Abstract
AIM
To assess the role of laparoscopic ultrasound (LUS) as a substitute for intraoperative cholangiography (IOC) during cholecystectomy.
METHODS
We present a MEDLINE and PubMed literature search, having used the key-words “laparoscopic intraoperative ultrasound” and “laparoscopic cholecystectomy”. All relevant English language publications from 2000 to 2016 were identified, with data extracted for the role of LUS in the anatomical delineation of the biliary tract, detection of common bile duct stones (CBDS), prevention or early detection of biliary duct injury (BDI), and incidental findings during laparoscopic cholecystectomy. Data for the role of LUS vs IOC in complex situations (i.e., inflammatory disease/fibrosis) were specifically analyzed.
RESULTS
We report data from eighteen reports, 13 prospective non-randomized trials, 5 retrospective trials, and two meta-analyses assessing diagnostic accuracy, with one analysis also assessing costs, duration of the examination, and anatomical mapping. Overall, LUS was shown to provide highly sensitive mapping of the extra-pancreatic biliary anatomy in 92%-100% of patients, with more difficulty encountered in delineation of the intra-pancreatic segment of the biliary tract (73.8%-98%). Identification of vascular and biliary variations has been documented in two studies. Although inflammatory disease hampered accuracy, LUS was still advantageous vs IOC in patients with obscured anatomy. LUS can be performed before any dissection and repeated at will to guide the surgeon especially when hilar mapping is difficult due to fibrosis and inflammation. In two studies LUS prevented conversion in 91% of patients with difficult scenarios. Considering CBDS detection, LUS sensitivity and specificity were 76%-100% and 96.2%-100%, respectively. LUS allowed the diagnosis/treatment of incidental findings of adjacent organs. No valuable data for BDI prevention or detection could be retrieved, even if no BDI was documented in the reports analyzed. Literature analysis proved LUS as a safe, quick, non-irradiating, cost-effective technique, which is comparatively well known although largely under-utilized, probably due to the perception of a difficult learning curve.
CONCLUSION
We highlight the advantages and limitations of laparoscopic ultrasound during cholecystectomy, and underline its value in difficult scenarios when the anatomy is obscured.
Keywords: Intraoperative ultrasound, Laparoscopic cholecystectomy, Bile duct injury, Choledocolithiasis, Biliary anomalies
Core tip: Laparoscopic ultrasound (LUS) during cholecystectomy allows a non-invasive study of the biliary tract, with an excellent ability to detect common bile duct stones and identify anatomy. Unlike intraoperative cholangiography, LUS can be performed before Calot’s triangle dissection, which facilitates the mapping of biliary and hilar structures during difficult scenarios such as severe inflammation and fibrosis. Cheap, quick, and non-irradiating LUS can be repeated at will during the operation. Adjacent organs can also be examined, allowing incidental findings. Our review of the recent literature highlights the advantages of LUS, despite its underuse, particularly in difficult cholecystectomies when the anatomy is obscured.
INTRODUCTION
The last few decades have seen the increased adoption of minimally invasive surgery in various abdominal procedures. A drawback of this laparoscopic approach is the inability of the surgeon to palpate abdominal organs. This loss of tactile feedback, combined with technical difficulties and an extensive learning curve, may collectively explain the slow uptake of laparoscopic surgery in the field of hepatic-biliary-pancreatic surgery (HPB)[1].
Cholecystectomy (LC) is the most common HPB operation and possibly represents the first widely accepted “gold standard” laparoscopic approach[2]. LC is a relatively easy and safe operation, as long as the biliary duct is adequately mapped. Indeed, delineation and meticulous evaluation of the biliary tract is critical for the detection of common bile duct stones (CBDS), and for the prevention of bile duct injury (BDI).
Over the past few decades the advantages of LC vs the open procedure have been widely acknowledged, but with one glaring blemish, the higher rate of BDI[3], despite a recent report describing a rate of BDI of 0.08%[4]. During LC the main cause of BDI is poor visibility of the biliary tract (71%-97% of patients) and inadequate surgical skills[5,6].
In order to clarify biliary anatomy during LC, different techniques have been proposed. These include intraoperative cholangiography (IOC), cholecystocholangiography, dye cholangiography, light cholangiography, passive infrared cholangiography, near-infrared fluorescence cholangiography, hyperspectral cholangiography, and laparoscopic ultrasound (LUS)[7]. Of these techniques, IOC is the most commonly used to determine bile duct anatomy and to diagnose CBDS. There has been much debate as to whether this examination helps to prevent, or improve the early detection of BDI. This controversy is of considerable importance to the patient, and their treatment[6], with uncertainty as to whether IOC should be routinely or more sparingly used[8-11].
The routine implementation of IOC poses several challenges. Practically, these include the need for dissection before IOC, which may be technically difficult (in acute or chronic inflammatory disease), together with cannulation of a short, thin, or tortuous cystic duct[12], and the risk of avulsion during cannulation of an inflamed cystic duct[13]. Additionally, IOC lengthens the procedure time[14] and increases costs, imposes a learning curve in terms of correctly interpreting images[5], and exposes the medical team and patient to ionizing radiation, even if this seems to be negligible concern for the adult population[15].
Soon after the outset of LC use, authors proposed that LUS be used to substitute for the lack of tactile palpation during laparoscopy, such that the surgeon could identify subsurface structures. Prior to 2000, multiple reports emphasized the benefits of LUS, and its efficacy in assessing CBDS and anatomy during LC[16-35].
Compared to IOC, LUS is described as less invasive, faster, cheaper, with no adverse events, and can be repeatedly used during the operation with no risk of irradiation, which is clearly preferable for pregnant or young patients. Nevertheless, despite these positives, the routine use of LUS during LC is virtually non-existent compared to IOC, with only 1% of surgeons using this technique[36].
This report aims to review the role of LUS as a substitute for IOC for the anatomical delineation of the biliary tract, anatomical evaluation during acute cholecystitis, CBDS detection, the prevention or early detection of BDI, and incidental findings during LC.
MATERIALS AND METHODS
A literature search of the PubMed and MEDLINE database was performed using the following keywords: “intraoperative laparoscopic ultrasound” and “laparoscopic cholecystectomy”. Overall, only English-language publications published between January 2000 and December 2016 were considered. All studies that contained material relevant to the topic were reviewed.
RESULTS
From 2000 to 2016, no randomized controlled trials were conducted. Eighteen reports were identified, 13 were prospective non-randomized trials, and 5 were retrospective trials. Two meta-analyses were found, one assessing the diagnostic accuracy of LUS in detecting CBDS vs IOC[37], and a second, analyzing CBDS detection, together with costs, time taken for the examination, and ability to identify anatomical landmarks[38]. Table 1 shows the published studies, together with their respective methodologies and principal evaluated variables.
Table 1.
Results of PubMed review
| Author | Year | Type of study | Number of patients | Surgeon | Routine LUS use | Detailed anatomical description | CBDS report | Specific aims of the study other than LUS efficacy |
| Tranter | 2001 | PNR | 367 | Several | + | Poor | + | |
| Biffl | 2001 | PNR | 248 | Several | + | No | + | CBDI |
| Halpin | 2002 | PNR | 380 | Single | + | Yes | + | Comparison with IOC |
| Catheline | 2002 | PNR | 900 | ni | + | No | + | Comparison with IOC |
| Tranter | 2003 | PNR | 135 | Several | + | No | + | Comparison with IOC, measurement of duct diameter |
| Onders | 2005 | PNR | 105 | Single | - | No | + | |
| Perry | 2007 | PNR | 236 | Single | + | Poor | + | Comparison with IOC |
| Machi | 2007 | PNR | 200 | Several | + | Poor | + | Cost |
| Hakamada | 2008 | RSS | 299 | Several | 1 | Yes | + | Educational program |
| Machi | 2009 | RMS | 1352 | Several | + | No | + | |
| Hublet | 2009 | PNR | 269 | Single | + | Poor | + | |
| Li | 2009 | PRN | 103 | Several | + | Yes | + | |
| Hashimoto | 2010 | RMS | 220 | Several | + | Yes2 | - | CBDI |
| Pfluke | 2011 | RSS | 50 | Several | + | Yes | + | |
| Nasu | 2012 | PNR | 71 | ni | + | Poor | + | |
| Kothari | 2013 | PNR | 253 | Several | + | Poor | - | Comparison with trans-abdominal US in obese patients |
| Gwinn | 2013 | PNR | 44 | Several | + | Poor | - | Impact of inflammatory disease |
| Shaaban | 2014 | RSS | 70 | Single | - | No | + | |
| Meta-analysis | ||||||||
| Aziz | 2014 | MA | ||||||
| Jamal | 2015 | MA |
Since instigation as part of an educational program ;
Focus on cystic duct-CBD junction. RSS: Retrospective single center study; RMS: Retrospective multicenter study; PNR: Prospective non-randomized study; MA: Meta-analysis; ni: No information; CBDS: Common bile duct stones; LUS: Laparoscopic ultrasound; IOC: Intraoperative cholangiography.
LUS and anatomy
During LC, an appreciation of bile duct and vascular anatomy is mandatory in order to perform fine dissection and prevent bile duct and vascular injuries. Indeed, errors whereby surgeons fix anatomical structures incorrectly, especially when the anatomy is obscured or where there is an anatomical variation, is the most common cause of injury[39]. The two structures that are most commonly misidentified as the cystic duct (neither of which are particularly rare) are the common bile duct, and an aberrant right hepatic duct that drains the posterolateral sector of the liver.
Izuishi et al[40] reported multi-slice-computed cholangiography of 113 patients and documented that a posterior inferior duct joined the common hepatic duct directly (parallel to the cystic duct) in 6% of patients, whereas a posterior segmental duct directly joined either the common bile duct in 7% of patients, or cystic duct in 1% of cases. An overall rate of anatomical variation of 16% was documented, which underlines the importance of accurately identifying all structures during LC. In a larger cohort study, anatomical variations of the bile duct were analyzed in 1094 direct cholangiograms by Yoshida et al[41]. The relative position of the right anterior (A), right posterior (P), right (R), left (L), and cystic ducts were documented. Arborizing patterns revealed that 67.7% were normal (i.e., RL, a normal bile duct convergence), whereas 17.7%, 8%, and 6%, demonstrated APL (i.e., trifurcation), A-PL (i.e., low implantation of the right anterior duct), and P-AL (i.e., low implantation of the right posterior duct), respectively. Cystic duct anomalies occurred in 1.6% of patients, the most frequent being the pattern (0.5%) in which the cystic duct merges with lower branch of the posterolateral segmental duct. This pattern has to be recognized correctly by the surgeon during LC in order to avoid misidentification and subsequent injury of the right posterior segmental duct.
LUS with the color Doppler application and transverse scanning generates the characteristic “Mickey Mouse” appearance of the CBD, portal vein, and common hepatic artery[22]. Occasionally, a prominent cystic duct that is parallel to the CBD can be identified in a “four tube sign”[23]. Hashimoto et al[42] studied the efficacy of LUS in identifying the cystic-common bile duct junction and found that LUS was inaccurate in 6% of patients, predominantly when the diameter of the CBD was less than 5 mm. In longitudinal scanning, LUS provides excellent anatomical information (Figure 1).
Figure 1.
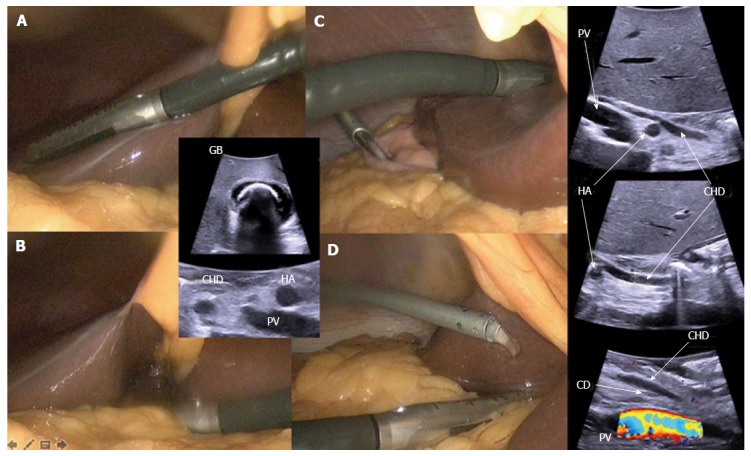
Laparoscopic ultrasonography: technique. Transversal approach - A: Through the liver; B: Directly on the hepatoduodenal pedicle. Longitudinal approach - C: Through the liver; D: Directly on the hepatoduodenal pedicle (isotonic solution’s irrigation that improves acoustic coupling). CD: Cystic duct junction with the the common bile duct; CHD: Common hepatic duct; HA: Hepatic artery; PV: Portal vein; GB: Gallbladder with macrolithiasis.
In order to complete a thorough examination of the biliary tract, the surgeon has to identify the biliary convergence with the left and right sectorial branches through the liver. Sequentially, the branch of the anterior right sector (direct extension of the CBD) is identified, followed by the posterior right sector duct. Then the gallbladder bed is visualized, followed by the walls of the gallbladder, then the trangential hepatic vein. This is a branch of the middle hepatic vein, tangential to the gallbladder bed, which is present in 15.38% of patients. When injured, this vein can provoke serious bleeding, mostly in cirrhotic patients[43-45]. A Doppler LUS is performed to identify the vascular anatomy and hepatic blood flux. The hepatoduodenal ligament is irrigated with an isotonic solution that improves acoustic coupling between the screened surface and probe. This permits analyses of the CBD (its integrity and diameter), the cystic duct, the junction between the cystic duct and the CBD, and the common hepatic duct and its intra-pancreatic portion (Figure 2). Other interesting anatomical findings include vascular variation or injuries[46], or even lymph nodes.
Figure 2.
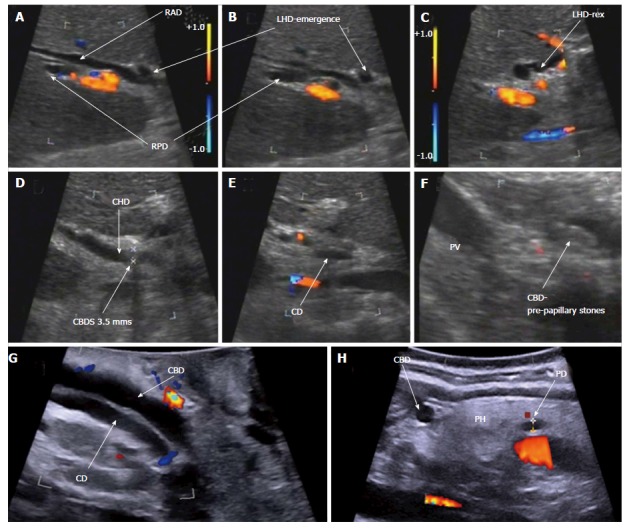
Laparoscopic ultrasonography: bile duct anatomy. A-C: Biliary convergence anatomy; D-F: Classical cystic duct junction with common bile ducts stones; G and H: Intra-pancreatic bile duct. RAD: Right anterior sector duct; RPD: Right posterior sector duct; LHD: Left hepatic duct; LHD-rex: Left hepatic duct at Rex recessus; CBDS: Common bile duct stones; CD (E): Cystic duct; CHD: Common hepatic duct; CBD: Common bile duct; CD (G): Cystic duct with low implantation in the common bile duct; PD: Pancreatic duct; PH: Pancreatic head.
An advantage of LUS is that it can be used before or after dissection of the Calot’s triangle, and, since it is not time consuming, can be repeated as needed. In the literature, 7 authors used LUS prior to dissection, and 7 after (Table 2). As shown in Table 2, LUS can be performed before or after dissection, according to perioperative findings, or before dissection to identify anatomy and systematically afterwards to confirm the correct dissection and absence of any injury. Considering the cystic duct-CBD junction, which is one of the most critical parts of the dissection, Hashimoto et al[42] , in a retrospective multicenter trial, reports an improved identification rate (of 98%) after dissection of the Calot’s triangle compared to 84% when LUS is completed before dissection. It is interesting to note that use of LUS at the end of the operation could be used to confirm the integrity of the common bile duct after clipping and transection of the cystic duct.
Table 2.
laparoscopic ultrasound performed pre- or post- dissection
| Author | Year | No. of patients | LUS pre-dissection | LUS post-dissection | |
| Tranter | 2001 | 367 | - | + | |
| Biffl | 2001 | 248 | + | + | |
| Catheline | 2002 | 900 | + | - | |
| Halpin | 2002 | 380 | - | + | |
| Tranter | 2003 | 135 | - | + | |
| Onders | 2005 | 105 | + | - | |
| Machi | 2007 | 200 | + | + | |
| Perry | 2007 | 236 | + | + | According to the situation |
| Hakamada | 2008 | 299 | + | +/- | After if necessary |
| Hublet | 2009 | 269 | - | + | |
| Li | 2009 | 103 | + | - | |
| Machi | 2009 | 1352 | + | +/- | After if necessary |
| Hashimoto | 2010 | 220 | + | + | |
| Pfluke | 2011 | 50 | - | + | |
| Nasu | 2012 | 71 | - | + | |
| Gwinn | 2013 | 44 | + | - | |
| Kothari | 2013 | 253 | + | - | |
| Shaaban | 2014 | 70 | - | + |
LUS: Laparoscopic ultrasound.
A review of the literature shows that most authors describe how to analyze the biliary tract, but very few provide details of the success with which each portion of the CBD is identified, which is essential in performing a safe LC. Table 3 provides data for the rates of “complete observation” and the ability of LUS to identify duct segments. According to these data, the rate of “complete observation” of the biliary tract with LUS ranged from 92%-100%, with very few reports providing an accurate rate of identification of each biliary duct segment. Complete anatomic analyses are reported in only four manuscripts[13,47-49], with vascular identification and/or variation in three[47,48,50]. Anatomic vascular and/or biliary variations have been described such as a foreshortened cystic duct in 14% of patients in a retrospective single center trial reported by Pfluke[47]), atypical cystic-bile duct junctions[51], aberrant hepatic ducts[47,51], or an accessory right hepatic artery[47].
Table 3.
Identification of biliary anatomy and variations
| Author | Year | No. of Patients | Complete observation | Intrahepatic BD | Bifurcation | CHD | CBD | CD-CBD junction | Intra-pancreatic BD | Vascular visualization | Biliary anomalies | Foreshortened cystic duct (< 1 cm) | Abnormal cystic duct anatomy | Aberrant vascular anatomy |
| Tranter | 2001 | 367 | 92% | 92% | 99% | |||||||||
| Halpin | 2002 | 380 | 90% | 95% | 94% | |||||||||
| Tranter | 2003 | 135 | 97.7% | |||||||||||
| Machi | 2007 | 200 | 96.5% | |||||||||||
| Perry | 2007 | 236 | 95.3% | 98.5% | 6.40% | |||||||||
| Hakamada | 2008 | 299 | 100% | 100%1 | 88.6%-97.1%2 | 88.6%-99.4%2 | 91.4%-100%2 | 88.6%-98.3%2 | 89.3%-100%2 | |||||
| Hublet | 2009 | 269 | 99% | |||||||||||
| Li | 2009 | 103 | 95.7% | 98.9 | 98.9% | 73.8% | ||||||||
| Machi | 2009 | 1352 | 98% | |||||||||||
| Hashimoto | 2010 | 200 | - | 94%3 | ||||||||||
| Pfluke | 2011 | 50 | 96% | 100% | 100% | 98% | 98% | 40% | 14% | 8% | 16%4 | |||
| Gwinn | 2013 | 44 | 100% |
Not influenced by inflammation;
Influenced by inflammation;
Junction not identified when CBD < 5 mm;
Accessory RHA (right hepatic artery) 8%, replaced RHA 6%, anterior cystic artery 2%. CHD: Common hepatic duct; CBD: Common bile duct.
Even if LUS imaging of the CBD provides excellent accuracy (Table 3), visualization of the intra-pancreatic portion appears to be more challenging, with rates of complete delineation ranging from 73% to 100%[12,13,47-49].
In a meta-analysis performed by Jamal et al[38] there was no significant difference between IOC and LUS in identifying the extra-pancreatic CBD, but IOC appeared to be more efficient in delineating the intra-pancreatic CBD. Other authors report discontinuous mapping of the biliary tract. In a prospective non-randomized trial, Halpin et al[13] reports discontinuous screening of the middle and/or distal CBD in 10% of patients. This agrees with other studies reporting rates of discontinuous mapping of the CBD of 4%-17%[20,52]. In Halpin’s experience, this did not translate into increased false negatives with LUS.
LUS and acute or chronic inflammatory disease
A major impediment to the conclusion of LC is the inability to identify, with surety, the location of the extra-hepatic bile duct and to assess its relationship with the gallbladder when the hepatoduodenal anatomy is obscured. Cholangitis or previous pancreatitis may render access to the biliary tract difficult. In such cases the risk of major bile duct and/or vascular injury is substantial, even for the most adept HPB surgeon. IOC is not possible without dissection. In such hazardous situations, LUS can be a valuable adjunct and can be performed before dissection, and repeated as needed to guide the surgeon. Many authors report their experience of LUS in scenarios of inflammatory disease (Table 4).
Table 4.
Reports of laparoscopic ultrasound used during acute or chronic cholecystitis
| Author | Year | No. of patients | Inflammatory disease % | Comments |
| Biffl | 2001 | 248 | 37.5 | |
| Catheline | 2002 | 900 | 28.2 | |
| Onders | 2005 | 105 | 6.3 | |
| Machi | 2007 | 200 | 28.5 | |
| Perry | 2007 | 236 | 5.5 | LUS considered extremely valuable in 5.5% |
| Hakamada | 2008 | 299 | 66.3 | 13.4% with severe inflammatory disease during 2nd period of study |
| Machi | 2009 | 1352 | 20.9 | LUS considered extremely valuable in 5.9% |
| Pfluke | 2011 | 50 | 66.0 | |
| Gwinn | 2013 | 44 | 100.0 |
LUS: Laparoscopic ultrasound.
Gwinn et al[53], in a prospective non randomized trial, reports a rate of 100% complete biliary tract analysis even with acute inflammation. In that study, LUS was critical in performing LC during acute cholecystitis in all 44 patients whose anatomy was obscured by acute or chronic cholecystitis, with a rate of 34.1% of gangrenous cholecystitis, but no mention of the fibrotic percentage. During the operation, for all cases, LUS was used to identify with precision the anatomy of the cystic duct, CBD, and the cystic duct-CBD junction. Indeed LUS was considered to be a crucial tool in avoiding conversion in 91% of patients[53] , with no BDIs observed. It seems that even when complete visualization of the biliary tract is difficult to achieve because of inflammatory disease or fibrosis, the most important dissection targets (cystic duct, CBD, and the cystic duct-CBD junction) can still be finely identified.
Machi et al[54], in a multicenter study that included 1352 patients, reported a feasibility rate for LUS of 98%, even with 20.90% of cases presenting with inflammatory disease. In their report, LUS proved to be remarkably valuable, given that mapping of the biliary tract avoided conversion in 5.9% of patients with anatomy obscured due to Mirizzi’s syndrome, acute or chronic cholecystitis, or pancreatitis. Even though no comment was made in this report considering the particularly difficult situation of fibrosis, 79.1% of patients were considered to be in a state of chronic cholecystitis. Biffl et al[55] in a prospective non-randomized study showed that LUS provided an excellent guide for dissection as its routine use during acute cholecystitis allowed operations to be completed with lower conversion rates than seen with patients operated on without LUS (P = 0.09). According to these data, LUS seems to play an essential role in mapping the biliary and hilar trunk when the anatomy is obscured such as in the fibrotic or inflammatory state. The possibility of identifying the anatomy before and/or during dissection could be one of this technique’s most valuable aspects.
Conversely, other authors have suggested that inflammation may hinder LUS analysis[51]. For example, Hakamada et al[48] , in a retrospective single center study, reported a high analysis rate for the complete biliary tract in LC for cholecystolithiasis, which then fell according to the severity of inflammation, while preserving an excellent feasibility rate of 100%.
LUS and biliary duct injury
BDI is a dreaded complication during cholecystectomy. The incidence of BDI during LC remains at 0.3%-0.6%[3], with a trend suggesting its diminution as surgical experience and expertise is acquired[4]. BDI combined with vascular injury is observed in 12% of patients, which may negatively impact treatment and recovery[56].
BDIs are best prevented by fine dissection using different techniques as recommended for simple vs more complex LC cases[57,58]. Described by Strasberg et al[28] in 1995, the critical view of safety (CVS), a systematic dissection that skeletonizes the Calot’s triangle and delineates the relationship of anatomic structures, has been suggested to play a protective role against BD1[59-61]. A drop in BDIs following the implementation of CVS as a dissection principle during LC was documented by Yamashita et al[62] in a Japanese report. Despite this evidence, CVS still appears to be underutilized by surgeons in current practice[36], and may even be insufficient in terms of minimizing CBDI. Further, major CBDIs continue to occur, even for surgical teams that have adopted CVS as a standard dissection technique as reported by de Reuver et al[63].
In 1996, Birth et al[18] reported a 100% recognition rate of BDIs using LUS in an experimental animal study without blinding (i.e., surgeons knew that BDIs were present). These data may therefore be biased and should be interpreted with caution.
Data for LUS and the prevention or detection of BDIs are sparse. Across the studies reviewed (Table 1), no BDIs were reported with only 2 studies emphasizing the importance of combining CVS and LUS[12,47]. However, delineation of the CBD, the possibility to repeat LUS during the procedure either before or after dissection, and the ability of LUS to detect aberrant vascular anatomy[47] may collectively play a role in preventing bile duct and vascular injuries. As an example, using LUS, Hublet et al[12] identified a stenosing clip placed too close to the junction between the CBD and CD, in a patient with a normal IOC. This underlines the fact that CBDI can still occur after IOC. Thanks to LUS performed at the very end of the operation, a diagnosis of CBD stenosis was made with subsequent repair, avoiding potential major postoperative complications.
LUS and common bile duct stones
The presence or absence of CBDS can be predicted to some extent using preoperative criteria, but these fail to reach 100% accuracy[64,65]. Catheline et al[20], in a retrospective trial published in 1999, reported a perioperative CBDS detection rate of 9%. In this group of patients, 30% manifested no preoperative risk factors. Olsen et al[24], in a prospective non randomized study, recorded 12% of patients as having CBDS, even after preoperative clearance by endoscopic retrograde cholangiopancreatography (ERCP). Thanks to LUS, CBDS can be identified early during the procedure, which gives the operating room personnel time to set up the required CBDS exploration equipment.
The sensitivity and specificity provided by LUS in detecting CBDS is very good (Table 5). In 2003, Tranter et al[66] , in a prospective non randomized study, reported specificity and sensitivity rates of 96% and 100%, respectively, compared to sensitivity and specificity rates of 86% and 99% in IOC. In another prospective non randomized study, Li et al[49] also observed higher sensitivity rates for LUS vs IOC (82.1% vs 75%), and an equal specificity rate of 98.7%.
Table 5.
Common bile duct stones identification
| Author | Year | No. of patients | Sensitivity % | Specificity % |
Criteria to evaluate CBS LUS accuracy |
||
| IOC | ERCP/surgical exploration | Follow-up | |||||
| Tranter | 2001 | 367 | 92 | 100 | Selective | + | + |
| Biffl | 2001 | 248 | 100 | 96.23 | ni | ||
| Halpin | 2002 | 380 | 97.5 | 100 | Selective | + | + |
| Catheline | 2002 | 900 | 80 | 99 | Systematic | ||
| Tranter | 2003 | 135 | 96 | 100 | Systematic | ||
| Onders | 2005 | 105 | 100 | 100 | Selective | + | |
| Perry | 2007 | 236 | 92.3 | 100 | Selective | + | |
| Machi | 2007 | 200 | 95 | 100 | Selective | + | + |
| Hakamada | 2008 | 299 | 76 | 99 | Selective | ||
| Machi | 2009 | 1352 | 98.6 | 99.58 | 1 | + | |
| Hublet | 2009 | 269 | 100 | 99.6 | Selective | + | |
| Li | 2009 | 103 | 82.1 | 98.7 | Selective | + | + |
| Pfluke | 2011 | 50 | 100 | 100 | Selective | ||
| Nasu | 2012 | 71 | 100 | 96.2 | Selective | ||
| Shaaban | 2014 | 70 | 92.3 | 98.2 | No | + | + |
Selective or systematic, according to center. ni: No information; LUS: Laparoscopic ultrasound; IOC: Intraoperative cholangiography; ERCP: Endoscopic retrograde cholangiopancreatography.
A meta-analysis of the literature performed by Jamal et al[38] confirmed a sensitivity and sensitivity rate for LUS that was superior to IOC (0.90 and 0.99 for LUS vs 0.87 and 0.98 for IOC, respectively), with heterogeneity found to be insignificant. In agreement with this observation, Aziz et al[37], in another meta-analysis, suggested that LUS is very accurate in detecting CBDS (pooled sensitivity of 0.87, and specificity of 1.00) vs IOC (pooled sensitivity of 0.87, and specificity of 0.99).
The measurement of CBD diameter was performed and reported in several studies[13,66-68]. In 2001, Tranter et al[68] observed that when dealing with a thin CBD (< 5 mm) there should be no concern regarding CBDS. In these circumstances, LUS could be an excellent negative predictor. Two years later, the same author reported[66] that for CBDs of between 6-10 mm in diameter, there was a large overlap between ducts with or without stones; 85% of ducts > 10 mm in width contained stones.
Considering sludge, defined as small areas (< 1 mm) of mobile echogenic material without acoustic shadowing, their clinical significance remains debatable, with some studies suggesting that sludge is related with acute pancreatitis[69,70] or cholangitis[71]. LUS appears to be more accurate in these diagnoses than IOC. Halpin et al[13] , in a prospective non randomized study, detected 14% of patients with sludge in the LUS group, but no diagnoses were made for the IOC group. This allowed the surgeon to proceed to a non-invasive treatment, such as saline flush via the cystic duct combined with glucagon injection. On the other hand, Halpin’s experience was that 62% of patients with sludge underwent no treatment, with no adverse events. Other authors also adopted a “wait and see” approach to sludge with good results[51]. The high detection rate of LUS agrees with reports observing a high accuracy of detection of microlithiasis by echoendoscopic examination[72].
In IOC, a higher number of false positive examinations may be due to micro-bubbles[73] or Oddi’s contractions. These drawbacks are not applicable to LUS. In LUS, only exceptional false positive examinations have been reported due to confusing pancreatic head micro-calcifications with CBDS[54].
To conclude, this literature review suggests that LUS is, at the very least, equivalent to IOC in terms of detecting choledocholithiasis, and may be more specific, leading to fewer negative explorations. It is important to note that LUS and IOC may be complementary, as combining the 2 techniques maximizes the intraoperative detection of CBDS, with a sensitivity rate of 95% and a specificity rate of 98%[73,49].
LUS and incidental findings
LUS has the benefit of substituting for the lack of tactile palpation during LC, and allows scanning of other organs such that additional underlying pathology can be identified. Liver abscesses or tumors, suspicious lesions in the gallbladder wall, or diverticulum of the common bile duct can be detected[25]. In 1995, in a prospective non randomized study, Stiegmann et al[19] reported the LUS identification of a large hilar lymph node, from which a frozen section was used to diagnose gallbladder carcinoma.
In the series published after 2000 (Table 6), Hublet et al[12], in a prospective non randomized study, reported the diagnosis of one case with hemobilia (which could have been interpreted as a filling defect in IOC imaging), 1 pancreatic pseudocyst, 1 case of IPMN, 1 pancreas divisum, and 1 patient with micro-calcifications of the head of the pancreas. Other authors report the identification of gallbladder polyps[74], Mirizzi syndrome[50], lobar atrophy/hypertrophy, or rotational anomalies of the liver[54]. In a prospective non randomized study published in 2007, Machi et al[51] diagnosed cystic or solid tumors of the liver or pancreas during systematic examination via LUS. Thus, LUS permitted the surgeon to proceed to biopsy or aspiration, and even radiofrequency ablation of tumors in 6 cases. Even if it remains unclear as to whether these tumors were incidental perioperative findings, or were diagnosed during the preoperative workup, LUS permitted localization of the disease, biopsy, and even treatment.
Table 6.
Incidental findings
| Author | Year | No. of patients examined using LUS | Incidental findings |
| Machi | 2007 | 200 | Cystic or solid tumors of the liver or pancreas in 31 patients; 14 biopsies and aspirations, 6 radiofrequency ablations |
| Perry | 2007 | 236 | Atrophic/hypertrophic or rotational anomalies or the liver, Mirizzi syndrome, vascular anomalies |
| Hakamada | 2008 | 299 | Polyps |
| Hublet | 2009 | 269 | 1 hemobilia, 1 pancreatic pseudocyst, 1 IPMT, 1 pancreas divisum, 1 micro-calcification of the pancreatic head, 1 liver abscess, 1 liver tumor |
| Machi | 2009 | 1352 | Atrophic/hypertrophic or rotational anomalies or the liver, Mirizzi syndrome, vascular anomalies |
| Gwinn | 2013 | 44 | 2 hepatic rotation anomalies |
| Kothari | 2013 | 253 | Polyps. Improved visualization of gallbladder walls in obese patient compared to trans-abdominal US |
LUS: Laparoscopic ultrasound.
Speed of the process
LUS can be completed more rapidly than IOC[38,48,73,75]. Catheline et al[73], in a prospective non randomized study, reports a LUS duration of 9.8 min vs 17.6 min for IOC. Further, in order to perform IOC, a radiological device, together with a technician capable of operating the device are needed. While surgical experience in using LUS seemed to significantly influence the operating time for cholecystolithiasis[48], Halpin et al[13] observed no differences when dealing with acute cholecystitis.
Learning curve
The number of LUS examinations performed as part of the learning curve varied in reports[13,48,67], with a broad agreement that the learning curve was greater than for IOC. What seems to be evident from the literature review is that surgeons that take the time and effort to perform LUS, not only become very efficient and accurate in their diagnoses, but also modify their practice. These surgeons use IOC more selectively and rarely[12,50]. Given that the accuracy of LUS improves with the expertise of the operator, standardization of the examination is essential.
Costs
In 2016, Sun et al[76] evaluated the cost effectiveness of LUS, IOC for the investigation of silent CBDS during LC. The authors concluded that LUS is a more cost-effective strategy than IOC.
DISCUSSION
During laparoscopic cholecystectomy, mapping of the dissection targets such as the common bile duct, cystic duct, and hilar vascular structures, is crucial for safely completing the operation. While careful dissection avoids injury, this may be difficult to achieve in the presence of fibrosis or extensive inflammation, or when there is an aberrant biliary anatomy (and/or a very short cystic duct).
The debate is ongoing as to whether an analysis of the hilar anatomy during cholecystectomy may help to prevent injury and postoperative complications. Many surgeons perform no analyses given that the proposed “gold standard” technique (IOC) has its own drawbacks including irradiation of the patient and the surgical team, dissection of the Calot’s triangle to identify the cystic duct, and cannulation of the cystic duct which may cause avulsion or perforation. IOC is also considered to be expensive and time-consuming.
On the other hand, LUS, which has a long history of use (> 30 years), allows a quick, repeatable, highly successful, non-irradiating, and non-invasive study of the biliary tract. In difficult scenarios, when anatomical structures are obscured, such as during inflammation or fibrosis, LUS can be pivotal to the success of the procedure, and is easily performed before the dissection in order to guide the surgeon. With the added advantage of re-use on demand during the operation as it is neither time-consuming nor expensive. Indeed, LUS provides an excellent analysis of the CBD, even if it would appear to be less accurate than IOC in the study of the intra-pancreatic segment of the bile duct.
Considering aberrant biliary anatomy, such as a cystic duct originating from the right posterior sector, very few authors provide detailed anatomical descriptions. More results for the precise anatomical evaluation, segment by segment, are warranted. Nevertheless, it seems that, in experienced hands, LUS can provide a precisely mapped biliary duct. When analyzing the cystic-common bile duct junction, a short cystic duct, or even Mirizzi’s syndrome, LUS might be effective in clarifying the anatomy and even preventing conversion.
While no precise data concerning the prevention of BDIs were reported, the ability to delineate anatomy may have a protective role as no BDIs were described in the reviewed series, even when patients with acute or chronic inflammatory disease were included.
The ability of LUS to detect CBDS and sludge is at least as good, if not better than IOC, and provides fewer false positive examinations. Moreover, LUS contributes to a complete examination of the adjacent organs, which allows for diagnoses of incidental pathology.
Finally, the use of LUS is not exclusive. IOC can be of importance in many situations. Consequently, any surgeon should be able to use both techniques, which are complementary in detecting common bile duct stones. Further, the advantages of LUS have led to the authors using this technique as a first line procedure.
A limitation of this review is that it is based on a relatively small number of non-randomized trials, with a limited number of patients, with heterogeneous, non standardized criteria in terms of anatomical analysis. Unfortunately, no specific data could be found for the hazardous situation of fibrosis, which is instead necessarily included in a broader “difficult” category.
To conclude, a large panel of techniques has been described that clarify anatomy during laparoscopic cholecystectomy. However, of these techniques, LUS would appear to be the most suitable as it provides the greatest number of advantages and can be used during other types of operation. LUS is also, probably, the most cost-effective, which is an essential quality in an era of financial constraints. The principal hurdle for the adoption of LUS as a standard imaging technique of the CBD during LC appears to be the reticence of surgeons, probably because of its supposed lengthy learning curve. However, as ultrasound and laparoscopy become standard techniques in modern surgery, most surgical trainees and junior surgeons will be exposed to them, and will be more inclined to include them in their skill set. In this fashion, we envisage that the reluctance to use LUS will become obsolete. Moreover, surgeons should consider that implementation of LUS during LC could serve as a valuable exercise to gain familiarity with a technique that should prove useful for multiple operations.
COMMENTS
Background
The detection of common bile duct stones and bile duct injury prevention remain hot topics in laparoscopic cholecystectomy, more so now that the laparoscopic approach is standardly used, even in difficult cases with acute or chronic inflammation and fibrosis. As a companion technique, intraoperative cholangiography (IOC) is usually proposed as the “gold standard” analysis method. Laparoscopic ultrasonography (LUS) is much less evaluated.
Research frontiers
LUS during cholecystectomy is a well-known technique described from more than 30 years ago. However as less than 1% of surgeons seem to adopt it probably due to its supposed longer learning curve. The specific benefits and the performance of the technique has to be been evaluated.
Innovations and breakthroughs
All manuscripts concerning the performance of LUS during laparoscopic cholecystectomy from the year 2000 were reviewed by the authors with a view to the performance of anatomical mapping, even with background inflammation.
Applications
This review confirmed the clinical benefits of LUS during cholecystectomy, especially in difficult situations. Compared to IOC, LUS remains under-used. Greater uptake of this technique by young surgeons, backed by large-scale studies to confirm its clinical impact, should help to eliminate the discrepancy between use and value.
Peer-review
In this review the authors present a critical analysis of the literature, from the year 2000, for the use of LUS during cholecystectomy and its performance in mapping the anatomy of the bile duct, detecting common bile duct stones, and preventing bile duct injury. A particular emphasis has been placed on complex inflammatory situations.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Belgium
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: No potential conflicts of interest.
Data sharing statement: These data were extracted from the referenced articles and are already in the public domain.
Peer-review started: February 8, 2017
First decision: March 3, 2017
Article in press: June 19, 2017
P- Reviewer: Chang YC, Kanat BH, Paduani GF S- Editor: Gong ZM L- Editor: A E- Editor: Li D
References
- 1.Wong-Lun-Hing EM, Lodewick TM, Stoot JH, Bemelmans MH, Olde Damink SW, Dejong CH, van Dam RM. A survey in the hepatopancreatobiliary community on ways to enhance patient recovery. HPB (Oxford) 2012;14:818–827. doi: 10.1111/j.1477-2574.2012.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallstones and laparoscopic cholecystectomy. NIH Consensus Development Panel on Gallstones and Laparoscopic Cholecystectomy. Surg Endosc. 1993;7:271–279. [PubMed] [Google Scholar]
- 3.Hogan NM, Dorcaratto D, Hogan AM, Nasirawan F, McEntee P, Maguire D, Geoghegan J, Traynor O, Winter DC, Hoti E. Iatrogenic common bile duct injuries: Increasing complexity in the laparoscopic era: A prospective cohort study. Int J Surg. 2016;33 Pt A:151–156. doi: 10.1016/j.ijsu.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Halbert C, Pagkratis S, Yang J, Meng Z, Altieri MS, Parikh P, Pryor A, Talamini M, Telem DA. Beyond the learning curve: incidence of bile duct injuries following laparoscopic cholecystectomy normalize to open in the modern era. Surg Endosc. 2016;30:2239–2243. doi: 10.1007/s00464-015-4485-2. [DOI] [PubMed] [Google Scholar]
- 5.Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, Hunter JG. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–469. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93:158–168. doi: 10.1002/bjs.5266. [DOI] [PubMed] [Google Scholar]
- 7.Buddingh KT, Nieuwenhuijs VB, van Buuren L, Hulscher JB, de Jong JS, van Dam GM. Intraoperative assessment of biliary anatomy for prevention of bile duct injury: a review of current and future patient safety interventions. Surg Endosc. 2011;25:2449–2461. doi: 10.1007/s00464-011-1639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sajid MS, Leaver C, Haider Z, Worthington T, Karanjia N, Singh KK. Routine on-table cholangiography during cholecystectomy: a systematic review. Ann R Coll Surg Engl. 2012;94:375–380. doi: 10.1308/003588412X13373405385331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slim K, Martin G. Does routine intra-operative cholangiography reduce the risk of biliary injury during laparoscopic cholecystectomy? An evidence-based approach. J Visc Surg. 2013;150:321–324. doi: 10.1016/j.jviscsurg.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Ford JA, Soop M, Du J, Loveday BP, Rodgers M. Systematic review of intraoperative cholangiography in cholecystectomy. Br J Surg. 2012;99:160–167. doi: 10.1002/bjs.7809. [DOI] [PubMed] [Google Scholar]
- 11.Sheffield KM, Han Y, Kuo YF, Townsend CM, Goodwin JS, Riall TS. Variation in the use of intraoperative cholangiography during cholecystectomy. J Am Coll Surg. 2012;214:668–679; discussion 679-681. doi: 10.1016/j.jamcollsurg.2011.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hublet A, Dili A, Lemaire J, Mansvelt B, Molle G, Bertrand C. Laparoscopic ultrasonography as a good alternative to intraoperative cholangiography (IOC) during laparoscopic cholecystectomy: results of prospective study. Acta Chir Belg. 2009;109:312–316. doi: 10.1080/00015458.2009.11680431. [DOI] [PubMed] [Google Scholar]
- 13.Halpin VJ, Dunnegan D, Soper NJ. Laparoscopic intracorporeal ultrasound versus fluoroscopic intraoperative cholangiography: after the learning curve. Surg Endosc. 2002;16:336–341. doi: 10.1007/s00464-001-8325-1. [DOI] [PubMed] [Google Scholar]
- 14.El Shallaly G, Seow C, Sharp C, Mughrabi A, Nassar AH. Intraoperative cholangiography time in laparoscopic cholecystectomy: timing the radiographer. Surg Endosc. 2005;19:1370–1372. doi: 10.1007/s00464-004-2242-z. [DOI] [PubMed] [Google Scholar]
- 15.Karthikesalingam A, Markar SR, Weerakkody R, Walsh SR, Carroll N, Praseedom RK. Radiation exposure during laparoscopic cholecystectomy with routine intraoperative cholangiography. Surg Endosc. 2009;23:1845–1848. doi: 10.1007/s00464-008-0279-0. [DOI] [PubMed] [Google Scholar]
- 16.Falcone RA, Fegelman EJ, Nussbaum MS, Brown DL, Bebbe TM, Merhar GL, Johannigman JA, Luchette FA, Davis K, Hurst JM. A prospective comparison of laparoscopic ultrasound vs intraoperative cholangiogram during laparoscopic cholecystectomy. Surg Endosc. 1999;13:784–788. doi: 10.1007/s004649901099. [DOI] [PubMed] [Google Scholar]
- 17.Birth M, Roblick U, Brugmans F, Weiser HF, Bruch HP. Laparoscopic ultrasonography reliably visualizes bile-duct injuries - a blind randomized porcine study. Langenbecks Arch Surg. 1999;384:360–365. doi: 10.1007/s004230050214. [DOI] [PubMed] [Google Scholar]
- 18.Birth M, Carroll BJ, Delinikolas K, Eichler M, Weiser H. Recognition of laparoscopic bile duct injuries by intraoperative ultrasonography. Surg Endosc. 1996;10:794–797. doi: 10.1007/BF00189535. [DOI] [PubMed] [Google Scholar]
- 19.Stiegmann GV, Soper NJ, Filipi CJ, McIntyre RC, Callery MP, Cordova JF. Laparoscopic ultrasonography as compared with static or dynamic cholangiography at laparoscopic cholecystectomy. A prospective multicenter trial. Surg Endosc. 1995;9:1269–1273. doi: 10.1007/BF00190157. [DOI] [PubMed] [Google Scholar]
- 20.Catheline J, Rizk N, Champault G. A comparison of laparoscopic ultrasound versus cholangiography in the evaluation of the biliary tree during laparoscopic cholecystectomy. Eur J Ultrasound. 1999;10:1–9. doi: 10.1016/s0929-8266(99)00028-2. [DOI] [PubMed] [Google Scholar]
- 21.Wu JS, Dunnegan DL, Soper NJ. The utility of intracorporeal ultrasonography for screening of the bile duct during laparoscopic cholecystectomy. J Gastrointest Surg. 1998;2:50–60. doi: 10.1016/s1091-255x(98)80103-0. [DOI] [PubMed] [Google Scholar]
- 22.Rijna H, Eijsbouts QA, Barkhof F, de Brauw LM, Cuesta MA. Assessment of the biliary tract by ultrasonography and cholangiography during laparoscopic cholecystectomy: a prospective study. Eur J Ultrasound. 1999;9:127–133. doi: 10.1016/s0929-8266(99)00018-x. [DOI] [PubMed] [Google Scholar]
- 23.Siperstein A, Pearl J, Macho J, Hansen P, Gitomirsky A, Rogers S. Comparison of laparoscopic ultrasonography and fluorocholangiography in 300 patients undergoing laparoscopic cholecystectomy. Surg Endosc. 1999;13:113–117. doi: 10.1007/s004649900917. [DOI] [PubMed] [Google Scholar]
- 24.Olsen AK, Bjerkeset OA. Laparoscopic ultrasound (LUS) in gastrointestinal surgery. Eur J Ultrasound. 1999;10:159–170. doi: 10.1016/s0929-8266(99)00053-1. [DOI] [PubMed] [Google Scholar]
- 25.Ohtani T, Kawai C, Shirai Y, Kawakami K, Yoshida K, Hatakeyama K. Intraoperative ultrasonography versus cholangiography during laparoscopic cholecystectomy: a prospective comparative study. J Am Coll Surg. 1997;185:274–282. doi: 10.1016/s1072-7515(97)00030-6. [DOI] [PubMed] [Google Scholar]
- 26.Soper NJ. Intraoperative detection: intraoperative cholangiography vs. intraoperative ultrasonography. J Gastrointest Surg. 2000;4:334–335. doi: 10.1016/s1091-255x(00)80003-7. [DOI] [PubMed] [Google Scholar]
- 27.Santambrogio R, Montorsi M, Bianchi P, Opocher E, Verga M, Panzera M, Cosentino F. Common bile duct exploration and laparoscopic cholecystectomy: role of intraoperative ultrasonography. J Am Coll Surg. 1997;185:40–48. doi: 10.1016/s1072-7515(97)00013-6. [DOI] [PubMed] [Google Scholar]
- 28.Strasberg SM, Herti M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J AM Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 29.Machi J. Accuracy of intraoperative ultrasound and cholangiography. Surg Endosc. 1996;10:363–364. doi: 10.1007/BF00187397. [DOI] [PubMed] [Google Scholar]
- 30.Kelly SB, Remedios D, Lau WY, Li AK. Laparoscopic ultrasonography during laparoscopic cholecystectomy. Surg Endosc. 1997;11:67–70. doi: 10.1007/s004649900297. [DOI] [PubMed] [Google Scholar]
- 31.Röthlin MA, Schöb O, Schlumpf R, Largiadèr F. Laparoscopic ultrasonography during cholecystectomy. Br J Surg. 1996;83:1512–1516. doi: 10.1002/bjs.1800831107. [DOI] [PubMed] [Google Scholar]
- 32.Tomonaga T, Filipi CJ, Lowham A, Martinez T. Laparoscopic intracorporeal ultrasound cystic duct length measurement: a new technique to prevent common bile duct injuries. Surg Endosc. 1999;13:183–185. doi: 10.1007/s004649900935. [DOI] [PubMed] [Google Scholar]
- 33.Kubota K, Bandai Y, Sano K, Teruya M, Ishizaki Y, Makuuchi M. Appraisal of intraoperative ultrasonography during laparoscopic cholecystectomy. Surgery. 1995;118:555–561. doi: 10.1016/s0039-6060(05)80373-3. [DOI] [PubMed] [Google Scholar]
- 34.Barteau JA, Castro D, Arregui ME, Tetik C. A comparison of intraoperative ultrasound versus cholangiography in the evaluation of the common bile duct during laparoscopic cholecystectomy. Surg Endosc. 1995;9:490–496. doi: 10.1007/BF00206833. [DOI] [PubMed] [Google Scholar]
- 35.Santambrogio R, Bianchi P, Opocher E, Mantovani A, Schubert L, Ghelma F, Panzera M, Verga M, Spina GP. Intraoperative ultrasonography (IOUS) during laparoscopic cholecystectomy. Surg Endosc. 1996;10:622–627. doi: 10.1007/BF00188514. [DOI] [PubMed] [Google Scholar]
- 36.Daly SC, Deziel DJ, Li X, Thaqi M, Millikan KW, Myers JA, Bonomo S, Luu MB. Current practices in biliary surgery: Do we practice what we teach? Surg Endosc. 2016;30:3345–3350. doi: 10.1007/s00464-015-4609-8. [DOI] [PubMed] [Google Scholar]
- 37.Aziz O, Ashrafian H, Jones C, Harling L, Kumar S, Garas G, Holme T, Darzi A, Zacharakis E, Athanasiou T. Laparoscopic ultrasonography versus intra-operative cholangiogram for the detection of common bile duct stones during laparoscopic cholecystectomy: a meta-analysis of diagnostic accuracy. Int J Surg. 2014;12:712–719. doi: 10.1016/j.ijsu.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 38.Jamal KN, Smith H, Ratnasingham K, Siddiqui MR, McLachlan G, Belgaumkar AP. Meta-analysis of the diagnostic accuracy of laparoscopic ultrasonography and intraoperative cholangiography in detection of common bile duct stones. Ann R Coll Surg Engl. 2016;98:244–249. doi: 10.1308/rcsann.2016.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babel N, Sakpal SV, Paragi P, Wellen J, Feldman S, Chamberlain RS. Iatrogenic bile duct injury associated with anomalies of the right hepatic sectoral ducts: a misunderstood and underappreciated problem. HPB Surg. 2009;2009:153269. doi: 10.1155/2009/153269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Izuishi K, Toyama Y, Nakano S, Goda F, Usuki H, Masaki T, Maeta H. Preoperative assessment of the aberrant bile duct using multislice computed tomography cholangiography. Am J Surg. 2005;189:53–55. doi: 10.1016/j.amjsurg.2004.06.039. [DOI] [PubMed] [Google Scholar]
- 41.Yoshida J, Chijiiwa K, Yamaguchi K, Yokohata K, Tanaka M. Practical classification of the branching types of the biliary tree: an analysis of 1,094 consecutive direct cholangiograms. J Am Coll Surg. 1996;182:37–40. [PubMed] [Google Scholar]
- 42.Hashimoto M, Matsuda M, Watanabe G. Intraoperative ultrasonography for reducing bile duct injury during laparoscopic cholecystectomy. Hepatogastroenterology. 2010;57:706–709. [PubMed] [Google Scholar]
- 43.Shen BY, Li HW, Chen M, Zheng MH, Zang L, Jiang SM, Li JW, Jiang Y. Color Doppler ultrasonographic assessment of the risk of injury to major branch of the middle hepatic vein during laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2003;2:126–130. [PubMed] [Google Scholar]
- 44.Yau HM, Lee KT, Kao EL, Chuang HY, Chou SH, Huang MF. Color Doppler ultrasound detection and classification of the tangential hepatic vein before laparoscopic cholecystectomy. Surg Endosc. 2005;19:1377–1380. doi: 10.1007/s00464-004-2251-y. [DOI] [PubMed] [Google Scholar]
- 45.Misawa T, Koike M, Suzuki K, Unemura Y, Murai R, Yoshida K, Kobayashi S, Yamazaki Y. Ultrasonographic assessment of the risk of injury to branches of the middle hepatic vein during laparoscopic cholecystectomy. Am J Surg. 1999;178:418–421. doi: 10.1016/s0002-9610(99)00202-0. [DOI] [PubMed] [Google Scholar]
- 46.Birth M, Lossin P, Brugmans F, Weiser HF. Vascular injuries within the hepatoduodenal ligament: recognition by laparoscopic color Doppler ultrasound. Surg Endosc. 2000;14:246–249. doi: 10.1007/s004640000028. [DOI] [PubMed] [Google Scholar]
- 47.Pfluke JM, Bowers SP. Laparoscopic intraoperative biliary ultrasonography: findings during laparoscopic cholecystectomy for acute disease. J Laparoendosc Adv Surg Tech A. 2011;21:505–509. doi: 10.1089/lap.2010.0280. [DOI] [PubMed] [Google Scholar]
- 48.Hakamada K, Narumi S, Toyoki Y, Nara M, Oohashi M, Miura T, Jin H, Yoshihara S, Sugai M, Sasaki M. Intraoperative ultrasound as an educational guide for laparoscopic biliary surgery. World J Gastroenterol. 2008;14:2370–2376. doi: 10.3748/wjg.14.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li JW, Feng B, Wu L, Wang ML, Lu AG, Zang L, Mao ZH, Dong F, Zheng MH. Intraoperative cholangiography in combination with laparoscopic ultrasonography for the detection of occult choledocholithiasis. Med Sci Monit. 2009;15:MT126–MT130. [PubMed] [Google Scholar]
- 50.Perry KA, Myers JA, Deziel DJ. Laparoscopic ultrasound as the primary method for bile duct imaging during cholecystectomy. Surg Endosc. 2008;22:208–213. doi: 10.1007/s00464-007-9558-4. [DOI] [PubMed] [Google Scholar]
- 51.Machi J, Oishi AJ, Tajiri T, Murayama KM, Furumoto NL, Oishi RH. Routine laparoscopic ultrasound can significantly reduce the need for selective intraoperative cholangiography during cholecystectomy. Surg Endosc. 2007;21:270–274. doi: 10.1007/s00464-005-0817-y. [DOI] [PubMed] [Google Scholar]
- 52.Catheline JM, Turner R, Rizk N, Barrat C, Buenos P, Champault G. Evaluation of the biliary tree during laparoscopic cholecystectomy: laparoscopic ultrasound versus intraoperative cholangiography: a prospective study of 150 cases. Surg Laparosc Endosc. 1998;8:85–91. [PubMed] [Google Scholar]
- 53.Gwinn EC, Daly S, Deziel DJ. The use of laparoscopic ultrasound in difficult cholecystectomy cases significantly decreases morbidity. Surgery. 2013;154:909–915; discussion 915-917. doi: 10.1016/j.surg.2013.04.041. [DOI] [PubMed] [Google Scholar]
- 54.Machi J, Johnson JO, Deziel DJ, Soper NJ, Berber E, Siperstein A, Hata M, Patel A, Singh K, Arregui ME. The routine use of laparoscopic ultrasound decreases bile duct injury: a multicenter study. Surg Endosc. 2009;23:384–388. doi: 10.1007/s00464-008-9985-x. [DOI] [PubMed] [Google Scholar]
- 55.Biffl WL, Moore EE, Offner PJ, Franciose RJ, Burch JM. Routine intraoperative laparoscopic ultrasonography with selective cholangiography reduces bile duct complications during laparoscopic cholecystectomy. J Am Coll Surg. 2001;193:272–280. doi: 10.1016/s1072-7515(01)00991-7. [DOI] [PubMed] [Google Scholar]
- 56.Deziel DJ. Complications of cholecystectomy. Incidence, clinical manifestations, and diagnosis. Surg Clin North Am. 1994;74:809–823. [PubMed] [Google Scholar]
- 57.Zha Y, Chen XR, Luo D, Jin Y. The prevention of major bile duct injures in laparoscopic cholecystectomy: the experience with 13,000 patients in a single center. Surg Laparosc Endosc Percutan Tech. 2010;20:378–383. doi: 10.1097/SLE.0b013e3182008efb. [DOI] [PubMed] [Google Scholar]
- 58.Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, Kato S, Yasukawa D, Aisu Y, Sasaki M, et al. Protocol for laparoscopic cholecystectomy: Is it rocket science? World J Gastroenterol. 2016;22:10287–10303. doi: 10.3748/wjg.v22.i47.10287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009;13:498–503. doi: 10.1007/s11605-008-0748-8. [DOI] [PubMed] [Google Scholar]
- 60.Sanjay P, Fulke JL, Exon DJ. “Critical view of safety” as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg. 2010;14:1280–1284. doi: 10.1007/s11605-010-1251-6. [DOI] [PubMed] [Google Scholar]
- 61.Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010;211:132–138. doi: 10.1016/j.jamcollsurg.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 62.Yamashita Y, Kimura T, Matsumoto S. A safe laparoscopic cholecystectomy depends upon the establishment of a critical view of safety. Surg Today. 2010;40:507–513. doi: 10.1007/s00595-009-4218-z. [DOI] [PubMed] [Google Scholar]
- 63.de Reuver PR, Rauws EA, Bruno MJ, Lameris JS, Busch OR, van Gulik TM, Gouma DJ. Survival in bile duct injury patients after laparoscopic cholecystectomy: a multidisciplinary approach of gastroenterologists, radiologists, and surgeons. Surgery. 2007;142:1–9. doi: 10.1016/j.surg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 64.Sherman JL, Shi EW, Ranasinghe NE, Sivasankaran MT, Prigoff JG, Divino CM. Validation and improvement of a proposed scoring system to detect retained common bile duct stones in gallstone pancreatitis. Surgery. 2015;157:1073–1079. doi: 10.1016/j.surg.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 65.Yang MH, Chen TH, Wang SE, Tsai YF, Su CH, Wu CW, Lui WY, Shyr YM. Biochemical predictors for absence of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2008;22:1620–1624. doi: 10.1007/s00464-007-9665-2. [DOI] [PubMed] [Google Scholar]
- 66.Tranter SE, Thompson MH. A prospective single-blinded controlled study comparing laparoscopic ultrasound of the common bile duct with operative cholangiography. Surg Endosc. 2003;17:216–219. doi: 10.1007/s00464-002-8911-x. [DOI] [PubMed] [Google Scholar]
- 67.Shaaban H, Welch A, Rao S. Laparoscopic ultrasound for the diagnosis of choledocholithiasis: quick, safe, and effective. Surg Laparosc Endosc Percutan Tech. 2014;24:274–276. doi: 10.1097/SLE.0b013e31828fa907. [DOI] [PubMed] [Google Scholar]
- 68.Tranter SE, Thompson MH. Potential of laparoscopic ultrasonography as an alternative to operative cholangiography in the detection of bile duct stones. Br J Surg. 2001;88:65–69. doi: 10.1046/j.1365-2168.2001.01622.x. [DOI] [PubMed] [Google Scholar]
- 69.Lee SP, Nicholls JF, Park HZ. Biliary sludge as a cause of acute pancreatitis. N Engl J Med. 1992;326:589–593. doi: 10.1056/NEJM199202273260902. [DOI] [PubMed] [Google Scholar]
- 70.Santambrogio R, Bianchi P, Opocher E, Verga M, Montorsi M. Prevalence and laparoscopic ultrasound patterns of choledocholithiasis and biliary sludge during cholecystectomy. Surg Laparosc Endosc Percutan Tech. 1999;9:129–134. [PubMed] [Google Scholar]
- 71.Grier JF, Cohen SW, Grafton WD, Gholson CF. Acute suppurative cholangitis associated with choledochal sludge. Am J Gastroenterol. 1994;89:617–619. [PubMed] [Google Scholar]
- 72.Mirbagheri SA, Mohamadnejad M, Nasiri J, Vahid AA, Ghadimi R, Malekzadeh R. Prospective evaluation of endoscopic ultrasonography in the diagnosis of biliary microlithiasis in patients with normal transabdominal ultrasonography. J Gastrointest Surg. 2005;9:961–964. doi: 10.1016/j.gassur.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 73.Catheline JM, Turner R, Paries J. Laparoscopic ultrasonography is a complement to cholangiography for the detection of choledocholithiasis at laparoscopic cholecystectomy. Br J Surg. 2002;89:1235–1239. doi: 10.1046/j.1365-2168.2002.02198.x. [DOI] [PubMed] [Google Scholar]
- 74.Kothari SN, Obinwanne KM, Baker MT, Mathiason MA, Kallies KJ. A prospective, blinded comparison of laparoscopic ultrasound with transabdominal ultrasound for the detection of gallbladder pathology in morbidly obese patients. J Am Coll Surg. 2013;216:1057–1062. doi: 10.1016/j.jamcollsurg.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 75.Nasu M, Yoshimura S, Uomori T, Takehara K, Tanaka R, Miyano S, Machida M, Kitabatake T, Fujisawa M, Kojima K. The efficacy of intraoperative ultrasonography during laparoscopic cholecystectomy. Hepatogastroenterology. 2012;59:1003–1005. doi: 10.5754/hge10540. [DOI] [PubMed] [Google Scholar]
- 76.Sun SX, Kulaylat AN, Hollenbeak CS, Soybel DI. Cost-effective Decisions in Detecting Silent Common Bile Duct Gallstones During Laparoscopic Cholecystectomy. Ann Surg. 2016;263:1164–1172. doi: 10.1097/SLA.0000000000001348. [DOI] [PubMed] [Google Scholar]


