Abstract
This cross-sectional study examined the: (1) association between food store environment (FSE), fruit and vegetable (FV) availability and access, and prevalence of early childhood overweight/obesity (COWOB); and (2) influence of young child actual FV intake on the relationship between the FSE and early COWOB prevalence. Anthropometric and socio-demographic data of children (2 to 8 years; N=466) in baseline communities on Guam participating in the Children's Healthy Living (CHL) Program community trial were included. CDC year 2000 growth charts were used to calculate BMI z-scores and categories. FSE factors (fresh FV scores, store type) were assessed using the CX3 Food Availability and Marketing Survey amended for CHL. ArcGIS maps were constructed with geographic coordinates of participant residences and food stores to calculate food store scores within 1 mile of participant's residences. A sub-sample of participants (n = 355) had Food and Activity Log data to calculate FV and energy intakes. Bivariate correlations and logistic regression evaluated associations. Of 111 stores surveyed, 73% were small markets, 16% were convenience stores, and 11% were large grocery/supermarkets. Supermarkets/large grocery stores averaged the highest FV scores. Most participants did not meet FV intake recommendations while nearly half exceeded energy intake recommendations. Living near a small market was negatively correlated with BMI z-score (r = - 0.129, P < .05) while living near a convenience store was positively correlated with BMI z-score (r = 0.092, P < .05). Logistic regression analysis yielded non-significant associations. The high density of small markets may be an opportunity for FSE intervention but further investigation of Guam's FSE influence on health is needed.
Keywords: Guam, nutrition environment, dietary intake, childhood obesity, food store
Introduction
Childhood overweight/obesity (COWOB) is a growing global epidemic affecting many countries.1–3 COWOB prevalence in Guam among children ages 3 to 5 years (39%) exceeds4 the United States (US) national average (23%) for children aged 2 to 5 years.1 Researchers have described certain “built environments”—the neighborhoods, roads, buildings, food sources, and recreational facilities in which people live5—to be obesogenic.6–8 Previous studies examined the nutrition environment in Guam, looking at sodium in food stores and restaurants, fast food restaurants, and a community garden program.9–11 A study by Fialkowski, et al, found Guam's retail food environment to have the highest number of small markets but the lowest percentage of fresh fruit availability compared to other jurisdictions in the Pacific Region.12 Matanane, et al, found a significant negative correlation between children's BMI (ages 2 to 8 years; N=536) and community food environment readiness for change in 3 communities in Guam.13 Little is known about the food store environment (FSE) in relation to weight status of young children in Guam.
Fruits and vegetables (FV) are a priority area in the nutrition environment and are one of five categories of target foods whose low dietary intakes are most closely related to obesity and non-communicable diseases.14 Despite recommendations by the 2010 US Dietary Guidelines for Americans (DGA's) to eat more FV,15 a study examining the nutritional status of a representative sample of adolescents in Guam in 1999 found that 75.3% reported consuming FV less than once a day.16 Recent data in 2015 showed that 54% and 42% of adolescents reported consuming fruits and vegetables, respectively, less than once a day.17 More data are needed that are representative of the nutritional status of young children in Guam.
Studies examining the role that the nutrition environment, especially the FSE, has on children's weight status, in addition to diet and activity behaviors, have produced inconsistent results. A cross-sectional study of Canadian adolescent students found no association between food retailers surrounding schools and childhood overweight,18 while other studies found that the presence of convenience stores was positively associated with higher body mass index (BMI) in young children19 and adolescents.20 In the Pacific Region, the Healthy Foods Hawai‘i Intervention found that increased store stocking of nutritious foods, point-of-purchase promotions, and interactive cooking sessions increased children's Healthy Eating Index scores.21 A systematic review of the literature affirms the association of FV availability (eg, in food stores, schools, home) with increased consumption.22
This study was conceptualized according to the Children's Healthy Living Program (CHL) Framework for Community Engagement.23 This framework emphasizes examining the upstream determinants of obesity-related behaviors. The primary objective was to test whether availability and access to FV in food stores was associated with early COWOB (2 – 8 years; ≥85th BMI percentile) prevalence. Secondary objectives were to describe Guam's FSE and examine if actual FV intake of young children influenced the relationship between the FSE and early COWOB prevalence. The authors hypothesized that increased FV availability and access in food stores would be negatively associated with early COWOB in Guam and that FV intake would mediate this relationship.
Methods
Study Design
This is a cross-sectional study of the FSE and weight status of children in Guam, participating in the CHL Program. CHL conducted a community randomized trial to prevent COWOB in children ages 2 to 8 years in Alaska, American Samoa, the Commonwealth of the Northern Mariana Islands, Guam, and Hawai‘i.24
The current study focuses on the FSE in five communities that participated in the CHL Guam community randomized trial. Four of the communities were matched to form two matched pairs while the fifth community served as a temporal indicator of anthropometry status, as previously described in another publication,24 where it did not receive the intervention program. Community selection criteria and other details about the CHL community randomized intervention trial, including power analysis, are described elsewhere. 24 Baseline measurement data were used in this study.
Participants and Recruitment
Children ages 2 to 8 years were recruited from Head Start, Elementary Schools, and Community Centers in the five communities from October 2012 through September 2013 (n=466). Parents/caregivers of child participants provided informed consent, and child participants provided assent to be measured.24
Community food stores were identified by field observation using grid-mapped Google Earth (Mountain View, CA) images to guide community boundaries that were obtained from the Government of Guam Department of Land Management. A comprehensive sample of food stores (ie, supermarket, large grocery, small market, convenience) in the CHL communities was surveyed from October 2012 to February 2013 with the exception of specialty stores (eg, bakeries, liquor stores).
The University of Hawai‘i IRB and the University of Guam IRB approved all study protocols.
Instruments and Measures
Anthropometry.
Height and weight were measured by trained CHL staff based on standardized procedures, protocols25–27 and measurement tools (ie, stadiometer and scale). Further details regarding CHL rationale and design of measurement tools have been published elsewhere.24
Socio-demographic Information.
Data on socio-demographic information were obtained through forms completed by a parent/caregiver. These forms asked parents to provide information about their educational attainment and participation in federal food assistance programs, such as Supplemental Nutrition Assistance Program (SNAP) and/or Supplemental Assistance for Women Infants and Children (WIC), as well as the child's age, sex, race/ethnicity,24 and sleep duration.
Dietary Intake.
FV and energy intake of child participants were collected from a subsample (n=355) using a two-day Food and Activity Log (FAL), completed by the parent/caregiver. The subsample was selected from the four matched communities at baseline. Instructions and training of record keeping techniques were provided by field research staff with the use of food models, service ware, and utensils in order to record the following: time consumed, amount consumed, detailed description of the food, where the food was consumed and other activities performed while eating.24 Along with a tool kit of calibrated utensils (ie, measuring cups and spoons), parents were given the FAL and a Ziploc® (Racine, WI) bag in which to place food wrappers, labels, and packages.24 The FAL was reviewed by a CHL staff person with the parent/caregiver upon collection after one week. Data were entered into the Pacific Tracker 3 (PacTrac3) food composition database and web application.28 PacTrac3 originated from the MyPyramid Tracker developed by the US Department of Agriculture's Center for Nutrition Policy and Promotion, which was modified to include information on local foods of the Pacific Region.28,29 PacTrac3 generated total energy as calorie intake, cups of fruits, and cups of vegetables.
Food Store Environment (FSE).
Community food stores were surveyed by CHL staff using the Communities of Excellence in Nutrition, Physical Activity, and Obesity Prevention (CX3) Food Availability and Marketing Survey and Store Environment Walkability Survey that were previously validated for reliability as an indicator of the FSE.30 The survey tool defined store type based on the food items sold (canned/frozen foods, produce, bread, and snacks), number of employees and cash registers, number of stores, and chain/franchise business.30
Availability and access to FV variables were assessed using the CX3 validated scoring system. 30 Preliminary results showed that few of the food stores (10 out of 111 stores surveyed) met the published standard (score of 18) for fruit (n=10, 9%) and vegetables (n=28, 25%), or a combined FV availability score of 36 out of 40 total. Considering the dependence on imported foods in the Pacific Region;31 the standards for FV were adjusted to give credit to moderate variety and mixed quality for a score of 14 each for fresh FV based on the CX3 to explore the research questions.30
Procedures and Data Analysis
Analysis was limited to participants with complete data for anthropometry, socio-demographics, and with a verified residential address (N=466). BMI z-scores and percentiles were calculated using the 2000 CDC growth charts, which defined children ages 2 to 19 in the ≥85th to <95th BMI percentile as overweight and ≥95th BMI percentile as obese.32 BMI was analyzed by CDC growth reference data using SAS® 9.3 Statistical Software (SAS Institute, Cary, NC).33 All variables followed normal distributions, so no adjustments were needed. BMI was categorized into two categories: <85th percentile (healthy weight and underweight) and ≥85th percentile (overweight and obese), to create dichotomous variables. Consolidation of BMI categories allowed for more inclusive analysis since fewer participants were classified as underweight, overweight or obese.
FSE data were analyzed at both the community and participant levels.14 At the community level, food store data assessed the number, type, and location of food stores, in addition to the availability of fresh FV. Mean scores were analyzed by community, as well as by store type using one-way ANOVA tests in IBM® SPSS® Statistics version 22 (Armonk, NY).
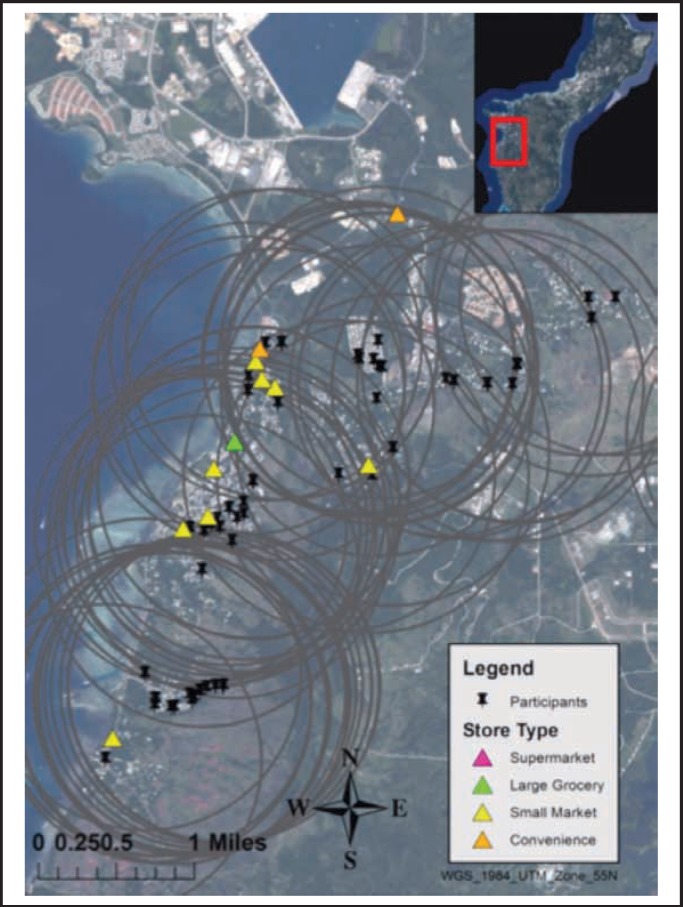
At the participant level, food store data were analyzed based on relative access from participants' residences. Residential addresses of participants and food stores were verified in-person using the Garmin Oregon® 600 GPS handheld unit. Waypoint geographic coordinates (ie, latitude, longitude) were recorded and uploaded to Garmin BaseCamp Version 4.3.5 (Olathe, KS). Figure 1 shows the mapping of coordinates in one community on Guam, which was done using ArcGIS Version 10.2 (ESRI; Redlands, CA). ArcGIS Buffer and Point Distance analysis toolkits identified stores within 1 mile of residential addresses. A previous study examining the FSE's influence on dietary fat intake in four counties in Southwest Georgia surveyed food stores less than 1 and within 1 to 5 miles of participants' homes.34 Given the geography of Guam (210 square mile area), the distance of 1 mile was used to evaluate direct access to food stores at the participant level. Food store scores were analyzed in two ways: (1) all scores averaged within a 1-mile radius of each participant's residence; (2) nearest store scores to each participant residence.
FV intake and total calorie intake were averaged between the two days. FV intake variables were coded as meeting appropriate age recommendations or not. 15 Likewise, energy was computed according to energy needs of children by age and sex, as above or below the cutoff for moderately active children in the 2010 DGA's as this is considered the middle range of physical activity for children.15
Bivariate correlation was used to test associations between FV availability scores (independent variable; mean and nearest scores), dietary intakes (mediator variable; cups of FV), and BMI (dependent variable; z-scores) of child participants. Logistic regression was then used to test associations between dichotomous variables for fresh FV availability scores (14 or above) and BMI (<85th percentile and ≥85th percentile), while controlling for socio-demographics, and to determine if FV intake mediates this relationship.35 All statistical tests were performed using IBM® SPSS® Statistics version 22 (Armonk, NY).
Results
Univariate Analyses
Characteristics of study participants (N=466) and their parent/caregiver are summarized in Table 1. The mean age of study participants was 5 years. The predominant race/ethnic group was Chamorro (56%). Prevalence of COWOB in this study was 29%. There were no significant differences in FV or energy intakes by sex. Fewer participants met vegetable intake recommendations (11%) in comparison to fruits (21%). More than half of participants (54%) exceeded estimated energy intake recommendations.
Table 1.
Characteristics of children ages 2 to 8 years who participated in baseline measurements for the Children's Healthy Living Program in 5 communities on Guam.
| Boys | Girls | All | |
| TOTASL SAMPLE | |||
| Sex [n (%)] | 238 (51%) | 228 (49%) | 466 (100%) |
| Age years (mean ± SD) | 5.5 ± 1.9 | 5.4 ± 1.8 | 5.4 ± 1.8 |
| Education of parent/caregiver [n (%)] | |||
| Less than high school graduate/GED | 76 (32%) | 73 (32%) | 149 (32%) |
| High school graduate/GED or more | 162 (68%) | 155 (68%) | 317 (68%) |
| Food Assistance [n (%)] | |||
| SNAP | 169 (71%) | 164 (72%) | 333 (71%) |
| WIC | 75 (32%) | 64 (28%) | 139 (30%) |
| Race/ethnicity [n (%)] | |||
| Native Hawaiian/Pacific Islander (NHPI) | 177 (74%) | 172 (75%) | 349 (75%) |
| Chamorro | 130 (55%) | 130 (57%) | 260 (56%) |
| Asian | 24 (10%) | 22 (10%) | 46 (10%) |
| White | 2 (1%) | 0 (0%) | 2 (0%) |
| More than one race | 35 (15%) | 34 (15%) | 69 (15%) |
| Sleep categories [n (%)] | |||
| Less than 8 hours | 44 (18%) | 36 (16%) | 80 (17%) |
| 8 hours or more | 194 (82%) | 192 (85%) | 386 (83%) |
| Weight Status (mean ± SD) | |||
| Body mass index (BMI) z-score | 0.4 ± 1.2 | 0.4 ± 1.1 | 0.4 ± 1.2 |
| BMI percentile | 59.7 ± 29.5 | 61.5 ± 29.9 | 60.6 ± 29.7 |
| Weight categories [n (%)] | |||
| Underweight | 10 (4%) | 7 (3%) | 17 (4%) |
| Healthy weight | 164 (69%) | 151 (66%) | 315 (68%) |
| Overweight | 30 (13%) | 42 (18%) | 72 (16%) |
| Obese | 34 (14%) | 28 (12%) | 62 (13%) |
| FOOD AND ACTIVITY LOG (FAL) SAMPLE | |||
| Sex [n (%)] | 177 (50%) | 178 (50%) | 355 (100%) |
| Dietary Intake (mean ± SD) | |||
| Fruit, cups | 0.82 ± 0.8 | 0.87 ± 0.9 | 0.84 ± 0.8 |
| Vegetable, cups | 0.61 ± 0.5 | 0.57 ± 0.6 | 0.59 ± 0.5 |
| Calories/day | 1675 ± 513 | 1608 ± 593 | 1641 ± 555 |
| Meets Recommendations [n (%)] | |||
| Fruits/day | 37 (21%) | 38 (21%) | 75 (21%) |
| Vegetables/day | 20 (11%) | 19 (11%) | 39 (11%) |
| Calories/day | 70 (40%) | 94 (53%) | 164 (46%) |
GED = General Education Development; SNAP = Supplemental Nutrition Assistance Program; WIC = Supplemental Program for Women, Infants, and Children. Percentages may not add up to 100% due to rounding; numbers rounded to the nearest tenth of a decimal.
Descriptive food store analyses.
A total of 111 food stores were surveyed, with the majority being small markets, and more stores were located in Community E in comparison to the other communities (Table 2). Supermarkets and large grocery stores were most similar in all scores, although supermarkets had the highest total store scores, while convenience stores scored lowest (Table 3). Of all stores surveyed, 85 (77%) had fresh FV for sale, but in regard to variety and good quality, only 23 (21%) and 41 (37%) met the modified cutoff score for FV, respectively (Table 3).
Table 2.
Type and characteristics of food stores by community using the CX3 Food Marketing and Availability Survey in 5 communities (A–E) participating in the Children's Healthy Living Program in Guam.
| Max Store |
A n=10 |
B n=10 |
C n = 22 |
D n = 13 |
E n = 56 |
All n = 111 |
|
| Store Type [n(%)] | |||||||
| Supermarket | 0 (0) | 1 (10) | 1 (5) | 0 (0) | 5 (9) | 7 (6) | |
| Large Grocery | 1 (10) | 0 (0) | 1 (5) | 1 (8) | 2 (4) | 5 (5) | |
| Small Market | 7 (70) | 7 (70) | 17 (77) | 10 (77) | 40 (71) | 81 (73) | |
| Convenience | 2 (20) | 2 (20) | 3 (14) | 2 (15) | 9 (16) | 18 (16) | |
| Store Scores [mean ± stand deviation (Minimum / Maximum)] | |||||||
| WIC/SNAP | 10 | 4.6 ± 3.4w (0/10) | 4.9 ± 3.3w (0/10) | 2.9 ± 2.7wx (0/9) | 5.7 ± 2.3wy (4/10) | 3.5 ± 2.2wxz (0/8) | 3.9 ± 2.6 (0/10) |
| Fresh Fruit (F) | 20 | 3.6 ± 6.7 (0/18) | 5.4 ± 7.5 (0/20) | 7.5 ± 6.4 (0/18) | 9.1 ± 5.6 (0/16) | 8.9 ± 7.0 (0/20) | 7.9 ± 6.9 (0/20) |
| Fresh Vegetable (V) | 20 | 8.0 ± 7.5 (0/18) | 8.8 ± 6.8 (0/20) | 11.0 ± 7.0 (0/18) | 12.9 ± 5.5 (0/20) | 11.6 ± 7.3 (0/20) | 11.0 ± 7.1 (0/20) |
| Fresh FV | 40 | 11.6 ± 13.3 (0/36) | 14.2 ± 13.5 (0/40) | 18.5 ± 12.7 (0/36) | 22.0 ± 9.7 (0/36) | 20.5 ± 13.8 (0/40) | 18.9 ± 13.2 (0/40) |
CX3= Communities of Excellence in Nutrition, Physical Activity, and Obesity Prevention; WIC= Supplemental Program for Women, Infants, and Children; SNAP= Supplemental Nutrition Assistance Program.
Mean values within a row with unlike superscript letters were significantly different (P<.05). Percentages may not add up to 100% due to rounding; numbers rounded to the nearest tenth of a decimal.
Table 3.
Characteristics of stores by store type using the CX3 Food Marketing and Availability Survey in 5 communities participating in the Children's Healthy Living Program on Guam.
| Max Score |
Supermarket n = 7 |
Large Grocery n = 5 |
Small Market n = 81 |
Convenience n = 18 |
Total n = 111 |
|
| Store Scores [mean ± stand deviation (Minimum / Maximum)] | ||||||
| WIC/SNAP | 10 | 7.3 ± 2.4w (4/10) | 4.6 ± 3.6wx (0/10) | 4.2 ± 2.1xy (0/10) | 0.7 ± 1.7z (0/5) | 3.9 ± 2.6 (0/10) |
| Fresh Fruit (F) | 20 | 18.3 ± 2.1w (14/20) | 17.6 ± 0.9wx (16/18) | 8.0 ± 6.0y (0/20) | 0.6 ± 2.4z (0/10) | 7.9 ± 6.9 (0/20) |
| Fresh Vegetable (V) | 20 | 18.9 ± 1.1w (18/20) | 18.4 ± 0.9wx (18/20) | 12.1 ± 5.8xy (0/20) | 1.1 ± 3.2z (0/10) | 11.0 ± 7.6 (0/20) |
| Fresh FV | 40 | 37.1 ± 3.0w (32/40) | 36.0 ± 0.0wx (36/36) | 20.1 ± 10.9y (0/40) | 1.7 ± 5.1z (0/20) | 18.9 ± 13.2 (0/40) |
| Store Type [n(%)] | ||||||
| FV Available | 7 (100) | 5 (100) | 71 (88) | 2 (1) | 85 (77) | |
| Meets F Score (18)a | 5 (71) | 3 (60) | 2 (2) | 0 (0) | 10 (9) | |
| Meets F Score (14)b | 6 (86) | 3 (60) | 14 (17) | 0 (0) | 23 (21) | |
| Meets V Score (18)a | 7 (100) | 4 (80) | 17 (21) | 0 (0) | 28 (25) | |
| Meets V Score (14)b | 7 (100) | 4 (80) | 30 (37) | 0 (0) | 41 (37) | |
CX3= Communities of Excellence in Nutrition, Physical Activity, and Obesity Prevention; WIC= Supplemental Program for Women, Infants, and Children; SNAP= Supplemental Nutrition Assistance Program.
Mean values within a row with unlike superscript letters were significantly different (P<.05).
FV score of 18 is the published standard for adequate availability.
FV score of 14 is the modified cutoff for adequate availability.
Bivariate Analyses
The mean number of food stores within 1 mile of a participant's residence was 6, while the mean FV availability scores were 7.9 and 11, respectively, out of 20 possible points (Table 2). Few stores (n=6; 5%) fell outside of participant buffer of 1 mile. Several participants (n=32, 7%) had no stores within 1 mile (data not shown). The mean distance to any store within 1 mile of a participant's residence was 0.07 miles (about 374 feet) and 0.09 miles (about 472 feet) for children categorized <85th BMI percentile and ≥85th BMI percentile, respectively, although not significantly different (data not shown). An inverse correlation was found between having a small market closest to participant residence and BMI z-score (R = −0.129, P <.05), while a positive correlation was found between having a convenience store closest to participant residence and BMI z-score (R = 0.092, P <.05) (Table 4).
Table 4.
Bivariate analysis examining the associations between access to food stores, availability of fruits and vegetables and childhood overweight/obesity (COWOB) in the total sample (N=466) in addition to the association between fruit and vegetable intake and COWOB in a subsample (n=355) of participants in the Children's Healthy Living Program in Guam.
| BMI Z-Score | COWOB | |||
| Correlation | P-value | Correlation | P-value | |
| Within 1 Mile Distance (n=466) | ||||
| Presence of Supermarket | 0.039 | .403 | 0.033 | .475 |
| Presence of Large Grocery | −0.049 | .291 | −0.054 | .245 |
| Presence of Small Market | −0.043 | .359 | −0.034 | .468 |
| Presence of Convenience | 0.041 | .378 | 0.019 | .690 |
| Mean Distance to Store | 0.029 | .526 | 0.013 | .781 |
| Number of Stores | 0.028 | .550 | 0.027 | .566 |
| Fruit Scores | −0.008 | .868 | −0.009 | .839 |
| Vegetable Scores | −0.023 | .613 | −0.039 | .407 |
| Nearest Store (n=466) | ||||
| Presence of Supermarket | 0.065 | .162 | 0.029 | .529 |
| Presence of Large Grocery | −0.012 | .802 | 0.008 | .861 |
| Presence of Small Market | −0.129 | .005 | −0.063 | .177 |
| Presence of Convenience | 0.092 | .047 | 0.033 | .473 |
| Distance to Store | 0.013 | .783 | 0.014 | .758 |
| Fruit Score | 0.015 | .740 | 0.035 | .445 |
| Vegetable Score | −0.047 | .307 | −0.006 | .900 |
| Fruit/Vegetable Intake (n=355) | ||||
| Fruit cups per day | −0.034 | .527 | −0.007 | .898 |
| Vegetable cups per day | −0.030 | .577 | 0.015 | .781 |
Correlation generated using Spearman's rho 2-tailed test.
Multivariate Analyses
The multivariate logistic regression model testing the relationship between FSE meeting FV standards and a child being ≥85th percentile adjusted for presence of supermarket/large grocery/small market/convenience store, parent/caregiver education, SNAP and WIC assistance, race/ethnicity, and sleep did not show significant association (Table 5). No significant interactions were found during the model-fitting.
Table 5.
Multivariate logistic regression examining the associations between access to food stores, availability of fruits and vegetables and childhood overweight/obesity in 5 communities participating in the Children's Healthy Living Program in Guam (N=466).
| Model 1a | Model 2b | |||||
| P-value | OR | 95% CI | P-value | OR | 95% CI | |
| Mean Scores within 1 Mile | ||||||
| High school/GED or higher | .231 | 1.32 | .84–2.1 | .252 | 1.31 | .82–2.1 |
| SNAP | .803 | 0.94 | .59–1.5 | .780 | 0.94 | .58–1.5 |
| WIC | .228 | 0.75 | .47–1.2 | .384 | 0.81 | .50–1.3 |
| Race/ethnicity is NHPI | .809 | 1.06 | .66–1.7 | .637 | 1.12 | .69–1.8 |
| ≥ 8 hours sleep/day | .728 | 1.10 | .64–1.9 | .725 | 1.11 | .63–1.9 |
| Above mean number of storesc | .304 | 1.38 | .75–2.5 | |||
| Presence of Supermarket | .483 | 0.81 | .46–1.5 | |||
| Presence of Large Grocery | .525 | 0.75 | .31–1.8 | |||
| Presence of Small Market | .365 | 1.38 | .69–2.8 | |||
| Presence of Convenience | .197 | 0.61 | .29–1.3 | |||
| Meets Fruit Score | .617 | 0.78 | .29–2.1 | |||
| Meets Vegetable Score | .723 | 1.14 | .54–2.4 | |||
| P-value | .571 | .797 | ||||
| Nearest Store Scores | ||||||
| High school/GED or higher | .231 | 1.32 | .84–2.1 | .216 | 1.34 | .84–2.1 |
| SNAP | .803 | 0.94 | .59–1.5 | .729 | 0.92 | .57–1.5 |
| WIC | .228 | 0.75 | .47–1.2 | .301 | 0.78 | .48–1.3 |
| Race/ethnicity is NHPI | .809 | 1.06 | .66–1.7 | .669 | 1.10 | .69–1.8 |
| ≥ 8 hours sleep | .728 | 1.10 | .64–1.9 | .773 | 1.08 | .62–1.9 |
| Presence of Supermarket | .586 | 0.72 | .22–2.4 | |||
| Presence of Large Grocery | .833 | 0.76 | .06–10.3 | |||
| Presence of Small Market | .303 | 0.65 | .28–1.5 | |||
| Presence of Convenience | .996 | 1.00 | .39–2.6 | |||
| Meets Fruit Score | .743 | 1.11 | .60–2.1 | |||
| Meets Vegetable Score | .546 | 1.18 | .69–2.0 | |||
| P-value | .571 | .848 | ||||
GED = General Education Development; SNAP = Supplemental Nutrition Assistance Program; WIC = Supplemental Program for Women, Infants, and Children; NHPI = Native Hawaiian / Pacific Islander; OR=odds ratio; CI=confidence interval.
Model 1 evaluated participant characteristics (education, SNAP, WIC, race/ethnicity, sleep) with childhood overweight/obesity in the regression model. The groups: ‘less than high school graduate/GED’, ‘no’ SNAP or WIC benefits, non-NHPI race/ethnicity, and ‘less than 8 hours sleep’ served as the reference categories.
Model 2 included access to food stores by store type and availability of fruits and vegetables in the regression model. For each food store type, the ‘no’ exposure group served as the reference category, while for availability of fruits and vegetables, the group not meeting the score cutoff served as the reference category.
The variable included to indicate high access to food stores within 1 mile of participant residence. The group falling below the mean served as the reference category.
Mean Scores within 1 mile Distance.
Neither the availability of FV nor the presence of individual store types within participant buffers were associated with an increased likelihood of being ≥85th BMI percentile (Table 5).
Nearest Store Scores.
Despite the correlations between the presence of small market or convenience stores nearest to participant residence and BMI z-scores, no significant association was evident in the logistic regression analysis (Table 5).
Dietary Fruit and Vegetable Intake.
The current FV intake analysis is based on participants (n=355) with valid FAL data. Given that no association was found between the FSE and BMI, further mediation analysis with dietary FV intake was not warranted.
Discussion
This study examined the relationship between the FSE and a child's likelihood for being ≥85th BMI percentile. This is a novel study in that it examines multiple influences on child weight status, including the nutrition community environment (eg, access to food stores nearby a residence), consumer environment (eg, availability of fresh FV within nearby food stores), and dietary intake. COWOB prevalence (29%) in this study was lower than previous estimates for Guam children ages 3 to 5 years from WIC and Head Start (39%),4 but higher than the US national average (23%) for ages 2 to 5 years.1
Significant correlations were found in the bivariate analysis, which showed lower BMI z-scores in participants having a small market closest to their residences. This may be an area of interest for future studies considering the popularity of small markets in all communities. Resources have been allocated to the improvement of small markets in other Pacific jurisdictions,21 but causation cannot be inferred at this time.
Additionally, participants having a convenience store closest to their residences were found to have higher BMI z-scores. These findings corroborate other studies such as Galvez, et al,19 which found an increased risk for obesity in children ages 6 – 8 years who lived near convenience stores and fast-food restaurants in East Harlem, New York. Similarly, the availability of convenience stores in school zip codes has been associated with higher BMI in adolescents.36
However, the multivariate correlations were not found to be significant between the FSE and increased risk for being ≥85th BMI percentile. These findings are supported by Seliske, et al, who found no association between food retailers surrounding schools within a 1 km and 5 km radius and overweight among adolescent students in Canada.18
For FV intake, most study participants did not meet FV or energy DGA recommendations, which is in alignment with the high prevalence of COWOB. Michimi and Wimberly found that as distance to supermarket increased the odds of adult obesity increased, and also that consuming ≥5 FV decreased the odds of adult obesity in contiguous US metropolitan areas. 37 Likewise, other studies found that FV availability in food stores and in the home were associated with increased consumption among children and adolescents.38,39 In Hawai‘i, a positive association was found between adults with a greater density of total or healthy food outlets and mean intakes of FV at 0.5 km.40
There are limitations to this study. This study did not examine all food stores on Guam but rather only those within the communities participating in CHL. Participants may have had food stores in adjacent communities that were within their 1 mile buffer that were not included in this analysis. Data were also not collected from participants to determine where they shop for groceries, so it cannot be assumed that participant families buy food within 1 mile of their homes. Data was also not collected from community farmer's markets as they were not operating during the survey collection period. In addition, other food outlets (eg, fast-food) were not surveyed and other consumer nutrition variables (eg, product placement, price comparison) were not evaluated. This could be a potential area to explore in the future as Rose, et al, 41 found that FV shelf-space was not significantly associated with BMI, but that cumulative shelf-space of energy-dense snack foods was positively associated with BMI. A study by Snowdon, et al, found approximately 67% of Guam's food supply is imported from the US, Philippines, and Japan. 31 Further, food stores alone in island communities may not adequately represent access and availability to FV because it does not account for produce grown locally (eg, family farm). With Guam's agricultural movement currently growing, this is an opportunity to compare changes in subsistence farming, community markets and their effects on FV intake.
This study did not reveal any association of the FSE on COWOB prevalence. Still, it is the first of its kind to evaluate the FSE using ArcGIS mapping on Guam. This is also the first study to evaluate dietary intake of young children ages 2 – 8 years on Guam. To date, there is no surveillance system in place to monitor health behaviors of Guam's young children. 42 In addition, this relationship may need to be examined in other islands, which may be as geographically isolated and remote as Guam, and may have even greater difficulties with access to FV in food stores.
Conclusions and Implications
There is still much to be learned about the FSE on Guam, and its influence on dietary behaviors and weight status, before policies and interventions targeting this domain can be effective in promoting and maintaining child health. This study found lower BMI z-scores in participants having a small market closest to their residences in bivariate analysis, but future research is needed to explore other aspects of the FSE, such as the consumer environment, the growing popularity of farmer's markets, community gardens, and subsistence farming. Comprehensive studies of all communities using ArcGIS mapping will provide a clearer picture of Guam's FSE. Further studies should establish temporality of relationships between the FSE, dietary intakes, and weight status of children. The physical activity environment should also be explored to examine its impacts on the lifestyles and weight outcomes of children on Guam.
Figure 1.
Map of food stores in relation to participants within a 1 mile buffer (indicated by gray circle) in 1 community participating in the Children's Healthy Living (CHL) Program on Guam.
Acknowledgements
The authors gratefully acknowledge the CHL Program team in Guam who conducted data collection and data entry, as well as the student assistant, Rosae Calvo, and Guam study participants. The CHL Training Program is acknowledged for master's thesis support, guidance, and contributions. The support of the Agriculture and Food Research Initiative Grant no. 2011-68001-30335 from the USDA National Institute of Food and Agricultural Science Enhancement Coordinated Agricultural Program is also acknowledged.
Abbreviations
- BMI
Body Mass Index
- CHL
Children's Healthy Living Program
- COWOB
childhood overweight and obesity
- CX3
Communities of Excellence in Nutrition, Physical Activity, and Obesity Prevention Food Availability and Marketing Survey and Store Environment Walkability Survey
- DGA
Dietary Guidelines for Americans
- FAL
Food and Activity Log
- FSE
Food store environment
- FV
Fruit and Vegetable
- SNAP
Supplemental Nutrition Assistance Program
- WIC
Supplemental Assistance for Women Infants and Children
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO, author. Global strategy on diet, physical activity and health: childhood overweight and obesity. 2014
- 3.Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutrition. 2010;92(5):1257–1264. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 4.Novotny R, Fialkowski M, Li F, et al. Systematic Review of Prevalence of Young Child Overweight and Obesity in the United States-Affiliated Pacific Region Compared With the 48 Contiguous States: The Children's Healthy Living Program. Am J Public Health. 2015;105(1):e22–e35. doi: 10.2105/AJPH.2014.302283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. The future of children. 2006. Available at: http://muse.jhu.edu/journals/foc/summary/v016/16.1sallis.html. [DOI] [PubMed]
- 6.Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol Behav. 2005;86(5):603–613. doi: 10.1016/j.physbeh.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 7.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 8.Swinburn B, Egger G, Raza F. Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity. Preventive Medicine. 1999;29(6):563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 9.Jackson S, VanFrank B, Lundeen E, et al. Sodium in Store and Restaurant Food Environments — Guam, 2015. Mmwr Morbidity Mortal Wkly Rep. 2016;65(20):510–513. doi: 10.15585/mmwr.mm6520a2. [DOI] [PubMed] [Google Scholar]
- 10.Nitta M, Tanner C, Narvarte K, et al. Policy, System, and Environment Strategies to Promote Physical Activity and Healthy Food Sources to Address Guam's Disparate Non-Communicable Disease Burden. J Health Care Poor U. 2015;26(2):96–103. doi: 10.1353/hpu.2015.0057. [DOI] [PubMed] [Google Scholar]
- 11.Dela Cruz-Talbert E, Li F, Fialkowski M. Fast food environment among low-income communities in the Pacific Region: findings from the Children's Healthy Living Program. The FASEB Journal. 2015;29(1 Supplement):903–915. [Google Scholar]
- 12.Fialkowski M, Li F, Bersamin A, Leon Guerrero R, Kim J, Novotny R. The Pacific retail food store environment: findings from the Children's Healthy Living Program. The FASEB Journal. 2015;29(1 Supplement):382–387. [Google Scholar]
- 13.Matanane L, Li F, Leon Guerrero R, Acosta M, Barber R, Fialkowski M. The influence of community food environment on weight status of young children participating in the Children's Healthy Living Program in Guam (1019.1) The FASEB Journal. 2014;28(1 Supplement):1019–1021. [Google Scholar]
- 14.Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am J Health Promot. 2005;19(5):330–333. ii. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- 15.USDA, USDHHS, author. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 16.LeonGuerrero RT, Workman RL. Physical activity and nutritional status of adolescents on Guam. Pacific health dialog. 2002. Available at: http://www.researchgate.net/publication/8909282_Physical_activity_and_nutritional_status_of_adolescents_on_Guam/file/504635232a5a7a9571.pdf. [PubMed]
- 17.CDC, author. High School YRBS: Guam 2015 Results. 2016
- 18.Seliske LM, Pickett W, Boyce WF, Janssen I. Association between the food retail environment surrounding schools and overweight in Canadian youth. Public health nutrition. 2009;12(09):1384–1391. doi: 10.1017/S1368980008004084. [DOI] [PubMed] [Google Scholar]
- 19.Galvez M, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food-store availability in an inner-city community. Academic pediatrics. 2009;9(5):339–343. doi: 10.1016/j.acap.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laska M, Hearst M, Forsyth A, Pasch K, Lytle L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? 2010 doi: 10.1017/S1368980010001564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gittelsohn J, Vijayadeva V, Davison N, et al. A Food Store Intervention Trial Improves Caregiver Psychosocial Factors and Children's Dietary Intake in Hawaii. Obesity. 2010;18(S1):S84–S90. doi: 10.1038/oby.2009.436. [DOI] [PubMed] [Google Scholar]
- 22.Jago R, Baranowski T, Baranowski J. Fruit and vegetable availability: a micro environmental mediating variable? PHN. 2007 doi: 10.1017/S1368980007441441. [DOI] [PubMed] [Google Scholar]
- 23.Fialkowski M, DeBaryshe B, Bersamin A, et al. A Community Engagement Process Identifies Environmental Priorities to Prevent Early Childhood Obesity: The Children's Healthy Living (CHL) Program for Remote Underserved Populations in the US Affiliated Pacific Islands, Hawaii and Alaska. Maternal and Child Health Journal. 2013 doi: 10.1007/s10995-013-1353-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilken L, Novotny R, Fialkowski M, et al. Children's Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health. 2013;13(1):944. doi: 10.1186/1471-2458-13-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC, National Center for Health Statistics, author. Anthropometric procedures. Hyattsville, MD: 2006. [Google Scholar]
- 26.Li F, Wilkens L, Novotny R, Fialkowski M, Paulino Y. Anthropometric standardization in the US Affiliated Pacific: The Children'S Healthy Living Program (1024.6) The FASEB Journal. 2014. Available at: http://www.fasebj.org/content/28/1_Supplement/1024.6.short. [DOI] [PMC free article] [PubMed]
- 27.Roche AF, Martorell R. In: Anthropometric Standardization Reference Manual. Lohman TG, editor. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 28.Novotny R, Nigg C, McGlone K, et al. Pacific Tracker 2 - expert system (PacTrac2-ES) behavioural assessment and intervention tool for the Pacific Kids DASH for Health (PacDASH) study. Food Chem. 2013;140(3):471–477. doi: 10.1016/j.foodchem.2012.11.047. [DOI] [PubMed] [Google Scholar]
- 29.Murphy S, Blitz C, Novotny R. Pacific Tracker (Pac Trac): an interactive dietary assessment program at the CRCH website. Hawaii Medical Journal. 2006;65(6):175–178. [PubMed] [Google Scholar]
- 30.Ghirardelli A, Quinn V, Sugerman S. Reliability of a retail food store survey and development of an accompanying retail scoring system to communicate survey findings and identify vendors for healthful food and marketing initiatives. Journal of Nutrition Education and Behavior. 2011;43(4 Suppl 2):S104–S112. doi: 10.1016/j.jneb.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Snowdon W, Raj A, Reeve E, et al. Processed foods available in the Pacific Islands. Globalization and Health. 2013;9(1):53. doi: 10.1186/1744-8603-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.CDC, author. Use and interpretation of the WHO and the CDC Growth Charts for children from birth to 20 years in the United States. 2013
- 33.CDC, author. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years) 2014
- 34.Hermstad A, Swan D, Kegler M, Barnette J, Glanz K. Individual and environmental correlates of dietary fat intake in rural communities: a structural equation model analysis. Soc Sci Med. 2010;71(1):93–101. doi: 10.1016/j.socscimed.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 35.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 36.Powell LM, Auld MC, Chaloupka FJ, O'Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine. 2007;33(4 Suppl):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Michimi A, Wimberly MC. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health …. 2010 doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bere E, Klepp K-I. Changes in accessibility and preferences predict children's future fruit and vegetable intake. Int J Behav Nutr Phys Act. 2005;2(1):15. doi: 10.1186/1479-5868-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cullen KW, Baranowski T, Owens E. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children's dietary behavior. Health Education & …. 2003 doi: 10.1177/1090198103257254. [DOI] [PubMed] [Google Scholar]
- 40.Ollberding NJ, Nigg CR, Geller KS, Horwath CC, Motl RW, Dishman RK. Food outlet accessibility and fruit and vegetable consumption. Am J Health Promot. 2012;26(6):366–370. doi: 10.4278/ajhp.101215-ARB-401. [DOI] [PubMed] [Google Scholar]
- 41.Rose D, Hutchinson P, Bodor J, et al. Neighborhood food environments and Body Mass Index: the importance of in-store contents. American Journal of Preventive Medicine. 2009;37(3):214–219. doi: 10.1016/j.amepre.2009.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Novotny R, Fialkowski MK, Areta AAR, et al. University of Hawai'i Cancer Center Connection: the Pacific way to child wellness: the Children's Healthy Living Program for Remote Underserved Minority Populations of the Pacific Region (CHL) Hawai'i Journal of Medicine & Public Health. 2013;72(11):406–408. [PMC free article] [PubMed] [Google Scholar]