Abstract
Objective
Theoretical models offer valuable insights for designing effective and sustainable behavioral health interventions, yet the application of theory for informing digital technology interventions for people with mental illness has received limited attention. We offer a perspective on the importance of applying behavior theories and models to developing digital technology interventions for addressing mental and physical health concerns among people with mental illness.
Methods
In this commentary, we summarize prominent theories of human behavior, highlight key theoretical constructs, and identify opportunities to inform digital health interventions for people with mental illness. We consider limitations with existing theories and models, and examine recent theoretical advances that can specifically guide development of digital technology interventions
Results
Established behavioral frameworks including Health Belief Model, Theory of Planned Behavior, Transtheoretical Model, and Social Cognitive Theory consist of important and overlapping constructs that can inform digital health interventions for people with mental illness. As digital technologies continue to evolve and enable longitudinal data collection, real-time behavior monitoring, and adaptive features tailored to users’ changing needs over time, there are new opportunities to broaden our understanding of health behaviors and mechanisms of behavior change. Recent advances include dynamic models of behavior, Persuasive System Design, the Behavioral Intervention Technology model, and behavioral models for Just-In-Time Adaptive Interventions.
Conclusions and Implications for Practice
Behavior theories offer advantages for guiding use of digital technologies. Future research must explore how theoretical models can effectively advance efforts to develop, evaluate, and disseminate digital health interventions targeting individuals with mental illness.
Keywords: mental illness, digital technology, behavior change, theory, model
Introduction
Each year in the United States nearly 1 in 5 adults experiences mental illness and about 4% live with a serious mental illness (Hedden, Kennet, Lipari, Medley, & Tice, 2015). The societal impact of mental illness is substantial, as reflected by lost productivity, disproportionate rates of homelessness, and dramatically reduced life expectancy compared to the general population (Folsom et al., 2005; Greenberg, Fournier, Sisitsky, Pike, & Kessler, 2015; Kessler et al., 2008; Walker, McGee, & Druss, 2015). People with mental illness experience elevated burden of co-occurring chronic medical conditions due to poor lifestyle behaviors, cardiometabolic effects of psychiatric medications, high rates of obesity and tobacco use, and increased risk of substance use (McGinty, Baller, Azrin, Juliano-Bult, & Daumit, 2016). Efforts to treat and prevent both mental and physical health concerns affecting people with mental illness represent an urgent public health priority.
In 2014, the Substance Abuse and Mental Health Services Administration (SAMHSA) estimated that fewer than half of the 43.6 million Americans with a mental illness received treatment (Hedden et al., 2015). This significant treatment gap can be attributed to a variety of societal, economic, and individual factors. Some people with mental illness may be reluctant to seek care due to societal stigma and fear of discrimination (Corrigan, 2004), while others face structural and economic barriers to obtaining care due to extreme poverty, poor housing, and few options for transportation (Hert et al., 2011). Mental health symptoms can also interfere with obtaining necessary care by negatively impacting motivation, functioning, and one’s ability to adhere to recommended treatment regimens (Hert et al., 2011). Among those who do have access to care, it can be highly variable and of poor quality (Druss, 2007). Studies have documented that people with mental illness are less likely to receive screening for common cancers, timely diagnoses and treatment of diabetes, and recommendations to seek routine preventative care for cardiovascular disease (Druss, 2007).
Digital technologies, such as mobile devices, smartphone applications, wearable technology, and remote sensors, may afford new opportunities to bridge the significant gap towards addressing the mental and physical health needs of people with mental illness. Rates of mobile device ownership among people with mental illness, including schizophrenia or bipolar disorder, are comparable with the general population (Firth et al., 2015; Glick, Druss, Pina, Lally, & Conde, 2015; Naslund, Aschbrenner, & Bartels, 2016a). Reviews have also highlighted the effectiveness of smartphone applications for reducing symptoms of depression or anxiety (Donker et al., 2013), supporting illness self-management and relapse prevention among people with schizophrenia (Alvarez-Jimenez et al., 2014), and promoting treatment adherence and retention in care among individuals receiving services through community mental health settings (Naslund, Marsch, McHugo, & Bartels, 2015). As digital technologies continue to evolve, it may be possible to scale efforts targeting the treatment and management of debilitating psychiatric symptoms among people with mental illness while simultaneously addressing harmful health behaviors that disproportionately impact this group, such as high rates of smoking, physical inactivity, poor diet, and chronic medical conditions.
As researchers and clinicians work to develop cutting edge digital technology interventions to promote the mental and physical health of people with mental illness, theories of human behavior should play a critical role in guiding these efforts. Numerous studies have shown that interventions informed by theories of human behavior are more effective compared to interventions not informed by theory (Glanz & Bishop, 2010). Despite advantages of applying theory to intervention development, few interventions using digital technologies to target health behaviors such smoking, weight loss, treatment adherence, and chronic illness management were guided by behavior theories (Riley et al., 2011). Concerns have been raised that new technologies may be driving the development of digital health interventions as opposed to drawing from theories of human behavior to inform this work (Glanz, Rimer, & Viswanath, 2008). Researchers have also called for new theoretical approaches to guide the use of digital technologies that enable intensive longitudinal data collection, tailoring to subjects’ specific needs, or delivering targeted feedback or prompts in response to changing conditions (Riley et al., 2011; Spruijt-Metz, Hekler, et al., 2015; Spruijt-Metz & Nilsen, 2014).
In this commentary, we offer a perspective on the importance of applying theories of human behavior to the development and dissemination of digital health interventions for mental disorders. Our aim is to provide mental health researchers with a practical overview of relevant theories that could inform future digital technology interventions for targeting mental and physical health concerns among people with mental illness. We begin by reviewing prominent theories of human behavior and by highlighting key constructs of these theories. Next, we consider limitations with these theories and examine recent theoretical advances that can specifically inform digital technology interventions for people with mental illness. We conclude by discussing how emerging behavior theories may play a central role in guiding future efforts.
Health Behavior Theories
Research shows that interventions informed and guided by behavior theories are more effective compared to those that are not (Glanz & Bishop, 2010). Theory affords a conceptual framework for illustrating causal processes or key constructs hypothesized to influence or change a target behavior (Glanz et al., 2008; Michie, Johnston, Francis, Hardeman, & Eccles, 2008). Theory suggests mechanisms for changing behavior, provides a foundation for developing, implementing, and evaluating behavior change interventions, and can keep empirical research and implementation efforts clearly focused (Crosby, Kegler, & DiClemente, 2002; Glanz et al., 2008). Theory can guide the interpretation of study findings and can allow researchers to conclude whether an intervention worked as intended (Glanz et al., 2008).
To date, few digital technology interventions have been informed by behavior theories or models (Bull & Ezeanochie, 2016; Riley et al., 2011). Highlighting the key constructs of important behavior theories could assist mental health services researchers in planning and guiding the development and delivery of interventions using emerging digital technologies. We summarize key constructs of the following prominent theories: 1) Health Belief Model; 2) Theory of Planned Behavior; 3) Transtheoretical Model; and 4) Social Cognitive Theory. These four theories, as illustrated in Table 1, are among the most widely cited models of health behavior, and have been used extensively to guide successful interventions targeting behaviors including lifestyle habits, chronic disease self-management, coping with mental health symptoms, and health service utilization (Glanz et al., 2008). These theories have also been specifically used to inform interventions for people with mental illness.
Table 1.
The role of existing behavior theories and models for informing digital health interventions
| Theoretical Model | Definition | How digital health interventions could support behavior change |
|---|---|---|
| Health Belief Model | Health behaviors are explained based on perceived susceptibility, perceived severity, perceived benefits of taking action, perceived barriers to taking action, and ability to take action. | Promote awareness about risks or benefits, deliver prompts or reminders for engaging in healthy behaviors, and provide encouragement or training to build confidence. |
| Theory of Planned Behavior | Behavioral intention and attitudes towards the behavior, beliefs about how others view the behavior, and perceived behavioral control are key determinants of performing a health behavior. | Use prompts and motivation strategies to support behavioral intention, and increase ability by building self-efficacy through encouragement and skill building. |
| Transtheoretical Model | Behavior change is conceptualized as progressing through 6 stages: 1) Precontemplation; 2) Contemplation; 3) Preparation; 4) Action; 5) Maintenance; and 6) Termination. | Tailor interventions to specific stages of readiness, use processes of change activities to support progression through the stages, and use techniques to build self-efficacy and avoid temptation. |
| Social Cognitive Theory | Behavior is determined by an individual’s social context and is influenced by personal factors, behavioral factors, and environmental factors. Self-efficacy is a key construct. | Support efforts to increase self-efficacy through mastery experiences, social modeling, improving physical and emotional states, and verbal or social persuasion. |
1) Health Belief Model
The Health Belief Model explains behavior by focusing on individuals’ beliefs and attitudes. Confidence in one’s ability to take action, referred to as self-efficacy, is also a key predictor of initiating or adopting the behavior (Baranowski, Cullen, Nicklas, Thompson, & Baranowski, 2003). If people believe that: they are at risk for a condition or that the condition is serious; acting on this would be effective in either reducing their risk or illness severity; the benefits of taking action outweigh potential barriers or costs; and they have the ability to take action (self-efficacy), then they will be likely to take action to reduce their risk or illness severity (Champion & Skinner, 2008). It is also posited that a stimulus, or cue to action, must be present to trigger engaging in the behavior. Cues to action are operationalized as strategies to prompt or instigate behavior and can come from social, environmental, or individual-level stimuli (Champion & Skinner, 2008). Among people with mental illness, the Health Belief Model has been used widely to inform medication adherence interventions (Valenstein et al., 2011), to conceptualize how mental illness stigma acts as a barrier to seeking care (Corrigan & Rüsch, 2002), and to guide the use of goal setting and lifestyle changes for reducing cardiovascular risk and psychiatric symptoms (Kilbourne et al., 2014).
2) Theory of Planned Behavior
The Theory of Planned Behavior emphasizes the role of behavioral intention as a determinant of performing a behavior (Montano & Kasprzyk, 2008). An individual’s behavioral intention is directly influenced by their attitudes towards the behavior (e.g., the belief that the likelihood of performing the behavior will have the expected outcome), their subjective norms (e.g., the view that other important individuals will approve or disapprove of the behavior) and the social norms associated with the behavior (e.g., belief about whether other important individuals will perform the behavior) (Montano & Kasprzyk, 2008). Together, motivation (i.e., an individual’s behavioral intention) and ability (i.e., an individual’s self-efficacy or perceived control over outside factors) are key determinants of performing the behavior (Ajzen, 1991). The Theory of Planned Behavior has been used to explain participation in daily activities such as housework, meal preparation, or taking medications among people with schizophrenia (Mausbach et al., 2013), and to inform programs to motivate people with serious mental illness to quit smoking (Brunette et al., 2011).
3) Transtheoretical Model
The Transtheoretical Model uses stages to illustrate how an individual’s decision-making occurs over time through a cyclical process (Prochaska, Redding, & Evers, 2008). Individuals move through six stages of behavior change: 1) Precontemplation: no intention to change behavior within the near future. Individuals may have limited awareness of the harms of their behavior, or may be demoralized due to numerous failed attempts to change. Individuals at this stage often appear resistant to change, unmotivated, and avoidant. 2) Contemplation: intention to change behavior within the near future. Individuals are aware of the harms of their behavior and understand the benefits of changing but can remain in this stage for long periods of time as they weigh pros and cons of making a change. 3) Preparation: intention to change behavior in the present. Individuals may have already started taking action, such as talking to their physician, joining a health education class or program, or buying a self-help book. 4) Action: behavior changes have already been made in recent months. Individuals have modified their problem behavior or adopted healthier behaviors, and they intend to keep making more changes going forward. 5) Maintenance: meaningful behavior changes sustained over several months with emphasis on preventing relapse. Individuals need to build confidence to continue behavior changes and to avoid relapse to earlier stages over the long term. 6) Termination: no temptation to relapse and to return to unhealthy behaviors.
Core constructs of the Transtheoretical Model illustrate the adoption and maintenance of health behaviors over time. For example, there are processes of change representing activities to support progression through the stages. These include obtaining social support for behavior change, increasing awareness about the harms and benefits of behavior change, learning about alternative behaviors, and finding strategies to manage or avoid cues for problem behaviors (Prochaska et al., 2008). Decisional balance, another core construct of the model, refers to how an individual assesses the benefits of a decision relative to the downsides. Lastly, self-efficacy reflects an individual’s confidence or ability to perform a behavior and to avoid relapse, whereas temptation accounts for urges to perform problem behaviors (Prochaska et al., 2008). Among people with mental illness, the Transtheoretical Model has been used to support psychiatric symptom management using stages of recovery (Andresen, Caputi, & Oades, 2006; Leamy, Bird, Le Boutillier, Williams, & Slade, 2011), tailor smoking cessation programs (Hickman, Delucchi, & Prochaska, 2015), and inform healthy lifestyle interventions (Park, Usher, & Foster, 2011).
4) Social Cognitive Theory
Social Cognitive Theory illustrates behavior change as occurring in the context of interactions between personal factors (e.g., an individual’s past experiences), behavioral factors (e.g., how an individual responds to external or internal stimuli), and environmental factors (e.g., how an individual perceives the external social context) (McAlister, Perry, & Parcel, 2008). The theory emphasizes several key determinants of behavior (McAlister et al., 2008). For example, outcome expectations are an individual’s beliefs about the outcome that might result from performing a behavior and the perceived value of that outcome. Similarly, social outcomes expectations consider an individual’s beliefs about how other people will evaluate them if they perform a behavior and how other people value the outcomes of that behavior. Self-evaluative outcomes expectations refer to an individual’s beliefs about how they will feel about themselves if they decide to perform a certain behavior. And, self-efficacy, the construct for which Social Cognitive
Theory is most widely known, consists of an individual’s confidence in their own ability to perform a behavior (Bandura, 1998). Self-efficacy is influenced by individuals’ past experiences, perceptions of their environment and social context, and their intellectual and physical capabilities (McAlister et al., 2008).
The application of Social Cognitive Theory for health behavior change has focused predominantly on increasing self-efficacy (Bandura, 1998). Four underlying behavioral mechanisms of the theory can be leveraged to increase self-efficacy (Bandura, 1998; McAlister et al., 2008). First, mastery experience involves providing an individual with ample opportunities to succeed, using small and easily mastered steps, followed by increasingly challenging tasks related to the desired behavior, which will gradually build their self-efficacy. Second, social modeling involves showing individuals that others like them can succeed through sustained efforts. Observing others who are successful can transfer knowledge such as skills and strategies. Third, improving physical and emotional states describes how mood influences an individual’s perceived self-efficacy. For example, improving mood by reducing stress and depression are beneficial before attempting a new behavior. Lastly, verbal or social persuasion refers to encouraging an individual and letting them know that they have the ability to perform the behavior, which can increase confidence and promote greater sustained effort to change. Social Cognitive Theory has informed numerous interventions for people with mental illness, including skills training (Patterson et al., 2006) and diabetes management and education (McKibbin et al., 2006) programs for middle-aged and older adults with schizophrenia, and lifestyle interventions for obese adults with serious mental illness (Aschbrenner, Naslund, & Bartels, 2016; Aschbrenner, Naslund, Shevenell, Mueser, & Bartels, 2016; Vazin et al., 2016).
Theoretical Advances
Few digital health interventions are informed by theory, which may be attributable to limitations with existing theories. Many theories have regarded human behavior as linear or static in nature, and as a result may not recognize that behavior is dynamic and ever changing in response to diverse social, biological, or environmental stimuli (Spruijt-Metz, Hekler, et al., 2015; Spruijt-Metz, Nilsen, Pavel, & Adibi, 2015). To date, theories have focused predominantly on between-person differences in behavior, yet digital technologies afford new opportunities to explore within-person differences in behavior through intensive collection of individual-level data using mobile devices, wearable sensors, continuous monitoring, or mapping digital footprints of online activities (Riley et al., 2011). Behavior theories must shift towards understanding within-person momentary differences in behavior, such as how an individual’s behavior responds to changing stimuli or context in real-world settings, in order to explore the mechanisms of behavior change and to inform how interventions can effectively promote adoption or maintenance of positive health behaviors (Spruijt-Metz, Hekler, et al., 2015; Spruijt-Metz & Nilsen, 2014).
This is not to suggest that existing behavior theories be discarded, because many key constructs of these theories are relevant even if the medium for delivering interventions continues to evolve rapidly. Most importantly, theory can inform more effective digital health interventions capable of achieving better outcomes (Riley, 2015), and therefore may be instrumental in advancing efforts to leverage digital technologies for targeting mental and physical health concerns among people with mental illness. Digital technologies could also help with advancing theories of human behavior by generating opportunities to test mediators of change, to illustrate causal mechanisms, and to identify the most potent intervention components (Riley, 2015). This is especially important as health behavior theories have remained largely unchanged over recent decades, because there have been few efforts by the developers of these theories to integrate new knowledge or to make necessary adaptations as new delivery platforms become available (Brewer & Rimer, 2008). In the sections that follow, we highlight four recent advances in the use of theory to guide the development of digital health interventions: 1) Dynamic Models of Behavior; 2) Persuasive System Design; 3) The Behavioral Intervention Technology Model; and 4) Behavior Models for Just-in-Time Adaptive Interventions. We selected these emerging behavioral models, as summarized in Table 2, because leading behavioral health researchers are actively working to refine these models for understanding the mechanisms of behavior change. There may be important opportunities for these theoretical models to inform digital health interventions targeting individuals with mental illness.
Table 2.
Emerging theoretical models for informing digital health interventions
| Theoretical Model | Definition | How digital health interventions could support behavior change |
|---|---|---|
| Dynamic Models of Behavior | Conceptualizes behaviors in real time and in response to constantly changing environmental, social, and biological stimuli by leveraging intensive individual-level data. | Adapt to an individual’s changing internal and external conditions throughout the day, inform immediate and momentary responses, and illustrate mechanisms of behavior change. |
| Persuasive System Design | Framework to recognize specific content, design, software, and functionality requirements so that a technology-based intervention can effectively change health behaviors. | Create user friendly interface with tailored content, support interactivity through feedback and reminders, and persuade users by facilitating cooperation and competition with other users. |
| Behavioral Intervention Technology Model | Defines both conceptual and technical aspects of a technology intervention in order to guide why, what, how, and when an intervention is delivered to a target population or individual. | Formalize the design, development, and delivery of digital technology-based behavioral health interventions by illustrating relationships between different conceptual and technical aspects of the intervention. |
| Behavior Models for Just-in-Time Adaptive Interventions | Provide timely treatments or tailored content to support an individual’s behavioral health goals by adapting seamlessly to their needs as they change over time. | Leverage real-time data about an individual’s context, behaviors, and location at a precise moment to deliver content when the individual is in a state of vulnerability and receptivity. |
1) Dynamic Models of Behavior
Dynamic models of behavior expand on existing theoretical frameworks by incorporating a time dimension to conceptualize human behaviors in real-time and in response to constantly changing environmental, social, and biological stimuli (Spruijt-Metz & Nilsen, 2014). Digital technologies afford powerful techniques to collect vast amounts of data in real time and continuously throughout the day, and advances in computational and mathematical modeling make it possible to analyze these data to more fully capture the complexities of human behavior. A key aspect of dynamic models is the ability to adapt to an individual’s changing internal and external conditions throughout the day to support immediate and momentary responses necessary to effect the behavior change of interest (Spruijt-Metz & Nilsen, 2014). Because digital technologies such as mobile devices allow increasingly sophisticated and intensive data collection techniques, computational models derived from the engineering and computer sciences may enable real time data analyses to illustrate behavior change processes over time and to identify the optimal moment when, where, and how often, to deliver specific intervention components (Riley et al., 2011). Dynamic models of behavior hold promise for illustrating mechanisms of behavior change by mapping how stimuli or inputs at a specific moment may influence subsequent behaviors at later points in time. As such, they can guide the development and delivery of interventions tailored to the needs and preferences of each individual (Spruijt-Metz & Nilsen, 2014).
2) Persuasive System Design
Persuasive technology influences the adoption and maintenance of behaviors through specific communication elements and design features aimed at shaping attitudes without using deceptive tactics (Oinas-Kukkonen & Harjumaa, 2008). The Persuasive System Design framework recognizes the content, design, software, and functionality of a digital technology intervention (Oinas-Kukkonen & Harjumaa, 2009). This framework illustrates the persuasive system development process beginning with outlining the key behavioral objectives of the system, then identifying the context of the system, followed by considering the specific design features of the system (Oinas-Kukkonen & Harjumaa, 2009). This model emphasizes four important design features to illustrate how conceptual principles translate into software requirements (Oinas-Kukkonen & Harjumaa, 2009). First, primary task refers broadly to design elements aimed at supporting the primary goals of the intervention for the target users, which can include creating a user friendly interface, tailoring content, and monitoring individual-level progress and performance over time (Oinas-Kukkonen & Harjumaa, 2009). Second, dialogue involves the design considerations to support system interactivity with users, where the system provides feedback to users through reminders, encouragement, or other virtual support techniques (Oinas-Kukkonen & Harjumaa, 2009). Third, credibility represents elements of the system focused on making it credible and trustworthy to users such as providing reliable, accurate and unbiased information and demonstrating competence and expertise (Oinas-Kukkonen & Harjumaa, 2009). Lastly, social support describes design features that leverage social and normative influences: to persuade users through opportunities to observe and learn from other users; to compare performance with other users; and to facilitate cooperation, competition, and recognition of successfully achieving behavior change goals (Oinas-Kukkonen & Harjumaa, 2009). This model affords a framework that can simplify the numerous design considerations for a multi-component persuasive intervention for behavior change, and it can guide efforts to implement and evaluate these systems.
3) The Behavioral Intervention Technology Model
The behavioral intervention technology model builds on existing theories of human behavior and defines the conceptual and technical aspects of a technology intervention to guide why, what, how, and when the intervention is delivered to a target user (Mohr, Schueller, Montague, Burns, & Rashidi, 2014). This model provides a framework to facilitate translation of a technology intervention from initial concept to development and then delivery, and to enable communication among those involved throughout this process (Mohr et al., 2014). Specifically, this model depicts how the aims, behavioral intervention strategies, and technology components and characteristics of the intervention, such as software elements or user interface, are interconnected and enable translation of clinical objectives into a technology-based platform (Mohr et al., 2014). Intervention workflow refers to when and in what order each of the intervention components will be delivered over time (Mohr et al., 2014). This framework illustrates the relationships between different conceptual and technical aspects of the intervention and provides an approach for formalizing the design, development, and delivery of technology-based behavioral health interventions (Mohr et al., 2014). Further research is needed to refine and modify this model as new digital technologies and analytic techniques become available and to accommodate the specific needs for addressing behavioral health needs of people with mental illness (Mohr, Burns, Schueller, Clarke, & Klinkman, 2013; Mohr et al., 2014).
4) Behavior Models for Just-in-Time Adaptive Interventions
Just-In-Time Adaptive Interventions use persuasive design elements to deliver timely treatments or tailored content to support an individual’s behavioral health goals by adapting seamlessly to their needs as they change over time (Murray, Hekler, Spruijt-Metz, Rivera, & Raij, 2016; Nahum-Shani, Hekler, & Spruijt-Metz, 2015). This type of intervention is guided by the notion that the right type of intervention content can be delivered to someone at the right time, and that this moment is theorized to be precisely when an individual is in a state of vulnerability and receptivity (Nahum-Shani et al., 2015). Vulnerability refers to the point when an individual needs targeted support, such as in response to environmental cues or emotional triggers known to precipitate unhealthy behaviors such as substance use, smoking, or at-risk drinking (Nahum-Shani et al., 2015). Receptivity emphasizes that the individual must be in an appropriate position to receive or be exposed to the intervention content as opposed to being preoccupied with other tasks or life demands such as work, family commitments, or while driving (Nahum-Shani et al., 2015). Advances in digital technology such as mobile devices or sensing technologies make this form of adaptive intervention possible by enabling real-time data collection about an individual’s context, behaviors, and current location at a precise moment, while also factoring in details about the individual’s history, environment and personal characteristics (Nahum-Shani et al., 2015).
Conceptually, the Just-In-Time Adaptive Intervention involves achieving a series of proximal outcomes at varying times or intervals depending on an individual’s unique needs towards accomplishing a meaningful distal behavioral health outcome (Nahum-Shani et al., 2015). Behavior models that incorporate existing scientific evidence are necessary to inform the timing of intervention delivery, specifying the type of content that is delivered, and determining how this content is adapted to individuals’ differing circumstances (Nahum-Shani et al., 2015). Computational models of human behavior have been proposed as an encouraging approach for facilitating the development of Just-In-Time Adaptive Interventions, especially as the complexity, frequency, and quantity of data made available using digital technologies will require increasingly sophisticated and robust analytic methods (Murray et al., 2016).
Theory for Informing Digital Technology Interventions for Mental Disorders
The behavior theories and models discussed in this commentary share many overlapping constructs, as outlined in Table 3 (Brewer & Rimer, 2008). Given the complexity of human behavior, it has been suggested that no single theory can fully explain how behaviors change over time (Prochaska et al., 2008). Theories may need to be combined to inform the development of multicomponent interventions with the potential for greatest impact (Brewer & Rimer, 2008). Behavioral health concerns among people with mental illness are often complex, co-occurring, closely interconnected, and span both mental and physical health domains (Whiteman, Naslund, DiNapoli, Bruce, & Bartels, 2016). Therefore, the application of constructs from multiple theories may be important for developing effective digital health interventions for this at-risk group.
Table 3.
Overlapping constructs across behavior theories and models
| Construct | Construct Definition | Behavior Theories | |||
|---|---|---|---|---|---|
| Health Belief Model | Theory of Planned Behavior | Trans-theoretical Model | Social Cognitive Theory | ||
| Attitudes | Experience positive or negative emotions associated with performing the behavior. | X | X | ||
| Awareness | Learning new facts about the behavior and what the risks of not performing the behavior might be. | X | X | X | |
| Behavioral Cues/Triggers | Use reminders to support healthy behaviors and remove or manage triggers for unhealthy behaviors. | X | X | ||
| Intentions | Personal motivation to perform the behavior. | X | |||
| Perceived Benefits | Perceived benefits or advantages of performing the behavior. | X | X | X | |
| Perceived Barriers | Perceived presence of barriers that makes performing the behavior difficult. | X | X | X | |
| Reinforcement | Rewards for performing the behavior and for avoiding unhealthy behaviors. | X | |||
| Self-efficacy | Confidence in one’s ability to overcome barriers to performing the behavior. | X | X | X | X |
| Self-evaluation | Individuals’ beliefs about how performing the behavior will make them feel and whether it represents who they want to be. | X | X | ||
| Social Modeling | Learning by observing others who have successfully performed the behavior. | X | |||
| Social Norms | Beliefs about whether other people perform the behavior or perceive the behavior as important. | X | X | ||
| Social Support | Helping relationships with others that support positive behavior change. | X | X | ||
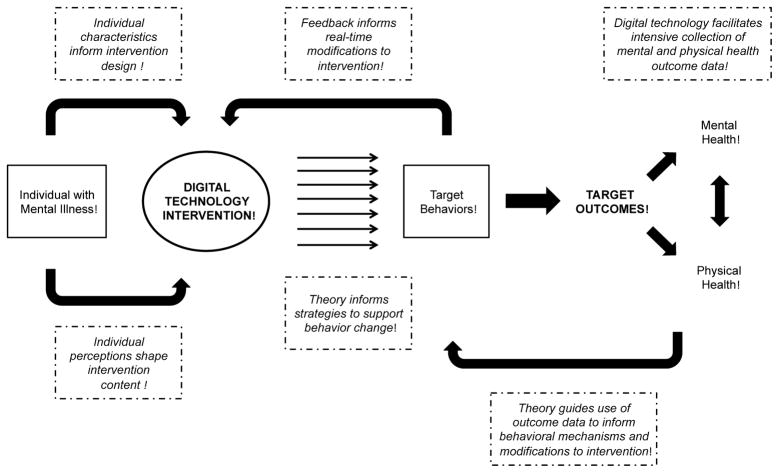
Multiple poor health behaviors, debilitating mental health symptoms, and chronic medical conditions compound to result in dramatically reduced life expectancy among people with mental illness. Consider that an individual living with schizophrenia may require targeted support for managing serious mental health symptoms, reminders to take psychiatric medications, while simultaneously requiring support for quitting smoking, managing a co-occurring chronic respiratory illness, and preventing relapse of a prior substance use disorder. This could be further complicated by ongoing need for overcoming symptoms of depression to encourage and support healthy eating and participation in regular exercise to reach a healthy weight. In Figure 1 we provide a conceptual illustration of how behavior theories and models can inform a digital technology intervention aimed at addressing co-occurring mental and physical health concerns affecting individuals with mental illness. By leveraging the potential of digital technologies through longitudinal data collection, real-time behavior monitoring, and adaptive features tailored to users’ changing needs over time, it may be possible to broaden our understanding of the complex interactions between different health behaviors among this at-risk group.
Figure 1.
Conceptual overview of theory for informing digital health interventions for mental and physical health concerns among people with mental illness
A rapidly growing literature demonstrates the potential of digital technology interventions for addressing mental and physical health concerns among people with mental illness (Alvarez-Jimenez et al., 2014; Naslund, Marsch, et al., 2015). Specific examples include studies that have demonstrated the feasibility of wearable sensing technology for recording physiological data and tracking mood changes among people with bipolar disorder (Lanata, Valenza, Nardelli, Gentili, & Scilingo, 2015), smartphone applications for monitoring and managing mental illness symptoms among people with schizophrenia (Ben-Zeev et al., 2014), wearable activity tracking devices for supporting lifestyle interventions delivered through community mental health settings (Naslund, Aschbrenner, Barre, & Bartels, 2015; Naslund, Aschbrenner, & Bartels, 2016b; Naslund, Aschbrenner, Scherer, et al., 2016), and comprehensive technology-delivered interventions to prevent relapse among inpatients with psychosis (Brunette et al., 2016). As the field continues to progress beyond feasibility studies, greater attention surrounding behavioral mechanisms involved in the use of digital technologies for health behavior change will be critical. Even simple interventions, such as text message reminders to take medications or attend appointments, involve changing a target behavior and can benefit from a guiding theoretical framework (Riley et al., 2011). Behavior change is not a straightforward process, and for even seemingly simple digital health interventions, the use of behavior theories can more fully identify the mechanisms of behavior change, address weaknesses in the intervention design, and improve transferability across settings (Riley et al., 2011). Developing an understanding of key behavioral mechanisms will be essential for ensuring that what we learn today can guide digital technology interventions developed tomorrow.
It is also important for researchers to consider more efficient ways to develop and evaluate digital health interventions, especially in the context of continuously evolving technologies (Patrick et al., 2016). The “agile science” process proposes an iterative development framework involving a generate phase followed by an evaluate phase to enable rapid optimization of digital health interventions towards achieving desired behavioral health outcomes (Hekler et al., 2016). The generate phase primarily focuses on feasibility with key activities involving formative work, simulation studies, and prototype testing, which can occur iteratively or simultaneously (Hekler et al., 2016). From this initial phase, promising products then advance onto the evaluate phase where emphasis shifts to achieving clinically meaningful outcomes (Hekler et al., 2016). Throughout the agile science process, early-and-often sharing of all products developed whether successful or failed attempts is key for advancing our cumulative knowledge base on behavior change (Hekler et al., 2016). An iterative approach helped guide the successful development of the theory-informed PRIME mobile application aimed at supporting motivation and improving quality of life among individuals with recent onset schizophrenia (Schlosser et al., 2016). Through workshops, a series of interviews, and multiple rounds of feasibility testing among stakeholders and participants, it was possible to refine the PRIME mobile application and increase user engagement with different components of the platform in preparation for a larger randomized controlled effectiveness study (Schlosser et al., 2016).
We believe that the future success of digital technology interventions for people with mental disorders will be dependent on whether theoretical models guide their development, delivery, and evaluation. Together, established behavior theories and emerging theoretical frameworks afford valuable opportunities to inform the design and delivery of digital technology interventions for people with mental illness. Important theoretical approaches to understanding human behavior including the Health Belief Model, the Theory of Planned Behavior, the Transtheoretical Model, and Social Cognitive Theory can provide a meaningful starting point for hypothesizing what factors or strategies may be necessary to change or modify health behaviors. For example, the Health Belief Model could illustrate perceived benefits and barriers related to coping with mental health symptoms, while Social Cognitive Theory could guide our understanding of how social relationships and social pressures shape smoking behaviors among people with mental illness who are at elevated risk of heavy tobacco use and who are often embedded in social environments with high rates of smoking. Emerging theoretical frameworks could provide a method for linking the complex data collection capacities of digital technologies with underlying behavioral constructs and for informing the specific timing and content of interventions. Theory could also inform strategies to promote engagement and sustained use of digital technology interventions over time by tailoring content for individual users.
We believe that important opportunities lie ahead for using behavior theories to inform digital health interventions for people with mental illness. We are currently at a crossroads where the advancing capacity of digital technologies is now enabling measurement of behavioral constructs that were previously not possible to evaluate. At the same time there is increasing availability, penetration, and use of digital technologies such as smartphones and other mobile devices among the target population of individuals with mental illness. It is now possible to develop and deliver comprehensive interventions aimed at supporting the mental and physical health needs of these individuals. To make this a reality, much work remains, and there are several important considerations needed to facilitate the use of behavior theories for guiding the development of digital technology interventions for mental disorders. Notably, greater collaboration across disciplines is essential. Mental health and psychiatric services researchers must work closely with software engineers, computer scientists, technologists, and behavioral specialists to support the development of new digital technology interventions. Additionally, as researchers have previously emphasized, there is a need for a common language across theories and common measures across studies to inform mathematical and computational models, and to facilitate communication across disciplines (Spruijt-Metz, Hekler, et al., 2015). It is critical for mental health services researchers to contribute to the development of this common language and to the use of common measures so that terminology can be incorporated from mental health and psychiatric services research. This will also advance our understanding of behavioral mechanisms associated specifically with health concerns among people with mental illness as data collection and measurement of behaviors using digital technologies become increasingly complex. Lastly, researchers have called for the development of a ‘knowledge commons’ where advances to theories or behavioral models can be conveniently and rapidly shared across disciplines (Spruijt-Metz & Nilsen, 2014). We believe that consideration of behavior theories as applied to the co-occurring mental and physical health concerns experienced by individuals with mental illness is necessary and that this must be included as part of proposed initiatives.
Conclusions and Implications for Practice
Mobile devices and technological platforms will continue to evolve rapidly in the years ahead. To ensure that current research can guide future efforts, behavior theories and models must inform our design, development, and delivery of interventions for mental disorders and our interpretation and analysis of findings. The success of digital health interventions for reaching and supporting individuals with mental illness will be largely determined by whether we can uncover specific behavioral mechanisms responsible for effectively managing mental health symptoms, preventing relapse, or reinforcing the adoption and maintenance of healthy behaviors. Future sustainability of digital technology interventions will also depend on carefully planned economic evaluation (McNamee et al., 2016), where the development, maintenance, and running costs of these interventions combined with the costs needed to adapt to rapidly changing technological platforms are balanced against potentially meaningful mental or physical health outcomes experienced by individuals living with mental illness. Mental disorders represent the leading cause of disability worldwide, and therefore identifying ways to effectively reach these individuals represents a major public health priority. Well-designed and rigorously tested digital technology interventions grounded in relevant behavior theories hold exciting promise for supporting the mental and physical health needs of individuals living with mental illness.
Acknowledgments
This study was supported by the Health Promotion Research Center at Dartmouth funded by the United States Centers for Disease Control and Prevention (Cooperative Agreement Number U48 DP005018) and the National Institute on Drug Abuse (P30 DA029926). The funders had no role in the design, content, decision to publish, or preparation of the manuscript.
Footnotes
Disclosure: Each of the authors contributed to the preparation of this manuscript and approved the final version to submit for publication. The authors report no competing interests.
References
- Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. 1991;50(2):179–211. [Google Scholar]
- Alvarez-Jimenez M, Alcazar-Corcoles M, Gonzalez-Blanch C, Bendall S, McGorry P, Gleeson J. Online, social media and mobile technologies for psychosis treatment: A systematic review on novel user-led interventions. Schizophrenia research. 2014;156(1):96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- Andresen R, Caputi P, Oades L. Stages of recovery instrument: development of a measure of recovery from serious mental illness. Australian and New Zealand Journal of Psychiatry. 2006;40(11–12):972–980. doi: 10.1080/j.1440-1614.2006.01921.x. [DOI] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Bartels SJ. A Mixed Methods Study of Peer-to-Peer Support in a Group-based Lifestyle Intervention for Adults with Serious Mental Illness. Psychiatric Rehabilitation Journal. 2016 doi: 10.1037/prj0000219. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, Bartels SJ. Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health Technology for Individuals with serious mental illness. Psychiatric Quarterly. 2016;87(3):401–415. doi: 10.1007/s11126-015-9395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and health. 1998;13(4):623–649. [Google Scholar]
- Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obesity research. 2003;11(S10):23S–43S. doi: 10.1038/oby.2003.222. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia bulletin. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Rimer BK. Perspectives on health behavior theories that focus on individuals. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 149–165. [Google Scholar]
- Brunette MF, Ferron JC, McHugo GJ, Davis KE, Devitt TS, Wilkness SM, Drake RE. An electronic decision support system to motivate people with severe mental illnesses to quit smoking. Psychiatric Services. 2011;62(4):360–366. doi: 10.1176/ps.62.4.pss6204_0360. [DOI] [PubMed] [Google Scholar]
- Brunette MF, Rotondi AJ, Ben-Zeev D, Gottlieb JD, Mueser KT, Robinson DG, … Schooler NR. Coordinated Technology-Delivered Treatment to Prevent Rehospitalization in Schizophrenia: A Novel Model of Care. Psychiatric Services. 2016;64(4):444–447. doi: 10.1176/appi.ps.201500257. [DOI] [PubMed] [Google Scholar]
- Bull S, Ezeanochie N. From Foucault to Freire Through Facebook Toward an Integrated Theory of mHealth. Health Education & Behavior. 2016;43(4):399–411. doi: 10.1177/1090198115605310. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 45–65. [Google Scholar]
- Corrigan PW. How stigma interferes with mental health care. American psychologist. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Rüsch N. Mental illness stereotypes and clinical care: do people avoid treatment because of stigma? Psychiatric Rehabilitation Skills. 2002;6(3):312–334. [Google Scholar]
- Crosby RA, Kegler MC, DiClemente RJ. Theory in Health Promotion Practice and Research. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research. 2. San Francisco, CA: Jossey-Bass; 2002. pp. 3–17. [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. Journal of medical Internet research. 2013;15(11):e247. doi: 10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG. Improving medical care for persons with serious mental illness: challenges and solutions. Journal of Clinical Psychiatry. 2007;68(suppl 4):40–44. [PubMed] [Google Scholar]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile Phone Ownership and Endorsement of “mHealth” Among People With Psychosis: A Meta-analysis of Cross-sectional Studies. Schizophrenia bulletin. 2015;42(2):448–455. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, … Jeste DV. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. American Journal of Psychiatry. 2005;162(2):370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual review of public health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 23–40. [Google Scholar]
- Glick G, Druss B, Pina J, Lally C, Conde M. Use of mobile technology in a community mental health setting. Journal of telemedicine and telecare. 2015;22(7):430–435. doi: 10.1177/1357633X15613236. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) The Journal of clinical psychiatry. 2015;76(2):155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- Hedden SL, Kennet J, Lipari R, Medley G, Tice P. Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health. 2015 Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.htm.
- Hekler EB, Klasnja P, Riley WT, Buman MP, Huberty J, Rivera DE, Martin CA. Agile science: creating useful products for behavior change in the real world. Translational behavioral medicine. 2016;6(2):317–328. doi: 10.1007/s13142-016-0395-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, … Moller HJ. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World psychiatry. 2011;10(2):138–151. doi: 10.1002/j.2051-5545.2011.tb00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickman NJ, Delucchi KL, Prochaska JJ. Treating tobacco dependence at the intersection of diversity, poverty, and mental illness: a randomized feasibility and replication trial. Nicotine & Tobacco Research. 2015;17(8):1012–1021. doi: 10.1093/ntr/ntv034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, … Zaslavsky AM. Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. American Journal of Psychiatry. 2008;165(6):703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne AM, Bramlet M, Barbaresso MM, Nord KM, Goodrich DE, Lai Z, … Duffy SA. SMI Life Goals: Description of a randomized trial of a Collaborative Care Model to improve outcomes for persons with serious mental illness. Contemporary clinical trials. 2014;39(1):74–85. doi: 10.1016/j.cct.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanata A, Valenza G, Nardelli M, Gentili C, Scilingo EP. Complexity index from a personalized wearable monitoring system for assessing remission in mental health. Biomedical and Health Informatics, IEEE Journal of. 2015;19(1):132–139. doi: 10.1109/JBHI.2014.2360711. [DOI] [PubMed] [Google Scholar]
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. The British Journal of Psychiatry. 2011;199(6):445–452. doi: 10.1192/bjp.bp.110.083733. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Moore RC, Davine T, Cardenas V, Bowie CR, Ho J, … Patterson TL. The use of the theory of planned behavior to predict engagement in functional behaviors in schizophrenia. Psychiatry Research. 2013;205(1):36–42. doi: 10.1016/j.psychres.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact: social cognitive theory. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 169–188. [Google Scholar]
- McGinty EE, Baller J, Azrin ST, Juliano-Bult D, Daumit GL. Interventions to address medical conditions and health-risk behaviors among persons with serious mental illness: A comprehensive review. Schizophrenia bulletin. 2016;42(1):96–124. doi: 10.1093/schbul/sbv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbin CL, Patterson TL, Norman G, Patrick K, Jin H, Roesch S, … Griver K. A lifestyle intervention for older schizophrenia patients with diabetes mellitus: a randomized controlled trial. Schizophrenia research. 2006;86(1):36–44. doi: 10.1016/j.schres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- McNamee P, Murray E, Kelly MP, Bojke L, Chilcott J, Fischer A, … Yardley L. Designing and Undertaking a Health Economics Study of Digital Health Interventions. American Journal of Preventive Medicine. 2016;51(5):852–860. doi: 10.1016/j.amepre.2016.05.007. [DOI] [PubMed] [Google Scholar]
- Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied psychology. 2008;57(4):660–680. [Google Scholar]
- Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. General hospital psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The behavioral intervention technology model: an integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of medical Internet research. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montano DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 67–96. [Google Scholar]
- Murray T, Hekler E, Spruijt-Metz D, Rivera DE, Raij A. Formalization of Computational Human Behavior Models for Contextual Persuasive Technology. Paper presented at the 11th International Conference on Persuasive Technology; Salzburg, Austria. 2016. [Google Scholar]
- Nahum-Shani I, Hekler EB, Spruijt-Metz D. Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. Health Psychology. 2015;34(Suppl):1209–1219. doi: 10.1037/hea0000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemedicine and e-Health. 2015;21(3):213–216. doi: 10.1089/tmj.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Bartels SJ. How People Living With Serious Mental Illness Use Smartphones, Mobile Apps, and Social Media. Psychiatric Rehabilitation Journal. 2016a doi: 10.1037/prj0000207. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Bartels SJ. Wearable devices and smartphones for activity tracking among people with serious mental illness. Mental health and physical activity. 2016b;10:10–17. doi: 10.1016/j.mhpa.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Scherer EA, McHugo GJ, Marsch LA, Bartels SJ. Wearable Devices and Mobile Technologies for Supporting Behavioral Weight Loss Among People with Serious Mental Illness. Psychiatry Research. 2016;244:139–144. doi: 10.1016/j.psychres.2016.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health. 2015;24(5):321–332. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oinas-Kukkonen H, Harjumaa M. Towards deeper understanding of persuasion in software and information systems. Paper presented at the First International Conference on Advances in Computer-Human Interaction; Sainte-Luce, Martinique. 2008. [Google Scholar]
- Oinas-Kukkonen H, Harjumaa M. Persuasive systems design: Key issues, process model, and system features. Communications of the Association for Information Systems. 2009;24 Article 28. [Google Scholar]
- Park T, Usher K, Foster K. Description of a healthy lifestyle intervention for people with serious mental illness taking second-generation antipsychotics. International journal of mental health nursing. 2011;20(6):428–437. doi: 10.1111/j.1447-0349.2011.00747.x. [DOI] [PubMed] [Google Scholar]
- Patrick K, Hekler EB, Estrin D, Mohr DC, Riper H, Crane D, … Riley WT. The Pace of Technologic Change: Implications for Digital Health Behavior Intervention Research. American Journal of Preventive Medicine. 2016;51(5):816–824. doi: 10.1016/j.amepre.2016.05.001. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach BT, McKibbin C, Goldman S, Bucardo J, Jeste DV. Functional adaptation skills training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophrenia research. 2006;86(1):291–299. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Evers KE. The Transtheoretical Model and Stages of Change. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass, John Wiley & Sons, Inc; 2008. pp. 97–121. [Google Scholar]
- Riley WT. Theoretical models to inform technology-based health behavior interventions. In: Marsch LA, Lord SE, Dallery J, editors. Behavioral Healthcare and Technology: Using Science-Based Innovations to Transform Practice. New York: Oxford; 2015. pp. 13–23. [Google Scholar]
- Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Translational behavioral medicine. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser D, Campellone T, Kim D, Truong B, Vergani S, Ward C, Vinogradov S. Feasibility of PRIME: A Cognitive Neuroscience-Informed Mobile App Intervention to Enhance Motivated Behavior and Improve Quality of Life in Recent Onset Schizophrenia. JMIR research protocols. 2016;5(2):e77. doi: 10.2196/resprot.5450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, … Asch DA. Building new computational models to support health behavior change and maintenance: new opportunities in behavioral research. Translational behavioral medicine. 2015;5(3):335–346. doi: 10.1007/s13142-015-0324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D, Nilsen W. Dynamic models of behavior for just-in-time adaptive interventions. IEEE Pervasive Computing. 2014;3(13):13–17. [Google Scholar]
- Spruijt-Metz D, Nilsen W, Pavel M, Adibi S. mHealth for behavior change and monitoring. mHealth Multidisciplinary Verticals. 2015:119–132. [Google Scholar]
- Valenstein M, Kavanagh J, Lee T, Reilly P, Dalack GW, Grabowski J, … Woltmann E. Using a pharmacy-based intervention to improve antipsychotic adherence among patients with serious mental illness. Schizophrenia bulletin. 2011;37(4):727–736. doi: 10.1093/schbul/sbp121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vazin R, McGinty EE, Dickerson F, Dalcin A, Goldsholl S, Oefinger Enriquez M, … Daumit GL. Perceptions of strategies for successful weight loss in persons with serious mental illness participating in a behavioral weight loss intervention: A qualitative study. Psychiatric Rehabilitation Journal. 2016;39(2):137–146. doi: 10.1037/prj0000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman KL, Naslund JA, DiNapoli EA, Bruce ML, Bartels SJ. Systematic review of integrated general medical and psychiatric self-management interventions for adults with serious mental illness. Psychiatric Services. 2016;67(11):1213–1225. doi: 10.1176/appi.ps.201500521. [DOI] [PMC free article] [PubMed] [Google Scholar]