Building off decades-long work, Healthy People 2010 (HP2010) is the national agenda-setting framework for the United States’ public health authorities at all levels of government for the first decade of the third millennium. HP2010 has two primary goals: 1. to improve quality and years of healthy life; and 2. to eliminate health disparities.1 Within these broad goals are 28 disease/condition-specific objectives based on best-available, evidence-based knowledge and surveillance.1
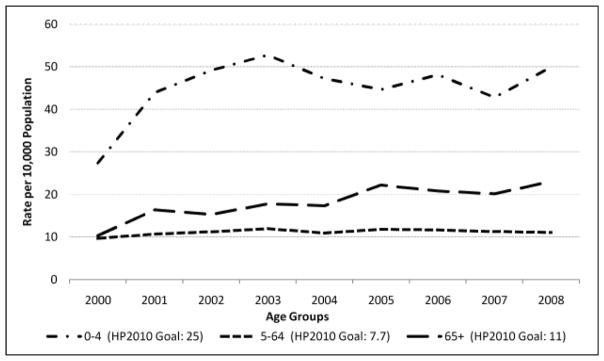
For respiratory diseases, HP2010 specifies eight asthma-specific objectives. Specifically, Objective 24-2 sets the following target rates for asthma hospitalization: (1) an age-specific rate of 25 per 10,000 children ages 0–4 years (2) an age-standardized* rate of 7.7 per 10,000 children and adults ages 5–64 years, and (3) an age-standardized rate of 11 per 10,000 adults ages 65+.
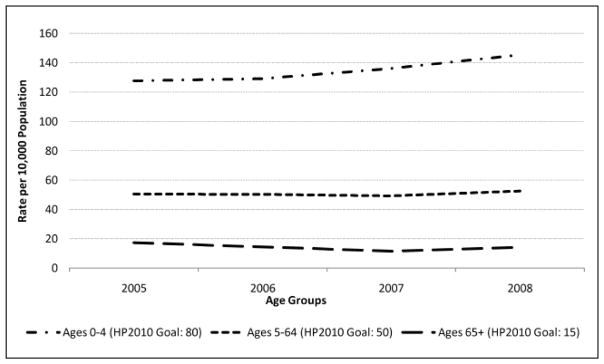
Similarly, there are well-defined targets for the reduction of hospital emergency department (ED) visits for asthma: from an age-specific rate of 150.0 per 10,000 in 1998 to 80 per 10,000 among children aged 0–4 in 2010; from an age-standardized rate of 71.1 per 10,000 in 1998 to 50 per 10,000 for children and adults 5–64 in 2010; and from an age-standardized rate of 29.5 per 10,000 in 1998 to 15 per 10,000 among adults ages 65+ in 2010.
Health departments charged with monitoring the burden of asthma in their state must track asthma-related hospitalization and ED visits. Hospitalization rates are an important population-level marker of asthma severity.2 Indeed, hospitalizations account for the single largest portion of the direct health care costs for asthma, estimated at nearly $18 billion a year.3,4 Large variations in the asthma-specific hospital discharge and ED visit rates across age groups may indicate differences in co-morbidities and/or the efficacy of asthma management in younger versus older age groups.
This brief assesses Rhode Island’s progress in meeting HP2010 goals for decreasing inpatient hospitalizations and ED visits for asthma. The information will help guide Rhode Island’s Asthma Control Program as it continues to develop infrastructure and interventions to improve the health of people with asthma. A more in-depth analysis of these hospitalization and ED visit rates for asthma by measures of disparity can be found elsewhere in this issue.
Methods
Data on asthma-related hospital discharges and ED visits were obtained from Rhode Island’s public-use Hospital Discharge Data and ED databases. These data contain de-identified health record level details on patient demographics, diagnoses, procedures, discharge status, residence location by census tract, and charges for every ED visit and hospitalization in Rhode Island to a non-federal hospital facility. This report covers hospital discharges beginning January 1, 2000 through December 31, 2008 and ED visits from January 1, 2005 through December 31, 2008. The data are based on the number of ED visits and hospital discharges or “events” and not the number of unique individuals who visited the ED or who were hospitalized. Thus, some of these events may include individuals with repeat admissions.
Asthma hospitalizations and ED visits were defined as a principal diagnosis using ICD-9-CM diagnosis code 493. Since some Rhode Island residents are hospitalized in neighboring states, only data on hospital discharges and ED visits for Rhode Island residents receiving treatment in one of Rhode Island’s 11 acute care hospitals were included in the analyses. Also excluded were out-of-state patients hospitalized for asthma in a Rhode Island hospital. We followed the HP2010 convention of calculating age-specific rates for children aged 0–4 and age-adjusted rates for those ages 5–64 and 65+ in order to compare Rhode Island data with HP2010 targets. Age adjustment was accomplished by first multiplying the age-specific rates of hospitalizations and ED visits by age-specific weights. The weights used in the age-adjustment of asthma data are the proportion of the 2000 US population within each age group (e.g., ages 0–4, ages 5–64, and ages 65+).
Results
Asthma Hospitalizations (2000–2008)
Rhode Island’s asthma hospitalization rates for 2000 to 2008 are significantly higher than the HP2010 targets established for all age groups. (Figure 1) In 2008, the most current year with available hospital discharge data, the asthma hospitalization rate was 49.9 per 10,000 for children under age 5, 11 per 10,000 children and adults aged 5–64 years, and 23 per 10,000 adults aged 65+.
Figure 1.
Rhode Island Asthma Hospitalization Rates by Age Groups, 2000–2008.
Between 2005 and 2008, Rhode Island ED visit rates due to asthma showed modest changes for children and adults aged 5–64 and those over age 65. (Figure 2) For these two groups, the ED visit rates either met or were only slightly higher than the HP2010 targets of 50 per 10,000 children and adults aged 5–64 and 15 per 10,000 among adults aged 65+. In contrast, the asthma ED visit rate for children under age 5 increased from 127.7 per 10,000 children aged 0–4 in 2005 to 145.4 per 10,000 children under age 5 in 2008. The HP2010 target for this age group is 80 per 10,000 children aged 0–4.
Figure 2.
Rhode Island Asthma Emergency Department Visit Rates by Age Groups, 2005–2008.
Conclusion
Rhode Island is making progress in meeting the HP2010 targets for decreasing asthma hospitalizations and ED visits. For hospitalizations, only those aged 5–64 were near HP2010 targets for hospitalization rates set at 7.7 hospitalizations per 10,000. ED visit rates among people 5–64 and 65+ were at or only slightly greater than the HP2010 specified targets. However, asthma hospitalization and ED visit rates were disturbingly high among children under age 5. Indeed, the rate of hospitalizations and ED visits among very young children (aged 0–4 years) exceeded the rates of other age groups as well as HP2010 goals of 25 hospitalizations per 10,000 boys and girls under age 5 and 80 ED visits per 10,000 boys and girls in the 0–4 age group.
While public health researchers have focused on improving clinical management of asthma through widespread implementation of the National Heart, Lung, and Blood Institute Expert Panel Report - 3 guidelines for the management of asthma,5 a substantial body of literature points to a strong relationship between asthma and broader physical and social environmental factors. Proximity to outdoor air pollution, poor housing quality, and urban poverty have been shown to greatly increase asthma exacerbations.6–9
There are limitations to our study. While non-federal hospitals must report all ED and hospitalization data to the Rhode Island Department of Health, some data may not be complete and/or may be incorrect. Furthermore, disease ascertainment and correct coding of asthma may prove difficult, especially in younger children.
Our results indicate that asthma ED visit and hospitalization rates are at or below HP2010 targets for some population groups in Rhode Island. As planners and stakeholders help shape the policies to improve asthma-related health, it will be critical to focus on individual-level interventions as well as community-level issues such as poverty. New asthma epidemiology paradigms point to the separate and joint effects of individual-and neighborhood-level factors that exacerbate asthma and may contribute to disparities in ED visit and hospitalization rates for asthma.9,10 By focusing on multilevel interventions, Rhode Island may be able to combat increasing rates of asthma acute care and meet targets for Healthy People 2020 goals.
Acknowledgments
Appreciation is extended to the staff of the Rhode Island Department of Health Center for Health Data and Analysis for their superb work in maintaining the datasets used in this brief. This publication was supported by the Cooperative Agreement Award Number: 5U59EH000199-03 from The Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Footnotes
All age-standardized rates were standardized to the year 2000 standard population.
Disclosure of Financial Interest of authors and/or spouses/significant others
The authors have no financial interests to disclose.
Contributor Information
Nicholas J. Everage, Epidemiologist for the RI Department of Health’s Asthma Control Program and a PhD candidate in Epidemiology at the Warren Alpert Medical School at Brown University.
Deborah N. Pearlman, Senior Epidemiologist for the RI Department of Health’s Asthma Control Program and Research Faculty at the Warren Alpert Medical School at Brown University.
Nancy Sutton, Program Manager for the RI Department of Health’s Asthma Control Program.
Dona Goldman, Team Lead for the RI Department of Health’s Chronic Care and Disease Management Programs.
References
- 1.US Department of Health and Human Services. Healthy People 2010: What Are Its Goals? http://www.healthypeople.gov/About/goals.htm.
- 2.Eisner MD, Katz PP, et al. Risk factors for hospitalization among adults with asthma. Respir Res. 2001;2:53–60. doi: 10.1186/rr37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asthma and Allergy Foundation of America. Information About Asthma, Allergies, Food Allergies and More! http://www.aafa.org/display.cfm?id=8&sub=42.
- 4.Weiss KB, Sullivan SD. The health economics of asthma and rhinitis. I. Assessing the economic impact. J Allergy Clin Immunol. 2001;107:3–8. doi: 10.1067/mai.2001.112262. [DOI] [PubMed] [Google Scholar]
- 5.National Heart, Lung, and Blood Institute and the National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. 2007 http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm.
- 6.Corburn J, Osleeb J, Porter M. Urban asthma and the neighbourhood environment in New York City. Health Place. 2006;12:167–79. doi: 10.1016/j.healthplace.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Gupta RS, Springston EE, Weiss KB. Eliminating asthma disparities. Curr Opin Pulm Med. 2009;15:72–8. doi: 10.1097/MCP.0b013e32831da911. [DOI] [PubMed] [Google Scholar]
- 8.Gold DR, Wright R. Population disparities in asthma. Ann Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 9.Williams DR, Sternthal M, Wright RJ. Social determinants. Pediatrics. 2009;123(Supplement):S174. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007 Nov;132(5 Suppl):757S–69S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]