Abstract
The neurological complications of AIDS (neuroAIDS) during the infection of human immunodeficiency virus (HIV) are symptomized by non-specific, multifaceted neurological conditions and therefore, defining a specific diagnosis/treatment mechanism(s) for this neuro-complexity at the molecular level remains elusive. Using an in silico based integrated gene network analysis we discovered that HIV infection shares convergent gene networks with each of twelve neurological disorders selected in this study. Importantly, a common gene network was identified among HIV infection, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and age macular degeneration. An mRNA microarray analysis in HIV-infected monocytes showed significant changes in the expression of several genes of this in silico derived common pathway which suggests the possible physiological relevance of this gene-circuit in driving neuroAIDS condition. Further, this unique gene network was compared with another in silico derived novel, convergent gene network which is shared by seven major neurological disorders (Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, and Restless Leg Syndrome). These networks differed in their gene circuits; however, in large, they involved innate immunity signaling pathways, which suggests commonalities in the immunological basis of different neuropathogenesis. The common gene circuits reported here can provide a prospective platform to understand how gene-circuits belonging to other neuro-disorders may be convoluted during real-time neuroAIDS condition and it may elucidate the underlying–and so far unknown–genetic overlap between HIV infection and neuroAIDS risk. Also, it may lead to a new paradigm in understanding disease progression, identifying biomarkers, and developing therapies.
Introduction
The clinicopathological characteristics of different neurological disorders are often indistinguishable. Symptoms such as hallucinations, memory loss, dementia, and other psychotic symptoms are common to almost all neuro-disorders. Accordingly, the existing “partial-treatment” strategy, which primarily includes several decades old prototype drugs, are meant to antagonize targets which are common for most neuro-disorders (e.g. D2 dopamine receptors antagonists) [1,2]. Improvement towards disease-specific targets will require sincere insight into their complex molecular mechanisms, which has started only recently with the advent of high-throughput genomic technologies. A correlation at the interface of neurobiology and human genetics is being drawn with the discovery of multiple genetic signatures belonging to a single disease or common to various neuro-disorders. Disrupted expression of even a single gene possesses the ability to affect several molecular pathways and therefore, multiple psychotic phenotypes may have connection in converged molecular circuits. Nonetheless, analysis of underlying disease processes based on a single gene annotation is less comprehensive[3]. Thus, the discovery of shared dysregulated molecular pathways among various neuro-disorders can accelerate mechanistic studies of their pathophysiology which, in turn, can lead to appropriate therapies.
Neuroinvasion by human immunodeficiency virus (HIV) cause several types of neurologic conditions which are collectively termed as the “neuroAIDS” [4–7]. The presence of HIV particles/proteins/genetic components and intrathecal anti-HIV antibodies in the brain and CNS are detected early during infections. This suggests that HIV enters the brain during early infection phase and therefore it is believed that the neuroAIDS condition in HIV patients can prevail throughout the infection period [6,8–10]. Initial entry of HIV into the brain is mediated via infected monocytes and macrophages from the peripheral circulation. These mononuclear phagocytes (irrespective of being non-infected and/or infected) intrinsically possess specific cytokines/chemokines-responsive, transendothelial migration ability to cross the blood-brain barrier (BBB) and go into the brain (e.g. monocyte chemotactic protein-1) [11–13]. Early HIV infection of brain cells triggers the release of BBB-compromising factors (e.g. matrix metalloproteinase) [14] which induces the influx rate of inflammation responsive leukocytes from peripheral body region into the brain [15]. Now, both infected and non-infected monocytes/macrophages from peripheral circulation reach to the brain in higher number than the normal condition [16]. Higher accumulation of infected leukocytes intensifies the progression of HIV infection in different brain cells. Among the major brain cells, the susceptibility of astrocytes and microglia to HIV infection has been shown in various studies [17]. However, HIV invasion to nerve cells remains highly debated. Nonetheless, neurotoxic effect of HIV proteins on neurons is a proven phenomenon [18]. HIV infections to different cell types are not always productive; rather, HIV acquires latency in a subpopulation of almost all cell types including brain cells [19–21]. Latency allows HIV to escape deleterious effects of cellular immune response and/or antiretroviral drugs. Transcription of host-integrated HIV genome during the latency phase is zero or minimum. Latency can persist for years and it can lead to chronic pathological implications because minimum viral genome transcription can continuously produce little virus and/or viremia can be rebound upon latency reactivation [22]. In fact, HIV reactivation in a fraction of latent cells due to specific endogenous or exogenous stimulus is a continuous occurrence in a real physiological condition which adds to the disease progression[6,20]. Thus, both latent, as well as active HIV infections, contribute to the neuroAIDS condition.
The health and function of brain regions and spinal cord involved in learning and information processing are significantly compromised due to the neuroAIDS condition. While nearly 50% HIV patients demonstrate one or other kind of neurological symptoms [23], a much higher percentage of autopsies of AIDS patients (~80%) shows mild to severe neurological deformities [24]. The neuroAIDS is shaping up as a global problem and this can be attributed to: (i) longevity of HIV patients upon consistent HAART treatment, (ii) ineffectiveness of HAART for HIV-associated neurological complications, (iii) lack of ARV therapies for ~ 40% of AIDS patients, (iv) existing non-specific, common “partial-treatment” strategy for most neuro-disorders, and (v) inability of more than 98% drugs to transmigrate across the blood-brain barrier (BBB) [6]. Some notable neurological complications within the spectrum of neuroAIDS are HIV-associated neurocognitive disorder (HAND), chronic meningitis, peripheral neuropathies, neurosyphilis, CNS lymphomas, progressive multifocal leukoencephalopathy, vacuolar myelopathy, etc. Also, neurological deformities of unknown origin are seen in HIV patients [4,5,7]. To date, the precise diagnosis of neuroAIDS onset remains a formidable task for scientific communities because of its intrinsic multifaceted symptoms and pathologies.
Neurodegeneration by HIV virion and neurotoxic HIV proteins involve complex etiology. Differentiation of HIV-infected monocytes into macrophages leads to astrocytes and microglia activation which cause severe neuroinflammation. The subsequent release of neuron-damaging molecules such as reactive oxygen species, nitric oxide, TNF-α, IL-1β, quinolinic acid, β-chemokines, arachidonic acid, etc. further exacerbates the pathological process [17,25,26]. The release of these proinflammatory factors in macrophages and microglia is elevated by HIV envelope protein gp120. The gp120 activates chemokine receptors (CXCR4 or CCR5) in neurons which induce rise of intracellular Ca2+ concentration leading to apoptosis [27]. In astrocytes, gp120 induces excitotoxicity and cell death via downregulating glutamate uptake and increasing production of nitric oxide synthase production, respectively [28,29]. The gp120 protein also inhibits neural progenitor cells (NPCs) migration and proliferation [30]. Additionally, gp120 induces apoptosis in the brain microvascular endothelial cells (BMVECs) to alter BBB integrity [31]. Activation of apoptosis by gp120/gp41, especially via the p53 pathway, is a common phenomenon across all three major brain cells i.e. macrophages/microglia, neurons, and astrocytes [25]. The HIV Tat protein stimulates hostile conditions for neurons and other brains cells in many ways which are similar to gp120. Exposure of Tat elevates the proinflammatory factors such as TNF-α and IP-10 in macrophages and microglia, induces apoptosis in BMVECs, upregulates MCP-1 and reduces glutamate uptake in astrocytes, and inhibits NPCs neurogenesis [25,32]. In neurons, Tat induces NMDA receptors, activate NO and Ca-release, inhibits tyrosine hydroxylase, and decrease dopamine [25,32]. These effects of Tat proteins lead to neuronal death by apoptosis or other cytotoxicity means. The HIV Vpr and Nef proteins also induce apoptosis in BMVECs, astrocytes, and neurons. In addition, Vpr exposure modulates ion channels and H2O2 upregulation in neurons, impairs neuron maturation, and induces mitochondrial dysfunction in NPCs [17,33]. Exposure of Nef protein elevates proinflammatory factors (TNF-α, MIP-1, IL-6, etc.) and superoxide release in macrophages and microglia [34,35]. In neurons, Nef modulates [K+] ion channels and in astrocytes, it upregulates complement factor C3, MCP-1, IP-10, and MMP-9 activity [17,25,26]. While all these mechanisms certainly aggravate the neuroAIDS pathologies in one or other way, HIV infection also leads to synaptodendritic injury. Neuronal spine density, dendritic diameter, total spine, and dendritic area are significantly compromised during the HIV infection [36–38]. This may be correlated with the atrophy of grey and white matter in the brain of HIV patients [39]. Many of similar molecular processes involving apoptosis, generation of reactive oxygen species, generation of proinflammatory factors, ionic channel modulations, synaptodendritic injury, etc. are seen in the case of Alzheimer’s disease [40], Parkinson’s disease [41], multiple sclerosis [42], age macular degeneration [43] or other neurological disease. In fact, gene expression changes during neuroAIDS condition show consistency with these neuro-disorders. Such as, HIV infection induces production of amyloid precursor protein and subsequently amyloid is accumulated in the brain [44]. Similarly, IGF signaling has been implicated in both neuroAIDS and PD; and ErbB2/B4 and NRG1, responsible for schizophrenia susceptibility, are found in neuroAIDS as well [45]. Thus multiple gene-circuit crossovers between neuroAIDS and other neuro-disorders are suspected. Nonetheless, barring some sporadic reports with few genes related to a specific disease; studies comparing gene-network signatures between HIV infection and neuro-disorders are lacking in entirety. As such discovering these molecular crossovers may reveal the reason for multifaceted symptoms and pathologies of the neuroAIDS condition.
An intensive bioinformatics analysis was performed between and among the molecular networks of risk-associated genetic markers for HIV infection and twelve major neurological disorders (Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, Restless Leg Syndrome, Glaucoma, Migraine, Creutzfeldt—Jakob disease, Narcolepsy, and Autism-Autism Spectrum) obtained from the genome-wide association study (GWAS) catalog. The bioinformatically discovered common gene circuits in this study, in combination with mRNA microarray for HIV latent and active infection model, suggest similarity in the pattern of genetic disruption for HIV infection and neuro-disorders. As such, common gene-network signatures reported here can have significant physiological relevance in driving convoluted nature of pathologies during neuroAIDS and other neurologic conditions.
Materials and methods
Bioinformatics analysis
All established at-risk alleles of HIV infection and twelve major neurological disorders (Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, Restless Leg Syndrome, Glaucoma, Migraine, Creutzfeldt—Jakob disease, Narcolepsy, and Autism-Autism Spectrum) delineated in Genome-Wide Association Studies (GWAS) online catalog were retrieved and were denoted as “at-risk” genes (S4 Data). These genome-disease associations listed in GWAS are based on different population-based studies across the globe where expression modulations and polymorphism in one and/or other genome have been shown to drive a specific disease in respective populations. One or more than one GWAS genes from a single study for a disease in one population may not be primary reason of the same disease in other population from another study. In many cases, the primary gene responsible for a disease in one population can be secondary or tertiary responsible gene or can be far-related as well in other population. Thus at-risk genes for a disease in GWAS are an accumulation of all reported genes for that disease from different study across the globe. Gene networks of risk-associated genes of each disease were obtained in silico (bioinformatically) using the Cytoscape open software bioinformatics program and two of its plugins, GPEC v2.8.3 (Gene Prioritization and biomedical Evidence Collection) and Genemania v3.3.1 [46]. At-risk genes were run through GPEC to identify gene network associated with specific diseases through a random walk algorithm with restart. The random walk algorithm with restart is a gene prioritization method where starting nodes are selected in a given network and subsequently with a certain probability value, random walker either moves to a random immediate neighbor node from the starting node or returns to one of the starting nodes [47]. Specifications for GPEC run are: Step 1: The network identified is the Default Human Functional Linkage (FLN), the identifier is Entrez Gene ID and the network weighed option is selected. Step 2: The other genes/proteins option is selected, and the identifier for this step is Official Symbol. The “check” option is selected, and all the at-risk genes are added to the list. Step 3: The candidate set is selected to be neighboring interactants of at-risk genes in the network with a neighboring distance of 1. Using a random walk with the algorithm, GPEC now finds any neighboring interactants of at-risk genes with a topological distance of 1. The genes in the developed network are now known as the “neighboring genes”. Step 4: Each neighboring set is then scored and ranked by a parameter of α = 0.5. The neighboring genes networks of each neurological disorder were individually venn-analyzed in comparison with that for HIV infection. Genes common to both diseases were manually verified and selected for functional analysis performed by the second Cytoscape plugin, Genemania v3.3.1. For each particular disease, the at-risk genes of that disease were inputted along with the at-risk genes of HIV infection and the genes shared between that specific neurological disease and HIV infection. The generated visual networks of common genes by Genemania v3.3.1 were further analyzed for their involvement in various molecular pathways. The q-value for these networks indicates the probability that appears significant due to random chance [48]. Eventually, different neighboring interactants were compared together to obtain a set of common genes which were used to generate common gene-network signatures using Genemania v3.3.1.
Microarray analysis
Unstimulated promonocytic U1 latent cells (AIDS Research and Reference Reagent Program, NIAID, National Institute of Health, Rockville, MD) were used to perform latent infection model [49,50]. Stimulation of U1 cells by PMA (10nM) for 4 hr and subsequent culture for 5 days was exerted for confirmation of latent condition (S1 Fig). The U-937 monocytes (American Type Culture Collection) infected with HIV-1Ba-L (NIH AIDS Research and Reference Reagent Program catalog no. 510) were used for the active infection model. In brief, after 4 hr PMA (10nM) treatment (to maintain equivalent treatment condition as that of U1) followed by 2 hr HIV treatment (@ 6.2ngml−1) cells were washed with PBS buffer and returned to culture for 5 days. In other words, a set of uninfected U937 cells and stimulated U1 cells were used as controls. Experiments were performed three times (N = 3) with two technical replicates in each case. After 5 days, supernatants from both active and latent cell culture were quantified for p24 antigen (N = 3) via ELISA kit (ZeptoMetrix, Buffalo, NY) (S2 Fig). Parallely, RNAs from cells were isolated using Illustra triplePrep Kit (GE Healthcare Life Sciences, UK) and were sent to Arraystar Inc., MD, USA for mRNA microarray analysis (N = 2). In brief, purified mRNA (mRNA-ONLY™ Eukaryotic mRNA Isolation Kit, Epicentre) was amplified and subsequently transcribed into fluorescent cRNA utilizing a mixture of oligo(dT) and random primers (Arraystar Flash RNA Labeling Kit, Arraystar). The GeneSpring GX v12.1 software package (Agilent Technologies) was used for quantile normalization and subsequent data processing. The mRNAs that at least four out of twelve samples have flags in present or marginal (“All Targets Value—mRNAs”) were selected for the screening of differentially expressed mRNAs. Differential expression was considered for mRNAs with statistical significance that passed Volcano Plot filtering (Fold Change > = 2.0 and P-value < = 0.05).
Results
Shared gene network between HIV/AIDS and neurological disorders
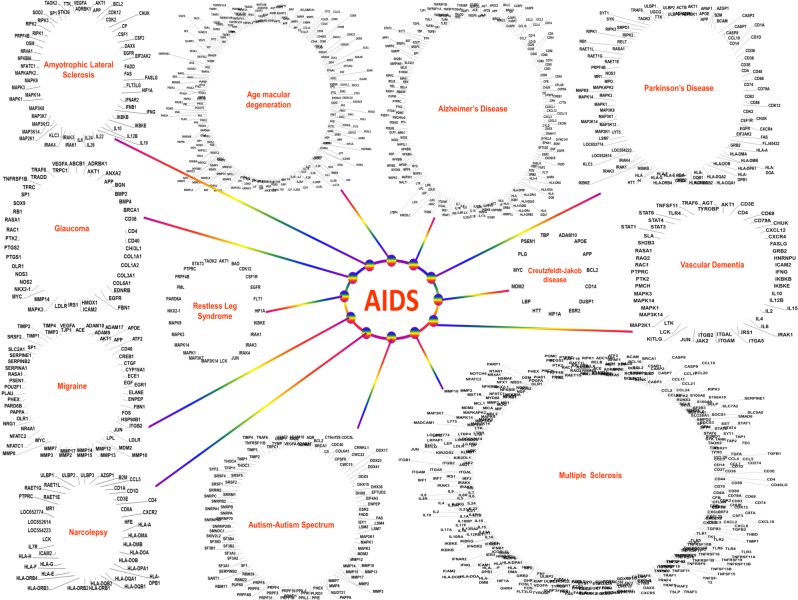
To examine the molecular linkage between HIV infection and different neurological disorders, we utilized a “random walk algorithm with restart” within the human functional linkage network using the Cytoscape open software bioinformatics program. Functional linkage network of each disease was derived using at-risk genes retrieved from the GWAS catalog. A total of 9 genetic loci (at-risk genes) associated with AIDS risk was found which were used for network generation using Gene Prioritization and Evidence Collection (GPEC) plug-in of Cytoscape-2.8.3. With a topological distance of ≤1, GPEC could find 785 neighboring genes in the interactants of these at-risk genes. Similarly, neighboring genes of other disease were obtained (S1 Table). Venn analysis of HIV infection interactants with other disease revealed shared neighboring genes between HIV infection and each of 12 neurological disorders selected in this study (Fig 1 & S1 Data). Multiple sclerosis showed the highest number of shared genes with AIDS, followed by age macular degeneration, Alzheimer’s disease, autism-autism spectrum, and so on. The least number of shared genes were found between HIV infection and Creutzfeldt—Jakob disease (S1 Table). Visual networks of at-risk and shared neighboring genes of AIDS and each neuro-disorder were created using Cytoscape’s geneMANIA plug-in, which revealed the involvement of several important functional pathways (S2 Data). In-large, pathways related to immune-response was seen in all visual networks.
Fig 1. AIDS share common molecular pathways (genes) with different neurological disorders (please see S2 Data for details): neighboring gene network of each neurological disorder was compared (Venn Analysis) with that of AIDS to obtain their shared genes.
All at-risk genes (S4 Data) for Schizophrenia, major depression, Bipolar and Attention Deficit Hyperactivity Disorder overlapped with Autism spectrum and as such was not classified as a separate disease.
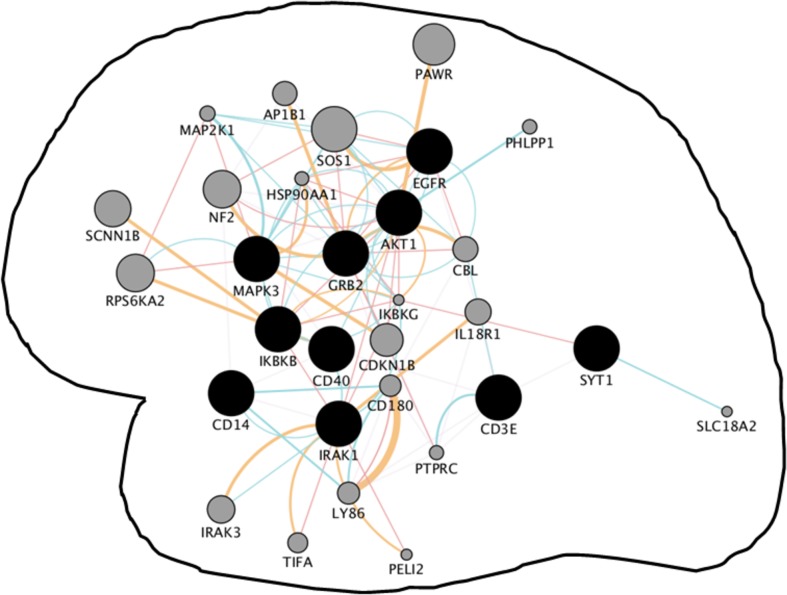
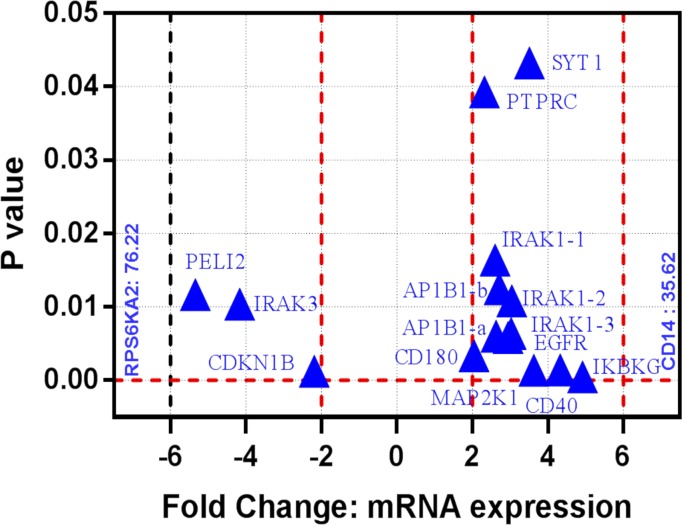
The physiological relevance of in silico discovered common gene-network signatures for AIDS and neurological disorders during latent and active HIV infections
Shared neighboring interactants of HIV infection and neurological disorders were venn-analyzed and subsequently manually verified to define common gene-network signatures. We discovered 10 common genes among HIV infection, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and age macular degeneration (S3 Data; Fig 2). Visual networks of these common genes were created using Cytoscape’s geneMANIA plug-in, which involved a total of 30 genes. Functional analysis of this gene cluster showed their involvement in pathways associated with immune response-activating signal transduction, toll-like receptor signaling, activation of immune response pattern recognition receptor signaling, MyD88-dependent signaling, etc. Further, the physiological relevance of this common network was established in the active and latent HIV infection model. For this purpose, mRNA microarray analysis was performed in the monocytes with active and latent HIV infection. It was found that > 55% genes of in silico derived common gene network are either upregulated or downregulated in active vs latent HIV infections. While most of these genes showed positive or negative dysregulation between 2 to 6 fold, a couple of them showed much higher fold-differences in active vs latent infection (Fig 3).
Fig 2. Convergent neighboring gene network shared by AIDS, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and age macular degeneration: Convergent gene networks are primarily the shared molecular pathways between networks of genes of two or more different diseases.
In our case, the term neighboring is added because networks of individual diseases represent neighboring interactants of at-risk genes. The developed network revealed the involvement of immunological pathways as retrieved by geneMANIA with P< 10−10. The network was developed using the 10 common genes (black dots) found via Venn analysis. Few of these common genes are also seen in other neuro-disorders: Amyotrophic Lateral Sclerosis (AKT1, EGFR, & IKBKB), Glaucoma (AKT1 & EGFR), Vascular Dementia (AKT1 & IKBKB), and Migraine and Restless leg syndrome (AKT1). Narcolepsy, Creutzfeldt-Jakob disease, and Autism-autism spectrum did not share genes with these common gene sets suggesting least chance of these symptoms during neuroAIDS. Genes in grey dots represent networking genes retrieved by geneMANIA where smaller to higher grey circle sizes represents weaker to the stronger degree of connectivity/associations between two proteins. Colored connecting line between two genes/proteins indicates interactions between them (red-physical; orange-predicated, and green-genetic) and blue lines are part of pathways. Pathways involved in this gene circuit, together with the pathways involved in Fig 4, suggests commonalities in the immunological basis of different neuropathogenesis.
Fig 3. Volcano plots of the unpaired t-tests of the mRNA expression fold change for active vs latent HIV infections in monocytes (N = 2): Volcano plot is primarily a scatter plot that is used for identification of changes in specific data sets by plotting significance value versus fold-change on the y- and x-axis respectively.
Our study show differentially expressed mRNAs with statistical significance that passed Volcano Plot filtering (Fold Change > = 2.0 and P-value < = 0.05). Most mRNAs showed variations with 2 to 6 fold; nonetheless, CD14 and RPS6KA2 mRNAs were 35.62 and 76.22 fold upregulated and downregulated, respectively. The vertical lines correspond to 2.0-fold up and down and the horizontal line represents a P-value up to 0.05. So the blue triangles in the plot represent the differentially expressed mRNAs with statistical significance. This represents subsets of differentially expressed mRNAs from common convergent neighboring gene network shared by AIDS, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and age macular degeneration.
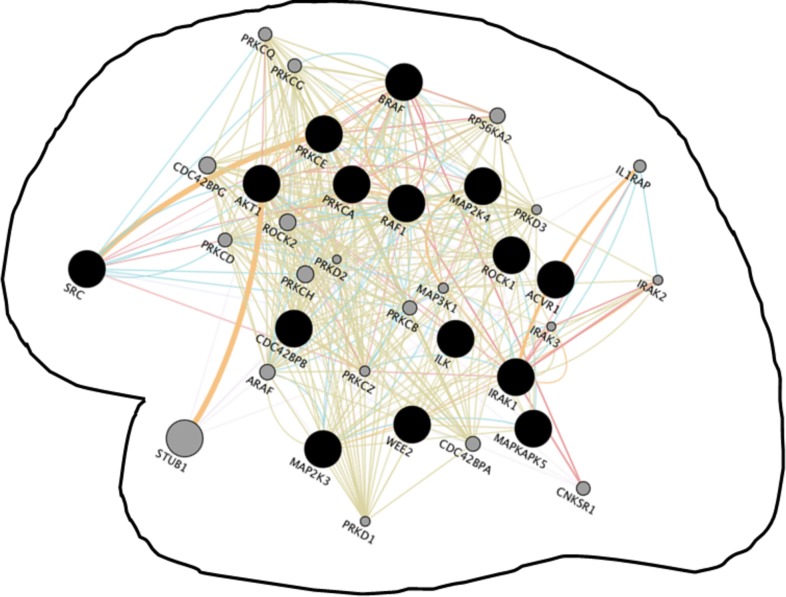
Converged molecular circuits of major neurological disorders
Common gene-network signatures of HIV infection and neurological disorders (Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and age macular degeneration) were compared with a unique convergent gene network shared by seven major neurological disorders. This common network of several neurological disorders was discovered by venn-analyzing neighboring networks of Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, and Restless Leg Syndrome (S3 Data; Fig 4). A total of 15 common genes were discovered in the network of seven neurological disorders which were used for network development using Cytoscape’s geneMANIA plug-in. The network involved a total of 35 genes which were associated with pathways related to Protein serine/threonine kinase activity, immune response-activating signal transduction, toll-like receptor signaling, activation of immune response pattern recognition receptor signaling, regulation of NF-kappaB, transcription factor activity, platelet activation, etc. Few of these common genes are also seen in other neuro-disorders, for example, AKT1, ILK, RAF1, and SRC gene was common to Glaucoma, Autism-Autism Spectrum included RAF1 and BRAF, Creutzfeldt-Jakob disease included ROCK1 and PRKCE, and Migraine has AKT1. Narcolepsy did not share any gene(s) with these common gene sets.
Fig 4. Convergent neighboring gene network shared by Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, and Restless Leg Syndrome.
The network revealed the involvement of immunological pathways as retrieved by geneMANIA with P< 10−10. Few of these common genes are also seen in other neuro-disorders: Glaucoma (AKT1, ILK, RAF1, & SRC), Autism-Autism Spectrum (RAF1 & BRAF), Creutzfeldt-Jakob disease (ROCK1 & PRKCE), and Migraine (AKT1). Narcolepsy did not share genes with these common gene sets suggesting possibility unrelated immunopathological mechanisms. Genes in grey dots represent networking genes retrieved by geneMANIA where smaller to higher grey circle sizes represents weaker to the stronger degree of connectivity/associations between two proteins. Colored connecting line between two genes/proteins indicates interactions between them (red-physical; orange-predicated, and green-genetic) and blue lines are part of pathways. Pathways involved here suggest the similar immunological basis of different neuropathogenesis.
Discussion
Existing categorizations of neuroAIDS depend on the preponderance of specific symptoms in neuroAIDS patients which have little or no relevance to the pathological hallmarks. In fact, neuroAIDS constitutes multifaceted symptoms and there are no clear distinctions between its different categories [51]. Moreover, neuroAIDS shows overlapping symptoms and abnormalities with other diseases. For example, dementia, seizures, mood disorders, neuropathic pain, epilepsy, myelopathy, cognitive motor impairment, etc. are common to neuro-disorders such as Alzheimer’s Disease, Parkinson’s Disease, vascular dementia, etc. [51]. This insinuates towards dysregulation of molecular processes which are common to other neuro-disorders. Now, the challenge is to dissect the molecular networks and dysregulated pathways shared between neuroAIDS and different neurological disorders. Some previous studies have identified involvement of few common genes between neuroAIDS and Alzheimer’s, Parkinson’s disease, etc. [44,45]. Here, to best of our knowledge, for the first time, we have analyzed the pathologic-specific genomic association between HIV infection and major neurological disorders. We utilized an integrated network approach based on “random walk algorithm with restart” to quantitatively prioritize genes. This prioritization is performed according to the topological distance and functional relatedness with known genes of other diseases in the functional linkage network (FLN) [46,47]. The basis of FLN ranking of potential disease-related genes utilizes the functional relatedness of those gene(s) which directly or indirectly contributes to a particular disease phenotype. Genetic associations that confer risk to HIV infection and twelve major neurological disorders were retrieved and selected from the Genome-Wide Associations Studies (GWAS) catalog. Although a number of at-risk genes varied among different diseases, these counts did not influence the number of shared-neighboring genes between a specific disease and HIV infection. For example, with only one at-risk gene of vascular dementia, the shared-neighboring genes between vascular dementia and HIV infection were higher than those between HIV and other diseases with more number of at-risk genes (S1 Table). The higher or lower number of shared-neighboring genes may reflect how close or distant a specific disease phenotype may appear during the neuroAIDS condition. Functional analysis of the network of shared-neighboring genes shows the involvement of several important functional pathways (S2 Data). This suggests neuroAIDS involvement in dysregulation of those basic neuronal metabolic machineries which are common to various neuro-disorders. Moreover, detail assessment of network topology reveal interactions of shared genes with at-risk genes (genetic loci) associated with both HIV infection and neurological disorders (Fig 1 & S2 Data). Several studies have implicated same genes or mutations in more than one neuro-disorder. In fact, these kinds of observations are reminiscent for autoimmune disorders. This genetic commonality (close association) may potentiate susceptibility of other neurological disorders and their phenotypic signature may have a reflection in clinical symptoms from the onset of neuroAIDS. In fact, studies have shown that copy number variants and differences in the temporal expression of a gene associated with a neurological disorder can put at risk of others [52].
Large-scale genetic network comparison involving multiples diseases of similar nature may unearth common genetic risk factors associated with a range of neurological illness. The venn analysis of shared-neighboring genes revealed a common set of 10 genes among HIV infection Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, age macular degeneration (Fig 2: EGFR, AKT1, GRB2, MAPK3, IKBKB, CD40, CD14, IRAK1, CD3E, and SYT1). Unlike Mendelian neuro-disorder, these four diseases are sporadic in nature where a slow progressive clinical course and neuronal loss with regional CNS specificity is acquired with their onset [3,52]. Even they feature similar mechanistic characteristics such as apoptosis, generation of reactive oxygen species, generation of proinflammatory factors, ionic channel modulations, and synaptodendritic injury. Sporadic neurodegenerative diseases generally involve modulation of multiple genetic factors at their molecular level [3]. Common genes discovered in this study have also been shown to play a significant role in the pathogenesis of these diseases. EGFR signaling plays a significant role in maintaining neuro-metabolic activities related to neurogenesis and neuron survival. Regulation of EGFR endocytosis via parkin protein drives Parkinson’s pathology [53]. In the case of Alzheimer’s disease, EGFR targeting has been proposed to treat amyloid-β induced memory loss [54]. Increased EGFR expression in cell bodies of astrocytes during multiple sclerosis suggests their role in pathological plaques [55]. The AKT signaling constitutes a significant part of major molecular pathways and has multifaceted role including neuroprotection, cell proliferation, and apoptosis inhibition. Inhibition of Akt signaling associated pathways can be a target for reducing age-related macular degeneration [56] Alzheimer’s disease [57], and Parkinson’s disease [58]. The PI3K/Akt signaling pathway is also involved in mediating an inflammatory response in multiple sclerosis [59]. GRB2 promotes autophagic removal of amyloid-β precursor overload and reduces Alzheimer’s disease-like pathology in neuronal cells [60]. Other proteins of the common network, MAPK3, CD40, CD14, IRAK1, IKBKB, and SYT1 drives different neuropathology in one or other way and they have been discussed below. The role of several proteins such as CD3E from our common network is yet to be defined in these diseases. In fact, genomic signatures of common sporadic forms largely remain unknown [3]. Considering association of common genes in driving different pathologies, we believe a network of these 10 genes may serve as a common canonical microcircuit to establish a link on their pathobiology. Gene-network signature based on these common genes suggests modulations of several pathways such as immune response-activating signal transduction, toll-like receptor signaling, activation of immune response pattern recognition receptor signaling, MyD88-dependent signaling, etc.
The relevance of common gene circuit was further interrogated via mRNA microarray analysis in HIV infection model. Unlike active HIV infection, the latent infection persists for long period and serves as a long-lasting reservoir of rebound viremia. Subpopulations of various cell types have been reported to maintain HIV latency. Cells of monocyte-macrophage lineage can migrate to and from periphery to brain or vice-versa and infect immune-privileged central nervous system during HIV infection. In fact, HIV-infected monocytes/macrophages from the periphery are a major factor in infecting CNS and subsequently neuroAIDS progress which is aggravated with time by active and/or latent infection of macrophages-originated microglia cells and other brain cell types [8,15,17]. Monocytes/macrophages may be considered as stepping stone for neuroAIDS condition and examination of molecular changes in these cells during HIV infection may reveal an inkling of neuroAIDS inception. Significant changes in the expression of 17 out of 29 genes of the bioinformatically discovered common network are found in active and/or latent HIV-infected monocytes (Fig 3). This included the significant change in the expression of 4 at-risk genes of HIV infection (PARD3B, HCP5, HLA-B, and MICB). Neighboring gene circuit may vary depending on presence or absence of one or more dysregulated at-risk genes. At-risk genes in GWAS are based on the different population of patients where each population shows only one (in some cases more than one) at-risk gene dysregulation. Modulations of even a single at-risk gene may be sufficient for infection vulnerability in a specific patients or populations. In the same line, differential expression of specific genes (not all) from the shared network, in our monocytes based in vitro study, may be a reflection of cell-specific reaction to HIV infection where only one or few HIV-specific at-risk genes may get dysregulated. Nonetheless, possible dysregulation of all HIV-specific at-risk genes in different cell types—taken together in a body- cannot be neglected. Different cell types of a patient may include dysregulation of all HIV-specific at-risk genes from GWAS and all common neighboring genes as well. This may be revealed by extending this preliminary study to the other cell types from periphery and brain region. Differentially expressed genes in monocytes, from our common network, have been correlated with different neuronal injury as exampled next. Mutations in SYT1 gene, which binds to SNARE complex, perturb synaptic vesicle cycling [61]. A point mutation in PTPRC gene is strongly associated with multiple sclerosis in the German population [62]. IRAK1 is one of the major genes that drive postnatal nervous system development and is differentially regulated in Alzheimer’s disease and in stressed human astroglial cells [63,64]. Gene AP1B1 has been correlated with the neural-regulated micro-exon in autism spectrum disorder [65]. EGFR is related to oligodendrocyte specification [66] and is a well-established gene for treating neurological disorders. Blocking of EGFR attenuates astrogliosis and protects against ischemic brain injury [67]. Altered expression of CD180 has been reported in peripheral blood leukocytes of Parkinson’s patients [68] and it is significantly dysregulated during cortical-striatal circuit dysfunction [69]. Mutation in IKBKG gene is closely related to CNS anomalies in incontinentia pigmenti patients [70] and Alzheimer’s disease [71]. The role of MAPK pathways is shown in neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis [72]. The CD40 promotes macrophages/microglia-induced inflammatory response and its interaction with CD154 enhances neurotoxins secretion [73]. Deletion of CD14 attenuates Alzheimer’s disease pathology [74] and polymorphism in a CD14 monocyte receptor is a genetic risk factor for Parkinson’s disease [75]. The PELI2 gene is differentially expressed in human neural progenitor cells containing overexpressed MEF-2 transcriptional factor which is a key determinant in synaptic plasticity and neuronal survival [76]. Also, PELI2 is one of the conserved targets of a brain-enriched microRNA, miRNA-128 which is differentially expressed in brain tumors and neuronal differentiation [77]. The CDKN1B (p27) regulates oligodendrocyte differentiation [78] and neurogenesis in the adult subventricular zone [79]. Interaction of CDKN1B with HIV Tat in driving neurotoxicity has been shown earlier [80,81]. The RPS6KA2 gene can influence brain network related to attention performance [82] and in glioma tumor formation [83]. Similarly, other genes of the common gene-circuits (Fig 2) regulate different aspects of neuronal regulations in one or other way. Once again, aforementioned correlation of altered genes expression during HIV infection should be seen as a reflection of complex neuroAIDS condition where characteristics of various neuronal pathologies appear. Therefore, the bioinformatically discovered common pathway in our study may have remarkable relevance in driving neuroAIDS condition. Nonetheless, an in vitro condition represents only a short HIV infection period in very specific artificial circumstances which can be little compared to the complex physiological networks in the body. The relevance of network discovered in our study should be considered cautiously while comparing with an infected subject. This should only be seen in a context to provide a prospective platform that how gene-circuits belonging to other neuro-disorders may be convoluted during real-time neuroAIDS condition. Again, an extension of this study to different cell types and/or population may reveal a more reasonable representation to be emulated for the real-time condition.
Moreover, we discovered a novel shared gene-network among neurological disorders (excluding HIV infection). Venn analysis of neighboring interactants of Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Age Macular Degeneration, Amyotrophic Lateral Sclerosis, Vascular Dementia, and Restless Leg Syndrome revealed a common set of 15 genes among these disorders (S2 Data and Fig 3). The visual network of these common genes showed the involvement of various innate immunity pathways suggesting commonalities in the immunological basis of different neuropathogenesis (Figs 2 & 3). Nonetheless, this network possesses little molecular crossover with the HIV infection-specific shared gene-circuit. This insinuates towards a different neuro-immunological molecular mechanism of neuroAIDS in compare to other neurological disorders. It is possible that difference in the expression of these marker genes and their genomic network(s) may unravel the common mechanism of sporadic neuro-disorders. Nonetheless, this can only represent a small subset of the network when the arrangement of billions of networks are dictated on the basis of neuronal cell morphology, electrophysiological properties, and choreography of the biosynthesis, trafficking and molecular interactions and connectivity [84]. Non-specific effects of disease-causing genomic mutations are putatively believed to be key driving factors of neuro-disorders and as such genes in common networks may provide a clue for additional risk factors. However, the in silico analysis based on publically available database possess an important caveat in their technical noise associated with the accuracy of clinical annotations. This is due to the variable quality of measurements in the different data source. Notably, this makes comparisons across different data sets challenging and any discovery solely based on in silico approach is unlikely to have clinical acceptance [85]. Exploratory follow-ups of these in silico findings—involving clinical resolution—may substantiate the gene functional similarities between the diseases. It is possible that quantitative variations of common genes set, depending upon individual genetic background, may drive either the presence or absence of specific neuro-disorders type. Prevailing inter-individual variability in neuroAIDS conditions among HIV patients–which is also a major confounding factor in the utility of in silico analysis–can be decoded by knowing if and when aspects of “on-and-off” switching of specific identified genes. This will require a systematic proof-of-concept study by first-hand verification of in silico findings in primary cells from uninfected and/or from HIV-infected individuals. Such study may reveal presence or absence of identified genes and effects of donor variation on gene targets in real time infection scenario. An extension of our analysis based on different peripheral and neuronal cell lines from infected individuals will be able to provide a wider screen to correlate progression of neuroAIDS to other neurological diseases. Furthermore, since the majority of genes from our discovered pathways target various inflammatory effects, a calculated effort towards immunosuppressive therapies (based on common genes) may prove critical for treatment of neuroAIDS and/or other neuropathologies.
In summary, the HAART treatment regimen has increased the longevity of HIV patients in recent years; nonetheless, it is ineffective on checking neuroAIDS which, in turn, has shaped up as a global problem. Currently, specific diagnosis tools or protocols for this epidemic is lacking in entirety. The classification of gene-network signatures of functionally associated neuropathology will dissect the multifaceted nature of the neuroAIDS condition and will provide a platform to prioritize genetic biomarkers and drug targets. In fact, the geno-bioinformatics analysis in this post-genomic era possesses unrealized opportunities to delineate molecular mechanisms of several neuro-disorders which are not feasible via conventional neurological examination. Such potential for neurodegenerative disorders is even higher because they show similar lesions and as such clues to their origin may be found in common genes circuit.
Ethics approval and consent to participate
As this study did not involve any animal or human participants, human data or human tissue, ethical committee approval is not required.
Supporting information
A control experiment was performed to determine presence of latent HIV in U1 cells. As such U1 cells were activated by PMS (10 nM) for 4 hr, washed with PBS, and cultured for 5 days. The p24 quantification study in culture supernatant suggests original U1 cells are latent because exposure of PMA resulted in very high load of p24 antigens.
(DOCX)
A control experiment was performed to determine initiation of active infection in U 937 cells. As such U937 cells were activated by PMS (10 nM) for 4 hr, washed with PBS, and infected with HIV for 5 days. The p24 quantification study in culture supernatant suggests active HIV infection in U937 cells.
(DOCX)
Venn analysis of neighboring genes between AIDS an each neurological disorders revealed their shared genes.
(DOCX)
Shared neighboring genes between AIDS and different neurological disorders.
(XLSX)
Visual networks of shared genes of AIDS and different neurological networks reveales involvement of several important functional pathways.
(XLSX)
Common genes from gene interactants of different neurological disorders are represented.
(XLSX)
At-risk alleles of AIDS and twelve major neurological disorders from GWAS catalog have been listed.
(XLSX)
Acknowledgments
This work was supported in part by grants R01DA040537, R01DA034547, and 1R03DA037782 from the National Institute of Health.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported in part by grants R01DA040537, R01DA034547, 1R21MH101025 and 1R03DA037782 from the National Institute of Health.
References
- 1.Tsuji S. Genetics of neurodegenerative diseases: Insights from high-throughput resequencing. Hum Mol Genet. 2010;19(R1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarroll SA, Feng G, Hyman SE. Genome-scale neurogenetics: methodology and meaning. Nat Neurosci [Internet]. 2014;17(6):756–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24866041 doi: 10.1038/nn.3716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitsui J, Tsuji S. Genomic aspects of sporadic neurodegenerative diseases. Biochem Biophys Res Commun [Internet]. 2014. [cited 2017 Apr 27];452(2):221–5. Available from: http://www.sciencedirect.com/science/article/pii/S0006291X14013473 doi: 10.1016/j.bbrc.2014.07.098 [DOI] [PubMed] [Google Scholar]
- 4.Letendre SL, Ellis RJ, Everall I, Ances B, Bharti A, McCutchan JA. Neurologic complications of HIV disease and their treatment. Top HIV Med. 2009;17(2):46–56. [PMC free article] [PubMed] [Google Scholar]
- 5.Singer EJ, Valdes-Sueiras M, Commins D, Levine A. Neurologic Presentations of AIDS. Neurol Clin [Internet]. 2010. [cited 2017 Apr 14];28(1):253–75. Available from: http://www.sciencedirect.com/science/article/pii/S0733861909000747 doi: 10.1016/j.ncl.2009.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sagar V, Pilakka-Kanthikeel S, Pottathil R, Saxena SK, Nair M. Towards nanomedicines for neuroAIDS. Rev Med Virol. 2014;24(2):103–24. doi: 10.1002/rmv.1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology [Internet]. 2007. October 30;69(18):1789–99. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4472366/ doi: 10.1212/01.WNL.0000287431.88658.8b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kramer-Hämmerle S, Rothenaigner I, Wolff H, Bell JE, Brack-Werner R. Cells of the central nervous system as targets and reservoirs of the human immunodeficiency virus. Virus Res [Internet]. 2005. [cited 2017 Apr 14];111(2):194–213. Available from: http://www.sciencedirect.com/science/article/pii/S0168170205001231 doi: 10.1016/j.virusres.2005.04.009 [DOI] [PubMed] [Google Scholar]
- 9.Gray F, Scaravilli F, Everall I, Chretien F, An S, Boche D, et al. Neuropathology of early HIV-1 infection. Brain Pathol. 1996;6(1 996):1–15. [DOI] [PubMed] [Google Scholar]
- 10.Anthony IC, Bell JE. The Neuropathology of HIV/AIDS. Int Rev Psychiatry. 2008;20(1):15–24. doi: 10.1080/09540260701862037 [DOI] [PubMed] [Google Scholar]
- 11.Burdo TH, Lackner A, Williams KC. Monocyte/Macrophages And Their Role In Hiv Neuropathogenesis. Immunol Rev. 2013;254(1):102–13. doi: 10.1111/imr.12068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boven LA, Middel J, Breij EC, Schotte D, Verhoef J, Soderland C, et al. Interactions between HIV-infected monocyte-derived macrophages and human brain microvascular endothelial cells result in increased expression of CC chemokines. J Neurovirol. 2000;6(5):382–9. [DOI] [PubMed] [Google Scholar]
- 13.Conant K, McArthur JC, Griffin DE, Sjulson L, Wahl LM, Irani DN. Cerebrospinal fluid levels of MMP-2,7, and 9 are elevated in association with human immunodeficiency virus dementia. [Internet]. Vol. 46, Annals of Neurology. 1999. p. 391–8. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc3&NEWS=N&AN=1999-11362-006 [DOI] [PubMed] [Google Scholar]
- 14.Sporer B, Paul R, Koedel U, Grimm R, Wick M, Goebel FD, et al. Presence of matrix metalloproteinase-9 activity in the cerebrospinal fluid of human immunodeficiency virus-infected patients. J Infect Dis. 1998;178(3):854–7. [DOI] [PubMed] [Google Scholar]
- 15.Atluri VSR, Hidalgo M, Samikkannu T, Kurapati KRV, Jayant RD, Sagar V, et al. Effect of human immunodeficiency virus on blood-brain barrier integrity and function: an update. Front Cell Neurosci [Internet]. 2015;9(June):212 Available from: http://journal.frontiersin.org/article/10.3389/fncel.2015.00212/abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bissel SJ, Wiley CA. Human Immunodeficiency Virus Infection of the Brain: Pitfalls in Evaluating Infected/Affected Cell Populations. Brain Pathol [Internet]. 2004;14(1):97–108. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1449744/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.González-Scarano F, Martín-García J. The neuropathogenesis of AIDS. Nat Rev Immunol. 2005;5(January):69–81. [DOI] [PubMed] [Google Scholar]
- 18.Kovalevich J, Langford D. Neuronal toxicity in HIV CNS disease. Future Virol [Internet]. 2012;7(7):687–98. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3632417&tool=pmcentrez&rendertype=abstract doi: 10.2217/fvl.12.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alexaki A, Liu Y, Wigdahl B. Cellular reservoirs of HIV-1 and their role in viral persistence. Curr HIV Res [Internet]. 2008;6(5):388–400. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2683678&tool=pmcentrez&rendertype=abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chun TW, Davey RT, Ostrowski M, Shawn Justement J, Engel D, Mullins JI, et al. Relationship between pre-existing viral reservoirs and the re-emergence of plasma viremia after discontinuation of highly active anti-retroviral therapy. Nat Med. 2000;6:757–61. doi: 10.1038/77481 [DOI] [PubMed] [Google Scholar]
- 21.Deeks SG, Autran B, Berkhout B, Benkirane M, Cairns S, Chomont N, et al. Towards an HIV cure: a global scientific strategy. Nat Rev Immunol [Internet]. 2012;12(8):607–14. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3595991&tool=pmcentrez&rendertype=abstract doi: 10.1038/nri3262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Lint C, Bouchat S, Marcello A. HIV-1 transcription and latency: an update. Retrovirology [Internet]. 2013;10(1):67 Available from: http://retrovirology.biomedcentral.com/articles/10.1186/1742-4690-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McArthur JC, Brew BJ, Nath A. Neurological complications of HIV infection. Vol. 4, Lancet Neurology. 2005. p. 543–55. doi: 10.1016/S1474-4422(05)70165-4 [DOI] [PubMed] [Google Scholar]
- 24.de Almeida SM, Letendre S, Ellis R. Human immunodeficiency virus and the central nervous system. Braz J Infect Dis [Internet]. 2006;10(1):41–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16767315 [DOI] [PubMed] [Google Scholar]
- 25.Lindl KA, Marks DR, Kolson DL, Jordan-Sciutto KL. HIV-associated neurocognitive disorder: Pathogenesis and therapeutic opportunities. Vol. 5, Journal of Neuroimmune Pharmacology. 2010. p. 294–309. doi: 10.1007/s11481-010-9205-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nair M, Jayant RD, Kaushik A, Sagar V. Getting into the brain: Potential of nanotechnology in the management of NeuroAIDS. Adv Drug Deliv Rev [Internet]. 2016;103:202–17. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0169409X1630059X doi: 10.1016/j.addr.2016.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agrawal L, Louboutin JP, Marusich E, Reyes BAS, Van Bockstaele EJ, Strayer DS. Dopaminergic neurotoxicity of HIV-1 gp120: Reactive oxygen species as signaling intermediates. Brain Res. 2010;1306:116–30. doi: 10.1016/j.brainres.2009.09.113 [DOI] [PubMed] [Google Scholar]
- 28.Vesce S, Bezzi P, Rossi D, Meldolesi J, Volterra A. HIV-1 gp120 glycoprotein affects the astrocyte control of extracellular glutamate by both inhibiting the uptake and stimulating the release of the amino acid. FEBS Lett [Internet]. 1997. [cited 2017 May 17];411(1):107–9. Available from: http://www.sciencedirect.com/science/article/pii/S0014579397006741 [DOI] [PubMed] [Google Scholar]
- 29.Kong L- Y, Wilson BC, McMillian MK, Bing G, Hudson PM, Hong J- S. The Effects of the HIV-1 Envelope Protein gp120 on the Production of Nitric Oxide and Proinflammatory Cytokines in Mixed Glial Cell Cultures. Cell Immunol [Internet]. 1996. August [cited 2017 May 17];172(1):77–83. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0008874996902178 doi: 10.1006/cimm.1996.0217 [DOI] [PubMed] [Google Scholar]
- 30.Okamoto S, Kang Y- J, Brechtel CW, Siviglia E, Russo R, Clemente A, et al. HIV/gp120 Decreases Adult Neural Progenitor Cell Proliferation via Checkpoint Kinase-Mediated Cell-Cycle Withdrawal and G1 Arrest [Internet]. Vol. 1, Cell Stem Cell. 2007. [cited 2017 May 17]. Available from: http://www.sciencedirect.com/science/article/pii/S1934590907000768 [DOI] [PubMed] [Google Scholar]
- 31.Louboutin J- P, Strayer DS. Blood-Brain Barrier Abnormalities Caused by HIV-1 gp120: Mechanistic and Therapeutic Implications. Sci World J [Internet]. 2012;2012:1–15. Available from: http://www.hindawi.com/journals/tswj/2012/482575/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.King JE, Eugenin EA, Buckner CM, Berman JW. HIV tat and neurotoxicity. Microbes Infect [Internet]. 2006. [cited 2017 May 17];8(5):1347–57. Available from: http://www.sciencedirect.com/science/article/pii/S1286457906000049 doi: 10.1016/j.micinf.2005.11.014 [DOI] [PubMed] [Google Scholar]
- 33.James T, Nonnemacher MR, Wigdahl B, Krebs FC. Defining the roles for Vpr in HIV-1-associated neuropathogenesis. J Neurovirol [Internet]. 2016;22(4):403–15. Available from: http://dx.doi.org/10.1007/s13365-016-0436-5 doi: 10.1007/s13365-016-0436-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olivetta E, Percario Z, Fiorucci G, Mattia G, Schiavoni I, Dennis C, et al. HIV-1 Nef Induces the Release of Inflammatory Factors from Human Monocyte/Macrophages: Involvement of Nef Endocytotic Signals and NF-κB Activation. J Immunol [Internet]. 2003. February 15;170(4):1716 LP–1727. Available from: http://www.jimmunol.org/content/170/4/1716.abstract [DOI] [PubMed] [Google Scholar]
- 35.Acharjee S, Branton WG, Vivithanaporn P, Maingat F, Paul AM, Dickie P, et al. HIV-1 Nef expression in microglia disrupts dopaminergic and immune functions with associated mania-like behaviors. Brain Behav Immun [Internet]. 2014. [cited 2017 May 17];40:74–84. Available from: http://www.sciencedirect.com/science/article/pii/S0889159114000622 doi: 10.1016/j.bbi.2014.02.016 [DOI] [PubMed] [Google Scholar]
- 36.Atluri VSR, Kanthikeel SP, Reddy PVB, Yndart A, Nair MPN. Human Synaptic Plasticity Gene Expression Profile and Dendritic Spine Density Changes in HIV-Infected Human CNS Cells: Role in HIV-Associated Neurocognitive Disorders (HAND). PLoS One. 2013;8(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atluri VSR, Pilakka-Kanthikeel S, Samikkannu T, Sagar V, Kurapati KRV, Saxena SK, et al. Vorinostat positively regulates synaptic plasticity genes expression and spine density in HIV infected neurons: role of nicotine in progression of HIV-associated neurocognitive disorder. Mol Brain [Internet]. 2014;7(1):37 Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4040511&tool=pmcentrez&rendertype=abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samikkannu T, Atluri VSR, Arias AY, Rao KVK, Mulet CT, Jayant RD, et al. HIV-1 subtypes B and C Tat differentially impact synaptic plasticity expression and implicates HIV-associated neurocognitive disorders. Curr HIV Res [Internet]. 2014;12(6):397–405. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25613138%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4554345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Avdoshina V, Bachis A, Mocchetti I. Synaptic dysfunction in human immunodeficiency virus type-1-positive subjects: Inflammation or impaired neuronal plasticity? Vol. 273, Journal of Internal Medicine. 2013. p. 454–65. doi: 10.1111/joim.12050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Obulesu M, Lakshmi MJ. Apoptosis in Alzheimer’s Disease: An Understanding of the Physiology, Pathology and Therapeutic Avenues. Neurochem Res [Internet]. 2014;39(12):2301–12. Available from: http://dx.doi.org/10.1007/s11064-014-1454-4 doi: 10.1007/s11064-014-1454-4 [DOI] [PubMed] [Google Scholar]
- 41.Wang Q, Liu Y, Zhou J. Neuroinflammation in Parkinson’s disease and its potential as therapeutic target. Transl Neurodegener [Internet]. 2015. October 12;4:19 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4603346/ doi: 10.1186/s40035-015-0042-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Naegele M, Martin R. Chapter 3 –The good and the bad of neuroinflammation in multiple sclerosis. In: Handbook of Clinical Neurology [Internet]. 2014 [cited 2017 Apr 27]. p. 59–87. Available from: http://www.sciencedirect.com/science/article/pii/B9780444520012000030 [DOI] [PubMed]
- 43.Kauppinen A, Paterno JJ, Blasiak J, Salminen A, Kaarniranta K. Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci [Internet]. 2016. February 6;73:1765–86. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4819943/ doi: 10.1007/s00018-016-2147-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kurapati KRV, Atluri VSR, Samikkannu T, Nair MPN. Ashwagandha (Withania somnifera) Reverses β-Amyloid1-42 Induced Toxicity in Human Neuronal Cells: Implications in HIV-Associated Neurocognitive Disorders (HAND). PLoS One. 2013;8(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Repunte-Canonigo V, Lefebvre C, George O, Kawamura T, Morales M, Koob GF, et al. Gene expression changes consistent with neuroAIDS and impaired working memory in HIV-1 transgenic rats. Mol Neurodegener [Internet]. 2014;9:26 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4107468/ doi: 10.1186/1750-1326-9-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Santiago JA, Potashkin JA. Integrative network analysis unveils convergent molecular pathways in Parkinson’s disease and diabetes. PLoS One. 2013;8(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Santiago JA, Potashkin JA. A network approach to clinical intervention in neurodegenerative diseases. Vol. 20, Trends in Molecular Medicine. 2014. p. 694–703. doi: 10.1016/j.molmed.2014.10.002 [DOI] [PubMed] [Google Scholar]
- 48.Ruan Q, Dutta D, Schwalbach MS, Steele JA, Fuhrman JA, Sun F. Local similarity analysis reveals unique associations among marine bacterioplankton species and environmental factors. Bioinformatics. 2006;22(20):2532–8. doi: 10.1093/bioinformatics/btl417 [DOI] [PubMed] [Google Scholar]
- 49.Nair M, Sagar V, Pilakka-Kanthikeel S. Gene-expression reversal of lncRNAs and associated mRNAs expression in active vs latent HIV infection. Sci Rep [Internet]. 2016;6:34862 Available from: http://www.nature.com/articles/srep34862 doi: 10.1038/srep34862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pilakka-Kanthikeel S, Raymond A, Atluri VSR, Sagar V, Saxena SK, Diaz P, et al. Sterile alpha motif and histidine/aspartic acid domain-containing protein 1 (SAMHD1)-facilitated HIV restriction in astrocytes is regulated by miRNA-181a. J Neuroinflammation [Internet]. 2015;12:66 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4410490/ doi: 10.1186/s12974-015-0285-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Minagar A, Commins D, Alexander JS, Hoque R, Chiappelli F, Singer EJ, et al. NeuroAIDS: characteristics and diagnosis of the neurological complications of AIDS. Mol Diagn Ther [Internet]. 2008;12(1):25–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18288880 [DOI] [PubMed] [Google Scholar]
- 52.Zhu X, Need AC, Petrovski S, Goldstein DB. One gene, many neuropsychiatric disorders: lessons from Mendelian diseases. Nat Neurosci [Internet]. 2014;17(6):773–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24866043 doi: 10.1038/nn.3713 [DOI] [PubMed] [Google Scholar]
- 53.Fallon L, Belanger CML, Corera AT, Kontogiannea M, Regan-Klapisz E, Moreau F, et al. A regulated interaction with the UIM protein Eps15 implicates parkin in EGF receptor trafficking and PI(3)K-Akt signalling. Nat Cell Biol [Internet]. 2006. August;8(8):834–42. Available from: http://dx.doi.org/10.1038/ncb1441 doi: 10.1038/ncb1441 [DOI] [PubMed] [Google Scholar]
- 54.Wang L, Chiang H-C, Wu W, Liang B, Xie Z, Yao X, et al. Epidermal growth factor receptor is a preferred target for treating amyloid-β-induced memory loss. Proc Natl Acad Sci U S A [Internet]. 2012;109(41):16743–8. Available from: http://www.pnas.org/content/109/41/16743.short%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3478595&tool=pmcentrez&rendertype=abstract doi: 10.1073/pnas.1208011109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holley JE, Gveric D, Newcombe J, Cuzner ML, Gutowski NJ. Astrocyte characterization in the multiple sclerosis glial scar. Neuropathol Appl Neurobiol. 2003;29(5):434–44. [DOI] [PubMed] [Google Scholar]
- 56.Lin CH, Li CH, Liao PL, Tse LS, Huang WK, Cheng HW, et al. Silibinin inhibits VEGF secretion and age-related macular degeneration in a hypoxia-dependent manner through the PI-3 kinase/Akt/mTOR pathway. Br J Pharmacol. 2013;168(4):920–31. doi: 10.1111/j.1476-5381.2012.02227.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kitagishi Y, Nakanishi A, Ogura Y, Matsuda S. Dietary regulation of PI3K/AKT/GSK-3β pathway in Alzheimer’s disease. Alzheimers Res Ther [Internet]. 2014;6(3):35 Available from: http://alzres.com/content/6/3/35 doi: 10.1186/alzrt265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xiromerisiou G, Hadjigeorgiou GM, Papadimitriou A, Katsarogiannis E, Gourbali V, Singleton AB. Association between AKT1 gene and Parkinson’s disease: A protective haplotype. Neurosci Lett. 2008;436(2):232–4. doi: 10.1016/j.neulet.2008.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sospedra M, Martin R. Immunology of Multiple Sclerosis. Semin Neurol. 2016;36(2):115–27. doi: 10.1055/s-0036-1579739 [DOI] [PubMed] [Google Scholar]
- 60.Roy K, Raychaudhuri M, Chakrabarti O, Mukhopadhyay D. Growth factor receptor-bound protein 2 promotes autophagic removal of amyloid-?? protein precursor intracellular domain overload in neuronal cells. J Alzheimer’s Dis. 2014;38(4):881–95. [DOI] [PubMed] [Google Scholar]
- 61.Baker K, Gordon SL, Grozeva D, van Kogelenberg M, Roberts NY, Pike M, et al. Identification of a human synaptotagmin-1 mutation that perturbs synaptic vesicle cycling. J Clin Invest [Internet]. 2015;125(4):1670–8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4396464/ doi: 10.1172/JCI79765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bomprezzi R, Kovanen P, Martin R. New approaches to investigating heterogeneity in complex traits. J Med Genet [Internet]. 2003. August;40(8):553–9. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1735544/ doi: 10.1136/jmg.40.8.553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang Q, Zhao Y, Yang Y, Bao X. MECP2 duplication syndrome in a Chinese family. BMC Med Genet [Internet]. 2015;16:112 Available from: http://dx.doi.org/10.1186/s12881-015-0264-0%5Cnhttp://bmcmedgenet.biomedcentral.com/articles/10.1186/s12881-015-0264-0%5Cnhttp://bmcmedgenet.biomedcentral.com/track/pdf/10.1186/s12881-015-0264-0?site=bmcmedgenet.biomedcentral.com doi: 10.1186/s12881-015-0264-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cui JG, Li YY, Zhao Y, Bhattacharjee S, Lukiw WJ. Differential regulation of interleukin-1-receptor-associated kinase-1 (IRAK-1) and IRAK-2 by micro RNA-146a and NF-{kappa}B in stressed human astroglial cells and in Alzheimer’s disease. J Biol Chem [Internet]. 2010;285(50):38951–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20937840 doi: 10.1074/jbc.M110.178848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Irimia M, Weatheritt RJ, Ellis J, Parikshak NN, Gonatopoulos-Pournatzis T, Babor M, et al. A highly conserved program of neuronal microexons is misregulated in autistic brains. Cell [Internet]. 2014. December 18;159(7):1511–23. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4390143/ doi: 10.1016/j.cell.2014.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galvez-Contreras AY, Quiñones-Hinojosa A, Gonzalez-Perez O. The role of EGFR and ErbB family related proteins in the oligodendrocyte specification in germinal niches of the adult mammalian brain. Front Cell Neurosci [Internet]. 2013. December 17;7:258 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865447/ doi: 10.3389/fncel.2013.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang Q, Wang E- Y, Huang X- J, Qu W- S, Zhang L, Xu J- Z, et al. Blocking epidermal growth factor receptor attenuates reactive astrogliosis through inhibiting cell cycle progression and protects against ischemic brain injury in rats. J Neurochem [Internet]. 2011;119(3):644–53. Available from: http://dx.doi.org/10.1111/j.1471-4159.2011.07446.x doi: 10.1111/j.1471-4159.2011.07446.x [DOI] [PubMed] [Google Scholar]
- 68.Kedmi M, Bar-Shira A, Gurevich T, Giladi N, Orr-Urtreger A. Decreased expression of B cell related genes in leukocytes of women with Parkinson’s disease. Mol Neurodegener [Internet]. 2011;6(1):66 Available from: http://www.molecularneurodegeneration.com/content/6/1/66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chambers RA, McClintick JN, Sentir AM, Berg SA, Runyan M, Choi KH, et al. Cortical–striatal gene expression in neonatal hippocampal lesion (NVHL)-amplified cocaine sensitization. Genes Brain Behav [Internet]. 2013. July 22;12(5):564–75. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4170677/ doi: 10.1111/gbb.12051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Minić S, Trpinac D, Obradović M. Systematic review of central nervous system anomalies in incontinentia pigmenti. Orphanet J Rare Dis [Internet]. 2013;8:25 Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3576363&tool=pmcentrez&rendertype=abstract doi: 10.1186/1750-1172-8-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu Y, Liu X, Hao W, Decker Y, Schomburg R, Fulop L, et al. IKKbeta deficiency in myeloid cells ameliorates Alzheimer’s disease-related symptoms and pathology. J Neurosci [Internet]. 2014;34(39):12982–99. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25253847 doi: 10.1523/JNEUROSCI.1348-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim EK, Choi E- J. Pathological roles of MAPK signaling pathways in human diseases. Biochim Biophys Acta—Mol Basis Dis [Internet]. 2010;1802(4):396–405. Available from: http://www.sciencedirect.com/science/article/pii/S0925443910000153 [DOI] [PubMed] [Google Scholar]
- 73.Benveniste EN, Nguyen VT, Wesemann DR. Molecular regulation of CD40 gene expression in macrophages and microglia. Vol. 18, Brain, Behavior, and Immunity. 2004. p. 7–12. [DOI] [PubMed] [Google Scholar]
- 74.Reed-Geaghan EG, Reed QW, Cramer PE, Landreth GE. Deletion of CD14 attenuates Alzheimer’s disease pathology by influencing the brain’s inflammatory milieu. J Neurosci [Internet]. 2010;30(46):15369–73. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2997622&tool=pmcentrez&rendertype=abstract doi: 10.1523/JNEUROSCI.2637-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lin JJ, Chen CH, Yueh KC, Chang CY, Lin SZ. A CD14 monocyte receptor polymorphism and genetic susceptibility to Parkinson’s disease for females. Parkinsonism Relat Disord [Internet]. 2006. [cited 2017 Apr 27];12(1):9–13. Available from: http://www.sciencedirect.com/science/article/pii/S1353802005001586 doi: 10.1016/j.parkreldis.2005.07.010 [DOI] [PubMed] [Google Scholar]
- 76.Chan SF, Huang X, McKercher SR, Zaidi R, Okamoto S, Nakanishi N, et al. Transcriptional profiling of MEF2-regulated genes in human neural progenitor cells derived from embryonic stem cells. Genomics Data [Internet]. 2015. March 7;3:24–7. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4255278/ doi: 10.1016/j.gdata.2014.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Adlakha YK, Saini N. Brain microRNAs and insights into biological functions and therapeutic potential of brain enriched miRNA-128. Mol Cancer [Internet]. 2014;13:33 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24555688%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3936914 doi: 10.1186/1476-4598-13-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Larocque D, Galarneau A, Liu H- N, Scott M, Almazan G, Richard S. Protection of p27(Kip1) mRNA by quaking RNA binding proteins promotes oligodendrocyte differentiation. Nat Neurosci. 2005;8(1):27–33. doi: 10.1038/nn1359 [DOI] [PubMed] [Google Scholar]
- 79.Gil-Perotin S, Haines JD, Kaur J, Marin-Husstege M, Spinetta MJ, Kim KH, et al. Roles of p53 and p27 Kip1 in the regulation of neurogenesis in the murine adult subventricular zone. Eur J Neurosci. 2011;34(7):1040–52. doi: 10.1111/j.1460-9568.2011.07836.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou BY, He JJ. Proliferation inhibition of astrocytes, neurons, and non-glial cells by intracellularly expressed human immunodeficiency virus type 1 (HIV-1) Tat protein. Neurosci Lett. 2004;359(3):155–8. doi: 10.1016/j.neulet.2004.02.012 [DOI] [PubMed] [Google Scholar]
- 81.Fields JA, Dumaop W, Crews L, Adame A, Spencer B, Metcalf J, et al. Mechanisms of HIV-1 Tat Neurotoxicity via CDK5 Translocation and Hyper-Activation: Role in HIV-Associated Neurocognitive Disorders. Curr HIV Res [Internet]. 2015;13(1):43–54. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455959/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.J. Feng, C. Chen, Q. Dong GX. RPS6KA2 gene is associated with attention: A preliminary imaging genetic study. In: 21st Annual meeting of the Organization for Human Brain Mapping. Hawaii Convention Center, Honolulu, Hawaii, June 14-18th, 2015.; 2015.
- 83.Baxter PA, Lin Q, Mao H, Kogiso M, Zhao X, Liu Z, et al. Silencing BMI1 eliminates tumor formation of pediatric glioma CD133+ cells not by affecting known targets but by down-regulating a novel set of core genes. Acta Neuropathol Commun [Internet]. 2014. December 20;2:160 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4289398/ doi: 10.1186/s40478-014-0160-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kitchen RR, Rozowsky JS, Gerstein MB, Nairn AC. Decoding neuroproteomics: integrating the genome, translatome and functional anatomy. Nat Neurosci [Internet]. 2014;17(11):1491–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25349915 doi: 10.1038/nn.3829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pusztai L, Leyland-Jones B. Promises and caveats of in silico biomarker discovery. Br J Cancer [Internet]. 99(3):385–6. Available from: http://dx.doi.org/10.1038/sj.bjc.6604495. doi: 10.1038/sj.bjc.6604495 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A control experiment was performed to determine presence of latent HIV in U1 cells. As such U1 cells were activated by PMS (10 nM) for 4 hr, washed with PBS, and cultured for 5 days. The p24 quantification study in culture supernatant suggests original U1 cells are latent because exposure of PMA resulted in very high load of p24 antigens.
(DOCX)
A control experiment was performed to determine initiation of active infection in U 937 cells. As such U937 cells were activated by PMS (10 nM) for 4 hr, washed with PBS, and infected with HIV for 5 days. The p24 quantification study in culture supernatant suggests active HIV infection in U937 cells.
(DOCX)
Venn analysis of neighboring genes between AIDS an each neurological disorders revealed their shared genes.
(DOCX)
Shared neighboring genes between AIDS and different neurological disorders.
(XLSX)
Visual networks of shared genes of AIDS and different neurological networks reveales involvement of several important functional pathways.
(XLSX)
Common genes from gene interactants of different neurological disorders are represented.
(XLSX)
At-risk alleles of AIDS and twelve major neurological disorders from GWAS catalog have been listed.
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.