Abstract
The aim of the study is (1) to describe and analyse health and social service use and medicine purchases in the last 2 years of life among older adults who died by suicide and (2) to compare use and purchases between three groups: those who died by suicide, died a natural death or who lived longer. Nation-wide Finnish register data were used. The data consist of 316,639 decedents who died at the age of 70 years or older in 1998–2008 and 222,967 people who lived longer. Use of hospital, long-term care and home care, and the purchase of prescribed psychotropic medications were studied for the 2-year period. Binary logistic regression analyses were applied. 1118 older adults died by suicide (0.4 % of all deaths). A majority of older adults who died by suicide had multiple somatic diseases and mental disorders, especially depression, and had contact with health and social services in the last 2 years of life. At the same level of morbidity, use of hospital and long-term care was less common among those who died by suicide than among those who died of natural causes, but more common than among those who lived longer. Those who died by suicide received less home care than those who lived longer. A high proportion of suicides occurred in the first month following hospital discharge. Health and social services should improve support for older adults with chronic diseases and depression.
Keywords: Suicide, Health and social service use, Psychotropic drugs, Last years of life, Depression, Finland
Introduction
Compared to other causes of death, the proportion of older people who die by suicide is not large, but compared to other age groups, suicide in many countries is more frequent among older people than in younger (Wu et al. 2014). Among older adults, suicide attempts are often premeditated and lead to death more often than among younger age groups (Conwell et al. 1998; Pitkälä et al. 2000). From the cognitive perspective, suicidal attempts can be understood as arising from perceptions of hopelessness and unbearability, often triggered by stressful life situations and the belief that one’s future will not improve (Wenzel and Beck 2008). The interpersonal–psychological theory of suicidal behaviour (Joiner 2005) proposes that, in addition to the ability to hurt oneself, the feeling of being a burden to family or society and the sense of isolation are important conditions underlying suicidal attempts. These theories provide important frameworks in understanding suicidal behaviour in later life, often characterized by chronic health problems and diminishing social networks. They are in line with common health-related risk factors identified in epidemiological studies, such as multiple somatic diseases (Erlangsen et al. 2015; Koponen et al. 2007; Timonen et al. 2002; Waern et al. 2002), mental health problems, especially depression (Cattell and Jolley 1995; Cavanagh et al. 2003; Conwell et al. 2002), and alcohol-use disorder (Szanto et al. 2002; Waern et al. 2002), the impact of somatic disease being typically mediated by depression (e.g., Conwell et al. 2002; Suominen et al. 2004).
Older adults in general have more contacts with health and social services than younger ones, and care services could have a major role in prevention of suicide, especially in selective prevention for those who have elevated risk of suicide and indicated prevention for those with acute suicidal ideation (Erlangsen et al. 2011). Of older adults (65+) who died by suicide in Finland in 1987–1988, 70 % had had a health care contact in the last month of life (Pitkälä et al. 2000). According to a review by Luoma et al. (2002), 58 % of people who died by suicide at the age of 55+ had had a contact with primary care in the last month of life and 77 % in the last year of life. For mental health care, the rates were 11 and 8.5 %, respectively (the figures were from different studies, which explain the logical discrepancy) (Luoma et al. 2002). In the UK, 58 % of older adults (65+) who died by suicide visited their GP and 20 % had contact with psychiatric services during the 6 months prior to dying by suicide (Cattell and Jolley 1995). Service use has been found to increase towards the end of life (Andersen et al. 2000; Deisenhammer et al. 2007a), with GP contacts occurring particularly among those aged 60 or over (Deisenhammer et al. 2007b).
Although mental health problems, particularly depression, are common among those older adults who die by suicide, a relatively low proportion use medication for depression at the time of their suicide: 16 % of older adults (65+) in Finland (Pitkälä et al. 2000), 29 % of older adults (60+) in the USA (Conwell et al. 2000) and 25 % in the UK (Cattell and Jolley 1995).
In this study, we (1) analyse the use of health and social services during the last phase of life among older adults who died by suicide and (2) compare it with the service use of those who died through natural causes and those who lived longer. It is known that older adults who are living their last phase of life use health and social services more than their age peers who live longer (Lubitz and Prihoda 1984; Polder et al. 2006; Pot et al. 2009; Yang et al. 2003) and the use of services differs by cause of death (Martikainen et al. 2012). Since several studies imply that people dying by suicide have more health problems than the general population (Waern et al. 2002), we hypothesize that they used health and social services more than those who lived longer. As adequate health and social care constitute an opportunity for prevention of suicide (Lapierre et al. 2011), we also hypothesize that those who died by suicide used services less than those who died through natural causes. The purpose is to improve our understanding of the role of health and social services in prevention of suicides in older age groups, and to identify crucial phases of care and subgroups needing special support. The study is part of a more comprehensive project: New dynamics of longevity and the changing needs for services (COCTEL).
Materials and methods
Study sample
The study sample was identified from nation-wide registers (Statistics Finland): the decedents were identified from the Causes of Death Register and those who lived longer from the Finnish Population Information System.
The data include all those who died in Finland at the age of 70 years or older in 1998 or 2002–2008 and a 40 % random sample of those who died at the same age in 1999–2001; the sample was smaller for reasons of convenience, but fully representative of all the deceased (Forma et al. 2007). From the decedents, we distinguished two groups on the basis of the cause of death: those who died by suicide (ICD-10 codes X60–X84 and Y87.0) and those who died of natural causes (the rest of the decedents, except those who died by accident or homicide, V01-Y98, who were excluded).
The control group, those who lived longer, was identified from the 40 % random samples of persons born in the same year as the decedents who died in 1998–2006, but who lived at least 2 years longer. For our earlier analyses, we have one-to-one individually matched case–control pairs of decedents and survivors. The controls have been matched by age, gender and municipality of residence for the decedents who died in 1998–2006 (Forma 2011). Use of services and the purchase of medicines were studied for the last 730 days of life for the decedents, and over the same calendar days for their matched counterparts. However, in this study the analyses were performed on a group level, and the matched case–control design was not used, since the comparison was done in this case between three groups instead of the two original groups (decedents and survivors).
Data sources for use of services and purchase of medicines
The data on health and social service use were derived from national administrative registers. The Care Register for Health Care and the Care Register for Social Welfare (National Institute for Health and Welfare, THL) cover the entire population and all hospitals and round-the-clock long-term care in Finland. The Home Care Census (THL) was taken on 1 day every other year in November up until 2007, and since then every year. It covers the clients of municipal home care and the services they received during the previous month. The information from the registers was linked using the unique Personal Identification Code. The care admissions were coded for each individual on the basis of the dates of admission to and discharge from care. The collating of data has been described earlier (Forma et al. 2007).
The data on the purchase of outpatient prescribed medicines were derived from the Prescription Database of the Social Insurance Institution of Finland (SII). The database covers 97 % of all prescription medicines purchased by outpatients and reimbursed by SII (Klaukka 2004).
Permission to access the register data was obtained from each register controller. The research plan was approved by the Pirkanmaa hospital district ethics committee.
Services and medicines
The services analysed were (1) hospital inpatient care, (2) round-the-clock long-term care and (3) regular home care, a service that combines home help and home nursing (occurring at least once a week). Hospital care included university hospital, general hospital (central, district and private) and the inpatient ward of a health centre if the length of stay (LOS) was less than 90 days. A health centre is a primary care hospital, which provides both acute and long-term care. Long-term care included residential home and sheltered housing with 24-hour assistance and health centre care if LOS ≥90 days. Hospital care is categorized as health care, while residential homes, sheltered housing and home care belong to social care; yet, to some extent, health care is provided in all categories of services.
Psychiatric inpatient care was recognized on the basis of the code for specialty (70) in the Care Register for Health Care. Psychiatric care was available in university and general hospitals as well as in health centres.
Medicine data concern the purchase of outpatient prescribed medicines. Data on the use of medicines in institutional care (hospitals and nursing homes) were not available. The analysed medicines were for depression (first digits of ATC codes N06A), psychosis (N05A) and neurosis (N05B). The controls of those who died in 2001 were excluded from the analyses concerning medicines, for the medicine data were not available for them.
The measure for each item of the service (medicine) was 1 = used (purchased) in the 2-year study period, or 0 = did not use (purchase) in the 2-year study period.
Morbidity
To take into account the effects of diseases on service use, we identified 11 major diseases or disease groups from which nine were somatic diseases, one was dementia and one mental disorders. The disease diagnoses were identified in the Care Register for Health Care and the purchased medicines in the Prescription Database. In addition, diagnoses in the Care Register for Social Welfare and Home Care Census were included, although the recording of diagnoses has not been very extensive in these registers. The ICD-10 codes and ATC codes are presented in Appendix, Table 5. We created a dummy variable for each of the disease groups.
Table 5.
The ICD-10 codes and ATC codes as the basis of morbidity variables
| Disease or disease group | ICD-10 codes | ATC codes |
|---|---|---|
| Arthritis or osteoarthritis | M05–M06, M15–M19 | M01 Antirheumatic drugs |
| Cancer | C00–C97 | L Antineoplastic and immunomodulating agents |
| Chronic asthma, COPD, other respiratory diseases | J00–J99 | R03 Drugs for obstructive airway diseases |
| Dementia | F00–F03 or G30 | N06D Anti-dementia drugs |
| Diabetes | E10–E14 | A10 Drugs used in diabetes |
| Hip fracture | S72 | |
| Ischemic and other heart diseasesa | I20–I25, I30–I425, I427–I52 | C01D Vasodilators used in cardiac diseases |
| Other diseases of the circulatory system | I00–I15, I26–I28, I70–I99 | |
| Parkinson’s disease or other neurological diseases | G00–G99 excluding G30, Alzheimer’s disease | N04 Antiparkinson drugs |
| Psychosis, depression, other mental health disorders | F04–F99 | N05 Psycholeptic drugsb |
| Stroke | I60–I69 |
aExcluding rheumatic and alcoholic heart diseases
bExcluding N05C hypnotic and sedative drugs
Statistical methods
Chi square tests were performed to examine whether there were differences by gender, prevalence of diseases and those who used services or purchased medicines between the three groups: those who died by suicide, died a natural death or lived longer. Independent sample t tests were used to compare the mean age between the groups. The analyses were performed for age groups 70–79 and ≥80 years and for women and men separately.
Binary logistic regression models were run to test the differences between the groups as to the probability of using each of the services and of purchasing psychotropic medications. In the preliminary analyses, the variations in service use between the three groups were remarkably different between the genders and therefore the models were run separately for women and for men. Models were run stepwise: in model 1 group and age, and in model 2 group, age and morbidity were included as independent variables.
Results
Descriptives
There were 539,606 older adults in the data. 316,639 of them died in 1998–2008, and 222,967 lived at least 2 years longer than the decedents. Of the decedents, 1118 died by suicide and 304,955 died of natural causes. 10,566 were excluded because their cause of death was an accident or a homicide.
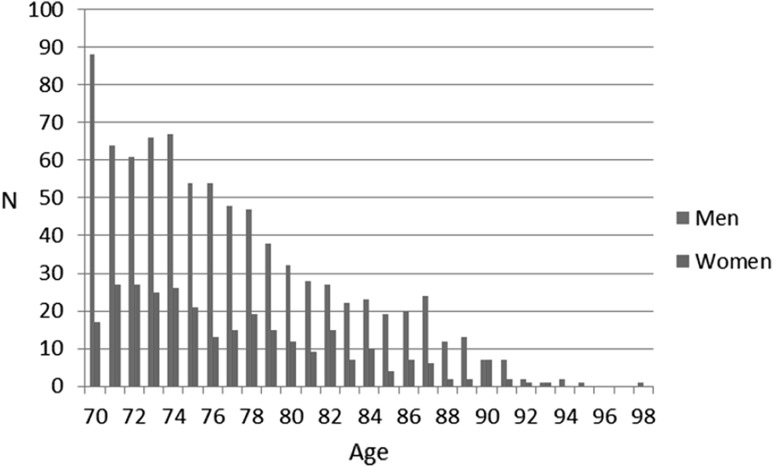
The rate of suicide was 0.4 % of all deaths, 0.6 % for men and 0.2 % for women, and it remained the same from 1998 to 2008. Suicides were more common among younger-old persons than among older ones (Table 1; Fig. 1). Those who died by suicide were on average 5.6 years younger than those who died of natural causes. Most of the older adults who died by suicide (82 %) died at home (i.e. not in a care facility), whereas 14 % of those who died of natural causes died at home (Table 1).
Table 1.
Descriptive characteristics
| Suicide N = 1118 |
Natural deatha
N = 304,955 |
Living longerb
N = 222,967 |
|
|---|---|---|---|
| Age | 77.5 | 83.1*** | 81.9*** |
| Women (%) | 25.9 | 58.7*** | 58.2*** |
| Morbidity | |||
| Arthritis | 4.7 | 5.8 | 4.3 |
| Cancer | 15.7 | 26.9*** | 5.2*** |
| Respiratory | 27.9 | 49.3*** | 15.6*** |
| Dementia | 4.1 | 26.4*** | 5.5* |
| Diabetes | 11.6 | 20.0*** | 11.5 |
| Hip fracture | 2.1 | 5.9*** | 2.0 |
| Ischemic | 38.6 | 63.9*** | 34.1 |
| Other circulatory | 13.7 | 33.3*** | 8.6*** |
| Neurological | 12.5 | 12.1 | 5.0*** |
| Mental disorders | 67.5 | 35.6*** | 24.4*** |
| Stroke | 6.5 | 22.6*** | 3.6*** |
| Place of death*** | |||
| Hospital | 13.1 | 72.7 | |
| Long-term care | 4.8 | 13.4 | |
| Home (not in a care facility) | 82.1 | 13.9 | |
Both of the other groups are compared to the suicide group
* p < 0.05
*** p < 0.001
aThe p values reported refer to Chi square tests and the t test of the significant differences between the suicide and natural death groups
bThe p values reported refer to Chi square tests and the t test of the significant differences between the suicide and living longer groups
Fig. 1.
Number of suicides by age and gender in 1998–2008 (n = 1118)
Mental disorders were more common among those who died by suicide (67.5 %) than among those who died of natural causes (35.6 %) or lived longer (24.4 %) (Table 1). All other diseases were more common among those who died of natural causes than among those who died by suicide. For neurological diseases and arthritis, the difference was not statistically significant. Dementia was less common among those who died by suicide than among those who lived longer, and all other diseases were more or equally common in the suicide group (Table 1).
Use of services in the last 2 years of life among those who died by suicide
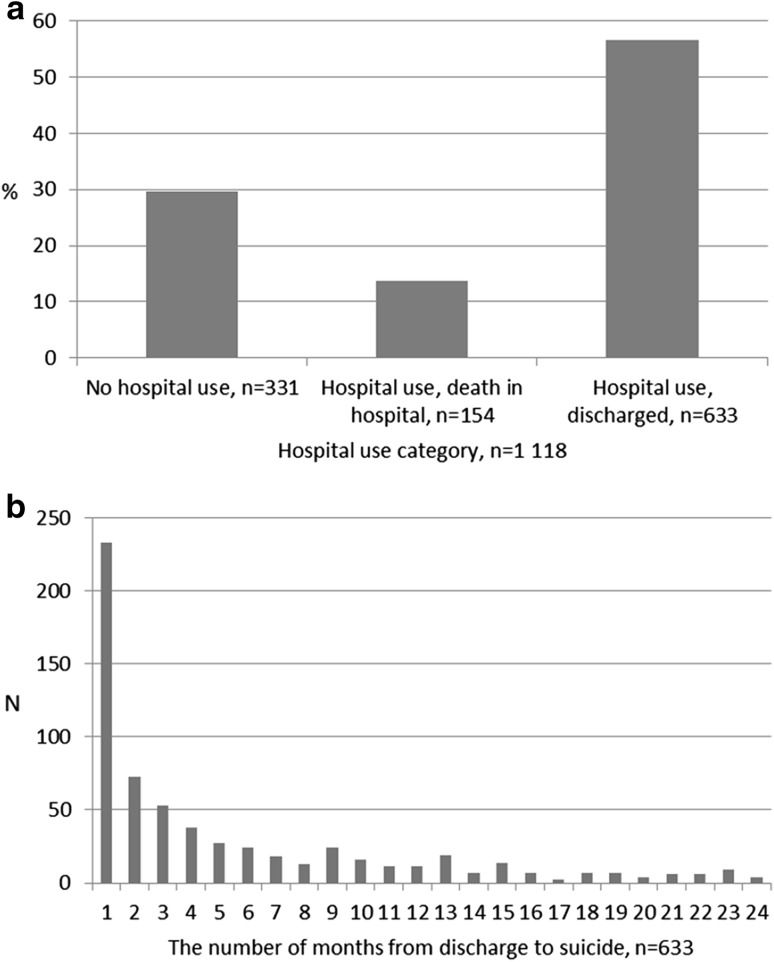
About 70 % of those who died by suicide were in hospital inpatient care at least once during the last 2 years of life (Table 2), and 19.6 % of them also died in hospital (Fig. 2a). Inpatient hospital care in the psychiatric specialty was highest (27.7 %) among women aged 70–79. Use of long-term care and home care was higher among older persons (80+) than for younger ones (70–79) and higher among women than among men. In both age groups, a higher proportion of women than men purchased psychotropic medications (Table 3), younger women more often than older ones.
Table 2.
Proportion of service users in the 2-year study period (%)
| Suicide | Natural deatha | Living longerb | |
|---|---|---|---|
| Women 70–79 years, n | 195 | 43,586 | 36,515 |
| Hospital | 73.8 | 85.5*** | 41.5*** |
| Psychiatric inpatient care | 27.7 | 2.8*** | 0.9*** |
| Long-term care | 17.4 | 36.8*** | 6.2*** |
| Home care | 13.8 | 15.7 | 9.6* |
| No service use or psychotropic medicationsc | 6.2 | 4.3 | 46.2*** |
| Women 80+ years, n | 95 | 135,513 | 93,198 |
| Hospital | 73.7 | 75.6 | 53.8*** |
| Psychiatric inpatient care | 10.5 | 1.4*** | 0.7*** |
| Long-term care | 27.4 | 66.0*** | 25.3 |
| Home care | 23.2 | 21.4 | 29.4 |
| No service use or psychotropic medicationsc | 6.3 | 1.6* | 24.1*** |
| Men 70–79 years, n | 570 | 57,704 | 47,989 |
| Hospital | 68.8 | 86.2*** | 41.3*** |
| Psychiatric inpatient care | 11.4 | 2.5*** | 0.6*** |
| Long-term care | 10.4 | 28.1*** | 4.5*** |
| Home care | 8.1 | 12.1* | 6.7 |
| No service use or psychotropic medicationsc | 20.2 | 7.5*** | 50.6*** |
| Men 80+ years, n | 258 | 68,152 | 45,265 |
| Hospital | 70.2 | 85.0*** | 53.9*** |
| Psychiatric inpatient care | 5.8 | 1.8*** | 0.5*** |
| Long-term care | 16.7 | 50.7*** | 14.6 |
| Home care | 19.0 | 20.0 | 20.9 |
| No service use or psychotropic medicationsc | 15.9 | 2.6*** | 32.2*** |
Both of the other groups are compared to the suicide group
* p < 0.05
** p < 0.01
*** p < 0.001
aThe p values refer to Chi square tests of the significant differences between the suicide and natural death groups
bThe p values refer to Chi square tests of the significant differences between the suicide and living longer groups
cThe control persons who lived longer than those who died in 2001 were excluded for lack of data
Fig. 2.
a Proportion of older adults in different hospital-use categories among those who died by suicide. b Time from hospital discharge to death among those who died by suicide. (Among those who used a hospital and who were discharged). (Color figure online)
Table 3.
Proportion (%) of those who purchased outpatient prescribed psychotropic medications in the 2-year study period
| Medicine (first digits of ATC) | Suicide | Natural deatha | Living longerb,c |
|---|---|---|---|
| Women 70–79 years, n | 195 | 43,586 | 34,351 |
| Depression (N06A) | 63.6 | 23.8*** | 12.7*** |
| Psychosis (N05A) | 40.5 | 15.6*** | 6.1*** |
| Neurosis (N05B) | 45.1 | 17.3*** | 11.8*** |
| Any of those | 79.0 | 38.9*** | 22.8*** |
| Women 80+ years, n | 95 | 135,513 | 87,510 |
| Depression (N06A) | 57.9 | 20.7*** | 16.2*** |
| Psychosis (N05A) | 28.4 | 15.4* | 9.7*** |
| Neurosis (N05B) | 30.5 | 12.8*** | 12.8*** |
| Any of those | 66.3 | 34.9*** | 29.0*** |
| Men 70–79 years, n | 570 | 57,704 | 45,257 |
| Depression (N06A) | 37.7 | 20.2*** | 7.3*** |
| Psychosis (N05A) | 20.2 | 13.6*** | 4.1*** |
| Neurosis (N05B) | 29.3 | 13.6*** | 7.7*** |
| Any of those | 51.1 | 31.5*** | 14.7*** |
| Men 80+ years, n | 258 | 68,152 | 42,554 |
| Depression (N06A) | 32.6 | 16.9*** | 10.1*** |
| Psychosis (N05A) | 15.5 | 15.1 | 6.3*** |
| Neurosis (N05B) | 29.8 | 12.2*** | 9.3*** |
| Any of those | 48.8 | 32.7*** | 20.1*** |
* p < 0.05
*** p < 0.001
aThe p values refer to Chi square tests of the significant differences between the suicide and natural death groups
bThe p values refer to Chi square tests of the significant differences between the suicide and control groups
cThe control persons who lived longer than those who died in 2001 were excluded for lack of data
The suicide rate was high in the months after discharge from a hospital. Among those who used hospital care, 36.8 % of suicides (20.8 % of all suicides in the study sample) occurred during the first month after their discharge (Fig. 2b). Yet, this group did not differ from those who died later by suicide in regard to age, gender or whether they received psychiatric inpatient care or not. Instead, ischemic heart disease and mental health disorders were more common among those who died by suicide in the month following their discharge than among those who died later [50.2 vs. 36.1 % and 70.4 vs. 61.9 %, respectively (p < 0.001)].
Use of services and the purchase of medicines: comparison between the groups
The proportion of hospital and long-term care users in the suicide group lay between those of the other two groups (Table 2). Use of these services was highest among those who died of natural causes and lowest among those who lived longer (the difference was not statistically significant in every age and gender group).
Psychiatric inpatient care and the purchase of psychotropic medications were more common among those who died by suicide than among those who died of natural causes or lived longer (Tables 2, 3). Antidepressants were the most common medicines purchased in all groups.
In the younger age group, use of home care among those who died by suicide lay between the two other groups; in women, it was significantly higher than among those who lived longer and in men significantly lower than in the natural death group (Table 2). Among those aged 80 years or over, use of home care did not differ between the groups.
The proportion of those with no contacts with health and social services and no psychotropic medications was higher among those who died by suicide than among those who died of natural causes (Table 2). However, being without any contact with services was most common among those who lived longer.
Multivariate analyses
Adjusted for age, use of both hospital care and long-term care was less likely among those who died by suicide than among those who died of natural causes, but more likely than among those who lived longer, both among men and women (Model 1, Table 4). There were no significant differences between the groups in home care. When also morbidity was adjusted for, those who died by suicide were more likely to use hospital care or long-term care and less likely to use home care than those who lived longer. Compared to those who died by natural death, those who died by suicide used less long-term care and, among men, also less hospital care. Instead, they were clearly more likely to purchase psychotropic medicines than the two other groups.
Table 4.
Any use of services and medications. Odds ratios of binary logistic regression analyses
| Model | Hospital | Long-term care | Home care | Psychotropic medicationsa | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Women, n = 309,102 | ||||||||
| Group | ||||||||
| Suicide (ref.) | ||||||||
| Natural death | 1.40* | 0.87 | 2.87*** | 3.04*** | 0.86 | 0.82 | 0.40*** | 0.31*** |
| Living longer | 0.39*** | 0.55*** | 0.48*** | 0.58*** | 1.16 | 1.64** | 0.29*** | 0.33*** |
| Age | 0.99*** | 0.99*** | 1.12*** | 1.12*** | 1.05*** | 1.06*** | 1.00*** | 1.01*** |
| Nagelkerke R2
-2LL |
0.113 368,387 |
0.398 290,880 |
0.308 341,178 |
0.431 302,043 |
0.029 316,706 |
0.113 298,900 |
0.007 536,006 |
0.870 120,970 |
| Men, n = 219,938 | ||||||||
| Group | ||||||||
| Suicide (ref.) | ||||||||
| Natural death | 2.48*** | 1.28** | 3.76*** | 3.59*** | 1.17 | 0.99 | 0.41*** | 0.32*** |
| Living longer | 0.38*** | 0.55*** | 0.58*** | 0.76* | 1.03 | 1.45** | 0.16*** | 0.27*** |
| Age | 1.02*** | 1.02*** | 1.10*** | 1.10*** | 1.07*** | 1.08*** | 1.00*** | 1.01*** |
| Nagelkerke R2
-2LL |
0.222 233,517 |
0.472 181,499 |
0.257 214,176 |
0.402 185,640 |
0.049 180,834 |
0.114 172,287 |
0.036 474,228 |
0.862 113,260 |
Model 1: group and age
Model 2: model 1 + morbidity in the Care registers and the Prescription Database (cancer, diabetes, dementia, mental, neurological, respiratory, arthritis, hip fracture, stroke, heart diseases, other circulatory)
* p < 0.05
** p < 0.01
*** p < 0.001
aThe control persons who lived longer than those who died in 2001 were excluded for lack of data
Discussion
We compared the use of health and social services in the last 2 years of life among older adults who died by suicide with service use by those who died through natural causes and those who lived longer. The higher service use in the last phase of life compared to those at the same age but living longer is well known (e.g., Lubitz and Prihoda 1984; Polder et al. 2006; Werblow et al. 2007). As a cause of death, suicide in many ways is different from disease. However, to our knowledge, the current study is the first to separate the suicide group in decedent–survivor comparisons.
We found that those who died by suicide used less hospital care than those who died a natural death, and, among men, the difference was maintained even when morbidity was adjusted for. At the same level of morbidity, long-term care, and in men also home care, was less frequent among those who died by suicide, but use of psychotropic medications was more common. All somatic diagnoses were less common in the suicide group than in those who died through natural causes, but most diseases were more common than in the longer-living group. Mental health disorders were distinctly more common in the suicide group, as were cancer and respiratory diseases. A notable exception was dementia, which was rarer in the suicide group than in the two other groups. The suicide group was younger than the other groups, which is likely to explain the lower prevalence of dementia. Mental disorders were clearly most common in the suicide group. We did not have detailed diagnoses available, but from the types of psychotropic medications used we can conclude that, particularly in women, the most frequent psychiatric problem is depression. This is similar to what earlier studies have found (Conwell et al. 2002; Paraschakis et al. 2012).
Lunney et al. (2003) presented four different trajectories before death; sudden death, terminal illness, organ failure and frailty. Service need and use in the last phase of life vary between these trajectories, e.g., before sudden death service use is typically not increased. Suicide is a premature death, but how imminent the natural death would have been cannot be known. Yet, our findings imply that suicide among older adults cannot be considered as a sudden death, but is preceded by a phase of somatic and/or mental health problems and contacts with services. Thus, suicide is not a separate event, but a process that may begin long before the act of terminating the individual’s existence (Järventie 1993; Joiner 2005). The theories attempting to understand the act of suicide refer to stressful life events such as serious health problems and disability, feelings of being a burden on other people and a sense of isolation. Depending on one’s personality, these situations may trigger perceptions of hopelessness and unbearability of life, and depression, something that, particularly in old age, is the main underlying factor in suicide (Conwell et al. 2002; Joiner 2005; Wenzel and Beck 2008). In later life, physical illness and disability are particularly important risk factors for suicide, but their effect is mainly mediated through depression. In this cascade of events, the obvious aim of health and social services is not only to prevent the physical act of suicide but, primarily, to alleviate suffering leading to suicidal ideation.
In this regard, three findings in our study are particularly interesting. First, a great majority, more than 80 %, of older adults who died by suicide had contacts with health and social services during the last 2 years of their lives. Earlier studies have found that the percentage of those who have contacts with health services during the last month of their life can be as high as 70 %, but the risk of suicide is seldom discussed during the visit (Pitkälä et al. 2000). Second, the risk of suicide was very high during the first month after discharge from a hospital; a fifth of all suicides occurred during this period. This is consistent with earlier studies (Andersen et al. 2000; Erlangsen et al. 2005; Karvonen et al. 2009). In our study, the risk of suicide in the first month after hospital discharge was highest among those who suffered from ischemic heart disease or mental disorders, including depression; however, the reasons for hospitalization are not known. It is possible that people were not discharged with an adequately conducted discharge plan, and that they did not receive the support they needed after returning home. Hospital discharge is a critical phase for continuity of care, and therefore the follow-up care especially for those who have depression should be carefully planned. Underlying the suicide may be stress caused by a disease and fear of its progression. Of those who died by suicide in hospital, it is not known whether the suicide was committed during the hospital stay or they had made suicide attempts somewhere out of the care facilities before being taken to the hospital and later died there due to injuries. However, inpatient suicides among old people have not been found to be very common: among old (65+) psychiatric inpatients, four suicides occurred during 7658 hospital episodes in Germany (Neuner et al. 2009). Third, at the same level of morbidity, staying in long-term care was more than three times more likely among those who died a natural death than among those who died by suicide. However, our data do not tell whether suicidal ideation was lower among those in long-term care or whether the means to realize these thoughts were less. In all, these findings suggest that those recently discharged from a hospital and those living outside long-term care but suffering from health conditions similar to those among people in long-term care are vulnerable groups among older adults and are at a higher risk of suicide. It is likely that in contacts with care services, the risk of suicide has not been recognized, and, also, that older adults with somatic and mental health problems have not received the care and support needed in their situation. In Finland, as in many other countries, there is a trend towards shorter hospital stays. In addition, official care policy prefers old people to stay at home, instead of in nursing homes or sheltered housing. Obviously, this increases the challenges service providers face in identifying the individuals at risk, diagnosing depressive mood disorders and starting adequate treatment.
Both the suicide rate and the patterns of service use differed between the genders and age groups. As a cause of death, suicide was three times as common in men as in women, and for both genders it was more common among the younger-old than the oldest-old. Being entirely without contacts with health and social services was more common for men than for women in all groups, as well as for those who died by suicide; the same gender difference has been found in earlier studies (Andersen et al. 2000; Deisenhammer et al. 2007b). Underlying this may be, e.g., self-stigma related to seeking for help, which men have been found to experience more often than women (Reynders et al. 2015). In multivariate analyses, use of all services was associated with a higher age among men, but among women a higher age was associated with a decrease in the use of hospital care and, in the model adjusted for morbidity, also home care, while it clearly was associated with an increase in the use of long-term care. This is likely due to the well-known differences between genders in functioning and in life situations; in old age, disability is higher among women, and they are also often widowed and live alone. Yet, it is remarkable that being without hospital care, long-term care or home care, particularly for men, seems to be a risk factor.
It is a weakness of our study that we did not have information on several factors that are known to be associated with suicide, such as marital status, family and other sources of social support, nor did we have data on functional status, disability or personality. What we do know, however, is that a majority of older women and an increasing proportion of older men are living alone (Official Statistics of Finland (OSF) 2009). Furthermore, it is known that in the period before dying by suicide, people often have contact with primary health care (Andersen et al. 2000; Luoma et al. 2002; Pitkälä et al. 2000); information on primary health care was also lacking in the national registers that were our data source. Yet, in the current study medication purchases refer to outpatient prescribed medications, for data on medication in hospitals and institutional long-term care were not available. In institutional long-term care, as much as 80 % of residents have been found to use psychotropic medications (Hosia-Randell and Pitkälä 2005). Therefore, use of these medications especially among the oldest women, who are more often inhabitants in institutions, would be higher if the medications in institutions were included.
Yet, using comprehensive and accurate register data (Keskimäki and Aro 1991; Sund 2003) is a clear strength of this study. Suicides were identified in the Causes of Death Register. In Finland, the cause of death must always be investigated and recorded. Under the law on detection of cause of death (1973/459, 7 §), a medical legal investigation has to be performed when a death is caused or is suspected to have been caused by, e.g., suicide, a crime or an accident. In 99.5 % of the suicides in 2002–2003 in Finland a medical legal autopsy was performed (Lunetta et al. 2007). The data can be considered to be reliable, e.g., in the case of fatal drug poisonings, there was 98.5 % agreement between medico-legal reports and the Causes of Death Register (Lahti and Vuori 2003).
Conclusions
Also among older adults, suicide is a tragic and potentially avoidable death, and should be a major public health concern. As disease and disability are particularly important underlying factors in later life suicides, there are several opportunities for interventions by health and social services. It is fair to believe that adequate and well-functioning health and social services that meet the needs of older adults are essential preventive factors through relieving the burden of disease and helping to cope with it. As to more focused measures, integration of care and carefully organized discharge plans are necessary when an older person returns home after hospital care. Sufficient long-term and home care should guarantee the quality of life and prevent isolation among disabled and frail older people. Adequate end-of-life care and knowledge of its availability are likely to alleviate distress among chronically ill older people. Finally, the ability of health and social care to diagnose and treat depression, the predominant risk factor for suicide in later life, must be improved, and, in addition to psychotropic medications, supportive interventions and therapy should be available.
Acknowledgments
The authors thank Professor Sami Pirkola for his valuable comments on the manuscript. This work was supported by Academy of Finland (250602 to MJ and 276189 to LF).
Funding
This study was funded by Academy of Finland (Grant Number 250602 to MJ and 276189 to LF).
Appendix
See Table 5.
Compliance with ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Responsible editor : D.J.H. Deeg.
References
- Andersen UA, Andersen M, Rosholm JU, Gram LF. Contacts to the health care system prior to suicide: a comprehensive analysis using registers for general and psychiatric hospital admissions, contacts to general practitioners and practising specialists and drug prescriptions. Acta Psychiatr Scand. 2000;102:126–134. doi: 10.1034/j.1600-0447.2000.102002126.x. [DOI] [PubMed] [Google Scholar]
- Cattell H, Jolley DJ. One hundred cases of suicide in elderly people. Br J Psychiatry. 1995;166:451–457. doi: 10.1192/bjp.166.4.451. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/S0033291702006943. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry. 1998;6:122–126. doi: 10.1097/00019442-199805000-00005. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, Caine ED. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/S0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- Deisenhammer EA, Huber M, Kemmler G, Weiss EM, Hinterhuber H. Psychiatric hospitalizations during the last 12 months before suicide. Gen Hosp Psychiatry. 2007;29:63–65. doi: 10.1016/j.genhosppsych.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Deisenhammer EA, Huber M, Kemmler G, Weiss EM, Hinterhuber H. Suicide victims’ contacts with physicians during the year before death. Eur Arch Psychiatry Clin Neurosci. 2007;257:480–485. doi: 10.1007/s00406-007-0751-1. [DOI] [PubMed] [Google Scholar]
- Erlangsen A, Mortensen PB, Vach W, Jeune B. Psychiatric hospitalisation and suicide among the very old in Denmark: population-based register study. Br J Psychiatry. 2005;187:43–48. doi: 10.1192/bjp.187.1.43. [DOI] [PubMed] [Google Scholar]
- Erlangsen A, Nordentoft M, Conwell Y, Waern M, De Leo D, Lindner R, Oyama H, Sakashita T, Andersen-Ranberg K, Quinnett P, Draper B, Lapierre S, International Research Group on Suicide Among the Elderly Key considerations for preventing suicide in older adults: consensus opinions of an expert panel. Crisis. 2011;32:106–109. doi: 10.1027/0227-5910/a000053. [DOI] [PubMed] [Google Scholar]
- Erlangsen A, Stenager E, Conwell Y. Physical diseases as predictors of suicide in older adults: a nationwide, register-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1427–1439. doi: 10.1007/s00127-015-1051-0. [DOI] [PubMed] [Google Scholar]
- Forma L (2011) Health and social service use among older people - the last two years of life (Acta Universitatis Tamperensis 1673). Tampere University Press, Tampere. http://tampub.uta.fi/bitstream/handle/10024/66837/978-951-44-8616-6.pdf?sequence=1
- Forma L, Rissanen P, Noro A, Raitanen J, Jylhä M. Health and social service use among old people in the last 2 years of life. Eur J Ageing. 2007;4:145–154. doi: 10.1007/s10433-007-0054-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosia-Randell H, Pitkälä K. Use of psychotropic drugs in elderly nursing home residents with and without dementia in Helsinki, Finland. Drug Aging. 2005;22:793–800. doi: 10.2165/00002512-200522090-00008. [DOI] [PubMed] [Google Scholar]
- Järventie I (1993) Social psychological and social psychiatric viewpoint to suicides. [Selviytyä hengiltä: Sosiaalipsykologinen ja sosiaalipsykiatrinen näkökulma itsemurhiin.]. National Research and Development Centre for Welfare and Health Research, Helsinki 34/1993
- Joiner T. Why people die by suicide. Campbridge: Harvard University Press; 2005. [Google Scholar]
- Karvonen K, Hakko H, Koponen H, Meyer-Rochow VB, Räsänen P. Suicides among older persons in finland and time since hospitalization discharge. Psychiatr Serv. 2009;60:390–393. doi: 10.1176/ps.2009.60.3.390. [DOI] [PubMed] [Google Scholar]
- Keskimäki I, Aro S. Accuracy of data on diagnoses, procedures and accidents in the Finnish hospital discharge register. Int J Health Sci. 1991;2:15–21. [Google Scholar]
- Klaukka T (2004) Using registers on medicines. Lecture at University of Tampere, Tampere
- Koponen HJ, Viilo K, Hakko H, Timonen M, Meyer-Rochow VB, Särkioja T, Räsänen P. Rates and previous disease history in old age suicide. Int J Geriatr Psychiatry. 2007;22:38–46. doi: 10.1002/gps.1651. [DOI] [PubMed] [Google Scholar]
- Lahti RA, Vuori E. Fatal drug poisonings: medico-legal reports and mortality statistics. Forensic Sci Int. 2003;136:35–46. doi: 10.1016/S0379-0738(03)00223-8. [DOI] [PubMed] [Google Scholar]
- Lapierre S, Erlangsen A, Waern M, De Leo D, Oyama H, Scocco P, Gallo J, Szanto K, Conwell Y, Draper B, Quinnett P, International Research Group for Suicide among the Elderly A systematic review of elderly suicide prevention programs. Crisis. 2011;32:88–98. doi: 10.1027/0227-5910/a000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubitz J, Prihoda R. The use and costs of medicare services in the last 2 years of life. Health Care Financ Rev. 1984;5:117–131. [PMC free article] [PubMed] [Google Scholar]
- Lunetta P, Lounamaa A, Sihvonen S. Surveillance of injury-related deaths: medicolegal autopsy rates and trends in Finland. Inj Prev. 2007;13:282–284. doi: 10.1136/ip.2006.012922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martikainen P, Murphy M, Metsä-Simola N, Häkkinen U, Moustgaard H. Seven-year hospital and nursing home care use according to age and proximity to death: variations by cause of death and socio-demographic position. J Epidemiol Community Health. 2012;66:1152–1158. doi: 10.1136/jech-2011-200756. [DOI] [PubMed] [Google Scholar]
- Neuner T, Schmid R, Hübner-Liebermann B, Felber W, Wolfersdorf M, Spiesl H. Suicidal behaviour of elderly psychiatric inpatients—prevalence and risk factors. Psychiatr Prax. 2009;36:225–231. doi: 10.1055/s-0028-1090179. [DOI] [PubMed] [Google Scholar]
- Official Statistics of Finland (OSF) (2009) Families. Living alone is more common among women than men. [Perheet. Naiset asuvat miehiä useammin yksin.] Statistics Finland
- Paraschakis A, Douzenis A, Michopoulos I, Christodoulou C, Vassilopoulou K, Koutsaftis F, Lykouras L. Late onset suicide: distinction between “young-old” vs. “old-old” suicide victims. How different populations are they? Arch Gerontol Geriatr. 2012;54:136–139. doi: 10.1016/j.archger.2011.02.011. [DOI] [PubMed] [Google Scholar]
- Pitkälä K, Isometsä ET, Henriksson MM, Lönnqvist JK. Elderly suicide in Finland. Int Psychogeriatr. 2000;12:209–220. doi: 10.1017/S1041610200006335. [DOI] [PubMed] [Google Scholar]
- Polder JJ, Barendregt JJ, van Oers H. Health care costs in the last year of life-the Dutch experience. Soc Sci Med. 2006;63:1720–1731. doi: 10.1016/j.socscimed.2006.04.018. [DOI] [PubMed] [Google Scholar]
- Pot AM, Portrait F, Visser G, Puts M, van Groenou MI, Deeg DJ. Utilization of acute and long-term care in the last year of life: comparison with survivors in a population-based study. BMC Health Serv Res. 2009;9:139. doi: 10.1186/1472-6963-9-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynders A, Kerkhof AJFM, Molenberghs G, van Audenhove C. Help-seeking, stigma and attitudes of people with and without a suicidal past. A comparison between a low and a high suicide rate country. J Affect Disord. 2015;178:5–11. doi: 10.1016/j.jad.2015.02.013. [DOI] [PubMed] [Google Scholar]
- Sund R. Utilisation of administrative registers using scientific knowledge discovery. Intell Data Anal. 2003;7:501–519. [Google Scholar]
- Suominen K, Isometsä E, Lönnqvist J. Elderly suicide attempters with depression are often diagnosed only after the attempt. Int J Geriatr Psychiatry. 2004;19:35–40. doi: 10.1002/gps.1031. [DOI] [PubMed] [Google Scholar]
- Szanto K, Gildengers A, Mulsant BH, Brown G, Alexopoulos GS, Reynolds CF. Identification of suicidal ideation and prevention of suicidal behaviour in the elderly. Drug Aging. 2002;19:11–24. doi: 10.2165/00002512-200219010-00002. [DOI] [PubMed] [Google Scholar]
- Timonen M, Viilo K, Väisänen E, Räsänen P, Hakko H, Särkioja T. Burden of illness and suicide in elderly people. Physical disease and depression are prevalent in elderly Finnish suicide victims. BMJ. 2002;325(7361):441. doi: 10.1136/bmj.325.7361.441/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waern M, Rubenowitz E, Runeson B, Skoog I, Wilhelmson K, Allebeck P. Burden of illness and suicide in elderly people: case-control study. BMJ. 2002;324(7350):1355. doi: 10.1136/bmj.324.7350.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A, Beck AT. A cognitive model of suicidal behavior: theory and treatment. Appl Prev Psychol. 2008;12:189–201. doi: 10.1016/j.appsy.2008.05.001. [DOI] [Google Scholar]
- Werblow A, Felder S, Zweifel P. Population ageing and health care expenditure: a school of ‘red herrings’? Health Econ. 2007;16:1109–1126. doi: 10.1002/hec.1213. [DOI] [PubMed] [Google Scholar]
- Wu J, Värnik A, Tooding L, Värnik P, Kasearu K. Suicide among older people in relation to their subjective and objective well-being in different European regions. Eur J Ageing. 2014;11:131–140. doi: 10.1007/s10433-013-0297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Norton EC, Stearns SC. Longevity and health care expenditures: the real reasons older people spend more. J Gerontol B Psychol Sci Soc Sci. 2003;58:2–10. doi: 10.1093/geronb/58.1.S2. [DOI] [PubMed] [Google Scholar]