Abstract
Rationale
Intensive care unit (ICU) resources are limited in many hospitals. Patients with little likelihood of surviving are often admitted to ICUs. Others who might benefit from ICU are not admitted.
Objective
To provide an updated consensus statement on the principles and recommendations for the triage of patients for ICU beds.
Design
The previous Society of Critical Care Medicine (SCCM) consensus statement was used to develop drafts of general and specific principles and recommendations. Investigators and consultants were sent the statements and responded with their agreement or disagreement.
Setting
The Eldicus project (triage decision making for the elderly in European intensive care units).
Participants
Eldicus investigators, consultants, and experts consisting of intensivists, users of ICU services, ethicists, administrators, and public policy officials.
Interventions
Consensus development was used to grade the statements and recommendations.
Measurements and main results
Consensus was defined as 80 % agreement or more. Consensus was obtained for 54 (87 %) of 62 statements including all (19) general principles, 31 (86 %) of the specific principles, and 10 (71 %) of the recommendations. Inconsistencies in responses were noted for ICU admission and discharge. Despite agreement for guidelines applying to individual patients and an objective triage score, there was no agreement for a survival cutoff for triage, not even for a chance of survival of 0.1 %.
Conclusions
Consensus was reached for most general and specific ICU triage principles and recommendations. Further debate and discussion should help resolve the remaining discrepancies.
Keywords: Consensus statement, Triage, Intensive care unit, Elderly
Introduction
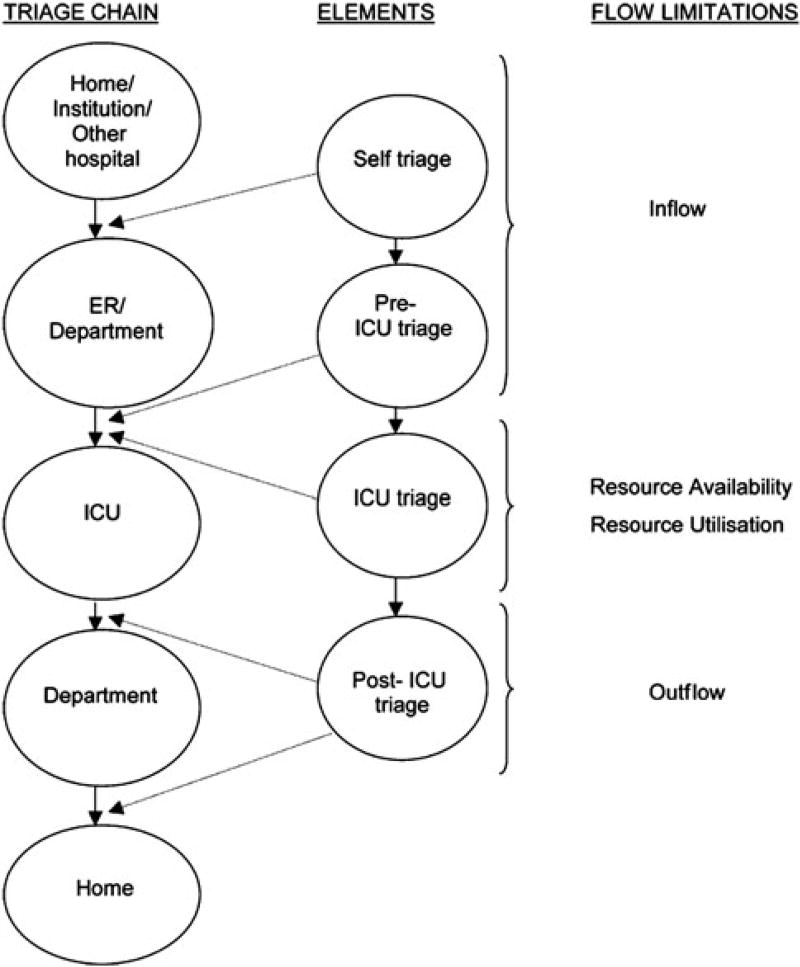
Demand for health care and especially intensive care will most likely continue to exceed supply [1–15]. At the present time there is a large difference in the availability of intensive care unit (ICU) beds around the world. In Europe, ICU bed numbers range from 4.2 beds per 100,000 inhabitants in Portugal to 29.2 beds per 100,000 inhabitants in Germany [16]. These differences likely have an impact on triage and allocation decisions for ICU resources and may contribute to the documented variability in how ICU beds are allocated [7, 17]. Previous consensus statements were published to provide explicit guidelines to help facilitate the fair use of the scarce resource of ICU beds [1, 18]. The Eldicus (triage decision making for the elderly in European intensive care units) study sought to develop an objective ICU triage score and to evaluate ICU benefit in the elderly [19–21]. The Eldicus project also updated the previous Society of Critical Care Medicine (SCCM) consensus recommendations [1] with a specific interest in addressing the elderly. New specific principles and recommendations were added. The present statement provides an update of the principles and recommendations for the distribution of ICU beds for individual patients. It does not address triage for mass casualty events or mass disasters which have been addressed elsewhere [22, 23]. The spectrum of intensive care triage is noted in Fig. 1.
Fig. 1.
The spectrum of intensive care triage. From Levin and Sprung [32]
Methods
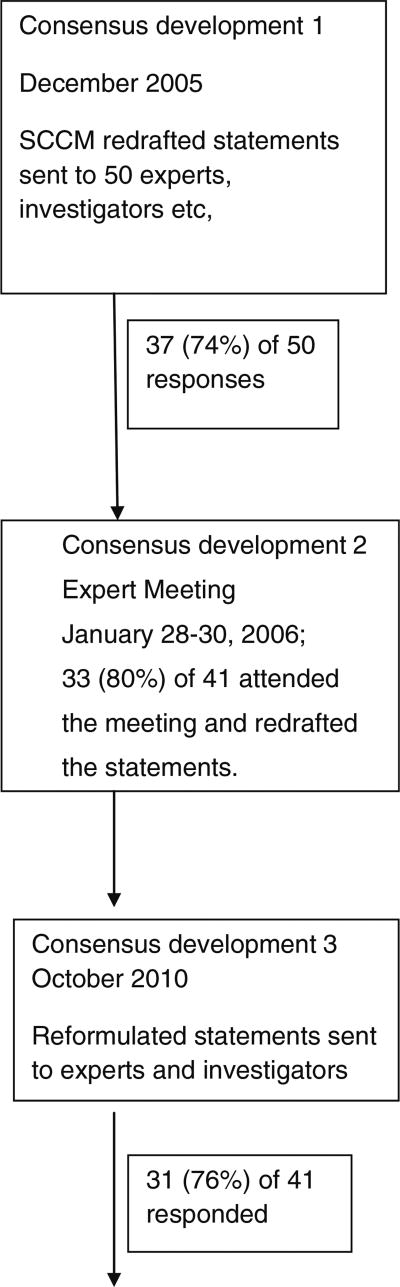
As part of the Eldicus project of the European Society of Intensive Care Medicine’s ethics section and the European Critical Care Research Network, consensus statements on the goals, general policy, and modalities of ICU triage decisions for the elderly were developed. Drafts of general and specific principles and recommendations were developed from the previous SCCM consensus statement [1] by the project coordinator. Although many of the present principles and recommendations relate to both ICUs and intermediate care units, this study primarily focused on the ICU [24]. Consensus development was used to grade the conclusions and recommendations with consensus defined as 80 % agreement or more. An outline of the consensus process and responses are demonstrated in Fig. 2. Fifty Eldicus investigators and consultants (intensivists, users of ICU services, ethicists, administrators, and public policy officials) were sent the conclusions and recommendations and 37 responded with their agreement, disagreement, and suggestions for changes. The project coordinator combined the revisions of the conclusions and recommendations for presentation and voting at an Eldicus expert meeting. A list of the consensus participants is shown in Supplemental Table 1. All participants were sent the revised conclusions and recommendations for them to evaluate prior to the meeting that took place in Estoril, Portugal on 28–30 January 2006. Thirty-three individuals participated in the second consensus round at the meeting. Improvements in the conclusions and recommendations were discussed in order to achieve consensus. The group discussed issues where consensus was not developed, recommended changes that might lead to consensus, and revoted. New statements were developed at the meeting, for which there was time in 6 of 15 for voting. Consensus was developed for 49 statements and recommendations but could not be achieved for 11. As agreed, reformulated statements were sent to the entire group to vote and obtain further consensus a few weeks later. A third consensus vote was completed in October 2010 with 31 responses.
Fig. 2.
The consensus development process
Results
The final consensus scores for triage consensus statements and conclusions are seen in Tables 1, 2, 3. Consensus was obtained for 54 (87 %) of 62 statements. General principles concerning ICU triage had overwhelming agreement with consensus for all 19 principles and 18 of 19 (95 %) principles receiving concurrence of 90 % or more. These principles included demand for ICU services will usually exceed supply; demand will likely increase with an increasing elderly population; explicit guidelines facilitate the fair use of scarce resources, the importance of triage guidelines; the importance of having a clear triage process and justification; the role of physicians as patient advocates; ICU use for patients that benefit and the possibility of occasionally denying certain life-sustaining treatments.
Table 1.
Final consensus scores for triage consensus statements and conclusions: general principles
| Number | Statement | Score (%) |
|---|---|---|
| 1 | Countries around the world face difficult questions regarding access to, delivery of, and payment for health care services, as well as the proportion of health care expenditures that should be appropriated for intensive care | 100 |
| 2 | It is likely that the demand for health care service including intensive care will usually exceed the supply | 100 |
| 3 | It is appropriate to develop explicit guidelines to help facilitate the fairest use of these services | 100 |
| 4 | Principles and guidelines for the distribution of intensive care resources among individual patients are needed | 100 |
| 5 | Demand is partly created by the inclination of critically ill patients and their families to seek and their physicians to provide intensive care | 100 |
| 6 | The advancing age of the population is likely to increase the demand for services as more elderly individuals who are frail, chronically ill, and subject to life-threatening illness become potential candidates for intensive care | 97 |
| 7 | “Triage” is a process in medicine of finding the most appropriate disposition for a patient based on an assessment of the patient’s illness and its urgency | 94 |
| 8 | The process of triage should be based on a sound understanding of the probable outcome of the patient’s illness, the availability of therapeutic modalities, the impact of therapy on outcome, and a judgment of the benefits and burdens of the therapy for the patient, the patient’s family, and society | 97 |
| 9* | Triage of critically ill patients that may limit individual patient and physician choices is justified when (1) the policy is aimed at achieving benefits for individual patients, the health care institution, or society and (2) the policy is announced in advance to notify the public | 94 |
| 10 | Guidelines should be formulated for expected categories of triage and should articulate the principles, justifications, and mechanisms pertaining to each situation as explicitly as possible | 100 |
| 11 | Notwithstanding the pressures exerted on health care providers to limit resource consumption during real or perceived conditions of scarcity, physicians should remain staunch advocates of their patients’ best interests | 94 |
| 12* | Conflicts of interest between the health care provider’s roles as gatekeeper and patient advocate may occur and should be anticipated. Because conflicts of interest cannot be altogether eliminated, attempts should be made to separate the roles of gatekeeper and advocate when possible | 90 |
| 13* | Physicians, nurses, and administrative staff and governmental agencies should collaborate in framing institutional local guidelines and recommendations for the prudent use of scarce resources | 97 |
| 14 | The formulation and promulgation of explicit triage policies should help to minimize the necessity for ad hoc triage decisions in individual cases | 94 |
| 15 | Health care providers, patients, policymakers, and the public at large must recognize that various treatments, including life-prolonging treatments such as intensive care, may be denied | 87 |
| 16 | Health care institutions may justifiably restrict the availability of certain services to use limited resources more effectively or to enhance equity in allocating them | 97 |
| 17 | Critical care units should, in general, be reserved for those patients who have a “reasonable prospect of substantial recovery.” The scope of ICU services should be limited to diagnostic and therapeutic procedures from which a benefit is anticipated | 94 |
| 18 | Each hospital should develop a policy for the accommodation of critically ill patients when all ICU beds capable of being staffed are full | 100 |
| 19* | ICU services of known or generally accepted therapeutic benefit should receive priority over ICU services that are of no proven value or are for experimental purposes | 90 |
Percentages represent the results of the third consensus round with 31 respondents. Recommendations that did not obtain consensus (80 % or greater) during the expert meeting 28–30 January 2006 or subsequently have an asterisk (*) after their number
Table 2.
Final consensus scores for triage consensus statements and conclusions: specific principles
| Number | Statement | Score (%) |
|---|---|---|
| 20 | The foremost consideration in triage decisions is the expected outcome of the patient in terms of survival and function, which in depends turns on the medical status of the patient | 84 |
| 21* | In general, patients with a greater likelihood of benefit have priority over patients unlikely to benefit | 94 |
| 22 | Decisions to be made for all patients should not be made on a first come, first served basis | 100 |
| 23 | Priority for admission to an ICU should correlate with the likelihood that ICU care will benefit the patient substantially more than non-ICU care | 100 |
| 24 | In general, patients with very poor prognoses and little likelihood of benefit should not be admitted to ICUs | 97 |
| 25 | Patients with a very good outcome with or without ICU care also should not be admitted to ICUs | 84 |
| 26* | Factors that should be considered in determining benefit and utility for triage decisions include the following: | |
| (a) | Likelihood of a successful outcome | 100 |
| (b) | Patient’s life expectancy due to disease(s) | 97 |
| (c) | Anticipated quality of life of the patient | 93 |
| (d) | Wishes of the patient and/or surrogate | 93 |
| (e)* | Burdens for those affected, including financial or psychological costs | 71 |
| (f) | Missed opportunities to treat other patients | 94 |
| (g) | Health and other needs of the community | 97 |
| (h)* | Institution’s, moral, and religious values | 32 |
| 27 | All triage decisions made for individual patients on grounds of scarcity must be made explicitly, fairly, and justly | 87 |
| 28 | Triage decisions should not be made in an arbitrary or prejudiced fashion | 93 |
| 29 | Ethnic origin, race, sex, creed, and social worth should never be factors in determining triage decisions | 93 |
| 30 | Age should never be the sole determining factor in triage decisions | 100 |
| 31 | Physiological status is more important than chronological age in triage decisions | 100 |
| 32 | Triage policies should be disclosed in advance to the general public and, when feasible, to patients and surrogates on admission | 94 |
| 33 | Triage decisions may be made without patient or surrogate consent | 100 |
| 34 | Disclosure of triage decisions may help to facilitate communication, understanding, and cooperation among patients, surrogates, and physicians | 100 |
| 35* | Obligations to patients already hospitalized in an ICU who continue to warrant ICU care usually outweigh obligations to accept new patients | 77 |
| 36 | There may be circumstances when it is justified to discharge a patient from the ICU to admit another patient | 100 |
| 37* | If admission of a new patient is likely to adversely affect the outcomes of patients already in the ICU, then that admission is usually justified only if the benefit to the new admission is significant and quite likely and the adverse effects on the present ICU patients are either conjectural or unlikely to be significant | 97 |
| 38 | Criteria for ICU admission, discharge, and exclusion should be explicitly described | 100 |
| 39 | Patients with little or no anticipated benefit from further ICU treatment may be discharged or transferred from the ICU | 93 |
| 40 | Patients with terminal, irreversible illness (excluding potential organ donors) who face imminent death should not be admitted to the ICU | 100 |
| 41 | All individuals who are failing to thrive due to irreversible, chronic illness should not be admitted to the ICU | 100 |
| 42 | The decision to exclude or discharge a patient from the ICU may appropriately be made despite the anticipation of an untoward outcome | 97 |
| 43 | Examples of terminally ill patients (excluding potential organ donors) who may be excluded from the ICU, whether beds are available or not, include those with severe, irreversible brain damage or irreversible multiorgan failure and those with metastatic cancer unresponsive to therapy | 100 |
| 44 | Examples of patients who should be excluded from the ICU, whether beds are available or not, include those who competently decline intensive care, those declared brain dead who are not organ donors, and those in a persistent vegetative or permanently unconscious state | 100 |
| 45 | A patient’s personal behavior should not influence triage decisions if it does not affect the patient’s outcome | 100 |
| 46 | Patients, their surrogates, or others may not compel a physician to provide treatment that the physician believes is not medically indicated | 100 |
| 47 | An objective triage score should be used by physicians to help triage patients to ICU | 100 |
| 48 | An objective triage score should be used by physicians to make triage decisions for individual patients | 71 |
Percentages represent the results of the third consensus round with 31 respondents. Recommendations that did not obtain consensus (80 % or greater) during the expert meeting 28–30 January 2006 or subsequently have an asterisk (*) after their number. New statements not present in the Society of Critical Care Medicine Consensus recommendations [1] included statements 30, 31, 47, and 48
Table 3.
Final consensus scores for triage consensus statements and conclusions: recommendations
| Number | Statement | Score (%) |
|---|---|---|
| 49* | In the setting of constraining conditions, individual providers, institutions, and governmental agencies must use some ethical framework for distributing the resources at hand | 97 |
| 50 | Triage recommendations are intended to be applicable whether or not an immediate shortage is apparent, because their continuous use will lead to more consistently equitable and efficient intensive care | 91 |
| 51 | It is recognized that limiting care of critically ill patients during acute shortages is more likely to result in adverse consequences for individual patients than limiting care during times without shortages | 100 |
| 52 | Triage is an ongoing process—from the decision to come to the hospital, to those regarding referral, admission, or discharge from the ICU | 100 |
| 53 | Medical students, doctors, and other health care professionals should be educated not to discriminate against the elderly in healthcare | 100 |
| 54 | Medical students, doctors, and other health care professionals should be educated about the benefits of intensive care for the elderly | 100 |
| 55 | It may be appropriate to give a patient with little likelihood of benefit from ICU care, a trial of limited duration of ICU care. If ICU care does not significantly improve the patient’s condition after the agreed time, the patient should be discharged from the ICU and/or therapies limited | 94 |
| 56 | ICUs must provide the proper facility, equipment, and trained personnel (intensivists and nurses) to care for critically ill patients. Areas that do not have the proper facilities, equipment, or trained personnel should not be called ICUs | 94 |
| 57 | Intensivists, institutions, and/or governmental agencies have the responsibility to find an appropriate ICU facility if the existing ICU areas cannot accept a critically ill patient requiring ICU care | 87 |
| 58 | Patients with a 1 % or less chance of survival should not be admitted to the ICU | 48 |
| 59 | Patients with a 0.2 % (1 in 500) or less chance of survival should not be admitted to the ICU | 65 |
| 60 | Patients with a 0.1 % (1 in 1,000) or less chance of survival should not be admitted to the ICU | 77 |
| 61 | Patients hospitalized in ICUs with little likelihood of further benefit should be discharged from the ICU | 77 |
| 62 | Quality assurance programs that decrease iatrogenic illness may allow for more ICU bed availability | 100 |
Percentages represent the results of the third consensus round with 31 respondents. Recommendations that did not obtain consensus (80 % or greater) during the expert meeting 28–30 January 2006 or subsequently have an asterisk (*) after their number. New statements not present in the Society of Critical Care Medicine Consensus recommendations [1] included statements 49–62
There was also consensus for specific ICU principles in 31 of 36 (86 %) statements with greater than 90 % agreement for 28 of the 36 (78 %) statements. These principles incorporated priority for patients with greater benefit (when admitted versus refused ICU admission); factors to be considered for determining benefit including likelihood of a successful outcome, the patient’s life expectancy, quality of life and values; triage decisions not to be based on a first come, first served (FCFS) basis; rejection of patients with little likelihood of ICU benefit either because of a very good or a very bad prognosis; ICU admission, discharge, and exclusion criteria should be explicit, fair, and disclosed in advance; decisions should not be based on ethnicity, race, sex, social worth, or solely on age; the importance of physiological not chronologic age; necessity for some decisions without patient or surrogate consent; the exclusion or discharge of patients despite the possibility of an untoward outcome and exclusion of imminently terminally ill patients.
Consensus was obtained for 10 of 14 (71 %) recommendations [>90 % for 9 of 14 (64 %)]. Recommendations contained the endorsement of the following: use of an ethical framework to distribute scarce resources; use of triage recommendations even without an immediate shortage; avoidance of discrimination against the elderly in health care; educating professionals about ICU benefits for the elderly; use of ICU trials for patients with little likelihood of benefit; avoidance of labeling as an ICU area without proper ICU facilities, equipment, and trained personnel; and searching for appropriate alternative ICU facilities for patients if existing ICUs cannot accept a critically ill patient requiring ICU care.
Experts could not agree on a cutoff for not admitting a patient to the ICU with little likelihood of survival. Only 77 % (24/31) of respondents agreed to exclude patients with a 0.1 % (1 in 1,000) or less chance of survival.
Discussion
Updated consensus was reached for most general and specific ICU triage principles and recommendations. There was consensus for the following: demand for ICU services will usually exceed supply; demand will likely increase; the importance of explicit, fair, and disclosed triage guidelines; priority for patients with greater benefit; deciding not on an FCFS basis; rejecting or discharging patients with little likelihood of benefit; and the importance of physiological, not chronologic age.
Despite agreement for many issues, there were several inconsistencies in responses related to fundamental areas of triage including criteria for admission and discharge. As ICU triage is such an important subject in intensive care medicine which frequently determines who will live and die [2–6, 8, 10, 19–21], an evaluation of the disparity of responses provides important insights into the ethical decision making triage problems of practicing physicians. Discrepancies included:
Admission—despite the fact that 100 % of respondents agreed with the need for guidelines that would apply to individual patients (statement 4) and an objective triage score (statement 47), only 71 % were in favor of using objective triage scores for individual patients (statement 48) and there was no agreement for a survival cutoff for triage, not even for a chance of survival as low as 0.1 % (statement 60).
Admission—although 100 % of respondents agreed that triage decisions should not be made on an FCFS basis (statement 22), 77 % agreed that patients already in the ICU (who came first) have priority over new patients (statement 35).
Discharge—despite the fact that 93 % agreed that patients with little benefit from further ICU treatment ‘may’ be discharged from the ICU (statement 39), only 77 % agreed that such patients ‘should’ be discharged (statement 61).
There are several explanations for the discrepancies. First, individuals appear willing to make broad generalizations about difficult ethical issues such as triage. When, however, they must make specific decisions, especially about individual patients, they are less willing to do so. Respondents want explicit guidelines, yet they are unwilling to accept concrete proposals for what these guidelines should be. This may be related to medical uncertainty. Prognostication for ICU patients is imprecise, at best [25]. Physicians may not believe that they can meaningfully discriminate between patients with very low chances of survival (e.g., 1 vs. 0.1 %) and hence would be reluctant to accept specific cutoffs that would be difficult for them to enforce. Perhaps because of this respondents (94 %) were willing to give a patient with little likelihood of ICU benefit a limited trial of ICU care with subsequent discharge if the patient does not improve (statement 55). Alternatively, participants may have thought that clinicians should have some established guidelines in making triage decisions to avoid making idiosyncratic, unfair decisions but they do not agree about the likelihood of benefit below which treatment should not be offered.
Second, allocation decisions always involve a balance between considerations of equity and efficiency [26]. Equity considerations address how to treat people fairly, whereas efficiency considerations seek to optimize medical outcomes. Respondents had divergent and inconsistent views about balancing these two considerations. FCFS is a popular tool for resource allocation, because if we assume that the order in which people become ill is randomly distributed, FCFS gives every person an equal chance of ICU admission. Unfortunately, FCFS ignores efficiency considerations, such as the likelihood that the patient will benefit from ICU admission. Given that there was 100 % agreement that FCFS should not be used for allocation of ICU beds, one would have predicted that the respondents would discharge a patient with little chance of survival in favor of admitting a patient with a greater chance of survival. We found, however, that 77 % actually gave priority to patients already in the ICU which is inconsistent with their views about FCFS. These inconsistencies suggest that intensivists reject views based solely upon equity (FCFS) or efficiency (maximize benefits) and instead gravitate towards a more moderate position that incorporates elements of both [9]. Respondents may also believe there are differences between triaging prospective versus existing ICU patients. Respondents had greater difficulties discharging patients and therefore prioritized efficiency over equity for the patients not already in the ICU.
Now that these discrepancies have been more clearly described, further debate and discussion may help resolve them. Fair guidelines could be developed by having communities conduct deliberative procedures for deciding what probability of benefit is low enough to forgo treatment. Participants in a priority setting exercise in the USA were able to understand the need for priority setting and were willing to trade off intensive care for the sake of other services and would accept a threshold probability of survival at which they would want intensive care [27]. On the other hand, it may be that some of these differences are deeply rooted in cultural views and traditions, in which case it is valuable to identify these areas of possible intractable disagreement.
The present revised recommendations continue to emphasize the patient’s medical status and the priority to patients with a greater likelihood to benefit. Such an approach has solid grounding in a consequentialist approach to distributive justice. Whether such an approach is compatible with other views of distributive justice is more a matter of contention. Baker and Strosberg [28] argued that a triage scheme that prioritizes those individuals who are most likely to benefit has some egalitarian justification. The diminished endorsement of obligations to patients already hospitalized in the current consensus compared to the SCCM consensus may also be a function of new developments and understanding of the importance of triage. Recent experiences with pandemics, as well as efforts to plan for them, have made intensivists aware that they must be prepared to perform reverse triage—moving many patients who are already under their care to other facilities so that they can take care of newly and acutely ill patients [22, 23].
Although respondents did not, on balance, entirely reject FCFS, 100 % did agree with the equity concern that age should never be the sole determining factor in triage decisions, similar to strongly held views about the impermissibility of discriminating on the basis of race or gender. New statements related to the elderly obtained unanimous agreement. These included that “age should never be the sole determining factor in triage decisions”, “physiological status is more important than chronological age in triage decisions”, and medical students, doctors, and other healthcare professionals should be educated not to discriminate against the elderly in health care and be educated about the benefits of intensive care for the elderly. Whether discrimination on the basis of age should be prohibited as it is for race and gender is a matter of debate. While each person has only one race or gender identity that does not vary over time, each person has the potential to experience all phases of life shifting from young to old age. If we believe that everyone should have a fair chance to experience a complete life (the so-called fair innings argument), then everyone should agree that preference for life-saving treatments should be given to the young, because they have not yet had a chance to experience phases of life that have already been enjoyed by the old. Although this survey shows strong consensus against the fair innings approach with regard to ICU resources, others have argued for the fair innings approach, as ethically acceptable and not discriminatory to treat the elderly differently than the young [29–31].
New recommendations included that triage recommendations should be used even when “shortage is not present to have more equitable and efficient ICU care” and that triage is an ongoing process that begins when the patient presents for medical treatment and ends at hospital discharge, with decisions about ICU care made throughout the continuum [32]. As many patients with poor prognoses are typically not admitted to the ICU, a trial of ICU care even for patients with little likelihood of benefit may be appropriate [33].
Many enhanced hospital facilities which do not contain the appropriate equipment or trained personnel to care for critically ill patients are sometimes labeled “ICUs”. These areas should not be called ICUs as it gives false hope to patients, their families, and third party payers.
New biological, technological, and prognostication breakthroughs may improve diagnostic and therapeutic possibilities thus changing the prognosis of critically ill patients and influencing triage decisions. Such advances could also change the capabilities of intermediate ICUs and their use in the triage process.
Strengths of the present study include the fact that internationally recognized experts in intensive care, users of ICU services, ethicists, administrators, and public policy officials participated in the project, that a triage update was performed, and that consensus was obtained for the majority of principles despite the diverse cultures of the participants. Weaknesses include the voting on previously developed principles and recommendations rather than a normative approach that could be explicitly designed to develop internally consistent principles, the consensus development approach which led to some internally inconsistent responses, three experts with an interest in the elderly taking part in the voting, and the long delay until the third consensus vote. Although the present participants were primarily European (90 %) compared to the original SCCM group (6 %), the results may not be representative of all of Europe.
In summary, updated consensus was reached for ICU triage principles and recommendations. Although agreement was obtained for most issues, inconsistencies were found in balancing equity and efficiency. Further debate and agreement will be required to move from ICU admission and discharge generalities to specific patient decisions.
Supplementary Material
Acknowledgments
Supported by the European Commission contract QLK6-CT-2002-00251, the European Society of Intensive Care Medicine and the European Critical Care Research Network, The Israel National Institute for Health Policy and Health Services Research grant number 1998/11/G and by Red GIRA G03/063. The EU Commission and other sponsors had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript. All authors participated in the design of the study, helped in the analysis of the data, and collaborated in drafting and revising the manuscript. As this is a study of triage and ethical issues, the authors’ have no financial or personal relationships or affiliations that could influence (or bias) their decisions, work, or manuscript.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-013-3033-6) contains supplementary material, which is available to authorized users.
Contributor Information
Charles L. Sprung, General Intensive Care Unit, Department of Anesthesiology and Critical Care Medicine, Hadassah Hebrew University Medical Center, P.O. Box 12000, Jerusalem 91120, Israel, sprung@cc.huji.ac.il, Tel.: +972-2-6778060, Fax: +972-2-5671413
Marion Danis, Section on Ethics and Health Policy, National Institutes of Health, Bethesda, MD, USA.
Gaetano Iapichino, San Paolo Hospital, Università degli Studi Milan, Milan, Italy.
Antonio Artigas, Critical Care Center, Sabadell Hospital, CIBER Enfermedades Respiratorias, Parc Tauli University Institute, Autonomous University of Barcelona, Sabadell, Spain.
Jozef Kesecioglu, Department of Intensive Care Medicine, University Medical Center Utrecht, Utrecht, Netherlands.
Rui Moreno, Unidade de Cuidados Intensivos Neurocríticos, Hospital de São José, Centro Hospitalar de Lisboa Central, E.P.E., Lisbon, Portugal.
Anne Lippert, Herlev University Hospital, Copenhagen, Denmark.
J. Randall Curtis, Division of Pulmonary and Critical Care Medicine, Harborview Medical Center, Seattle, WA, USA.
Paula Meale, Division of Surgery and Interventional Science, University College London, London, UK.
Simon L. Cohen, Department of Intensive Care Medicine, University College London, London, UK
Mitchell M. Levy, Division of Pulmonary and Critical Care Medicine, Rhode Island Hospital, The Warren Alpert Medical School of Brown University, Providence, RI, USA
Robert D. Truog, Divisions of Medical Ethics, Anaesthesiology and Pediatrics, Children’s Hospital, Harvard Medical School, Boston, MA, USA
References
- 1.Society of Critical Care Medicine. Ethics Committee. Consensus statement on the triage of critically ill patients. JAMA. 1994;271:1200–1203. [PubMed] [Google Scholar]
- 2.Metcalfe MA, Sloggett A, McPherson K. Mortality among appropriately referred patients refused admission to intensive care units. Lancet. 1997;350:7–11. doi: 10.1016/S0140-6736(96)10018-0. [DOI] [PubMed] [Google Scholar]
- 3.Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, Nimrod A, Oppenheim A, Epstein L, Cotev S. Evaluation of triage decisions for intensive care admission. Crit Care Med. 1999;27:1073–1079. doi: 10.1097/00003246-199906000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Joynt GM, Gomersall CD, Tan P, Lee A, Cheng CA, Wong EL. Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome. Intensive Care Med. 2001;27:1459–1465. doi: 10.1007/s001340101041. [DOI] [PubMed] [Google Scholar]
- 5.Simchen E, Sprung CL, Galai N, Zitser-Gurevich Y, Bar-Lavi Y, Gurman G, Klein M, Lev A, Levi L, Zveibil F, Mandel M, Mnatzaganian G. Survival of critically ill patients hospitalized in and out of intensive care units under paucity of intensive care unit beds. Crit Care Med. 2004;32:1654–1661. doi: 10.1097/01.ccm.0000133021.22188.35. [DOI] [PubMed] [Google Scholar]
- 6.Garrouste-Orgeas M, Montuclard L, Timsit JF, Reignier J, Desmettre T, Karoubi P, Moreau D, Montesino L, Duguet A, Boussat S, Ede C, Monseau Y, Paule T, Misset B, Carlet J French ADMISSIONREA Study Group. Predictors of intensive care unit refusal in French intensive care units: a multiple-center study. Crit Care Med. 2005;33:750–755. doi: 10.1097/01.ccm.0000157752.26180.f1. [DOI] [PubMed] [Google Scholar]
- 7.Hurst SA, Slowther AM, Forde R, et al. Prevalence and determinants of physician bedside rationing: data from Europe. J Gen Int Med. 2006;21:1138–1143. doi: 10.1111/j.1525-1497.2006.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simchen E, Sprung CL, Galai N, Zitser-Gurevich Y, Bar-Lavi Y, Levi L, Zveibil F, Mandel M, Mnatzaganian G, Goldschmidt N, Ekka-Zohar A, Weiss-Salz I. Survival of critically ill patients hospitalized in and out of intensive care. Crit Care Med. 2007;35:449–457. doi: 10.1097/01.CCM.0000253407.89594.15. [DOI] [PubMed] [Google Scholar]
- 9.Hope T, McMillan J, Hill E. Intensive care triage: priority should be independent of whether patients are already receiving intensive care. Bioethics. 2012;26:259–266. doi: 10.1111/j.1467-8519.2010.01852.x. [DOI] [PubMed] [Google Scholar]
- 10.Reignier JRR, Tournoux-Facon C, Boulain T, Lesieur O, et al. Refusal of intensive care unit admission due to a full unit: impact on mortality. Am J Respir Crit Care Med. 2012;185:1081–1087. doi: 10.1164/rccm.201104-0729OC. [DOI] [PubMed] [Google Scholar]
- 11.Akkaoui M, Abidi K, Louriz M, et al. Determinants and outcomes associated with decisions to deny or to delay intensive care unit admission in Morocco. Intensive Care Med. 2012;38:830–837. doi: 10.1007/s00134-012-2517-0. [DOI] [PubMed] [Google Scholar]
- 12.Mery E, Kahn JM. Does space make waste? The influence of ICU bed capacity on admission decisions. Crit Care. 2013;17:315. doi: 10.1186/cc12688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sinuff T, Kahnamoui K, Cook DJ, Luce JM, Levy MM For the Values Ethics and Rationing in Critical Care (VERICC) Task Force. Rationing critical care beds: a systematic review. Crit Care Med. 2004;32:1588–1597. doi: 10.1097/01.ccm.0000130175.38521.9f. [DOI] [PubMed] [Google Scholar]
- 14.Strech D, Synofzik M, Marckmann G. How physicians allocate scarce resources at the bedside: a systematic review of qualitative studies. J Med Phil. 2008;33:80–99. doi: 10.1093/jmp/jhm007. [DOI] [PubMed] [Google Scholar]
- 15.Azoulay E, Pochard F, Chevret S, Vinsonneau C, Garrouste M, Cohen Y, Thuong M, Paugam C, Apperre C, De Cagny B, Brun F, Bornstain C, Parrot A, Thamion F, Lacherade JC, Bouffard Y, Le Gall JR, Herve C, Grassin M, Zittoun R, Schlemmer B, Dhainaut JF For the PROTOCETIC Group. Compliance with triage to intensive care recommendations. Crit Care Med. 2001;29:2132–2136. doi: 10.1097/00003246-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 17.Cooper AB, Sibbald R, Scales DC, Rozmovits L, Sinuff T. Scarcity: the context of rationing in an Ontario ICU. Crit Care Med. 2013;41:1476–1482. doi: 10.1097/CCM.0b013e31827cab6a. [DOI] [PubMed] [Google Scholar]
- 18.American Thoracic Society Bioethics Task Force. Fair allocation of intensive care unit resources. Am J Respir Crit Care Med. 1997;156:1282–1301. doi: 10.1164/ajrccm.156.4.ats7-97. [DOI] [PubMed] [Google Scholar]
- 19.Iapichino G, Corbella D, Minelli C, Mills G, Artigas A, Edbooke D, Pezzi A, Kesecioglu J, Patroniti N, Baras M, Sprung CL. Reasons for refusal of admission to intensive care and impact on mortality. Intensive Care Med. 2010;36:1772–1779. doi: 10.1007/s00134-010-1933-2. [DOI] [PubMed] [Google Scholar]
- 20.Sprung CL, Baras M, Iapichino G, Kesecioglu J, Lippert A, Hargreaves C, Pezzi A, Pirrachio R, Edbrooke DL, Pesenti A, Bakker J, Gurman G, Cohen SL, Wiis J, Payen D, Artigas A. The Eldicus prospective, observational study of triage decision making in European intensive care units: part I—European intensive care admission triage score (EICATS) Crit Care Med. 2012;40:125–131. doi: 10.1097/CCM.0b013e31822e5692. [DOI] [PubMed] [Google Scholar]
- 21.Sprung CL, Artigas A, Kesecioglu J, Pezzi A, Wiis J, Pirrachio R, Baras M, Edbrooke DL, Pesenti A, Bakker J, Hargreaves C, Gurman G, Cohen SL, Lippert A, Payen D, Corbella D, Iapichino G. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: intensive care benefit for the elderly. Crit Care Med. 2012;40:132–138. doi: 10.1097/CCM.0b013e318232d6b0. [DOI] [PubMed] [Google Scholar]
- 22.Christian MD, Joynt GM, Colvn J, Hick JL, Danis M, Sprung CL. Critical care triage. In: Sprung CL, Cohen R, Adini B, editors. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. Vol. 36. 2010. pp. S55–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Satterthwaite PS, Atkinson CJ. Using ‘reverse triage’ to create hospital surge capacity: Royal Darwin Hospital’s response to the Ashmore Reef disaster. Emerg Med J. 2012;29:160–162. doi: 10.1136/emj.2010.098087. [DOI] [PubMed] [Google Scholar]
- 24.Valentin A, Ferdinande P ESICM Working Group on Quality Improvement. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011;37:1575–1587. doi: 10.1007/s00134-011-2300-7. [DOI] [PubMed] [Google Scholar]
- 25.Knaus WA, Wagner DP, Lynn J. Short-term mortality predictions for critically ill hospitalized adults: science and ethics. Science. 1991;254:389–394. doi: 10.1126/science.1925596. [DOI] [PubMed] [Google Scholar]
- 26.Truog RD. Triage in the ICU. Hast Cent Rep. 1992;22:13–17. [PubMed] [Google Scholar]
- 27.Danis M, Biddle AK, Goold SD. Enrollees choose priorities for Medicare. Gerontologist. 2004;44:58–67. doi: 10.1093/geront/44.1.58. [DOI] [PubMed] [Google Scholar]
- 28.Baker R, Strosberg M. Triage and equality: an historical reassessment of utilitarian analyses of triage. Kennedy Inst Ethics J. 1992;2:103–123. doi: 10.1353/ken.0.0035. [DOI] [PubMed] [Google Scholar]
- 29.Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373:423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 30.Callahan D. Medical goals in an aging society. Simon and Schuster; New York: 1987. Setting limits. [PubMed] [Google Scholar]
- 31.Daniels N. Justice between age groups: am I my parents’ keeper? Milbank Mem Fund Q Health Soc. 1983;61:489–522. [PubMed] [Google Scholar]
- 32.Levin PD, Sprung CL. The process of intensive care triage. Intensive Care Med. 2001;27:1441–1445. doi: 10.1007/s001340101042. [DOI] [PubMed] [Google Scholar]
- 33.Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E. The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med. 2007;35:808–814. doi: 10.1097/01.CCM.0000256846.27192.7A. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.