Abstract
Hair casts (HCs) are thin, elongated, firm, whitish cylindrical concretions which ensheath the hair shaft and can be easily dislodge. They are of two different types: peripilar and parakeratotic keratin cast. Due to its clinical resemblance to pediculosis capitis, the entity is also known as pseudonits. Al though not unusual, false diagnoses are common, and thus, it is very important to correctly differentiate it from other similar conditions. We report here a case of HC involving scalp as well as body hair in association with androgenetic alopecia in a 22-year-old male patient. The patient's sister was also affected with pseudonits.
Key words: Hair casts, Pseudonits, Peripilar cast
INTRODUCTION
Hair casts (HCs) or pseudonits are 2–8 mm long, slender, discrete, shiny, white to yellow, nonadherent, freely movable tube like concretions ensheathing the hair shafts.[1]
HCs are of two types – parakeratotic (“secondary”) or nonparakeratotic peripillar (“idiopathic”) casts. The secondary form is more common and often coexists with pathological conditions involving the scalp scaling such as in psoriasis, pityriasis amiantacea, seborrheic dermatitis or scalp infections or hair shaft defects.[2]
The idiopathic peripillar keratin cast is uncommon. It affects young children and females and not found in association with any disease or scalp condition.[3]
Even though the condition is not unusual, there is a scarcity of literature on it.
They are often underdiagnosed. The condition is often confused with pediculosis capitis which is more common symptomatic infection of the scalp.
CASE REPORT
A 22-year-old male born of nonconsanguineous marriage presented to outpatient dermatology department with the history of receding hairline and balding of anterior scalp for last 2 years. The patient had also noticed the development of small, thin whitish to gray structures surrounding hair shafts for last 3–4 years. Itching was conspicuously absent.
There was no history of hair spray, hair gel application, or traction to hair.
The patient did not report any other symptom because of this, and he noticed reduction in them after hair wash without complete disappearance.
These lesions first started on the scalp, they resembled nits in their appearance; on little effort, it was possible to slid them along the entire length of hair shaft.
His 24-year-old married sister was also suffering from similar disorder for last 1 year.
Family history of androgenetic alopecia was positive in father which started in the fourth decade.
The dermatological examination of scalp showed overall thinning of hair and grade IV androgenetic alopecia [Figure 1a].
Figure 1.
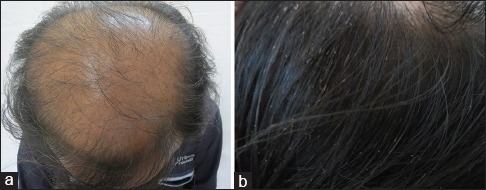
(a) Androgenetic alopecia. (b) Hair casts – whitish concretions along hair shaft
On closer view, hair shafts showed whitish, shiny, firm cylindrical concretions of 2–7 mm along its entire length, which were easily movable along the shaft and removable [Figure 1b].
They were present all over scalp, especially on the occipital and parietal regions, sparing 1–2 cm proximal hairs root area.
His beard, chest, axillary, and pubic hair were also affected [Figure 2a and b].
Figure 2.
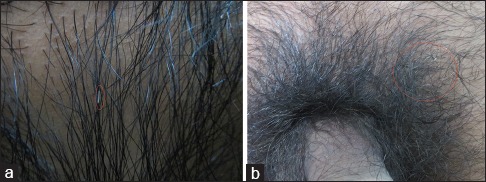
(a) Hair cast involving chest hair. (b) Hair cast involving pubic hair
To rule out mycological infection, culture and potassium hydroxide mount of hair were performed but it failed to show any fungal growth.
Dermatoscopy revealed a cylindrical, keratohyaline mass surrounding the hair shaft and absence of true nits [Figure 3a].
Figure 3.
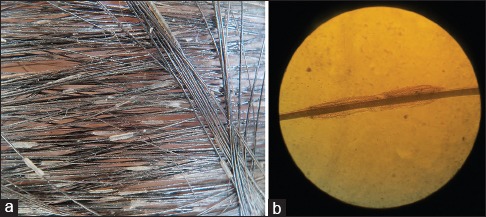
(a) Dermoscopy showing cylindrical, keratohyaline mass. (b) Light microscopy of affected hair
Light microscopic examination of the plucked hair showed the presence of a thin, tubular accretions around the hair shaft [Figure 3b].
Electron, polarized, or optical microscopy could not be performed due to unavailability.
The patient was prescribed salicylic acid containing shampoo which helped in temporary reduction of hair cast without complete disappearance.
CASE DISCUSSION
The term HC was coined by Kligman in 1957.[3]
HCs of both parakeratotic and peripilar keratin casts results due to the failure of disintegration of root sheath which gets pulled out of hair follicle and surrounds the shaft leading to its persistence during hair growth.[4]
Multiple etiological factors are implicated in their causation.
The parakeratotic HCs are also called secondary as they are associated with scaly scalp conditions[2] such as psoriasis, seborrheic dermatitis, pityriasis amiantacea, dandruff, or infective scalp conditions which include pediculosis capitis, trichorrhexis nodosa, white piedra, and trichomycosis. Sometimes, hair shaft structural abnormalities such as trichorrhexis nodosa and monilethrix may also cause HCs.
Apparently, the HCs are more frequently seen in females, who tightly plate their hair for prolong period. This excessive traction by causing local scalp ischemia and inflammation promotes the development of HC.[5]
HCs may occur as a result of regular use of hair sprays or deodorants as these may lead to concretions on these materials.[6]
In cases of pemphigus vulgaris of scalp, acantholysis occurring in the outer root sheath epithelium can lead to the formation of HC.[7]
Scanning electron microscopy, optical microscopy, electron dispersive X-ray analysis, and direct immunofluorescence can help in knowing the composition of the cast.[8]
Electron microscopy studies have revealed that both parakeratotic and peripillar cast are composed of external root sheath, but the latter peripillous HC in addition can be made up of internal as well as outer root sheaths.[6]
There are multiple case reports in the literature showing casual association of HC with lichen planopilaris, pseudopelade of Brocq,[9] following psychological trauma,[10] propionibacterium acne,[11] and familial preponderance.[12]
The most important characteristic of these casts is its easy sliding along the hair shaft, which helps in differentiating them from other similar conditions.
Most of the times, HCs are confused with true nits or pediculosis capitis[13] which are usually itchy, contagious, attached to hair shaft by an angle. Dermoscopy helps in definite differentiation, nits from relatively asymptomatic HC.
Accurate differentiation of HC from true nits can not only help in proper diagnosis and treatment of this benign condition but also avoid patient's apprehension.
The condition may respond to keratolytic or coal tar-containing shampoos.
A volume of 0.025% retinoic acid was used by Taïeb et al.[14] and was found to be effective.
Manual removal of cylinders with comb is often required.
Usually, the condition is benign but tends to recur after discontinuation of medication and can cause a lot of anxiety in patients as well as treating physicians.
CONCLUSION
HCs are benign and not associated with any morbidity, but little known about them leads to frequent diagnostic confusion, which may generate unnecessary costs and anxiety for both patients and physicians.
This case has been reported to delineate HC involving scalp as well as body hair in association with androgenetic alopecia in a 22-year-old male patient. Patient's sister was also affected with similar pseudonits.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank department of dermatology BJMC Ahmedabad Gujarat, specially Head of Department – Dr. Bela J Shah, Dr. Rima Joshi, Dr. Apeksha Solanki and our patients without whom it would have not been possible to complete this work.
REFERENCES
- 1.Thappa DM, Kumar V, Sharma RC, Lal S. Hair casts. Indian J Dermatol Venereol Leprol. 1993;59:201–2. [Google Scholar]
- 2.Dawber R, Van ND, Lorivaldo M, Airton SG, Nádia CM. Capillary cylinders: report of three cases and literature review. An. Bras. Dermatol. [Internet] 2006;81(2):159–62. [Google Scholar]
- 3.Klingman AM. Hair casts; parakeratotic comedones of the scalp. AMA Arch Derm. 1957;75:509–11. doi: 10.1001/archderm.1957.01550160035004. [DOI] [PubMed] [Google Scholar]
- 4.Scott MJ, Jr, Roenigk HH., Jr Hair casts classification, staining characteristics and differential diagnosis. J Am Acad Dermatol. 1983;8:27–32. doi: 10.1016/s0190-9622(83)70003-4. [DOI] [PubMed] [Google Scholar]
- 5.Tosti A, Miteva M, Torres F, Vincenzi C, Romanelli P. Hair casts are a dermoscopic clue for the diagnosis of traction alopecia. Br J Dermatol. 2010;163:1353–5. doi: 10.1111/j.1365-2133.2010.09979.x. [DOI] [PubMed] [Google Scholar]
- 6.Ena P, Mazzarello V, Chiarolini F. Hair casts due to a deodorant spray. Australas J Dermatol. 2005;46:274–7. doi: 10.1111/j.1440-0960.2005.00200.x. [DOI] [PubMed] [Google Scholar]
- 7.Pirmez R. Acantholytic hair casts: A dermoscopic sign of pemphigus vulgaris of the scalp. Int J Trichology. 2012;4:172–3. doi: 10.4103/0974-7753.100087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu WY, Xia MY, Wu JH, Do DA. Hair casts: A clinical and electron microscopic study. Pediatr Dermatol. 1990;7:270–4. doi: 10.1111/j.1525-1470.1990.tb01023.x. [DOI] [PubMed] [Google Scholar]
- 9.Bayerl C, Moll I. Hair casts in lichen ruber. Hautarzt. 1993;44:37–9. [PubMed] [Google Scholar]
- 10.Held JL, Bernstein RM. Hair casts or pseudonits acquired following psychological trauma. Cutis. 1989;43:380–1. [PubMed] [Google Scholar]
- 11.Wang E, Lee JS, Hee TH. Is Propionibacterium acnes associated with hair casts and alopecia? Int J Trichology. 2012;4:93–7. doi: 10.4103/0974-7753.96907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minelli L, Gon AS, Sales NC. Casts: Three cases report and literature review. An Bras Dermatol. 2006;81:159–62. [Google Scholar]
- 13.Zalaudek I, Argenziano G. Dermoscopy of nits and pseudonits. N Engl J Med. 2012;367:1741. doi: 10.1056/NEJMicm1103059. [DOI] [PubMed] [Google Scholar]
- 14.Taïeb A, Surlève-Bazeille JE, Maleville J. Hair casts. A clinical and morphologic study. Arch Dermatol. 1985;121:1009–13. [PubMed] [Google Scholar]


