Abstract
Endobronchial valves (EBVs) are increasingly deployed in the management of severe emphysema. Initial studies focussed on volume reduction as the mechanism, with subsequent improvement in forced expiratory volume in 1 s (FEV1). More recent studies have emphasized importance of perfusion on predicting outcomes, though findings have been inconsistent. Gallium‐68 ventilation–perfusion (V/Q) photon emission tomography (PET)/computed tomography (CT) is a novel imaging modality with advantages in spatial resolution, quantitation, and speed over conventional V/Q scintigraphy. We report a pilot case in which V/Q‐PET/CT demonstrated discordant findings compared with quantitative CT analysis, and directed left lower lobe EBV placement. The patient experienced a significant improvement in 6‐min walk distance (6MWD) without change in spirometry. Post‐EBV V/Q‐PET/CT demonstrated a marked decrease in unmatched (detrimental) V/Q areas and improvement in overall V/Q matching on post‐EBV V/Q‐PET/CT. These preliminary novel findings suggest that EBVs improve V/Q matching and may explain the observed functional improvements.
Keywords: Bronchial valve implants, bronchoscopy, positron emission tomography, ventilation
Introduction
Endobronchial valves (EBVs) are one‐way valves implanted via bronchoscopy in patients with advanced emphysema. These allow air to leave but not to enter emphysematous portions of lung, with benefits including improved exercise tolerance, health status, and lung function. A recent meta‐analysis indicates that EBVs have superior efficacy and a good level of safety compared with standard medications 1.
The basis for these improvements is not known with great certainty. Published studies demonstrate that functional improvements are greater in patients in whom hyperinflation is relieved, though improvements in 6‐min walk distance (6MWD) and symptom scores correlate poorly with reductions in residual volume (RV) and improvements in forced expiratory ratio in 1 s (FEV1) 2. Recent studies indicate that changes in lung perfusion may be significant factors in predicting response to EBV 3, 4.
Ventilation–perfusion (V/Q) matching can be assessed non‐invasively by two‐dimensional (2D) planar V/Q scintigraphy or three‐dimensional (3D) single‐photon emission computed tomography (SPECT) which may be combined with CT (SPECT/CT). Our group has demonstrated the utility of V/Q photon emission tomography (PET)/computed tomography (CT) owing to improved spatial and temporal resolution compared with SPECT/CT 5.
Case Report
A 71‐year‐old man with severe hyperinflation (residual volume 187% predicted) and functional limitation (6MWD 160 m) presented for EBV implantation. At baseline, he had a modified medical research council (mMRC) score of 3, requiring a wheelchair for mobility outside the home. He had completed pulmonary rehabilitation and was adherent to optimal chronic obstructive pulmonary disease (COPD) pharmacotherapy.
Pre‐procedure assessment included quantitative CT analysis to examine fissure integrity and emphysematous severity/distribution, and Gallium‐68 (Ga‐68) V/Q‐PET/CT using a technique we have previously described 5. Briefly, ventilation images were acquired following inhalation of Galligas (Cyclomedia, Sydney, NSW, Australia), and perfusion following injection of Ga‐68 macroaggregated albumin. Quantitative assessment of V/Q matching was calculated by dividing the volume of normal V/Q, unmatched defects, and matched defects by the total lung volume 5.
qCT indicated the left upper lobe (LUL) to be the optimal target, with integrity of the left oblique fissure, volume expansion, and high destruction scores (43% <910 HU). However, V/Q‐PET/CT demonstrated good LUL function contributing to 41% of overall lung perfusion (Table 2). Significantly, the left lower lobe (LLL) contributed only 4% of perfusion and demonstrated a high proportion of unmatched V/Q (Table 2). We therefore targeted the LLL despite reduced volume and lower severity score (35% <910 HU).
Table 2.
Ventilation and perfusion relationships at baseline and post‐EBV.
| Left lung | Left lower lobe (target lobe) | Left upper lobe | Right lung | Right lower lobe | Right middle lobe | Right upper lobe | Whole lung | |
|---|---|---|---|---|---|---|---|---|
| V/Q‐PET/CT baseline | ||||||||
| Ventilation (%) | 46 | 7 | 38 | 54 | 7 | 6 | 41 | N/A |
| Perfusion (%) | 45 | 4 | 41 | 55 | 4 | 5 | 46 | N/A |
| CT volume (%) | 47 | 13 | 34 | 53 | 11 | 7 | 34 | N/A |
| Matched V/Q defects (%) | 13 | 30 | 6 | 10 | 21 | 20 | 5 | 12 |
| Unmatched V/ Q defects (%) | 37 | 67 | 26 | 34 | 76 | 44 | 18 | 35 |
| Normal V/Q (%) | 50 | 3 | 68 | 56 | 3 | 36 | 77 | 53 |
| V/Q‐PET/CT post‐EBV | ||||||||
| Ventilation (%) | 43 | 6 | 38 | 57 | 9 | 9 | 38 | N/A |
| Perfusion (%) | 45 | 5 | 40 | 55 | 7 | 8 | 41 | N/A |
| CT volume (%) | 46 | 14 | 32 | 54 | 15 | 9 | 29 | N/A |
| Matched V/Q defects (%) | 31 | 75 | 12 | 26 | 56 | 40 | 7 | 29 |
| Unmatched V/Q defects (%) | 13 | 16 | 11 | 14 | 25 | 15 | 7 | 13 |
| Normal V/Q | 56 | 9 | 76 | 60 | 19 | 46 | 86 | 58 |
CT, computed tomography; EBV, endobronchial valve; PET, photon emission tomography.
Ventilation, perfusion, and CT volume results are expressed as percentage of whole lung volume; matched, unmatched, and normal V/Q results are expressed as percentage of lobe volume.
At 4 weeks, there was significant clinical improvement with 6MWD improved to 240 m, 50% greater than baseline. mMRC improved to 2 at one month and he rejoined participation in community activities. Spirometry and plethysmographic changes were minimal (Table 1).
Table 1.
Pre‐ and post‐bronchodilator spirometry and body plethysmography.
| Parameter | Prior to endobronchial valve insertion | 4 weeks after endobronchial valve insertion |
|---|---|---|
| FEV1 | 0.7 L (26% predicted) | 0.7 L (25% predicted) |
| FVC | 2.4 L (63% predicted) | 2.3 L (62% predicted) |
| FEV1/FVC | 31% | 32% |
| DLCO (unadjusted for haemoglobin) | 16 mL/mmHg/min (64% predicted) | 11 mL/mmHg/min (44% predicted)* |
| KCO | 3.9 mL/mHg/min/L (103% predicted) | 3.1 mL/min/mHg/min (84% predicted) |
| VA | 4.2 L (62% predicted) | 3.5 L (52% predicted) |
| TLC | 7.8 L (116% predicted) | 7.4 L (110% predicted) |
| RV | 4.9 L (187% predicted) | 5.0 L (190% predicted) |
| RV/TLC | 62% predicted | 67% predicted |
| 6‐min walk distance | 160 m | 280 m |
| Resting spo2, spo2 nadir | 92%, 90% at 1 min | 94%, 91% at 4 min |
FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
DLCO likely underestimated as patient did not inhale to >85% FVC; at 5 months, repeat DLCO was 58% predicted.
V/Q‐PET/CT at 4 weeks demonstrated no significant change in LLL volume but major changes in V/Q matching (Table 2 and Fig. 1). Within the LLL, normal V/Q remained low (<10%) but unmatched V/Q decreased from 67 to 16%. There was also a substantial reduction in unmatched V/Q in non‐target lobes.
Figure 1.
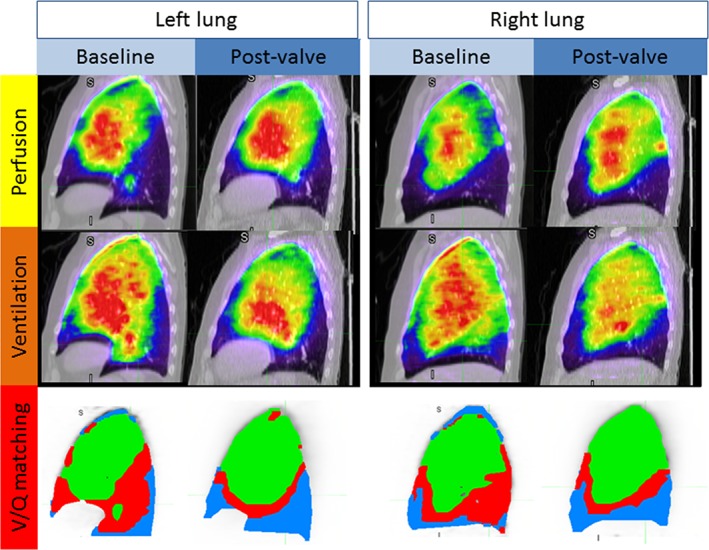
Ventilation–perfusion (V/Q) relationships at baseline and post‐endobronchial valve by Gallium‐68 (Ga‐68) V/Q photon emission tomography/computed tomography (PET/CT). Sagittal images of V/Q relationships at baseline and post‐left lower lobe endobronchial valve insertion. In the bottom third of the figure, areas of unmatched V/Q defects (red) are fewer post‐valve insertion. Areas of normal V/Q matching (green), and areas of matched V/Q defects (blue) are increased post‐valve insertion.
Discussion
We have used pre‐procedure V/Q‐PET/CT to direct EBV therapy in this patient and achieved an excellent functional improvement. This is despite minimal changes in lobar volumes. Symptomatic benefit has mostly been ascribed to relief from hyperinflation; however, more recent studies demonstrate that redistribution of pulmonary perfusion may also be significant. Our report advances understanding of the physiology underlying the symptomatic responses to EBV. V/Q‐PET/CT demonstrates marked improvement in V/Q matching, leading to reduction in physiologic dead space ventilation, which we believe is the mechanism for improvement in our patient.
The literature examining the effect of EBVs on V/Q so far has largely focused on perfusion, with lesser examination of the role of ventilation, and no examination of V/Q matching. Pizarro et al. 4 used planar V/Q and found increased contralateral perfusion, whereas Thomsen et al. 3 used SPECT/CT to identify no predictive value of target lobe perfusion, but instead that high ipsilateral non‐target lobe perfusion predicted 6MWD improvement. Our report provides a basis for these seemingly contradictory findings.
V/Q‐PET/CT has greater spatial and temporal resolution 5 compared with conventional scintigraphic techniques described previously 3, 4, enabling accurate quantification of sub‐lobar physiologic function. Neither group performed respiratory gating, and both analysed images in 2D, which is inherently limited by the superimposition of structures, compromising assessment of lobar anatomy thereby negating accurate quantitation.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Leong, P. , Le Roux, P.‐Y. , Callahan, J. , Siva, S. , Hofman, M.S. and Steinfort, D.P. (2017) Reduced ventilation–perfusion (V/Q) mismatch following endobronchial valve insertion demonstrated by Gallium‐68 V/Q photon emission tomography/computed tomography. Respirology Case Reports, 5 (5), e00253. doi: 10.1002/rcr2.253.
Associate Editor: Semra Bilaceroglu
References
- 1. Liu H, Xu M, Xie Y, et al. 2015. Efficacy and safety of endobronchial valves for advanced emphysema: a meta analysis. J. Thorac. Dis. 7:320–328. https://doi.org/10.3978/j.issn.2072‐1439.2014.11.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Klooster K, ten Hacken NHT, Hartman JE, et al. 2015. Endobronchial valves for emphysema without interlobar collateral ventilation. N. Engl. J. Med. 373:2325–2335. https://doi.org/10.1056/NEJMoa1507807. [DOI] [PubMed] [Google Scholar]
- 3. Thomsen C, Theilig D, Herzog D, et al. 2016. Lung perfusion and emphysema distribution affect the outcome of endobronchial valve therapy. Int. J. Chron. Obstruct. Pulmon. Dis. 11:1245–1259. https://doi.org/10.2147/COPD.S101003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pizarro C, Ahmadzadehfar H, Essler M, et al. 2015. Effect of endobronchial valve therapy on pulmonary perfusion and ventilation distribution. PLoS One 10:e0118976 https://doi.org/10.1371/journal.pone.0118976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Roux P‐YL, Siva S, Steinfort DP, et al. 2015. Correlation of 68Ga ventilation–perfusion PET/CT with pulmonary function test indices for assessing lung function. J. Nucl. Med. 56:1718–1723. https://doi.org/10.2967/jnumed.115.162586. [DOI] [PubMed] [Google Scholar]


