Abstract
Purpose
Given high levels of obesity among U.S. children, we examine whether obesity in childhood is a passing phenomenon or remains entrenched into adolescence.
Methods
Data are from the prospective nationally representative Early Childhood Longitudinal Study, Kindergarten Class of 1998–1999 (analytic sample=6,600). Anthropometrics were measured 6 times during 1998–2007. Overweight and obesity were defined using CDC cut-points. Entrenched obesity was defined as obesity between ages 5–9 coupled with persistent obesity at ages 11 and 14.
Results
Almost 30% of children experienced obesity at some point between ages 5.6 and 14.1 years; 63% of children who ever had obesity between ages 5.6 and 9.1 and 72% of those who had obesity at kindergarten entry experienced entrenched obesity. Children with severe obesity in kindergarten or who had obesity at more than one year during early elementary were very likely to experience obesity through age 14, regardless of their sex, race, or socio-economic background.
Conclusions
Prevention should focus on early childhood, as obesity at school entry is not often a passing phenomenon. Even one timepoint of obesity measured during the early elementary school years may be an indicator of risk for long-term obesity.
Keywords: obesity, overweight, childhood, adolescence, early onset, longitudinal
Introduction
Childhood obesity has become a major concern for individual and population health. With 12% of children in the U.S. already having obesity by the age of 5 years,(1) the implications of long term obesity are indeed serious, given the associations between obesity and health problems such as diabetes and CVD.(2–4)
An important question about obesity in childhood is whether it is a fleeting or entrenched health problem. That is, children grow at different rates, and a brief period of obesity may not be a reason for major worry for parents and pediatricians. On the other hand, if obesity becomes entrenched, that is, firmly established and difficult to reverse, this is indeed a major concern, as it entails that the child is likely to continue having obesity into adulthood, with the major health consequences of long-term exposure to obesity.(5–7)
Several studies have suggested that people tend to maintain their weight trajectories as they age, and that, to the extent that weight changes, it increases.(1, 8–13) While many individuals with normal weight in childhood first developed overweight or obesity in adulthood, few children who had overweight or obesity eventually achieve normal weight.(12–15) In urban Greenland, schoolchildren with obesity tended to retain obesity: of children with obesity at school entry, 10% achieved normal weight by age 15 years.(10) In a nationally representative British cohort followed from ages 3 to 11, an obese trajectory was already distinct by age 3 and an overweight trajectory diverged from normal-weight trajectories around age 5.(16) In rural U.K., less than 2% of 7 year- olds with obesity had normal weight at age 11 years, while among normal weight children, less than 1% developed obesity.(12) In one nationally representative U.S. study, children with obesity at age 5 years had a 47% probability of obesity at age 14 years.(1) Regional data from longitudinal studies of adults in the U.S. showed that individuals who had overweight or obesity in childhood or adolescence were more likely to have obesity in adulthood.(7, 17–20)
Most of the evidence on weight tracking comes from studies from outside the U.S. or from sub-national studies in the U.S. This study presents nationally representative data on entrenched obesity based on a recent cohort of children in the U.S., the Early Childhood Longitudinal Study (ECLS-K). Using multiple direct anthropometric measurements between the ages of 5 and 14 years, we assess the extent to which obesity in early childhood becomes entrenched, the ages of greatest risk, and which children are at highest risk, if ever they do developed obesity, to retain obesity into adolescence. While previous papers have focused on the incidence or prevalence of obesity, the contribution of this paper is to describe what happens after an incident case – to understand whether childhood obesity is a temporary or absorbing state, and what characteristics are associated with staying in the obese state.
Material and Methods
Data
We analyzed data from the Early Childhood Longitudinal Study, Kindergarten Class of 1998–1999 (ECLS-K), developed by the National Center for Education Statistics (NCES) of the U.S. Department of Education to study children’s development and experiences from kindergarten through the eighth grade. The ECLS-K is a nationally representative cohort selected with multistage probability sampling. The primary sampling units (PSUs) were counties or groups of counties, the secondary stage of selection was schools within the sampled PSUs and the third stage unit was students within schools.(21) The ECLS-K enrolled 21,260 children around the country in Fall 1998 (mean age 5.6 years), with 6,600 (all numbers are rounded to the nearest 10, per NCES restricted use data agreement), followed with complete data through study waves in Spring 1999 (mean age 6.1 years), 2000 (mean age 7.1 years), 2002 (mean age 9.1 years), 2004 (mean age 11.1 years), and 2007 (mean age 14.1 years).
The primary source of attrition from the original kindergarten sample resulted from random selection for non-sampling due to survey costs. That is, the attrition bias was minimized because the ECLS-K followed a random sub-sample of half the movers in each wave prior to 5th grade and all the movers between grades 5 and 8.(21) Appropriate weights for adjusting for attrition and non-response were created by ECLS-K staff and we used these for all analyses. Children with missing follow-up data were more likely to be Black and of lower socioeconomic status relative to those with complete data, but there were no substantial differences have been found between respondents and non-respondents, and non-response bias is addressed by the use of weights.(22)
Trained assessors measured height and weight for all participants twice per wave. Height was measured in inches to the nearest 0.25 inch using a Shorr Board and weight was measured in pounds using a digital scale.(23) Primary caregivers were asked about the child’s health at birth, including birth weight, during the baseline interview, and invited to add details at subsequent waves. Primary caregivers were asked detailed questions about child characteristics and about household social and economic circumstances and family characteristics at each wave of data collection.
Analysis
The analytic cohort consists of children with complete data over 9 years of follow-up on height and weight, age, sex, and race/ethnicity (n=6600). We used longitudinal weights and survey adjustments constructed by NCES to account for attrition and to make nationally representative inferences.
We use the 2000 CDC Growth Reference to calculate each child’s BMI z-score, standardized to the reference population for the child’s age and sex.(24) Children were categorized as having normal-weight, overweight, or obesity at each data wave using CDC cut-points of the 85th percentile for overweight and the 95th percentile for obesity. For some analyses, to distinguish between levels of obesity, we followed the commonly used approach of measuring severe obesity as the lower of BMI>120% of the 95th percentile or a BMI>35.
Entrenched obesity was defined as having or developing obesity between kindergarten entry (average age 5.6 years) and third grade (age 9.1 years) and retaining obesity between 5th grade (average age 11.1 years) and 8th grade (average age 14.1 years). Thus, entrenchment considers not only the occurrence of obesity in early childhood, but the extent to which it then persists through middle childhood and early adolescence. The age span of 11 to 14 years encompasses a long period during early adolescence that is an important stage of development for body weight.(25) Obesity at these ages is a strong indicator of subsequent obesity and morbidity.(26) Also, as the incidence of new cases of obesity drops to low levels between 5th and 8th grades,(1) it is reasonable to consider this period of childhood as a “steady state” period for identifying entrenched obesity.
We defined three other terms to help identify the nature of the early onset of entrenched obesity. We have two measures of “ever obesity” to indicate whether the child was ever measured at or above the 95th BMI percentile between Kindergarten and 3rd grade and between Kindergarten and 8th grade. The third is “consistent obesity” indicating prevalent obesity at kindergarten entry or incident obesity any time until 3rd grade and obesity at all waves following the first obese observation within that period.
We examined entrenched obesity from three perspectives. First, we measure the prevalence of and risk factors for entrenched obesity among the total population. Secondly, we estimate the risk of entrenched obesity among a set of kids who had even fleeting obesity between Kindergarten and 3rd grade. Thirdly, we show the risks of entrenched obesity among children with consistent obesity within the first four years of elementary school.
We calculated unadjusted and adjusted risk ratios from multivariable logistic regression models. To understand variation in children’s risks of entrenched obesity, models were adjusted for child’s sex (male, female), family socioeconomic status quintile in kindergarten, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Other), birthweight (<2500, 2500-3999, 4000+ grams), weight at kindergarten entry (normal weight [z-score<85th percentile], overweight [85th ≥z-score<95th percentiles] obesity [95th ≥z-score<99th percentiles] and severely obesity [the lower of BMI>120% of the 95th percentile or a BMI>35]) and BMI change during kindergarten, modeled as a continuous variable and reported as specific contrasts (e.g. -0.5, -0.25, 0.25, 0.5 relative to 0). Effect estimates for children with changes in BMI of −0.5 and +0.5 represent approximately the 25th and 75th percentile of change among all children. Z-scores are most appropriate for assessing children’s weight at 1 point in time, while BMI change is a better measure for assessing change in an individual child because the variability of z-scores is lower for the heaviest children;(27) results were consistent in alternative models using change in BMI z-score instead.
Analyses were conducted using SUDAAN 10.1 (Research Triangle Park, NC). The Institutional Review Board of Emory University reviewed this data analysis project prior to its commencement and determined it to be exempt.
Results
Timing and entrenchment of childhood obesity
Table 1 shows the timing and persistence of obesity between ages 5 and 14 years. Nearly three fourths (70.3%, 95% CI: 68.4–72.2) of children did not have obesity during the 9 years of follow-up. More than one in ten (12.2%, 95% CI: 8.9–15.5) children entered kindergarten obese and these children represent 55% of children who ever had obesity by age 14 years. Between kindergarten and 8th grade, less than 5% of children developed obesity between each study period.
Table 1.
Timing and persistence of obesity between ages 5 to 14 years in the U.S. 1998–2007
|
|
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weight pattern | Na | % of total | 95% CI | % among ever with obesity K- 3 | 95%CI | % entrenched obesityb. | 95%CI | % among ever with obesity K- 8 | 95%CI | ||||
|
|
|
||||||||||||
| Never had obesity | 4740 | 70.3 | 68.4 | 72.2 | 0.0 | 0.0 | |||||||
| Ever had obesity between K and 3rd grade | 1860 | 29.7 | 27.8 | 31.6 | 100.0 | 62.6 | 57.8 | 67.1 | |||||
| Entered obese in Kindergarten | 780 | 12.2 | 8.9 | 15.5 | 55.1 | 50.7 | 59.3 | 72.0 | 66.1 | 77.2 | 41.0 | 37.2 | 45.0 |
| Entered Kindergarten without obesity but developed obesity in kindergarten | 150 | 2.4 | 1.7 | 3.1 | 11.0 | 8.3 | 14.6 | 46.4 | 33.1 | 60.3 | 8.2 | 6.2 | 10.9 |
| Developed obesity between Kindergarten & 1st grade (age 6–7 years) | 170 | 2.6 | 2.0 | 3.2 | 11.8 | 9.4 | 14.9 | 62.0 | 50.3 | 72.5 | 8.8 | 7.0 | 11.1 |
| Developed obesity between 1st & 3rd grade (age 7–9 years) | 310 | 4.9 | 3.9 | 5.8 | 22.1 | 18.7 | 25.9 | 47.3 | 38.9 | 55.9 | 16.5 | 13.9 | 19.4 |
| Developed obeseity between 3rd & 5th grade (age 9–11 years) | 270 | 4.3 | 3.5 | 5.1 | 14.6 | 12.3 | 17.4 | ||||||
| Developed obesity between 5th & 8th grade (age 11–14 years) | 170 | 3.2 | 2.4 | 4.0 | 10.8 | 8.7 | 13.4 | ||||||
Data source: Early Childhood Longitudinal Study, Kindergarten Class of 1998–1999
N rounded to nearest ten per National Center for Educational Statistics guidelines
Having or developing obesity between kindergarten entry and 3rd grade (age 5.6–9.1 years) and retaining obesity between 5th nd 8th grades (age 11.1-14.1 years) (average age 14.1 years).
Among the 29.7% of children who ever experienced obesity between ages 5 and 9 years, 62.6% (95%CI: 57.8-67.1) experienced entrenched obesity, while only about a third returned to normal or overweight status. In particular, children who started school with obesity were most likely to experience entrenched obesity in adolescence (72%; 95% CI: 66.1–77.2), even compared to children who developed obesity subsequently during elementary school.
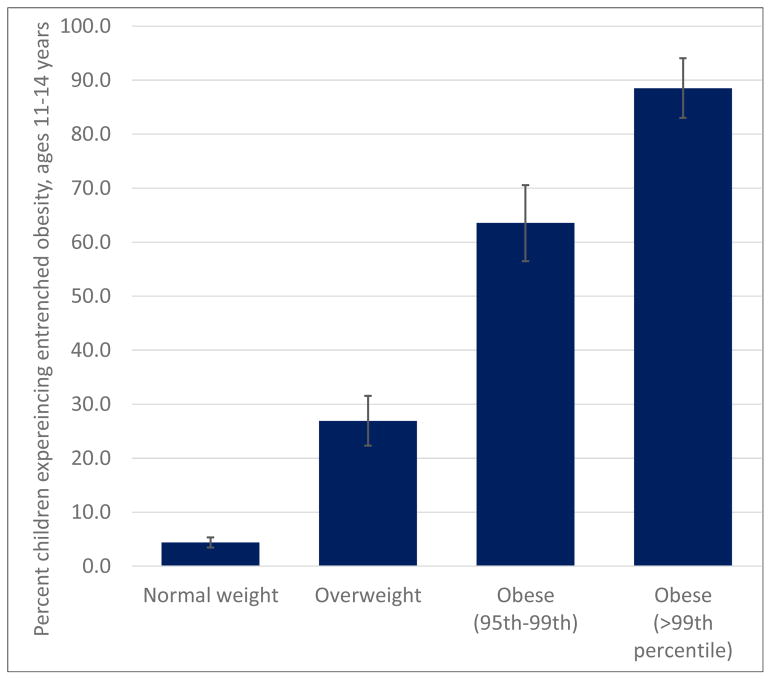
Prevalence of entrenched obesity was not only higher for kindergarteners with obesity, but increased steadily with kindergarten weight. Figure 1 shows the proportion of children experiencing entrenched obesity according to their weight at age 5 years. Only about 2.5% of normal-weight kindergarteners would experience entrenched obesity; the percentage experiencing entrenched obesity was 10 times higher among overweight compared with normal-weight kindergarteners. Among children with obesity at the 95th to 99th percentile, over 65% experienced entrenched obesity and among those with severe obesity at age 5 years, 93% would experience entrenched obesity.
Figure 1.
Percent of children experiencing entrenched obesity at ages 11–14 years, according to their weight category based on BMI z-score at age 5 years
Factors associated with entrenched obesity
Table 2 represents the prevalence of and risk factors for entrenched obesity in the entire cohort. Overall, 13.9% (95% CI: 12.6 –15.3) of children experienced entrenched obesity. The prevalence of entrenched obesity differed by child’s sex (15.2% of boys vs. 12.4% of girls), race and ethnicity (19.8% of Hispanic vs. 10.7% of Non-Hispanic white children), and socioeconomic status (17.5% of children from the middle quintile of families vs. 6.5% of children from the wealthiest quintile). The prevalence of entrenched obesity was highest among children who had been born large (20.9%); it affected 2.4% of children who were normal weight at kindergarten entry, 22.3% of those who were overweight, 65.3% of those who were obese, and 93% of those who were already severely obese at kindergarten entry.
Table 2.
| Prevalence Entrenched | Unadjusted | Adjusted | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Na | % | 95% CI | RR | 95% CI | RR | 95% CI | ||||
|
|
||||||||||
| Total Sample | 6600 | 13.9 | 12.6 | 15.3 | ||||||
| Race/ethnicity | ||||||||||
| NH White | 4200 | 10.7 | 9.3 | 12.3 | 1.00 | 1.00 | ||||
| NH Black | 630 | 17.0 | 12.8 | 22.2 | 1.59 | 1.15 | 2.21 | 1.70 | 1.00 | 2.89 |
| Hispanic | 1060 | 19.8 | 16.7 | 23.4 | 1.86 | 1.50 | 2.30 | 1.42 | 0.96 | 2.11 |
| Other | 720 | 17.3 | 12.4 | 23.6 | 1.62 | 1.14 | 2.31 | 1.26 | 0.82 | 1.96 |
| SES in kindergartenb | ||||||||||
| Q1 (lowest) | 850 | 16.6 | 13.6 | 20.0 | 2.55 | 1.81 | 3.59 | 1.54 | 0.98 | 2.43 |
| Q2 | 1090 | 17.0 | 13.6 | 20.9 | 2.61 | 1.79 | 3.82 | 1.47 | 0.89 | 2.43 |
| Q3 | 1290 | 17.5 | 14.2 | 21.4 | 2.70 | 1.94 | 3.77 | 2.26 | 1.45 | 3.53 |
| Q4 | 1380 | 12.0 | 9.3 | 15.4 | 1.85 | 1.26 | 2.72 | 1.56 | 1.01 | 2.42 |
| Q5 (highest) | 1740 | 6.5 | 4.8 | 8.7 | 1.00 | 1.00 | ||||
| Child sex | ||||||||||
| Male | 3290 | 15.2 | 13.4 | 17.3 | 1.23 | 1.01 | 1.51 | 1.34 | 0.95 | 1.90 |
| Female | 3310 | 12.4 | 10.6 | 14.4 | 1.00 | 1.00 | ||||
| Child birthweightb | ||||||||||
| <2500 grams | 440 | 12.3 | 8.9 | 16.8 | 0.95 | 0.69 | 1.32 | 1.21 | 0.77 | 1.92 |
| 2500–3999 grams | 5150 | 12.9 | 11.4 | 14.5 | 1.00 | 1.00 | ||||
| 4000+ grams | 800 | 20.9 | 16.4 | 26.2 | 1.62 | 1.23 | 2.14 | 0.90 | 0.57 | 1.42 |
| BMI category in Kindergarten | ||||||||||
| Normal weight | 4850 | 2.4 | 1.8 | 3.1 | 1.00 | 1.00 | ||||
| Overweight (85th – 95th percentile) | 970 | 22.3 | 18.2 | 27.0 | 9.33 | 6.54 | 13.31 | 10.47 | 7.27 | 15.08 |
| Obesity (95th %ile BMI≤120% of 95th %ile) | 510 | 65.3 | 58.3 | 71.7 | 27.37 | 20.88 | 35.87 | 31.40 | 24.13 | 40.85 |
| Severe obesity (BMI≥120% of 95th %ile or BMI>35) | 270 | 93.0 | 85.9 | 96.7 | 38.95 | 29.80 | 50.92 | 46.50 | 36.04 | 59.99 |
| BMI change from Wave 1-Wave2c | ||||||||||
| −0.5 vs 0 (smaller in W2 than W1) | 0.91 | 0.85 | 0.98 | 0.82 | 0.76 | 0.89 | ||||
| −0.25 vs 0 | 0.96 | 0.92 | 0.99 | 0.91 | 0.87 | 0.94 | ||||
| +0.25 vs0 | 1.05 | 1.01 | 1.08 | 1.10 | 1.06 | 1.15 | ||||
| +0.5 vs 0 (larger in W2 than W1) | 1.09 | 1.02 | 1.17 | 1.22 | 1.13 | 1.32 | ||||
N rounded to nearest 10 per National Center for Education Statistics guidelines
N for SES and birthweight to not sum to total sample because of missing information
BMI change is modeled as a continuous variable; effect estimates for children with changes in BMI of −0.5 and +0.5 represent approximately the 25th and 75th percentile of change among all children
Entrenched obesity calculated for the entire cohort
Having or developing obesity between kindergarten entry and 3rd grade (age 5.6–9.1 years) and retaining obesity between 5th nd 8th grades (age 11.1–14.1 years)
After adjusting for demographic, socioeconomic, and early life weight patterns (Table 2, Panel 3), Non-Hispanic Black children had 70% higher risks of entrenched obesity than non-Hispanic white children (95% CI: 1.00–2.89) and children from middle-income (third and forth quintile) families had significantly higher risks – 126% and 56% respectively - than those from the wealthiest (top quintile) families. The elevated risks of children who were large at birth were explained by childhood growth patterns.
The strongest predictor of entrenched obesity was weight at kindergarten entry– after all other observed characteristics were controlled for, overweight kindergarteners had more than 10 times (95% CI: 7.27–15.08) higher risk of entrenched obesity than their normal-weight classmates; children who came to kindergarten between the 95th and the 99th percentiles of weight were at over 30 times higher risk (95% CI: 24.13–40.85) and those at and above 120% of the 95th percentile had over 46 times (95% CI: 36.04–59.99) the risk of experiencing entrenched obesity.
Growth patterns during kindergarten were associated with entrenched obesity even after accounting for weight at kindergarten entry. Compared with children who stayed at the same BMI throughout their kindergarten year, those who lost even a modest amount of weight relative to height had lower risks of entrenched obesity, while those who gained weight for their height had increased risks of entrenched obesity. Specifically, children whose BMI decreased by 0.5 points between Fall and Spring of their kindergarten year had 18% lower risks (95% CI: 0.76–0.89) of entrenched obesity, while those whose BMI increased by 0.5 experienced 22% higher risks.
Table 3 focuses on children who had obesity early in life and therefore may have higher risk of entrenched obesity. First we show the prevalence of ever having experienced obesity in elementary or middle school, ages 5–14 years. Almost one third of children had obesity at one point between ages 5 and 14 years. A subset of them, 22.1% of the population, had obesity at one point between kindergarten and third grade, ages 5–9 years. About half of these children, 11.5% of the entire population, had consistent obesity at these ages, with incident obesity followed by persistent weight for height at or above the 95th percentile.
Table 3.
Associations between children’s characteristics and risks of entrenched obesity among children who had obesity in elementary schoold
| Prevalence of'ever obesity from K-8 (age 5.6–14.1 years) | Prevalence of ever obesity from K-3 (age 5.6–9.1 years) | Prevalence of 'consistent obesity' within K-3 (age 5.6– 9.1 years) | Adjusted relative risk of entrenched obesity among those with obesity ever within K-3e | Adjusted relative risk of entrenched obesity among children with obesity in kindergarten e | Adjusted relative risk of entrenched obesity among children with consistent obesity during K-3 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||||||||||
| Prevalence overall | 29.7 | 27.8 | 31.6 | 22.1 | 20.6 | 23.8 | 11.5 | 10.3 | 12.8 | 62.6f | 57.8 | 67.1 | 72g | 66.1 | 77.2 | 81.63h | 77.1 | 85.5 |
|
|
||||||||||||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||||||
|
|
|
|
|
|||||||||||||||
| Race/ethnicity | ||||||||||||||||||
| NH White | 25.5 | 23.4 | 27.8 | 18.8 | 16.9 | 20.8 | 9.0 | 7.6 | 10.5 | 1.00 | 1.00 | 1.00 | ||||||
| NH Black | 35.2 | 28.9 | 42.0 | 24.1 | 19.2 | 29.9 | 13.5 | 9.7 | 18.5 | 1.24 | 1.05 | 1.47 | 1.25 | 1.04 | 1.52 | 0.98 | 0.82 | 1.17 |
| Hispanic | 36.8 | 31.7 | 42.2 | 30.4 | 26.0 | 35.1 | 16.4 | 13.5 | 19.6 | 1.11 | 0.92 | 1.32 | 1.16 | 0.96 | 1.41 | 1.03 | 0.92 | 1.16 |
| Other | 33.4 | 27.3 | 40.2 | 24.1 | 19.2 | 29.8 | 14.6 | 10.1 | 20.7 | 1.19 | 0.99 | 1.42 | 1.16 | 0.93 | 1.43 | 1.08 | 0.96 | 1.21 |
| SES in kindergartenb | ||||||||||||||||||
| Q1 (lowest) | 34.7 | 30.1 | 39.6 | 24.7 | 20.9 | 29.0 | 11.4 | 9.1 | 14.1 | 1.21 | 0.91 | 1.60 | 1.31 | 0.97 | 1.77 | 1.08 | 0.93 | 1.25 |
| Q2 | 34.4 | 30.3 | 38.7 | 27.1 | 22.9 | 31.7 | 14.5 | 11.5 | 18.1 | 1.20 | 0.94 | 1.53 | 1.11 | 0.81 | 1.52 | 1.05 | 0.89 | 1.24 |
| Q3 | 35.5 | 31.1 | 40.3 | 25.6 | 21.7 | 29.9 | 14.9 | 11.8 | 18.6 | 1.36 | 1.09 | 1.70 | 1.36 | 1.04 | 1.77 | 0.97 | 0.85 | 1.12 |
| Q4 | 24.9 | 21.3 | 29.0 | 19.1 | 15.7 | 23.0 | 10.6 | 8.0 | 13.9 | 1.23 | 0.97 | 1.56 | 1.34 | 1.00 | 1.80 | 0.99 | 0.85 | 1.15 |
| Q5 (highest) | 19.6 | 16.3 | 23.3 | 14.1 | 11.6 | 17.1 | 6.0 | 4.4 | 8.1 | 1.00 | 1.00 | 1.00 | ||||||
| Child gender | ||||||||||||||||||
| Male | 31.6 | 29.2 | 34.1 | 22.7 | 20.5 | 25.0 | 12.3 | 10.5 | 14.2 | 1.19 | 1.03 | 1.37 | 1.03 | 0.91 | 1.17 | 1.10 | 0.99 | 1.21 |
| Female | 27.7 | 25.0 | 30.6 | 21.6 | 19.5 | 23.9 | 10.6 | 9.0 | 12.4 | 1.00 | 1.00 | 1.00 | ||||||
| Child birthweightb | ||||||||||||||||||
| <2500 grams | 23.8 | 18.8 | 29.7 | 17.24 | 12.99 | 22.52 | 11.9 | 8.4 | 16.5 | 1.13 | 0.95 | 1.35 | 1.11 | 0.90 | 1.38 | 1.03 | 0.91 | 1.18 |
| 2500–3999 grams | 28.7 | 26.5 | 31.0 | 21.03 | 19.39 | 22.76 | 10.4 | 9.1 | 11.7 | 1.00 | 1.00 | 1.00 | ||||||
| 4000+ grams | 40.9 | 34.4 | 47.7 | 33.46 | 27.08 | 40.50 | 18.6 | 13.8 | 24.5 | 0.88 | 0.73 | 1.07 | 0.97 | 0.78 | 1.20 | 1.01 | 0.90 | 1.13 |
| BMI category in Kindergarten | ||||||||||||||||||
| Normal weight | 13.4 | 11.8 | 15.3 | 5.76 | 4.71 | 7.03 | 1.2 | 0.8 | 1.8 | 1.00 | 1.00 | |||||||
| Overweight (85th - 95th percentile) | 51.7 | 45.9 | 57.4 | 38.44 | 33.31 | 43.84 | 16.0 | 12.1 | 20.7 | 1.43 | 1.06 | 1.93 | 1.13 | 0.85 | 1.49 | |||
| Obesity (95th %ile BMI≤120% of 95th %ile) 100.0 | 100.0 | 57.4 | 50.2 | 64.2 | 1.58 | 1.22 | 2.04 | 1.15 | 0.90 | 1.48 | ||||||||
| Severe obesity (BMI≥120% of 95th %ile or BMI>35) 100.0 | 100.0 | 97.7 | 91.5 | 99.4 | 2.22 | 1.74 | 2.84 | 1.34 | 1.02 | 1.75 | ||||||||
| BMI change from Wave 1-Wave2c | ||||||||||||||||||
| −0.5 vs 0 (smaller in W2 than W1) | 0.99 | 0.97 | 1.01 | 0.98 | 0.95 | 1.00 | 0.99 | 0.97 | 1.01 | |||||||||
| −0.25 vs 0 | 1.00 | 0.99 | 1.01 | 0.99 | 0.98 | 1.00 | 1.00 | 0.98 | 1.01 | |||||||||
| +0.25 vs0 | 1.00 | 0.99 | 1.01 | 1.01 | 1.00 | 1.02 | 1.00 | 0.99 | 1.02 | |||||||||
| +0.5 vs 0 (larger in W2 than W1) | 1.01 | 0.99 | 1.03 | 1.02 | 1.00 | 1.05 | 1.01 | 0.99 | 1.03 | |||||||||
N rounded to nearest 10 per National Center for Education Statistics guidelines
N for SES and birthweight to not sum to total sample because of missing information
BMI change is modeled as a continuous variable; effect estimates for children with changes in BMI of −0.5 and +0.5 represent approximately the 25th and 75th percentile of change among all children
Having or developing obesity between kindergarten entry and 3rd grade (age 5.6–9.1 years) and retaining obesity between 5th nd 8th grades (age 11.1–14.1 years)
Parameters are marginal conditional risk ratios not odds ratios because outcome is non-rare
Prevalence of entrenchment among those with ever-obesity from K-3
Prevalence of entrenchment among children with obesity in kindergarten
Prevalence of entrenchment among children with consistent obesity during K-3
Among children who ever experienced obesity between kindergarten and 3rd grade, 62.6% of them would experience entrenched obesity (95% CI: 57.8–67.1). Non-Hispanic Black children, children from middle-income families and boys who ever experienced obesity in early elementary school were more likely to experience entrenched obesity than Non-Hispanic whites, children from higher-income families and girls, respectively. Children who were overweight or obese at kindergarten entry, were more likely to continue obesity into adolescence than normal weight children: RR: 1.43 (95% CI: 1.06–1.93) for overweight, 1.58 for obesity (95% CI: 1.22–2.04) and 2.22 (95% CI: 1.74–2.84) higher for severe obesity. Among this high-risk group, weight losses or gains in elementary school were not associated with risks of entrenched obesity. Among children with ‘consistent obesity’—those with incident obesity followed by persistence at each subsequent wave—risk of entrenchment was 82%. Notably, among these children, there were no differences in risks of obesity among children according to their sex, race/ethnic, socioeconomic, or early growth.
Discussion
One third of children who entered kindergarten in 1998–1999 in the U.S. had obesity at some point during elementary or middle school. But is this an indicator of longer-term obesity? To understand this, we examined prolonged exposure to obesity during several critical years of development, which we call entrenched obesity, in a nationally representative sample of children.
We first showed risks of entrenched obesity in the overall population, an approach that is useful as a description of the epidemiology of obesity. In the general population, 14% of children experience entrenched obesity, having had obesity at least at 1 point between K-3rd grades that persisted in both 5th and 8th grades (mean ages 11.1 and 14.1 years). After adjusting for several characteristics, boys, children who were Non-Hispanic black, were from middle-income families, had entered school overweight or obese, and had had increases in weight during the first year of school were more likely to experience entrenched obesity.
Then, we showed risks of entrenched obesity among children who ever had obesity; an approach that is clinically informative in that knowledge about body weight at any single point-intime during early childhood could be translated into a measureable risk of longer-term obesity . Among children who had obesity in Kindergarten or who had even fleeting obesity during the subsequent 3 years, 72% and 63% of them respectively would have obesity through ages 11–14 years.
Risks of entrenched obesity were highest among children who had severe obesity in Kindergarten, 93% of whom would experience entrenched obesity. In addition, and also with clinical relevance, among those who had consistent obesity in elementary school, meaning that obesity was observed at multiple times until 3rd grade, 84% remained obese in both 5th and 8th grade. Risks were higher among those who developed obesity earlier rather than later in childhood. Together, these patterns indicate that childhood obesity is often not temporary - once a child developed obesity, the risk of continuing obesity is high.
In the general population, the risk of entrenched obesity is associated with race, ethnicity, sex and socioeconomic status. However, among children who had already experienced obesity, the risk of entrenched obesity did not differ across race, ethnicity, gender, and socio-economic status.
Weight change early in childhood was correlated with longer-term weight trajectories in the overall population: compared with children who stayed at the same BMI throughout kindergarten, those whose BMI decreased between entering kindergarten in the Fall and finishing kindergarten the following Spring had lower risks of entrenched obesity, while those who gained BMI points had higher risk. However, such increases and decreases in BMI were not associated with entrenched obesity among the children who had already experienced obesity early in their middle-school years. Further, it may not be clinically feasible or recommended for children with severe obesity to move down to normal weight or overweight categories at these ages; thus, a child above the 95% percentile would be at a very high risk of continuing to have obesity for several years. A useful step for future research will be to characterize weight loss patterns in early childhood, distinguishing intentional weight loss from changes due to patterns of maturation and growth or illness. Identifying successful strategies used in intentional weight loss can also be useful to parents and pediatricians. It will be important for future studies to explore longer-term implications of weight changes in large representative samples of children.
Our estimates are consistent with previous studies indicating that weight trajectories are established early in childhood,(28, 29) that obesity even in childhood is difficult to reverse,(30, 31) and that children with obesity seldom reach normal weight.(32) For example, parents of children with obesity either recalled their child always having obesity or developing obesity by age 5 years.(29) In Australia, 5-10 year-olds with overweight or obesity had 25 times and 240 times higher odds respectively of having overweight or obesity 3 years later than children with normal-weight.(28) In Greenland, over half of children who had overweight or obesity at school entry styed in that weight category into adolescence and only 10% of those who had obesity at school entry reached normal weight in adolescence.(10) In three US metropolitan areas, 65% of fifth graders with obesity retained obesity through tenth grade.(33) This study strengthened the literature by providing evidence from a large nationally representative prospective cohort of U.S. children with multiple anthropometric measures throughout middle childhood.
This study has certain limitations. We did not have information on weight between birth and kindergarten or after 8th grade, so we cannot map the entire trajectory of obesity, nor identify the age at which children who entered kindergarten with overweight or obesity had developed overweight or obesity. Lack of data before and after a period of observation is common in studies of disease incidence.(34) The cohort to which this study pertains is representative of children who were in kindergarten in 1998-99 and may not reflect the experiences of earlier or later cohorts. Still, this cohort is of particular interest because they were growing up during the 1990s and 2000s, when obesity became a major health concern.
Other studies have documented relationships between children’s environments, beverage and food intake, and physical activity and obesity.(16, 35-40) After accounting for these, previous weight continues to be a major explanatory factory, so the focus of this research has been on understanding weight trajectories rather than on the environmental or behavioral exposure that may be linked to those trajectories.
This study was only able to follow children to the age of 14 and we cannot speak to what happens thereafter. Other studies have indicated that individuals who experience obesity in childhood are more likely to experience obesity in adulthood, but representative data on recent cohorts are very limited. In addition, the long-term trajectories of individuals who did not experience obesity in childhood may also involve obesity later. While children who are heavy early in life are at greatest risk of developing obesity, others do develop obesity for the first time in adolescence and adulthood, resulting in an increasing prevalence of obesity as a cohort ages. Nationally representative U.S. data from a study following youth from High School into adulthood found major increases in obesity levels from adolescence to the 2nd and 3rd decades of life, especially among people of color and women (13, 41). While many individuals who were normal weight in childhood develop overweight or obesity in adulthood (12-15), few who had overweight or obesity eventually reached normal weight.(12, 13, 41)
From a clinical perspective, weight status at school entry and change in weight during the following year may be a combination of measurable factors that can predict risk of long-term obesity: observing a child with obesity when they enter school and continuing to gain weight during the kindergarten year may be a red flag. The risk of entrenchment is somewhat lower among children who develop obesity in later grades, but is still substantial.
Conclusions
Obesity with onset during the preschool or elementary school years is generally not a transient phenomenon, but one that portends risk for long-term obesity, at least into adolescence. Among children with early onset of obesity, the majority are affected by entrenched obesity, regardless of sex, race, ethnicity, and socioeconomic status.
Acknowledgments
Funding M. Kramer’s collaboration on this project was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development Award Number K01HD074726. K.M. Venkat Narayan was partly supported by the National Institute of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number P30DK111024.The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Solveig A. Cunningham, Hubert Department of Global Health, Emory University 1518 Clifton Road; Atlanta, GA 30322 USA.
Ashlesha Datar, Center for Economic and Social Research, University of Southern California 635 Downey Way, Los Angeles, CA 90089 USA.
K.M. Venkat Narayan, Hubert Department of Global Health, Emory University 1518 Clifton Road; Atlanta, GA 30322 USA.
Michael R. Kramer, Department of Epidemiology, Emory University 1518 Clifton Road; Atlanta, GA 30322 USA.
References
- 1.Cunningham SA, Kramer MR, Narayan K. Incidence of childhood obesity in the United States. New England Journal of Medicine. 2014;370:401–9. doi: 10.1056/NEJMc1402397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fagot-Campagna A, Narayan KMV, Imperatore G. Type 2 diabetes in children. BMJ 2001. 2001 Feb 17;322(7283):377–8. doi: 10.1136/bmj.322.7283.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Must A, Anderson SE. Effects of Obesity on Morbidity in Children and Adolescents. Nutrition in Clinical Care. 2003;6(1):4–12. [PubMed] [Google Scholar]
- 4.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998 Mar;101(3 Pt 2):518–25. [PubMed] [Google Scholar]
- 5.Goldhaber-Fiebert JD, Rubinfeld RE, Bhattacharya J, Robinson TN, Wise PH. The utility of childhood and adolescent obesity assessment in relation to adult health. Med Decis Making. 2013;33(2):163–75. doi: 10.1177/0272989X12447240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo S, Huang C, Maynard L, Demerath E, Towne B, Chumlea W, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. International Journal of Obesity and Related Metabolic Disorders. 2000;24(12):1628–35. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 7.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. The American journal of clinical nutrition 2002. 2002 Sep 1;76(3):653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 8.Wang LY, Chyen D, Lee S, Lowry R. The association between body mass index in adolescence and obesity in adulthood. J Adolescent Health. 2008 May;42(5):512–8. doi: 10.1016/j.jadohealth.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Dubois L, Girard M. Early determinants of overweight at 4.5 years in a population-based longitudinal study. International journal of obesity. 2006 Apr;30(4):610–7. doi: 10.1038/sj.ijo.0803141. [DOI] [PubMed] [Google Scholar]
- 10.Niclasen BV, Petzold MG, Schnohr C. Overweight and obesity at school entry as predictor of overweight in adolescence in an Arctic child population. Eur J Public Health. 2007 Feb;17(1):17–20. doi: 10.1093/eurpub/ckl246. [DOI] [PubMed] [Google Scholar]
- 11.Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring) 2007 Mar;15(3):760–71. doi: 10.1038/oby.2007.585. [DOI] [PubMed] [Google Scholar]
- 12.Wright CM, Emmett PM, Ness AR, Reilly JJ, Sherriff A. Tracking of obesity and body fatness through mid-childhood. Archives of Disease in Childhood. 2010 Aug;95(8):612–7. doi: 10.1136/adc.2009.164491. [DOI] [PubMed] [Google Scholar]
- 13.Gordon-Larsen P, The NS, Adair LS. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity (Silver Spring) 2010 Sep;18(9):1801–4. doi: 10.1038/oby.2009.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity. 2009;4(4):281–8. doi: 10.3109/17477160802596171. [DOI] [PubMed] [Google Scholar]
- 15.Williams S. Overweight at age 21: the association with body mass index in childhood and adolescence and parents' body mass index. A cohort study of New Zealanders born in 1972–1973. International journal of obesity. 2001 Feb;25(2):158–63. doi: 10.1038/sj.ijo.0801512. [DOI] [PubMed] [Google Scholar]
- 16.Stuart B, Panico L. Early-childhood BMI trajectories: evidence from a prospective, nationally representative British cohort study. Nutrition & diabetes. 2016 Mar 07;6:e198. doi: 10.1038/nutd.2016.6. Epub 2016/03/08. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarke WR, Lauer RM. Does childhood obesity track into adulthood? Critical Reviews in Food Science and Nutrition 1993. 1993 Jan 01;33(4–5):423–30. doi: 10.1080/10408399309527641. [DOI] [PubMed] [Google Scholar]
- 18.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997 Sep 25;337(13):869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 19.Srinivasan SR, Bao W, Wattigney WA, Berenson GS. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: The Bogalusa Heart Study. Metabolism. 1996 Feb;45(2):235–40. doi: 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 20.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do Obese Children Become Obese Adults? A Review of the Literature. Preventive Medicine. 1993;22(2):167–77. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 21.Tourangeau K, Lê T, Nord C, Sorongon AG. Early Childhood Longitudinal Study, Kindergarten Class of 1998–99 (ECLS-K), Eighth-Grade Methodology Report (NCES 2009–003) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2009. [Google Scholar]
- 22.Bose J, West J. Examining additional nonresponse bias introduced through attrition. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- 23.U.S. Department of Education - National Center for Education Statistics. User's manual for the ECLS-K Base Year Public-Use Data Files and Electronic Codebook: NCES 2001-029 (revised) Washington, DC: Author; 2004. [Google Scholar]
- 24.Vidmar S, Caelin J, Hesketh K, Cole TJ. Standardizing anthropometric measures in children and adolescents with niew functions for egen. The Stata Journal. 2004;4(1):50–5. [Google Scholar]
- 25.Lytle LA, Seifert S, Greenstein J, McGovern P. How do children's eating patterns and food choices change over time? Results from a cohort study. Am J Health Promot. 2000 Mar-Apr;14(4):222–8. doi: 10.4278/0890-1171-14.4.222. Epub 2000/08/01. eng. [DOI] [PubMed] [Google Scholar]
- 26.Suchindran C, North K, Popkin B, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–7. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cole T, Faith M, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? European Journal of Clinical Nutrition. 2005;59:419–25. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- 28.Hesketh K, Wake M, Waters E, Carlin J, Crawford D. Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public health nutrition. 2004 Apr;7(2):303–9. doi: 10.1079/phn2003537. [DOI] [PubMed] [Google Scholar]
- 29.Franzese A, Valerio G, Argenziano A, Esposito-Del Puente A, Iannucci MP, Caputo G, et al. Onset of obesity in children through the recall of parents: relationship to parental obesity and life events. J Pediatr Endocrinol Metab. 1998 Jan-Feb;11(1):63–7. doi: 10.1515/JPEM.1998.11.1.63. [DOI] [PubMed] [Google Scholar]
- 30.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2008 Sep;9(5):474–88. doi: 10.1111/j.1467-789X.2008.00475.x. Epub 2008/03/12. eng. [DOI] [PubMed] [Google Scholar]
- 31.Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Clinical review: behavioral interventions to prevent childhood obesity: a systematic review and metaanalyses of randomized trials. The Journal of clinical endocrinology and metabolism. 2008 Dec;93(12):4606–15. doi: 10.1210/jc.2006-2411. Epub 2008/09/11. eng. [DOI] [PubMed] [Google Scholar]
- 32.Hernandez RG, Marcell AV, Garcia J, Amankwah EK, Cheng TL. Predictors of Favorable Growth Patterns During the Obesity Epidemic Among US School Children. Clinical pediatrics 2015. 2015 May 1;54(5):458–68. doi: 10.1177/0009922815570579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schuster MA, Elliot MN, Bogart LM, Klein DJ, Feng JY, Wallander JL, et al. Changes in Obesity Between Fifth and Tenth Grades: A Longitudinal Study in Three Metropolitan Areas. Pediatrics. 2014;134(6):1051–8. doi: 10.1542/peds.2014-2195. Epub November 10, 2014. [DOI] [PubMed] [Google Scholar]
- 34.Kleinbaum D, Klein M. Survival Analysis: A self-learning text. 2. New York: Springer; 2005. [Google Scholar]
- 35.Shah PM, Sudharsanan N, Cunningham SA. Before-school and after-school childcare and children's risk of obesity. Pediatric obesity. 2017 Feb;12(1):58–66. doi: 10.1111/ijpo.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Galaviz KI, Zytnick D, Kegler MC, Cunningham SA. Parental Perception of Neighborhood Safety and Children's Physical Activity. Journal of physical activity & health. 2016 Oct;13(10):1110–6. doi: 10.1123/jpah.2015-0557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oza-Frank R, Zavodny M, Cunningham SA. Beverage displacement between elementary and middle school, 2004–2007. Journal of the Academy of Nutrition and Dietetics. 2012 Sep;112(9):1390–6. doi: 10.1016/j.jand.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cunningham SA, Zavodny M. Does the sale of sweetened beverages at school affect children's weight? Social science & medicine. 2011 Nov;73(9):1332–9. doi: 10.1016/j.socscimed.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nicosia N, Shier V, Datar A. The Role of School Environments in Explaining Racial-Ethnic Disparities in Body Mass Index Among U.S. Adolescents. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2016 Aug;59(2):215–21. doi: 10.1016/j.jadohealth.2016.04.018. Epub 2016/06/15. eng. [DOI] [PubMed] [Google Scholar]
- 40.Shier V, Nicosia N, Datar A. Neighborhood and home food environment and children's diet and obesity: Evidence from military personnel's installation assignment. Social science & medicine. 2016;158:122–31. doi: 10.1016/j.socscimed.2016.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. American Journal of Clinical Nutrition. 2004 Sep;80(3):569–75. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]