Abstract
Background: Prior studies indicate that chronic stress is associated with obesity in adults. However, whether parental/caregiver stress is associated with obesity in their offspring has not been widely examined in Hispanic/Latino populations. In this study, we evaluated the role of caregiver chronic stress on child obesity and whether home food environment or child lifestyle behaviors explained the association.
Methods: The study included a sample of Hispanic/Latino youth and their caregivers (n = 473) from the Study of Latinos (SOL) Youth study and the Hispanic Community Health Study/SOL Sociocultural Study, which enrolled children aged 8–16 years from four cities (Bronx, Chicago, Miami, and San Diego), and provided assessments of adult chronic stress. Poisson regression models were used to assess the association between parental/caregiver stress and child obesity, adjusting for potential confounders.
Results: Twenty-two percent of caregivers did not report any chronic stressors, 48% reported 1–2, and 29% reported ≥3 stressors. The prevalence of obesity in youth increased with number of caregiver stressors from 23% among those without caregiver stressors to 35% among those with ≥3 stressors (p for trend 0.03). After model adjustment, youths whose caregivers reported ≥3 stressors were more likely to be obese than youths whose caregivers reported no stressors (prevalence ratio = 1.53; 95% confidence interval 1.01–2.32). This association was independent of food home environment, child diet quality, and child physical activity, but it was not independent of caregiver obesity.
Conclusions: These findings suggest that parental/caregiver chronic stress is related to obesity in their children. Future research is needed to confirm this association in longitudinal studies and in other population groups.
Keywords: : obesity, caregiver stress, youth, home environment
Introduction
Prior studies in adults indicate that psychosocial stress is related to cardiovascular disease risk.1,2 In the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), we showed that among Hispanic/Latino adults, chronic stress is associated with traditional cardiovascular risk factors, obesity, and lower diet quality.3,4 In particular, chronic stress was associated with obesity and adiposity measures (waist circumference and percentage body fat), associations that were independent of energy intake and physical activity.4 There is a growing literature in adolescents suggesting that psychosocial stress is associated with unhealthy lifestyle behaviors and excess weight.5–8
Relationships between some aspects of the family context and youth responses to stress are well documented.9–11 For example, findings from recent studies link poverty,12 family conflict,13,14 and parental mental health15,16 to youth's biological stress dysregulation. A recent meta-analysis also indicated that parental psychosocial stress is associated with youth's obesity status.17 In this regard, data from NHANES showed that there was a higher likelihood of childhood obesity in stressed mothers from food-secure households,18 an association that was not found among food-insecure households. Another study of Swedish young children reported higher odds of obesity in children from families reporting higher stress levels.19
Elevated stress in parents could affect the characteristics of the home environment, decreasing the availability of healthy foods and support for physical activity, which in turn could contribute to obesity in their children. Parenting practices, such as monitoring and limit setting, are associated with children's food intake and TV time,20–22 on the other hand, parental psychosocial stress could also affect parenting practices23 and therefore it could increase the risk of obesity in the child by increasing obesogenic lifestyle behaviors (high energy intake and increased sedentary time).
In this study, we examined the association of caregiver chronic and perceived stress with obesity in their children in a sample of low-income Hispanic/Latino youth, a population that has been understudied and whose families are at high risk of obesity and experience high levels of stress.3,4 We also tested whether this association was explained by the food home environment or youth's lifestyle behaviors (e.g., diet and physical activity) to understand potential mediators of the association between caregiver stress and obesity in youth.
Methods
HCHS/SOL is a population-based cohort study of 16,415 Hispanic/Latino adults (ages 18–74 years) who were selected using two-stage probability sampling design from four US communities (Chicago, IL; Miami, FL; Bronx, NY; and San Diego, CA). The HCHS/SOL Sociocultural Ancillary Study (SCAS) enrolled 5313 participants from HCHS/SOL between February 2010 and June 2011, with a participation rate of 85%.24 Participants were asked to return to the HCHS/SOL clinic within 9 months of their baseline examination to complete a comprehensive set of psychosocial measures that included self-reported stress. However, the majority of participants (72%) completed the psychosocial assessment within 4 months.
SOL Youth is an ancillary study to HCHS/SOL that enrolled a subset of the offspring of HCHS/SOL participants from the same four field centers. Between 2012 and 2014, 6741 households were screened by a phone call using a standardized script; the screening identified 1777 eligible children between the ages of 8–16 years, of whom 1466 were enrolled, achieving a participation rate of 82%. Details about the aims and methodology of HCHS/SOL, SOL Youth, and HCHS/SOL SCAS are published elsewhere.24–28
The study was conducted with approvals of the Institutional Review Boards of each of the institutions involved in the study (Albert Einstein College of Medicine, Feinberg School of Medicine, Northwestern University, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, University of Miami Miller School of Medicine, and San Diego State University). For this analysis, a subset of the SOL Youth sample was identified in which 680 children had parents who also participated in SCAS and completed the chronic stress scale. One child per family was randomly selected leaving a final analytic sample of 473 children. Included and excluded children were similar in age and sex distribution, sociodemographic characteristics, and obesity.
Measures
Obesity
Child and caregiver height and weight were obtained at each field center. Height (cm) was measured with a wall stadiometer (SECA 222, Germany) and weight (kg) was obtained with a digital scale (Tanita Body Composition Analyzer, TBF 300, Japan). Weight categories in the child were defined using age- and sex-specific percentile.29 Obesity in the adult was defined as BMI ≥ 30.
Chronic stress burden
Chronic stress burden (8 items) asked parents/caregivers about ongoing stressors in important life domains (health, work, and relationships) that have lasted for at least 6 months.30,31 The validity of this instrument in this population is supported by theoretically expected associations with adult obesity and cardiovascular disease risk factors.3,4 A score was created by summing the number of ongoing stressors reported (range 0–8), which was later categorized into number of reported stressors (0, 1, 2, or ≥3).
Perceived stress scale
Perceived stress scale32 queried participants' perceptions of feeling stressed during the last month (10 items). Responses were on a five-point scale from never to very often. Scores were summed to indicate current stress levels, with higher scores suggesting greater perceived stress (Cronbach's α for participants answering questionnaire in English = 0.86; Cronbach's α = 0.84 in Spanish).
Home food environment
Home food environment (17 items) asked parents/caregivers about the availability at home of food items such as fruit and vegetables, milk, juices, sugared beverages, chips, and other types of snacks during the past month. Response items ranged from never to always. This measure was adapted from the 3-day Home Food Environment Survey to assess healthful and less healthful food items that are most common in households.33–35 This 17-item scale has been used in multiethnic samples of adolescents with good reliability (Cronbach's α varying from 0.60 to 0.83) and expected associations with dietary intake.33–35 A score for home food environment was created by summing responses of each item, and a higher score indicated a healthier home environment.
Healthy Eating Index 2010
Child dietary intake was obtained with two interviewer-administered 24-hour recalls using the Nutrition Data System for Research software developed by the University of Minnesota. Healthy Eating Index 2010 (HEI-2010) is a measure of overall diet quality, independent of quantity, derived from twelve dietary components that reflect key aspects of dietary quality, including fruit, vegetables, grains, dairy, protein foods, fatty acids, sodium, and empty calories. HEI scores were calculated from the average of two 24-hour dietary recalls. HEI-2010 scores range from 0 to 100 with higher scores indicating greater adherence to the 2010 Dietary Guidelines for Americans.36
Physical activity and sedentary behavior
Detailed description of methods to assess physical activity is reported elsewhere.37 Participants were asked to wear an Actical accelerometer (version B-1, model 198-0200-03) positioned above the iliac crest, with removal only for swimming, showering, and sleeping, for 1 week. Data collected from 5:00 am the day following the clinic visit through midnight on day six were used for all participants. Epoch length was set to 15 seconds to capture more variable and intermittent activity patterns in youth.38
Nonwear time was defined as consecutive zero counts for at least 90 minutes, allowing for short time intervals with nonzero counts lasting up to 2 minutes if no counts were detected during both the 30 minutes upstream and downstream from that interval. Any nonzero counts except the allowed short intervals were considered as wear time.39 Data were summarized for children with at least three adherent days (wear time ≥8 to <19 hours/day) and were categorized into the following intensity levels according to the following cut points: sedentary (<18 counts/15-second epoch), light (18–440 counts/15 seconds), and moderate or vigorous (>440 counts/15 seconds).37,40
Sociodemographic variables
Participants also reported their Hispanic/Latino background (Central American, Cuban, Dominican, Mexican, Puerto Rican, South American, and other/mixed), age, sex, place of birth (foreign born vs. US born, a proxy for acculturation), and years living in the United States. Caregivers reported their annual household income and educational attainment.
Statistical Analyses
Percentages are presented for categorical variables, mean and standard deviation are presented for normally distributed continuous variables, and median and interquartile range are shown for skewed continuous variables. Due to non-normal distribution of the total number of stressors of parent/caregiver, stressor count was categorized into 4 groups (0, 1, 2, or ≥3). Poisson models with robust variance estimates were used to model the prevalence ratios of child obesity associated with the number of stressors. Models, including parental perceived stress, used this predictor as a continuous measure.
The models were adjusted for child age, sex, place of birth, household income, and field center. p-Values for linear trend were reported to examine the dose–response effect of childhood obesity prevalence by increased number of chronic stressors. We further adjusted for home food environment and objectively measured moderate to vigorous physical activity, sedentary time, HEI-2010, and caregiver obesity one at a time to assess the possibility of mediation through these variables. The daily average wear time of accelerometer was adjusted in models with physical activity or sedentary time.
Due to missing Actical data (25%), we conducted multiple imputations for missing physical activity, sedentary time, and wear time. We used monotone regression method in SAS to generate five imputation datasets. The imputation model included chronic stress, child age, sex, and place of birth, field center, and household income. Because of limited sample size in some strata, analyses were not stratified by child sex. All p-values were two-sided with a significance level at 0.05. All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
In this sample of Hispanic/Latino youth, 50% were males, 55% were between the ages of 8–12, 75% were born in the United States, and 44% were of Mexican heritage (Table 1). Fifty-seven percent of caregivers reported having a household income of ≤$20,000, and 29% of caregivers reported three or more chronic stressors. The majority of caregivers (80%) reported to be the child's biological mother, and 85% caregivers were born outside of the US 50 states. Sociodemographic characteristics and presence of obesity did not vary by child sex.
Table 1.
Characteristics of the Study Population
| Overall | Girls | Boys | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Age group | ||||||
| 8–12 | 260 | 55.0 | 116 | 49.8 | 144 | 60.0 |
| 13–14 | 129 | 27.3 | 72 | 30.9 | 57 | 23.8 |
| 15–16 | 84 | 17.8 | 45 | 19.3 | 39 | 16.3 |
| Nativity | ||||||
| Foreign born | 117 | 24.7 | 62 | 26.6 | 55 | 22.9 |
| US born | 352 | 74.4 | 169 | 72.5 | 183 | 76.3 |
| Missing | 4 | 0.8 | 2 | 0.9 | 2 | 0.8 |
| Hispanic/Latino group | ||||||
| Dominican | 61 | 12.9 | 30 | 12.9 | 31 | 12.9 |
| Puerto Rican | 36 | 7.6 | 18 | 7.7 | 18 | 7.5 |
| Cuban | 38 | 8.0 | 20 | 8.6 | 18 | 7.5 |
| Central American | 44 | 9.3 | 27 | 11.6 | 17 | 7.1 |
| Mexican | 193 | 40.8 | 97 | 41.6 | 96 | 40.0 |
| South American | 16 | 3.4 | 6 | 2.6 | 10 | 4.2 |
| Mixed/other | 55 | 11.6 | 24 | 10.3 | 31 | 12.9 |
| Missing | 30 | 6.3 | 11 | 4.7 | 19 | 7.9 |
| Household income | ||||||
| <$20k | 261 | 55.2 | 133 | 57.1 | 128 | 53.3 |
| $20 to <$40k | 134 | 28.3 | 66 | 28.3 | 68 | 28.3 |
| ≥$40k | 64 | 13.5 | 23 | 9.9 | 41 | 17.1 |
| Missing | 14 | 3.0 | 11 | 4.7 | 3 | 1.3 |
| Parental chronic stress | ||||||
| 0 | 105 | 22.2 | 46 | 19.7 | 59 | 24.6 |
| 1 | 123 | 26.6 | 70 | 30.0 | 53 | 22.1 |
| 2 | 106 | 22.4 | 49 | 21.0 | 57 | 23.8 |
| 3 or more | 139 | 29.4 | 68 | 29.2 | 71 | 29.6 |
| BMI | ||||||
| Obese | 139 | 29.4 | 63 | 27.0 | 76 | 31.7 |
| Overweight | 103 | 21.8 | 48 | 20.6 | 55 | 22.9 |
| Underweight/normal weight | 231 | 48.8 | 122 | 52.4 | 109 | 45.4 |
The number of caregivers' chronic stressors was positively associated with obesity in the offspring (Fig. 1); the proportion of youth with obesity increased with the number of caregivers' stressors from 23% among youth whose caregivers did not report any stressors to 35% among youth whose caregivers reported three or more stressors (p for linear trend = 0.03). In multivariate analyses (Table 2), after adjusting for potential confounders, youth with caregivers reporting ≥3 chronic stressors were more likely to be obese than those with caregivers without stressors (odds ratio = 1.56; 95% confidence interval 1.03–1.21). There was a linear response; as the number of caregivers' chronic stressors increased, the association became stronger (p for linear trend = 0.019). No interaction was found with child age or gender. The additional adjustment for home food environment did not substantially affect the magnitude of the association between caregiver chronic stress and child obesity. Similar findings were observed when adjusting for moderate/vigorous physical activity or sedentary time, suggesting that the association between caregiver stress and child obesity was independent of home environment, physical activity, and sedentary time. When the models were adjusted for child HEI, a measure of diet quality, the association of parental stress and child obesity was slightly attenuated. However, when the models were adjusted for caregiver obesity status, the association between caregiver stress and child obesity became nonsignificant (Table 2). Separate similar models were conducted to test the association of caregiver perceived stress with obesity in youth, but no association was observed.
Figure 1.
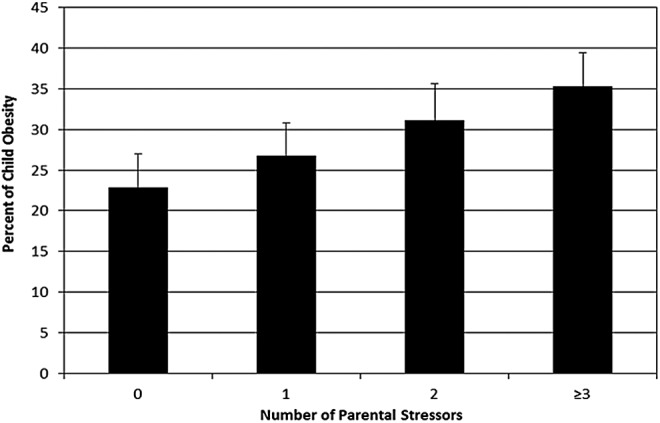
Percent of youth obesity by number of parental chronic stressors.
Table 2.
Prevalence Ratios for the Association between Parental Stress and Child Obesity
| PrR (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| Number of parental chronic stressors | ||||||
| 0 | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 | 1.15 (0.72–1.83) | 1.17 (0.73–1.86) | 1.17 (0.73–1.86) | 1.15 (0.72–1.84) | 1.14 (0.71–1.81) | 1.10 (0.69–1.75) |
| 2 | 1.38 (0.88–2.16) | 1.39 (0.89–2.19) | 1.35 (0.86–2.13) | 1.33 (0.84–2.10) | 1.36 (0.87–2.14) | 1.35 (0.86–2.12) |
| 3 or more | 1.56 (1.03–2.36) | 1.57 (1.04–2.38) | 1.58 (1.04–2.39) | 1.56 (1.03–2.37) | 1.53 (1.01–2.32) | 1.43 (0.94–2.11) |
| p for linear trend | 0.019 | 0.018 | 0.019 | 0.021 | 0.025 | 0.050 |
| Parental perceived stress | ||||||
| Per unit change | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) | 1.01 (0.99–1.04) | 1.01 (0.99–1.04) | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) |
Model 1 is adjusted by child age, child sex, child place of birth, household income, and field center. Model 2 is adjusted by covariates included in model 1 and additionally adjusted by home food environment. Model 3 is adjusted by covariates included in model 1 and additionally adjusted for objective moderate/vigorous activity and daily average wear time. Model 4 is adjusted by covariates included in model 1 and additionally adjusted for sedentary time and daily average wear time. Model 5 is adjusted by covariates included in model 1 and additionally adjusted for Healthy Eating Index 2010. Model 6 is adjusted by covariates included in model 1 and additionally adjusted for parental obesity.
95% CI, 95% confidence interval; PrR, prevalence ratio.
Discussion
Our main finding that caregiver chronic stress was associated with higher odds of obesity in their offspring is consistent with prior studies.18,19,41 It has been postulated that parents with high stress levels may lack the energy for keeping less obesogenic environments at home, for example, decreasing the availability of healthier food items, cooked meals, and regular family meals. At the same time, parents experiencing high levels of stress may lack the energy or may be time constrained for engaging their children in greater physical activity and for monitoring their children's food habits, all of which may result in higher child obesity risk.
In fact, studies have shown that parental psychosocial stress was related to family and child food habits. Results from Project-EAT showed that parental work–life stress was associated with less frequent family meals and higher fast-food intake.42 In another study, there was an association of family stressors on child BMI that reported to be mediated by less positive family meal patterns (e.g., eating meals together and eating meals prepared away from home).23 In a diverse sample of children and adolescents, higher number of parental stressors was significantly related to child obesity and child fast-food consumption, but not with self-reported child physical activity levels.43
We did not observe an association of parental perceived stress and obesity in their children, these results are consistent with our previous reports that indicate that the perceived stress scale, which asks for appraisals of stress during the past 30 days, is not related to obesity or cardiovascular disease in Hispanic/Latino adults, perhaps because the pathways to obesity and cardiovascular disease involve protracted processes.3,4
Home food availability is consistently associated with dietary intake in youth44; but in our study, when models were adjusted for home food environment, the effect estimates did not change, suggesting that the association of parental stress and child obesity was independent of the home food environment. However, after adjusting for caregiver obesity status, the association was no longer significant, suggesting that there may be other home environment characteristics at play. Because our measure of home food environment has not been fully validated, it is also possible that measurement error obscured the role of this variable.
Whether caregiver's weight status is a confounder or a mediator remains to be elucidated. Previously, we reported in adult Hispanics/Latinos associations of chronic stress and obesity,4 which may indicate that caregiver obesity is in the pathway from caregiver stress to child obesity. Caregiver weight status is a strong predictor of childhood obesity, with environmental and genetic factors playing an important role. Thus, it may be that caregivers' stress influences their own lifestyle behaviors and obesity, and these in turn influence the characteristics of the home environment and obesity risk of their children.
Future studies with more comprehensive measures of the home environment may help elucidate the links between parental stress and child weight. In addition, prospective research will be needed to fully understand the temporal nature of these associations. The association of caregiver chronic stress and youth obesity was independent of youth lifestyle behaviors, indicating that this association could be mediated by other behavioral risk factors for childhood obesity (e.g., child sleep habits and mental health functioning), which were not included in the present study.
In addition, direct biological pathways, such as epigenetic changes, may be involved. Recent studies in adults indicate that exposure to psychosocial stress induces methylation changes, which in turn are associated with increased adiposity and chronic diseases. Epigenetic studies in youth are scarce and it is an area that needs to be further investigated.
Caution is needed when interpreting the study findings due to some limitations in the study design. First, because the ascertainment of caregiver stress preceded the assessment of childhood obesity, we cannot distinguish between incident vs. prevalent obesity. The study did not assess stress levels in the child, and we cannot determine the impact of caregiver stress on childhood stress levels. Furthermore, biological measures of stressors, such as cortisol levels, were not obtained in the caregiver or the child, which precludes us from gaining insights into the biological pathways for stress exposure. Parenting practices were not included in the study, and prior research indicates that it could influence the association of caregiver stress with childhood obesity.23,45
Another limitation of the study is the relatively small sample size, which prevented us from exploring sex differences; studies in adults have reported differences in men and women when studying the association of stress on health.46–48 Despite these limitations, the study findings have important implications. Recently, the American Academy of Pediatrics identified environmental stressors as important influences of child health and there are calls to address them in primary care.49
Although a number of studies point out the effects of socioeconomic adversity, limited attention has been paid to parent psychosocial stress as another contributor to what is referred as a toxic environment. Parental chronic stress may be a less severe risk factor than overt child stressors such as maltreatment or neglect. Nevertheless, because psychosocial stressors are more common, the effects could be more pervasive and could affect a much larger number of children.
Thus, this study contributes to the growing literature documenting the role of parental stressors on child health in a population that is underserved and experiences high levels of stressors.3 Whereas limitations in the study design and the generalizability of our study findings limit drawing causal inferences, other investigators suggest that addressing parental psychosocial stress could improve preventive or treatment programs targeting childhood obesity.17
Acknowledgments
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study was supported by grant number RC2HL101649 and SOL Youth study was supported by grant number R01HL102130 from the National Heart, Lung, and Blood Institute (NHLBI). The HCHS/SOL was supported by contracts from NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communication Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. J Am Med Assoc 2007;298:1685–1687 [DOI] [PubMed] [Google Scholar]
- 2.Richardson S, Shaffer JA, Falzon L, et al. . Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol 2012;110:1711–1716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallo LC, Roesch SC, Fortmann AL, et al. . Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Psychosom Med 2014;76:468–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Isasi CR, Parrinello CM, Jung MM, et al. . Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol 2015;25:84–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cartwright M, Wardle J, Steggles N, et al. . Stress and dietary practices in adolescents. Health Psychol 2003;22:362–369 [DOI] [PubMed] [Google Scholar]
- 6.Jenkins SK, Rew L, Sternglanz RW. Eating behaviors among school-age children associated with perceptions of stress. Issues Compr Pediatr Nurs 2005;28:175–191 [DOI] [PubMed] [Google Scholar]
- 7.Ozier AD, Kendrick OW, Leeper JD, et al. . Overweight and obesity are associated with emotion- and stress-related eating as measured by the eating and appraisal due to emotions and stress questionnaire. J Am Diet Assoc 2008;108:49–56 [DOI] [PubMed] [Google Scholar]
- 8.Vanaelst B, Michels N, Clays E, et al. . The association between childhood stress and body composition, and the role of stress-related lifestyle factors—cross-sectional findings from the baseline ChiBSD survey. Int J Behav M 2014;21:292–301 [DOI] [PubMed] [Google Scholar]
- 9.Evans GW, Kim P, Ting AH, et al. . Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol 2007;43:341–351 [DOI] [PubMed] [Google Scholar]
- 10.Luecken LJ, Rodriguez AP, Appelhans BM. Cardiovascular stress responses in young adulthood associated with family-of-origin relationship experiences. Psychosom Med 2005;67:514–521 [DOI] [PubMed] [Google Scholar]
- 11.Gunnar MR, Frenn K, Wewerka SS, Van Ryzin MJ. Moderate versus severe early life stress: Associations with stress reactivity and regulation in 10-12-year-old children. Psychoneuroendocrinology 2009;34:62–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marsman R, Nederhof E, Rosmalen JG, et al. . Family environment is associated with HPA-axis activity in adolescents. The TRAILS study. Biol Psychol 2012;89:460–466 [DOI] [PubMed] [Google Scholar]
- 13.Saxbe DE, Margolin G, Spies Shapiro LA, Baucom BR. Does dampened physiological reactivity protect youth in aggressive family environments? Child Dev 2012;83:821–830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spies LA, Margolin G, Susman EJ, Gordis EB. Adolescents' cortisol reactivity and subjective distress in response to family conflict: The moderating role of internalizing symptoms. J Adolesc Health 2011;49:386–392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ronsaville DS, Municchi G, Laney C, et al. . Maternal and environmental factors influence the hypothalamic-pituitary-adrenal axis response to corticotropin-releasing hormone infusion in offspring of mothers with or without mood disorders. Dev Psychopathol 2006;18:173–194 [DOI] [PubMed] [Google Scholar]
- 16.Luecken LJ, Lemery KS. Early caregiving and physiological stress responses. Clin Psychol Rev 2004;24:171–191 [DOI] [PubMed] [Google Scholar]
- 17.Tate EB, Wood W, Liao Y, Dunton GF. Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index. Obes Rev 2015;16:351–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gundersen C, Lohman BJ, Garasky S, et al. . Food security, maternal stressors, and overweight among low-income US children: Results from the National Health and Nutrition Examination Survey (1999–2002). Pediatrics 2008;122:e529–e540 [DOI] [PubMed] [Google Scholar]
- 19.Koch FS, Sepa A, Ludvigsson J. Psychological stress and obesity. J Pediatr 2008;153:839–844 [DOI] [PubMed] [Google Scholar]
- 20.Arredondo EM, Elder JP, Ayala GX, et al. . Is parenting style related to children's healthy eating and physical activity in Latino families? Health Educ Res 2006;21:862–871 [DOI] [PubMed] [Google Scholar]
- 21.Ayala GX, Baquero B, Arredondo EM, et al. . Association between family variables and Mexican American children's dietary behaviors. J Nutr Educ Behav 2007;39:62–69 [DOI] [PubMed] [Google Scholar]
- 22.Conlon BA, McGinn AP, Lounsbury DW, et al. . The role of parenting practices in the home environment among underserved youth. Child Obes 2015;11:394–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lytle LA, Hearst MO, Fulkerson J, et al. . Examining the relationships between family meal practices, family stressors, and the weight of youth in the family. Ann Behav Med 2011;41:353–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallo LC, Penedo FJ, Carnethon M, et al. . The Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study: Sample, design, and procedures. Ethn Dis 2014;24:77–83 [PMC free article] [PubMed] [Google Scholar]
- 25.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. . Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010;20:629–641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lavange LM, Kalsbeek WD, Sorlie PD, et al. . Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010;20:642–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Isasi CR, Carnethon MR, Ayala GX, et al. . The Hispanic Community Children's Health Study/Study of Latino Youth (SOL Youth): Design, objectives, and procedures. Ethn Dis 2014;24:29–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ayala GX, Carnethon M, Arredondo E, et al. . Theoretical foundations of the Study of Latino (SOL) Youth: Implications for obesity and cardiometabolic risk. Ethn Dis 2014;24:36–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NHCS. 2000 CDC Growth Charts: United States. 2000. Available at www.cdc.gov/growthcharts Last accessed December15, 2015
- 30.Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging 1996;11:207–213 [DOI] [PubMed] [Google Scholar]
- 31.Shivpuri S, Gallo LC, Crouse JR, Allison MA. The association between chronic stress type and C-reactive protein in the multi-ethnic study of atherosclerosis: Does gender make a difference? J Behav Med 2012;35:74–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396 [PubMed] [Google Scholar]
- 33.Nepper MJ, Ludeman M, Chai W. Validation of instruments to assess home food environment of pre-adolescents: A pilot study. J Nutr Health Food Sci 2014;2:1–9 [Google Scholar]
- 34.Ding D, Sallis JF, Norman GJ, et al. . Community food environment, home food environment, and fruit and vegetable intake of children and adolescents. J Nutr Educ Behav 2012;44:634–638 [DOI] [PubMed] [Google Scholar]
- 35.Couch SC, Glanz K, Zhou C, et al. . Home food environment in relation to children's diet quality and weight status. J Acad Nutr Diet 2014;114:1569.e1–1579.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guenther PM, Casavale KO, Reedy J, et al. . Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113:569–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gallo LC, Roesch SP, McCurley JL, et al. . Youth and caregiver physical activity and sedentary time: HCHS/SOL Youth. Am J Health Behav 2017;41:67–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 2005;37:S531–S543 [DOI] [PubMed] [Google Scholar]
- 39.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc 2011;43:357–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romanzini M, Petroski EL, Ohara D, et al. . Calibration of ActiGraph GT3X, Actical and RT3 accelerometers in adolescents. Eur J Sport Sci 2014;14:91–99 [DOI] [PubMed] [Google Scholar]
- 41.Wilson SM, Sato AF. Stress and paediatric obesity: What we know and where to go. Stress Health 2014;30:91–102 [DOI] [PubMed] [Google Scholar]
- 42.Bauer KW, Hearst MO, Escoto K, et al. . Parental employment and work-family stress: Associations with family food environments. Soc Sci Med 2012;75:496–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parks EP, Kumanyika S, Moore RH, et al. . Influence of stress in parents on child obesity and related behaviors. Pediatrics 2012;130:e1096–e1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loth KA, MacLehose RF, Larson N, et al. . Food availability, modeling and restriction: How are these different aspects of the family eating environment related to adolescent dietary intake? Appetite 2016;96:80–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lohman BJ, Stewart S, Gundersen C, et al. . Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. J Adolesc Health 2009;45:230–237 [DOI] [PubMed] [Google Scholar]
- 46.Wardle J, Chida Y, Gibson EL, et al. . Stress and adiposity: A meta-analysis of longitudinal studies. Obesity (Silver Spring) 2011;19:771–778 [DOI] [PubMed] [Google Scholar]
- 47.Iversen LB, Strandberg-Larsen K, Prescott E, et al. . Psychosocial risk factors, weight changes and risk of obesity: The Copenhagen City Heart Study. Eur J Epidemiol 2012;27:119–130 [DOI] [PubMed] [Google Scholar]
- 48.Fowler-Brown AG, Bennett GG, Goodman MS, et al. . Psychosocial stress and 13-year BMI change among blacks: The Pitt County Study. Obesity (Silver Spring) 2009;17:2106–2109 [DOI] [PubMed] [Google Scholar]
- 49.Garner AS, Shonkoff JP, Siegel BS, et al. . Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics 2012;129:e224–e231 [DOI] [PubMed] [Google Scholar]


