Abstract
Ear prominence is a relatively common cosmetic deformity with no associated functional deficits, but with profound psychosocial impact, especially in young patients. Protruding ears in children have propagated surgical advances that incorporate reconstructive techniques. Here we outline a systematic framework to evaluate the protruding ear and present various reconstructive surgical options for correction. Both cosmetic and reconstructive perspectives should be entertained when addressing this anatomical deformity.
Keywords: protruding ear, prominent ear correction, otoplasty, cosmetic, reconstruction
The protruding ear, also known as prominent ear, is one of the most common facial deformities affecting children. The aesthetic and psychosocial concerns surrounding an ear deformity serve as a catalyst for parents to seek correction. The social manifestations and psychological repercussions of a craniofacial abnormality can be devastating, thereby propagating the strong desire for otoplasty at an early age.
Management of protruding ear has evolved over time to include countless innovative surgical techniques (i.e., Mustardé, Furnas, and Stenstrom techniques). These methods have been continuously modified with the goal of improving aesthetic results while simultaneously minimizing the need of surgical revision. Because the purpose of protruding ear surgery is mostly aesthetic in nature, considerable attention is given toward producing reliable, stable, and satisfactory outcomes using advanced reconstructive techniques. This then proposes an intriguing theoretical question: Is protruding ear correction a cosmetic or reconstructive procedure?
In this review, we outline a systematic approach to evaluating ear prominence and planning the appropriate timing of reconstructive surgery. We discuss various surgical techniques that can be employed depending on the specific anatomical variables contributing to ear prominence. We propose that surgical intervention for protruding ear encompasses both cosmetic and reconstructive features. Advanced reconstructive techniques frequently used in microtia repair or correction of traumatic auricular defects have now been refined and applied to cosmetic protruding ear surgery. 1 This reconstructive approach to an aesthetic problem enhances cosmesis of the ear and subsequently reduces the overwhelming psychological burden of a visible auricular deformity in self-conscious children.
Ear Anatomy
A comprehensive understanding of auricular shape and structure is necessary when evaluating any form of ear deformity, including protruding ear. Mastery of auricular anatomy will guide the surgeon in determining the best management approach for maximally aesthetic outcomes.
Auricular anatomy varies greatly between individuals, but the fundamental components of the ear are defined to describe the overall structure. Ear architecture is primarily composed of the helix, antihelix, concha, tragus, and lobule, with ancillary structures such as the antitragus, intertragal incisures, and Darwin's tubercle ( Fig. 1 ). 1 In an average adult, the height of the ear is approximately 6 cm, and the width is approximately 55% of the height. 2 The conchal bowl extends to a depth of 1.5 cm with a sharp outer rim. 2 From an anterior view; the helix is visible approximately 2to 5 mm laterally from the antihelix. 1 Without the distinct curvature of the antihelix, the helical rim will flop forward, creating the appearance of a prominent ear. The conchoscaphal angle, which is normally less than 90 degrees, increases due to an inadequately folded antihelix and contributes to the lateral projection of the ear ( Fig. 2 ). 3
Fig. 1.
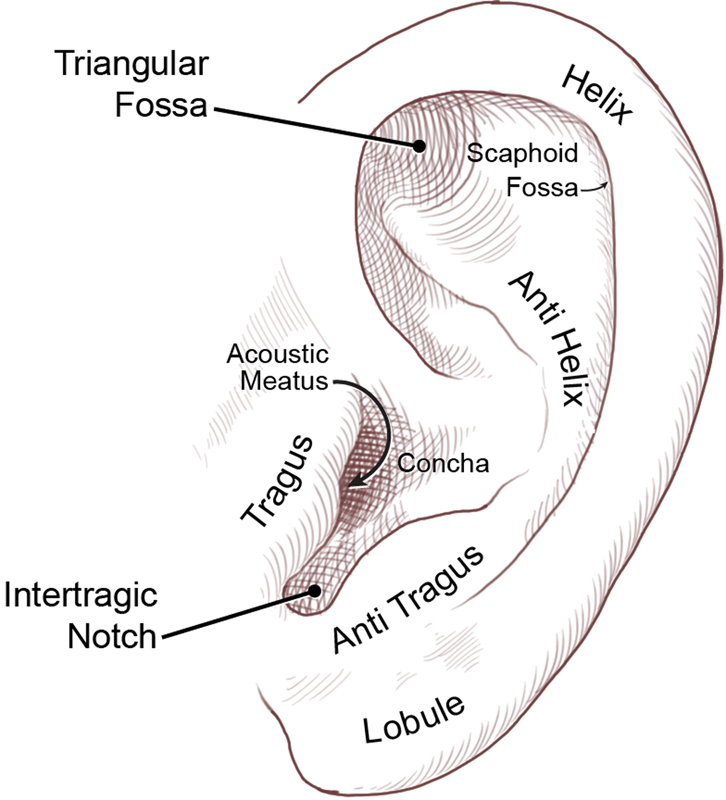
Ear anatomy.
Fig. 2.
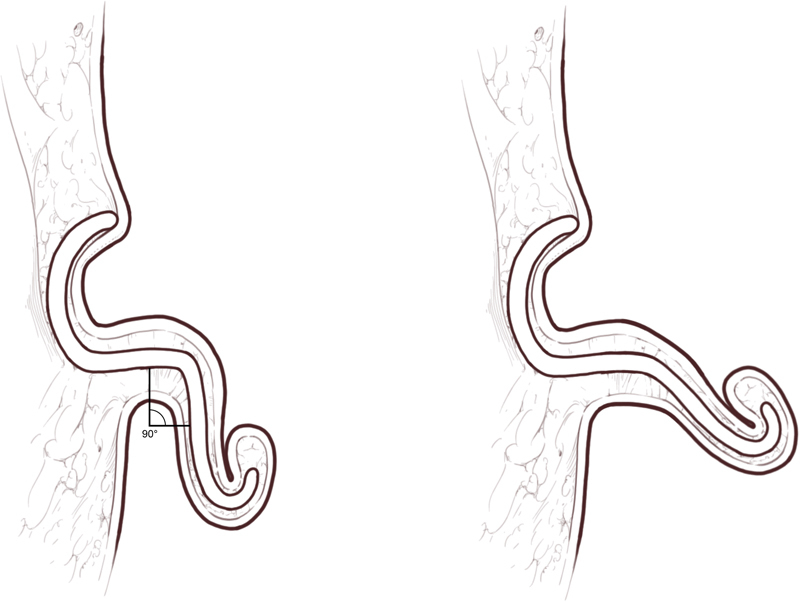
The conchoscaphal angle in a normal ( left ) and prominent ear ( right ).
The auricle normally projects no more than 2 cm from the mastoid process, forming an auriculocephalic angle of less than 25 degrees. The distance between the helix and mastoid is typically 10 to 12 mm in the upper third, 16 to 18 mm in the middle third, and 20 to 22 mm in the lower third of the ear. 4 When comparing both ears, the helix-to-mastoid distance at any point is usually within 3 mm. 4
Ear position on the scalp is just as important aesthetically as three-dimensional structure and projection. The Frankfort horizontal plane is a useful axis to gauge spatial relationships between the ear, eyebrow, eyes, and nose. 5 The Frankfort horizontal plane passes through the inferior orbital rim and intersects at the top of the tragus. 5 Superiorly, the upper border of the helical rim falls along the horizontal plane extending from the lateral brow and parallel to the Frankfort line. Inferiorly, the lobule of the ear is at the same horizontal level as the nasal tip. Along the vertical axis, the auricle is deviated 15 to 30 degrees posterolaterally; 3 this slope creates the normal, slightly rotated appearance of the ear upon the lateral view of the head.
When the above auricular proportions surpass normal limits, the ear appears aesthetically large and prominent. Although this is easily noticeable in unilateral conditions due to asymmetry, bilateral protruding ears are clinically perceptible if they significantly deviate from average dimensions. A thorough understanding of auricular anatomy and spatial relationships aids in proper evaluation and surgical management of the protruding ear, as described below.
Epidemiology and Contributing Factors
Protruding ear is the most common congenital auricular deformity and typically occurs bilaterally. 1 Approximately 5% of the population suffers from some degree of ear prominence, presenting as a cosmetic concern rather than a physiological deficit. 6 The specific etiology of this auricular malformation is unknown, and only a few cases are associated with distinct congenital or genetic diseases, such as Fragile X syndrome. 7 Furthermore, hypoxia or radiation exposure during pregnancy may aberrantly affect embryogenesis of the second branchial arch, leading to auricular malformations; however, this pathophysiologic mechanism has not been definitively linked to protruding ear deformities.
Weerda 8 proposed a classification method that broadly defined the spectrum of auricular dysplasia. In grade I auricular deformities, the majority of basic ear architecture is intact. Grade II describes both skin and cartilage defects, such as severe cup ear deformities and microtia. Grade III includes unrecognizable normal auricular architecture like with anotia, requiring total ear reconstruction for correction. Most cases of protruding ear and macrotia fall within the grade I group and do not require additional skin or cartilage for reconstruction. 8 9
The two most common anatomical abnormalities contributing to ear prominence are an underdeveloped antihelical fold and increased conchal bowl depth. 1 3 An inadequately curved antihelix prevents the normal posterior folding of the helical-scaphal unit; the conchoscaphal angle becomes more obtuse, which lengthens the distance from the helical rim to the scalp. 1 3 The ear in effect gains prominence as the auriculocephalic angle increases. In addition, conchal excess deepens the conchal bowl and displaces the helical rim laterally. The auricle no longer sits near the scalp and protrudes out due to the decreased acuity of the auriculocephalic angle. 1 3
In general, a poorly defined antihelical fold leads to prominence of the upper and middle thirds of the ear. A deep concha brings forward primarily the middle third of the auricle. Less commonly, a prominent lobule causes protrusion of the lower third of the ear. These irregularities may cause protrusion in isolation, but more frequently occur together, amplifying the overall prominence of the ear ( Fig. 3 ). 10
Fig. 3.
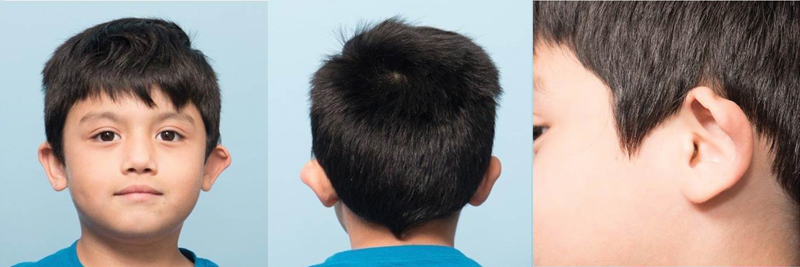
Left unilateral prominent ear.
Other exacerbating anomalies and variations in auricular development are associated with ear prominence, including underdeveloped helical curling, macrotia, Stahl's ear, and Darwin's tubercle. 4 6 Cup ear is an advanced form of protruding ear involving auricular constriction, stiff cartilage, and an incomplete opening of the ear canal. 6 10
Psychological Morbidity
An obvious aesthetic deformity, such as a prominent ear, has profound psychological impacts, especially in school-age children, when they become aware of their appearance and may feel ostracized as a result of being labeled as “different.” 11 These difficulties with social integration can result in behavioral problems and poor school performance. 4
Often, the psychological stress load of an auricular deformity serves as a catalyst for parents to seek surgical correction. 12 Although it is natural to assume that immediate intervention decreases the risk of psychological morbidity, corrective surgery at too early an age can result in poor aesthetic outcomes. This resurfaces psychoemotional expressions of deficiency and may plague the child with feelings of inadequacy and low self-appreciation lasting a lifetime. 11 Despite the psychological burden associated with a craniofacial deformity, surgeons must not feel pressured to perform correction until the optimal age is reached, as discussed below.
Timing of Surgical Intervention
Protruding ear usually manifests at an early age. However, the appropriate time for corrective surgery should balance auricular growth, cartilage pliability, psychological burden secondary to the auricular deformity, and patient maturity level. 3 In the golden window between ages 4 and 6, these elements align, thereby allowing optimal execution of reconstructive techniques to improve the cosmesis of the ear. 3
Auricular Growth
Following birth, the child's external ear continues to grow, reaching approximately 85% of its maximal width, and 50 to 60% of its maximal height by the age of 4 to 6 years. 3 13 Mature ear width is achieved at 6 to 7 years, while height grows at a slower rate, maturing by 12 to 13 years. 3 13 In addition, the auriculocephalic angle, or the projection of the helical root from the scalp, gradually increases from 16 degrees at age 1 to 22 degrees by age 10, plateauing at this angle. 4 13 Balogh and Millesi 14 observed that auricular growth was not restricted after a 7-year follow-up in children who underwent cartilage excision otoplasty; the corrected ear continued to grow following surgery with normal proportional increases in height and width. Ear growth harmoniously matched the growth of the contralateral ear, indicating that children could undergo correction of ear prominence as young as 4 years with the unlikely risk of auricular growth retardation. Furthermore, Mustardé 15 found a 1.8% recurrence rate 10 years following repair when the correction was performed in patients younger than 6 years, compared with a 30% relapse rate in patients who underwent correction after the age of 6.
Cartilage Pliability
Cartilage pliability contributes to higher success rates of prominent ear correction in patients younger than 6 years old. With increasing age, auricular cartilage becomes less malleable and more calcified, proving to be harder to manipulate in reconstructive procedures. 1 3
Psychological Burden
Studies have shown that prior to age 5, it is rare for children to experience peer ridicule or develop significant psychological anguish from ear prominence. 11 12 Delaying surgical intervention to some point between 4 and 6 years does not overwhelmingly contribute to psychological morbidity later in life. 12 Within this golden age window, surgeons can achieve optimal aesthetic outcomes without compromising the critical psychosocial development of children. In fact, almost all patients undergoing prominent ear correction at this age report enhanced self-confidence and well-being postoperatively, leading to better socialization and school performance. 12 16
Patient Maturity Level
Because functional hearing deficits are not associated with ear prominence, parents should opt to delay intervention until the child is mature enough to engage in his or her own postoperative care. This allows optimal adherence with postoperative instructions and restrictions and enables children to actively participate in decisions for corrective surgery. There is no maximum age when otoplasty must be performed, so patients can wait until adulthood for surgical correction if they desire. 4
Preoperative Evaluation
Ear size falls along a broad spectrum of variation between individuals, making it difficult to define normalcy. Although absolute parameters of external ear dimensions are good quantitative measures, ear prominence should always be examined in the overall context of the individual's facial structure. Slight deviations from normalcy can be considered abnormal ear projection, but may not be viewed as such by the patient or family. For this reason, special attention should be taken to understand how the protruding ear appears in relation to overall facial architecture. Aesthetic judgment is typically used in practice when initially examining protruding ears, while objective measurements of auricular dimensions and projection are recorded when planning the specific reconstructive approach.
It is in the surgeon's best interest to systematically evaluate protruding ears. An objective algorithm to measure auricular dimensions is necessary to avoid missing any deviation from normal parameters. With accurate preoperative measurements, the surgeon can minimize dissatisfaction due to asymmetry or size distortion following corrective surgery.
Numerous anatomical variables are used to evaluate ear architecture ( Table 1 ), being ear size, position, projection, rotation, contour, and symmetry the most important for surgical planning. 17 18 Auricular height and width determine ear size. Ear position on the scalp is measured along two horizontal distances: the first between the superior border of the helical rim and the lateral brow, and the second between the inferior border of the lobule and nasal columellar base. 4 A three-dimensional analysis of ear projection is particularly important to determine the degree of ear prominence. The auriculocephalic angle and helix-to-mastoid distance along the entirety of the auricular rim are the most commonly used parameters for ear projection. Special attention must be given to examining the contour of the antihelix and conchal bowl because abnormalities in these two features are the primary contributors to the protruding ear. 2 In some cases, conchal hypertrophy is difficult to appreciate, so placing gentle medial pressure along the helical rim can allow better visualization of prominent conchal cartilage. 1 Lastly, measurements of the prominent ear must be compared with the contralateral ear to compute the amount of correction needed for symmetrical results. 17 18
Table 1. Basic anatomical variables in the preoperative assessment of the protruding ear.
| Ear size |
|---|
| Auricular height from tip of lobule to superior margin of helical rim |
| Auricular width from anterior base of tragus to lateral margin of helical rim |
| Ear position and rotation |
| Distance between the superior border of the helical rim and lateral brow |
| Distance between the ear lobule and nasal columellar base |
| Vertical axis of the ear (normally rotated posterolaterally by 15–30 degrees) |
| Ear contour |
| Degree of antihelical folding and conchoscaphal angle (normally < 90 degrees) |
| Depth of hemispherical conchal bowl (normally < 1.5 cm) |
| Ear projection |
| Auriculocephalic angle (normally < 25 degrees) |
| Distance between the helix and mastoid, along the entirety of the auricular rim |
| Other |
| Quality and malleability of auricular cartilage |
| Other exacerbating anomalies or anatomical variations in the auricle |
It is important to assess for other exacerbating anomalies and correctable auricular defects, such as macrotia, constricted ears, conchal crus (abnormal transverse fold in the conchal cartilage), Stahl's ear, or Darwin's tubercle. 4 6 By including this assessment, the surgeon can potentially address these abnormalities simultaneously with protruding ear correction to maximize aesthetic outcomes.
No specific preoperative imaging or consultations are required in children with normal acoustic function. Standard preoperative photographs are taken from anterior, posterior, and lateral views.
The psychological impact of ear prominence is an important facet of preoperative evaluation. When discussing the implications and management of ear deformities with the patient and family, the surgeon must portray compassion and empathy. Most importantly, the surgeon should ascertain how much insight the child has regarding his or her ear deformity and discuss their expectations. This can shed light on how ear prominence has influenced the child's self-confidence and social interactions. 11 Bradbury et al 16 highly recommend psychological evaluation of any child with severe social isolation or psychological anguish prior to surgery. If the child is mature enough, the surgeon should also interview the child regarding his or her thoughts on a corrective operation. This engages children in the decision-making process and enables them to feel as though they are taking active measures toward uplifting their self-confidence. 16
Goals of Surgery
The surgeon should strive to leave the ear with an “unoperated” appearance with soft, natural contours. The setback should be harmonious—that is, each portion should appear in an appropriate position relative to the rest of the ear. 19 McDowel 20 published more specific goals of otoplasty to consider:
Correct protrusion of the upper third of the ear; protrusion of the middle or lower third is acceptable as long as the upper third is completely corrected, but the reverse is not true.
From the front view, the helix of both ears should extend beyond the antihelix, at least to the mid ear.
The helix should have a smooth and regular line throughout.
The postauricular sulcus should not be markedly decreased or distorted.
The ear should not be placed too closely to the head, especially in boys; the posterior measurement from the outer edge of the helix to the skin of the mastoidal region should be 10 to 12 mm in the upper third, 16 to 18 mm in the middle third, and 20 to 22 mm in the lower third.
The positions of the two ears (i.e., the distances from the lateral borders to the head) should match fairly closely to within 3 mm at any point.
The patient should be examined from three views (front, side, and back) prior to closing the skin incisions. Notably, in the posterior view, the helical rim should be a straight line; iatrogenic helical deformities, such has a “C” or a “hockey stick” shape, should be corrected. Sharp, unnatural contours, overcorrection, and obliteration of the normal sulcus are unacceptable results. 19 Overall, surgeons can take advantage of advanced reconstructive methods to strive for a harmonious setback of the protruding ear without compromising the shape, contour, or overall architecture of the auricle.
Management Options
The protruding ear can be managed through a multitude of approaches, both surgical and nonsurgical.
Molding techniques are frequently successful in infants with protruding or deformed ears. The pliability and moldability of neonatal cartilage are due to circulating maternal estrogens. 21 Byrd et al 21 instituted a strict protocol to initiate molding therapy with the EarWell TM Infant Ear Correction System (Becon Medical Ltd.) within 1 to 2 weeks of birth if the deformity did not resolve spontaneously. By continuing molding therapy for 6 weeks, they achieved more than a 90% success rate, defined as a good to excellent result, on 58 deformed ears. Others authors 1 19 also advocate for early, extended molding therapy with splinting, taping, or gluing.
Laser-assisted cartilage remodeling (LACR) is based on the temperature-dependent characteristics of cartilage. Cartilage biomechanics are temperature-dependent, and temperatures between 50 and 70°C induce stress relaxation leading to gross morphological changes. The ideal wavelength for cartilage reshaping is 1540 nm because the penetration depth matches the thickness of cartilage, thereby allowing for homogenous heat generation. 22 A systematic review of seven clinical series 22 utilizing LACR to correct a prominent ear revealed a similar degree of correction when compared with conventional techniques. The authors claim that LACR provides a smoother, more natural curvature than conventional techniques, but without the incisions and subsequent scarring. In the two studies that patient satisfaction scores were recorded, many patients were pleased or satisfied with the result; the average satisfaction ratings were 8.6/10 and 16.8/20 (10-point scale for each ear). All patients surveyed would undergo the operation again. Skins burns and dermatitis were the most commonly encountered complications.
Surgery continues to be the main therapy to correct the protruding ear.
Surgical Technique Overview
There are two key principles to the correction of the prominent ear: recreation of the antihelical fold and normalization of the concha size and position. The auricle is often approached through an incision in the retroauricular sulcus, 10 but an anterior approach is also possible.
Antihelical Fold Manipulation
Correction of the ear's upper third is mainly accomplished by recreating the antihelical fold. Many techniques have been described and can be subdivided by the means of cartilage manipulation: molding, breaking, and/or scoring techniques. 10
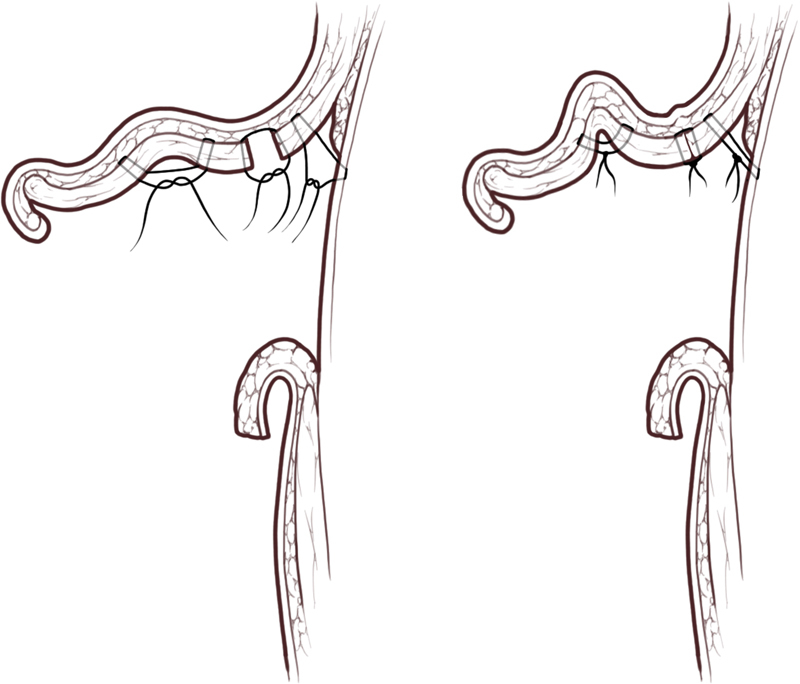
Cartilage molding or suturing techniques rely on suture fixation to maintain the new position of the scaffold. Various techniques have been pioneered to recreate the antihelix, with the Mustardé 23 technique being the most popular. This entails placement of nonabsorbable conchoscaphal mattress sutures in the posterior cartilage to recreate the antihelical fold ( Fig. 4 ). Kaye 24 and Tramier 25 advocated for an anterior approach to place the conchoscaphal mattress sutures in the anterior cartilage. This was believed to be technically simpler and to require less skin flap dissection, thereby minimizing postoperative discomfort and risk of hematoma.
Fig. 4.
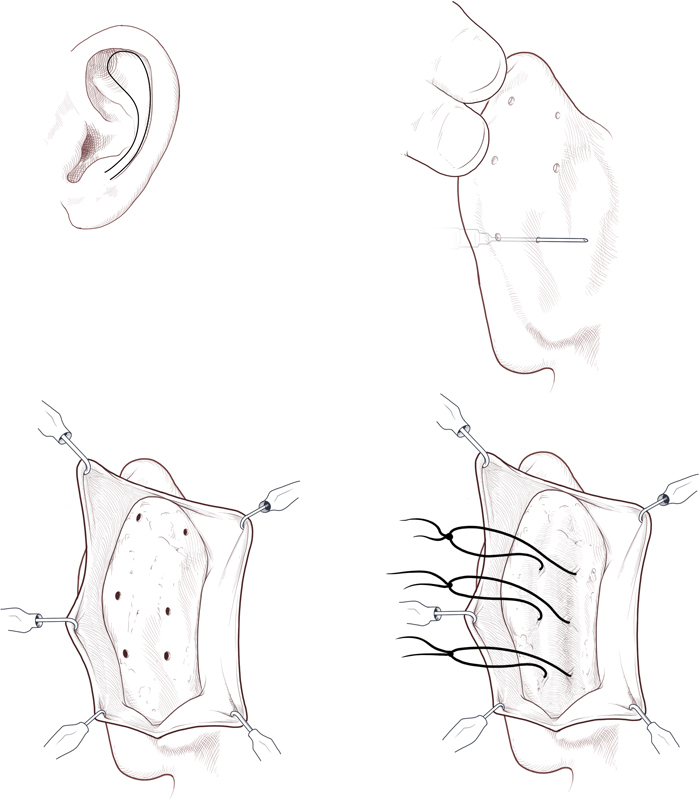
Intraoperative marking and conchoscaphal sutures placement to recreate the antihelical fold.
The Converse and Wood-Smith 26 breaking technique involves making full-thickness incisions through the cartilage (but not the anterior perichondrium) parallel to the location of the desired antihelical fold. The cartilage between the incisions is thinned, bent into a tube shape, and sutured to maintain the desired contour of the antihelix.
Alternatively, Stenstrom 27 and Chongchet 28 both utilized anterior scoring, based upon Gibson's principle that cartilage tends to bowstring in the direction opposite of its injured surface to create the desired concavity or convexity. 29 The degree of cartilage warping can be adjusted by the extent of the abrasion. 27
These techniques may be used alone or in combination, but benefits and drawbacks accompany each. Cartilage breaking and scoring techniques may have the advantage of a lower recurrence of deformity, but cartilage scoring is difficult to control, and may result in sharp edges or an overdone appearance. 10
Skin excision has also been described in various techniques, but some 10 believe it is unnecessary as it does not contribute to the correction and may result in hypertrophic scarring.
Conchal Deformity Management
Several methods have been used to address conchal deformity, including suturing, conchal excision, and scoring.
Conchomastoid sutures can be placed to address conchal excess and prominence of the superior two-thirds of the ear. 1 Furnas 30 describes placement of nonabsorbable sutures through the conchal cartilage, through the mastoid fascia, and into the periosteum of the mastoid fascia. This technique sets back the concha and, as a result, pushes back the middle part of the ear. Extensive rotation of the conchal cup may result in external auditory canal obstruction, especially if the sutures are placed too far anteriorly on the mastoid or too far posteriorly on the concha; 30 if this occurs, the sutures should be adjusted, or a conchal resection should be performed. 19 Conchomastoid suturing alone is rarely adequate to achieve an optimal outcome ( Fig. 5 ).
Fig. 5.
Otoplasty cartilage sutures—conchoscaphal, conchal approximation after excision, and conchal-mastoid fascial.
Like many of the otoplasty techniques, the Furnas approach has undergone multiple modifications. Taboada-Suarez et al 9 investigated the efficacy of knotless, bidirectional, barbed absorbable sutures (BBAS) compared with nonabsorbable sutures in the correction of Weerda grade I protruding ears. In the BBAS group, there was significantly less pain, the operation was faster, and there were no reoperations despite no use of a headband postoperatively.
Conchal excision is necessary if there is excess conchal depth. 19 It is performed at the junction of the posterior wall and floor of the concha 19 and can be accomplished through either an anterior or a posterior approach. Skin excision in addition to cartilage excision is usually done through an anterior approach, while cartilage only excision is often performed through a posterior approach. There is no proven advantage to either approach. 1
Additionally, the conchal defect can be managed with cartilage scoring applying Gibson's principle. The anterior surface of the concha is scored to induce posterior warping of the conchal wall. This converts the prominent conchal wall into a scaphal surface. 1
Lobule
The aforementioned techniques do not address lobule positioning and in fact, may amplify lobule protuberance. 10 The lobule should be assessed and addressed as the final step of the otoplasty. 31 The goal is for the helical rim and the ear lobule to align in a straight line, being careful to avoid over- or undercorrection resulting in “telephone” or “reverse telephone” deformity. The approach of Gosain 31 hinges upon identifying the point of control—the point closest to the retrolobular sulcus that repositions the entire lobule without significantly distorting it. A perpendicular incision is made on the medial side of the lobule from the point of control to the postauricular skin incision, and two triangular areas of excess skin on either side of the point of control are excised. The suture is passed through the point of control, fastened to the mastoid fascia, and tightened until the lobule is adequately controlled. Wood-Smith uses a modified fishtail excision to correct the protruding lobule, 1 whereas Spira et al 32 make a wedge excision and produce the desired degree of correction with a deep dermis to scalp periosteum suture.
Endoscopic Otoplasty
Endoscopic-assisted otoplasty was developed as a minimally invasive alternative to traditional, open approach otoplasty techniques. In Graham and Gault's 33 technique, the skin excision is transposed from the postauricular region to the temporal scalp. The postauricular cartilage is accessed through this temporal scalp incision and weakened by abrasion. Nonabsorbable sutures are inserted, via postauricular stab incisions, between the scaphal cartilage and the mastoid fascia to create a new antihelical fold, resulting in good outcomes with no recurrence. 33 There is avoidance of skin excision and excessive dissection of the cartilage; hypertrophic scarring or keloid formation is less common due to the position of the incision from the postauricular region to the temporal scalp. 33
Incisionless Otoplasty
Incisionless otoplasty adds another minimally invasive technique to the surgeon's armamentarium, with an easy recovery and no need for long-term dressings. 34 The foundations of this technique, pioneered by Fritsch, 35 are percutaneous conchoscaphal and conchomastoid retention sutures. The cartilage is first scored in the location of the new antihelical fold to reduce the tension on the sutures that will be placed. Percutaneous retention sutures hold the new antihelical fold in place. The current incisionless technique (version 3.0) can be used for antihelical correction, conchal recession, simultaneous antihelical and conchal alteration, and lobule manipulation. 35 Mehta and Gantous 34 retrospectively analyzed the efficacy of incisionless otoplasty by a single surgeon for the correction of the prominent ear. None experienced significant complications (infection, hematoma, perichondritis, cartilage necrosis), the revision rate was 13%, and there were no overcorrections. The authors concluded that the technique is less invasive yet equally effective when compared with open otoplasty. 34
Complications
Otoplasty complications are classified as either acute or chronic. Acute complications include postoperative hematoma or hemorrhage, infection, chondritis, perichondritis, and skin or cartilage necrosis. 1 19 36 Chronic complications include keloid or hypertrophic scarring, suture complications, dysesthesia, residual deformity, asymmetry, narrowing of the external auditory meatus, and patient dissatisfaction. 1 19 36
Acute complications arise within hours to days of surgery. A postoperative hematoma is one of the most feared complications. It commonly presents as an acute onset of severe, persistent, unilateral, or asymmetric pain. 1 36 Chondritis is a surgical emergency, frequently resulting from infection, and may lead to cartilage necrosis with eventual auricular deformity. 1 3
Residual deformity is the most common late sequelae and is usually apparent by 6 months postoperatively. 1 Suture complications are also very common. 19 36 Braided, polyfilament sutures are more reactive and thus more likely to lead to infection or granuloma formation. Monofilament sutures are more prone to skin erosion, bowstring appearance beneath the skin, and slippage resulting in malpositioning. 36 Because otoplasty for the prominent ear is primarily judged by aesthetic goals, loss of correction and patient satisfaction are important long-term sequelae. Loss of correction occurs in approximately 6.5 to 12% of cases and is primarily determined by the category of technique performed. 36 Cartilage-molding techniques have higher rates of loss of correction when compared with cartilage breaking or cartilage scoring techniques, and skin only excision (not described here) results in the highest rates. 36
Conclusion
Protruding ears may not harbor true functional deficits, but the cosmetic and psychological impacts can be profound, especially in the pediatric population. A strong grasp of auricular anatomy is needed when evaluating the deformity so that the best, individualized surgical approach can be planned. Generally, the golden rule for treating ear prominence is to fit the ear to the face for a more natural appearance. To achieve this goal, complex reconstruction of auricular skin and cartilage is performed to harmoniously setback the ear without distorting shape, contour, or architecture. By implementing reconstructive methods, the surgeon can optimize aesthetic outcomes with minimal evidence of surgical intervention. For this reason, both cosmetic and reconstructive perspectives to managing protruding ears are recommended.
References
- 1.Janis J E, Rohrich R J, Gutowski K A. Otoplasty. Plast Reconstr Surg. 2005;115(04):60e–72e. doi: 10.1097/01.prs.0000156218.93855.c9. [DOI] [PubMed] [Google Scholar]
- 2.Furnas D W.Otoplasty for prominent ears Clin Plast Surg 20022902273–288., viii [DOI] [PubMed] [Google Scholar]
- 3.Janz B A, Cole P, Hollier L H, Jr, Stal S.Treatment of prominent and constricted ear anomalies Plast Reconstr Surg 2009124(1, Suppl)27e–37e. [DOI] [PubMed] [Google Scholar]
- 4.Adamson J E, Horton C E, Crawford H H. The growth pattern of the external ear. Plast Reconstr Surg. 1965;36(04):466–470. doi: 10.1097/00006534-196510000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Siegert R, Weerda H, Remmert S. Embryology and surgical anatomy of the auricle. Facial Plast Surg. 1994;10(03):232–243. doi: 10.1055/s-2008-1064574. [DOI] [PubMed] [Google Scholar]
- 6.Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003;14(05):643–653. doi: 10.1097/00001665-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Yugueros P, Friedland J A.Otoplasty: the experience of 100 consecutive patients Plast Reconstr Surg 2001108041045–1051., discussion 1052–1053 [DOI] [PubMed] [Google Scholar]
- 8.Weerda H. Classification of congenital deformities of the auricle. Facial Plast Surg. 1988;5(05):385–388. doi: 10.1055/s-2008-1064778. [DOI] [PubMed] [Google Scholar]
- 9.Taboada-Suárez A, Brea-García B, Couto-González I, Vila-Moriente J L. Correction of protruding ears (Weerda grade I deformity) using knotless bidirectional barbed absorbable sutures. Otolaryngol Head Neck Surg. 2014;151(06):939–944. doi: 10.1177/0194599814551541. [DOI] [PubMed] [Google Scholar]
- 10.Thorne C H. Philadelphia: Lippincott Williams & Wilkins; 2014. Otoplasty; pp. 530–536. [Google Scholar]
- 11.Macgregor F C. Ear deformities: social and psychological implications. Clin Plast Surg. 1978;5(03):347–350. [PubMed] [Google Scholar]
- 12.Cooper-Hobson G, Jaffe W. The benefits of otoplasty for children: further evidence to satisfy the modern NHS. J Plast Reconstr Aesthet Surg. 2009;62(02):190–194. doi: 10.1016/j.bjps.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Bradbury E T, Hewison J, Timmons M J. Psychological and social outcome of prominent ear correction in children. Br J Plast Surg. 1992;45(02):97–100. doi: 10.1016/0007-1226(92)90165-t. [DOI] [PubMed] [Google Scholar]
- 14.Ellis D A, Keohane J D. A simplified approach to otoplasty. J Otolaryngol. 1992;21(01):66–69. [PubMed] [Google Scholar]
- 15.Adamson P A, Litner J A. Otoplasty technique. Otolaryngol Clin North Am. 2007;40(02):305–318. doi: 10.1016/j.otc.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Farkas L G, Posnick J C, Hreczko T M. Anthropometric growth study of the ear. Cleft Palate Craniofac J. 1992;29(04):324–329. doi: 10.1597/1545-1569_1992_029_0324_agsote_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 17.Balogh B, Millesi H. Are growth alterations a consequence of surgery for prominent ears? Plast Reconstr Surg. 1992;90(02):192–199. [PubMed] [Google Scholar]
- 18.Mustardé J C. The treatment of prominent ears by buried mattress sutures: a ten-year survey. Plast Reconstr Surg. 1967;39(04):382–386. [PubMed] [Google Scholar]
- 19.Thorne C H, Wilkes G. Ear deformities, otoplasty, and ear reconstruction. Plast Reconstr Surg. 2012;129(04):701e–716e. doi: 10.1097/PRS.0b013e3182450d9f. [DOI] [PubMed] [Google Scholar]
- 20.McDowell A J. Goals in otoplasty for protruding ears. Plast Reconstr Surg. 1968;41(01):17–27. doi: 10.1097/00006534-196801000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Byrd H S, Langevin C J, Ghidoni L A. Ear molding in newborn infants with auricular deformities. Plast Reconstr Surg. 2010;126(04):1191–1200. doi: 10.1097/PRS.0b013e3181e617bb. [DOI] [PubMed] [Google Scholar]
- 22.Leclère F M, Vogt P M, Casoli V, Vlachos S, Mordon S. Laser-assisted cartilage reshaping for protruding ears: a review of the clinical applications. Laryngoscope. 2015;125(09):2067–2071. doi: 10.1002/lary.25260. [DOI] [PubMed] [Google Scholar]
- 23.Mustardé J C. The correction of prominent ears using simple mattress sutures. Br J Plast Surg. 1963;16:170–178. doi: 10.1016/s0007-1226(63)80100-9. [DOI] [PubMed] [Google Scholar]
- 24.Kaye B L. A simplified method for correcting the prominent ear. Plast Reconstr Surg. 1967;40(01):44–48. doi: 10.1097/00006534-196707000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Tramier H. Personal approach to treatment of prominent ears. Plast Reconstr Surg. 1997;99(02):562–565. doi: 10.1097/00006534-199702000-00042. [DOI] [PubMed] [Google Scholar]
- 26.Converse J M, Wood-Smith D. Technical details in the surgical correction of the lop ear deformity. Plast Reconstr Surg. 1963;31:118–128. doi: 10.1097/00006534-196302000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Stenstroem S J. “Natural” technique for correction of congenitally prominent ears. Plast Reconstr Surg. 1963;32:509–518. [PubMed] [Google Scholar]
- 28.Chongchet V. A method of antihelix reconstruction. Br J Plast Surg. 1963;16:268–272. doi: 10.1016/s0007-1226(63)80120-4. [DOI] [PubMed] [Google Scholar]
- 29.Gibson T, Davis W. The distortion of autogenous cartilage grafts: its cause and prevention. Br J Plast Surg. 1958;10:257–274. [Google Scholar]
- 30.Furnas D W. Correction of prominent ears with multiple sutures. Clin Plast Surg. 1978;5(03):491–495. [PubMed] [Google Scholar]
- 31.Gosain A K, Recinos R F. A novel approach to correction of the prominent lobule during otoplasty. Plast Reconstr Surg. 2003;112(02):575–583. doi: 10.1097/01.PRS.0000071000.80092.2A. [DOI] [PubMed] [Google Scholar]
- 32.Spira M, McCrea R, Gerow F J, Hardy S B. Correction of the principal deformities causing protruding ears. Plast Reconstr Surg. 1969;44(02):150–154. [PubMed] [Google Scholar]
- 33.Graham K E, Gault D T. Endoscopic assisted otoplasty: a preliminary report. Br J Plast Surg. 1997;50(01):47–57. doi: 10.1016/s0007-1226(97)91283-2. [DOI] [PubMed] [Google Scholar]
- 34.Mehta S, Gantous A. Incisionless otoplasty: a reliable and replicable technique for the correction of prominauris. JAMA Facial Plast Surg. 2014;16(06):414–418. doi: 10.1001/jamafacial.2014.552. [DOI] [PubMed] [Google Scholar]
- 35.Fritsch M H. Incisionless otoplasty. Otolaryngol Clin North Am. 2009;42(06):1199–1208. doi: 10.1016/j.otc.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Handler E B, Song T, Shih C. Complications of otoplasty. Facial Plast Surg Clin North Am. 2013;21(04):653–662. doi: 10.1016/j.fsc.2013.08.001. [DOI] [PubMed] [Google Scholar]


