Abstract
Context:
Dentinal hypersensitivity is a sharp pain occurring on exposure of the exposed dentin to various stimuli such as hot, cold, air, tactile, and chemical.
Aim:
This study aimed to compare the effectiveness of three desensitizing pastes in the treatment of dentinal hypersensitivity.
Materials and Methods:
A total of 45 individuals (with two teeth per patient) were considered for this study and randomly divided into three groups, Group 1: treated with 5% NovaMin-containing toothpaste, Group 2: treated with 8% arginine-containing toothpaste, and Group 3: herbal desensitizing toothpaste. Using tactile stimulus and air stimulus, the sensitivity scores were recorded on visual analog scale (VAS), immediately after paste application, then at 2 weeks, and then at the end of 4 weeks and compared.
Results:
There was a significant change in the VAS scores in Group 1 when compared to Group 2 and Group 3. Group 1 showed better reduction in the hypersensitivity in long term.
Statistical Analysis:
One-way ANOVA test, post hoc Tukey test, and post hoc Bonferroni test were used for statistical analysis.
Conclusion:
Desensitizing pastes can be an effective and economical option in the treatment of the dentinal hypersensitivity.
Keywords: Air stimulus, desensitization, Sharp pain, tactile stimulus
Introduction
Dentinal hypersensitivity is a sharp pain of short duration occurring on exposure to the stimuli which can be thermal, evaporative, tactile, osmotic, or chemical, and it cannot be ascribed as other dental pathology.[1]
Always a differential diagnosis should be made for dentinal hypersensitivity by the clinician to rule out other dental diseases which present themselves with similar symptoms;[1] for example, dental caries, cracked tooth, and periodontal disease. The correct diagnosis always plays an important role for treatment to be implemented correctly.
Periodontal disease leading to the gingival recession results in exposure of the dentinal tubules and causes hypersensitivity; once hypersensitivity occurs, it gets stimulated on exposure to any external stimulus and is uncomfortable for the patient.[1] The response of the patient is variable ranging from minor to severe discomfort.[2]
In patients with periodontal disease, oral hygiene maintenance is a problem leading to carious lesion formation and further periodontal destruction.[3]
Brannstrom's hydrodynamic theory is the most accepted one, which states that sensitivity is the cause of the activation of the mechanoreceptors in the nerve endings inside the tubules or in the pulp superficially, due to the changes in the fluid volume within tubules.[4]
Despite a huge amount of published data, the “gold standard” in the management of dentinal hypersensitivity still lacks.[5]
There is a lack of data which compares herbal desensitizing pastes with other commercially available desensitizing pastes, so the purpose of this study was to compare them.
Materials and Methods
The duration of this study was 4 weeks, the sensitivity scores were recorded at baseline, at 2 weeks, and at 4 weeks. A total of 45 individuals were selected from the outpatient section of the Department of Dentistry, Shri Mahant Indiresh Hospital, Dehradun.
Inclusion criteria
Patients in the age range of 20–50 years and otherwise healthy patients were included in the study with cervical abrasion and complaints of hypersensitivity [Figure 1].
Figure 1.

Preoperative picture showing cervical abrasion
Before starting the treatment, the teeth were isolated using rubber dam and the baseline sensitivity values were recorded using the tactile method and the air blast stimuli.
Exclusion criteria
Patients with gross underlying pathologies, patients with existing systemic medical condition, and pregnant and lactating females were excluded from the study.
Tactile sensitivity record
Tactile sensitivity was recorded under slight manual pressure using a blunt probe over the hypersensitive areas of the tooth.[6]
Air blast sensitivity record
Air blast sensitivity was recorded using the controlled air pressure from the standard dental airway syringe at 40–65 psi at room temperature, directed perpendicular to the hypersensitive area from a distance of around 3 mm, with adjacent teeth protected with the gloved fingers to prevent false results.[7]
The record of hypersensitivity was based on the visual analog scale (VAS), the scores were recorded on the 10 cm scale, with stipulated ratings ranging as from 0 to 1 with no pain, 2–3 with slight pain, from 4 to 6 with moderate pain, and from 7 to 10 with severe pain. Individuals who had baseline scores ≥4 were taken up for the study.[6]
The individuals who qualified the tactile as well as the air blast sensitivity assessment were selected and randomly assigned to the three study groups, 15 patients in each group with two teeth per patient to be considered in the study:
Group 1: Desensitizing paste with 5% NovaMin (n = 30 teeth) (Vantej Toothpaste, Dr. Reddy's Laboratories, Hyderabad, India)
Group 2: Desensitizing paste with 8% arginine (n = 30 teeth) (Colgate Sensitive Pro-Relief® Desensitizing Paste, Colgate-Palmolive)
Group 3: Desensitizing herbal tooth paste (n = 30 teeth) (HiOra-K, Himalaya Herbal Healthcare).
Using a disposable applicator tip, an assigned amount (pea sized) of tooth paste was applied over the isolated hypersensitive area of the tooth for 10 s [Figure 2] and a rotary polishing cup was used to polish the paste over this surface for 1 min. Patients were prescribed to use the respective toothpaste twice daily at home.
Figure 2.

Paste application using a disposable applicator tip
Scores immediately postapplication, after 2 weeks, and 4 weeks were recorded by the same examiner using the same methodology of tactile stimuli and evaporative stimuli.
Results
The mean VAS score at baseline was compared between Groups 1, 2, and 3 using the one-way ANOVA test. There was no significant difference in the mean VAS score at baseline between Groups 1, 2, and 3 [Table 1 and Graph 1].
Table 1.
Comparison of visual analog scale scores at baseline
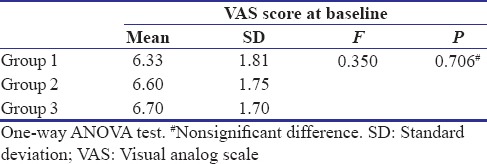
Graph 1.
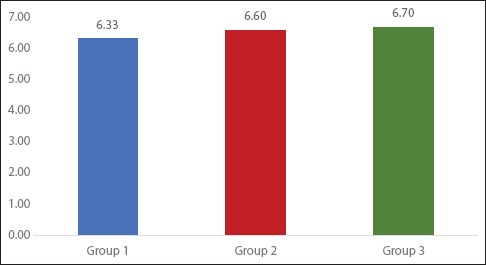
Mean visual analog scale scores at baseline
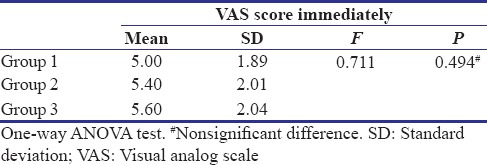
The mean VAS score immediately was compared between Groups 1, 2, and 3 using the one-way ANOVA test. There was no significant difference in the mean VAS score immediately between Groups 1, 2, and 3 [Table 2].
Table 2.
Comparison of visual analog scale scores immediate posttreatment
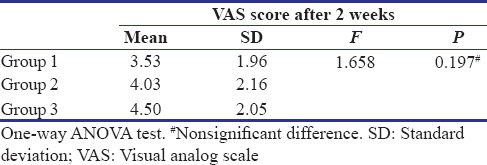
The mean VAS score after 2 weeks was compared between Groups 1, 2, and 3 using the one-way ANOVA test. There was no significant difference in the mean VAS score after 2 weeks between Groups 1, 2, and 3 [Table 3].
Table 3.
Comparison of visual analog scale scores at 2 weeks
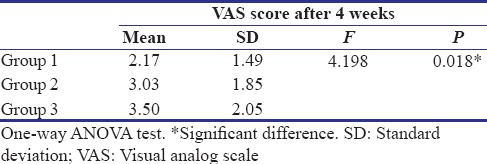
The mean VAS score after 4 weeks was compared between Groups 1, 2, and 3 using the one-way ANOVA test. There was a significant difference in the mean VAS score after 4 weeks between Groups 1, 2, and 3 [Table 4].
Table 4.
Comparison of visual analog scale scores at 4 weeks
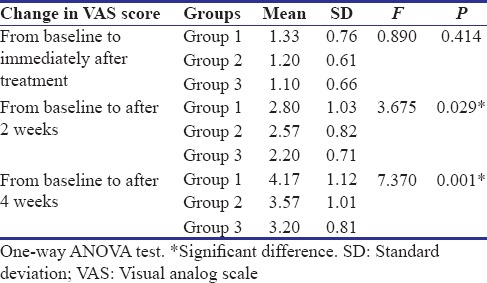
The mean change in VAS score from baseline to immediately after treatment, from baseline to after 2 weeks, and from baseline to after 4 weeks was compared between Groups 1, 2, and 3 using the one-way ANOVA test. There was a significant difference in the mean change in VAS score from baseline to after 2 weeks and from baseline to after 4 weeks between Groups 1, 2, and 3 [Table 5 and Graph 2].
Table 5.
Comparison of change in visual analog scale scores from baseline to 4 weeks
Graph 2.
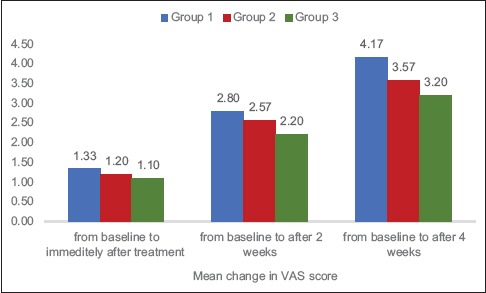
Mean change in visual analog scale scores
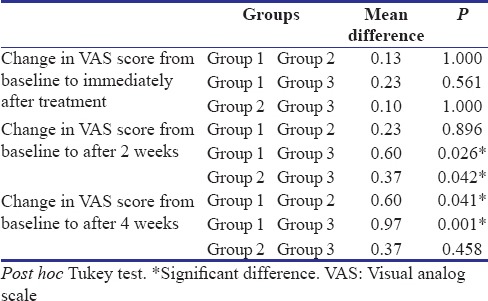
Intergroup comparison of mean change in VAS score from baseline to immediately after treatment, from baseline to after 2 weeks, and from baseline to after 4 weeks was done using the post hoc Tukey test. The mean change in VAS score from baseline to after 2 weeks and from baseline to after 4 weeks was significantly more among Group 1 in comparison to Groups 2 and 3 [Table 6].
Table 6.
Mean of change in the visual analog scale scores from baseline to 4 weeks
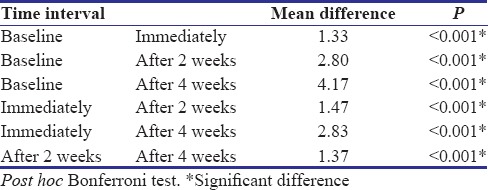
The mean VAS score was compared between the different time intervals using the repeated-measures ANOVA test. There was a significant difference in mean VAS score between different time intervals [Table 7].
Table 7.
Comparison of time interval within Group 1
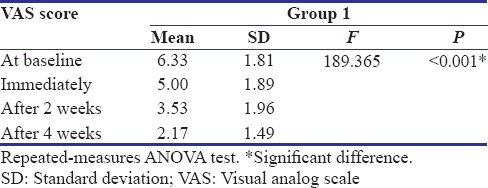
The inter-interval comparison of the mean VAS score between baseline, immediately, after 2 weeks, and after 4 weeks was done using the post hoc Bonferroni test. The mean VAS score decreased significantly from baseline to immediately after treatment to after 2 weeks to after 4 weeks [Table 8].
Table 8.
Mean of time interval within Group 1
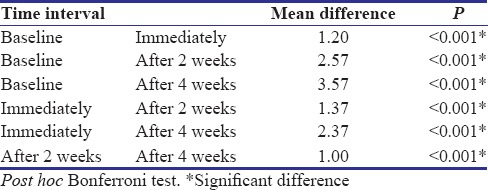
The mean VAS score was compared between the different time intervals using the repeated-measures ANOVA test. There was a significant difference in mean VAS score between different time intervals [Table 9].
Table 9.
Comparison of time interval within Group 2
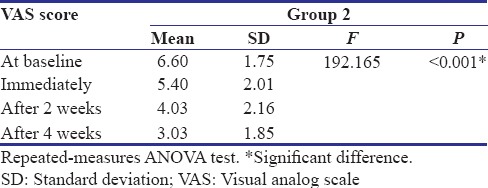
The inter-interval comparison of the mean VAS score between baseline, immediately, after 2 weeks, and after 4 weeks was done using the post hoc Bonferroni test. The mean VAS score decreased significantly from baseline to immediately after treatment to after 2 weeks to after 4 weeks [Table 10].
Table 10.
Mean of time interval within Group 2
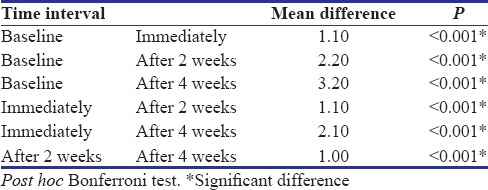
The mean VAS score was compared between the different time intervals using the repeated-measures ANOVA test. There was a significant difference in mean VAS score between different time intervals [Table 11].
Table 11.
Comparison of time interval within Group 3
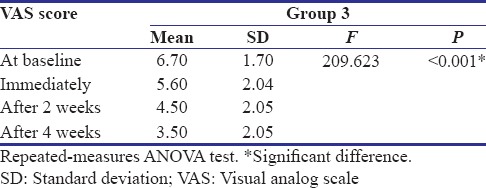
The inter-interval comparison of the mean VAS score between baseline, immediately, after 2 weeks, and after 4 weeks was done using the post hoc Bonferroni test. The mean VAS score decreased significantly from baseline to immediately after treatment to after 2 weeks to after 4 weeks [Table 12].
Table 12.
Mean of time interval within Group 3
Discussion
Pain due to dentinal hypersensitivity is a largely subjective symptom and so achieving effective pain control requires careful assessment and regular review of the patient's experience of dental pain.
The satisfactory material for the treatment of the dentinal hypersensitivity is required to be nonirritant to the pulp, painless on application, should be easy to apply, rapid acting, long-term effective, and consistent.[8]
Desensitizing pastes are the easy and economical option to relieve dentinal hypersensitivity, and majority of them contain potassium salts to numb the pain of hypersensitivity.[9]
The mechanism of action of the newer technologies such as pro-Argin and NovaMin seems to be binding of the exposed dentin tubules by the biologically formed product, hence causing reduction in the hypersensitivity.[10]
Arginine and calcium carbonate at the physiologic pH interact with each other and get bonded to the negatively charged dentin, hence forming a calcium-rich layer onto and into the tubules, consequently sealing them and resulting in the reduction of dentinal hypersensitivity.[11]
Whereas the herbal paste contains naturally derived potassium nitrate (Suryakshara) which seems to help in desensitization of the dental nerves and the other natural ingredients such as spinach (Palakya) contains natural oxalates which help in the formation of phytocomplexes and occlude the exposed dentinal tubules, and also the presence of clove (Lavanga) controls pain due to the obtundant action of eugenol.
The purpose of this study was to investigate which paste among these three can alleviate the symptoms of the patient immediately or in shorter duration, and results show that the mean change in VAS scores from baseline to after 2 weeks and from baseline to after 4 weeks was significantly more among Group 1 in comparison to Groups 2 and 3, so the reduction in the hypersensitivity was more in the Group 1 when compared to other groups.
In this study, the stimuli used were both tactile and evaporative, as it was recommended by Holland et al.[12] that always more than one stimulus should be used because different stimuli stimulate different pain sensations of different intensities.
Other costly options such as iontophoresis and laser therapy exist, but they carry their own disadvantages such as cost, complex apparatus, and long-term ineffectiveness.[13,14]
Conclusion
All the groups showed lower VAS sensitivity values compared with baseline, with group 1 showing better reduction in hypersensitivity in long term, which concludes that desensitizing pastes can be an effective and economical option in the management of the dentinal hypersensitivity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Addy M. Dentine hypersensitivity: New perspectives on an old problem. Int Dent J. 2002;52:367–75. [Google Scholar]
- 2.Bissada NF. Symptomatology and clinical features of hypersensitive teeth. Arch Oral Biol. 1994;39(Suppl):31S–2S. doi: 10.1016/0003-9969(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 3.Carranza FA. Clinical Periodontology. 10th ed. St. Louis: Saunders; 2009. General principles of periodontal surgery; pp. 87–901. [Google Scholar]
- 4.Brännström M. A hydrodynamic mechanism in the transmission of pain production stimuli through dentine. In: Anderson DJ, editor. Sensory Mechanisms in Dentine. Oxford: Pergamon Press; 1963. pp. 73–9. [Google Scholar]
- 5.Orchardson R, Gillam DG. Managing dentin hypersensitivity. J Am Dent Assoc. 2006;137:990–8. doi: 10.14219/jada.archive.2006.0321. [DOI] [PubMed] [Google Scholar]
- 6.Clark GE, Troullos ES. Designing hypersensitivity clinical studies. Dent Clin North Am. 1990;34:531–44. [PubMed] [Google Scholar]
- 7.Pradeep AR, Agarwal E, Naik SB, Bajaj P, Kalra N. Comparison of efficacy of three commercially available dentifrices [corrected] on dentinal hypersensitivity: A randomized clinical trial. Aust Dent J. 2012;57:429–34. doi: 10.1111/j.1834-7819.2012.01726.x. [DOI] [PubMed] [Google Scholar]
- 8.Dowell P, Addy M. Dentine hypersensitivity – A review. Aetiology, symptoms and theories of pain production. J Clin Periodontol. 1983;10:341–50. doi: 10.1111/j.1600-051x.1983.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 9.Docimo R, Montesani L, Maturo P, Costacurta M, Bartolino M, Zhang YP, et al. Comparing the efficacy in reducing dentin hypersensitivity of a new toothpaste containing 8.0% arginine, calcium carbonate, and 1450 ppm fluoride to a benchmark commercial desensitizing toothpaste containing 2% potassium ion: An eight-week clinical study in Rome, Italy. J Clin Dent. 2009;20:137–43. [PubMed] [Google Scholar]
- 10.Jena A, Shashirekha G. Comparison of efficacy of three different desensitizing agents for in-office relief of dentin hypersensitivity: A 4 weeks clinical study. J Conserv Dent. 2015;18:389–93. doi: 10.4103/0972-0707.164052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kleinberg I. SensiStat. A new saliva-based composition for simple and effective treatment of dentinal sensitivity pain. Dent Today. 2002;21:42–7. [PubMed] [Google Scholar]
- 12.Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol. 1997;24:808–13. doi: 10.1111/j.1600-051x.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 13.Singal P, Gupta R. Pandit N 2% sodium fluoride-iontophoresis compared to a commercially available desensitizing agent. J Periodontol. 2005;76:351–7. doi: 10.1902/jop.2005.76.3.351. [DOI] [PubMed] [Google Scholar]
- 14.Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Lasers for the treatment of dentin hypersensitivity: A meta-analysis. J Dent Res. 2013;92:492–9. doi: 10.1177/0022034513487212. [DOI] [PubMed] [Google Scholar]


