Abstract
Background:
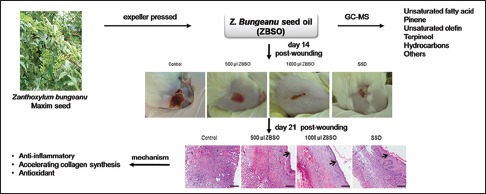
The seed oil of Zanthoxylum bungeanum Maxim (ZBSO) is considered to be rich source of fatty acids, mainly oleic and linoleic acids, and has been used for the treatment of burns in Chinese medicine.
Objective:
We evaluated the healing efficacy of ZBSO and explored its possible mechanism on scalded rats.
Materials and Methods:
Sprague-Dawley rat models with deep second-degree burns were set up, and ZBSO (500 and 1000 μl/wound) was topically applied twice daily for 7 days and then once daily until wound healing. The therapeutic effects of ZBSO were evaluated by observing wound closure time, decrustation time, wound-healing ratio, and pathological changes. Collagen type-III, matrix metalloproteinase-2 (MMP-2), MMP-9, phospho-nuclear factor-κB (p-NF-κB) p65, inhibitor of NF-κB subunit α p-IκBα, and inhibitor of NF-κB subunit α (IκBα) expression were determined using Western blotting.
Results:
The ZBSO-treated group showed a higher wound-healing ratio and shorter decrustation and wound closure times than the untreated group. The topical application of ZBSO increased collagen synthesis as evidenced by an increase in hydroxyproline level and upregulated expression of collagen type-III on days 7, 14, and 21 posttreatment. A reduction in MMP-2 and MMP-9 expressions also confirmed the collagen formation efficacy of ZBSO. Furthermore, there was a significant increase in superoxide dismutase levels and a decrease in malondialdehyde levels in ZBSO-treated wounds. ZBSO also decreased tumor necrosis factor alpha, interleukin-1 (IL-1) β, and IL-6 levels in serum, upregulated IκBα, and downregulated p-NF-κB p65 and p-IκBα expression in vivo, indicating the anti-inflammatory action of ZBSO.
Conclusion:
ZBSO has significant potential to treat burn wounds by accelerating collagen synthesis and the anti-inflammatory cascade of the healing process.
SUMMARY
The seed oil of Zanthoxylum bungeanum Maxim (ZBSO) is rich of fatty acids
The healing efficacy of ZBSO on experimentally scalded rats was evaluated
ZBSO has significant potential to treat deep second-degree burn wounds
ZBSO could accelerate collagen synthesis and inhibit the inflammatory signaling.
Abbreviations used: ECL: Enhanced chemiluminescence; ECM: Extracellular matrix; ELISA: Enzyme-linked immunosorbent assay; GC-MS: Gas chromatography-mass spectrometry; HRP: Horseradish peroxidase; HYP: Hydroxyproline; IκBα: Inhibitor of NF-κB subunit α; IL: Interleukin; MDA: Malondialdehyde; MMP: Matrix metalloproteinase-2; NF-κB: Nuclear factor-κB; SFE: Supercritical fluid extraction; SOD: Superoxide dismutase; SSD: Silver sulfadiazine; TCM: Traditional Chinese medicine; TNF: Tumor necrosis factor.
Keywords: Antioxidant, inflammation, terpenes, wound healing
INTRODUCTION
Burns are one of the most common trauma events treated by physicians.[1] Approximately 450,000 patients per year receive medical treatment related to burns, and there are over 40,000 hospital admissions due to burns every year in the United States.[2] Hence, the treatment of burn wound represents a major medical and economic problem.[3]
The skin as a physical barrier provides primary protection against infection and injury. One of the largest organs in the body, the skin, performs many vital functions including thermoregulation, fluid homeostasis, and immunologic and neurosensory functions.[4] When skin is scalded, the epithelial barrier is destroyed, making it vulnerable to infection. Moreover, the presence of degraded proteins and devitalized tissue provides an excellent environment for the growth and proliferation of microorganisms, which further exacerbates the infection.[5] Healing of a burn wound is a complex and protracted process that is categorized into three overlapping phases: Inflammation, proliferation, and tissue remodeling.[6] Among these phases, the inflammatory cells debride injured tissue during the inflammatory phase, while epithelialization, fibroplasia, and angiogenesis occur during the proliferative phase. Meanwhile, granulation tissue forms, followed by collagen constructing tight cross-links with other collagen and protein molecules. At present, many effective antibacterial substances such as silver sulfadiazine (SSD), sulfamylon, and xeroform are now available for topical application in burn. Other agents used for cleaning and barrier protection meet the majority of clinical demands.[7] However, more effort is needed to find better and more cost-effective products, especially for developing countries.[8]
In alternative and complementary systems of medicine such as traditional Chinese medicine (TCM) and aromatherapy, medicinal plants are widely used for the treatment of many injuries and demonstrate efficacy in burn wound repair.[9,10] Natural remedies to treat burn injury appear to possess moderate efficacy in addition to being safer and cheaper when compared with synthetic drugs.[9,11] The fruits and leaves of Zanthoxylum bungeanum Maxim are a TCM treatment that has been widely used as an analgesic, anesthetic, antibacterial, anti-asthma, and anti-tumor.[12,13] According to the statement on Li Yue Pian Wen (published in 1870), an ancient classic text on topical remedies in China, Z. bungeanum oil can effectively promote the percutaneous absorption of the active components in a prescription.[14] The oil content in seed is 24%–28% (percent dry basis),[15] and the seed oil of Z. bungeanum (ZBSO) is considered to be rich source of fatty acids, mainly oleic and linoleic acids. Although ZBSO has been used for the treatment of burns in folk medicine, there remain few studies on the role of ZBSO in wound healing.
The purpose of the present study was to investigate the healing efficacy of ZBSO topical application on scald wounds in rats and dissect its underlying mechanisms.
MATERIALS AND METHODS
Experimental materials
Seeds of Z. bungeanum were collected in Hancheng County, Shaanxi Province, China, in October 2010. A voucher specimen (1039) was then deposited in the Department of Natural medicine, Fourth Military Medical University (FMMU). The identity of the plant was confirmed by Prof. Xiaofeng Niu (Department of Pharmacognosy in Xi’an Jiaotong University, China). The oil was expeller pressed and then stored in a well-closed vessel for later use.
The chemical standards such as palmitic acid, oleic acid, stearic acid, linoleic acid, and α-linolenic acid were purchased from Sigma-Aldrich (St. Louis, MO, USA). The superoxide dismutase (SOD), malondialdehyde (MDA), hydroxyproline (HYP), and protein assay kits were purchased from Nanjing Jiancheng Bioengineering Institute Co., Ltd. (Nanjing, China). SSD cream was purchased from Hengjian Pharmaceutical Co., Ltd. (Jiangmen, Guangdong, China). Rat tumor necrosis factor (TNF)-α, interleukin (IL)-1 β, and IL-6 enzyme-linked immunosorbent assay (ELISA) kits were purchased from R & D Systems Inc. (Minneapolis, MN, USA). The antibodies for phospho-nuclear factor-κB (p-NF-κB), p65 (ser536), inhibitor of NF-κB subunit α (IκBα), and p-IκBα (ser32) were purchased from Cell Signaling Technology, Inc. (Beverly, MA, USA). Anti-collagen type-III, matrix metalloproteinase-2 (MMP-2), and MMP-9 antibodies were purchased from Abcam (Cambridge, MA, USA). β-actin antibody was purchased from Sigma-Aldrich. The horseradish peroxidase (HRP)-conjugated secondary antibodies were purchased from CWBio Inc. (Beijing, China). The bicinchoninic acid (BCA) protein assay reagent and enhanced chemiluminescence (ECL) kits were purchased from Pierce (Rockford, USA).
Gas chromatography-mass spectrometry analysis
The compositions of ZBSO were analyzed by gas chromatography-mass spectrometry (GC-MS) (GCMS-QP2010, Shimazu, Japan) with a RTX-l MS (30 m × 0.25 mm i.d., 0.25 μm of film thickness) column. The temperature program was as follows: 40°C for 3 min with a linear increase of 5°C/min up to 280°C and standing for 1 min at this temperature. The rate of helium carrier gas was at a rate of 2.0 ml/min. The samples (1 μl) were injected in the split mode (split ratio, 100:1) with ion source temperature at 200°C and interface temperature at 250°C (70 eV ionization energy). The mass analysis mode was two scans per se cond with range, 20–450 m/z. Retention times were utilized as primary criterion for the peaks identification. Using the mass spectrometer as detector offered additional data for the identification of the separated compounds. The isolated compositions were identified and compared with recorded spectra in NIST 08 Mass Spectral Library (Wiley). The percentages of compounds were calculated by the area normalization method without considering response factors.
Fatty acid methyl esters analysis
This method followed the steps previously described[16] and resulted in the formation of fatty acid methyl esters. For this procedure, 2 ml tetradecanoic acid solution (1.5 mg/ml) was added, as an internal standard, to 50 mg of ZBSO in a conical tube. Five milliliters of a methanolic KOH solution (0.5 M) was added to the mixture. The tube was carefully sealed and placed in a water bath at 65°C for 30 min. After the tube was cooled to room temperature, 2 ml of 14% BF3 ether solution was added and placed in boiling water for 5 min. When the saponification was complete, 2 ml of n-hexane and 5 ml of saturated NaCl solution were added. The mixture was shaken and allowed to separate. The n-hexane phase containing methyl esters was injected onto an Agilent 4890D gas chromatograph equipped with a flame ionization detector in the presence of nitrogen as a carrier gas (40 ml/min). A glass column (15% diethylene glycol succinate, 2 m × 3 mm i.d.) at a temperature of 180°C was used for the separation. The injection and detection temperatures were 300°C and 320°C, respectively. The fatty acid standards were also methyl esterified and used for qualitative identification and quantitative determination.
Animals
Male Sprague-Dawley rats (weight 250–300 g) were purchased from the Center of Experimental Animals of FMMU. All the animals were housed five per plastic cages with wood chip bedding for 6 days in an animal room with 12/12 h light-dark cycle and allowed free access to standard chow diet and water. All procedures were approved by the Institutional Animal Care and Use Committee of FMMU and in accordance with the Guidelines for the Care and Use of Laboratory Animals published by the US National Institutes of Health.
Effects of experimental drugs on scald wounds in rat models
The hair on the dorsal surfaces of the rats was shaved with electric clippers and depilated with 10% sodium sulfide solution 24 h before inducing scald injury. After a 12-h fast, the animals were anesthetized with 50 mg/kg body weight of sodium pentobarbital (intraperitoneally [i.p.]). The rats were placed in a prefabricated template with a rectangular opening that exposed the dorsal skin surface while protecting the remaining skin from exposure. The template limits the burn area to about 3 cm × 3 cm, <20% body surface area.[17] The exposed skin surface was immersed in 100°C water for 12 s.[18] Rats were immediately dried and resuscitated with lactated Ringer's solution (4 ml/kg/percentage of total body surface area burn). One-half of the calculated resuscitation volume was administered i.p., and the remaining volume was administered as divided dose by subcutaneous injections immediately postburn. All rats were injected subcutaneously with the analgesic buprenorphine (0.2 mg/kg) immediately after burn injury and again 12 h later. Animals were allowed to recover from anesthesia and housed individually in cages. After 24 h, the rats were randomly divided into four groups (n = 28 per group). Different doses of ZBSO were topically applied to two treatments groups (500 and 1000 μl/wound) twice daily for 7 days and then once daily until wound healing. Likewise, SSD cream was applied to the positive control group twice daily for 7 days and then once daily until wound healing. The rats of the control group were kept under standard conditions without any treatment. On days 7, 14, and 21 postwounding, six animals per group were sacrificed by whole blood collection from the abdominal aorta under anesthesia with sodium pentobarbital. The scalded skin was excised and portions of the skin samples were fixed in buffered formalin and embedded in paraffin for histological examination. The rest of the tissue samples were stored at −80°C.
Macroscopic analyses
The wound surface area was traced on a transparent paper and measured planimetrically every 7 days as describe previously[2] until complete reepithelialization. The wound area was measured using the image analyzing computer program (Image-Pro Plus 6.0). Wound-healing ratio was calculated as following: Wound-healing ratio (%) = (specific day wound surface area − initial wound area)/initial wound area × 100%. Wound closure time and decrustation time were also observed.
Histological examination
Wound samples were collected 1, 7, 14, and 21 days after injury from four animals per group euthanized with an overdose of the anesthetic. The scald wounds were fixed in buffered 10% formaldehyde for more than 24 h. The fixed tissues were processed with increasing concentrations of alcohol and xylol and then embedded in paraffin wax. Sections (5 μm thick) were placed on glass slides and stained with hematoxylin and eosin reagent. Examination and photographs were taken with a light microscope (Eclipse 80i, Nikon, Japan). The morphometric parameters were analyzed using image analysis computer software (Image-Pro Plus 6.2).[19] The thickness of the newly formed epidermis was measured at 0.1-mm intervals in two fields per slide from four skin samples in each group and the mean was calculated.[20] Dermal thickness was determined by measuring the distance from the epidermal-dermal junction to the dermal-fat junction for five randomly selected sites in two fields (×200) per slide from four skin samples in each group.[21] The measurements were taken three times by examining the slides in random sequence, blinded to treatment.
Superoxide dismutase, malondialdehyde, and hydroxyproline analysis
The scald wounds were weighed, cut into small pieces, and homogenized in ice-cold normal saline. The homogenate was then centrifuged at 5000 g for 30 min to remove debris. The SOD, MDA, and HYP levels in the supernatant were determined using commercial kits according to the manufacturer's instructions. Protein concentrations were determined using Lowry's method.[22]
Cytokine assays
TNF-α, IL-1 β, and IL-6 levels in the serum were determined using commercially available ELISA kits according to the manufacturers’ instructions.
Western blot
Scald wounds, including the surrounding wound margin tissue, were excised down to the level of the muscle fascia,[23] chopped into small pieces, and lysed in a radioimmunoprecipitation assay buffer (1% protease inhibitor cocktail and 1% phosphatase inhibitor cocktail) by sonication. The samples were centrifuged at 10,000 ×g for 15 min at 4°C, and supernatants were stored at −80°C. The protein assay was performed using the BCA method. The homogenized tissue samples mixed in a sample buffer were heat reduced in a boiling water bath. After electrophoretic separation by 10%–12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis, the proteins were electrotransferred onto a nitrocellulose membrane. The membrane was blocked for 1 h in Tris-buffered saline with 0.1% Tween-20 (TBST) containing 5% milk protein. After incubation with anti-collagen type-III, MMP-2, TIMP-1, β-actin, p-NF-κBp65, p-IκBα, and IκBα primary antibodies for 2 h, the blots were washed extensively with TBST. The membrane was incubated with HRP-conjugated secondary antibodies for 1 h. After washing, band detection was performed using an ECL kit. Densitometric scanning was performed using Quantity One software (Bio-Rad).
Statistical analyses
The results are expressed as mean ± standard error of the mean. An unpaired Student's t-test was used to compare data between two groups, whereas one-way ANOVA with Tukey's post hoc tests were used for multiple comparisons. A P < 0.05 was considered statistically significant.
RESULTS
Chemical compounds of ZBSO
ZBSO was analyzed by GC-MS, resulting in the identification of 29 compounds. The results are shown in Table 1. ZBSO is rich in unsaturated fatty acid, pinene, unsaturated olefin, terpineol, hydrocarbons, and saturated fatty acids. The main constituents, calculated by the area normalization method, were cis-9, cis-12, cis-15-octadecadienoic acid (α-linolenic acid), cis-9, cis-12-octadecadienoic acid (linoleic acid), (-)-β-pinene, 9,12,15-octadecatrienoic acid, (2R)-2,3-dihydroxypropyl ester, and (9Z,12Z,15Z)-α-pinene. Due to the high boiling points of fatty acids, which are difficult to evaporate,[24] we further characterized fatty acid profiles. At present, fatty acid composition in biological materials is commonly carried out by GC after converting lipid components into corresponding methyl esters.[24] This process changes the volatility of lipid components and improves peak shape. Table 2 shows the fatty acid composition of ZBSO. ZBSO contained high amounts of unsaturated fatty acids including palmitoleic acid, oleic acid, linoleic acid, and α-linolenic acid and the saturated fatty acid including palmitic acid and stearic acid. The predominant fatty acid in ZBSO was α-linolenic acid, which accounted for 46.17%. In addition, ZBSO contained linoleic acid (20.26%), oleic acid (14.48%), palmitic acid (5.15%), stearic acid (2.39%), and palmitoleic acid (1.27%).
Table 1.
Chemical component analysis of the send oil from Zanthoxylum bungeanum Maxim
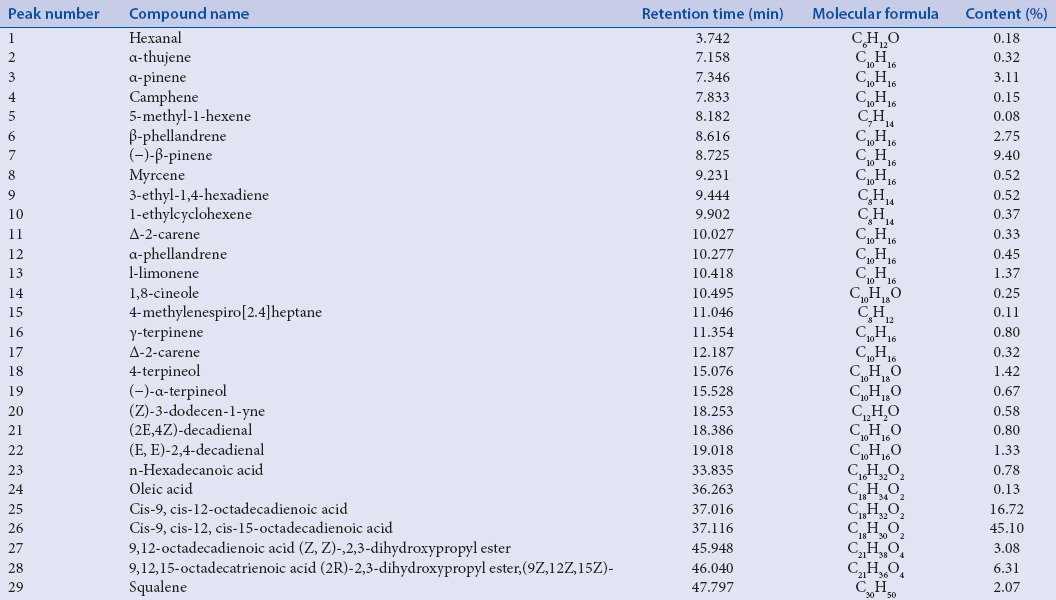
Table 2.
Fatty acid compositions of ZBSO
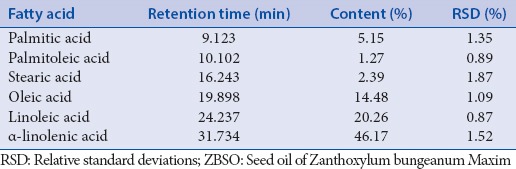
Effects of ZBSO on burn healing
In both groups, the repair process after scalding injury was studied by comparing wound area, wound closure, and decrustation on days 7, 14, 21, and 31. In the first 3 days, the scalding wounds were necrotic eschars and there was no obvious difference among the groups. On the day 14, untreated burn wounds showed edema, whereas wounds treated with ZBSO and SSD showed reduced or no edema [Figure 1a]. There was increased wound-healing ratio in ZBSO treated burn wounds at days 7, 14, 21, and 31 postwounding as compared with untreated control wounds, and the effect was in a dose-dependent manner [Figure 1b]. As shown in Figure 1c, the 1000 μl/wound ZBSO treatment significantly decreased the wound decrustation time (16.9%) and full closure time (10.7%). SSD treatment animals also showed reduced closure comparable with that of ZBSO treated burn wounds, but the decrustation time was longer compared to 1000 μl/wound ZBSO-treated scald wounds.
Figure 1.
Wound healing effects of Zanthoxylum bungeanum Maxim seed oil (ZBSO) on experimentally scalded rats. (a) Photomicrographs showing faster wound contraction in the ZBSO group on day 14 postwounding compared to untreated scald wounds. (b) Wound-healing ratio (n = 6–24). (c) Wound closure time and decrustation time (n = 6–14). These data are expressed as mean ± standard error of the mean. *P < 0.05 versus time-matched control. SSD, silver sulfadiazine
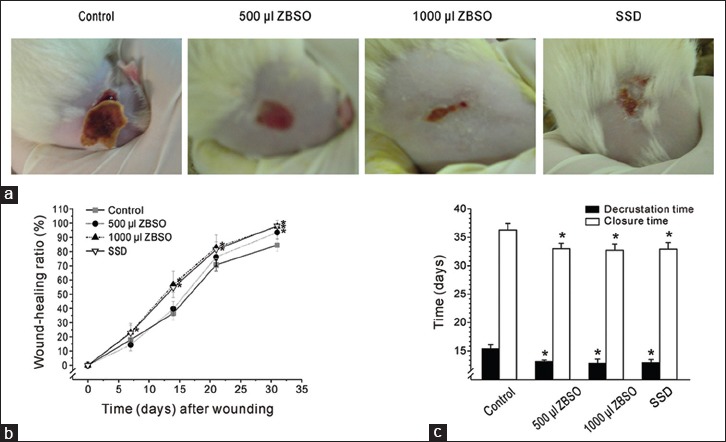
The histological examinations showed that tissue regeneration was much greater in the ZBSO-treated scald wounds [Figure 2a]. In second-degree burns, the epidermis and superficial dermis are the main layers affected. On days 1 and 7 after injury, wound sections of control rats showed a denuded epidermis with a loose crust of inflammatory cells, less blood capillary penetration in granulation tissue, and collagen degeneration. Granulation tissue of the ZBSO- and SSB-treated rats showed reduced congestion, edema, polymorphonuclear leukocyte infiltration, and necrosis, which was present in control animals on days 7 and 14. Proliferation of new epithelium was observed in the ZBSO- and SSD-treated rats on day 7. On day 21, few hair follicles structures existed, and a mass of disorganized red collagen was present in the dermal layer of the control skin. In contrast, new layers of cells originating from the lesion edges gradually occupied the entire surface of the lesion in the ZBSO and SSD groups on day 21. Furthermore, skin wound section of ZBSO-treated groups showed more orderly arrangement of epithelium and collagen fibers than the SSD group, which developed irregular epithelium. Qualitative analyses of samples showed that the thickness of newly formed epidermis was significantly higher in ZBSO groups than in the control group on days 14 and 21 [Figure 2b]. The dermal thickness was highest in SSD-treated groups on day 14 and increased slightly on day 21. However, the dermal thickness in ZBSO groups was comparable to the control group on days 14 and 21 [Figure 2c].
Figure 2.
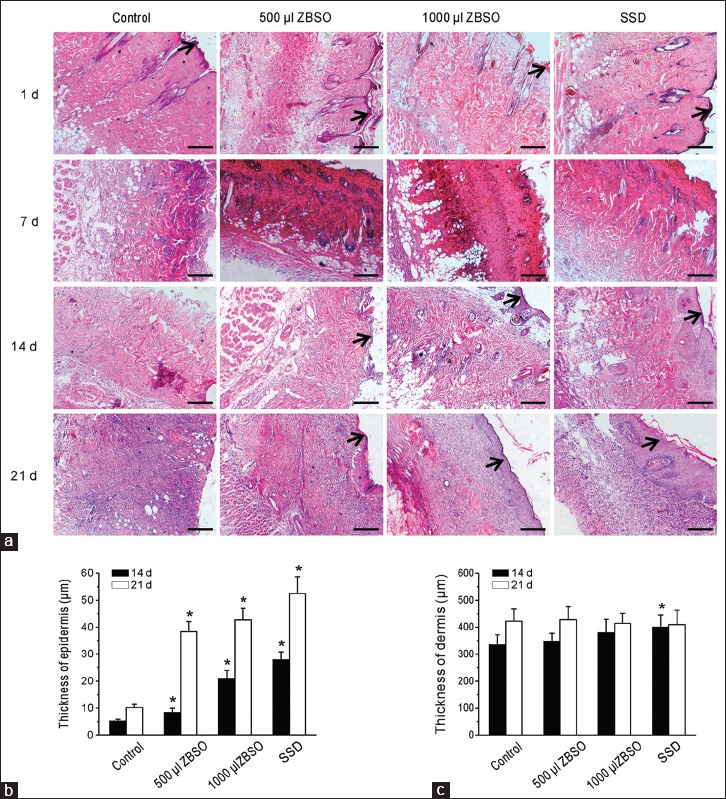
Histological examination of ZBSO on second-degree scald burns in rats. (a) Representative photographs. Scald wounds were collected from each group on days 1, 7, 14 and 21 after injury. The sections were stained with hematoxylin and eosin (→) epidermis. Scale bar = 100 μm. (b and c) Morphometric analysis of the histologic sections showing thickness of epidermis and dermis on 14th and 21st postwounding day, respectively. *P < 0.05 versus time-matched control
Antioxidant effects of ZBSO
MDA is the end product of fatty acid peroxidation. SOD is an important antioxidant enzyme that catalyzes the transformation of superoxide radicals to hydrogen peroxide and oxygen.[25] We measured MDA and SOD as markers for lipid oxidation. Figure 3 shows the MDA and SOD levels in scald wounds of different groups. There was a significant reduction of MDA levels in the 1000 μl ZBSO group and SSD group on the days 7, 14, and 21, and the 1000 μl ZBSO had more inhibition effect than SSD. Five hundred microliters ZBSO also showed reduced MDA levels, particularly on day 21, but there was no significant difference compared to control group on days 7 and 14. Furthermore, ZBSO treatment increased the SOD levels in a dose-dependent manner on days 7, 14, and 21 postwounding. The SOD levels of both the 500 μl- and 1000 μl-ZBSO groups increased more than the SSD group.
Figure 3.
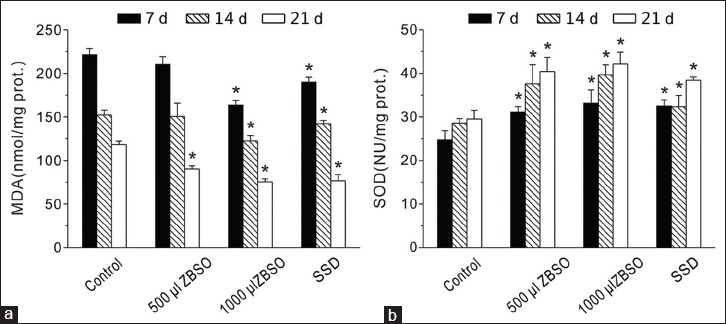
Effect of ZBSO and silver sulfadiazine treatment on the levels of (a) superoxide dismutase and (b) malondialdehyde in deep second-degree scald wounds (n = 5). *P < 0.05 versus time-matched control
Effect of ZBSO on collagen generation
HYP is a marker of collagen content.[26] As shown in Figure 4a, a significant increase in the level of HYP was observed at the beginning of the repair process (days 7 and 14) in ZBSO and SSD groups compared to control group, but on day 21, there was no obvious difference among these groups. Western blotting was used to analyze the collagen type-III expression in scald wounds [Figure 4b]. There were increases in the expression of collagen type-III throughout the experimental period in the ZBSO- and SSD-treated groups. Densitometric quantification analysis demonstrated that the 500 μl- and 1000 μl-ZBSO groups significantly increased collagen type-III protein expression in the wounds and that these enhancement effects peaked on day 14. Treatment with SSD on days 7 and 14 increased expression of collagen type-III protein compared with the control group but decreased on day 21.
Figure 4.
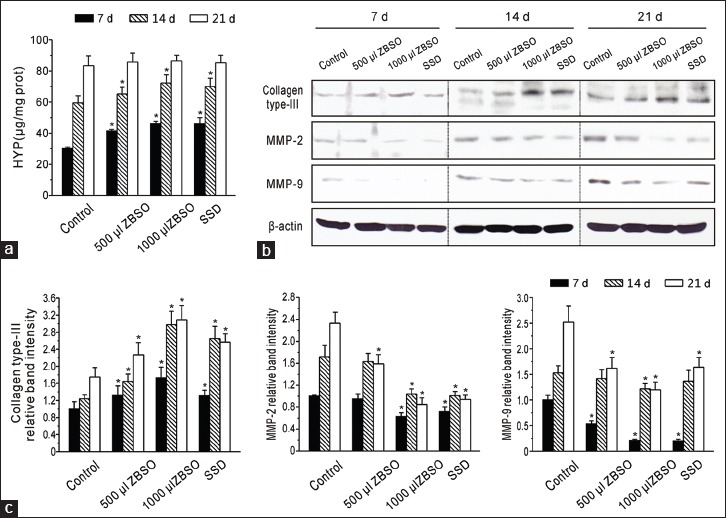
The effect of ZBSO on collagen generation the wound healing process of scalded rats. (a) The level of hydroxyproline in the scald wounds (n = 5). (b) Representative Western blots of collagen type-III, metalloproteinase-2 and metalloproteinase-9. Scald wounds were collected from each group on days 7, 14, and 21 after injury. (c) Densitometric quantification of collagen type-III, metalloproteinase-2, or metalloproteinase-9 to β-actin are summarized (n = 4). *P < 0.05 versus time-matched control
MMPs play important roles during tissue remodeling. MMP-2 and MMP-9 were the major proteins that participated in wound healing in the present study. The expressions of MMP-2 and MMP-9 proteins were evaluated using Western blotting [Figure 4b and c]. A significant time-dependent increase in the expression of MMP-2 was observed in control group. Treatment with ZBSO and SSD decreased the expression of MMP-2 throughout the experimental period. On days 7, 14, and 21, the expression of MMP-2 in the 1000 μl-ZBSO group was reduced to 0.63-fold, 0.60-fold, and 0.36-fold of those in the control groups, respectively. We observed similar results in MMP-9 expression throughout the experimental period in all the groups. On day 7, topical treatment of low- and high-dose ZBSO showed significant inhibition of MMP-9 expression, with a respective 0.52-fold and 0.21-fold increase over that of the control group (P < 0.05).
Effect of ZBSO on inflammation
The inflammatory process plays an important role in the repair of burn injuries. Using ELISA analysis to determine the serum levels of inflammation markers TNF-α, IL-6, and IL-1 β [Figure 5a], we found that the levels of TNF-α and IL-6 were reduced significantly in the ZBSO and SSD groups when compared to the control group on different days after injury (P < 0.05) and that the reduction effects of ZBSO were dose-dependent. Similarly, the level of IL-1 β in the serum of the ZBSO and SSD groups was reduced significantly compared to the control on days 7 and 14 and approached control group levels on day 21. Since the NF-κB signaling pathway plays a key role in the regulation of inflammation, we further investigated whether ZBSO affects the expressions of p-IκBα, IκBα, and p-NF-κBp65 in burn wounds. As shown in Figure 5b and c, ZBSO treatment reduced p-IκBα and p-NF-κBp65 expressions in a dose-dependent and time-dependent manner, while the IκBα expressions increased in ZBSO and SSD groups compared with the control group. IκBα expression in the ZBSO groups peaked on day 7 and then declined on days 14 and 21. Compared to the control group, the 500 μl and 1000 μl ZBSO groups showed a respective 0.87- and 0.49-fold decreased expression of p-IκBα, a respective 0.49- and 0.19-fold decreased expression of p-NF-κBp65, and a respective 1.26- and 2.28-fold increased IκBα expression on day 7. These data suggest that ZBSO topical treatment inhibits the NF-κB signaling pathway in burn wounds.
Figure 5.
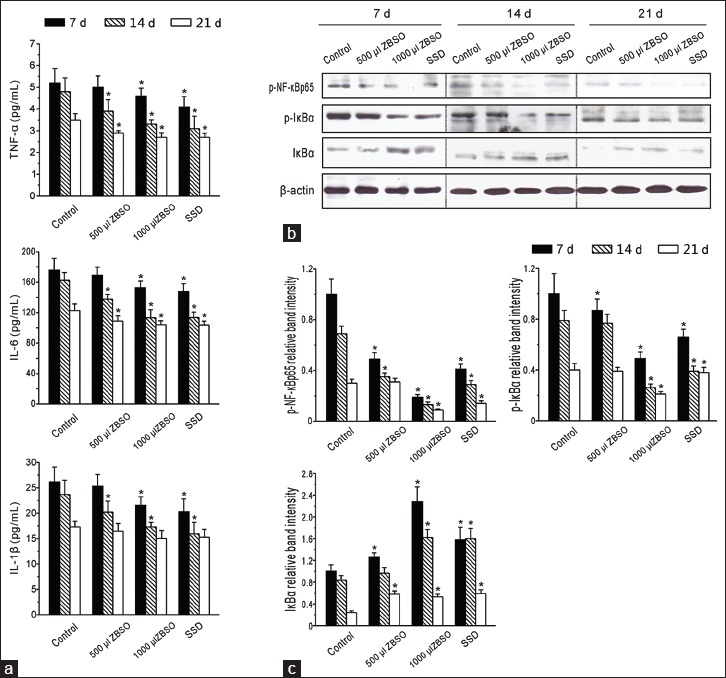
Effect of ZBSO on inflammation in the wound healing process of scalded rats. (a) The levels of tumor necrosis factor-α, interleukin-1 β, and interleukin-6 in serum of experimentally scalded rats (n = 5). (b) Representative Western blots of phospho-nuclear factor-κB p65, phospho-inhibitor of nuclear factor-κB subunit α, and inhibitor of nuclear factor-κB subunit α. (c) Densitometric quantification of phospho-nuclear factor-κB p65, phospho-inhibitor of nuclear factor-κB subunit α, or inhibitor of nuclear factor-κB subunit α to β-actin are summarized (n = 4). *P < 0.05 versus time-matched control
DISCUSSION
The seeds of Z. bungeanum have anti-inflammatory and cicatrizing activities and are used in Chinese folk medicine for asthma and burns. In the present study, we demonstrate that ZBSO significantly reduces the repair time of second-degree scald wounds.
Burns are classified into first, second, and third degrees, with first-degree burns being limited to the epidermis, second-degree burns involving the epidermis and part of the dermis, and third-degree burns destroying the epidermis and all of the dermis.[27,28] The most frequent burn models are the scalding burn and contact burn. In response to burn injury, resident dermal fibroblasts in the neighborhood of the wound proliferate and migrate into the provisional matrix, and then, reepithelialization results in wound closure.[29] Thus, the healing process of burn wound involves complex molecular and cellular events that include cell migration, inflammation, extracellular matrix (ECM) synthesis, and angiogenesis.[30] In the present study, histological findings showed faster reepithelialization and wound closure in ZBSO-treated scald wounds, and these effects might also be associated with the enhanced cell proliferation and collagen generation.
Collagen is a major ECM protein that confers strength and integrity to the tissue matrix.[6] In this study, we observed a well-distributed accumulation of collagen in the scalded skin of the ZBSO-treated groups. The enhanced levels of HYP and collagen type-III in ZBSO-treated scald wounds further demonstrated that ZBSO treatment regulated the collagen biosynthesis and had positive impact on ECM synthesis. The MMPs are a family of enzymes that degrade ECM proteins and play an important role in tissue remodeling associated with various physiological or pathological processes. At present, a total of 24 MMPs subdivided into six types have been reported, which include collagenases (MMP-1 [interstitial collagenase], -8 [neutrophil collagenase], and -13 [collagenase 3]), gelatinases (MMP-2 and -9), stromelysins (MMP-3 and -10), matrilysins (MMP-7 and -26), transmembrane MMPs (MT-MMPs: MMP-14, -15, -16, and -24), and others (MMP-12, -19, -20, -21, -23, -27, and -28).[31] Numerous studies have confirmed a relationship between a delayed healing process and increased levels of MMPs (mainly MMP-2 and MMP-9) in wound healing.[32] Likewise, previous research demonstrates that neutralization of MMPs or modulation of MMP activity may improve wound treatment efficacy.[33] Therefore, we evaluated the expressions of MMP-2 and MMP-9 in wound tissues to clarify whether the wound healing effectiveness of ZBSO treatment may depend on its interference with MMP expression. The western blotting results revealed reduced expressions of MMP-2 and MMP-9 in ZBSO-treated rats, suggesting that ZBSO regulated ECM production and remodeling by inhibiting MMP-2 and MMP-9.
Inflammatory reaction cascades play an important role in wound healing. The activation of the host immune system helps fight infection, whereas overproduced inflammation can lead to tissue damage or even multiple organ failure. Pro-inflammatory cytokines produced by a variety of cells, including the epidermis and macrophages, are involved in inflammation, defective tissue repair, ECM deposition, and tissue contraction.[4,34] TNF-α, IL-6, and IL-1 β also participate in wound healing.[35] In the present study, serum samples collected on days 7, 14, and 21 showed that TNF-α, IL-6, and IL-1 β levels were downregulated by ZBSO treatment, suggesting that ZBSO inhibited the pro-inflammatory response. NF-κB is found in the cytoplasm of inactivated cells, complexed to its inhibitory protein IκB. On activation, IκB dissociates from NF-κB and undergoes ubiquitination and degradation, while NF-κB migrates to the nucleus, where it undergoes phosphorylation on serine 276 of its p65 subunit.[35] It subsequently promotes the transcription of several pro-inflammatory cytokines. To confirm and further elucidate the effects of ZBSO on these genes in the progress of wound healing, we measured their expression in burn wounds. The wounds treated with ZBSO showed reduced p-NF-κBp65 and p-IκBα and increased IκBα expressions, representing the inhibition of NF-κB signaling.
Z. bungeanum Maxim belongs to the Rutaceae family and has been widely used as an important spice and TCM for its special flavors and medicative characters.[36] The plants of this genus are well known for containing several types of compounds, including volatile oil, flavonoids, alkaloids, alkamide, lignans, coumarins, fatty acids, polyphenols, and sterols.[37] Wang et al.[38] identified 51 compounds from the volatile oil of dried Z. bungeanum. The volatile oil from Z. bungeanum was mainly composed of oxygenated monoterpenes and monoterpene hydrocarbons, and the major compounds were 4-terpineol, 1,8-cineole, limonene, α-terpineol, γ-terpinene, terpinyl acetate, and linalool based on the GC-MS analysis.[36,39] Previous studies have verified that this volatile oil can effectively promote the percutaneous permeation of both hydrophilic and lipophilic model drugs and possesses low skin irritation potential.[13] The flavonoids were mainly composed of quercitrin, hyperoside, rutin, and afzelin and displayed free radical scavenging activity.[40] The alkamide fraction, identified as the tingling principles of this plant, was rich in α-sanshool, hydroxy-β-sanshool, and hydroxy-γ-sanshool and displayed anti-itching and anti-wrinkles activities.[41] Yang et al.[42] identified the polyphenols including vanillic acid-4-glucoside (0.0023%), quinic acid (0.0059%), chlorogenic acid (0.25%), epicatechin (0.0078%), 5-feruloylquinic acid (0.0017%), and syringetin-3-glucoside (0.010%) from the leaves of Z. bungeanum. Although many studies have shown the chemical constituents of Z. bungeanum extracted from the pericarps and leaves, there is little research on the compositions of seeds, except the fatty acids. Using GC-MS analysis and computer spectrum search technique, we identified 29 compounds from ZBSO and found that ZBSO composed of monoterpenes and monoterpene hydrocarbons, mainly including (-)-β-pinene (9.40%), α-pinene (3.11%), β-phellandrene (2.75%), 4-terpineol (1.42%), and l-limonene (1.37%). Moreover, ZBSO was rich in unsaturated fatty acids, mainly α-linolenic acid. It has reported that α-linolenic acid had anti-inflammatory and anti-thrombotic properties and was beneficial for the treatment of asthma and thrombosis.[13,43] Further fatty acid composition analysis demonstrated that ZBSO contained six kinds of fatty acids, palmitic acid, palmitoleic acid, oleic acid, linoleic acid, α-linolenic acid, and stearic acid. The content of total unsaturated fatty acids was over 80%, which similar to the data reported by Tang et al.[13] and Yang et al.[15] The chemical composition of ZBSO extracted by supercritical fluid extraction (SFE) was largely consistent with that obtained by mechanical expeller, but the yield of each component is different. Xiao et al.[44] reported that ZBSO extracted by SFE contained 19.25% oleic acid, 27.22% linoleic acid, and 33.26% α-linolenic acid. These components analysis’ results may help to understand the biological activity of ZBSO.
Experimental studies have shown that some oils extracted from plants or animals, such as sea buckthorn (Hippophae rhamnoides L.) seed oil (SBT), ozonated sesame oil, and crocodile oil, are effective in treating burn injuries and accelerating the healing of burns.[20,45,46] SBT seed oil, being rich in polyunsaturated fatty acids such as oleic acid (30%), linoleic acid (26%), and linolenic acid (18%), possessed significant wound healing activity and antioxidant properties.[20] Crocodile oil, of which the main constitutes were oleic acid, linoleic acid, and palmitoleic acid, could enhance cutaneous burn wound healing and reduce scar formation in rats.[45] Collectively, these oils are abundant in unsaturated fatty acid. Previous research has demonstrated the efficacy of fatty acid agents in accelerating wound healing.[47,48] Topical administration of poly- and mono-unsaturated fatty acids, such as linolenic, linoleic, and oleic fatty acids, modulate the closure of surgically induced skin wounds.[47,49] Unsaturated fatty acids can be oxidized to generate lipid mediators such as intermediate hydroperoxides and lipoxins, which can alter the immune response and thereby alter tissue repair.[50] MDA is a stable end product of lipid peroxidation. SOD is an important antioxidant enzyme that protects cells from damage due to superoxide radicals. In the present study, we observed decreased MDA and increased SOD levels in ZBSO-treated wounds. The antioxidant effects of unsaturated fatty acids in ZBSO might help promote burn wound healing. However, the composition of the remainder of the oil remains unknown. Hence, whether and how other known and unknown compounds in ZBSO contribute to its wound-healing effects requires further study.
CONCLUSION
ZBSO showed effective wound healing activities in the skin of experimentally scalded rats. The early reepithelialization and faster wound closure in ZBSO-treated wounds might be associated with the increased antioxidant activity as evidenced by the increase in SOD level and decrease in MDA level, anti-inflammatory action through NF-κB signaling pathway, and accelerated collagen synthesis through the decreasing of MMP-2 and MMP-9 expressions. The enhanced wound healing activity of ZBSO may also be attributed to its phytoconstituents, either due to their individual activity or a synergistic effect. This study provides a basis for the further development and utilization of ZBSO resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank Hui-min Xiao for his technical assistance in GC-MS analysis. This work was supported by National Natural Science Foundation of China (81173513, 81370241, and 81170107). This work was supported by National Natural Science Foundation of China (81370241, 81170107 and 81173513).
REFERENCES
- 1.Singer AJ, Taira BR, Anderson R, McClain SA, Rosenberg L. Does pressure matter in creating burns in a porcine model? J Burn Care Res. 2010;31:646–51. doi: 10.1097/BCR.0b013e3181e4ca73. [DOI] [PubMed] [Google Scholar]
- 2.Venter NG, Monte-Alto-Costa A, Marques RG. A new model for the standardization of experimental burn wounds. Burns. 2015;41:542–7. doi: 10.1016/j.burns.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Lay-flurrie K. Honey in wound care: Effects, clinical application and patient benefit. Br J Nurs. 2008;17:S30–S32-6. doi: 10.12968/bjon.2008.17.Sup5.29649. [DOI] [PubMed] [Google Scholar]
- 4.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev. 2006;19:403–34. doi: 10.1128/CMR.19.2.403-434.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pruitt BA, Jr, McManus AT. The changing epidemiology of infection in burn patients. World J Surg. 1992;16:57–67. doi: 10.1007/BF02067116. [DOI] [PubMed] [Google Scholar]
- 6.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–46. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 7.Ross DA, Phipps AJ, Clarke JA. The use of cerium nitrate-silver sulphadiazine as a topical burns dressing. Br J Plast Surg. 1993;46:582–4. doi: 10.1016/0007-1226(93)90110-w. [DOI] [PubMed] [Google Scholar]
- 8.Gunjan K, Shobha C, Sheetal C, Nanda H, Vikrant C, Chitnis DS. A comparative study of the effect of different topical agents on burn wound infections. Indian J Plast Surg. 2012;45:374–8. doi: 10.4103/0970-0358.101320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fahimi S, Abdollahi M, Mortazavi SA, Hajimehdipoor H, Abdolghaffari AH, Rezvanfar MA. Wound healing activity of a traditionally used poly herbal product in a burn wound model in rats. Iran Red Crescent Med J. 2015;17:e19960. doi: 10.5812/ircmj.19960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nayak BS, Ramlogan S, Chalapathi Rao A, Maharaj S. Neurolaena lobata L. promotes wound healing in Sprague Dawley rats. Int J Appl Basic Med Res. 2014;4:106–10. doi: 10.4103/2229-516X.136791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bahramsoltani R, Farzaei MH, Rahimi R. Medicinal plants and their natural components as future drugs for the treatment of burn wounds: An integrative review. Arch Dermatol Res. 2014;306:601–17. doi: 10.1007/s00403-014-1474-6. [DOI] [PubMed] [Google Scholar]
- 12.Fu TT, Wu JY, Wang L, Ma Y, Wang Y, Liu Y, et al. Study on the Chinese herbal formula for treatment of vaginitis and the antimicrobial activity in murine models. Zhong Yao Cai. 2006;29:931–6. [PubMed] [Google Scholar]
- 13.Tang W, Xie Q, Guan J, Jin S, Zhao Y. Phytochemical profiles and biological activity evaluation of Zanthoxylum bungeanum Maxim seed against asthma in murine models. J Ethnopharmacol. 2014;152:444–50. doi: 10.1016/j.jep.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Xiong QB, Shi DW. Morphological and histological studies of Chinese traditional drug “hua jiao” (pericarpium zanthoxyli) and its allied drugs. Yao Xue Xue Bao. 1991;26:938–47. [PubMed] [Google Scholar]
- 15.Yang FX, Su YQ, Li XH, Zhang Q, Sun RC. Studies on the preparation of biodiesel from Zanthoxylum bungeanum Maxim seed oil. J Agric Food Chem. 2008;56:7891–6. doi: 10.1021/jf801364f. [DOI] [PubMed] [Google Scholar]
- 16.Brian BL, Gracy RW, Scholes VE. Gas chromatography of cyclopropane fatty acid methylesters prepared with methanolic boron trichloride and boron trifluoride. J Chromatogr. 1972;66:138–40. doi: 10.1016/s0021-9673(01)82938-1. [DOI] [PubMed] [Google Scholar]
- 17.Pfurtscheller K, Petnehazy T, Goessler W, Wiederstein-Grasser I, Bubalo V, Trop M. Innovative scald burn model and long-term dressing protector for studies in rats. J Trauma Acute Care Surg. 2013;74:932–5. doi: 10.1097/TA.0b013e31827d0fc3. [DOI] [PubMed] [Google Scholar]
- 18.Cao W, Xie YH, Li XQ, Zhang XK, Chen YT, Kang R, et al. Burn-induced apoptosis of cardiomyocytes is survivin dependent and regulated by PI3K/Akt, p38 MAPK and ERK pathways. Basic Res Cardiol. 2011;106:1207–20. doi: 10.1007/s00395-011-0199-3. [DOI] [PubMed] [Google Scholar]
- 19.Upadhyay NK, Kumar R, Siddiqui MS, Gupta A. Mechanism of wound-healing activity of Hippophae rhamnoides L. leaf extract in experimental burns. Evid Based Complement Alternat Med 2011. 2011:659705. doi: 10.1093/ecam/nep189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Upadhyay NK, Kumar R, Mandotra SK, Meena RN, Siddiqui MS, Sawhney RC, et al. Safety and healing efficacy of sea buckthorn (Hippophae rhamnoides L.) seed oil on burn wounds in rats. Food Chem Toxicol. 2009;47:1146–53. doi: 10.1016/j.fct.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Takagawa S, Lakos G, Mori Y, Yamamoto T, Nishioka K, Varga J. Sustained activation of fibroblast transforming growth factor-beta/Smad signaling in a murine model of scleroderma. J Invest Dermatol. 2003;121:41–50. doi: 10.1046/j.1523-1747.2003.12308.x. [DOI] [PubMed] [Google Scholar]
- 22.Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265–75. [PubMed] [Google Scholar]
- 23.Frank S, Kämpfer H. Excisional wound healing. An experimental approach. Methods Mol Med. 2003;78:3–15. doi: 10.1385/1-59259-332-1:003. [DOI] [PubMed] [Google Scholar]
- 24.Liu KS. Preparation of fatty acid methyl esters for gas-chromatographic analysis of lipids in biological materials. JAOCS. 1994;71:1179–87. [Google Scholar]
- 25.McCord JM, Fridovich I. Superoxide dismutase: The first twenty years (1968-1988) Free Radic Biol Med. 1988;5:363–9. doi: 10.1016/0891-5849(88)90109-8. [DOI] [PubMed] [Google Scholar]
- 26.Venturi M, Bonavina L, Annoni F, Colombo L, Butera C, Peracchia A, et al. Biochemical assay of collagen and elastin in the normal and varicose vein wall. J Surg Res. 1996;60:245–8. doi: 10.1006/jsre.1996.0038. [DOI] [PubMed] [Google Scholar]
- 27.Singh V, Devgan L, Bhat S, Milner SM. The pathogenesis of burn wound conversion. Ann Plast Surg. 2007;59:109–15. doi: 10.1097/01.sap.0000252065.90759.e6. [DOI] [PubMed] [Google Scholar]
- 28.Walker HL, Mason AD., Jr A standard animal burn. J Trauma. 1968;8:1049–51. doi: 10.1097/00005373-196811000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Martin P. Wound healing – Aiming for perfect skin regeneration. Science. 1997;276:75–81. doi: 10.1126/science.276.5309.75. [DOI] [PubMed] [Google Scholar]
- 30.Clark RA. Cutaneous tissue repair: Basic biologic considerations. I. J Am Acad Dermatol. 1985;13(5 Pt 1):701–25. doi: 10.1016/s0190-9622(85)70213-7. [DOI] [PubMed] [Google Scholar]
- 31.Rohani MG, Parks WC. Matrix remodeling by MMPs during wound repair. Matrix Biol. 2015;44-46:113–21. doi: 10.1016/j.matbio.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Krejner A, Grzela T. Modulation of matrix metalloproteinases MMP-2 and MMP-9 activity by hydrofiber-foam hybrid dressing – Relevant support in the treatment of chronic wounds. Cent Eur J Immunol. 2015;40:391–4. doi: 10.5114/ceji.2015.54605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grzela T, Niderla-Bielinska J, Litwiniuk M, White R. The direct inhibition of MMP-2 and MMP-9 by an enzyme alginogel: A possible mechanism of healing support for venous leg ulcers. J Wound Care. 2014;23:278–280. doi: 10.12968/jowc.2014.23.5.278. [DOI] [PubMed] [Google Scholar]
- 34.Kandhare AD, Alam J, Patil MV, Sinha A, Bodhankar SL. Wound healing potential of naringin ointment formulation via regulating the expression of inflammatory, apoptotic and growth mediators in experimental rats. Pharm Biol. 2016;54:419–32. doi: 10.3109/13880209.2015.1038755. [DOI] [PubMed] [Google Scholar]
- 35.Pasparakis M. Regulation of tissue homeostasis by NF-kappaB signalling: Implications for inflammatory diseases. Nat Rev Immunol. 2009;9:778–88. doi: 10.1038/nri2655. [DOI] [PubMed] [Google Scholar]
- 36.Lan Y, Li H, Chen YY, Zhang YW, Liu N, Zhang Q, et al. Essential oil from Zanthoxylum bungeanum Maxim. and its main components used as transdermal penetration enhancers: A comparative study. J Zhejiang Univ Sci B. 2014;15:940–52. doi: 10.1631/jzus.B1400158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu YY, Shen X, Zhang Y, Cao W, Wang K, Xu SZ, et al. Analysis of chemical constituents of volatiles and petroleum ether extract from the branch of Zanthoxylum bungeanum by GC-MS. Asian J Chem. 2014;26:3863–7. [Google Scholar]
- 38.Wang Z, Ding L, Li T, Zhou X, Wang L, Zhang H, et al. Improved solvent-free microwave extraction of essential oil from dried Cuminum cyminum L. and Zanthoxylum bungeanum Maxim. J Chromatogr A. 2006;1102:11–7. doi: 10.1016/j.chroma.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 39.Li Y, Zeng J, Liu L, Jin X. GC-MS analysis of supercritical carbon dioxide extraction products from pericarp of Zanthoxylum bungeanum. Zhong Yao Cai. 2001;24:572–3. [PubMed] [Google Scholar]
- 40.He F, Li D, Wang D, Deng M. Extraction and purification of quercitrin, hyperoside, rutin, and afzelin from Zanthoxylum bungeanum maxim leaves using an aqueous two-phase system. J Food Sci. 2016;81:C1593–602. doi: 10.1111/1750-3841.13331. [DOI] [PubMed] [Google Scholar]
- 41.Artaria C, Maramaldi G, Bonfigli A, Rigano L, Appendino G. Lifting properties of the alkamide fraction from the fruit husks of Zanthoxylum bungeanum. Int J Cosmet Sci. 2011;33:328–33. doi: 10.1111/j.1468-2494.2010.00629.x. [DOI] [PubMed] [Google Scholar]
- 42.Yang LC, Li R, Tan J, Jiang ZT. Polyphenolics composition of the leaves of Zanthoxylum bungeanum Maxim. grown in Hebei, China, and their radical scavenging activities. J Agric Food Chem. 2013;61:1772–8. doi: 10.1021/jf3042825. [DOI] [PubMed] [Google Scholar]
- 43.Yang Q, Cao W, Zhou X, Cao W, Xie Y, Wang S. Anti-thrombotic effects of a-linolenic acid isolated from Zanthoxylum bungeanum Maxim seeds. BMC Complement Altern Med. 2014;14:348. doi: 10.1186/1472-6882-14-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiao HM, He Y, Yang Q, Wang SW, Wang JB, Xie YH. Determination of α-linoleic acid, linoleic acid and oleic acid in hemp seed by HPLC. Zhong Cheng Yao. 2011;33:1361–4. [Google Scholar]
- 45.Li HL, Chen LP, Hu YH, Qin Y, Liang G, Xiong YX, et al. Crocodile oil enhances cutaneous burn wound healing and reduces scar formation in rats. Acad Emerg Med. 2012;19:265–73. doi: 10.1111/j.1553-2712.2012.01300.x. [DOI] [PubMed] [Google Scholar]
- 46.Valacchi G, Lim Y, Belmonte G, Miracco C, Zanardi I, Bocci V, et al. Ozonated sesame oil enhances cutaneous wound healing in SKH1 mice. Wound Repair Regen. 2011;19:107–15. doi: 10.1111/j.1524-475X.2010.00649.x. [DOI] [PubMed] [Google Scholar]
- 47.Cardoso CR, Souza MA, Ferro EA, Favoreto S, Jr, Pena JD. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004;12:235–43. doi: 10.1111/j.1067-1927.2004.012216.x. [DOI] [PubMed] [Google Scholar]
- 48.Feng X, Cheng G, Chen SY, Yang H, Huang W. Evaluation of the burn healing properties of oil extraction from housefly larva in mice. J Ethnopharmacol. 2010;130:586–92. doi: 10.1016/j.jep.2010.05.044. [DOI] [PubMed] [Google Scholar]
- 49.Pereira LM, Hatanaka E, Martins EF, Oliveira F, Liberti EA, Farsky SH, et al. Effect of oleic and linoleic acids on the inflammatory phase of wound healing in rats. Cell Biochem Funct. 2008;26:197–204. doi: 10.1002/cbf.1432. [DOI] [PubMed] [Google Scholar]
- 50.Aliberti J, Hieny S, Reis e Sousa C, Serhan CN, Sher A. Lipoxin-mediated inhibition of IL-12 production by DCs: A mechanism for regulation of microbial immunity. Nat Immunol. 2002;3:76–82. doi: 10.1038/ni745. [DOI] [PubMed] [Google Scholar]


