditional and community clinics is needed to improve access to care for all youth. To optimize the clinical encounter, promising clinician-focused strategies to improve delivery of preventive services include screening and decision support tools, particularly when integrated into electronic medical record systems and supported by training and feedback. Although results have been mixed, interventions have moved beyond increasing service delivery to demonstrating behavior change. Research on emerging technology—such as gaming platforms, mobile phone applications, and wearable devices—suggests opportunities to expand clinicians’ reach; however, existing research is based on limited clinical settings and populations. Improved monitoring systems and further research are needed to examine preventive services facilitators and ensure that interventions are effective across the range of clinical settings where youth receive preventive care, across multiple populations, including young adults, and for more vulnerable populations with less access to quality care.
Adolescence and young adulthood bring opportunities and challenges for improving health and preventing disease in the short and long term [1]. The psychological, physical, and social role changes—shaped by social determinants and other risk and protective factors—affect health-related behavior. The life course framework posits that health is a trajectory in which early events and influences shape outcomes throughout the lifespan [2]. Transitional periods, when individuals can be particularly sensitive to environmental inputs, assume a critical role in this framework. Although the life course framework has mostly been applied to early childhood, it also suggests that improving adolescent and young adult health is critical as adolescent and young adult behaviors, and the social and biological contexts shaping those, lay the foundation for future health behaviors and outcomes (Figure 1) [3,4]. Behaviors often initiated during adolescence, such as substance use, high-risk sexual behavior, and risky driving, contribute to poor health outcomes and mortality during adolescence and later life; in addition, almost 20% of adolescents experience impairment due to behavioral and mental health disorders [5,6]. Young adults fare worse than adolescents in many areas, with rates of motor vehicle deaths, homicide, substance use, sexually transmitted infections, and mental health problems peaking during young adulthood [6].
Figure 1.
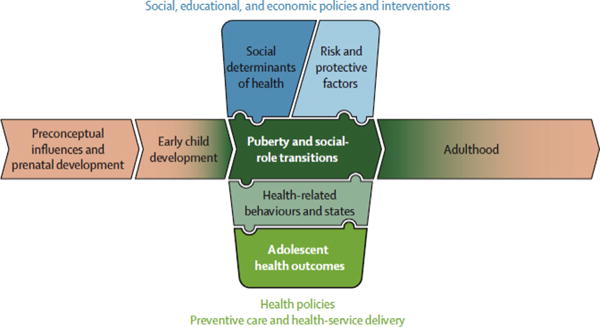
The framework emphasizes the crucial importance of a life course perspective in the understanding of adolescent health and development (represented by the horizontal flow of the framework) and the importance of social determinants of health (vertical flow). The axes intersect around the unique characteristics of adolescence (the complex interactions between puberty, neurocognitive maturity, and social role transitions) to emphasize how these factors affect adolescent health and development. The text outside the boxes refers to settings and scope of policies, preventive interventions, and services that affect adolescent health. From Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: A foundation for future health. Lancet 2012;379:1630–40.
Emerging evidence suggests that puberty and the broader period of adolescent brain development present a unique window of opportunity for social experiences to shape neural systems in enduring ways [7–9]. This developmental science research offers additional insight into the opportunities for preventive intervention and the nature of health risks during adolescence and early adulthood. The health care system can play a key role in supporting adolescents and young adults (AYAs) and their parents with healthy developmental transitions [10]. Optimizing clinical encounters to deliver effective preventive interventions to this age group may yield dividends in the near term and across the life course.
Clinical preventive services
The World Health Organization has set broad guidelines and standards for “youth-friendly care” that aims to make health care services and systems accessible, acceptable, equitable, appropriate, and effective for young people [11,12]. Primary care visits represent a key opportunity for preventive screening and intervention, and a broad consensus for clinical preventive services for adolescents has emerged in the United States since the 1990s [13,14]. The Bright Futures guidelines from the American Academy of Pediatrics provide comprehensive preventive care recommendations for youth up to age 21 years [15], and the forthcoming edition includes greater focus on the social determinants of health [16]. The guidelines generally focus on an annual well visit to a primary care provider where clinicians can screen for risky behavior and reinforce healthy behaviors, strengths, and competencies. Professional recommendations for an annual adolescent visit were first issued by the American Medical Association in 1994 [17]. In 2011, rates of attending an annual visit ranged from 43% to 74% among adolescents aged 10–17 years and 26% to 58% among young adults aged 18–25 years, according to an analysis of national surveillance systems. This analysis yielded significantly higher rates of preventive visits among insured AYAs across all data sources [18]. Confidentiality for adolescent care, when appropriate and ensured by law, is recommended, as is parental guidance and engagement consistent with the need for confidential care [11,15,17,19,20]. Currently, the evidence supporting the efficacy of recommended clinical preventive services varies across services, according to the U.S. Preventive Services Task Force (USPSTF) ratings [21,22].
From a life course perspective, young adulthood (ages 18–25 years) is distinct from adolescence, bringing greater autonomy and unique health-related vulnerabilities [23,24]. However, there are currently no comprehensive preventive care guidelines developed specifically for young adults. Bright Futures covers up to 21 years of age and thus intersects with the young adult age group; guidelines from other professional organizations are also relevant to young adults. Several recommended preventive services in these guidelines have sufficient evidence to warrant a USPSTF recommendation [25]; indeed, the evidence is stronger for clinical preventive services among young adults (≥18 years) than for adolescents (Table 1). However young adults’ range of medical service sources is a challenge for the consistent delivery of preventive services. Although young adults obtain care from several specialties, including internal and family medicine, obstetrics, gynecology, emergency medicine, and pediatrics, they typically do not represent a priority focus for any of these specialties [26,27].
Table 1.
Services covered by the Affordable Care Act, by guideline source
| Measure | USPSTF <18 | USPSTF ≥18 | Bright futures | HRSA Women’s Guidelines |
|---|---|---|---|---|
| Nutrition/exercise/obesity | ||||
| Obesity/body mass index | ✓>6 y | ✓All adults | ✓ | ✓All adults and children |
| Hypertension/blood pressure | — | ✓≥18 y | ✓ | “Covered in child well visit” |
| Lipid disorder | — | ✓≥20 y and risk factors | ✓In late adolescence | ✓Children and adults with risk factors |
| Healthy diet | — | ✓Adults with risk factors | ✓ | ✓Adults with risk factors |
| Routine counseling for physical activity | — | — | ✓ | — |
| Substance use | ||||
| Tobacco use | ✓School-aged children and adolescents | ✓Adults, including pregnant women who use tobacco >18 | After risk assessment | ✓All adults and cessation interventions for tobacco users |
| Alcohol use | NR | ✓All adults | After risk assessment | ✓Adults and adolescents |
| Mental health | ||||
| Suicide screening | NR | NR | ✓ | — |
| Screening for depression | ✓12–18 y, screening for major depressive disorder should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up. | ✓Adults, including pregnant and postpartum women. Screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up. | ✓ | ✓Adults and adolescents |
| Other illicit drug use (screening and counseling) | NR | NR | After risk assessment | — |
| Safety/violence | ||||
| Family/partner violence | ✓Women of childbearing age | ✓Women of childbearing age | ✓ | ✓All women |
| Fighting | — | — | ✓ | — |
| Helmets | — | — | ✓ | — |
| Seat belts | — | — | ✓ | — |
| Guns | — | — | ✓ | — |
| Bullying | — | — | ✓ | — |
| Reproductive health | ||||
| STI screening | ✓Sexually active adolescents and adults at increased risk | ✓Sexually active adolescents and adults at increased risk | ✓If sexually active | ✓Adults and adolescents with risk factors |
| STI counseling | ✓Sexually active adolescents and adults at increased risk | ✓Sexually active adolescents and adults at increased risk | ✓If sexually active | ✓Adults and adolescents with risk factors |
| Cervical cancer screening | — | ✓≥21, every 3 years | ✓If sexually active within 3 years of onset of sexual activity or no later than age 21 | ✓Sexually active women |
| Chlamydia screening (female) | ✓Sexually active ≤24 y | ✓Sexually active ≤24 y | ✓If sexually active | ✓Younger women and other women with risk factors |
| Chlamydia screening (male) | NR | NR | Screen in sexually active adolescents | — |
| Gonorrhea screening | ✓Sexually active ≤24 y | ✓Sexually active ≤24 y | ✓If sexually active | ✓Women at increased risk |
| HIV screening | ✓Adolescents and adults (16–65 y) at increased risk for HIV infection | ✓Adolescents and adults (16–65 y) at increased risk for HIV infection | ✓If sexually active and + on risk assessment | ✓Anyone 15 to 65 y at least once |
| Syphilis screening | ✓All persons at increased risk for syphilis infection | ✓All persons at increased risk for syphilis infection | ✓If sexually active and + on risk assessment | ✓Women at increased risk |
| Pregnancy | — | — | ✓Sexually active females w/o contraception, late menses, amenorrhea, or heavy or irregular bleeding | — |
| Birth control methods | — | — | ✓ | Most insurance plans must cover birth control that is prescribed by a woman’s doctor |
| Screening | ||||
| Testicular cancer | Recommended against | Recommended against | ✓In late adolescence | — |
| Anemia test | — | — | After risk assessment | ✓Routinely for pregnant women |
| Tuberculosis test | Update in progress | Update in progress | After risk assessment | ✓Children at high risk of tuberculosis |
| Hearing test: audiometry | — | — | After risk assessment | — |
| Vision test: Snellen test | — | — | ✓ln each stage of adolescence | ✓Children of all ages |
|
| ||||
| Immunizations As Recommended By the CDC | 11–12 | 13–18 | 19–26 | |
|
| ||||
| Tetanus, diphtheria, pertussis (Tdap/TD) | * | Catch up | Substitute one-time dose of Tdap for Td booster; then boost with Td every 10 y | |
| Human papillomavirus | *** | Catch up | ***For males if risk factor present or as catch up. ***For females as catch up only | |
| MCV4 (Meningococcal) | * | Booster at age 16 or catch up | *Or more if risk factor is present | |
| HepB (Hepatitis B) | Catch up | Catch up | ***If risk factor is present | |
| Polio | Catch up | Catch up | ***If at increased risk of exposure to poliovirus or who have never been vaccinated against polio | |
| MMR (measles, mumps, rubella) | Catch up | Catch up | * Or **doses if risk factor present or as catch up | |
| Varicella (chickenpox) | Catch up | Catch up | **If risk factor is present | |
| Hepatitis A | Catch up For those meeting CDC’s risk criteria |
Catch up For those meeting CDC’s risk criteria |
**If risk factor is present | |
| Pneumococcal (polysaccharide) | For those meeting CDC’s risk criteria | For those meeting CDC’s risk criteria | For those meeting CDC’s risk criteria | |
| Influenza | Recommended annually | Recommended annually | Recommended annually | |
*, **, *** denote number of doses.
NR = insufficient evidence to recommend for or against; Recommend Against = recommend against; USPSTF = U.S. Preventive Services Task Force; y = years; ✓ = a recommendation; – = No mention of recommendation.
Adapted from Centers for Disease Control and Prevention. 2015 Recommended Immunizations for Children from 7 through 18 years old. http://www.cdc.gov/vaccines/who/teens/downloads/parent-version-schedule-7-18yrs.pdf.
The 2010 Patient Protection and Affordable Care Act (ACA) includes provisions that aim to increase delivery of preventive services to AYAs. The ACA requires that private insurers cover selected preventive services with no out-of-pocket cost, including services drawn from Bright Futures [28], the USPSTF recommendations [21], immunizations recommended by the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices [29], and the women’s preventive health guidelines issued by the Health Resources and Services Administration [30] (Table 1).
Estimates of receipt of clinical preventive services among AYAs, based on clinician [31–33] and patient/caregiver report [34–39], suggest suboptimal levels. Only 40% of sexually active 15- to 21-year-old females reported receiving a chlamydia test in the prior year (2006–2010 data [40]), and only 66% of pediatricians in a 2012 national survey reported counseling most of their adolescent patients about tobacco use [41]. A chart review study showed a higher rate of screening for hypertension (76%, 2007–2010 data) within preventive visits for H- to 21-year-olds [42]. Limited research on young adults, utilizing both clinician and young adult report in national and state-wide surveys, shows even lower rates of receipt of preventive services than for adolescents [23,24,43–46], although data were mostly collected before ACA implementation.
Given the opportunities for improving the receipt of preventive services presented by the ACA and the increasing recognition of developmental and contextual factors on health, clinical preventive services are a major focus of the Adolescent and Young Adult Health Research Network established in 2014 by the Maternal and Child Health Bureau within the U.S. Health Resources and Services Administration. The Network undertook a scoping review to identify research opportunities to advance the delivery of these services to AYAs. Specifically, we reviewed research regarding (1) system-level strategies to enhance clinical preventive service delivery and access and (2) clinician-targeted or visit-level strategies to optimize the clinical encounter and the preventive interventions delivered. The review includes a focus on technological strategies to enhance the delivery and quality of clinical preventive services to AYAs, given the growing role of technology in their lives and in health care delivery.
Methods
Scoping reviews are designed to identify major thematic areas of a still developing field, to help hone in on areas of knowledge accrual or “breadth of evidence” and gaps. Scoping studies center less on elucidating a specific research question than do systematic reviews and provide a mechanism for assembling and reviewing a broad body of multidimensional work in which methods and standards of evidence may vary and where systematic review of component areas is not feasible [47]. We limited the review to studies published through February 2016 accessible on the PubMed platform as a first-tier review and bibliographies of relevant articles as a second-tier review. Thematically, our interest was in articles that provided evidence of strategies that show promise in increasing the delivery and quality of AYA clinical preventive services. Key words associated with these searches included combinations of terms that map to population descriptors (e.g., young people, adolescents, young adults), crossed with terms that map to settings of care (e.g., pediatrics, primary care, child services, preventive services, preventive interventions, school health services, community health services); dimensions of care (youth-friendly services, culturally competent care, health care quality, access/accessibility); technologically enabled systems (e.g., social media, mobile health, gaming applications, wearable devices or technology or sensors, electronic medical/health record), policy concerns (e.g., ACA, health equity, health care disparities, health status disparities), and behavioral health targets (e.g., screening, mental health, health risk behaviors, behavior change). A thematic framework of evidence/results was derived from consultative discussion among the authors to clarify the question and audience (step 1); followed by a review of published articles and selection of relevant studies (steps 2 and 3). These initial steps involved critical review of potential thematic areas to hone in on key topics and winnow the breadth of potential areas to those representing unique and complementary dimensions of adolescent/young adult–centered clinical preventive services. For each dimension, subgroups of authors outlined main findings and assessed the relative maturity of the field or evidence base, presenting results to the full team for discussion and iteration until a consensus on the “result” was achieved (step 4). A final step involved charting and summation of data/findings across the thematic areas, undertaken iteratively by the team following the same process and using a consensus as the criterion for inclusion of material (steps 5 and 6). Recommendations were developed with group input, following the same iterative inductive process—working from the larger framework to specifics, as informed by the review and status of evidence [47].
Results
System-level strategies to enhance delivery of clinical preventive services to adolescents and young adults
This review focused on two system-level topics: federal policies expanding health insurance coverage and community–clinic linkages to bring preventive services into settings more accessible for youth.
Expansion of health insurance for adolescents and young adults
Two significant federal health care policies affecting youth in recent decades include the establishment of the Children’s Health Insurance Program (CHIP) in 1997 and passage of the ACA in 2010. The CHIP program substantially expanded coverage to children ages 0–18 years from low-income families. A recent comprehensive evaluation of the program highlights the importance of continuous financial access to care [48–50]. Compared to previously uninsured new CHIP enrollees, established enrollees were more likely to have received a past-year well visit and preventive services, including a flu shot, recommended screenings, and anticipatory guidance. Disparities remained, however, with less preventive care received by black and Hispanic children and those whose parents had less than a high school education. Additional research could identify effective models of care and policies to reduce these disparities [48–50].
A key ACA insurance provision requires most private insurers to allow adult children to remain on a family health insurance plan to age 26 years. Before the ACA, young adults historically had the lowest rate of insurance coverage (29% in 2010) of any age group [51]. Rates of insurance coverage among young adults increased significantly after the ACA’s passage [52–55]; however, the impact on receipt of preventive services has been less clear. Three of six studies found an increase in clinical preventive services receipt (e.g., annual physicals, blood pressure and cholesterol screening, human papilloma virus vaccination) [27,52,56], whereas the remaining studies found no change [55,57,58].
Beyond insurance expansions, other areas of health system reform include the growth of value-based payments and system redesigns, such as accountable care organizations and patient-centered medical homes, which aim to improve health care quality while controlling costs [59–61]. Although research has largely focused on younger children or older adults, a recent study indicates that AYAs within patient-centered medical homes were more likely to receive preventive visits and screening across multiple preventive services [62]. More studies are needed that examine the effects of these models on AYA health care.
The effects of ACA and CHIP will continue to unfold over time, particularly as the ACA’s state insurance market places and, in some states, Medicaid expansion took effect in 2014 and federal CHIP funding increased in 2015. Current monitoring systems lack standardized measures across surveys and do not correspond to any set of guidelines (except for Centers for Disease Control and Prevention Advisory Committee on Immunization Practices), resulting in varied estimates of clinical preventive service delivery or receipt. For example, reported rates of past-year well visits vary widely, even across large nationally representative samples [18]. Ongoing surveillance, using a set of standardized measures, is needed to elucidate the extended effects of these policies on AYA preventive services utilization and potentially, health outcomes later in life. Special attention is warranted for specific subpopulations of youth that may derive differential benefit from these programs, such as those with chronic health problems and disadvantaged youth.
Community–clinic linkages
Linking health care systems with schools and community settings—through school-based health centers [63,64], retail clinics, and community family planning clinics and other coordinated networks [65–67], is a promising strategy for increasing youth receipt of clinical preventive services. A substantial evidence base links school-based clinics to increased receipt of preventive services, including preventive visits, immunizations, screening for mental health, and reduced emergency department visits [68] and high-risk behaviors [69–73]. Retail clinics are a growing source of care for youth, offering convenient locations (e.g., stores or pharmacies), hours, and sometimes lower cost, with AYAs more likely than children to seek primary care at retail clinics [67]. Family planning clinics also facilitate access to preventive services and have been associated with decreased unintended pregnancies, partner violence, sexually transmitted diseases (STDs), and cervical cancer rates. In addition, coordinated networks that link traditional health care facilities, AYA-serving community-based organizations, governmental public health, juvenile justice, and child/family services agencies have been shown to be successful in engaging underserved or hard-to-reach at-risk populations of youth in care, such as street-involved youth and youth involved with the juvenile justice system [74,75]. Thus, building and evaluating such systems should be an important part of the effort to increase clinical preventive services to AYAs.
Optimizing the clinical encounter
Strategies to improve preventive services that target the clinical encounter have included increasing clinician delivery of preventive services with screening and decision support tools, leveraging parent involvement, identifying effective health behavior interventions for the primary care setting, and using technology to facilitate preventive services delivery and extend reach beyond the clinic setting.
Clinician-targeted strategies
Identified barriers to clinician delivery of preventive services include lack of knowledge or confusion about guidelines or available tools, lack of time, low self-efficacy (i.e., belief by the clinician that he/she can deliver the recommended services), low outcome expectancy (i.e., belief that the delivery of services will lead to the desired outcome), and/or lack of motivation to change practice [36,76–79]. Of particular promise in addressing these barriers are (1) using brief screening tools and (2) integrating screening and clinician decision support (CDS) tools into electronic medical record (EMR) systems [80–85].
Brief screening tools, in conjunction with appropriate clinician training, have been shown to improve clinician screening rates across multiple areas of adolescent health. For example, provider screening across the areas of substance use, sexual behavior, and safety improved after an intervention in pediatric clinics that combined training in the delivery of preventive services with the integration of customized adolescent screening tools [82,86]. An intervention that included a primary care previsit computerized substance use screening system, which produced a clinician report and guidance for brief counseling, led to significant increases in clinician advice and counseling about the health risks of alcohol and drug use [87]. A violence screening module intervention found that youth were 2.6 times more likely to discuss youth violence with their providers compared to controls [88]. In the area of emotional health, a computer self-administered previsit health screener significantly increased clinician mental health–related counseling and adolescent patient disclosure of mental health issues [89]. Such use of previsit screening with a validated standardized tool has been shown to be more sensitive than clinician impression [90] and more time efficient [91], increasing the quality of clinical preventive services [92].
Integrating screeners and CDS tools into EMR systems may further improve delivery of recommended preventive services [81,83,93–95]. There has been rapid growth in EMR system adoption in recent years, fueled by federal funding [96] and EMR systems’ potential to improve care quality, efficiency, and safety [97]. Beyond basic features, such as the ability to record a patient’s problem, medication lists, and physician notes, EMRs can allow exchange of clinical information across care settings and online patient access to medical records, prescription refills, appointment booking, and previsit questionnaires through “patient portals” [98]. Accumulating evidence supports the acceptability and utility of EMR systems in clinical preventive services delivery [83,87,94,98–108]. CDS tools help automate the assessment of a patient’s risks and guide clinical practice with “computer-generated clinical knowledge and patient-related information, intelligently filtered or presented at appropriate times” [109].
Recent systematic reviews evaluating CDS tools found strong evidence among adults for increased delivery of preventive services [110,111]and screenings [112], fewer emergency department visits and hospitalizations, and better blood pressure control [100,113,114]. Several factors appear to improve CDS effectiveness, including greater level of integration within an existing EMR and clinicians’ adherence to CDS recommendations, immediate availability of screening result feedback to clinicians, concurrent provision of advice to both the patient and clinician, a requirement that clinicians give reasons for overriding advice prompts, and careful training of clinician and program staff in CDS use [105,115,116].
The relatively few studies in pediatric care settings show mixed findings. A 2012 systematic review of EMR-based intervention studies in pediatric primary care found increased screening for developmental concerns [117] and lead levels [118] but not for chlamydia [119]. A 2007–2010 national analysis of child and adolescent well visits found increased counseling and coverage of more topics at clinics with a full-featured EMR system than those with no EMR [120]. Although full-featured EMR systems with integrated CDS tools can increase clinician delivery of preventive services, less evidence exists showing an impact on patient outcomes, in part due to small, short-term studies that may miss clinically important, longer-term effects [110]. Given the promising findings of studies of EMR and CDS systems, larger, as well as longitudinal, studies are needed to examine their effects on AYA clinical preventive service delivery and patient outcomes.
As use of EMR systems increases, research is needed to assess their impact on the confidentiality of care received by AYAs [121]. Adolescents forego needed care when they fear that confidentiality is not assured [19,122]. Young adults’ privacy may also be at increased risk as more young adults retain coverage on their parents’ insurance plan [123]. Several EMR features pose threats to confidentiality, such as automated insurance claim generation, facilitation of clinical information exchange, and online patient/parent access. There are currently no universal standards for EMR systems regarding access to a young person’s record or disclosure of protected information with electronic billing [124–126]. Recent position papers of the Society for Adolescent Health and Medicine recommend that standards for EMR systems should include customizable, granular privacy controls to limit parent/guardian access to AYAs’ confidential information and the ability to prevent billing information and other e-notices about confidential services (e.g., visit reminders, e-prescriptions) from being sent to parents [124,126,127].
Parent engagement
Parents continue to play an important role in health care as AYAs assume increasing responsibilities in their own lives. [128] Parents of adolescents report greater involvement in their children’s medical care than do the adolescents themselves [129], and recent research indicates that adolescents are less likely to receive preventive care services when parents perceive preventive care is unnecessary [130]. Tools and models of care have been developed to actively engage parents as partners, while providing care that is developmentally appropriate, including confidential care [10]. Additional research is needed to understand how to best support clinicians in encouraging adolescents to actively participate in their own health care decisions, while also involving parents in healthy developmental transitions. A greater research focus on developmentally appropriate ways to involve parents in preventive service delivery may also enhance the effectiveness of AYA interventions.
Improving behavior/health of adolescents and young adults: efficacy of clinical preventive interventions
The research reviewed previously shows that it is possible to increase preventive services delivery to young people [131]. The key question is whether these services improve AYA health. Relative to the literature focused on the general adult population, few studies have investigated the effects of clinical preventive health services on AYA health, particularly in regard to preventing and reducing risky behaviors. Most studies have evaluated interventions targeting a single risk area. Evidence, although mixed, suggests that such preventive interventions show some success in improving adolescent behaviors [132]. Primary care office-based interventions have increased condom use (but not shown significant effects for reducing rates of sexual intercourse among adolescents) [133,134]; improved depressive symptoms [135,136], nutrition, and physical activity [137]; and decreased marijuana initiation [138], alcohol use [87], and STDs [139]. However, because adolescent risk behaviors tend to co-occur [140] and increase with age [141,142], guidelines recommend the delivery of services that target multiple behaviors. Yet, outcomes data on interventions with “generalized approaches”—targeting more than one health domain—are limited. That said, generalized intervention approaches have resulted in positive behavioral outcomes for adolescents or young adults in the areas of helmet [143–145] and seatbelt use [144]; sexual behavior [146,147], diet, and exercise [148,149]; illicit drug use [147]; and drinking and driving among college students [149].
The effective interventions reviewed previously used a screening tool [87,148,149] and included some form of motivational interviewing or brief counseling session(s). Although interventions vary, components tend to include priming the adolescent patient for discussion with a provider through completing the screening tool (either paper or computerized) and tailoring the providers’ counseling to the individual adolescent through personalized feedback with information obtained through the screening tool. Before discussion with adolescents, providers receive training on screening and brief counseling in the targeted health areas and incorporating the screening and/or charting tools with prompts and cues for providers into their clinical workflow.
Despite promising evidence that clinical preventive interventions may influence young people’s health behavior, many questions remain as to how to best leverage the time spent in a clinical visit for improving AYA health [150]. Furthermore, it is unclear whether there are key developmental time points [9] that are particularly suited for targeting specific individual or groups of behaviors and may contribute to interventions being more effective. Developing and evaluating interventions through a developmental science lens—with potential windows of opportunity—may increase the impact of preventive services interventions. It is also important to note that all but one of the studies reviewed [147] were limited to participants aged <20 years. Thus, little is known about the relevance of these interventions for young adults.
Most studies reviewed previously reflect single-site/health care setting efficacy studies. Moreover, the quality of study designs varies considerably, with need for additional research, particularly randomized controlled trials that focus on health outcomes. Thus, research is needed both to test more rigorous interventions in different settings and to implement and evaluate the interventions’ effectiveness on a broader scale [151]. Furthermore, the lack of consistent publication or reporting criteria for sharing the content of the intervention poses barriers both to identifying what components of the intervention are particularly effective and to translating the interventions in other settings. For example, in the studies reviewed previously, screening tools were found to be an important component of effective interventions; however, minimal information was included about the administration of the screening tools or the design and development of the electronic tools [150].
Using technology to extend clinicians’ preventive reach
A rapidly growing area of research examines technological strategies to enhance the efficiency and effectiveness of the clinical encounter or extend clinical preventive interventions beyond the face-to-face visit to motivate behavior change among AYAs between clinical visits. Clinicians’ efforts can be augmented by digital tools, such as self-guided online-based mental health disease prevention and treatment modules that are assigned to patients and/or their families in addition to provider interactions [152,153]. AYAs’ nearly universal access to, and facility with, computers, mobile technology, and the Internet [154,155] coupled with a burgeoning of information technologies—encompassing social networking tools, mobile, and wearable devices—offers numerous options for extending clinical preventive service delivery and access beyond the clinical setting. For example, after counseling in the provider office, youth’s compliance with preventive recommendations can be improved using social gaming platforms, as demonstrated in studies targeting physical activity, healthy eating, and STD prevention [156–158]. Gamification, which uses game design elements (e.g., virtual reality and video games, “playful” design), can leverage developmental windows during the AYA years by providing an opportunity to develop confidence and learn and practice behavior change in a motivating, engaging, and personalized manner [159,160].
Moreover, social media enable creation, sharing, and exchange of information in online communities and networks. Whether interactions occur within groups of family or friends, through blogging or microblogging (e.g., Twitter), image sharing, crowdsourcing, or gaming, social media platforms can enable clinician delivery of anticipatory guidance [161], provide more in-depth information to youth than might otherwise be possible during a visit [162,163], and allow further discussion of preventive health topics with online peers [163]. Youth interest in obtaining health information through social media is high, although they may be uncomfortable sharing personal health information on public platforms [155,164].
Preventive services–related activities can also be supported through mobile devices configured with software applications (“apps”) to record and track health-related behaviors, provide tailored education, and send reminders and prompts [165,166]. More than one in five teens report downloading a health-related mobile app, mostly exercise/fitness or calorie-counting/nutritional apps [155]. Although some apps are developed to support research by clinicians and investigators, many are commercially developed and marketed. Studies of these tools have suggested their efficacy for promoting smoking cessation, better dietary habits, and greater use of mental health screening among youth [167–169].
Finally, wearable devices comprise a novel area of mobile health tools and include pedometers, trackers, and sensors built into clothing. Similar to social media and mobile apps, wearables can be used to support behavior changes recommended by providers in visits. Promotion of these devices is predicated on the hypothesis that enabling people to quantify their own behaviors will drive health behavior change through contextualization (benchmarking against temporal trends or peer behaviors) and goal setting [170]. Nationally, about 7% of teens report using wearable health devices, although smart phones increasingly include similar technology such as accelerometers. Although uptake is low among youth, evidence points to the efficacy of wearable devices for driving health behavior change among adults in some domains, including weight loss [171,172]. Whether these devices offer affordable, acceptable, and effective means for sustained use among youth is not yet known [173], and there are few demonstrations about the safe and effective integration of these approaches into care.
An important goal is interoperability of social media, digital, and wearable systems across platforms with EMRs or other avenues that link to care. If achieved, such interoperability and integration would create effective flows of information among patients, clinicians, and even public health, although legal and privacy issues must be considered [174]. Such systems are emerging. For example, adolescent/young adult patients in one study were referred to join an online disease-centered social networking community and prescribed an app that supported collection of self-management and risk behavior data, all of which were aggregated for the panel and shared with providers to support care [175]. Another program is developing a multiplatform deployment of a self-adaptive personalized behavior change system for adolescents that links to primary care with a focus on preventing and decreasing risky behaviors and substance use [176].
This research area has tremendous potential for transforming AYA clinical preventive service delivery and enhancing efficiency and effectiveness. However, numerous challenges need attention, notably concerns around safety and privacy, and a robust understanding of health literacy issues underpinning effective deployment of these approaches. With wide access to online information and the powerful influence of social network sites on youth, there are concerns about youths’ ability to distinguish the quality and reliability of electronic information sources and advice [177,178]. Similarly, patients, families, and providers may find it difficult to identify safe and effective apps [179]. Another challenge is ensuring that information or interventions provided on technology platforms are evidence based, health promoting, and updated to align with changing clinical guidelines and evolving technology standards [180]. These concerns suggest the importance of promoting AYA health and media literacy and safety, which could occur during clinical encounters or more broadly through system-level endorsement of high-quality technology tools [181].
Little rigorous research exists on health outcomes resulting from integration of these technology platforms. Much remains to be learned about this evolving ecosystem, including identifying the developers and users of these tools and platforms and how reasons for use and effectiveness of approaches differ by issues and groups. The assurance of quality and safety for systems deployed within the health care system also bears further investigation. Examining these and other issues will help identify opportunities to more effectively leverage technology to improve AYA health.
Summary and Recommendations for Future Research
This review of the literature identified system- and visit-level strategies to increase the delivery of clinical preventive services to AYAs and reflects promise that the receipt of preventive interventions may influence AYA behavior and health. Several areas bear further investigation to best leverage the time in a preventive visit and maximize the potential of these services.
To summarize the results of the review findings, our broad recommendations call for expanding the body of research on young adults; using advances in developmental science to inform models of care and brief interventions, including leveraging greater parent involvement; increasing focus on expanding the evidence for behavioral/health effects of preventive services; and continuing to develop innovative ways to use technology. In addition, to improve our understanding of clinical preventive service delivery gaps and trends nationally, a comprehensive monitoring system that collects standardized data across health systems is needed. Toward that end, embedding standardized structured fields in EMR systems (e.g., records of immunizations, screenings, and risk assessments) offers one promising strategy [182]. Table 2 provides a summary of these broad recommendations and lists the more specific recommendations for future system-, clinician-, and intervention-focused research described in the Results section.
Table 2.
Summary of recommendations for future research in adolescent and young adult clinical preventive services
Broad recommendations
|
Systems-focused recommendations
|
| Recommendations on optimizing the clinical encounter |
Clinician-targeted strategies
|
| Parent engagement |
| Implement developmentally and culturally appropriate strategies to engage parents in the clinical encounters of AYAs and evaluate their effects on the receipt of clinical preventive services and health outcomes. |
| Recommendations on optimizing the clinical encounter (continued) |
Improving AYA behavior/health: efficacy of clinical preventive interventions
|
| Using technology to extend clinicians’ preventive reach |
| Leverage new technological tools (e.g., computer programs, mobile devices, wearable sensors) to enhance/improve AYA health services (e.g., for clinicians, youth, parents, and integrated systems) with attention to privacy and confidentiality concerns.
|
IMPLICATIONS AND CONTRIBUTION.
This review identified system- and visit-level strategies that increase the delivery of clinical preventive services to adolescents and young adults and interventions that influence the behavior of adolescents and young adults. Recommendations include expanding research on young adults, parent involvement, health effects of preventive services, and innovative technology and utilizing developmental science to inform models of care.
Acknowledgments
The authors thank Robin Harwood, Ph.D., MCHB Project Officer for guidance, and Fion Ng, Project Analyst for the Adolescent and Young Adult Health Research Network, for assistance in manuscript preparation.
Funding Sources
This project is supported primarily by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under Cooperative Agreement UA6MC27378. Additional support was received from the HHS/HRSA Leadership Education in Adolescent Health program (grants T71MC00009, T71MC00006, and T71MC00003); the National Research Service Award in Primary Medical Care (T32HP22239) of the HRSA’s Bureau of Health Professions; the National Science Foundation (IIS-1344670); and a grant from the Merck Foundation to J.S.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Disclaimer: This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau.
References
- 1.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: A foundation for future health. Lancet. 2012;379:1630–40. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 2.Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–79. iii. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Catalano RF, Fagan AA, Gavin LE, et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379:1653–64. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callahan T, Stampfel C, Cornell A, et al. From theory to measurement: Recommended state MCH life course indicators. Matern Child Health J. 2015;19:2336–47. doi: 10.1007/s10995-015-1767-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park MJ, Scott JT, Adams SH, et al. Adolescent and young adult health in the United States in the past decade: Little improvement and young adults remain worse off than adolescents. JAdolesc Health. 2014;55:3–16. doi: 10.1016/j.jadohealth.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Crone EA, Dahl RE. Understanding adolescence as a period of social-affective engagement and goal flexibility. Nat Rev Neurosci. 2012;13:636–50. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- 8.Nelson EE, Jarcho JM, Guyer AE. Social re-orientation and brain development: An expanded and updated view. Dev Cogn Neurosci. 2016;17:118–27. doi: 10.1016/j.dcn.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suleiman A, Dahl RE. Leveraging neuroscience to inform adolescent health: The need for an innovative transdisciplinary developmental science of adolescence. doi: 10.1016/j.jadohealth.2016.12.010. In press. [DOI] [PubMed] [Google Scholar]
- 10.Svetaz MV, Garcia-Huidobro D, Allen M. Parents and family matter: Strategies for developing family-centered adolescent care within primary care practices. Prim Care. 2014;41:489–506. doi: 10.1016/j.pop.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Maternal Newborn Child and Adolescent Health. Making health services adolescent friendly - developing national quality standards for adolescent friendly health services. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 12.World Health Organization. Volume 1: Standards and criteria. Geneva, Switzerland: World Health Organization; 2015. Global standards for quality health-care services for adolescents. [Google Scholar]
- 13.Reif CJ, Elster AB. Adolescent preventive services. Prim Care. 1998;25:1–21. doi: 10.1016/s0095-4543(05)70323-7. [DOI] [PubMed] [Google Scholar]
- 14.Lawrence RS, Gootman JA, Sim LJ. Adolescent health services: Missing opportunities. Washington, DC: National Research Council and Institute of Medicine of the National Academies; 2009. [PubMed] [Google Scholar]
- 15.Hagan JF, Shaw JS, Duncan P. Bright futures guidelines for health supervision of infants, children, and adolescents. 3rd. Elks Lodge, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 16.Shaw JS. Bright futures and social determinants ofhealth. Available at: http://nahic.ucsf.edu/wp-content/uploads/2015/10/Shaw.summit.slides.pdf. Accessed April 14, 2016.
- 17.Elster AB, Kuznets NJ. AMA guidelines for adolescent preventive services (GAPS): Recommendations and rationale. Baltimore, MD: Wilkins & Wilkins; 1994. [Google Scholar]
- 18.Adams SH, Park MJ, Irwin CE. Adolescent and young adult preventive care: Comparing national survey rates. Am J Prev Med. 2015;49:238–47. doi: 10.1016/j.amepre.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Ford C, English A, Sigman G. Confidential health care for adolescents: Position paper for the Society for Adolescent Medicine. J Adolesc Health. 2004;35:160–7. [PubMed] [Google Scholar]
- 20.National District Attorneys Association. Minor consent to medical treatment laws. Alexandria, VA: National District Attorney’s Association; 2013. [Google Scholar]
- 21.U.S. Preventive Services Task Force. The guide to clinical preventive services 2014: Recommendations of the US Preventive Services Task Force. Rockville, Maryland: Agency for Healthcare Quality and Research; 2014. [Google Scholar]
- 22.Melnyk BM, Grossman DC, Chou R, et al. USPSTF perspective on evidence-based preventive recommendations for children. Pediatrics. 2012;130:e399–407. doi: 10.1542/peds.2011-2087. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine and National Research Council. Investing in the health and well-being of young adults. Washington, D.C.: National Academies Press; 2015. [Google Scholar]
- 24.Health care for young adults. Washington, D.C.: National Academies Press; 2014. Institute of Medicine, Committee on Improving the Health, Safety, and Well-Being of Young Adults. [Google Scholar]
- 25.Ozer EM, Urquhart JT, Brindis CD, et al. Young adult preventive health care Guidelines: There but can’t be found. Arch Pediatr Adolesc Med. 2012;166:240–7. doi: 10.1001/archpediatrics.2011.794. [DOI] [PubMed] [Google Scholar]
- 26.Callahan ST. Focus on preventive health care for young adults. Arch Pediatr Adolesc Med. 2012;166:289–90. doi: 10.1001/archpediatrics.2011.898. [DOI] [PubMed] [Google Scholar]
- 27.Wong CA, Ford CA, French B, et al. Changes in young adult primary care under the Affordable Care Act. Am J Public Health. 2015;105(Suppl 5):e1–6. doi: 10.2105/AJPH.2015.302770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics Committee on Practice and Ambulatory Medicine and Bright Futures Periodicity Schedule Workgroup. 2016 Recommendations for preventive pediatric health care. Pediatrics. 2016;137:1–3. doi: 10.1542/peds.2015-2009. [DOI] [PubMed] [Google Scholar]
- 29.Advisory Committee on Immunizations Practices Vaccine recommendations of the ACIP. Atlanta, GA: Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 30.Health Resources and Services Administration. Women’s preventive services guidelines. Rockville, Maryland: U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 31.Ma J, Wang Y, Stafford RS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36:441. doi: 10.1016/j.jadohealth.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 32.Rand CM, Auinger P, Klein JD, et al. Preventive counseling at adolescent ambulatory visits. J Adolesc Health. 2005;37:87–93. doi: 10.1016/j.jadohealth.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 33.Cook S, Weitzman M, Auinger P, et al. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116:112–6. doi: 10.1542/peds.2004-1517. [DOI] [PubMed] [Google Scholar]
- 34.Irwin CE, Adams SH, Park MJ, et al. Preventive care for adolescents: Few get visits and fewer get services. Pediatrics. 2009;123:e565–72. doi: 10.1542/peds.2008-2601. [DOI] [PubMed] [Google Scholar]
- 35.Ozer EM, Zahnd EG, Adams SH, et al. Are adolescents being screened for emotional distress in primary care? J Adolesc Health. 2009;44:520–7. doi: 10.1016/j.jadohealth.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 36.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357:1515–23. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 37.Halpern-Felsher BL, Ozer EM, Millstein SG, et al. Preventive services in a health maintenance organization: How well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000;154:173–9. doi: 10.1001/archpedi.154.2.173. [DOI] [PubMed] [Google Scholar]
- 38.Burstein GR, Lowry R, Klein JD, et al. Missed opportunities for sexually transmitted diseases, human immunodeficiency virus, and pregnancy prevention services during adolescent health supervision visits. Pediatrics. 2003;111:996–1001. doi: 10.1542/peds.111.5.996. [DOI] [PubMed] [Google Scholar]
- 39.Jasik CB, Adams SH, Irwin CE, et al. The association of BMI status with adolescent preventive screening. Pediatrics. 2011;128:e317–23. doi: 10.1542/peds.2010-2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoover KW, Leichliter JS, Torrone EA, et al. Chlamydia screening among females aged 15-21 years—multiple data sources, United States, 1999–2010. MMWR Surveill Summ. 2014;63(Suppl 2):80–8. [PubMed] [Google Scholar]
- 41.Duncan P, Kemper A, Shaw J, et al. What do pediatricians discuss during health supervision visits? National surveys comparing 2003 to 2012. Pediatric Academic Societies annual meeting; Washington D.C.. 2013. [Google Scholar]
- 42.George MG, Tong X, Wigington C, et al. Hypertension screening in children and adolescents—National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, and Medical Expenditure Panel Survey, United States, 2007–2010. MMWR Surveill Summ. 2014;63(Suppl 2):47–53. [PubMed] [Google Scholar]
- 43.Callahan ST, Cooper WO. Changes in ambulatory health care use during the transition to young adulthood. J Adolesc Health. 2010;46:407–13. doi: 10.1016/j.jadohealth.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 44.Lau JS, Adams SH, Irwin CE, et al. Receipt of preventive health services in young adults. J Adolesc Health. 2013;52:42–9. doi: 10.1016/j.jadohealth.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151:379–85. doi: 10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]
- 46.Ozer EM, Scott JT, Brindis CD. Seizing the opportunity: Improving young adult preventive health care. Adolesc Med State Art Rev. 2013;24:507–25. [PubMed] [Google Scholar]
- 47.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 48.Smith KV, Dye C. How well is CHIP addressing primary and preventive care needs and access for children? Acad Pediatr. 2015;15:S64–70. doi: 10.1016/j.acap.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 49.Clemans-Cope L, Kenney G, Waidmann T, et al. How well is CHIP addressing health care access and affordability for children? Acad Pediatr. 2015;15:S71–7. doi: 10.1016/j.acap.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 50.Harrington M, Kenney GM, Smith K, et al. Report Submitted to the Office of the Assistant Secretary for Planning and Evaluation. Ann Arbor, MI: Mathematica Policy Research; 2014. CHPRA mandated evaluation of the Children’s Health Insurance Program: Final findings. [Google Scholar]
- 51.DeNavas-Walt C, Proctor B, Smith J. Income, poverty, and health insurance coverage in the United States: 2010. Washington, D.C.: Census Bureau; 2011. [Google Scholar]
- 52.Lau JS, Adams SH, Park MJ, et al. Improvement in preventive care of young adults after the Affordable Care Act: The Affordable Care Act is helping. JAMA Pediatr. 2014;168:1101–6. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- 53.Sommers BD, Gunja MZ, Finegold K, et al. Changes in self-reported insurance coverage, access to care, and health under the affordable care Act. JAMA. 2015;314:366–74. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 54.Barbaresco S, Courtemanche CJ, Qi Y. Impacts of the Affordable Care Act dependent coverage provision on health-related outcomes of young adults. J Health Econ. 2015;40:54–68. doi: 10.1016/j.jhealeco.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 55.Wallace J, Sommers BD. Effect of dependent coverage expansion of the Affordable Care Act on health and access to care for young adults. JAMA Pediatr. 2015;169:495–7. doi: 10.1001/jamapediatrics.2014.3574. [DOI] [PubMed] [Google Scholar]
- 56.Lipton BJ, Decker SL. Aca provisions associated with increase in percentage of young adult women initiating and completing the HPV vaccine. Health Aff. 2015;34:757–64. doi: 10.1377/hlthaff.2014.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kotagal M, Carle AC, Kessler LG, et al. Limited impact on health and access to care for 19- to 25-year-olds following the patient protection and affordable care Act. JAMA Pediatr. 2014;168:1023–9. doi: 10.1001/jamapediatrics.2014.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chua K-P, Sommers BD. Changes in health and medical spending among young adults under health reform. JAMA. 2014;311:2437–9. doi: 10.1001/jama.2014.2202. [DOI] [PubMed] [Google Scholar]
- 59.Lynn J, McKethan A, Jha AK. Value-based payments require valuing what matters to patients. JAMA. 2015;314:1445–6. doi: 10.1001/jama.2015.8909. [DOI] [PubMed] [Google Scholar]
- 60.Wilkinson C, Champion JD, Sabharwal K. Promoting preventive health screening through the use of a clinical reminder tool: An accountable care organization quality improvement initiative. J Healthc Qual. 2013;35:7–19. doi: 10.1111/jhq.12024. [DOI] [PubMed] [Google Scholar]
- 61.Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care. The patient centered medical home. A systematic review. Ann Intern Med. 2013;158:169–78. doi: 10.7326/0003-4819-158-3-201302050-00579. [DOI] [PubMed] [Google Scholar]
- 62.Garcia-Huidobro D, Shippee N, Joseph-Di Caprio J, et al. Effect of patient-centered medical home on preventive services for adolescents and young adults. Pediatrics. 2016 Jun;137(6):e20153813. doi: 10.1542/peds.2015-3813. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fothergill K, Ballard E. The school-linked health center: A promising model of community-based care for adolescents. J Adolesc Health. 1998;23:29–38. doi: 10.1016/s1054-139x(98)00012-3. [DOI] [PubMed] [Google Scholar]
- 64.Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42:132–56. doi: 10.1016/j.cppeds.2012.03.002. discussion 157–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: A fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696–749. doi: 10.1111/1468-0009.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kavanaugh ML, Jerman J, Ethier K, et al. Meeting the contraceptive needs of teens and young adults: Youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J Adolesc Health. 2013;52:284–92. doi: 10.1016/j.jadohealth.2012.10.276. [DOI] [PubMed] [Google Scholar]
- 67.Bain A, Wong C, Polsky D, et al. Use of urgent care and retail based clinics by children, adolescents and young adults. Presented at the Academy Health Annual Research Meeting; Minneapolis, MN. 2013. [Google Scholar]
- 68.Kempe A, Barrow J, Stokley S, et al. Effectiveness and cost of immunization recall at school-based health centers. Pediatrics. 2012;129:e1446–52. doi: 10.1542/peds.2011-2921. [DOI] [PubMed] [Google Scholar]
- 69.Kaplan DW, Calonge BN, Guernsey BP, et al. Managed care and school-based health centers. Use of health services. Arch Pediatr Adolesc Med. 1998;152:25–33. doi: 10.1001/archpedi.152.1.25. [DOI] [PubMed] [Google Scholar]
- 70.Federico SG, Abrams L, Everhart RM, et al. Addressing adolescent immunization disparities: A retrospective analysis of school-based health center immunization delivery. Am J Public Health. 2010;100:1630–4. doi: 10.2105/AJPH.2009.176628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bains RM, Diallo AF. Mental health services in school-based health centers: Systematic review. J Sch Nurs. 2016;32:8–19. doi: 10.1177/1059840515590607. [DOI] [PubMed] [Google Scholar]
- 72.Ethier KA, Dittus PJ, DeRosa CJ, et al. School-based health center access, reproductive health care, and contraceptive use among sexually experienced high school students. J Adolesc Health. 2011;48:562–5. doi: 10.1016/j.jadohealth.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 73.Braun RA, Provost JM. Bridging the gap: Using school-based health services to improve chlamydia screening among young women. Am J Public Health. 2010;100:1624–9. doi: 10.2105/AJPH.2009.186825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Woods ER, Samples CL, Melchiono MW, et al. Initiation of services in the Boston HAPPENS Program: Human immunodeficiency virus-positive, homeless, and at-risk youth can access services. AIDS Patient Care STDS. 2002;16:497–510. doi: 10.1089/10872910260351276. [DOI] [PubMed] [Google Scholar]
- 75.Harris SK, Samples CL, Keenan PM, et al. Outreach, mental health, and case management services: Can they help to retain HIV-positive and at-risk youth and young adults in care? Matern Child Health J. 2003;7:205–18. doi: 10.1023/a:1027386800567. [DOI] [PubMed] [Google Scholar]
- 76.Boyle CA, Perrin JM, Moyer VA. Use of clinical preventive services in infants, children, and adolescents. JAMA. 2014;312:1509–10. doi: 10.1001/jama.2014.12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Harris BR, Shaw BA, Sherman BR, et al. Screening, brief intervention and referral to treatment for adolescents: Attitudes, perceptions and practice of New York school-based health center providers. Subst Abus. 2016;37:161–7. doi: 10.1080/08897077.2015.1015703. [DOI] [PubMed] [Google Scholar]
- 78.Van Hook S, Harris SK, Brooks T, et al. The “Six T’s”: Barriers to screening teens for substance abuse in primary care. J Adolesc Health. 2007;40:456–61. doi: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 79.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 80.Duncan P, Frankowski B, Carey P, et al. Improvement in adolescent screening and counseling rates for risk behaviors and developmental tasks. Pediatrics. 2012;130:e1345–51. doi: 10.1542/peds.2011-2356. [DOI] [PubMed] [Google Scholar]
- 81.Olson AL, Gaffney CA, Hedberg VA, et al. Use of inexpensive technology to enhance adolescent health screening and counseling. Arch Pediatr Adolesc Med. 2009;163:172–7. doi: 10.1001/archpediatrics.2008.533. [DOI] [PubMed] [Google Scholar]
- 82.Ozer EM, Adams SH, Lustig JL, et al. Increasing the screening and counseling of adolescents for risky health behaviors: A primary care intervention. Pediatrics. 2005;115:960–8. doi: 10.1542/peds.2004-0520. [DOI] [PubMed] [Google Scholar]
- 83.Stevens J, Kelleher KJ, Gardner W, et al. Trial of computerized screening for adolescent behavioral concerns. Pediatrics. 2008;121:1099–105. doi: 10.1542/peds.2007-1878. [DOI] [PubMed] [Google Scholar]
- 84.Van Cleave J, Kuhlthau KA, Bloom S, et al. Interventions to improve screening and follow-up in primary care: A systematic review of the evidence. Acad Pediatr. 2012;12:269–82. doi: 10.1016/j.acap.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wintersteen MB. Standardized screening for suicidal adolescents in primary care. Pediatrics. 2010;125:938–44. doi: 10.1542/peds.2009-2458. [DOI] [PubMed] [Google Scholar]
- 86.Ozer EM, Adams SH, Lustig JL, et al. Can it be done? Implementing adolescent clinical preventive services. Health Serv Res. 2001;36:150–65. [PMC free article] [PubMed] [Google Scholar]
- 87.Harris SK, Csemy L, Sherritt L, et al. Computer-facilitated substance use screening and brief advice for teens in primary care: An international trial. Pediatrics. 2012;129:1072–82. doi: 10.1542/peds.2011-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Riese A, Mello MJ, Baird J, et al. Prompting discussions of youth violence using electronic previsit questionnaires in primary care: A cluster randomized trial. Acad Pediatr. 2015;15:345–52. doi: 10.1016/j.acap.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 89.Gadomski AM, Fothergill KE, Larson S, et al. Integrating mental health into adolescent annual visits: Impact of previsit comprehensive screening on within-visit processes. J Adolesc Health. 2015;56:267–73. doi: 10.1016/j.jadohealth.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wilson CR, Sherritt L, Gates E, et al. Are clinical impressions of adolescent substance use accurate? Pediatrics. 2004;114:e536–40. doi: 10.1542/peds.2004-0098. [DOI] [PubMed] [Google Scholar]
- 91.Harris SK, Knight JR, Van Hook S, et al. Adolescent substance use screening in primary care: Validity of computer self-administered vs. clinician-administered screening Subst Abus. 2016;37:197–203. doi: 10.1080/08897077.2015.1014615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Harris SK, Knight JR. Putting the screen in screening: Technology-based alcohol screening and brief interventions in medical settings. Alcohol Res. 2014;36:63–79. [PMC free article] [PubMed] [Google Scholar]
- 93.Tai B, Wu L-T, Clark H. Electronic health records: Essential tools in integrating substance abuse treatment with primary care. Subst Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Anand V, Carroll AE, Downs SM. Automated primary care screening in pediatric waiting rooms. Pediatrics. 2012;129:e1275–81. doi: 10.1542/peds.2011-2875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chisolm D, Gardner W, Julian T, et al. Adolescent satisfaction with computer-assisted behavioral risk screening in primary care. Child Adolesc Ment Health. 2008;13:163–8. doi: 10.1111/j.1475-3588.2007.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Blumenthal D, Tavenner M. The “Meaningful Use” regulation for electronic health records. N Engl J Med. 2010;363:501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 97.Council on Clinical Information Technology. Health information technology and the medical home. Pediatrics. 2011;127:978–82. doi: 10.1542/peds.2011-0454. [DOI] [PubMed] [Google Scholar]
- 98.Jasik CB, Ozer EM. Preventive health care for adolescents and young adults. In: Neinstein LS, Gordon CM, Katzman DK, editors. Adolesc Heal Care a Pract Guid. 6th. Philadelphia, PA: Lippincott Williams & Wilkins; 2016. [Google Scholar]
- 99.Papernya DM, Aonoa JY, Lehmana RM, et al. Computer-assisted detection and intervention in adolescent high-risk health behaviors. J Pediatr. 1990;116:456–62. doi: 10.1016/s0022-3476(05)82844-6. [DOI] [PubMed] [Google Scholar]
- 100.Moja L, Kwag KH, Lytras T, et al. Effectiveness of computerized decision support systems linked to electronic health records: A systematic review and meta-analysis. Am J Public Health. 2014;104:e12–22. doi: 10.2105/AJPH.2014.302164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Biondich PG, Downs SM, Anand V, et al. Automating the recognition and prioritization of needed preventive services: Early results from the CHICA system. AMIA Annu Symp Proc. 2005:51–5. [PMC free article] [PubMed] [Google Scholar]
- 102.Hunt DL, Haynes RB, Hanna SE, et al. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: A systematic review. JAMA. 1998;280:1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 103.Johnston ME, Langton KB, Haynes RB, et al. Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994;120:135–42. doi: 10.7326/0003-4819-120-2-199401150-00007. [DOI] [PubMed] [Google Scholar]
- 104.Shaikh U, Berrong J, Nettiksimmons J, et al. Impact of electronic health record clinical decision support on the management of pediatric obesity. Am J Med Qual. 2015;30:72–80. doi: 10.1177/1062860613517926. [DOI] [PubMed] [Google Scholar]
- 105.Chisolm DJ, Klima J, Gardner W, et al. Adolescent behavioral risk screening and use of health services. Adm Policy Ment Health. 2009;36:374–80. doi: 10.1007/s10488-009-0245-8. [DOI] [PubMed] [Google Scholar]
- 106.Diamond G, Levy S, Bevans KB, et al. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126:e163–70. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- 107.Julian TW, Kelleher K, Julian DA, et al. Using technology to enhance prevention services for children in primary care. J Prim Prev. 2007;28:155–65. doi: 10.1007/s10935-007-0086-8. [DOI] [PubMed] [Google Scholar]
- 108.Skiba DJ, Gance-Cleveland B, Gilbert K, et al. NI 2012 Proc 11th Int Congr Nurs Informatics. Vol. 2012. American Medical Informatics Association; 2012. Comparing the effectiveness of CDSS on provider’s behaviors to implement obesity prevention guidelines; p. 376. Vol 2012. [PMC free article] [PubMed] [Google Scholar]
- 109.Osheroff J, Pifer E, Teigh J, et al. Improving outcomes with clinical decision support: An implementer’s guide. Chicago, IL: Society, Healthcare Information and Management Systems; 2005. [Google Scholar]
- 110.Jaspers MWM, Smeulers M, Vermeulen H, et al. Effects of clinical decision-support systems on practitioner performance and patient outcomes: A synthesis of high-quality systematic review findings. J Am Med Inform Assoc. 2011;18:327–34. doi: 10.1136/amiajnl-2011-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.De Leon SF, Shih SC. Tracking the delivery of prevention-oriented care among primary care providers who have adopted electronic health records. J Am Med Inform Assoc. 2011;18(Suppl 1):i91–5. doi: 10.1136/amiajnl-2011-000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Friedberg MW, Coltin KL, Safran DG, et al. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med. 2009;151:456–63. doi: 10.7326/0003-4819-151-7-200910060-00006. [DOI] [PubMed] [Google Scholar]
- 113.Samal L, Linder JA, Lipsitz SR, et al. Electronic health records, clinical decision support, and blood pressure control. Am J Manag Care. 2011;17:626–32. [PubMed] [Google Scholar]
- 114.Reed M, Huang J, Brand R, et al. Implementation of an outpatient electronic health record and emergency department visits, hospitalizations, and office visits among patients with diabetes. JAMA. 2013;310:1060–5. doi: 10.1001/jama.2013.276733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Downs SM, Anand V, Dugan TM, et al. AMIA Annu Symp Proc. Vol. 2010. American Medical Informatics Association; 2010. You can lead a horse to water: Physicians’ responses to clinical reminders; pp. 167–71. [PMC free article] [PubMed] [Google Scholar]
- 116.Roshanov PS, Fernandes N, Wilczynski JM, et al. Features of effective computerised clinical decision support systems: meta-regression of 162 randomised trials. BMJ. 2013;346:f657. doi: 10.1136/bmj.f657. [DOI] [PubMed] [Google Scholar]
- 117.Adams WG, Mann AM, Bauchner H. Use of an electronic medical record improves the quality of urban pediatric primary care. Pediatrics. 2003;111:626–32. doi: 10.1542/peds.111.3.626. [DOI] [PubMed] [Google Scholar]
- 118.Gioia PC. Quality improvement in pediatric well care with an electronic record. Proc AMIA Symp. 2001:209–13. [PMC free article] [PubMed] [Google Scholar]
- 119.Scholes D, Grothaus L, McClure J, et al. A randomized trial of strategies to increase chlamydia screening in young women. Prev Med (Baltim) 2006;43:343–50. doi: 10.1016/j.ypmed.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 120.Rand CM, Blumkin A, Szilagyi PG. Electronic health record use and preventive counseling for US children and adolescents. J Am Med Inform Assoc. 2014;21:e152–6. doi: 10.1136/amiajnl-2013-002260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bayer R, Santelli J, Klitzman R. New challenges for electronic health records. JAMA. 2015;313:29. doi: 10.1001/jama.2014.15391. [DOI] [PubMed] [Google Scholar]
- 122.Reddy DM, Fleming R, Swain C. Effect of mandatory parental notification on adolescent girls’ use of sexual health care services. JAMA. 2002;288:710–4. doi: 10.1001/jama.288.6.710. [DOI] [PubMed] [Google Scholar]
- 123.English A, Gold RB, Nash E, et al. Confidentiality for individuals insured as dependents: A review of state laws and policies. New York, NY: The Guttmacher Institute; 2012. [Google Scholar]
- 124.Blythe MJ, Del Beccaro MA. Standards for health information technology to ensure adolescent privacy. Pediatrics. 2012;130:987–90. doi: 10.1542/peds.2012-2580. [DOI] [PubMed] [Google Scholar]
- 125.Anoshiravani A, Gaskin GL, Groshek MR, et al. Special requirements for electronic medical records in adolescent medicine. J Adolesc Health. 2012;51:409–14. doi: 10.1016/j.jadohealth.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 126.Gray SH, Pasternak RH, Gooding HC, et al. Recommendations for electronic health record use for delivery of adolescent health care. J Adolesc Health. 2014;54:487–90. doi: 10.1016/j.jadohealth.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 127.Society for Adolescent Health and Medicine; American Academy of Pediatrics. Confidentiality protections for adolescents and young adults in the health care billing and insurance claims process. J Adolesc Health. 2016;58:374–7. doi: 10.1016/j.jadohealth.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 128.Koepke S, Denissen JJA. Dynamics of identity development and separation—individuation in parent–child relationships during adolescence and emerging adulthood—a conceptual integration. Dev Rev. 2012;32:67–88. [Google Scholar]
- 129.Byczkowski TL, Kollar LM, Britto MT. Family experiences with outpatient care: Do adolescents and parents have the same perceptions? J Adolesc Health. 2010;47:92–8. doi: 10.1016/j.jadohealth.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 130.Aalsma MC, Gilbert AL, Xiao S, et al. Parent and adolescent views on barriers to adolescent preventive health care utilization. J Pediatr. 2016;169:140–5. doi: 10.1016/j.jpeds.2015.10.090. [DOI] [PubMed] [Google Scholar]
- 131.Tylee A, Haller DM, Graham T, et al. Youth-friendly primary-care services: How are we doing and what more needs to be done? Lancet. 2007;369:1565–73. doi: 10.1016/S0140-6736(07)60371-7. [DOI] [PubMed] [Google Scholar]
- 132.Solberg LI, Nordin JD, Bryant TL, et al. Clinical preventive services for adolescents. Am J Prev Med. 2009;37:445–54. doi: 10.1016/j.amepre.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 133.Boekeloo BO, Schamus LA, Simmens SJ, et al. A STD/HIV prevention trial among adolescents in managed care. Pediatrics. 1999;103:107–15. doi: 10.1542/peds.103.1.107. [DOI] [PubMed] [Google Scholar]
- 134.Kamb ML, Fishbein M, Douglas JM, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT study group. JAMA. 1998;280:1161–7. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 135.Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: A randomized clinical trial. JAMA. 2014;312:809–16. doi: 10.1001/jama.2014.9259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Williams SB, O’Connor EA, Eder M, et al. Screening for child and adolescent depression in primary care settings: A systematic evidence review for the US preventive services Task Force. Pediatrics. 2009;123:e716–35. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- 137.Patrick K, Calfas KJ, Norman GJ, et al. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2006;160:128–36. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- 138.Walton MA, Resko S, Barry KL, et al. A randomized controlled trial testing the efficacy of a brief cannabis universal prevention program among adolescents in primary care. Addiction. 2014;109:786–97. doi: 10.1111/add.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lin JS, Whitlock E, O’Connor E, et al. Behavioral counseling to prevent sexually transmitted infections: A systematic review for the U.S. Preventive services Task Force Ann Intern Med. 2008;149:497–508. W96–9. doi: 10.7326/0003-4819-149-7-200810070-00011. [DOI] [PubMed] [Google Scholar]
- 140.Lindberg LD, Boggess S, Porter L, et al. Teen risk-taking: A statistical portrait. Washington, D.C.: Urban Institute; 2000. [Google Scholar]
- 141.Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 142.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the future national results on adolescent drug use: Overview of key findings, 2011. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012. [Google Scholar]
- 143.Ozer EM, Adams SH, Orrell-Valente JK, et al. Does delivering preventive services in primary care reduce adolescent risky behavior? J Adolesc Health. 2011;49:476–82. doi: 10.1016/j.jadohealth.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 144.Stevens MM, Olson AL, Gaffney CA, et al. A pediatric, practice-based, randomized trial of drinking and smoking prevention and bicycle helmet, gun, and seatbelt safety promotion. Pediatrics. 2002;109:490–7. doi: 10.1542/peds.109.3.490. [DOI] [PubMed] [Google Scholar]
- 145.Johnston BD, Rivara FP, Droesch RM, et al. Behavior change counseling in the emergency department to reduce injury risk: A randomized, controlled trial. Pediatrics. 2002;110:267–74. doi: 10.1542/peds.110.2.267. [DOI] [PubMed] [Google Scholar]
- 146.Chen X, Murphy DA, Naar-King S, et al. A clinic-based motivational intervention improves condom use among subgroups of youth living with HIV. J Adolesc Health. 2011;49:193–8. doi: 10.1016/j.jadohealth.2010.11.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sanci L, Chondros P, Sawyer S, et al. Responding to young people’s health risks in primary care: A cluster randomised trial of training clinicians in screening and motivational interviewing. PLoS One. 2015;10:e0137581. doi: 10.1371/journal.pone.0137581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Olson AL, Gaffney CA, Lee PW, et al. Changing adolescent health behaviors: The healthy teens counseling approach. Am J Prev Med. 2008;35:S359–64. doi: 10.1016/j.amepre.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 149.Werch CE, Bian H, Moore MJ, et al. Brief multiple behavior interventions in a college student health care clinic. J Adolesc Health. 2007;41:577–85. doi: 10.1016/j.jadohealth.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Webb MJ, Kauer SD, Ozer EM, et al. Does screening for and intervening with multiple health compromising behaviours and mental health disorders amongst young people attending primary care improve health outcomes? A systematic review. BMC Fam Pract. 2016;17:104. doi: 10.1186/s12875-016-0504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sterling S, Kline-Simon AH, Satre DD, et al. Implementation of screening, brief intervention, and referral to treatment for adolescents in pediatric primary care. JAMA Pediatr. 2015;169:e153145. doi: 10.1001/jamapediatrics.2015.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gladstone TG, Marko-Holguin M, Rothberg P, et al. An internet-based adolescent depression preventive intervention: Study protocol for a randomized control trial. Trials. 2015;16:203. doi: 10.1186/s13063-015-0705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Siemer CP, Fogel J, Van Voorhees BW. Telemental health and web-based applications in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20:135–53. doi: 10.1016/j.chc.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pew Internet Project. Teens Fact Sheet. Available at: http://www.pewinternet.org/fact-sheets/teens-fact-sheet/. Accessed March 19, 2014.
- 155.Center on Media and Human Development. Teens, health, and technology: A national survey. Chicago, IL: Northwestern University; 2015. [Google Scholar]
- 156.Gotsis M, Wang H, Spruijt-Metz D, et al. Wellness partners: Design and evaluation of a web-based physical activity diary with social gaming features for adults. JMIR Res Protoc. 2013;2:e10. doi: 10.2196/resprot.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lin RJ, Zhu X. Leveraging social media for preventive care-A gamification system and insights. Stud Health Technol Inform. 2012;180:838–42. [PubMed] [Google Scholar]
- 158.Gabarron E, Schopf T, Serrano JA, et al. Gamification strategy on prevention of STDs for youth. Stud Health Technol Inform. 2013;192:1066. [PubMed] [Google Scholar]
- 159.Morris BJ, Croker S, Zimmerman C, et al. Gaming science: The “gamification” of scientific thinking. Front Psychol. 2013;4:607. doi: 10.3389/fpsyg.2013.00607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ozer EJ, Piatt A, Holsen I, et al. Innovative approaches to promoting positive youth development in diverse contexts: Novel applications of participatory research and new technologies. In: Petersen A, Motti-Stefanidi F, Koller S, et al., editors. Posit Youth Dev Glob Context Soc Econ Chang. Routledge: Taylor and Francis Group; 2016. [Google Scholar]
- 161.Wong CA, Merchant RM, Moreno MA. Using social media to engage adolescents and young adults with their health. Healthcare. 2014;2:220–4. doi: 10.1016/j.hjdsi.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Evans Y. Teenology 101. Available at: http://teenology101.seattlechildrens.org/. Accessed July 23, 2015.
- 163.Yonker LM, Zan S, Scirica CV, et al. “Friending” teens: Systematic review of social media in adolescent and young adult health care. J Med Internet Res. 2015;17:e4. doi: 10.2196/jmir.3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Selkie EM, Benson M, Moreno M. Adolescents’ views regarding uses of social networking Websites and text messaging for adolescent sexual health education. Am J Health Educ. 2011;42:205–12. doi: 10.1080/19325037.2011.10599189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: Qualitative study. J Med Internet Res. 2013;15:e86. doi: 10.2196/jmir.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gal N, Zite NB, Wallace LS. Evaluation of smartphone oral contraceptive reminder applications. Res Social Adm Pharm. 2015;11:584–7. doi: 10.1016/j.sapharm.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 167.Haug S, Schaub MP, Venzin V, et al. Efficacy of a text message-based smoking cessation intervention for young people: A cluster randomized controlled trial. J Med Internet Res. 2013;15:e171. doi: 10.2196/jmir.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Nollen NL, Mayo MS, Carlson SE, et al. Mobile technology for obesity prevention: A randomized pilot study in racial- and ethnic-minority girls. Am J Prev Med. 2014;46:404–8. doi: 10.1016/j.amepre.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Reid SC, Kauer SD, Hearps SJC, et al. A mobile phone application for the assessment and management of youth mental health problems in primary care: Health service outcomes from a randomised controlled trial of mobile type. BMC Fam Pract. 2013;14:84. doi: 10.1186/1471-2296-14-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313:459–60. doi: 10.1001/jama.2014.14781. [DOI] [PubMed] [Google Scholar]
- 171.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: A systematic review. JAMA. 2007;298:2296–304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 172.Shuger SL, Barry VW, Sui X, et al. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: A randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:41. doi: 10.1186/1479-5868-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Audrey S, Bell S, Hughes R, et al. Adolescent perspectives on wearing accelerometers to measure physical activity in population-based trials. Eur J Public Health. 2013;23:475–80. doi: 10.1093/eurpub/cks081. [DOI] [PubMed] [Google Scholar]
- 174.Klann JG, McCoy AB, Wright A, et al. Health care transformation through collaboration on open-source informatics projects: Integrating a medical applications platform, research data repository, and patient summarization. Interact J Med Res. 2013;2:e11. doi: 10.2196/ijmr.2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Weitzman ER, Kelemen S, Garvey K, et al. Prescribing social networking to adolescent diabetes clinic patients. 5th World Congress on social media, Mob. Apps, Internet.; Boston, MA. 2012. [Google Scholar]
- 176.Lester JC, Ozer EM. A self-adaptive personalized behavior change system for adolescent preventive healthcare. NSF Smart Connected Health PI Meeting; Arlington, VA. 2014. [Google Scholar]
- 177.Moreno MA, Whitehill JM. New media, old risks: Toward an understanding of the relationships between online and offline health behavior. Arch Pediatr Adolesc Med. 2012;166:868–9. doi: 10.1001/archpediatrics.2012.1320. [DOI] [PubMed] [Google Scholar]
- 178.Weitzman ER, Cole E, Kaci L, et al. Social but safe? Quality and safety of diabetes-related online social networks. J Am Med Inform Assoc. 2011;18:292–7. doi: 10.1136/jamia.2010.009712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014;311:1851–2. doi: 10.1001/jama.2014.2564. [DOI] [PubMed] [Google Scholar]
- 180.Direito A, Dale LP, Shields E, et al. Do physical activity and dietary smartphone applications incorporate evidence-based behaviour change techniques? BMC Public Health. 2014;14:646. doi: 10.1186/1471-2458-14-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Moreno M. Sex, drugs ’n Facebook. Alameda, CA: Hunter House Inc., Publishers; 2013. [Google Scholar]
- 182.Wasserman RC. Electronic medical records (EMRs), epidemiology, and epistemology: Reflections on EMRs and future pediatric clinical research. Acad Pediatr. 2011;11:280–7. doi: 10.1016/j.acap.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


