Abstract
The use of a service-oriented architecture (SOA) has been identified as a promising approach for improving health care by facilitating reliable clinical decision support (CDS). A review of the literature through October 2013 identified 44 articles on this topic. The review suggests that SOA related technologies such as Business Process Model and Notation (BPMN) and Service Component Architecture (SCA) have not been generally adopted to impact health IT systems’ performance for better care solutions. Additionally, technologies such as Enterprise Service Bus (ESB) and architectural approaches like Service Choreography have not been generally exploited among researchers and developers. Based on the experience of other industries and our observation of the evolution of SOA, we found that the greater use of these approaches have the potential to significantly impact SOA implementations for CDS
Keywords: Literature review, service oriented architecture, clinical decision support, business process management, service orientation
1. Introduction
1.1. Service Oriented Architecture in Health Care
Service-oriented architecture (SOA) can be defined as “an open, agile, extensible, federated, composable architecture comprised of autonomous, Quality of Service (QoS)-capable, vendor diverse, interoperable, discoverable, and potentially reusable services, implemented as Web services” [1]. SOA has been generally accepted as an enterprise information technology (IT) architecture approach and is being increasingly adopted by various enterprises according to a recent report published by Gartner [2].
Although there is an increasing trend in adoption of SOA in other sectors of the economy, its implementation in health care has been relatively slow. According to a survey of 2,165 companies conducted by Forrester Research, SOA adoption in healthcare and public sectors remains low, whereas utilities, financial institutions and insurance companies show a high rate of acceptance and implementation [3]. An example of the high impact of SOA in other industries is the Banking Industry Architecture Network (BIAN), which is a worldwide not-for-profit organization with more than 30 technology and banking members that have adopted SOA as a strategy to face the challenges of a dynamic, competitive and globalized market [4].
Despite its slow start, pioneering healthcare organizations have adopted SOA as an integration strategy [5]. These organizations have recognized that by integrating and automating their systems, they can reduce costs and improve quality of service. Some other benefits that the SOA approach provides to healthcare organizations include interoperability, increased accuracy of medical data and compliance with new regulations [6]. Recognizing the importance of SOA, a number of organizations and governments have undertaken initiatives to support its advancement in health care. A prominent effort in this area is the Healthcare Services Specification Project (HSSP), which is a joint effort between Health Level 7 (HL7) and the Object Management Group (OMG) that focuses on service specification standards based on SOA principles [7]. HL7 is an international authority on standards for interoperability of health information technology [8] and OMG is an international authority on computer standards for a wide range of industries [9]. There are several national efforts worldwide aimed at advancing and leveraging SOA-based health IT architectures. Of note, Canada Health Infoway is an effort to accelerate the adoption of Electronic Health Records (EHR) across Canada that leverages SOA as a core architectural foundation [10].
1.2. Clinical Decision Support
Health care is a heterogeneous environment consisting of different types of information systems and domains. Examples of information systems in health care include electronic health record (EHR) systems, picture archiving and communication systems (PACS), laboratory information systems (LIS) and clinical decision support systems (CDSS).
Clinical decision support (CDS) provides clinicians, patients, or other individuals with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and health care [11]. CDS is an important driver for health information technology (HIT) because it can support clinical decision making, improve patient outcomes, reduce unnecessary mistakes and expenses, and increase efficiency [12].
Indeed, improving and creating new CDS modules is often an important IT initiative for many healthcare organizations. The importance of CDS has also been emphasized by a number of initiatives. For example, maturity models focusing on the management of information system technologies in health care such as the Electronic Healthcare Maturity Model (eHMM) developed by Quintegra [13], the Electronic Health Record Adoption Model (EHRAM) established by the Healthcare Information and Management Systems Society (HIMSS) [14, 15] and the Electronic Patient Record (EPR) maturity model established by the United Kingdom National Health Service (NHS) [16] all identify CDS as an essential aspect of achieving advanced HIT capabilities. Similarly, the Institute of Medicine (IOM) recognized CDS as an important strategy for improving the quality of patient care [17].
Despite the benefits offered by CDS to improve health and healthcare, most clinical decisions are made without the assistance of computerized CDS [11, 18], and only a limited number of organizations are implementing advanced CDS functionalities [19]. Research on this subject suggests a number of barriers to the adoption of CDS [11, 12, 20], with one critical obstacle being the tight coupling of many CDS functionalities to specific software systems [11, 21]. This makes it difficult to transfer clinical knowledge across applications. SOA has been proposed as a potential solution to this problem [22–24]. Other benefits that a SOA approach provides CDS include the following:
Facilitate knowledge maintenance: CDS content can be centralized, thereby reducing maintenance efforts [23, 25]. For example, specialized medical organizations can develop and maintain clinical guidelines and expose their services to healthcare organizations [23].
Reduce costs: SOA allows cost reduction by reusing existing CDS services, thus minimizing time of software development and simplifying software maintenance [22, 23, 25].
Improve agility: SOA allows implementation of new CDS functionalities in a timely manner [7].
Despite the potential of SOA to provide a transforming approach to enabling CDS at scale, there has been no comprehensive summary and analysis of the relevant literature on SOA for CDS. Thus, in order to accelerate progress in this field, this manuscript reviews the relevant literature, highlights gaps in research, and provides recommendations to move this field forward. The scope of the review is to describe and assess recent progress regarding the use of SOA in the context of CDS.
This manuscript encompasses a review of (1) current implementations of SOA for CDS, (2) associated architectural approaches, and (3) relevant health IT standards. We believe that this manuscript will serve as a useful guide for future research and implementation of SOA in CDS.
2. Methods
The systematic review was conducted following the process proposed by Kitchenham [26] and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. The process consisted of three phases: planning, conduction and reporting. In the planning phase, the research questions and systematic review protocol were defined. During the conduction phase, primary studies were identified, selected, and evaluated according to the inclusion and exclusion criteria previously defined. Data were extracted and synthesized for each selected study using data extraction forms developed at the planning phase. Finally, in the reporting phase, the final report was created and presented.
2.1. Data Sources and Searches
The electronic bibliographic databases screened included the Association for Computing Machinery (ACM) Digital Library, Compendex, IEEE Explore, Science Direct, Springer, Web of Science, and Scopus (through 20 October 2013). The first six databases are considered efficient for conducting a systematic review in the context of software engineering [28]. We added Scopus since it is considered the largest database of abstracts and citations [29]. Scopus encompasses approximately 4600 health science titles, includes 100% MEDLINE and EMBASE coverage [30], and provides coverage of medical journals.
“Service oriented” and “clinical decision support” were used as the main keywords for the search, along with the following related terms:
service oriented: “service-oriented”, “service based”, “service-based”, “service orientation”, “service-orientation”, “SOC” and “SOA”
clinical decision support: “CDS” and “CDSS”
The following search string was applied and adapted to each publications database:
(“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOC” OR “SOA”) AND (“clinical decision support” AND “CDS” AND “CDSS”)
The exact search method for each database is showed in Appendix A.
2.2. Study Selection
Only publications written in English were included in this systematic review. The following inclusion and exclusion criteria were used:
Inclusion criteria (at least one required):
The study proposes or reports on the design and development of service-oriented CDS.
The study proposes or reports on a new technology for developing service-oriented CDS systems.
The study proposes or reports on a process, method, technique, or reference architecture that supports either the design or the development of service-oriented CDS systems.
The study proposes or reports on a healthcare standard that supports either the design or development of service-oriented CDS systems.
Exclusion criteria:
The study proposes or reports on the design of CDS systems without using service orientation.
The study presents contributions in areas other than CDS.
The study is a table of contents, short course description, tutorial, copyright form or a conference or workshop agenda.
The study selection was performed by one of the authors (SR) in two stages. In the first phase, all potentially relevant studies were selected based on titles, abstracts, and keywords and in consideration of the inclusion and exclusion criteria. In the second phase, each of the studies selected from the previous stage were read in full and analyzed again according to the inclusion and exclusion criteria. In addition, the related works cited by these studies were evaluated and included in the review if they were considered relevant to the search area.
2.3. Data Extraction and Quality Assessment
Data extraction and quality assessment were undertaken by one author (SR) and confirmed by another (VH). Data related to architectural approach, technology adopted, healthcare standards implemented, and challenges and potential solutions were extracted and categorized.
2.4. Data Synthesis and Analysis
The extracted data was tabulated and summarized, any disagreement was resolved by discussion and, when necessary, by involving a third reviewer. The extracted data was grouped into the following topics: publications per year, architectural approach, healthcare standards, and challenges and lessons learned. In the architectural approach, the review focused on categorizing what architectural approaches have been adopted for the implementation of SOA in the CDS domain. In terms of healthcare standards, we extracted from the reviewed articles which medical standards were adopted to achieve semantic interoperability. Finally, we summarized challenges and lessons identified in the reviewed articles.
3. Results
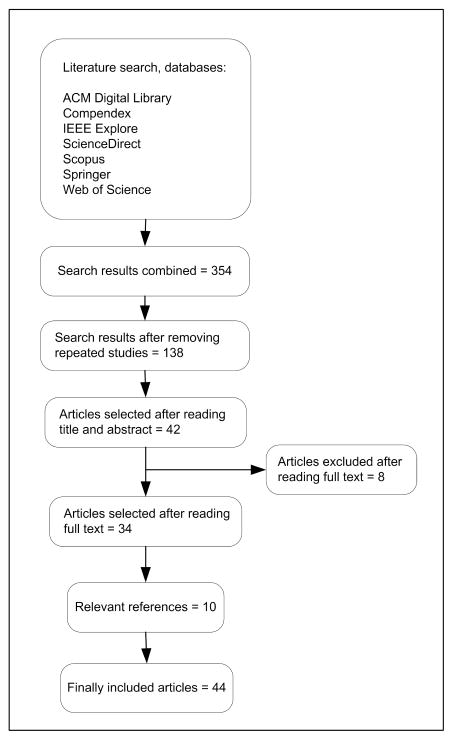
Figure 1 shows the study process selection. The search strategy yielded 138 unique studies. After title and abstract screening of those studies, 42 studies were selected for full text analysis. Eight studies were excluded during the full text review and an additional 10 related works cited by the reviewed studies were added into the reviewed set. In the end, a total of 44 studies were included in the final systematic review (see Figure 1). Appendix B lists all included articles.
Fig. 1.
Study selection process
3.1. Publications per year
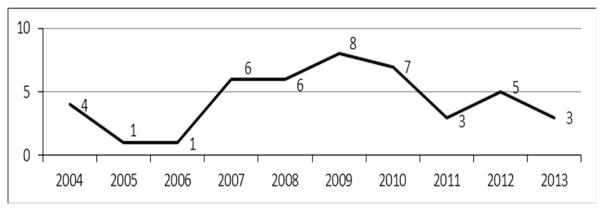
In order to identify the research activity in the area of service oriented CDS, we classified the studies by year of publication (Figure 2). It is important to note that only studies available as of October 2013 were considered in the systematic review. Figure 2 suggests that articles describing the use of SOA for CDS first appeared in the literature in 2004. The volume of articles peaked in 2009 with a slight decline in 2011 and 2013.
Fig. 2.
Number of publications per year
3.2. Architectural approach
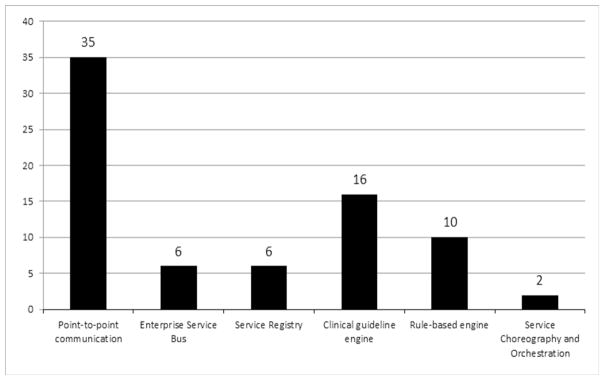
There are a number of possibilities for architectural approaches when implementing SOA based systems [31]. We identified six general architectural themes that are evident in the use of SOA-based CDS: (1) point to point, (2) enterprise service bus (ESB), (3) service registry, (4) clinical guideline engine, (5) rule based engine, and (6) service choreography and orchestration. Figure 3 shows the number of publications addressing each architectural approach. Some studies adopted more than one of these approaches and are therefore counted in multiple categories.
Fig. 3.
Number of publications per architectural approach
These categories were based on topic analysis of all reviewed articles as well as prior literature that described architectural approaches that were most commonly presented when adopting SOA for CDS systems [31–35].
When comparing which architectural approach is most commonly used, the results suggest that point-to-point communication is the most popular architectural approach whereas service choreography seems to be the least explored (Figure 3). We comment on each approach in the following subsections, with sections on guideline engine and rule based engine combined into a single subsection because they are closely related.
3.2.1. Point-to-point communication
The results suggest that point-to-point communication is the most common approach used in the development of SOA-based CDS systems. None of the articles explain the rationale for choosing this approach. However, we assume that it is a natural first step in evolving the integration of services. As discussed in section 3.2.2, ESB provides a more flexible communications approach. In the point-to-point communication approach, each interaction between the applications (e.g., service provider and service consumer) is individually designed, implemented, and administered. Thirty five publications suggested or reported the use of this approach, which represents 79.5 % of the articles included in the review. These studies show that Simple Object Access Protocol (SOAP) seems to be the communication technology of choice to facilitate point to point communication. Table 1 shows in detail the system name, communication approach and clinical implementation area. One critical factor in selecting a communication technology for point to point communication is security, due to the need to transfer and use confidential medical data. SOAP is based on OASIS standards and has in-built security features. However, SOAP does consume more bandwidth when compared to another communication technology, Representational State Transfer (REST). Whilst REST has some advantages, it requires significant effort to make secure data communications.
Table 1.
Publications that adopted or suggested a point to point communication approach
| Communication approach | System name | Clinical implementation area | Publication reference |
|---|---|---|---|
| SOAP | OPNI-Web | Neonatal intensive care unit | [36] |
| SOAP | NewGuide | Homecare-based pressure ulcer prevention, acute ischemic stroke treatment, heart failure management | [37] |
| SOAP | GLEE | Childhood immunization, cough | [38] |
| SOAP | SAGE | Immunization | [39] |
| SOAP | ARTEMIS | Not specified | [40] |
| SOAP | -- | Not specified | [41] |
| SOAP | -- | Chronic disease management | [42] |
| Not specified | -- | Pediatric immunization | [43] |
| SOAP | -- | Asthma, drug-drug interaction checking | [44] |
| SOAP | -- | Not specified | [45] |
| SOAP | -- | Not specified | [25] |
| SOAP | DDSOnt | Collaborative diagnosis decision making among physicians | [46] |
| SOAP | EGADSS | Not specified | [22] |
| SOAP | EGADSS | Not specified | [47] |
| SOAP | SANDS | Drug interaction checking, syndromic surveillance, diagnostic decision support, inappropriate prescribing in older adults, information at point of care, personal health record | [23] |
| Not specified | -- | Translational medicine | [48] |
| Not specified | -- | Childhood immunization | [49] |
| Not specified | OncoTheraper | Pediatric oncology | [50] |
| Not specified | TRIACS | Diabetic retinopathy screening and research | [51] |
| SOAP | SAPHIRE | Hospital and homecare environment | [52, 53] |
| Not specified | DeGeL/Gesher | Preeclampsia/eclampsia toxemia guideline | [54] |
| Not specified | MATE | Cancer multidisciplinary meeting | [55] |
| SOAP | -- | Medication management | [56] |
| Not specified | -- | Intensive care unit | [57] |
| SOAP | -- | Not specified | [24] |
| Not specified | -- | Hypertension guideline | [58] |
| SOAP | -- | Detection and automated monitoring of hospital-acquired infections | [59] |
| Not specified | HealthFlow | Osteoporosis | [60] |
| SOAP | CBPsp | Neonatal intensive care unit | [61] |
| SOAP | -- | -- | [62] |
| Not specified | -- | Palliative care | [63] |
| SOAP | -- | Colon cancer screening | [64] |
| SOAP | -- | Hypertension, chronic care management | [65] |
| SOAP | -- | Diabetes | [66] |
3.2.2. Enterprise Service Bus (ESB)
The ESB is another architectural approach which aims to provide loose coupling for applications with a universal bus that can accept all data formats from any source and integrate data flows into the appropriate applications. An ESB separates the integration logic into manageable pieces and is highly scalable [34]. There is a large spectrum of ESB systems offering different levels of functionality. We identified six articles that proposed or used this architectural pattern. In contrast to the point-to-point communication approach, the messages pass through the ESB, which serves as an intermediary between the service provider and service consumer. Some of the advantages of using an ESB include the ability to support message routing, event triggering, data transformation, security, monitoring and management [67].
In our review, we identified which ESB functionalities are commonly used for the development of service oriented CDS. The most common features are listed in table 2. Table 2 suggests that protocol bridging and data transformation are the main features exploited, whereas only one study suggests using an ESB’s event-driven functionalities to provide CDS services.
Table 2.
ESB based features used or proposed in the analyzed studies
| ESB features used | System name | Implementation or proposed services | Publication reference |
|---|---|---|---|
| Event-driven functionalities | Infoway | Identify patterns of interactions such as spread of epidemics, distribution patterns of patients in particular regions or distribution patterns of particular health services | [68] |
| Protocol bridging, data transformation | HEARTFAID | Intensive care unit | [53, 69] |
| Protocol bridging, data transformation | COSARA | Intensive care unit | [70, 71] |
| Protocol bridging, data transformation | SOCBeS | Chronic disease prevention | [72] |
| Protocol bridging, data transformation | SCP | Multiple morbidities | [73] |
3.2.3. Service registry
The service registry supports different strategies in SOA-based systems such as standardization of service contracts, metadata centralization and notification of service contract changes to consumers [32]. The service registry is a system component that stores information related to each service (e.g., description, policies, contract location, and versions). Thus, service consumers can find the services that fulfill their requirements by querying the service registry.
Table 3 suggests that the provision of service descriptions is the main feature exploited from the service registry.
Table 3.
Architectures that include a service registry
3.2.4. Clinical guideline engine and rule engine
In addition to point to point communication, ESB and service registry, a fourth important architectural approach in the context of SOA-enabled CDS is the use of a clinical guideline engine or a rule engine. We considered a clinical guideline engine to be a program capable of interpreting clinical knowledge expressed in a computerized format [74], whereas we considered a rule engine to be a software system that is designed to manage and enforce business rules expressed in a specified format such as if-then formats [75].
Table 4 presents an overview of which clinical guideline engines and rule engines were employed, as well as the guideline or rule languages used by these systems.
Table 4.
Systems that suggest or adopt guideline engine or rule engine
| System name | Rule/guideline engine | Language | Publication reference |
|---|---|---|---|
| GLEE | GLEE | GuideLine Interchange Format (GLIF) | [38] |
| SAPHIRE | GLEE | GLIF | [52] |
| NewGuide | -- | Flow-chart like approach with strong connection with Petri Nets | [37] |
| SAGE | SAGE | SAGE guideline model | [39] |
| -- | ActiveBPEL | Business Process Execution Engine (BPEL) | [41] |
| -- | Collaxa BPEL Engine | BPEL | [44] |
| BJC Healthcare | -- | BPEL | [45] |
| -- | SEBASTIAN | Rule-based | [42] |
| -- | Jess | Rule-based | [44] |
| HEARFAID | Jena | Rule-based | [69] |
| EGADSS | C Language Integrated Production System (CLIPS) | Rule-based | [22, 47] |
| -- | iLog Rules | Rule-based | [48] |
| -- | -- | Rule-based | [49] |
| -- | SEBASTIAN | Rule-based | [56] |
| -- | SEBASTIAN | Rule-based | [24] |
| -- | -- | Rule-based | [58] |
| -- | Arden Syntax engine | Arden Syntax | [59] |
| -- | -- | Rule-based | [65] |
| SCP | OpenCDS | Rule-based | [73] |
| TRIACS | Triana | Triana workflow language | [51] |
| DeGeL/Gesher | Asbru engine | Asbru | [54] |
| MATE | Tallis | PROforma | [55] |
| COSARA | -- | BPEL | [71] |
| -- | -- | SAGE guideline model | [58] |
| HealthFlow | Shark | XML Process Definition Language (XPDL) | [60] |
| -- | -- | BPEL | [64] |
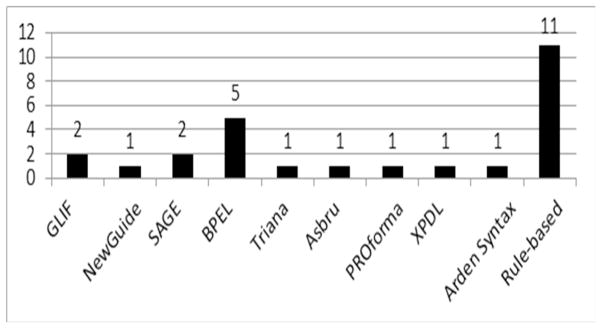
We identified a number of standards for presenting clinical guidelines, also referred to as guideline-modeling methodologies, namely GLIF, NewGuide, SAGE, Asbru, PROForma, Arden Syntax and rule-based standards (rule-based standards can be further refined by various rule languages – see table 5). We also found that BPEL and XPDL, which are typically used for businesses other than healthcare, are also used as a representation language in these systems. The systems listed in table 4 show different trends in adopting the use of the above mentioned guideline representation standards. This is shown in Figure 4.
Table 5.
Rule language used and publication reference
Fig. 4.
Number of systems per language type
It can be seen in Figure 4 that rule-based engines are popular among the developers and that the Business Process Execution Language (BPEL) is beginning to be adopted at a higher rate than clinical guideline representation languages. Additionally, table 5 shows that there is not a clear preference for a specific rule language.
3.2.5. Service choreography and orchestration
The final architectural approach from the reviewed studies that is evident in SOA based CDS is service choreography. In Web service choreography, each participating service defines its part in the interaction and services can interact directly with one another. Architecture closely related to Web service choreography is Web service orchestration. Unlike service choreography, in Web service orchestration (e.g., BPEL), the logic is specified by a single participant which is referred to as the orchestrator [35]. Web service choreographies describe the observable interactions between services from a global perspective, and none of the participants control the interaction. The survey suggests that choreography was only adopted by one research project (OpenKnowledge) [76, 77].
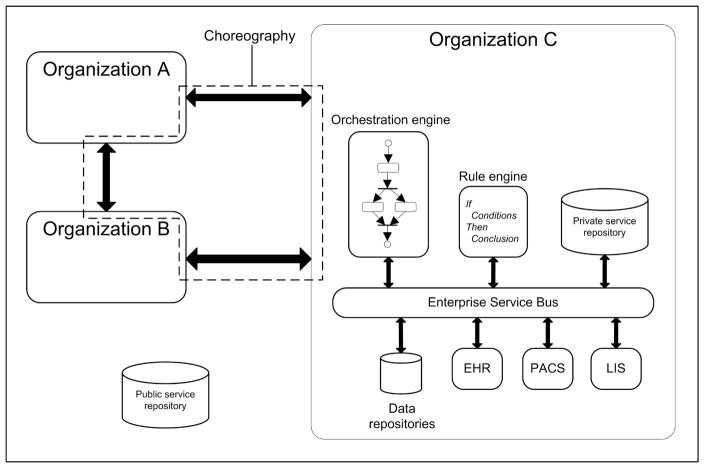
It can be inferred from the studies that all the architectural approaches described above can exist in multiple combinations within a SOA based CDS implementation. For example, in a setting where several healthcare organizations or units have to interact, service choreography can be used to describe the message-based interactions from a global point of view and service orchestration can be used to control the internal processes of each organization. Figure 5 describes a hypothetical scenario where all of these approaches can coexist among organizations A, B, and C. The SOAP-based interactions between the organizations are defined by the Web Service Choreography Description Language (WS-CDL) [78]. Organization C uses an orchestrator engine to deploy processes that define clinical pathways. These clinical pathways are developed based on clinical guidelines and according to the resources available in the organization. The ESB provides connectivity with other systems and monitors service interactions in order to detect health-specific patterns. Additionally, clinical knowledge is captured in the form of rules in the rule engine. The rules have the form: IF conditions THEN conclusion. These rules are integrated in the clinical pathways as tasks on the processes deployed in the orchestration engine. The private service registry contains information on each of the services available inside the organization and also provides a subscription mechanism in order to notify service consumers when a service is modified or updated. The public service registry maintains information about the services available between communicating organizations.
Fig. 5.
Example scenario: co-existence of multiple architectural patterns
3.3. Healthcare standards
It is a very well established issue that semantic interoperability is essential for SOA architectures [1]. Without semantic interoperability, service providers and service consumers cannot make use of the data exchanged. For example, a service that requires past patient diagnoses using a standard terminology will not be able to properly process diagnoses provided using local proprietary codes or free text. Thus, achieving semantic interoperability is an important goal when implementing SOA for CDS.
In order to obtain an accurate picture of how semantic interoperability is accomplished, we extracted and categorized all healthcare standards adopted or suggested by the reviewed studies. The overview below describes the standard categories, and table 6 lists the individual standards identified in the specific articles. The healthcare standards identified were categorized as follows:
Table 6.
Healthcare standards referenced by included studies
| Focus | Name | Publication reference |
|---|---|---|
| Clinical guideline representation | GLIF (Guideline Interchange Format) | [38, 52, 68] |
| NewGuide | [37] | |
| SAGE (Standards-based Sharable Active Guideline Environment) | [39, 58] | |
| Asbru | [54] | |
| PROforma | [55] | |
| Arden Syntax | [22, 47, 59] | |
| GELLO (Guideline Element Language, Object Oriented) | [41] | |
| Patient information | vMR (Virtual Medical Record) | [23, 37–39, 41, 45, 62, 65, 66, 73] |
| CCD (Continuity of Care Document) | [65, 73] | |
| OpenEHR | [40, 57, 66] | |
| CDA (Clinical Document Architecture) | [22, 40, 44, 47, 66, 68] | |
| CEN EN 13606-1 | [40, 52, 66] | |
| HL7 v2.x and HL7 v3 | [23, 57, 65, 73] | |
| Web services and exchange of clinical documents | HSSP Decision Support Service standard | [24, 25, 42, 56, 62, 73] |
| HSSP Retrieve, Locate, and Update Service standard | [24, 25, 62] | |
| HSSP Common Terminology Service standard | [24, 25, 62] | |
| HSSP Identity Cross-Reference Service standard | [62] | |
| HSSP Healthcare and Community Services Provider Directory Service standard | [62] | |
| Healthcare Information Technology Standards Panel (HITSP) SC109 | [62] | |
| IHE XDS (Integrating the Healthcare Enterprise, Cross-enterprise Document Sharing) profile | [52] | |
| NHIN (Nationwide Health Information Network) standards | [23] | |
| IHE Query for Existing Data profile | [62] | |
| IHE Request for Clinical Guidance profile | [62] | |
| Medical terminology | SNOMED CT (Systematized Nomenclature of Medicine - Clinical Terms) | [39, 40, 62, 65, 66] |
| LOINC (Logical Observation Identifiers Names) | [37, 39, 40, 62, 65] | |
| ICD (International Classification of Diseases) | [37, 44, 62] | |
| CPT (Current Procedural Terminology) | [62] | |
| UMLS (Unified Medical Language System) | [62] | |
| HL7 | [62] | |
| RxNorm | [62, 65] | |
| Medical devices | ISO/IEEE 11073-10101 (Health informatics - point-of-care medical device communication - part 10101: nomenclature) | [52] |
Patient information standards: The objective of these standards is to document important patient information such as diagnoses, medications, and lab results. The HL7 Virtual Medical Record (vMR) was specially designed to integrate patient information with CDS systems [79].
Medical terminology standards: These standards define a common terminology and vocabulary to be used in a healthcare domain. Some of these standards, such as the International Classification of Diseases (ICD) for diagnoses and LOINC for laboratory results, have been adopted internationally, whereas other standards, such as drug descriptions, have been adopted in specific regions (e.g., RxNorm in the United States and Anatomical Therapeutic Chemical (ATC) in Europe).
Standards for Web services and exchange of clinical documents: Standards used for exchange of clinical information were grouped in this category. The HSSP Web service standards have been developed specifically to support SOA architectures. The HSSP project is a joint activity between HL7 and OMG [7].
Standards for medical devices: These standards focus on the communication between medical devices and external systems.
Clinical guideline representation standards: Most of these standards have been influenced by workflows and are based on XML syntax. Some of them allow the creation of XML-based clinical guidelines using a graphical editor. Comprehensive comparative reviews of some of these standards have been published elsewhere [74, 80, 81].
In summary, a large number of organizations have taken initiatives to develop and promote standards. This finding indicates a relative consensus on the need for organizations implementing SOA-based CDS to adhere to relevant standards in order to achieve semantic interoperability.
3.4. Challenges and lessons learned
In addition to the architectural and standards analysis, we also analyzed reported challenges and lessons learned during the development and implementation of SOA-based CDS systems. It is important to note, however, that many of the reviewed articles described planned future architectures and could not comment on actual deployment.
Lobach et al. reported an excessive time for data retrieval from the data repository, which slows down the CDS service considerably. They suggested introducing performance-enhancing strategies including multi-threaded data retrieval and pre-caching of patient data [42].
Wright and Sitting highlighted the problem of duplicate and conflicting data distributed in different systems [23]. They solved data inconsistencies, such as different values on vital signals, height, and weight, by using only the most recent observation. Other data points, such as medication lists, were semi-automatically reconciled.
Cucino and Eccher pointed out the lack of mechanisms for defining interactions with people within the BPEL process language [64]. They suggested using BPEL4People [82] in their future work in order to overcome this limitation. The authors of the HealthFlow system highlighted the difficulty in representing complex algorithms in graphical-based representations, such as the XPDL language [60]. The authors proposed two strategies to alleviate this problem and to simplify complex process flowcharts. First, they suggested adopting a hierarchical arrangement of scenarios where a node in a higher lever flowchart expands into a sub-flow, which may consist of multiple steps. Secondly, the authors suggested moving some of the logic into single rule-based nodes which call a comprehensive rule base or other expert system.
Paterno et al. reported that the main limitation of SOA-based CDS systems evaluated in their article is the long time required to receive a CDS response [65]. For future work, the authors suggest optimizing dependent services to speed up service response times and monitoring processes across hardware and software platforms to identify and study latency issues between services.
In summary, the reviewed articles reported the typical challenges of distributed applications. However, time of response seems to be the most critical aspect for SOA-based CDS systems. Some high risk clinical scenarios have little tolerance for latency.
4. Discussion
One of the main goals of the review was to identify the technologies and architectural approaches adopted for the development of SOA based CDS environments. We identified 44 studies that suggested or implemented service oriented CDS. The first studies in this area were published in 2004, with the most publications published in 2009. We discuss further aspects of our findings below.
4.1. Software architecture and development techniques
Point-to-point communication appears to be the current architectural approach of choice, whereas service choreography has been explored in only one project. A comparison of service choreography and service orchestration approaches revealed important results. In choreography, the services interact directly with one another, resulting in less overhead and delay. Using the orchestration approach, the interaction is controlled by one of the participant systems, thus increasing the time for communication [83]. It is important to understand this issue, as the speed of CDS result delivery has been identified as a key aspect in successfully implementing CDS in the clinical workflow [65]. However, orchestration allows simple Web services to perform their function without knowing they are participating in a high level functionality of the application. ESB is the architectural approach that is mainly used to integrate disparate applications, but only one study in our reviewed set [68] identified the event-driven features of ESB as a mechanism to provide CDS services. We believe that CDS should also exploit other features provided by the ESB, such as load balancing, service version selection, service selection based on message data, access control, and exception handling [32].
Similarly, the service registry has not been fully exploited. The main functionality of the service registry is to provide service descriptions, but it can also provide other useful functionalities, such as dependency management, event notification, access control, policy management, and federation [32].
Interestingly, none of the studies reported or suggested the use of Service Component Architecture (SCA), which is a set of OASIS [84] specifications specially designed to build distributed applications based on SOA. The SCA effort was started in 2005 by a group of vendors that includes IBM, Oracle, SAP, and others and handed over to OASIS in 2007. SCA represents the next step in the evolution of SOA, raising the level of abstraction and addressing two issues of software development: complexity and reuse [85]. Additionally, SCA hides the complexity of specifying security, reliability and other quality of service from the application code. Some of the open source SCA implementations include Apache Tuscany [86], Fabric3 [87], FraSCAti [88] and Red Hat Switchyard [89]. The use of SCA would facilitate developers of CDS solutions to follow SOA principles and best practices.
4.2. Business process languages and Web service specifications
Although there are several executable clinical guideline standards that are specific to the medical field, it appears that general-purpose business process languages, such as BPEL, are being used more often for executing simple clinical guideline logic. Interestingly, BPMN 2.0 [90], which has become the preferred standard for business process modeling [91], has not been used by any of the systems we reviewed. Unlike the BPEL language, BPMN supports human tasks, which was one of the reported challenges [64].
An essential aspect of SOA is semantic interoperability, without which service providers and consumers cannot make use of the data exchanged [1]. Efforts such as the HSSP project that provide Web service specifications that can be used to implement CDS represent a major step forward for achieving SOA for CDS. Examples of such HSSP services are the HSSP Decision Support Service, the HSSP Common Terminology Service, and the HSSP Retrieve, Locate, and Update Service.
4.3. HL7 initiatives supporting SOA use in CDS
We believe that providing common building blocks across various software vendors would greatly enhance current CDS capabilities of healthcare systems. Such common building blocks would enable greater use of SOA principles in CDS development. HL7 has a working group devoted to facilitating interoperable CDS that in the past helped developed several CDS standards, such as the Arden Syntax. In 2012, this workgroup identified 10 services and 8 capabilities as being desired for clinical information systems (CIS) to offer SOA-based CDS capabilities [62]. Examples of services identified as being desired are event subscription and notification, cohort identification and entity identification services; table 7 provides the complete list. As for the CDS capabilities identified as being desired, examples include use of standard information models and terminologies, the ability to leverage a DSS and the ability to leverage a unit conversion; table 8 provides the complete list. It is unlikely that current systems can support all of these capabilities and services. In both table 7 and table 8, we have included the SOA architectural approach identified in this review as an additional column that could enable this capability or service. We believe that these services and capabilities could be implemented combining SOA strategies such as ESB and business process management (BPM). We have extended the workgroup description of services with SOA patterns that could fulfill these requirements.
Table 7.
Services required from CIS to enable SOA for CDS identified by HL7 CDS working group (first and second columns [62] ) and SOA architectural approaches that can fulfill these requirements (third column)
| Service or capability | Description, example use case, and relevant standards | SOA architectural approach that could enable this capability or service |
|---|---|---|
| Event subscription and notification service |
Description: Publishes relevant CIS events, which can be listened to by a CDS system to trigger CDS. Allows systems to subscribe to specific types of event notifications. Use case: EHR system publishes events such as the entry of new labs into the clinical data repository, patients checking into appointments, and users logging into the system. CDS system subscribes to types of events that will trigger specific CDS processes. Relevant standards: CORBA event service and notification service; WS-Notification |
ESB: The ESB facilitates integration of legacy systems and can provide content/topic-based routing capabilities which can be based on standards such as WS-Notification or WS-Eventing [92]. Examples of commercial and open source ESBs that support these standards: WS-Notification: Apache ServiceMix, IBM WebSphere, SwitchYard ESB WS-Eventing: WSO2 ESB |
| Cohort identification service |
Description: Identifies a patient cohort (i.e., population) matching search criteria. The result returned is typically a list of identifiers for matching patients. Use case: A population health management system identifies patients with diabetes, hypertension, and congestive heart failure using an EHR system’s cohort identification service Relevant standards: None identified |
ESB: The ESB provides adapters for several communication protocols and mechanisms to access databases. If the CIS does not support Web services, the ESB can provide this capability or directly query databases and return the list of identifiers for the matching patients. |
| Entity identification service |
Description: Identifies whether there is an individual patient matching demographic search criteria (e.g., name, gender, date of birth). Also may be applied to identify other entities such as healthcare providers or facilities. Use case: A vaccine forecasting system identifies whether care organizations A, B, or C have data on a patient for whom a vaccine forecast has been requested. Relevant standards: HSSP Identity Cross-Reference Service standard |
ESB: The HSSP identity Cross-Reference Service standard is based on XML, which is highly supported by the ESB. Therefore, legacy systems can provide this service through the ESB. |
| Clinical data query service |
Description: Retrieves existing clinical data from clinical information system. Use case: Drug-drug interaction alert system retrieves patient medications from an EHR system. Relevant Relevant standards: HSSP Retrieve, Locate, Update Service standard. IHE Query for Existing Data profile. |
ESB: These standards are based on XML which is supported by the ESB. Therefore, legacy systems can provide this service through the ESB. |
| Resource query service |
Description: Retrieves data about local availability of material and human resources. Use case: Based on local availability of dialysis machine, refer patient to external dialysis facility. Relevant standards: HSSP Healthcare and Community Services Provider Directory Service standard; Wf-XML specification (http://www.wfmc.org/wfmc-wf-xml.html) |
ESB: These standards are based on XML, which is supported by the ESB. Therefore, legacy systems can provide this service through the ESB. |
| Data acquisition service |
Description: Retrieves data directly from users. Use case: CDS system asks user if patient is pregnant. Relevant standards: HSSP Retrieve, Locate, Update Service standard. Description: |
ESB: These standards are based on XML, which is highly supported by the ESB. Therefore, legacy systems can provide this service through the ESB. |
| Data addition/update service |
Description: Updates or adds data into a clinical information system. Use case: Health maintenance module updates EHR that patient had an influenza vaccine at grocery store on date X. Relevant standards: HSSP Retrieve, Locate, Update Service standard. |
ESB: These standards are based on XML, which is supported by the ESB. Therefore, legacy systems can provide this service through the ESB. |
| Order placement service |
Description: Places a clinical order. Use case: CPOE CDS module places a pending order for lisinopril 5mg PO QD. Relevant standards: None identified |
ESB: The ESB provides adapters for several communication protocols and mechanisms to access databases. If the CIS does not support Web services, the ESB can provide this capability or directly query databases and return the list of identifiers for the matching patients. |
| User communication service |
Description: Communicates CDS results with appropriate end users. Use case: A CDS system places a note in the EHR system’s alert inbox; CDS system provides a popup alert; physician is paged regarding urgent CDS finding. Relevant standards: None identified |
ESB: The ESB provides adapters for several communication protocols and mechanisms to access databases. If the CIS does not support Web services, the ESB can provide this capability or directly query databases and return the list of identifiers for the matching patients. |
| Task management service |
Description: Allows tasks to be added, tracked, and retrieved. Use case: A population health management system is able to distribute the tasks from a care plan to the task lists of various users. Relevant standards: Wf-XML specification (http://www.wfmc.org/wfmc-wf-xml.html). |
BPM: This capability can be provided by a business process management systems based on workflow languages such as BPMN, which allows modeling of different sets of processes such as orchestration and collaboration and also extends the definition of human interactions[90]. ESB: The results of the BPM can be distributed to legacy systems through the ESB. |
Table 8.
Capabilities required from CIS to enable SOA for CDS identified by HL7 CDS working group (1st and 2nd columns [62] ) and SOA approaches that can fulfill these requirements (3th column)
| Service or capability | Description, example use Case, and relevant Standards | SOA architectural approach that could enable this capability or service |
|---|---|---|
| Use of appropriate, standard information models and terminologies |
Description: Appropriate, standard information models and terminologies are used to instantiate data in the payloads of various services. Use case: A Clinical Data Query Service uses a standard information model to represent the data it provides. Relevant standards: HL7 version 2 and 3 messaging standards; HL7 Virtual Medical Record standard; IHE profiles; HITSP standards; OpenEHR templates; Detailed Clinical Models; SNOMED CT; LOINC; ICD; CPT; various others. |
ESB: Mapping technologies such as XSLT are highly supported by ESB and can be used to map proprietary CIS terminologies and models using an external terminology server such as UMLS. BPM: The interaction between the CIS and the terminology service can be orchestrated using a business process management system based on business process languages such as BPMN. |
| Ability to leverage a DSS |
Description: The CIS is able to use a DSS to obtain patient-specific care assessments and recommendations. Use case: The disease management module of an EHR system uses a DSS to obtain diabetes care recommendations based on national guidelines. Relevant standards: HSSP Decision Support Service standard; IHE Request for Clinical Guidance profile. Description: |
ESB: The ESB provides adapters for several communication protocols and mechanisms to access databases. If the CIS does not support Web services, the ESB can provide this capability or directly query databases. |
| Ability to leverage a terminology service |
Description: The CIS is able to use a service to fulfill terminology needs. Use case: A CIS uses a terminology service to convert internal laboratory codes into the LOINC codes required by a DSS. Relevant standards: HSSP Common Terminology Services 2 standard |
ESB: The ESB provides adapters for several communication protocols and mechanisms to access databases. Thus, if the CIS is not able to call an external terminology service, the ESB can be used to deploy a micro flow that could perform the terminology Web service call and transform the request according to the requirements of the CDS service. BPM: The interaction between the CIS and the terminology service can be orchestrated using a business process management system based on business process languages such as BPMN. |
| Ability to leverage a unit conversion service |
Description: The CIS is able to use a service to convert units. Use case: A CIS uses a unit conversion service to convert laboratory units used by the local CIS into the different laboratory units required by a DSS. Relevant standards: The Unified Code for Units of Measure (http://aurora.regenstrief.org/~ucum/ucum.html). |
ESB: The ESB can be used to consume external services and convert the response to the data format and communication protocol supported by the CIS. BPM: The interaction between the CIS and the unit conversion service can be orchestrated using a business process management system based on business process languages such as BPMN. |
| Ability to leverage a data transformation service |
Description: The CIS is able to use a service to render structured data into a human-readable format. Use case: The disease management module of an EHR system uses a data presentation service to convert an XML document representing diabetes care needs into an HTML diabetes management dashboard to be presented to a clinician. Relevant standards: W3C XSL Formatting Objects (http://www.w3.org/wiki/Xsl-fo) |
ESB: The ESB can be used to consume external services and convert the response to the data format and communication protocol supported by the CIS. BPM: The interaction between the CIS and the data transformation service can be orchestrated using a business process management system based on business process languages such as BPMN. |
| Ability to leverage a data presentation service |
Description: The CIS is able to use a service to render structured data into a humanreadable format. Use case: The disease management module of an EHR system uses a data presentation service to convert an XML document representing diabetes care needs into an HTML diabetes management dashboard to be presented to a clinician. Relevant standards: W3C XSL Formatting Objects (http://www.w3.org/wiki/Xsl-fo). |
ESB: Data model transformation is one of the main functionalities of the ESB. Thus, this transformation can be performed inside the ESB using technologies such as XSLT. |
| Ability to populate a data warehouse in real-time |
Description: The CIS is able to populate an enterprise data warehouse in real-time, as opposed to nightly batches. Use case: A healthcare organization builds CDS functionality against the data warehouse. Relevant standards: None identified. |
ESB: The CIS can perform this task using the different database communication protocols supported by the ESB. BPM: The interaction between the CIS and the data warehouse can be defined using a business process management system based on business process languages such as BPMN. |
| Maintenance of audit logs |
Description: The CIS maintains an audit log of all service interactions. Use case: A CIS maintains an audit log of data provided to, and recommendations received from, an external CDS service. Relevant standards: Healthcare Information Technology Standards Panel (HITSP) SC109. |
ESB: Audit logs of service interactions are often part of the monitoring and management tools provided by the ESB [32]. Additionally, other technologies such as Business Activity Monitor (BAM) and Complex Event Processing (CEP), which are commonly used on SOA architectures, can also be implemented for this purpose [93]. |
5. Limitations
The search was limited to English-language articles published until the end of October 2013. Also, our review is based on published literature only, whereas there could be additional relevant CDS implementations that have not yet been described in the literature.
6. Conclusion
The great promise of SOA for CDS can be achieved more rapidly if best practices identified in other industries such as finance are adopted. Several technologies and methodologies have been developed around the concept of SOA, and they have the potential to enable a new range of opportunities for CDS. These include BPMN for optimizing clinical pathways and SCA for Web service composition. We also recommend that service choreography be further explored for use in SOA based CDS implementations.
Future work
One recommended focal area for future work is studying other industries and applying best practices from those industries when implementing SOA-based CDS. Another critical aspect that needs further investigation is improvement in the overall response time for real-time CDS. For integrated systems dealing with large amounts of patient data, improved response times could potentially be achieved through the incorporation of systematic approaches for estimating and planning for computational resource requirements based on prior utilization data. Furthermore, performance optimization techniques identified in this review, such as multi-threaded database queries and pre-caching of patient data, could be systematically applied to further optimize service response times and to enable real-time CDS.
Acknowledgments
VH is supported by the Intramural Research Program of the National Institutes of Health Clinical Center and the National Library of Medicine.
KK’s effort for this review was supported by the University Of Utah Department Of Biomedical Informatics. KK has in the recent past or is currently serving as a consultant on CDS to the following organizations: the U.S. Office of the National Coordinator for Health IT, Partners HealthCare, RAND Corporation, ESAC, Inc., McKesson InterQual, ARUP Laboratories, Inflexxion, Inc., and Intelligent Automation, Inc. KK receives royalties for a Duke University-owned CDS technology for infectious disease management known as CustomID that he helped develop. KK was formerly a consultant for Religent, Inc. and a co-owner and consultant for Clinica Software, Inc., both of which provide commercial CDS services. KK no longer has a financial relationship with either Religent or Clinica Software.
Appendix A. ACM Digital Library
The search in the ACM Digital Library was performed on October 16, 2013 and four studies were obtained. Because of the options available in this database the search string had to be divided into the following two substrings:
ACM Digital Library
The search in the ACM Digital Library was performed on October 16, 2013 and four studies were obtained. Because of the options available in this database the search string had to be divided into the following two substrings:
Table. 1.
Search strings used on the ACM Digital Library database
| Search string | Number of publications obtained |
|---|---|
| (Abstract:”service oriented” OR Abstract:”service-oriented” OR Abstract:”service based” OR Abstract:”service-based” OR Abstract:”service orientation” OR Abstract:”service-orientation” OR Abstract:”SOC” OR Abstract:”SOA”) AND (Abstract:”Clinical Decision Support” OR Abstract:”CDS” OR Abstract:”CDSS”) | 3 |
| (Title:”service oriented” OR Title:”service-oriented” OR Title:”service based” ORTitle:”service-based” OR Abstract:”service orientation” ORAbstract:”service-orientation” OR Title:”SOC” OR Title:”SOA”) AND (Title:”Clinical Decision Support” OR Title:”CDS” ORTitle:”CDSS”) | 1 |
Compedex
The search in the Compendex database was performed on October 16, 2013 and 80 studies were returned. The search was conducted in the subject, title and abstract of all the databases available. The result was filtered by language, considering only studies written in English. The defined search is presented in the following table.
Table. 2.
Search string used on Compendex
| Search string | Number of publications obtained |
|---|---|
| (((“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOA” OR “SOC”) WN KY) AND ((“clinical decision support” OR “CDS” OR “CDSS”) WN KY)), English only | 80 |
IEEE Explore
Since IEEE Xplore does now allow searching in the abstract and title in the same string, the search string was divided into the following two substrings. The search was performed on October 16, 2013 and 13 studies were returned.
Table. 3.
Search string used on IEEE Xplore
| Search strings | Number of publications obtained |
|---|---|
| ( “Abstract”:”service oriented” OR “Abstract”:”service-oriented” OR “Abstract”:”service based” OR “Abstract”:”service-based” OR “Abstract”:”service orientation” OR “Abstract”:”service-orientation” OR “Abstract”:”SOC” OR “Abstract”:”SOA”) AND ( “Abstract”:”Clinical decision support” OR “Abstract”:”CDS” OR “Abstract”:”CDSS”) | 13 |
| ( “Document Title”:”service oriented” OR “Document Title”:”service-oriented” OR “Document Title”:”service based” OR “Document Title”:”service-based” OR “Document Title”:”service orientation” OR “Document Title”:”service-orientation” OR “Document Title”:”SOC” OR “Document Title”:”SOA”) AND ( “Document Title”:”Clinical decision support” OR “Document Title”:”CDS” OR “Document Title”:”CDSS”) | 0 |
ScienceDirect
The search in ScienceDirect was performed on October 17, 2013. The title, abstract, and keywords were included and 12 studies were returned. The following table shows the search string and number of publications retrieved.
Table. 4.
Search string used on ScienceDirect
| Search strings | Number of publications obtained |
|---|---|
| TITLE-ABSTR-KEY(“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOC” OR “SOA”) and TITLE-ABSTR-KEY(“clinical decision support” OR “CDS” OR “CDSS”) | 12 |
Scopus
The search in Scopus was performed on October 17, 2013 and 79 studies were retrieved. The following table shows the string used in this database.
Table. 5.
Search string used on Scopus
| Search strings | Number of publications obtained |
|---|---|
| TITLE-ABS-KEY((“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOC” OR “SOA”) AND (“clinical decision support” OR “CDS” OR “CDSS”)) | 79 |
Springer
The search in Springer was performed on October 17, 2013. The following table shows the string used in the Springer search engine.
Table. 6.
Search string used on Springer
| Search strings | Number of publications obtained |
|---|---|
| (“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation”) AND (“clinical decision support”) | 118 |
We removed the terms “CDS” and “CDSS” from the search string because we obtained several not related studies (393). This is because Springer does not provide a search tool that could limit the search to the abstract and title; it does search in the whole content of the studies.
Web of Science
The search in Web of Science was performed on October 17, 2013 and a set of 48 articles was obtained. Since this database does not allow searching by abstract, the search was performed using the title and “topic”. The defined search string is presented in the following table.
Table. 7.
Search string used on Web of Science
| Search strings | Number of publications obtained |
|---|---|
| Topic=((“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOC” OR “SOA”) AND (“clinical decision support” OR “CDS” OR “CDSS”)) OR Title=((“service oriented” OR “service-oriented” OR “service based” OR “service-based” OR “service orientation” OR “service-orientation” OR “SOC” OR “SOA”) AND (“clinical decision support” OR “CDS” OR “CDSS”)) | 48 |
Total of search results
The following table shows the total of articles before and after removing the repeated studies.
Table. 8.
Combined search results
| Database or search engine | Number of search results |
|---|---|
| ACM Digital Library | 4 |
| Compendex | 80 |
| IEEE Explore | 13 |
| ScienceDirect | 12 |
| Scopus | 79 |
| Springer | 118 |
| Web of Science | 48 |
| Combined studies | 354 |
| Repeated studies | 216 |
| Total of studies after removing repeated results | 138 |
Appendix B
- 1.Erl T. Service-Oriented Architecture Concepts, Technology, and Design. Prentice Hall PTR; 2005. [Google Scholar]
- 2.Malinverno P, Plummer DC, Van Huizen G. Magic Quadrant for Application Services Governance. 2013. [Google Scholar]
- 3.Heffner R, Leganza G. SOA Adoption 2010: Still Important, Still Strong. 2011. [Google Scholar]
- 4.Tesselaar H. What’s SOA got to do with it. [Accessed 6 Dec 2013];Bobsguide. http://bian.org/participate/bian-blog/whats-soa-got-to-do-with-it/
- 5.Dobrescu R, Purcarea V. Impact of Information Technology on the Quality of Health Services. In: Borangiu T, Thomas A, Trentesaux D, editors. Serv Orientat Holonic Multi-Agent Manuf Control SE - 23. Springer; Berlin Heidelberg: 2012. pp. 307–319. [Google Scholar]
- 6.Konstantinos K, Marinos T, Da Cunha PR. SOA Implementation Critical Success Factors in Healthcare. J Enterp Inf Manag. 2013;26:343– 362. doi: 10.1108/JEIM-06-2012-0036. [DOI] [Google Scholar]
- 7.Kawamoto K, Honey A, Rubin K. The HL7-OMG Healthcare Services Specification Project: Motivation, Methodology, and Deliverables for Enabling a Semantically Interoperable Service-oriented Architecture for Healthcare. J Am Med Inf Assoc. 2009;16:874–881. doi: 10.1197/jamia.M3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.HL7 Health Level Seven International. [Accessed 17 Jan 2014]; http://www.hl7.org/
- 9.OMG Object Magement Group. [Accessed 17 Jan 2014]; http://www.omg.org/
- 10.Canada Health Infoway Inc. EHRS BluePrint an Interoperable EHR framework, Version 2. 2006. [Google Scholar]
- 11.Osheroff JA, Teichc JM, Middletone B, et al. A Roadmap for National Action on Clinical Decision Support. J Am Med informatics Assoc. 2007;14:141–145. doi: 10.1197/jamia.M2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawamoto K, Houlihan Ca, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma B. Electronic Healthcare Maturity Model (eHMM): A White paper. Chennai, India: 2008. [Google Scholar]
- 14.Garets D, Davis M. Policy white Pap. Chicago: HIMSS Anal; 2006. Electronic Medical Records vs. Electronic Health Records : Yes, There Is a Difference. [Google Scholar]
- 15.HIMSS Analytics Electronic Medical Record Adoption Model (EMRAM) [Accessed 10 Jul 2013]; http://www.himssanalytics.org/emram/emram.aspx.
- 16.Wainwright D, Waring T. The information management and technology strategy of the UK National Health Service – Determining progress in the NHS acute hospital sector. Int J Public Sect Manag. 2000;13:241–259. doi: 10.1108/09513550010346152. [DOI] [Google Scholar]
- 17.Graham R, Mancher M, Wolman DM, et al. Clinical Practice Guidelines We Can Trust. National Academies Press; 2011. [PubMed] [Google Scholar]
- 18.SRS, RK, PDC, et al. Physicians and electronic health records: A statewide survey. Arch Intern Med. 2007;167:507–512. doi: 10.1001/archinte.167.5.507. [DOI] [PubMed] [Google Scholar]
- 19.Wu S, Chaudhry B, Wang J, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 20.Sittig DF, Wright A, Osheroff JA, et al. Grand challenges in clinical decision support. J Biomed Inform. 2008;41:387–392. doi: 10.1016/j.jbi.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawamoto K. Integration of Knowledge Resources into Applications to Enable Clinical Decision Support: Architectural Considerations. In: Greenes RA, editor. Clin Decis Support Road Ahead. Elsevier Academic Press; Boston: 2007. pp. 503–38. [Google Scholar]
- 22.Jahnke-Weber JH, Price M, McCallum G. Making available Clinical Decision Support in Service-Oriented Architectures. J Inf Technol Healthc. 2008;6:42–54. [Google Scholar]
- 23.Wright A, Sittig DF. SANDS: A service-oriented architecture for clinical decision support in a National Health Information Network. J Biomed Inform. 2008;41:962–981. doi: 10.1016/j.jbi.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawamoto K, Del Fiol G, Orton C, Lobach DF. System-agnostic clinical decision support services: benefits and challenges for scalable decision support. Open Med Inform J. 2010;4:245–54. doi: 10.2174/1874431101004010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kawamoto K, Lobach DF. Proposal for Fulfilling Strategic Objectives of the U.S. Roadmap for National Action on Decision Support through a Service-oriented Architecture Leveraging HL7 Services. J Am Med Informatics Assoc. 2007;14:146–155. doi: 10.1197/jamia.M2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kitchenham B. Technical Report TR/SE-0401 and NICTA Tecnical Report 0400011T1. 2004. Procedures for Performing Systematic Reviews. [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 [PMC free article] [PubMed] [Google Scholar]
- 28.Dyba T, Dingsoyr T, Hanssen GK. Applying Systematic Reviews to Diverse Study Types: An Experience Report. Empir Softw Eng Meas 2007 ESEM 2007 First Int Symp. 2007:225–234. doi: 10.1109/ESEM.2007.59. [DOI] [Google Scholar]
- 29.Kitchenham B, Charters S. Guidelines for performing Systematic Literature Reviews in Software Engineering. 2007. [Google Scholar]
- 30.Burnham JF. Scopus database: a review. Biomed Digit Libr. 2006;3:1. doi: 10.1186/1742-5581-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arsanjani A. Service-oriented modeling and architecture. IBM Dev Work. 2004:1–15. [Google Scholar]
- 32.Bianco P, Lewis GA, Merson P, Simanta S. TECHNICAL NOTE CMU/SEI-2011-TN-008 Research. 2011. Architecting Service-Oriented Systems. [Google Scholar]
- 33.Charfi A, Mezini M. Proc 2Nd Int Conf Serv Oriented Comput. ACM; New York, NY, USA: 2004. Hybrid Web Service Composition: Business Processes Meet Business Rules; pp. 30–38. [Google Scholar]
- 34.Papazoglou MP, Traverso P, Dustdar S, Leymann F. Service-Oriented Computing: State of the Art and Research Challenges. Computer (Long Beach Calif) 2007;40:38–45. doi: 10.1109/MC.2007.400. [DOI] [Google Scholar]
- 35.Baryannis G, Danylevych O, Karastoyanova D, et al. Service Composition. In: Papazoglou M, Pohl K, Parkin M, Metzger A, editors. Serv Res Challenges Solut Futur Internet SE - 3. Springer; Berlin Heidelberg: 2010. pp. 55–84. [Google Scholar]
- 36.Catley C, Petriu DC, Frize M. Software performance engineering of a Web service-based clinical decision support infrastructure. Softw Eng Notes USA. 2004:130–8. doi: 10.1109/IEMBS.2004.1403937. [DOI] [PubMed] [Google Scholar]
- 37.Ciccarese P, Caffi E, Boiocchi L, et al. A Guideline Management System. Medinfo. 2004:28–32. [PubMed] [Google Scholar]
- 38.Wang D, Peleg M, Tu SW, et al. Design and implementation of the GLIF3 guideline execution engine. J Biomed Inform. 2004;37:305–318. doi: 10.1016/j.jbi.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 39.Ram P, Berg D, Tu S, et al. Executing clinical practice guidelines using the SAGE execution engine. Stud Health Technol Inform. 2004:251–5. [PubMed] [Google Scholar]
- 40.Bicer V, Kilic O, Dogac A, Laleci GB. Archetype-Based Semantic Interoperability of Web Service Messages in the Health Care Domain. Int’l J Semant Web Inf Syst. 2005;1:1–22. [Google Scholar]
- 41.Heard KM, Huang C, Noirot La, et al. AMIA Annu Symp Proc. American Medical Informatics Association; 2006. Using BPEL to define an executable CDS rule process; p. 947. [PMC free article] [PubMed] [Google Scholar]
- 42.Lobach DF, Kawamoto K, Anstrom KJ, et al. Development, Deployment and Usability of a Point-of-Care Decision Support System for Chronic Disease Management Using the Recently-Approved HL7 Decision Support Service Standard. In: Kuhn KA, Warren JR, Leong TY, editors. Medinfo 2007 Proc 12th World Congr Heal. 2007. pp. 861–865. [PubMed] [Google Scholar]
- 43.Nakamura MM, Simons WW, Samuels R, et al. Service-oriented architecture for pediatric immunization decision support. AMIA 2007 Symp Proc. 2007:1056. [PubMed] [Google Scholar]
- 44.Morrison I, Nugrahanto S. Decision Support With BPEL and Web Services. Int J Healthc Inf Syst Informatics. 2007;2:67–74. doi: 10.4018/jhisi.2007040105. [DOI] [Google Scholar]
- 45.Huang Y, Noirot La, Heard KM, et al. Migrating toward a next-generation clinical decision support application: the BJC HealthCare experience. AMIA Annu Symp Proc. 2007:344–8. [PMC free article] [PubMed] [Google Scholar]
- 46.Pires DFF, Teixeira CACAC, Ruiz EESESdESd, et al. A UMLS interoperable solution to support collaborative diagnosis decision making over the internet. Proc ACM Symp Appl Comput Fortaleza, Ceara. 2008:1400–1404. [Google Scholar]
- 47.Jahnke-Weber JH. Design of decoupled clinical decision support for service-oriented architectures. Int J Softw Eng Knowl Eng. 2009;19:159–183. [Google Scholar]
- 48.Kashyap V. From the Bench to the Bedside: The Role of Semantic Web and Translational Medicine for Enabling the Next Generation Healthcare Enterprise. In: Fred A, Filipe J, Gamboa H, editors. Biomed Eng Syst Technol SE - 3. Springer; Berlin Heidelberg: 2009. pp. 35–56. [Google Scholar]
- 49.Zhu VJ, Grannis SJ, Rosenman MB, Downs SM. Implementing broad scale childhood immunization decision support as a web service. AMIA Annu Symp Proc. 2009:745–9. [PMC free article] [PubMed] [Google Scholar]
- 50.Fdez-olivares J, Juan AC, Castillo L. OncoTheraper : Clinical Decision Support for Oncology Therapy Planning Based on Temporal Hierarchical Tasks Networks. Knowl Manag Heal Care Proced. 2009:25–41. [Google Scholar]
- 51.Riposan A, Taylor IJ, Rana O, et al. The TRIACS analytical workflows platform for distributed clinical decision support. 2009 22nd IEEE Int. Symp. Comput. Med. Syst; Piscataway, NJ, USA. 2009. p. 8. [Google Scholar]
- 52.Laleci GB, Dogac A. A Semantically Enriched Clinical Guideline Model Enabling Deployment in Heterogeneous Healthcare Environments. Inf Technol Biomed IEEE Trans. 2009;13:263–273. doi: 10.1109/TITB.2008.2010542. [DOI] [PubMed] [Google Scholar]
- 53.Kameas A, Calemis I. Pervasive Systems in Health Care. In: Nakashima H, Aghajan H, Augusto J, editors. Handb Ambient Intell Smart Environ SE - 12. Springer; US: 2010. pp. 315–346. [Google Scholar]
- 54.Hatsek A, Shahar Y, Taieb-Maimon M, et al. A scalable architecture for incremental specification and maintenance of procedural and declarative clinical decision-support knowledge. Open Med Inform J. 2010;4:255–277. doi: 10.2174/1874431101004010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Acosta DD, Patkar VV, Keshtgar MM, Fox JJ. Challenges in delivering decision support systems: The MATE experience. Lect Notes Comput Sci (including Subser Lect Notes Artif Intell Lect Notes Bioinformatics) 2010;5943:124–140. doi: 10.1007/978-3-642-11808-1_11. LNAI. [DOI] [Google Scholar]
- 56.Del Fiol G, Kawamoto K, Lapointe NMA, et al. Improving Medication Adherence in a Regional Healthcare Information Exchange using a Scalable, Claims-Driven, and Service-Oriented Approach. AMIA Annu Symp Proc. 2010:137–141. [PMC free article] [PubMed] [Google Scholar]
- 57.Backere FD, Steurbaut K, Turck FD, et al. On the Design of a Management Platform for Antibiotic Guidelines in the Intensive Care Unit. Proc. Fifth Int. Conf. Softw. Eng. Adv. (ICSEA 2010); Los Alamitos, CA, USA. 2010. pp. 406–11. [Google Scholar]
- 58.Kim JA, Shim, Kim S, et al. Implementation of Guideline-Based CDSS. Proc. 2011 Int. Conf. Ubiquitious Comput. Multimed. Appl. (UCMA 2011); Los Alamitos, CA, USA. 2011. pp. 96–9. [Google Scholar]
- 59.Fehre K, Adlassnig KP. Service-Oriented Arden-Sysntax-Based Clinical Decision Support. In: Schreier G, Hayn D, Ammenwerth E, editors. Ehealth2011 Heal Informatics Meets Ehealth Von Der Wiss Zur Anwendung Und Zurueck Grenzen Uberwinden Contin Care. 2011. pp. 123–128. [Google Scholar]
- 60.Huser V, Rasmussen LV, Oberg R, Starren JB. Implementation of workflow engine technology to deliver basic clinical decision support functionality. BMC Med Res Methodol. 2011;11:43. doi: 10.1186/1471-2288-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kamaleswaran R, McGregor C. CBPsp: Complex business processes for stream processing. 2012 25th IEEE Can. Conf. Electr. Comput. Eng. Vis. a Greener Futur. CCECE.2012. [Google Scholar]
- 62.Kawamoto K, Jacobs J, Welch BM, et al. Clinical information system services and capabilities desired for scalable, standards-based, service-oriented decision support: consensus assessment of the Health Level 7 clinical decision support Work Group. AMIA Annu Symp Proc. 2012:446–55. [PMC free article] [PubMed] [Google Scholar]
- 63.Mouttham A, Kuziemsky C, Langayan D, et al. Interoperable support for collaborative, mobile, and accessible health care. Inf Syst Front. 2012;14:73–85. doi: 10.1007/s10796-011-9296-y. [DOI] [Google Scholar]
- 64.Cucino R, Eccher C. Modeling Healthcare Processes in BPEL: A Colon Cancer Screening Case Study. In: Szomszor M, Kostkova P, editors. Electron Healthc SE - 10. Springer; Berlin Heidelberg: 2012. pp. 78–85. [Google Scholar]
- 65.Paterno MD, Goldberg HS, Simonaitis L, et al. Using a service oriented architecture approach to clinical decision support: performance results from two CDS Consortium demonstrations. AMIA Annu Symp Proc. 2012:690–698. [PMC free article] [PubMed] [Google Scholar]
- 66.Hussain M, Khattak aM, Khan Wa, et al. Cloud-based Smart CDSS for chronic diseases. Health Technol (Berl) 2013;3:153–175. doi: 10.1007/s12553-013-0051-x. [DOI] [Google Scholar]
- 67.Papazoglou M. What’s in a Service? In: Oquendo F, editor. Softw Archit SE - 3. Springer; Berlin Heidelberg: 2007. pp. 11–28. [Google Scholar]
- 68.Sartipi K, Yarmand MH, Down DG. Mined-knowledge and decision support services in electronic health. Proc. - ICSE 2007 Work. Int. Work. Syst. Dev. SOA Environ. SDSOA’07.2007. [Google Scholar]
- 69.Colantonio S, Martinelli M, Moroni D, et al. A decision support resource as a kernel of a semantic Web based platform oriented to heart failure. Proc. 2008 Int. Conf. Semant. Web Web Serv. SWWS 2008; Las Vegas, NV, United states. 2008. pp. 142–148. [Google Scholar]
- 70.Van Den Bossche B, Van Hoecke S, Danneels C, et al. Design of a {JAIN} SLEE/ESB-based platform for routing medical data in the {ICU} Comput Methods Programs Biomed. 2008;91:265–277. doi: 10.1016/j.cmpb.2008.05.003. doi: http://dx.doi.org/10.1016/j.cmpb.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 71.Steurbaut K, Colpaert K, Gadeyne B, et al. COSARA: Integrated Service Platform for Infection Surveillance and Antibiotic Management in the ICU. J Med Syst. 2012;36:3765–3775. doi: 10.1007/s10916-012-9849-8. [DOI] [PubMed] [Google Scholar]
- 72.Benharref A, Serhani M. Novel Cloud and SOA Based Framework for E-health Monitoring Using Wireless Biosensors. Biomed Heal Informatics, IEEE J. 2013:1. doi: 10.1109/JBHI.2013.2262659. [DOI] [PubMed] [Google Scholar]
- 73.Martínez-García A, Moreno-Conde A, Jódar-Sánchez F, et al. Sharing clinical decisions for multimorbidity case management using social network and open-source tools. J Biomed Inform. 2013 doi: 10.1016/j.jbi.2013.06.007. doi: http://dx.doi.org/10.1016/j.jbi.2013.06.007. [DOI] [PubMed]
- 74.Peleg M, Tu S, Bury J, et al. Comparing Computer-interpretable Guideline Models: A Case-study Approach. J Am Med Informatics Assoc. 2003;10:52–68. doi: 10.1197/jamia.M1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boyer J, Mili H. Agile Business Rule Development. Process, Architecture, and JRules Examples. 2011:251–257. doi: 10.1007/978-3-642-19041-4. [DOI] [Google Scholar]
- 76.Besana P, Patkar V, Glasspool D, Robertson D. Distributed Workflows: The OpenKnowledge Experience. In: Meersman R, Tari Z, Herrero P, editors. Move to Meaningful Internet Syst OTM 2008 Work SE - 123. Springer; Berlin Heidelberg: 2008. pp. 965–975. [Google Scholar]
- 77.Besana P, Patkar V, Barker A, et al. Sharing Choreographies in OpenKnowledge: A Novel Approach to Interoperability. J Softw. 2009;4:833–842. doi: 10.4304/jsw.4.8.833-842. [DOI] [Google Scholar]
- 78.W3C Web Services Choreography Description Language, Version 1.0, W3C Candidate Recommendation. 2005 Nov 9; http://www.w3.org/TR/ws-cdl-10/
- 79. [Accessed 3 Jun 2013];Health Level 7 HL7 Virtual Medical Record (vMR) http://wiki.hl7.org/index.php?title=Virtual_Medical_Record_(vMR)
- 80.De Clercq PA, Blom JA, Korsten HHM, Hasman A. Approaches for creating computer-interpretable guidelines that facilitate decision support. Artif Intell Med. 2004;31:1–27. doi: 10.1016/j.artmed.2004.02.003. doi: http://dx.doi.org/10.1016/j.artmed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 81.Isern D, Moreno A. Computer-based execution of clinical guidelines: A review. Int J Med Inform. 2008;77:787–808. doi: 10.1016/j.ijmedinf.2008.05.010. doi: http://dx.doi.org/10.1016/j.ijmedinf.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 82. [Accessed 21 Jan 2014];OASIS OASIS WS-BPEL Extension for People (BPEL4People) TC. https://www.oasisopen.org/committees/tc_home.php?wg_abbrev=bpel4people.
- 83.Pontes Guimaraes F, Kuroda EH, Batista DM. Performance Evaluation of Choreographies and Orchestrations with a New Simulator for Service Compositions. Comput Aided Model Des Commun Links Networks (CAMAD), 2012 IEEE 17th Int Work; 2012. pp. 140–144. [DOI] [Google Scholar]
- 84.OASIS Service Component Architecture Assembly Model Specification, Version 1.1. [Accessed 22 Jun 2013];Committee Specification Draft 08/Public Review Draft 03. 2011 May 31; http://docs.oasis-open.org/opencsa/sca-assembly/sca-assembly-spec-v1.1-csprd03.pdf.
- 85.Hinchey M, Coyle L. Conquering Complexity. Springer; London: 2012. [Google Scholar]
- 86.The Apache Software Foundation Apache Tuscany. [Accessed 28 Dec 2013]; http://tuscany.apache.org/
- 87.Fabric3 Fabric3. [Accessed 28 Dec 2013]; http://www.fabric3.org/
- 88.OW2 Consortium FraSCAti. [Accessed 28 Dec 2913]; https://wiki.ow2.org/frascati/Wiki.jsp?page=FraSCAti.
- 89.Red Hat Inc. [Accessed 28 Dec 2013];SwitchYard. http://www.jboss.org/switchyard.
- 90. [Accessed 31 May 2013];OMG Business process model and notation (BPMN 2.0) http://www.omg.org/spec/BPMN/2.0/
- 91.Chinosi M, Trombetta A. BPMN: An introduction to the standard. Comput Stand Interfaces. 2012;34:124–134. doi: 10.1016/j.csi.2011.06.002. [DOI] [Google Scholar]
- 92.Papazoglou MP, Heuvel W-J. Service oriented architectures: approaches, technologies and research issues. VLDB J. 2007;16:389–415. doi: 10.1007/s00778-007-0044-3. [DOI] [Google Scholar]
- 93.Safy FZ, El-Ramly M, Salah A. Runtime Monitoring of SOA Applications: Importance, Implementations and Challenges. Serv Oriented Syst Eng (SOSE), 2013 IEEE 7th Int Symp; 2013. pp. 315–319. [DOI] [Google Scholar]
References
- 1.Erl T. Service-Oriented Architecture Concepts, Technology, and Design. Prentice Hall PTR; 2005. [Google Scholar]
- 2.Malinverno P, Plummer DC, Van Huizen G. Magic Quadrant for Application Services Governance. 2013. [Google Scholar]
- 3.Heffner R, Leganza G. SOA Adoption 2010: Still Important, Still Strong. 2011. [Google Scholar]
- 4.Tesselaar H. What’s SOA got to do with it. [Accessed 6 Dec 2013];Bobsguide. http://bian.org/participate/bian-blog/whats-soa-got-to-do-with-it/
- 5.Dobrescu R, Purcarea V. Impact of Information Technology on the Quality of Health Services. In: Borangiu T, Thomas A, Trentesaux D, editors. Serv Orientat Holonic Multi-Agent Manuf Control SE - 23. Springer; Berlin Heidelberg: 2012. pp. 307–319. [Google Scholar]
- 6.Konstantinos K, Marinos T, Da Cunha PR. SOA Implementation Critical Success Factors in Healthcare. J Enterp Inf Manag. 2013;26:343– 362. doi: 10.1108/JEIM-06-2012-0036. [DOI] [Google Scholar]
- 7.Kawamoto K, Honey A, Rubin K. The HL7-OMG Healthcare Services Specification Project: Motivation, Methodology, and Deliverables for Enabling a Semantically Interoperable Service-oriented Architecture for Healthcare. J Am Med Inf Assoc. 2009;16:874–881. doi: 10.1197/jamia.M3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.HL7 Health Level Seven International. [Accessed 17 Jan 2014]; http://www.hl7.org/
- 9.OMG Object Magement Group. [Accessed 17 Jan 2014]; http://www.omg.org/
- 10.Canada Health Infoway Inc. EHRS BluePrint an Interoperable EHR framework, Version 2. 2006. [Google Scholar]
- 11.Osheroff JA, Teichc JM, Middletone B, et al. A Roadmap for National Action on Clinical Decision Support. J Am Med informatics Assoc. 2007;14:141–145. doi: 10.1197/jamia.M2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawamoto K, Houlihan Ca, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma B. Electronic Healthcare Maturity Model (eHMM): A White paper. Chennai, India: 2008. [Google Scholar]
- 14.Garets D, Davis M. Policy white Pap. Chicago: HIMSS Anal; 2006. Electronic Medical Records vs. Electronic Health Records : Yes, There Is a Difference. [Google Scholar]
- 15.HIMSS Analytics Electronic Medical Record Adoption Model (EMRAM) [Accessed 10 Jul 2013]; http://www.himssanalytics.org/emram/emram.aspx.
- 16.Wainwright D, Waring T. The information management and technology strategy of the UK National Health Service – Determining progress in the NHS acute hospital sector. Int J Public Sect Manag. 2000;13:241–259. doi: 10.1108/09513550010346152. [DOI] [Google Scholar]
- 17.Graham R, Mancher M, Wolman DM, et al. Clinical Practice Guidelines We Can Trust. National Academies Press; 2011. [PubMed] [Google Scholar]
- 18.SRS, RK, PDC, et al. Physicians and electronic health records: A statewide survey. Arch Intern Med. 2007;167:507–512. doi: 10.1001/archinte.167.5.507. [DOI] [PubMed] [Google Scholar]
- 19.Wu S, Chaudhry B, Wang J, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 20.Sittig DF, Wright A, Osheroff JA, et al. Grand challenges in clinical decision support. J Biomed Inform. 2008;41:387–392. doi: 10.1016/j.jbi.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawamoto K. Integration of Knowledge Resources into Applications to Enable Clinical Decision Support: Architectural Considerations. In: Greenes RA, editor. Clin Decis Support Road Ahead. Elsevier Academic Press; Boston: 2007. pp. 503–38. [Google Scholar]
- 22.Jahnke-Weber JH, Price M, McCallum G. Making available Clinical Decision Support in Service-Oriented Architectures. J Inf Technol Healthc. 2008;6:42–54. [Google Scholar]
- 23.Wright A, Sittig DF. SANDS: A service-oriented architecture for clinical decision support in a National Health Information Network. J Biomed Inform. 2008;41:962–981. doi: 10.1016/j.jbi.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawamoto K, Del Fiol G, Orton C, Lobach DF. System-agnostic clinical decision support services: benefits and challenges for scalable decision support. Open Med Inform J. 2010;4:245–54. doi: 10.2174/1874431101004010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kawamoto K, Lobach DF. Proposal for Fulfilling Strategic Objectives of the U.S. Roadmap for National Action on Decision Support through a Service-oriented Architecture Leveraging HL7 Services. J Am Med Informatics Assoc. 2007;14:146–155. doi: 10.1197/jamia.M2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kitchenham B. Technical Report TR/SE-0401 and NICTA Tecnical Report 0400011T1. 2004. Procedures for Performing Systematic Reviews. [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 [PMC free article] [PubMed] [Google Scholar]
- 28.Dyba T, Dingsoyr T, Hanssen GK. Applying Systematic Reviews to Diverse Study Types: An Experience Report. Empir Softw Eng Meas 2007 ESEM 2007 First Int Symp. 2007:225–234. doi: 10.1109/ESEM.2007.59. [DOI] [Google Scholar]
- 29.Kitchenham B, Charters S. Guidelines for performing Systematic Literature Reviews in Software Engineering. 2007. [Google Scholar]
- 30.Burnham JF. Scopus database: a review. Biomed Digit Libr. 2006;3:1. doi: 10.1186/1742-5581-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arsanjani A. Service-oriented modeling and architecture. IBM Dev Work. 2004:1–15. [Google Scholar]
- 32.Bianco P, Lewis GA, Merson P, Simanta S. TECHNICAL NOTE CMU/SEI-2011-TN-008 Research. 2011. Architecting Service-Oriented Systems. [Google Scholar]
- 33.Charfi A, Mezini M. Proc 2Nd Int Conf Serv Oriented Comput. ACM; New York, NY, USA: 2004. Hybrid Web Service Composition: Business Processes Meet Business Rules; pp. 30–38. [Google Scholar]
- 34.Papazoglou MP, Traverso P, Dustdar S, Leymann F. Service-Oriented Computing: State of the Art and Research Challenges. Computer (Long Beach Calif) 2007;40:38–45. doi: 10.1109/MC.2007.400. [DOI] [Google Scholar]
- 35.Baryannis G, Danylevych O, Karastoyanova D, et al. Service Composition. In: Papazoglou M, Pohl K, Parkin M, Metzger A, editors. Serv Res Challenges Solut Futur Internet SE - 3. Springer; Berlin Heidelberg: 2010. pp. 55–84. [Google Scholar]
- 36.Catley C, Petriu DC, Frize M. Software performance engineering of a Web service-based clinical decision support infrastructure. Softw Eng Notes USA. 2004:130–8. doi: 10.1109/IEMBS.2004.1403937. [DOI] [PubMed] [Google Scholar]
- 37.Ciccarese P, Caffi E, Boiocchi L, et al. A Guideline Management System. Medinfo. 2004:28–32. [PubMed] [Google Scholar]
- 38.Wang D, Peleg M, Tu SW, et al. Design and implementation of the GLIF3 guideline execution engine. J Biomed Inform. 2004;37:305–318. doi: 10.1016/j.jbi.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 39.Ram P, Berg D, Tu S, et al. Executing clinical practice guidelines using the SAGE execution engine. Stud Health Technol Inform. 2004:251–5. [PubMed] [Google Scholar]
- 40.Bicer V, Kilic O, Dogac A, Laleci GB. Archetype-Based Semantic Interoperability of Web Service Messages in the Health Care Domain. Int’l J Semant Web Inf Syst. 2005;1:1–22. [Google Scholar]
- 41.Heard KM, Huang C, Noirot La, et al. AMIA Annu Symp Proc. American Medical Informatics Association; 2006. Using BPEL to define an executable CDS rule process; p. 947. [PMC free article] [PubMed] [Google Scholar]
- 42.Lobach DF, Kawamoto K, Anstrom KJ, et al. Development, Deployment and Usability of a Point-of-Care Decision Support System for Chronic Disease Management Using the Recently-Approved HL7 Decision Support Service Standard. In: Kuhn KA, Warren JR, Leong TY, editors. Medinfo 2007 Proc 12th World Congr Heal. 2007. pp. 861–865. [PubMed] [Google Scholar]
- 43.Nakamura MM, Simons WW, Samuels R, et al. Service-oriented architecture for pediatric immunization decision support. AMIA 2007 Symp Proc. 2007:1056. [PubMed] [Google Scholar]
- 44.Morrison I, Nugrahanto S. Decision Support With BPEL and Web Services. Int J Healthc Inf Syst Informatics. 2007;2:67–74. doi: 10.4018/jhisi.2007040105. [DOI] [Google Scholar]
- 45.Huang Y, Noirot La, Heard KM, et al. Migrating toward a next-generation clinical decision support application: the BJC HealthCare experience. AMIA Annu Symp Proc. 2007:344–8. [PMC free article] [PubMed] [Google Scholar]
- 46.Pires DFF, Teixeira CACAC, Ruiz EESESdESd, et al. A UMLS interoperable solution to support collaborative diagnosis decision making over the internet. Proc ACM Symp Appl Comput Fortaleza, Ceara. 2008:1400–1404. [Google Scholar]
- 47.Jahnke-Weber JH. Design of decoupled clinical decision support for service-oriented architectures. Int J Softw Eng Knowl Eng. 2009;19:159–183. [Google Scholar]
- 48.Kashyap V. From the Bench to the Bedside: The Role of Semantic Web and Translational Medicine for Enabling the Next Generation Healthcare Enterprise. In: Fred A, Filipe J, Gamboa H, editors. Biomed Eng Syst Technol SE - 3. Springer; Berlin Heidelberg: 2009. pp. 35–56. [Google Scholar]
- 49.Zhu VJ, Grannis SJ, Rosenman MB, Downs SM. Implementing broad scale childhood immunization decision support as a web service. AMIA Annu Symp Proc. 2009:745–9. [PMC free article] [PubMed] [Google Scholar]
- 50.Fdez-olivares J, Juan AC, Castillo L. OncoTheraper : Clinical Decision Support for Oncology Therapy Planning Based on Temporal Hierarchical Tasks Networks. Knowl Manag Heal Care Proced. 2009:25–41. [Google Scholar]
- 51.Riposan A, Taylor IJ, Rana O, et al. The TRIACS analytical workflows platform for distributed clinical decision support. 2009 22nd IEEE Int. Symp. Comput. Med. Syst; Piscataway, NJ, USA. 2009. p. 8. [Google Scholar]
- 52.Laleci GB, Dogac A. A Semantically Enriched Clinical Guideline Model Enabling Deployment in Heterogeneous Healthcare Environments. Inf Technol Biomed IEEE Trans. 2009;13:263–273. doi: 10.1109/TITB.2008.2010542. [DOI] [PubMed] [Google Scholar]
- 53.Kameas A, Calemis I. Pervasive Systems in Health Care. In: Nakashima H, Aghajan H, Augusto J, editors. Handb Ambient Intell Smart Environ SE - 12. Springer; US: 2010. pp. 315–346. [Google Scholar]
- 54.Hatsek A, Shahar Y, Taieb-Maimon M, et al. A scalable architecture for incremental specification and maintenance of procedural and declarative clinical decision-support knowledge. Open Med Inform J. 2010;4:255–277. doi: 10.2174/1874431101004010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Acosta DD, Patkar VV, Keshtgar MM, Fox JJ. Challenges in delivering decision support systems: The MATE experience. Lect Notes Comput Sci (including Subser Lect Notes Artif Intell Lect Notes Bioinformatics) 2010;5943:124–140. doi: 10.1007/978-3-642-11808-1_11. LNAI. [DOI] [Google Scholar]
- 56.Del Fiol G, Kawamoto K, Lapointe NMA, et al. Improving Medication Adherence in a Regional Healthcare Information Exchange using a Scalable, Claims-Driven, and Service-Oriented Approach. AMIA Annu Symp Proc. 2010:137–141. [PMC free article] [PubMed] [Google Scholar]
- 57.Backere FD, Steurbaut K, Turck FD, et al. On the Design of a Management Platform for Antibiotic Guidelines in the Intensive Care Unit. Proc. Fifth Int. Conf. Softw. Eng. Adv. (ICSEA 2010); Los Alamitos, CA, USA. 2010. pp. 406–11. [Google Scholar]
- 58.Kim JA, Shim, Kim S, et al. Implementation of Guideline-Based CDSS. Proc. 2011 Int. Conf. Ubiquitious Comput. Multimed. Appl. (UCMA 2011); Los Alamitos, CA, USA. 2011. pp. 96–9. [Google Scholar]
- 59.Fehre K, Adlassnig KP. Service-Oriented Arden-Sysntax-Based Clinical Decision Support. In: Schreier G, Hayn D, Ammenwerth E, editors. Ehealth2011 Heal Informatics Meets Ehealth Von Der Wiss Zur Anwendung Und Zurueck Grenzen Uberwinden Contin Care. 2011. pp. 123–128. [Google Scholar]
- 60.Huser V, Rasmussen LV, Oberg R, Starren JB. Implementation of workflow engine technology to deliver basic clinical decision support functionality. BMC Med Res Methodol. 2011;11:43. doi: 10.1186/1471-2288-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kamaleswaran R, McGregor C. CBPsp: Complex business processes for stream processing. 2012 25th IEEE Can. Conf. Electr. Comput. Eng. Vis. a Greener Futur. CCECE; 2012.2012. [Google Scholar]
- 62.Kawamoto K, Jacobs J, Welch BM, et al. Clinical information system services and capabilities desired for scalable, standards-based, service-oriented decision support: consensus assessment of the Health Level 7 clinical decision support Work Group. AMIA Annu Symp Proc. 2012:446–55. [PMC free article] [PubMed] [Google Scholar]
- 63.Mouttham A, Kuziemsky C, Langayan D, et al. Interoperable support for collaborative, mobile, and accessible health care. Inf Syst Front. 2012;14:73–85. doi: 10.1007/s10796-011-9296-y. [DOI] [Google Scholar]
- 64.Cucino R, Eccher C. Modeling Healthcare Processes in BPEL: A Colon Cancer Screening Case Study. In: Szomszor M, Kostkova P, editors. Electron Healthc SE - 10. Springer; Berlin Heidelberg: 2012. pp. 78–85. [Google Scholar]
- 65.Paterno MD, Goldberg HS, Simonaitis L, et al. Using a service oriented architecture approach to clinical decision support: performance results from two CDS Consortium demonstrations. AMIA Annu Symp Proc. 2012:690–698. [PMC free article] [PubMed] [Google Scholar]
- 66.Hussain M, Khattak aM, Khan Wa, et al. Cloud-based Smart CDSS for chronic diseases. Health Technol (Berl) 2013;3:153–175. doi: 10.1007/s12553-013-0051-x. [DOI] [Google Scholar]
- 67.Papazoglou M. What’s in a Service? In: Oquendo F, editor. Softw Archit SE - 3. Springer; Berlin Heidelberg: 2007. pp. 11–28. [Google Scholar]
- 68.Sartipi K, Yarmand MH, Down DG. Mined-knowledge and decision support services in electronic health. Proc. - ICSE 2007 Work. Int. Work. Syst. Dev. SOA Environ. SDSOA’07.2007. [Google Scholar]
- 69.Colantonio S, Martinelli M, Moroni D, et al. A decision support resource as a kernel of a semantic Web based platform oriented to heart failure. Proc. 2008 Int. Conf. Semant. Web Web Serv. SWWS; 2008; Las Vegas, NV, United states. 2008. pp. 142–148. [Google Scholar]
- 70.Van Den Bossche B, Van Hoecke S, Danneels C, et al. Design of a {JAIN} SLEE/ESB-based platform for routing medical data in the {ICU} Comput Methods Programs Biomed. 2008;91:265–277. doi: 10.1016/j.cmpb.2008.05.003. doi: http://dx.doi.org/10.1016/j.cmpb.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 71.Steurbaut K, Colpaert K, Gadeyne B, et al. COSARA: Integrated Service Platform for Infection Surveillance and Antibiotic Management in the ICU. J Med Syst. 2012;36:3765–3775. doi: 10.1007/s10916-012-9849-8. [DOI] [PubMed] [Google Scholar]
- 72.Benharref A, Serhani M. Novel Cloud and SOA Based Framework for E-health Monitoring Using Wireless Biosensors. Biomed Heal Informatics, IEEE J. 2013:1. doi: 10.1109/JBHI.2013.2262659. [DOI] [PubMed] [Google Scholar]
- 73.Martínez-García A, Moreno-Conde A, Jódar-Sánchez F, et al. Sharing clinical decisions for multimorbidity case management using social network and open-source tools. J Biomed Inform. 2013 doi: 10.1016/j.jbi.2013.06.007. doi: http://dx.doi.org/10.1016/j.jbi.2013.06.007. [DOI] [PubMed]
- 74.Peleg M, Tu S, Bury J, et al. Comparing Computer-interpretable Guideline Models: A Case-study Approach. J Am Med Informatics Assoc. 2003;10:52–68. doi: 10.1197/jamia.M1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boyer J, Mili H. Agile Business Rule Development. Process, Architecture, and JRules Examples. 2011:251–257. doi: 10.1007/978-3-642-19041-4. [DOI] [Google Scholar]
- 76.Besana P, Patkar V, Glasspool D, Robertson D. Distributed Workflows: The OpenKnowledge Experience. In: Meersman R, Tari Z, Herrero P, editors. Move to Meaningful Internet Syst OTM 2008 Work. SE - 123. Springer; Berlin Heidelberg: 2008. pp. 965–975. [Google Scholar]
- 77.Besana P, Patkar V, Barker A, et al. Sharing Choreographies in OpenKnowledge: A Novel Approach to Interoperability. J Softw. 2009;4:833–842. doi: 10.4304/jsw.4.8.833-842. [DOI] [Google Scholar]
- 78.W3C Web Services Choreography Description Language, Version 1.0, W3C Candidate Recommendation. 2005 Nov 9; http://www.w3.org/TR/ws-cdl-10/
- 79. [Accessed 3 Jun 2013];Health Level 7 HL7 Virtual Medical Record (vMR) http://wiki.hl7.org/index.php?title=Virtual_Medical_Record_(vMR)
- 80.De Clercq PA, Blom JA, Korsten HHM, Hasman A. Approaches for creating computer-interpretable guidelines that facilitate decision support. Artif Intell Med. 2004;31:1–27. doi: 10.1016/j.artmed.2004.02.003. doi: http://dx.doi.org/10.1016/j.artmed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 81.Isern D, Moreno A. Computer-based execution of clinical guidelines: A review. Int J Med Inform. 2008;77:787–808. doi: 10.1016/j.ijmedinf.2008.05.010. doi: http://dx.doi.org/10.1016/j.ijmedinf.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 82. [Accessed 21 Jan 2014];OASIS OASIS WS-BPEL Extension for People (BPEL4People) TC. https://www.oasisopen.org/committees/tc_home.php?wg_abbrev=bpel4people.
- 83.Pontes Guimaraes F, Kuroda EH, Batista DM. Performance Evaluation of Choreographies and Orchestrations with a New Simulator for Service Compositions. Comput Aided Model Des Commun Links Networks (CAMAD), 2012 IEEE 17th Int Work; 2012. pp. 140–144. [DOI] [Google Scholar]
- 84.OASIS Service Component Architecture Assembly Model Specification, Version 1.1. [Accessed 22 Jun 2013];Committee Specification Draft 08/Public Review Draft 03. 2011 May 31; http://docs.oasis-open.org/opencsa/sca-assembly/sca-assembly-spec-v1.1-csprd03.pdf.
- 85.Hinchey M, Coyle L. Conquering Complexity. Springer; London: 2012. [Google Scholar]
- 86.The Apache Software Foundation Apache Tuscany. [Accessed 28 Dec 2013]; http://tuscany.apache.org/
- 87.Fabric3 Fabric3. [Accessed 28 Dec 2013]; http://www.fabric3.org/
- 88.OW2 Consortium FraSCAti. [Accessed 28 Dec 2913]; https://wiki.ow2.org/frascati/Wiki.jsp?page=FraSCAti.
- 89.Red Hat Inc. [Accessed 28 Dec 2013];SwitchYard. http://www.jboss.org/switchyard.
- 90. [Accessed 31 May 2013];OMG Business process model and notation (BPMN 2.0) http://www.omg.org/spec/BPMN/2.0/
- 91.Chinosi M, Trombetta A. BPMN: An introduction to the standard. Comput Stand Interfaces. 2012;34:124–134. doi: 10.1016/j.csi.2011.06.002. [DOI] [Google Scholar]
- 92.Papazoglou MP, Heuvel W-J. Service oriented architectures: approaches, technologies and research issues. VLDB J. 2007;16:389–415. doi: 10.1007/s00778-007-0044-3. [DOI] [Google Scholar]
- 93.Safy FZ, El-Ramly M, Salah A. Runtime Monitoring of SOA Applications: Importance, Implementations and Challenges. Serv Oriented Syst Eng (SOSE), 2013 IEEE 7th Int Symp; 2013. pp. 315–319. [DOI] [Google Scholar]