Abstract
Objective
Each year in the United States 1.5–2.5 million individuals are so severely injured that they require hospitalization. Multiple psychiatric, substance use, and chronic medical disorders are endemic among injury survivors with and without traumatic brain injury, yet few investigations have assessed the association between the cumulative burden of these conditions and healthcare outcomes. The investigation aimed to assess the associations between comorbid psychiatric disorders, alcohol and drug use disorders, medical disorders, traumatic brain injury, and violent and suicide related index injury hospitalizations, and subsequent post-injury outcomes that included recurrent hospitalization and death.
Method
Recurrent hospitalization and all-cause mortality were examined in this population-based retrospective cohort study. A total of 76,942 patients hospitalized in Washington State during 2006–2007 were followed for five years. ICD-9-CM codes were used to identify conditions prior to or at the index admission; E-Codes were used to identify firearm, assaultive violence, and suicide/overdose index injury hospitalization mechanisms.
Results
Adjusted regression analyses demonstrated a significant, “dose-response” relationship between an increasing cumulative burden of disorders and an increasing risk of recurrent hospitalization (≥ 4 conditions, Relative Risk =3.89, 95% Confidence Interval (CI) =3.66–4.14). Adjusted Cox proportional hazard regression demonstrated a similar relationship between increasing cumulative burden of disorders and all-cause mortality (≥ 4 conditions, Hazard Ratio =5.33, 95% CI =4.71–6.04).
Conclusions
Increasing cumulative burden of disorders was associated with greater post-injury risk of recurrent hospitalization and death. Orchestrated investigative and policy efforts could introduce screening and intervention procedures that target this spectrum of comorbidity.
INTRODUCTION
Injury constitutes a major public health problem for United States (US) civilian and veteran patient populations (1). Each year, approximately 30 million Americans are seen in emergency departments after injury and approximately 1.5–2.5 million patients require hospitalization (2). Injury is a leading cause of death for individuals under the age of 45 and accounts for 12% of medical expenditures in the US (2). Globally, injury accounts for approximately 16% of the world’s burden of disease (3, 4).
Initial studies in trauma-exposed veteran patients have documented an association between increasing cumulative burden of disorders and poorer health outcomes including increased health service use and mortality (5–7). These investigations have identified a comorbidity cluster that includes traumatic brain injury, psychiatric and substance use disorders, suicidality, and chronic medical disorders.
Prior studies suggest that acutely injured civilian trauma survivors may carry a substantial burden of psychiatric, substance use, and medical disorders, as well as injury related comorbidities. A series of US prospective cohort investigations suggest that between 20–40% of physically injured trauma survivors may go on to develop symptoms consistent with posttraumatic stress disorder (PTSD) and/or depression after hospitalization for injury (8, 9). Posttraumatic stress and depressive symptom levels appear to contribute to poorer post-injury outcomes (10). Substance use disorders are also endemic among hospitalized trauma survivors (11). A series of other investigations suggest that suicide attempts and violence, including firearm related and other assaultive injuries, frequently occur in patients presenting to US acute care medical emergency department and trauma center settings (12, 13). Patients who incur traumatic brain injury may be particularly vulnerable to recurrent violent trauma, suicidal ideation, and death (14). Initial studies suggest that pre-existing chronic medical disorders may also occur frequently among hospitalized injury trauma survivors (15).
Approximately 30 years ago, a single small-scale investigation documented an increased risk of mortality among civilian injury survivors in Detroit, suggesting that traumatic injury and its sequelae could be considered a “chronic recurrent disease” (16). The reasons that injury may be recurrent are complex and likely influenced by the constellation of comorbid psychiatric, substance abuse, and medical conditions, as well as lifestyle behaviors reflected in the mechanism of the index injury, such as assault or other violence related causes (5, 6, 17–19). However, few population-based investigations have assessed the association between the full spectrum of psychiatric, substance use, and medical disorders and the risk for poor health outcomes.
The current population-based retrospective cohort study first aimed to examine the frequencies of a comorbidity constellation that included psychiatric disorders, alcohol and drug use disorders, and chronic medical disorders, as well as violent, suicidal, and traumatic brain injury related hospitalizations among injury survivors. The investigation also aimed to assess the associations between these comorbidities present at the time of an index injury hospitalization and subsequent post-injury outcomes that included recurrent hospitalization and death. The investigation hypothesized that a greater cumulative burden of disorders would be associated with an increased risk of recurrent hospitalizations and all-cause mortality.
METHODS
Design, Setting and Participants
The investigation was a population-based retrospective cohort study of all Washington State residents hospitalized for injury admission during the index period of 2006–2007. All study procedures were approved by the Washington State Institutional Review Board; approval included a waiver of patient informed consent for this secondary analysis of de-identified data. Injured patients included in the cohort were identified through the Washington State Comprehensive Abstract Reporting System (CHARS) that aggregates all hospital inpatient and discharge information for the population of Washington State.
The independent variables for the study included psychiatric disorders, alcohol and drug use disorders and medical disorders present at the time of the index injury hospitalization. Additional independent variables examined included an index injury admission associated with a violent or suicide injury event and an index injury event associated with a traumatic brain injury. The study outcomes/dependent variables were any re-hospitalization or death occurring after the index injury admission. The specific methods used to identify independent and dependent variables as well as study covariates are described below.
Psychiatric, Alcohol and Drug Use, and Medical Disorders
Psychiatric and alcohol and drug use disorders were identified by review of International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes contained within the medical record for the index admission and any other Washington State hospital admissions in the five years prior to the index injury (Appendix 1). Medical disorders were also derived from CHARS ICD-9-CM codes; definitions and ICD-9-CM codes for each of these conditions are shown in Appendix 1.
Injury Type and Severity
All inpatient hospital records for the index admission were reviewed for ICD-9-CM codes indicative of traumatic injury (Appendix 1). Severity of injury by body region, including traumatic brain injury, was coded using the Abbreviated Injury Scale in order to determine the Maximum Abbreviated Injury Scale injury score and Injury Severity Score (20). Firearm, assaultive violence, suicide, and other overdose related index hospital admissions were identified through injury E-codes recorded in the CHARS database.
Covariates
The Washington State CHARS database contains information on patient age, sex, insurance payor status, the county of hospitalization, and the year/season of discharge. These variables were used as covariates in adjusted regression models. Race is not a variable included in the CHARS database.
Outcome Assessments
Hospital records for the cohort were reviewed for the five years before and after the index 2006–2007 admission; the first hospitalization occurring for each individual during 2006–2007 was identified as the index admission. The cohort was followed up until December 31, 2011 to identify recurrent hospitalization or death. Record linkage between CHARS and Washington State death records allowed for the assessment of both recurrent hospitalization and all-cause mortality outcomes. Probabilistic algorithms were used to link patient index hospitalization records with prior and subsequent hospitalization and death records data (21). The first two letters of the patient’s first name, the first two letters of the last name, date of birth, sex, and the first three digits of the zip code of residence were used as a subsequent set of identifiers to perform the linkage. The final database used for analyses was restricted to matches with an accuracy likelihood of at least 99% (21).
Statistical Analyses
The study first described the demographic, clinical, and injury characteristics of the cohort. Next, the medical record-documented frequencies of all independent variables were assessed. Frequencies of psychiatric disorders, alcohol and drug use disorders, chronic medical disorders, and traumatic brain injury diagnoses were ascertained for the index hospitalization and for all hospitalizations in the five years prior; patterns of comorbidity were also examined. The medical record-documented frequencies of firearm, assaultive violence, suicide, and overdose related admissions were assessed for the index hospitalization.
The main study hypothesis was that an increasing cumulative burden of disorders would be associated with an increased risk of recurrent hospitalization and all-cause mortality over the course of the five years after the index injury admission. A cumulative burden index was created that relied upon yes/no counts of discrete disorders. Conditions considered for the cumulative burden index were: one or more psychiatric disorders, one or more alcohol related disorders, one or more drug use disorders, one or more chronic medical disorders, traumatic brain injury, and an index hospitalization involving firearm or assaultive violence, suicide, or overdose. All disorders except traumatic brain injury demonstrated a significant association with poorer outcomes and were included in the index.
The study next examined the pattern of recurrent hospitalization and all-cause mortality over the course of the five years post-injury. Each disorder’s association to five year post-injury recurrent hospitalization and all-cause mortality outcomes were ascertained, adjusting for a single covariate: patient age.
Regression models were constructed to assess the adjusted associations between an increasing number of disorders and the health outcomes of recurrent hospitalization and all-cause mortality. Age, gender, payor status, injury severity, discharge year/season, and county were adjusted for in all regression models. Generalized estimation equation models (22) with the negative binomial link were used to assess the adjusted association between the cumulative burden of disorders and recurrent injury hospitalization outcomes; the dependent variable for these models was an annually repeated measurement of the number of recurrent hospitalizations over the five year post-injury period. Cox proportional hazard models were used to assess the associations between cumulative disorder burden and all-cause mortality while adjusting for age, gender, payor status, injury severity, discharge year/season, and county.
Sensitivity analyses assessed the impact of including 0, 1, and ≥2 disorders for each disorder (rather than dichotomized yes/no variables) on the pattern and strength of the observed associations with recurrent hospitalization and mortality outcomes. Sensitivity analyses also assessed the robustness of the observed associations between cumulative burden of disorders and increased risk of poorer outcome by adjusting for the impact of including any history of hospitalization before the index injury admission. In order to assess the impact of re-hospitalizations possibly related to the initial injury admission, sensitivity analyses assessed the impact of including readmissions that occurred 30, 90, and 180 days after the initial index admission on the pattern and strength of observed associations with outcomes (21, 23). Analyses were conducted using the SAS (Version 9.4, Cary, NC: SAS Institute; 2013) and STATA (STATA Version 13, College Station, TX: Stata Corp LP; 2013) software packages.
RESULTS
In the index period, there were 76,942 patients with an injury admission (Table 1). Approximately 79% of injured patients had one or more comorbid disorders (Table 2). Approximately 29% of participants had one or more psychiatric disorders (Table 2). Depression was the most frequently diagnosed psychiatric disorder (14.3%), followed by dementia (8.4%). The frequency of all other psychiatric disorders, including anxiety disorders (3.9%) and PTSD (2.4%), was less than 5% in the cohort. Twenty-five percent of patients were diagnosed with alcohol abuse/dependence, 2.0% with marijuana abuse/dependence, 3.7% with stimulant abuse/dependence, and 2.6% with opiate abuse/dependence. Sixty-two percent of patients had one or more chronic medical disorders. The most frequently diagnosed medical disorder was hypertension (33.7%), followed by ischemic heart disease (24.1%), pain related disorders (21.9%), pulmonary disorders (16.4%), diabetes (14.2%), cerebrovascular disease (7.2%), renal (5.6%), and liver disorders (5.1%). All other disorders were diagnosed in less than 5% of hospitalized injury survivors.
TABLE 1.
Patient demographic, injury, and clinical characteristics, Washington State, 2006–2007 (N = 76,942)
| Characteristic | N | %a |
|---|---|---|
| Demographic | ||
| Female | 38,390 | 49.9 |
| Insurance | ||
| Self-pay | 6,158 | 8.0 |
| Public | 42,628 | 55.4 |
| Private | 28,156 | 36.6 |
| Injury admission | ||
| Injury severity category | ||
| 0–8 | 44,808 | 58.2 |
| 9–15 | 17,473 | 22.7 |
| ≥ 16 | 6,711 | 8.7 |
| Missing | 7,950 | 10.3 |
| Traumatic brain injury | ||
| None | 69,293 | 90.1 |
| Mild | 2,011 | 2.6 |
| Moderate | 1,482 | 1.9 |
| Severe | 4,156 | 5.4 |
| Injury type | ||
| Gunshot/assault | 3,206 | 4.2 |
| Suicide/overdose | 10,686 | 13.9 |
| Unintentional/undetermined | 63,050 | 81.9 |
| Prior hospitalizations | 27,781 | 36.1 |
| Age (M±SD)b | 25.8±54.5 |
Percentages may not total 100 due to rounding
M, mean; SD, standard deviation
TABLE 2.
Association between alcohol, drug, psychiatric, injury, and medical comorbidity and recurrent hospitalization and all-cause mortality outcomes, adjusted for age, Washington State, 2006–2007
| Patients | Outcomesa | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Re-hospitalization | Mortality | |||||
|
|
||||||
| Conditions | N | % | RR | CI | HR | CI |
| Alcohol disorders | 19,167 | 24.9 | 1.47 | 1.41–1.52 | 1.57 | 1.49–1.67 |
| Drug disorders | 16,387 | 21.3 | 1.59 | 1.53–1.66 | 1.61 | 1.52–1.70 |
| Psychiatric disorders | 22,062 | 28.7 | 1.60 | 1.55–1.66 | 1.53 | 1.48–1.59 |
| Chronic medical disorders (yes/no) | 47,365 | 61.6 | 2.70 | 2.59–2.82 | 2.14 | 2.00–2.30 |
| Violent or suicide hospitalization | 13,892 | 18.1 | 1.64 | 1.57–1.71 | 1.42 | 1.32–1.54 |
| Traumatic brain injury (yes/no) | 7,649 | 9.9 | 0.81 | 0.77–0.86 | 0.87 | 0.82–0.94 |
| Cumulative disorder burdenb | ||||||
| 0 (Ref) | 16,322 | 21.2 | ||||
| 1 | 26,712 | 34.7 | 2.13 | 2.02–2.24 | 2.56 | 2.30–2.86 |
| 2 | 18,262 | 23.7 | 2.31 | 2.18–2.43 | 3.57 | 3.20–3.98 |
| 3 | 8,800 | 11.4 | 3.18 | 3.00–3.38 | 4.08 | 3.62–4.59 |
| ≥4 | 6,846 | 8.9 | 4.21 | 3.96–4.47 | 5.64 | 4.99–6.38 |
RR, relative risk; CI, confidence interval; HR, hazard ratio
Cumulative disorders: alcohol, drug, psychiatric, medical, violent/suicide hospitalization
Psychiatric and substance use disorders frequently occurred as comorbid conditions. For example, 99% of patients with a drug use diagnosis (16,198/16,387) had one or more comorbid psychiatric, alcohol, or chronic medical disorders or traumatic brain injury. Similarly, 95% of patients with an alcohol use diagnosis (18,173/19,167) and 89% of patients with psychiatric diagnosis (19,691/22,062) had one or more comorbid disorders.
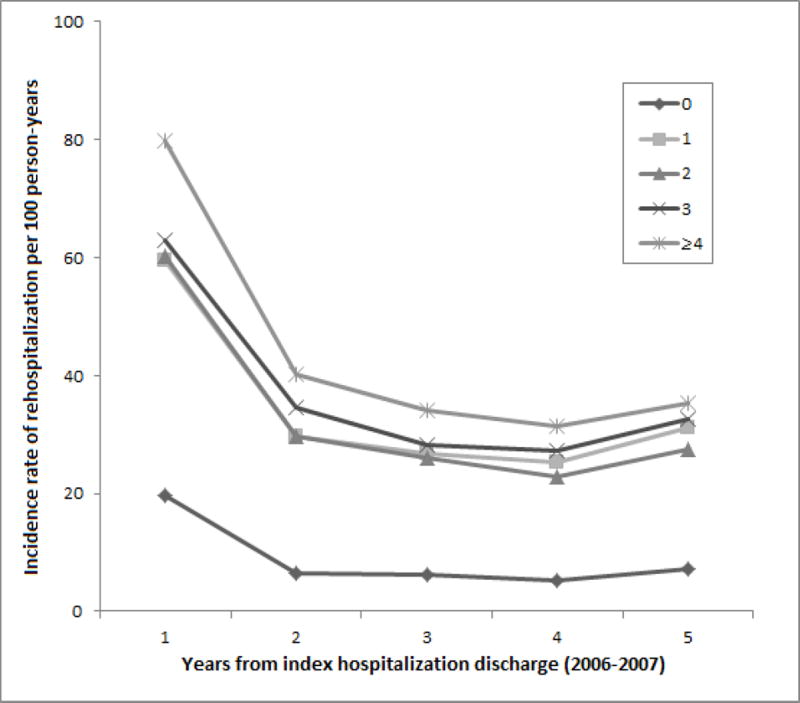
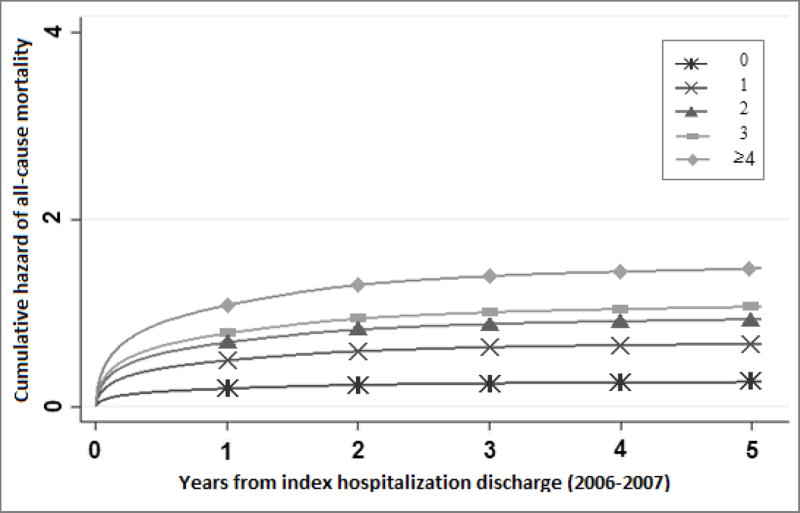
In age-adjusted analysis, all disorders except traumatic brain injury had a significantly increased risk of recurrent hospitalization and death (Table 2). After adjusting for age, patients with a greater cumulative burden of disorders demonstrated a pattern of greater risk of recurrent hospitalization and death over the course of the five years after hospital admission (Figure 1 and Figure 2).
FIGURE 1.
Cumulative disorders and incidence rate of recurrent hospitalizations over time (per 100 person-years), Washington State, 2006–2007
FIGURE 2.
Cumulative disorders and all-cause mortality over time (age adjusted), Washington State, 2006–2007
In regression models that adjusted for age, gender, payor status, injury severity, county of hospital, and discharge year/season, a greater number of disorders was associated with an increased risk of recurrent hospitalization (Table 3). These associations manifested in a dose-response pattern such that the addition of a single disorder increased risk in an incremental graded manner. Cox proportional hazard models that adjusted for age, gender, payor status, injury severity, county of hospital, and discharge year/season showed a similar dose-response pattern such that a greater number of disorders was associated with incremental increases in the risk of mortality (Table 3).
TABLE 3.
Impact of cumulative burden of disorders on recurrent hospitalizations and all-cause mortality, Washington State, 2006–2007
| Recurrent Hospitalizationsb | Mortalityc | |||
|---|---|---|---|---|
|
|
||||
| Conditionsa | Relative Risk | 95% CId | Hazard Ratio | 95% CI |
| 1 | 2.03 | 1.93–2.14 | 2.47 | 2.21–2.75 |
| 2 | 2.20 | 2.08–2.32 | 3.46 | 3.10–3.86 |
| 3 | 3.03 | 2.85–3.21 | 3.83 | 3.40–4.32 |
| ≥4 | 3.89 | 3.66–4.14 | 5.33 | 4.71–6.04 |
Cumulative disorders: alcohol, drug, psychiatric, medical, violent/suicide hospitalization
Regression results; reference group = no disorders
Cox Proportional Hazard Model Results; reference group = no disorders
CI, confidence interval
Results adjusted for age, gender, payor status, injury severity, discharge year/season, and county
Sensitivity analyses that used 0, 1, and ≥2 coding of the disorders did not substantially alter the magnitude, pattern, or significance of the observed associations for recurrent hospitalizations or all-cause mortality. Similarly, analyses that varied the number of days assessed post index injury hospitalization (i.e., 30, 90, or 180 days) did not substantially alter the pattern or magnitude of the recurrent hospitalization outcome regressions. Finally, including prior hospitalizations in the regression models did not modify the dose-response pattern but did weaken the strength of the observed associations for recurrent hospitalization (≥4 conditions, RR = 2.31, 95% CI = 2.17–2.45) and all-cause mortality (≥4 conditions, HR = 3.90, 95% CI = 3.44–4.42).
DISCUSSION
The investigation corroborates and extends observations from prior studies and suggests that a broad profile of psychiatric, substance use and medical disorders, as well as violent and suicide related events, frequently occur in civilian injury survivors (9, 11, 15, 16). This investigation documents that psychiatric, alcohol and drug use disorders rarely occur in isolation after injury and in the majority of patients are comorbid.
This large scale population-based investigation also demonstrates the remarkable heterogeneity of psychiatric, substance use, and chronic medical diagnostic presentations after injury. A literature review reveals few large-scale investigations that document a broad spectrum of highly prevalent chronic medical disorders including hypertension, ischemic heart disease, pain related disorders, pulmonary disorders, diabetes, cerebrovascular disease, renal, and liver conditions. This heterogeneity is further complicated by the addition of violent and suicide/overdose hospital admission etiologies. Few prior investigations have considered combining these multiple heterogeneous disorders into a single comorbidity index for injured civilians.
This is the first population-based investigation in civilians to demonstrate a dose-response relationship between the cumulative burden of psychiatric, substance use, and medical disorders and poor health outcomes after injury hospitalization. The health outcomes assessed included recurrent hospitalization and all-cause mortality over the course of the five years after injury admission. Investigation in trauma-exposed veterans suggest a similar dose-response relationship between cumulative burden of psychiatric, substance use, and medical conditions as well as traumatic brain injury and poorer health outcomes including increased health service utilization and death (5, 6).
In the current investigation, traumatic brain injury did not contribute to poorer health outcomes after the index injury admission. Prior investigation documenting poorer health outcomes in survivors of traumatic brain injury have used general population or non-injured controls (5, 14). Future investigation could explore the possibility that in hospitalized patients with multiple physical injuries, traumatic brain injury alone may not increase the risk of recurrent hospitalization or death.
This investigation has a number of important limitations. The study used a large administrative database to ascertain psychiatric diagnoses, alcohol and drug related diagnoses, and other injury and medical diagnoses. Assignment of diagnoses relied on diagnostic codes that frequently derived from assessments by acute care medical providers rather than expert diagnostic interviews. Additionally, information derived from outpatient visits is not included in the CHARS data. This may have impacted the accuracy of specific ICD-9-CM diagnostic categories in the investigation. Also, the administrative database did not contain a variable identifying patients racial or ethnic group status.
Approximately 10% of patients were missing ICD-9-CM codes related to injury severity. This may have resulted in underestimates of the number of patients diagnosed with traumatic brain injury in the investigation, and may explain why patients with traumatic brain injury did not demonstrate a consistent pattern of worsening outcomes in univariate and minimally adjusted analyses. In addition, the investigation did not account for individuals who were injured during the index period but were not residents of Washington State.
The investigation did not employ a pre-existing comorbidity index to assess injured patients’ risk for recurrent hospitalization and death. Although some of the conditions endemic among trauma survivors are captured by commonly employed and validated indices, multiple conditions including posttraumatic stress disorder, violence and suicide related hospital admissions, and traumatic brain injury are not (24). As with initial studies in returning veterans (5–7), the current approach aimed to include these conditions unique to injured civilians. Future investigation could productively explore the creation of comorbidity indices tailored to the unique constellation of conditions endemic to injured patients.
Finally, the investigation assessed longer term outcomes including recurrent hospitalization over a five year period; the current investigation did not focus intensively on 30-day readmission rates. Systematic investigation has begun of unplanned readmissions in general and trauma surgery, yet these investigations have tended to focus on short-term outcomes such as 30-day readmission rates (25, 26).
Beyond these considerations, this investigation has important implications for the detection and treatment of injured patients with comorbid psychiatric, substance use and chronic medical disorders, as well as violent and suicide related admissions. Prior investigations document shortcomings in the quality of post-injury psychiatric screening and service coordination (27). Commentary from the Centers for Disease Control and others suggests that screening and intervention procedures should be developed for the increasing number of Americans who suffer from multiple chronic conditions. The current investigation suggests that screening and intervention development could productively focus on multiple chronic disorders among injured trauma survivors (27, 28). Screening and intervention development could target both the prevention of the onset of new disorders (e.g., chronic PTSD in the wake of an injury hospitalization) and the mitigation of the impact of injury hospitalization on pre-existing chronic conditions (e.g., hypertension, diabetes) (18).
CONCLUSIONS
Ultimately, population-based surveillance procedures that incorporate pragmatic trials of real-time, workflow-integrated screening and stepped care interventions targeting the full spectrum of posttraumatic comorbidity clusters could be developed and implemented. One recent investigation utilized automated electronic medical record ICD-9-CM code screening to recruit patients and found that approximately two-thirds of hospitalized injured patients had one or more chronic medical disorders (29). Future pragmatic trials could test broadly targeted automated screening algorithms and computerized decision support tool facilitated intervention strategies (28, 30). A series of investigations suggest that collaborative care intervention models may be optimal intervention strategies for targeting the multiple chronic disorders that afflict injured trauma survivors (27, 29). Collaborative care intervention models productively combine care management targeting injury and medical conditions with evidence-based interventions for psychiatric and substance use related comorbidity. Measurement-based stepped care procedures allow collaborative care teams to systematically target multiple disorders over the weeks and months post-injury. Orchestrated investigative and policy efforts could systematically introduce and evaluate screening and intervention that broadly target the full spectrum of comorbid disorders afflicting hospitalized injured patients at US trauma centers (31).
Supplementary Material
Acknowledgments
Funding: This work was supported by Contract 124195 awarded by the City of Seattle and grants K24 MH086814 and U54 AT007748 and UH2/U3 MH106338 awarded by the National Institutes of Health
Footnotes
The authors declare no conflict of interest.
A preliminary version of this Manuscript was presented at the NIMH Mental Health Services Research Meeting August 1, 2016 in Bethesda, Maryland.
Contributor Information
Douglas Zatzick, University of Washington School of Medicine Ringgold standard institution - Psychiatry and Behavioral Sciences, Seattle, Washington; University of Washington School of Medicine Ringgold standard institution - Harborview Injury Prevention and Research Center.
Ali Rowhani-Rahbar, University of Washington School of Medicine Ringgold standard institution - Department of Epidemiology, Seattle, Washington; University of Washington School of Medicine Ringgold standard institution - Harborview Injury Prevention and Research Center, Seattle, Washington.
Jin Wan, University of Washington School of Medicine Ringgold standard institution - Harborview Injury Prevention and Research Center, Seattle, Washington.
Joan Russo, University of Washington School of Medicine - Psychiatry and Behavioral Science, Box 359911.
Doyanne Darnell, University of Washington School of Medicine Ringgold standard institution - Psychiatry and Behavioral Sciences, Seattle, Washington.
Leah Ingraham, University of Washington - Psychiatry and Behavioral Sciences, Seattle, Washington.
Lauren K. Whiteside, University of Washington School of Medicine Ringgold standard institution - Emergency Medicine, Seattle, Washington University of Washington School of Medicine Ringgold standard institution - Harborview Injury Prevention and Research Center, Seattle, Washington.
Roxanne Guiney, University of Washington School of Medicine Ringgold standard institution - Psychiatry and Behavioral Sciences, Seattle, Washington; University of Washington School of Medicine Ringgold standard institution - Harborview Injury Prevention and Research Center, Seattle, Washington.
Margot Kelly Hedrick, University of Washington School of Medicine Ringgold standard institution - Psychiatry and Behavioral Sciences, Seattle, Washington.
Frederick P. Rivara, University of Washington School of Medicine Ringgold standard institution - Pediatrics, Seattle, Washington University of Washington School of Medicine - Harborview Injury Prevention and Research Center, Seattle, Washington.
References
- 1.United States: President's Commission on Care for America's Returning Wounded Warriors: Serve, support, simplify: Report of the President's Commission on Care for America's Returning Wounded Warriors. Washington, DC: President's Commission on Care for America's Returning Wounded Warriors; 2007. [Google Scholar]
- 2.Office of Statistics and Programming, editor. National Center for Injury Prevention: CDC 2012. Atlanta, GA: Center for Disease Control and Prevention; 2012. [Google Scholar]
- 3.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000;90:523–6. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization: Disease and injury country estimates. 2012 Available from: http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html.
- 5.Pugh MJ, Finley EP, Copeland LA, et al. Complex comorbidity clusters in OEF/OIF veterans: The polytrauma clinical triad and beyond. Med Care. 2014;52:172–81. doi: 10.1097/MLR.0000000000000059. [DOI] [PubMed] [Google Scholar]
- 6.Finley EP, Bollinger M, Noel PH, et al. A national cohort study of the association between the polytrauma clinical triad and suicide-related behavior among US Veterans who served in Iraq and Afghanistan. Am J Public Health. 2015;105:380–7. doi: 10.2105/AJPH.2014.301957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trivedi RB, Post EP, Sun H, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health. 2015;105:2564–9. doi: 10.2105/AJPH.2015.302836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shih RA, Schell TL, Hambarsoomian K, et al. Prevalence of posttraumatic stress disorder and major depression after trauma center hospitalization. J Trauma. 2010;69:1560–6. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zatzick D, Rivara FP, Nathens AB, et al. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol Med. 2007;37:1469–80. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- 10.Zatzick D, Jurkovich G, Rivara F, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after injury hospitalization. Ann Surg. 2008;248:429–37. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 11.Soderstrom CA, Smith GS, Dischinger PC, et al. Psychoactive substance use disorders among seriously injured trauma center patients. Jama. 1997;277:1769–74. [PubMed] [Google Scholar]
- 12.Cunningham RM, Bernstein SL, Walton M, et al. Alcohol, tobacco, and other drugs: Future directions for screening and intervention in the emergency department. Acad Emerg Med. 2009;16:1078–88. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- 13.D'Onofrio G, Jauch E, Jagoda A, et al. NIH roundtable on opportunities to advance research on neurologic and psychiatric emergencies. Ann Emerg Med. 2010;56:551–64. doi: 10.1016/j.annemergmed.2010.06.562. [DOI] [PubMed] [Google Scholar]
- 14.Fazel S, Wolf A, Pillas D, et al. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury. JAMA Psychiatry. 2014;71:326–33. doi: 10.1001/jamapsychiatry.2013.3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 16.Sims DW, Bivins BA, Obeid FN, et al. Urban trauma: A chronic recurrent disease. J Trauma. 1989;29:940–7. [PubMed] [Google Scholar]
- 17.Goodman RA, Posner SF, Huang ES, et al. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. doi: 10.5888/pcd10.120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parekh AK, Goodman RA, Gordon C, et al. Managing multiple chronic conditions: A strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126:460–71. doi: 10.1177/003335491112600403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U. S. Department of Health and Human Services: Multiple chronic conditions - A strategic framework: Optimum health and quality of life for individuals with multiple chronic conditions. Washington, DC: Dec, 2010. [Google Scholar]
- 20.Civil ID, Schwab CW. The Abbreviated Injury Scale: 1985 revision. Morton Grove, IL: Committee on Injury Scaling, American Association for the Advancement of Automotive Medicine; 1985. [Google Scholar]
- 21.Rowhani-Rahbar A, Zatzick D, Wang J, et al. Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: A cohort study. Ann Intern Med. 2015;162:492–500. doi: 10.7326/M14-2362. [DOI] [PubMed] [Google Scholar]
- 22.Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1987;73:13–22. [Google Scholar]
- 23.Worrell SS, Koepsell TD, Sabath DR, et al. The risk of reinjury in relation to time since first injury: A retrospective population-based study. J Trauma. 2006;60:379–84. doi: 10.1097/01.ta.0000203549.15373.7b. [DOI] [PubMed] [Google Scholar]
- 24.Austin SR, Wong YN, Uzzo RG, et al. Why summary comorbidity measures such as the Charlson Comorbidity Index and Elixhauser Score work. Med Care. 2015;53:e65–72. doi: 10.1097/MLR.0b013e318297429c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. Jama. 2015;313:483–95. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 26.Moore L, Stelfox HT, Turgeon AF, et al. Rates, patterns, and determinants of unplanned readmission after traumatic injury: A multicenter cohort study. Ann Surg. 2014;259:374–80. doi: 10.1097/SLA.0b013e31828b0fae. [DOI] [PubMed] [Google Scholar]
- 27.Zatzick D, Jurkovich G, Rivara FP, et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013;257:390–9. doi: 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry. 2013;35:485–91. doi: 10.1016/j.genhosppsych.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zatzick D, O'Connor SS, Russo J, et al. Technology enhanced stepped collaborative care targeting posttraumatic stress disorder and comorbidity after injury: A randomized controlled trial. Journal of traumatic stress. 2015;28:391–400. doi: 10.1002/jts.22041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sugarman J, Califf RM. Ethics and regulatory complexities for pragmatic clinical trials. Jama. 2014;311:2381–2. doi: 10.1001/jama.2014.4164. [DOI] [PubMed] [Google Scholar]
- 31.American College of Surgeons Committee on Trauma: Resources for Optimal Care of the Injured Patient. Washington, DC: 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.