Abstract
Toxoplasma gondii is a widespread parasitic pathogen that infects over a third of the world’s population. Following an acute infection, the parasite can persist within its mammalian host as intraneuronal or intramuscular cysts. Cysts will occasionally reactivate, and depending on the host’s immune status and site of reactivation, encephalitis or myositis can develop. Because these diseases have high levels of morbidity and can be lethal, it is important to understand how Toxoplasma traffics to these tissues, how the immune response controls parasite burden and contributes to tissue damage, and what mechanisms underlie neurological and muscular pathologies that toxoplasmosis patients present with. This review aims to summarize recent important developments addressing these critical topics.
Keywords: Chronic Infections, Parasite, Plasmodium, Seizures, Myositis, Blood Brain Barrier
TOXOPLASMA GROWTH AND DEVELOPMENT WITHIN TISSUES
Toxoplasma gondii infects approximately a third of the world’s population making it one of the most prominent foodborne pathogens [1]. In humans and other intermediate hosts, the parasite exists as two distinct forms – tachyzoites and bradyzoites. Tachyzoites are the rapidly replicating and disease causing form. While drugs and immune responses can control tachyzoite growth, some tachyzoites escape destruction and develop into bradyzoites, which progress encased into cysts in a variety of tissues including the brain and skeletal muscle (SM). Because cysts are impervious to drugs and host immune responses and do not cause overt disease, they can remain undetected as a relatively benign chronic infection. Recent work has, however, revealed increasingly strong correlations between chronic Toxoplasma infections and the onset of behavioral changes and neuropsychiatric disorders such as schizophrenia. While an important subject, this topic is beyond the scope of this review and instead we refer readers to several recent review articles [2, 3].
Uncontrolled tachyzoite replication causes severe and potentially life-threatening disease to: i) fetuses whose mothers were infected for the first time during pregnancy, ii) immune-compromised individuals after a tissue cyst reactivates, and iii) otherwise healthy individuals who are susceptible to developing severe disease and particularly, ocular toxoplasmosis, when infected by specific Toxoplasma strains that are endemic to South America [4–7]. In each case, clinical severity is due to a combination of parasite growth, tissue damage, and inflammatory responses. In addition, the host and parasite genotypes are also important contributors to disease severity. A significant amount of work has focused on how Toxoplasma replicates and how immune responses control the infection. Less work, however, has addressed how the tissue damage caused by the parasite and resulting immune response leads to clinical disease. These studies are of particular importance in the nervous system for two reasons. First, the central nervous system (CNS), which includes the brain and retina, is the most common site for toxoplasmosis disease to develop and these patients will present with a combination of vision loss, seizures, and other neurological symptoms [8]. Second, Toxoplasma forms tissue cysts in SM and this represents an important step in the parasite’s life cycle since tissue cyst ingestion from undercooked meat is the primary route of transmission [9]. In this review, we will highlight recent work and discoveries on how Toxoplasma enters, persists, and causes disease in SM and the brain of an infected host (Figure 1).
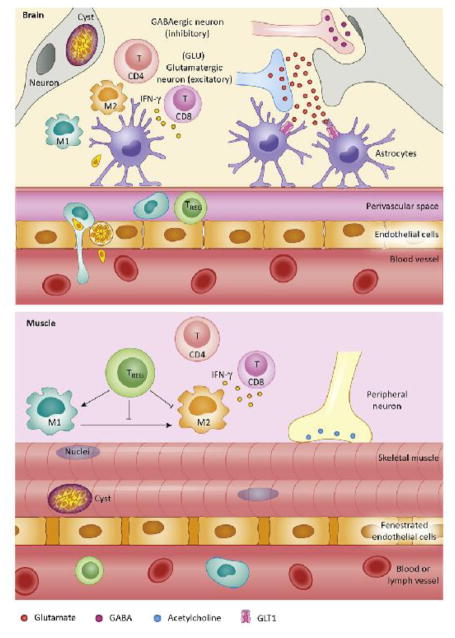
Figure 1. Toxoplasma Interactions in the Brain and Skeletal Muscle.
In the brain, Toxoplasma gains entry by traversing across endothelial cells. Once inside the brain, the parasite forms tissue cysts within neurons. Immune pressure from a variety of central nervous system resident and peripheral cells prevents cyst reactivation and infection of non-neuronal cells. The presence of Toxoplasma and infection-induced inflammation can lead to a combination of increased excitatory and decreased inhibitory neurotransmission causing increased susceptibility to seizures. In skeletal muscle, Toxoplasma forms tissue cysts and can induce tissue damage due to the development of pathogenic regulatory T cells (Treg). T cell production of interferon-gamma (IFN-γ) remains important, however, in contrast to the brain little is known about Toxoplasma-induced changes to the peripheral nervous system. M1, pro-inflammatory macrophages; M2, pro-regenerative macrophages.
TRANSIT TO AND ENTRY INTO THE NERVOUS SYSTEM
Following digestion of tissue cysts in undercooked meat or oocysts from felid fecal matter, the acid hydrolases of the stomach rupture the cysts and the released parasites go on to infect intestinal epithelial cells. This triggers the recruitment and activation of innate immune cells including dendritic cells and inflammatory monocytes [10]. These in turn are infected by Toxoplasma and become hypermigratory, a process that increases their emigration from the intestine to peripheral tissues [11]. Parasite induction of hypermigratory dendritic cells and inflammatory monocytes is a multi-step process that includes alterations of the host cells’ actin cytoskeleton, upregulation of the CCR7 chemokine receptor, and activation of gamma-aminobutyric acid (GABA) receptor signaling [12, 13].
Unlike most tissues, entry of cells, pathogens, and proteins from the blood into the brain is a challenge due to the presence of the highly impermeable blood-brain barrier (BBB) [14]. The BBB is composed of endothelial cells with high numbers of tight junctions that are supported by a rich basement membrane network. In addition, pericytes and astrocytic endfeet surround the endothelial cells providing structural and biochemical support as well as preventing substances from traversing the endothelium and entering the brain parenchyma. How then does Toxoplasma get through this barrier to enter the brain?
A number of distinct mechanisms have been explored. The first was a Trojan Horse-like mechanism in which Toxoplasma-infected monocytes and other myeloid-derived cells could extravasate from capillaries into the brain [15]. Support for this model initially came from experiments in which parasites accumulated more rapidly in brains of mice intravenously infected with Toxoplasma-infected monocytes than if they were infected with extracellular tachyzoites [15]. Additional experiments showed that Toxoplasma preferentially infects cells expressing the integrins CD11b+/CD11c+ and that parasite-infected CD11b+/CD11c+ cells could attach to and then migrate across murine brain derived endothelium in vitro based assay. Transendothelial migration across human endothelial cells is CD11b/ICAM1 dependent and occurs more frequently under fluidic shear stress conditions [15, 16]. These data suggest that CD11b+/CD11c+ cells are primary host cells mediating parasite dissemination although more recent work indicated that parasites accumulated in murine brains via CD11b+ cells that were either CD11c+ or CD11c− [17].
It is also possible that individual Toxoplasma tachyzoites enter the CNS on their own by either transcytosis or paracytosis. Early support for this model came from transwell tissue culture systems in which tachyzoites were able to cross retinal endothelial cell layers [18]. More recently, two-photon in vivo imaging studies demonstrated that extracellular tachyzoites are capable of crossing the BBB [19]. Moreover, these extracellular tachyzoites, and not those egressing from Toxoplasma-infected cells that were attached to the endothelium, are the majority of those parasites crossing the BBB. This study also demonstrated that prior to egress into the brain parenchyma, that tachyzoites must replicate within endothelial cells. This ‘naked’ extracellular tachyzoite transmigration is extremely efficient and therefore may represent the primary mechanism (as opposed to a Trojan Horse mechansism using infected monocytes) for parasite extravasation into the CNS [19].
TISSUE CYSTS AND CHRONIC INFECTIONS
After tachyzoites enter the brain and other tissues they are engaged by an immune response that will be described below. Although this immune response is highly efficient at killing tachyzoites, some escape destruction and transform into cyst-forming bradyzoites. Tissue cysts are responsible for transmission to new intermediate or definitive hosts [20] and are also important because they are impervious to drugs and can avoid immune-mediated destruction. While drugs likely cannot gain access to the interior of the tissue cyst due to the highly glycosylated cyst wall encapsulating the bradyzoites and because they are intracellular [21], tissue cysts avoid immune responses through mechanisms that are not fully understood.
A key difference between tachyzoites and bradyzoites are the distinct repertoire of immunogenic proteins expressed by the two [20] such that T-cells are significantly more likely to engage and attack a tachyzoite-infected host cell [22, 23]. But why are bradyzoite antigens less likely to trigger protective immune responses? An answer to this came from studies in which tachyzoites were engineered to constitutively express the dominant bradyzoite surface antigen, SRS9 [24]. These parasites induced a strong anti-SRS9 response that resulted in reduced cyst burdens in brains of parasite-infected mice. This suggests that it is not the bradyzoite or cyst itself that is poorly immunogenic but the location and timing of the immune response that is able to see it. This is further supported by recent work manipulating ApiAP2 transcription factors, which are a novel family of transcriptional regulators (67 ApiAP2 genes are present in the Toxoplasma genome) that regulate stage specific gene expression [25]. For example, Api2IV-4 normally expressed by tachyzoites, inhibits bradyzoite gene expression. Parasites in which Api2IV-4 is deleted increase their expression of bradyzoite antigens, leading to enhanced immune responses and a complete absence of cysts in the brain [26]. This suggests that turning off bradyzoite antigen expression is as important to chronic infection as turning it on.
Bradyzoites spontaneously form cysts within neurons in vitro [27] and a small sample of human autopsy specimens supports tropism for the brain [28], the basis of which is still to be understood. In addition, in vivo experiments using Cre recombinase-expressing parasites supports the concept that the neuron is not only the primary host cell for cysts but is the only cell that is productively infected within the brain [29]. This is despite multiple types of CNS resident cells being capable of supporting tachyzoite growth in tissue culture [30]. This tropism for neurons is astounding as the tachyzoite has to migrate across and not invade the multiple non-neuronal cells of the BBB and the parenchyma. Thus, neurons provide an, as yet, unknown niche conducive for bradyzoite development, which could be a unique metabolic or immunological feature. For example, earlier studies by Schluter and colleagues showed that unlike most other cell types, neurons did not respond in any quantitative way to stimulation with interferon-gamma (IFN-γ) or tumor necrosis factor α (TNFα) and therefore may simply be the only cells, in the brain, that are unable to mount an appropriate anti-parasitic response [31]. Alternatively, GABA has been reported to be utilized as a metabolite in Toxoplasma and therefore it is possible that it is scavenged by Toxoplasma and used as a carbon source [32]. Further studies are required to understand this neuronal niche and the effects such a niche may have on the health of the host.
Whether there is tropism for certain parts of the brain has been revisited several times [33–35]. Most, if not all, studies identified cysts in cortical regions. On the other hand, some but not all reports have found cysts in subcortical regions, such as the amygdala, which has provided an explanation for changes in behavior associated with Toxoplasma infections [36, 37]. However, this distribution and cyst burden is variable within a host, between species and dependent upon parasite strain [38]. Perhaps the previously discussed new finding that extracellular parasites cross the BBB [19] provides an explanation for this heterogeneity as the site of infection of the brain and cyst location within the brain are more likely due to blood vessel location and site of extravasation.
IMMUNE RESPONSES IN THE BRAIN
Toxoplasmic encephalitis (TE) occurs following unchecked reactivation of cysts, neuronal cell death, and inflammation. The critical requirement for an immune response to establish a chronic infection and to prevent reactivation of Toxoplasma has been known since the identification of Toxoplasma as an opportunistic pathogen in AIDS and transplant patients [8]. This was experimentally demonstrated in mice by Sher and colleagues using depletion studies solidifying the absolute requirement for CD8+ and CD4+ T cells during chronic infection to prevent fatal encephalitis [39].
The type of immune response required to prevent reactivation in the brain is currently understood to be the same as required to control acute infections -namely a dominant type 1 immune response characterized by IFN-γ production to activate cells enabling local effector responses. Furthermore, treatment of TE is associated with the restoration of the IFN-γ response [40]. As with acute infections and most other type I responses, production of IFN-γ and other pro-inflammatory cytokines must be regulated by anti-inflammatory cytokines including IL-10 and IL-27, without which continued recruitment of highly activated immune cells into the brain leads to encephalitis independent of parasite burden [41–44]. The role of regulatory T cells has still to be fully assessed, however a recent study suggests that Tregs inhabit a restricted niche in the meninges and perivascular space where they interact with CD11c expressing antigen-presenting cells [45]. Understanding the function and specificity of these interactions will be of future interest.
The brain is enclosed within the rigid casing of the skull making the immune cell recruitment and swelling normally associated with immune responses a potentially fatal outcome. There is normally low expression of antigen presenting molecules and the BBB limits immune cells and antibody infiltration. The prevalence of Toxoplasma and the requirement for ongoing immunity to this parasite in the brain suggests a highly controlled immune response that is robust enough to contain the parasite yet limited to prevent clinical symptoms. The dynamics of this response are only beginning to be unraveled. Our knowledge of the kinetics and type of inflammation in the brain is limited to murine models with the exception of histological descriptions of infection and inflammation in autopsy samples [28, 46]. During infection, however, the BBB becomes compromised [47, 48] and large numbers of macrophages, dendritic cells, and T cells are found in the murine brain. Whether changes in BBB permeability or instead an upregulation of factors that promote immune cell extravasation (e.g. adhesion molecules) is the primary route for immune cell extravasation during infection needs to be determined. Histological examination and in vivo imaging demonstrates considerable accumulation of cells in perivascular spaces and meningeal areas [22, 23, 49, 50] with additional routes through the fenestrated endothelium of the choroid plexus in the ventricles likely [51, 52]. Considerable tissue remodeling takes place early during infection with second harmonic imaging revealing a network of fibers in inflamed areas of the brain (and not present in naïve brains) [22] particularly at layers I and II of the frontal cortex. Lymphocytes can be observed crawling on these fibers but it is not yet clear whether these structures facilitate cell migration or are generated as a result of protease activity during cell infiltration [53].
IFN-γ controls parasite replication by several means including stimulating degradation of the parasitophorous vacuole, increasing the expression of MHC genes and antigen presentation, and upregulation of other anti-parasitic factors such as nitric oxide synthetase and indoleamine dioxygease [54–60]. In the brain, microglia as well as infiltrating CD4 and CD8 T cells are the primary sources of IFN-γ [39, 41, 61]. IFN-γ signals through STAT1 and deleting this transcription factor specifically in astrocytes leads to cyst formation in STAT1−/− astrocytes (as opposed to no cysts in astrocytes of WT mice) and mice succumb to infection [62]. This points to brain resident astrocytes as being critical effector cells in limiting Toxoplasma in the brain. Astrocytic endfeet are a key component of the BBB and likely sense any systemic concentrations of IFN-γ. Thus, it is unclear whether changes in cyst burden and location in the absence of astrocytic STAT1 is due to an inability to respond to local or systemic IFN-γ. Regardless, these data demonstrate that astrocytic IFN-γ signaling is required for resistance and also suggest that cyst formation in neurons in WT mice is because astrocytes can resist infection rather than parasites having a specific tropism for neurons.
In infected brains, astrocytes express CCL21 and CXCL10 (and other chemokines) that recruit T-cells into the parenchyma [63] and directs their migration within the brain [49]. Live multi-photon imaging visualized a number of different T cell behaviors in the brain including division, random search strategies and sustained interactions with CNS resident and peripheral antigen presenting cells [22, 49, 50, 56]. Flow cytometry and histological studies further show that in an infected brain CD4+ and CD8+ T cells can express markers of tissue residency [64], exhaustion (e.g. PD-1) [22, 65–67] or are PD-1 negative and secrete IFN-γ. The coexistence of seemingly opposite types of T-cells in the infected brain may be explained by the finding that T-cells directed against the dominant parasite antigen, GRA6, led to the development of T-cells that did not enter a contraction phase but rather exhibited effector and memory phenotypes. Importantly, these T-cells are highly responsive to antigen enabling them to rapidly respond following cyst reactivation [68].
Brain cyst burdens are also controlled by CD8+ T cell-derived perforin and chitinase synthesized by macrophages or microglia [69–71]. The use of perforin to kill infected cells depends on the recognition of cognate antigen by activated NK or CD8+ T cells. It remains to be determined whether perforin-secreting cells recognize peptides presented by cyst-containing neurons or by tachyzoite-infected cells before they undergo differentiation. While ROP7 and GRA6 are sources for CD8 T-cell responses [72–74], it is still possible that cyst-derived antigens are presented during chronic infection. Indeed, there is evidence that a switch in T cell specificity occurs as the infection progresses to a chronic stage [72]. While cysts were thought to evade surrounding inflammatory cells, live imaging shows both a complete avoidance of cysts [23] and a keen interest with seemingly long term attachments made between cysts and immune cells [22]. This may be explained by heterogeneity in the cysts and/or T-cells. For example, recent data indicates that within a cyst parasite replication continues, albeit slower than in tachyzoites, [35, 38]. Thus, cysts are far more dynamic than realized and further studies are required to fully understand the development of cysts and the specific immune response elicited by them.
NEUROLOGICAL COMPLICATIONS DURING TOXOPLASMIC ENCEPHALITIS
Tissue cyst reactivation in a host whose immune response cannot properly control growth of the emerging parasites leads to toxoplasmosis. Clinically, toxoplasmosis presents as a broad spectrum of disorders but the most common is TE whose neurological symptoms include dizziness, headaches, and seizures. But how Toxoplasma induces the brain to develop these symptoms has been an underexplored area. Mice infected with the type II ME49 strain develop spontaneous seizures [75, 76]. Seizures form due to unbalanced levels of excitatory and inhibitory neurotransmission causing excessive electrical activity.
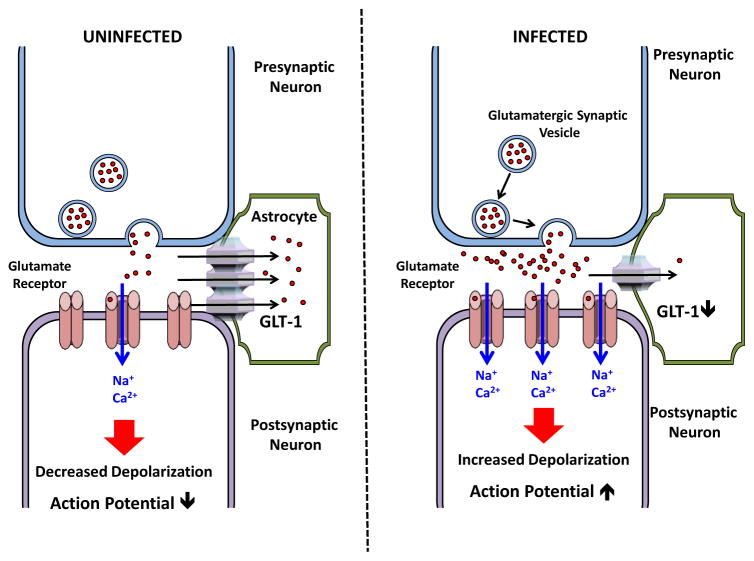
In the brain, glutamate is the major excitatory neurotransmitter and decreases in its clearance from synapses leads to increased levels of neurotransmission and neuronal damage due to glutamate excitotoxicity [77]. The glutamate transporter, GLT-1, is expressed on the surface of astrocytes and is the primary transporter in clearing extracellular glutamate from synaptic termini [78]. In Toxoplasma-infected brains, GLT-1 is significantly down regulated leading to increased extracellular glutamate levels (Figure 2). Neurons in infected brains have morphological changes consistent with excitotoxicity and functional electroencephalogram point to a loss of neuronal circuitry and seizures [76]. Importantly, treatment with ceftriaxone, a β-lactam known to increase GLT-1 expression [79], lowered extracellular glutamate concentrations and restored neuronal health without any apparent anti-parasitic activity [76].
Figure 2. Toxoplasma Down Regulates GLT-1 to Increase Excitatory Glutamatergic Synaptic Transmission.
GLT-1 is an astrocytic glutamate transporter that removes extracellular glutamate from the synaptic cleft (left panel). Upon Toxoplasma infection, GLT-1 expression is downregulated leading to increased levels of extracellular glutamate and excitatory glutamatergic signaling and neuronal damage (right panel).
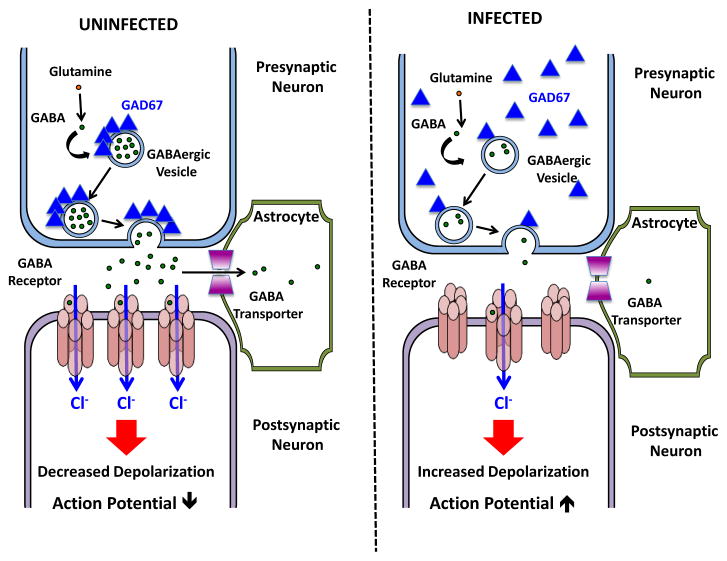
As discussed above, balanced excitatory and inhibitory neurotransmission maintains normal synaptic activity. GABA is the primary inhibitory neurotransmitter in the brain and is synthesized primarily by glutamate decarboxylase 67 (GAD67) [80]. In Toxoplasma-infected brains, GAD67 localization changes from being clustered on synaptic vesicles to being more diffuse throughout the neuron [75] (Figure 3). Changes in GAD67 localization are thought to lower its ability to synthesize GABA and thus reduce GABAergic signaling [81]. Indeed, Toxoplasma-infected mice develop longer and more severe seizures when treated with GABA receptor antagonists [75]. Thus, seizures develop in TE mice due to changes in both excitatory and inhibitory neurotransmission.
Figure 3. Toxoplasma Alters GAD67 Localization to Decrease Inhibitory GABAergic Synaptic Transmission.
GAD67 is clustered in presynaptic termini on the surface synaptic vesicles, which facilitates efficient GABA synthesis and packaging within the vesicles (left panel). Toxoplasma infection leads to a loss of clustering and subsequent decrease in GABAergic synaptic activity (right panel). This decrease in activity will increase the probability that an action potential will be triggered in the postsynaptic neuron.
How does Toxoplasma alter GLT-1 and GAD67? It is unlikely that cysts in the relatively few infected neurons [82] are directly involved because these two proteins are affected throughout the brain regardless of proximity to cysts or reactivation sites [75, 76]. Toxoplasma can modulate larger numbers of host neurons independently of invasion by injection of effector molecules into host cells [83]. However, it is unclear whether these effectors remain active long enough to contribute to neuropathologies that take several weeks to develop. Intracerebral inflammation can also contribute to the onset of seizures [84]. Given the significant number of activated microglia and astrocytes in Toxoplasma-infected brains [85], parasite-induced inflammation could contribute to seizures in infected mice. Overexpression of several cytokines that are upregulated by infection (e.g. IL-1β) can trigger or enhance seizures [84]. Inflammation can also compromise BBB integrity, which triggers a number of profound changes in the CNS [84]. First, BBB breakdown will alter intracerebral potassium homeostasis leading to membrane depolarization and increased synaptic firing. In addition, potassium can cause tissue damage by activating the inflammasome. Breakdown of the BBB will also allow antibodies, complement, and other immunomodulatory factors to gain access to the brain. Autoantibodies against excitatory and inhibitory synaptic proteins have been associated with the onset of epilepsy and other neurological disorders. Even though infection leads to increases in glutamate receptor subunit autoantibodies, it remains to be tested whether these and other autoantibodies could trigger seizures during TE [86].
The primary functions for microglia are constant monitoring of the parenchyma and surveying synaptic activity [87]. When a microglia encounters a dysfunctional synapse, it eliminates the synapse by phagocytosis via microglial expression of the C3 complement receptor engaging C1q on the surface of complement-tagged neurons [88]. Although this process was originally identified to play a key role in synapse elimination during development [89], it has more recently been linked to various pathological events in mature animals [90–93].
Systemic inflammation (such as low dose intraperitoneal lipopolysaccharide injections) leads to synaptic loss that requires microglia. Here, microglia enshroud a synapse and then physically displaces it from the neuronal soma [94]. Synaptic displacement differs from synaptic elimination in several ways. First, displacement specifically impacts inhibitory synapses while elimination primarily targets excitatory synapses. Second, displacement is thought to have a neuroprotective role whereas elimination is associated with neuropathological conditions. Finally, elimination is dependent on C1q-mediated phagocytosis whereas displacement is not. Given that Toxoplasma appears to impact GABAergic (i.e. inhibitory) synaptic composition, elimination is likely to not be relevant in parasite-induced changes to GABAergic synapses. However, as a loss of dendritic spines is observed in cortical regions [76] microglia may additionally be playing a role in eliminating glutamatergic synapses.
TOXOPLASMA IN SKELETAL MUSCLE
Although there is a clear need to understand Toxoplasma-induced changes in the brain an overlooked area of pathology and a prime route of transmission is the SM. Both acute infections and reactivated infections in AIDS patients can cause myositis [6, 95–97]. Despite its clinical significance and importance in Toxoplasma’s life cycle, Toxoplasma-SM interactions are not well studied. Given the similarities between the brain and SM (both tissues have high numbers of post-mitotic cells and neuronal synapses) and differences (the brain is immune-privileged and SM is not), a comparison between the two may highlight important differences with regard to how inflammation and infections proceed in these two distinct tissues.
The brain and SM are the two primary tissues where tissue cysts develop. Because of the predominance of post-mitotic cells (neurons and myocytes) in both tissues - it has been hypothesized that the post-mitotic nature of these cells is conducive for bradyzoite development. Indeed, in vitro work showed that bradyzoite formation is more efficient in differentiated muscle cells [98, 99], which is consistent with earlier studies that demonstrated that deletion of CDA1, a protein that controls host cell proliferation, leads to increases in bradyzoite development [100]. However, other immunological or metabolic traits of post-mitotic cells may also contribute to cyst development.
Immune responses to Toxoplasma in the brain and SM were originally believed to be quite similar and typified by an influx of monocytes, macrophages, as well as CD4+, CD8+, and regulatory T-cells [101]. Indeed, IFN-γ is also critical for controlling Toxoplasma in SM and appears to function by activating IFN-γ stimulated GTPases and nitric oxide [102]. Unstimulated mature myocytes, however, express low levels of MHC Class I and II and high levels of inhibitory co-receptors e.g. PD-L1 and HLA-G [103, 104]. In response to infections and other pathological insults, muscle cells respond to pro-inflammatory cytokines by upregulating MHC molecules and pro-inflammatory cytokines. But what cells in the muscle detect the parasite remains unknown.
As discussed above, continuous immune surveillance is required to prevent a reactivated infection from developing into toxoplasmosis and this is also true in SM and other tissues. However, these immune responses must be tightly regulated to prevent immune-mediated tissue damage and regulatory T-cells (Tregs) have been proposed to limit immunopathology during the acute phase of the infection. But what role Tregs play during chronic infections has been largely unexplored and remains unresolved [43, 105–107]. To address this, we explored the basis for the development of myositis in C57Bl/6 mice chronically infected with Toxoplasma [101]. Surprisingly, when Tregs are depleted from chronically infected mice, SM damage is significantly reduced suggesting that Tregs actively promote infection-induced muscle damage and/or impair SM regeneration [101].
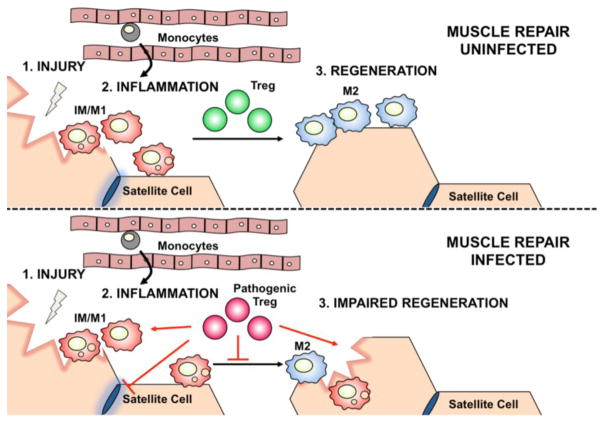
How do Tregs promote SM damage in Toxoplasma-infected mice? Damage to SM triggers a reparative program that ensures the efficacious activation and differentiation of stem cells (satellite cells) to intermediary myoblasts and terminally differentiated, functional myotubes. SM repair begins with an inflammatory phase mediated by inflammatory monocyte/pro-inflammatory macrophages (IM/M1), which is followed by a shift in macrophage polarization to a pro-regenerative (M2) phenotype. Tregs are important for proper execution of each step and an inability to limit number of IM/M1 cells or a block in M1–M2 conversion leads to SM damage [108] (Figure 4). Phenotyping macrophages from infected and uninfected SM revealed an accumulation of IM/M1 macrophages and Treg depletion lead to an increase in numbers of M2 cells in the parasite infected samples [101]. However, it remains to be determined whether increased IM/M1 macrophages and/or decreased M2 cells is/are the mechanism(s) by which SM damage develops in parasite-infected mice. Pathogenic Tregs may also limit the ability for IM/M1 cells to remove SM debris from a damage nerve fiber or for M2 cells to promote regeneration [101]. It also remains to be determined whether Tregs have a similar pathogenic role in the brain and other tissues of chronically infected mice. A second question that remains to be investigated is whether loss of muscle control is entirely due to SM damage or if Toxoplasma impacts neurotransmission in SM as it does in brain.
Figure 4. Toxoplasma Induces Pathogenic Tregs That Hinder Skeletal Muscle Regeneration.
Regeneration of skeletal muscle from injury is a stepwise process that requires monocytes and pro-inflammatory macrophages (IM/M1) for the clearance of damaged myofibers and a transition in situ to pro-regenerative macrophages (M2) and activation of satellite cells for the regeneration of myofibers. Suppressive regulatory T cells (Tregs) are required for the IM/M1 to M2 transition (top panel). Toxoplasma infection in skeletal muscle significantly alters the function of Tregs such that they acquire pathogenic action and promote IM/M1 accumulation and persistence, which results in an impaired skeletal muscle repair response (bottom panel).
CONCLUDING REMARKS
In this review, we highlighted recent advances regarding how Toxoplasma traffics to the brain and SM and causes overt pathology as well as highlighted several questions that we believe are important for the field to address. Although we have covered a wide range of topics we believe that these should not be seen in isolation but rather are highly interrelated. How are the immune responses to Toxoplasma in the brain and SM similar and also what makes them unique. This could help us understand locally driven and tissue specific immunity as well as tissue specific parasite-induced pathology. In addition, as our understanding of changes in neurotransmitters in the brain improves can we see similar alterations in the peripheral nervous system. This could apply not only to SM but the critical network of neurons at the site of infection in the gut and mucosal tissues. Further questions include, does Toxoplasma need to replicate within an endothelial cell for it to alter its gene expression and allow it to become competent for growth in the brain or other tissues? Or, are pathogenic Tregs present in other tissues, such as the brain, and do they contribute to the changes in neuronal chemistry that are involved in the onset of seizures? And, how do the discovery of pathogenic Tregs impact the development of T-cell-based vaccines as well as new therapies aimed at disarming the as yet unknown parasite factors that trigger seizures and myositis. Finally, recent work has reported strong correlations between Toxoplasma infections and onset of neuropsychological disorders but it is unclear whether these are related to changes in GLT-1 and GAD67 expression and localization as well as neuronal inflammation.
TRENDS BOX.
Toxoplasma gondii establishes a chronic infection state in the brain and skeletal muscle of its mammalian host.
Toxoplasma crosses the blood-brain barrier as either extracellular tachyzoites that infect and replicate with brain endothelial cells or within an infected monocyte.
There is limited understanding of how Toxoplasma infections of the brain and skeletal muscle and the resulting inflammation impacts the tissues’ function.
Recent studies have revealed that Toxoplasma alters both excitatory and inhibitory neurotransmission in the central nervous system and that these changes lead to unbalanced synaptic activity and seizures.
Regulatory T-cells have a pathogenic role in Toxoplasma infected skeletal muscle.
OUTSTANDING QUESTIONS.
Why must a parasite replicate in an endothelial cell before entering the brain parenchyma?
What parasite and host factors promote changes in brain chemistry including GLT-1 down regulation and GAD67 mislocalization?
Following resolution of an acute infection in the brain, how are excitatory and inhibitory synapses reset? Do Toxoplasma-induced changes in neuronal circuitry contribute to an onset of psychological disorders associated with infection?
Do Tregs have a pathogenic function in other Toxoplasma-infected tissues?
Does Toxoplasma impact other proteins or biochemical processes in the brain or skeletal muscle?
Acknowledgments
We appreciate the many thoughtful discussions we have had with members of our laboratories. We also apologize to the many investigators whose contributions we were unable to discuss and/or cite owing to space limitations. Work in the Wohlfert laboratory is supported by funds from the State University of New York, work in the Blader laboratory is partially supported by NIH grants AI124677 and AI069986, and work in the Wilson laboratory by NIH grant NS072298.
GLOSSARY
- Astrocytes
brain resident glial cells
- Blood brain barrier
A specialized cellular structure lining the vasculature of the brain separating it from circulating factors and one of the reasons that the brain is described as immune privlidged.
- Dendritic cells
myeloid derived cells particularly adept at presenting antigen to T cells.
- Encephalitis
inflammation of the brain parenchyma
- Gamma-aminobuteryic acid (GABA)
an inhibitory neurotransmitter produced by GABAergic neurons
- GLT-1
Glutamate transporter -1 (EAAT2) expressed on astrocytes is responsible for uptake of the excitatory neurotransmitter glutamate
- Interferon-gamma (IFN-γ)
a cytokine produced primarily by T cells and required for activating anti-parasitic effector mechanisms
- Myositis
chronic inflammation of the muscle
- Paracytosis
Crossing of endothelial barrier through intracellular juctions.
- Post-mitotic Cells
Cells that have exited the cell cycle and are non-dividing.
- Second harmonic imaging
When excited with two-photon laser light certain tissue structures emit light at half the wavelength and twice the frequency of excitation. These structures are non-centrosymmetric, with collagen and myosin being the most well characterized.
- Transcytosis
Transfer of an extracellular macromolecule from one side of a cell to the other via pinocytic-derived membrane bound vesicle.
- Transendothelial migration
the trafficking of cells across an endothelial barrier
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Scallan E, et al. Foodborne illness acquired in the United States--major pathogens. Emerg Infect Dis. 2011;17(1):7–15. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elsheikha HM, et al. The known and missing links between Toxoplasma gondii and schizophrenia. Metab Brain Dis. 2016;31(4):749–59. doi: 10.1007/s11011-016-9822-1. [DOI] [PubMed] [Google Scholar]
- 3.Torrey EF, et al. Toxoplasma gondii and other risk factors for schizophrenia: an update. Schizophr Bull. 2012;38(3):642–7. doi: 10.1093/schbul/sbs043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arantes TE, et al. Ocular Involvement Following Postnatally Acquired Toxoplasma gondii Infection in Southern Brazil: A 28-Year Experience. Am J Ophthalmol. 2015;159(6):1002–1012. e2. doi: 10.1016/j.ajo.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Pereira-Chioccola VL, et al. Toxoplasma gondii infection and cerebral toxoplasmosis in HIV-infected patients. Future Microbiol. 2009;4(10):1363–79. doi: 10.2217/fmb.09.89. [DOI] [PubMed] [Google Scholar]
- 6.Plonquet A, et al. Toxoplasmic myositis as a presenting manifestation of idiopathic CD4 lymphocytopenia. Muscle Nerve. 2003;27(6):761–5. doi: 10.1002/mus.10376. [DOI] [PubMed] [Google Scholar]
- 7.Singh S. Congenital toxoplasmosis: Clinical features, outcomes, treatment, and prevention. Trop Parasitol. 2016;6(2):113–122. doi: 10.4103/2229-5070.190813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luft BJ, Remington JS. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15(2):211–22. doi: 10.1093/clinids/15.2.211. [DOI] [PubMed] [Google Scholar]
- 9.Su C, et al. Recent expansion of Toxoplasma through enhanced oral transmission. Science. 2003;299(5605):414–6. doi: 10.1126/science.1078035. [DOI] [PubMed] [Google Scholar]
- 10.Cohen SB, Denkers EY. The gut mucosal immune response to Toxoplasma gondii. Parasite Immunol. 2015;37(3):108–17. doi: 10.1111/pim.12164. [DOI] [PubMed] [Google Scholar]
- 11.Lambert H, et al. Induction of dendritic cell migration upon Toxoplasma gondii infection potentiates parasite dissemination. Cell Microbiol. 2006;8(10):1611–23. doi: 10.1111/j.1462-5822.2006.00735.x. [DOI] [PubMed] [Google Scholar]
- 12.Fuks JM, et al. GABAergic signaling is linked to a hypermigratory phenotype in dendritic cells infected by Toxoplasma gondii. PLoS Pathog. 2012;8(12):e1003051. doi: 10.1371/journal.ppat.1003051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weidner JM, et al. Rapid cytoskeleton remodelling in dendritic cells following invasion by Toxoplasma gondii coincides with the onset of a hypermigratory phenotype. Cellular Microbiology. 2013;15(10):1735–1752. doi: 10.1111/cmi.12145. [DOI] [PubMed] [Google Scholar]
- 14.Chow BW, Gu C. The molecular constituents of the blood-brain barrier. Trends Neurosci. 2015;38(10):598–608. doi: 10.1016/j.tins.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Courret N, et al. CD11c- and CD11b-expressing mouse leukocytes transport single Toxoplasma gondii tachyzoites to the brain. Blood. 2006;107(1):309–16. doi: 10.1182/blood-2005-02-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ueno N, et al. Real-time imaging of Toxoplasma-infected human monocytes under fluidic shear stress reveals rapid translocation of intracellular parasites across endothelial barriers. Cell Microbiol. 2014;16(4):580–95. doi: 10.1111/cmi.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lachenmaier SM, et al. Intracellular transport of Toxoplasma gondii through the blood-brain barrier. J Neuroimmunol. 2011;232(1–2):119–30. doi: 10.1016/j.jneuroim.2010.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furtado JM, et al. Toxoplasma gondii tachyzoites cross retinal endothelium assisted by intercellular adhesion molecule-1 in vitro. Immunol Cell Biol. 2012;90(9):912–5. doi: 10.1038/icb.2012.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konradt C, et al. Endothelial cells are a replicative niche for entry of Toxoplasma gondii to the central nervous system. Nat Microbiol. 2016;1:16001. doi: 10.1038/nmicrobiol.2016.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss LM, Kim K. The development and biology of bradyzoites of Toxoplasma gondii. Front Biosci. 2000;5:D391–405. doi: 10.2741/weiss. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tomita T, et al. Making Home Sweet and Sturdy: Toxoplasma gondii ppGalNAc-Ts Glycosylate in Hierarchical Order and Confer Cyst Wall Rigidity. MBio. 2017;8(1) doi: 10.1128/mBio.02048-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson EH, et al. Behavior of parasite-specific effector CD8+ T cells in the brain and visualization of a kinesis-associated system of reticular fibers. Immunity. 2009;30(2):300–11. doi: 10.1016/j.immuni.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schaeffer M, et al. Dynamic imaging of T cell-parasite interactions in the brains of mice chronically infected with Toxoplasma gondii. J Immunol. 2009;182(10):6379–93. doi: 10.4049/jimmunol.0804307. [DOI] [PubMed] [Google Scholar]
- 24.Kim SK, Boothroyd JC. Stage-specific expression of surface antigens by Toxoplasma gondii as a mechanism to facilitate parasite persistence. J Immunol. 2005;174(12):8038–48. doi: 10.4049/jimmunol.174.12.8038. [DOI] [PubMed] [Google Scholar]
- 25.Radke JB, et al. ApiAP2 transcription factor restricts development of the Toxoplasma tissue cyst. Proc Natl Acad Sci U S A. 2013;110(17):6871–6. doi: 10.1073/pnas.1300059110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radke JB, et al. Transcriptional repression by ApiAP2 factors is central to chronic toxoplasmosis. bioRxiv. 2017:100628. doi: 10.1371/journal.ppat.1007035. https://doi.org/10.1101/100628. [DOI] [PMC free article] [PubMed]
- 27.Luder CG, et al. Toxoplasma gondii in primary rat CNS cells: differential contribution of neurons, astrocytes, and microglial cells for the intracerebral development and stage differentiation. Exp Parasitol. 1999;93(1):23–32. doi: 10.1006/expr.1999.4421. [DOI] [PubMed] [Google Scholar]
- 28.Alvarado-Esquivel C, et al. Prevalence of infection with Toxoplasma gondii in landrace and mixed breed pigs slaughtered in Baja California Sur State, Mexico. Eur J Microbiol Immunol (Bp) 2015;5(1):112–5. doi: 10.1556/EUJMI-D-15-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koshy AA, et al. Toxoplasma secreting Cre recombinase for analysis of host-parasite interactions. Nat Methods. 2010;7(4):307–9. doi: 10.1038/nmeth.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halonen SK, et al. Growth and development of Toxoplasma gondii in human neurons and astrocytes. J Neuropathol Exp Neurol. 1996;55(11):1150–6. doi: 10.1097/00005072-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Schluter D, et al. Toxoplasma gondii infection of neurons induces neuronal cytokine and chemokine production, but gamma interferon- and tumor necrosis factor-stimulated neurons fail to inhibit the invasion and growth of T. gondii. Infect Immun. 2001;69(12):7889–93. doi: 10.1128/IAI.69.12.7889-7893.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacRae JI, et al. Mitochondrial metabolism of glucose and glutamine is required for intracellular growth of Toxoplasma gondii. Cell Host Microbe. 2012;12(5):682–92. doi: 10.1016/j.chom.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hermes G, et al. Neurological and behavioral abnormalities, ventricular dilatation, altered cellular functions, inflammation, and neuronal injury in brains of mice due to common, persistent, parasitic infection. J Neuroinflammation. 2008;5:48. doi: 10.1186/1742-2094-5-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dellacasa-Lindberg I, et al. Localized recrudescence of Toxoplasma infections in the central nervous system of immunocompromised mice assessed by in vivo bioluminescence imaging. Microbes Infect. 2007;9(11):1291–8. doi: 10.1016/j.micinf.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Watts E, et al. Novel approaches reveal that Toxoplasma gondii bradyzoites within tissue cysts are dynamic and replicating entities in vivo. MBio. 2015;6(5) doi: 10.1128/mBio.01155-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McConkey GA, et al. Toxoplasma gondii infection and behaviour - location, location, location? J Exp Biol. 2013;216(Pt 1):113–9. doi: 10.1242/jeb.074153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vyas A, et al. Behavioral changes induced by Toxoplasma infection of rodents are highly specific to aversion of cat odors. Proc Natl Acad Sci U S A. 2007;104(15):6442–7. doi: 10.1073/pnas.0608310104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dubey JP, et al. Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts. Clinical Microbiology Reviews. 1998;11(2):267–99. doi: 10.1128/cmr.11.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gazzinelli R, et al. Simultaneous depletion of CD4+ and CD8+ T lymphocytes is required to reactivate chronic infection with Toxoplasma gondii. J Immunol. 1992;149(1):175–80. [PubMed] [Google Scholar]
- 40.Meira CD, et al. Evolution of cytokine profile during the treatment of cerebral toxoplasmosis in HIV-infected patients. Journal of Immunological Methods. 2015;426:14–18. doi: 10.1016/j.jim.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 41.Wilson EH, et al. A critical role for IL-10 in limiting inflammation during toxoplasmic encephalitis. J Neuroimmunol. 2005;165(1–2):63–74. doi: 10.1016/j.jneuroim.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 42.Stumhofer JS, et al. Interleukin 27 negatively regulates the development of interleukin 17-producing T helper cells during chronic inflammation of the central nervous system. Nat Immunol. 2006;7(9):937–45. doi: 10.1038/ni1376. [DOI] [PubMed] [Google Scholar]
- 43.Jankovic D, et al. Conventional T-bet(+)Foxp3(−) Th1 cells are the major source of host-protective regulatory IL-10 during intracellular protozoan infection. J Exp Med. 2007;204(2):273–83. doi: 10.1084/jem.20062175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gazzinelli RT, et al. In the absence of endogenous IL-10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accompanied by overproduction of IL-12, IFN-gamma and TNF-alpha. J Immunol. 1996;157(2):798–805. [PubMed] [Google Scholar]
- 45.O’Brien CA, et al. CD11c-expressing cells affect Treg behavior in the meninges during CNS infection. J Immunol. 2017 doi: 10.4049/jimmunol.1601581. https://doi.org/10.4049/jimmunol.1601581. [DOI] [PMC free article] [PubMed]
- 46.Neuen-Jacob E, et al. Neuropathological studies in the brains of AIDS patients with opportunistic diseases. Int J Legal Med. 1993;105(6):339–50. doi: 10.1007/BF01222119. [DOI] [PubMed] [Google Scholar]
- 47.Arsenijevic D, et al. Metabolic-cytokine responses to a second immunological challenge with LPS in mice with T. gondii infection. Am J Physiol. 1998;274(3 Pt 1):E439–45. doi: 10.1152/ajpendo.1998.274.3.E439. [DOI] [PubMed] [Google Scholar]
- 48.Jacobson JM, et al. Pyrimethamine pharmacokinetics in human immunodeficiency virus-positive patients seropositive for Toxoplasma gondii. Antimicrob Agents Chemother. 1996;40(6):1360–5. doi: 10.1128/aac.40.6.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris TH, et al. Generalized Levy walks and the role of chemokines in migration of effector CD8+ T cells. Nature. 2012;486(7404):545–8. doi: 10.1038/nature11098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.John B, et al. Analysis of behavior and trafficking of dendritic cells within the brain during toxoplasmic encephalitis. PLoS Pathog. 2011;7(9):e1002246. doi: 10.1371/journal.ppat.1002246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Falangola MF, Petito CK. Choroid plexus infection in cerebral toxoplasmosis in AIDS patients. Neurology. 1993;43(10):2035–40. doi: 10.1212/wnl.43.10.2035. [DOI] [PubMed] [Google Scholar]
- 52.Alvarado-Esquivel C, et al. Prevalence of Toxoplasma gondii infection in brain and heart by Immunohistochemistry in a hospital-based autopsy series in Durango, Mexico. Eur J Microbiol Immunol (Bp) 2015;5(2):143–9. doi: 10.1556/1886.2015.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clark RT, et al. T-cell production of matrix metalloproteinases and inhibition of parasite clearance by TIMP-1 during chronic Toxoplasma infection in the brain. ASN Neuro. 2011;3(1):e00049. doi: 10.1042/AN20100027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martens S, et al. Disruption of Toxoplasma gondii parasitophorous vacuoles by the mouse p47-resistance GTPases. PLoS Pathog. 2005;1(3):e24. doi: 10.1371/journal.ppat.0010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ling YM, et al. Vacuolar and plasma membrane stripping and autophagic elimination of Toxoplasma gondii in primed effector macrophages. J Exp Med. 2006;203(9):2063–71. doi: 10.1084/jem.20061318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Melzer T, et al. The gamma interferon (IFN-gamma)-inducible GTP-binding protein IGTP is necessary for Toxoplasma vacuolar disruption and induces parasite egression in IFN-gamma-stimulated astrocytes. Infect Immun. 2008;76(11):4883–94. doi: 10.1128/IAI.01288-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Scharton-Kersten TM, et al. Inducible nitric oxide is essential for host control of persistent but not acute infection with the intracellular pathogen Toxoplasma gondii. J Exp Med. 1997;185(7):1261–73. doi: 10.1084/jem.185.7.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sturge CR, Yarovinsky F. Complex immune cell interplay in the gamma interferon response during Toxoplasma gondii infection. Infect Immun. 2014;82(8):3090–7. doi: 10.1128/IAI.01722-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Degrandi D, et al. Murine guanylate binding protein 2 (mGBP2) controls Toxoplasma gondii replication. Proc Natl Acad Sci U S A. 2013;110(1):294–9. doi: 10.1073/pnas.1205635110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yamamoto M, et al. A cluster of interferon-gamma-inducible p65 GTPases plays a critical role in host defense against Toxoplasma gondii. Immunity. 2012;37(2):302–13. doi: 10.1016/j.immuni.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 61.Suzuki Y, et al. Microglia and macrophages as innate producers of interferon-gamma in the brain following infection with Toxoplasma gondii. Int J Parasitol. 2005;35(1):83–90. doi: 10.1016/j.ijpara.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 62.Hidano S, et al. STAT1 Signaling in Astrocytes Is Essential for Control of Infection in the Central Nervous System. MBio. 2016;7(6) doi: 10.1128/mBio.01881-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ploix CC, et al. CNS-derived CCL21 is both sufficient to drive homeostatic CD4+ T cell proliferation and necessary for efficient CD4+ T cell migration into the CNS parenchyma following Toxoplasma gondii infection. Brain Behav Immun. 2011;25(5):883–96. doi: 10.1016/j.bbi.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Landrith T, et al. CD103+ CD8 T cells in the Toxoplasma-infected exhibit a tissue-resident memory transcriptional profile. Frontiers in Immunology. 2017;8(335) doi: 10.3389/fimmu.2017.00335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bhadra R, et al. PD-1-mediated attrition of polyfunctional memory CD8+ T cells in chronic toxoplasma infection. J Infect Dis. 2012;206(1):125–34. doi: 10.1093/infdis/jis304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bhadra R, et al. Control of Toxoplasma reactivation by rescue of dysfunctional CD8+ T-cell response via PD-1-PDL-1 blockade. Proc Natl Acad Sci U S A. 2011;108(22):9196–201. doi: 10.1073/pnas.1015298108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bhadra R, et al. Donor CD8+ T cells prevent Toxoplasma gondii de-encystation but fail to rescue the exhausted endogenous CD8+ T cell population. Infect Immun. 2013;81(9):3414–25. doi: 10.1128/IAI.00784-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chu HH, et al. Continuous Effector CD8(+) T Cell Production in a Controlled Persistent Infection Is Sustained by a Proliferative Intermediate Population. Immunity. 2016;45(1):159–71. doi: 10.1016/j.immuni.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nance JP, et al. Chitinase dependent control of protozoan cyst burden in the brain. PLoS Pathog. 2012;8(11):e1002990. doi: 10.1371/journal.ppat.1002990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Denkers EY, et al. Perforin-mediated cytolysis plays a limited role in host resistance to Toxoplasma gondii. J Immunol. 1997;159(4):1903–8. [PubMed] [Google Scholar]
- 71.Suzuki Y, et al. Interferon-gamma- and perforin-mediated immune responses for resistance against Toxoplasma gondii in the brain. Expert Rev Mol Med. 2011;13:e31. doi: 10.1017/S1462399411002018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Frickel EM, et al. Parasite stage-specific recognition of endogenous Toxoplasma gondii-derived CD8+ T cell epitopes. J Infect Dis. 2008;198(11):1625–33. doi: 10.1086/593019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sanecka A, et al. Transnuclear CD8 T cells specific for the immunodominant epitope Gra6 lower acute-phase Toxoplasma gondii burden. Immunology. 2016;149(3):270–279. doi: 10.1111/imm.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Blanchard N, et al. Immunodominant, protective response to the parasite Toxoplasma gondii requires antigen processing in the endoplasmic reticulum. Nat Immunol. 2008;9(8):937–44. doi: 10.1038/ni.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brooks JM, et al. Toxoplasma gondii Infections Alter GABAergic Synapses and Signaling in the Central Nervous System. MBio. 2015;6(6) doi: 10.1128/mBio.01428-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.David CN, et al. GLT-1-dependent disruption of CNS glutamate homeostasis and neuronal function by the protozoan parasite Toxoplasma gondii. PLoS Pathog. 2016;12(6):e1005643. doi: 10.1371/journal.ppat.1005643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barker-Haliski M, White HS. Glutamatergic mechanisms sssociated with seizures and epilepsy. Cold Spring Harb Perspect Med. 2015;5(8):a022863. doi: 10.1101/cshperspect.a022863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Danbolt NC. Glutamate uptake. Prog Neurobiol. 2001;65(1):1–105. doi: 10.1016/s0301-0082(00)00067-8. [DOI] [PubMed] [Google Scholar]
- 79.Rothstein JD, et al. Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature. 2005;433(7021):73–7. doi: 10.1038/nature03180. [DOI] [PubMed] [Google Scholar]
- 80.Asada H, et al. Cleft palate and decreased brain gamma-aminobutyric acid in mice lacking the 67-kDa isoform of glutamic acid decarboxylase. Proc Natl Acad Sci U S A. 1997;94(12):6496–9. doi: 10.1073/pnas.94.12.6496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kanaani J, et al. Two distinct mechanisms target GAD67 to vesicular pathways and presynaptic clusters. J Cell Biol. 2010;190(5):911–25. doi: 10.1083/jcb.200912101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cabral CM, et al. Neurons are the primary target cell for the brain-tropic intracellular parasite Toxoplasma gondii. PLoS Pathog. 2016;12(2):e1005447. doi: 10.1371/journal.ppat.1005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koshy AA, et al. Toxoplasma co-opts host cells it does not invade. PLoS Pathog. 2012;8(7):e1002825. doi: 10.1371/journal.ppat.1002825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Marchi N, et al. Inflammatory pathways of seizure disorders. Trends Neurosci. 2014;37(2):55–65. doi: 10.1016/j.tins.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dellacasa-Lindberg I, et al. Migratory activation of primary cortical microglia upon infection with Toxoplasma gondii. Infect Immun. 2011;79(8):3046–52. doi: 10.1128/IAI.01042-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Graus F, et al. Antibodies and neuronal autoimmune disorders of the CNS. Journal of Neurology. 2010;257(4):509–517. doi: 10.1007/s00415-009-5431-9. [DOI] [PubMed] [Google Scholar]
- 87.González-Scarano F, Baltuch G. MICROGLIA AS MEDIATORS OF INFLAMMATORY AND DEGENERATIVE DISEASES. Annual Review of Neuroscience. 1999;22(1):219–240. doi: 10.1146/annurev.neuro.22.1.219. [DOI] [PubMed] [Google Scholar]
- 88.Stephan AH, et al. The complement system: an unexpected role in synaptic pruning during development and disease. Annu Rev Neurosci. 2012;35:369–89. doi: 10.1146/annurev-neuro-061010-113810. [DOI] [PubMed] [Google Scholar]
- 89.Stevens B, et al. The classical complement cascade mediates CNS synapse elimination. Cell. 2007;131(6):1164–78. doi: 10.1016/j.cell.2007.10.036. [DOI] [PubMed] [Google Scholar]
- 90.Tremblay ME, et al. Microglial interactions with synapses are modulated by visual experience. PLoS Biol. 2010;8(11):e1000527. doi: 10.1371/journal.pbio.1000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hong S, et al. Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science. 2016;352(6286):712–6. doi: 10.1126/science.aad8373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vasek MJ, et al. A complement-microglial axis drives synapse loss during virus-induced memory impairment. Nature. 2016;534(7608):538–43. doi: 10.1038/nature18283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schafer DP, et al. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron. 2012;74(4):691–705. doi: 10.1016/j.neuron.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen Z, et al. Microglial displacement of inhibitory synapses provides neuroprotection in the adult brain. Nat Commun. 2014;5:4486. doi: 10.1038/ncomms5486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Montoya JG, et al. Toxoplasmic myocarditis and polymyositis in patients with acute acquired toxoplasmosis diagnosed during life. Clin Infect Dis. 1997;24(4):676–83. doi: 10.1093/clind/24.4.676. [DOI] [PubMed] [Google Scholar]
- 96.Gherardi R, et al. Skeletal muscle toxoplasmosis in patients with acquired immunodeficiency syndrome: a clinical and pathological study. Ann Neurol. 1992;32(4):535–42. doi: 10.1002/ana.410320409. [DOI] [PubMed] [Google Scholar]
- 97.Cuturic M, et al. Toxoplasmic polymyositis revisited: case report and review of literature. Neuromuscul Disord. 1997;7(6–7):390–6. doi: 10.1016/s0960-8966(97)00098-9. [DOI] [PubMed] [Google Scholar]
- 98.Ferreira-da-Silva MD, et al. Primary skeletal muscle cells trigger spontaneous Toxoplasma gondii tachyzoite-to-bradyzoite conversion at higher rates than fibroblasts. Int J Med Microbiol. 2009;299(5):381–388. doi: 10.1016/j.ijmm.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 99.Swierzy IJ, Luder CG. Withdrawal of skeletal muscle cells from cell cycle progression triggers differentiation of Toxoplasma gondii towards the bradyzoite stage. Cell Microbiol. 2015;17(1):2–17. doi: 10.1111/cmi.12342. [DOI] [PubMed] [Google Scholar]
- 100.Radke JR, et al. Changes in the expression of human cell division autoantigen-1 influence Toxoplasma gondii growth and development. PLoS Pathog. 2006;2(10):e105. doi: 10.1371/journal.ppat.0020105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jin RM, et al. Regulatory T cells promote myositis and muscle damage in Toxoplasma gondii infection. J Immunol. 2017;198(1):352–362. doi: 10.4049/jimmunol.1600914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Takacs AC, et al. Interferon-gamma restricts Toxoplasma gondii development in murine skeletal muscle cells via nitric oxide production and immunity-related GTPases. PLoS One. 2012;7(9):e45440. doi: 10.1371/journal.pone.0045440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Karpati G, et al. Expression of immunoreactive major histocompatibility complex products in human skeletal muscles. Ann Neurol. 1988;23(1):64–72. doi: 10.1002/ana.410230111. [DOI] [PubMed] [Google Scholar]
- 104.Emslie-Smith AM, et al. Major histocompatibility complex class I antigen expression, immunolocalization of interferon subtypes, and T cell-mediated cytotoxicity in myopathies. Hum Pathol. 1989;20(3):224–31. doi: 10.1016/0046-8177(89)90128-7. [DOI] [PubMed] [Google Scholar]
- 105.Oldenhove G, et al. Decrease of Foxp3+ Treg cell number and acquisition of effector cell phenotype during lethal infection. Immunity. 2009;31(5):772–86. doi: 10.1016/j.immuni.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hall AO, et al. The cytokines interleukin 27 and interferon-gamma promote distinct Treg cell populations required to limit infection-induced pathology. Immunity. 2012;37(3):511–23. doi: 10.1016/j.immuni.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Couper KN, et al. Anti-CD25 antibody-mediated depletion of effector T cell populations enhances susceptibility of mice to acute but not chronic Toxoplasma gondii infection. J Immunol. 2009;182(7):3985–94. doi: 10.4049/jimmunol.0803053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rayavarapu S, et al. Idiopathic inflammatory myopathies: pathogenic mechanisms of muscle weakness. Skelet Muscle. 2013;3(1):13. doi: 10.1186/2044-5040-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]