Abstract
Objectives. To examine changes in maternal–child health surrounding the April 2015 civil unrest in Baltimore, Maryland, following Freddie Gray’s death while in police custody.
Methods. We conducted cross-sectional Children’s HealthWatch surveys January 2014 through December 2015 in pediatric emergency departments and primary care clinics on maternal–child health and June 2015 through October 2015 on daily and community routines. We used trend analysis and piecewise logistic regression to examine effects of time, residential proximity moderation, and mediation analysis to assess proximity and maternal–child health relations via maternal concerns.
Results. Participants comprised 1095 mothers, 93% of whom were African American and 100% of whom had public or no insurance; 73% of participants’ children were younger than 24 months. Following the unrest, prevalence of maternal depressive symptoms increased significantly in proximal, but not distal, neighborhoods (b = 0.41; 95% confidence interval [CI] = 0.03, 0.79; P = .03). Maternal concerns were elevated in proximal neighborhoods and associated with depressive symptoms; mediation through maternal concern was not significant. Five months after the unrest, depressive symptoms returned to previous levels.
Conclusions. Civil unrest has an acute effect on maternal depressive symptoms in neighborhoods proximal to unrest.
Public Health Implications. To mitigate depressive symptoms associated with civil unrest, maintain stability of community routines, screen for maternal depressive symptoms, and provide parent–child nurturing programs.
Community violence is a serious threat in many US cities. Although the consequences of community violence affect the entire community, the detrimental effects on maternal–child health are of particular concern.1–3 Mothers exposed to violence are at increased risk for poor physical and mental health,1,3 including depression, aggressive behaviors, and negative parenting practices.3 Violence exposure is associated with negative child health indicators, particularly behavioral and emotional problems that may undermine children’s physical health and academic performance.2,4
Community violence often occurs in the context of other adversities, increasing the risk for civil unrest.5,6 Multiple stressful circumstances can have lifelong consequences on physical and psychological health, consistent with stress accumulation theories7 and illustrated by adults with adverse childhood experiences.8
Previous studies on community violence have rarely included data before episodes of civil unrest or focused on children younger than 5 years.4,9 We took advantage of a unique opportunity to track changes in maternal–child health surrounding an episode of civil unrest. On April 12, 2015, Baltimore, Maryland, police officers arrested Freddie Gray, an African American man aged 25 years, who sustained neck and spinal injuries while in a police vehicle. His death led to protests citing racism and social injustice. Baltimore erupted in civil unrest: fires, property destruction, and violence. A state of emergency was declared from April 27 until May 6, 6 police officers were indicted, and 2015 ended with 344 murders, one of the highest rates in the city’s history. In a city experiencing multiple adverse events,10 families living in neighborhoods proximal to the civil unrest (zip codes where civil unrest occurred) may have experienced disruptions to their daily routines (e.g., sleeping, eating, shopping) and concerns about safety. These disruptions may add stress, increasing the risk for maternal–child health problems.
To examine how civil unrest relates to maternal–child health,7 we tested 3 hypotheses: (1) the prevalence of maternal depressive symptoms and poor physical health, poor child physical health, and material hardships changes over time (before, during, and following civil unrest); (2) residential proximity to civil unrest moderates the relation between time and maternal–child health problems; and (3) maternal concerns regarding daily and community routines and safety mediate the relation between residential proximity to civil unrest and maternal–child health problems.
METHODS
The study occurred in Baltimore, Maryland. The segregated city11 has more than 620 000 residents, comprising 64% African American, 81% high school graduates, and 24% living below the federal poverty level.12 On the basis of data from the Baltimore City Health Department (Open Baltimore available at: https://data.baltimorecity.gov), the average monthly number of property and violent crime victims varied from 3065 before the unrest to 3831 during the acute unrest, and 3528 five months after the unrest. Family disturbance calls (January–December 2015) increased 16% from an average monthly rate of 2150 before civil unrest to 2499 during and then decreased 8% to 2319 following the unrest.
Study Design and Participants
We collected data between January 2014 and December 2015 from Children’s HealthWatch (http://www.childrenshealthwatch.org), an ongoing cross-sectional investigation of associations among material hardships, public assistance programs, and the health and well-being of young children and their caregivers.13
We collected data among mothers of children younger than 48 months accessing health care at the pediatric emergency department or primary care site at the University of Maryland Medical System. After obtaining informed consent, research assistants recorded children’s weight and length or height and interviewed mothers in private settings using a computer-based survey. To be eligible for the study, participants needed to be English speakers (the Children’s HealthWatch survey is administered in English in Baltimore; fewer than 10% of patients are Spanish speakers), to have state residency, and to have knowledge of the child’s household. We excluded mothers of critically ill or injured children. We limited our analysis to mothers residing in Baltimore. Fewer than 4% had private health insurance (those with private health insurance were primarily University of Maryland Medical System faculty, house officers, and staff), and we eliminated these. We included 1095 mother–child dyads.
To test the third hypothesis, from June to October 2015, we invited a subset of the participants to participate in an additional survey regarding the effect of the civil unrest on their daily life and perceived safety. Participants gave a second consent. Of 212 eligible mothers, 137 consented and completed the additional survey. Refusal to participate was mainly owing to time constraints. There were no differences in residential proximity to civil unrest, child’s gender and age, or maternal country of birth, education, employment, and marital status between participants and nonparticipants.
Measures
There were 3 dependent variables: maternal psychological health (depressive symptoms), maternal and child physical health, and material hardships.
We administered a 3-item depressive symptom screen, with a sensitivity of 100%, a specificity of 88%, and a positive predictive value of 66% with the 8-item Rand screen.14 Items were (1) “Would you say that you have ever felt depressed? If yes, how many times in the past week has this statement been true for you? I have felt depressed . . . no days, 1–2 days, 3–4 days, 5–7 days.” (2) “In the past year, have you had 2 weeks or more during which you felt sad, blue, or depressed or lost pleasure in things that you usually cared about or enjoyed?” (3) “Have you had 2 or more years in your life when you felt depressed or sad most days, even if you felt okay sometimes?” We considered the endorsement of 2 or more items as indicating depressive symptoms.
We measured maternal and child physical health with this single item from the National Health and Nutrition Examination Survey: “In general, would you say your own [your child’s] physical health is . . . ? Excellent, good, fair, or poor.”15 We selected the screening measure because it is easy to administer during a pediatric visit and has been validated.16 We categorized responses as excellent or good versus fair or poor.
Material hardships include food and housing insecurity. We measured food insecurity—the inability to consistently afford enough food for active, healthy lives for all household members in the past 12 months—with the 18-item US Food Security Survey Module, using US Department of Agriculture procedures. We classified mothers who endorsed 3 or more items as food insecure.17 We defined housing insecurity as providing an affirmative response to 1 or more of the following conditions in the past year: behind on rent, crowding (> 2 people per bedroom or > 1 family per residence), or multiple moves (> 2 moves).18
There were 2 independent variables: time in months and periods. Time in months was continuous time elapsed between January 2014 and December 2015. We defined 3 periods using a method recommended and used in other investigations of time trends.19,20 The previous period occurred before the incident on April 14, 2015. The acute period occurred during and immediately after the civil unrest. In the absence of a definition of the conclusion of the acute period, we used change in the monthly prevalence of maternal depressive symptoms (the only dependent variable with a statistically significant change in prevalence) to define the period after.
Proximity to civil unrest was a moderating variable. We defined proximity as residing in the zip codes identified by the Baltimore Police Department as sites of civil unrest, as reported in the Baltimore Sun21 and the Wall Street Journal22 (21201, 21205, 21213, 21223, 21215, 21217) and verified by the Baltimore City Health Department. We defined the 16 other Baltimore zip codes reported by families as distal.
Maternal concerns were a mediating variable. We derived the 18-item maternal concerns questionnaire from topics identified in a Baltimore community violence investigation.1 We determined concerns by endorsements of routine home and community activities for mothers and young children (e.g., sleeping, eating, shopping) or perceived safety. The internal reliability for items addressing concerns regarding daily and community routines was 0.60 and 0.82 for safety (Cronbach α).
We considered sociodemographic factors to be other variables. Mothers provided information on their age, race/ethnicity (race: Asian, Black, White, American Indian, Somali, others [may choose ≥ 1]; ethnicity: Hispanic or not Hispanic), country of origin, marital and employment status, educational level, and participation in public assistance programs (WIC [Special Supplemental Nutrition Program for Women, Infants and Children] and SNAP [Special Nutrition Assistance Program]), as well as the child’s birthdate and gender.
Statistical Analyses
Hypotheses 1 and 2.
We used descriptive statistics to characterize study participants by residence (proximal or distal) and by period (before, acute, or after). We assessed differences in sample characteristics via the χ2 statistic for categorical variables (the Fisher exact test when appropriate) or the t test and analysis of variance for continuous variables (Table 1). As preliminary analyses, we conducted the Cochran-Armitage trend test to examine whether the prevalence of maternal psychological and physical health problems, child physical health problems, or material hardships differed significantly during 2014 to 2015 for proximal and distal neighborhoods separately.
TABLE 1—
Sample Characteristics by Period and Residential Proximity to Civil Unrest: Children’s HealthWatch; Baltimore, MD; January 2014–December 2015
| Proximala No. (%) or Mean ±SD |
Distal No. (%) or Mean ±SD |
||||||||
| Characteristic | Before (Jan. 2014–Mar. 2015), n = 423 | Acute (Apr. 2015–Aug. 2015), n = 104 | After (Sept. 2015–Dec. 2015), n = 115 | Pc | Before (Jan. 2014–Apr. 2015), n = 271 | Acute (Apr. 2015–Aug. 2015), n = 88 | After (Sept. 2015–Dec. 2015), n = 94 | Pc | Pb |
| Child age groups, y | .54 | .07 | .38 | ||||||
| < 1 | 184 (43.5) | 44 (42.3) | 56 (48.7) | 125 (46.1) | 39 (44.3) | 57 (60.6) | |||
| 1 to < 2 | 122 (28.8) | 28 (26.9) | 35 (30.4) | 72 (26.6) | 24 (27.3) | 15 (16.0) | |||
| 2 to < 3 | 70 (16.6) | 15 (14.4) | 14 (12.2) | 41 (15.1) | 19 (21.6) | 11 (11.7) | |||
| 3 to < 4 | 47 (11.1) | 17 (16.4) | 10 (8.7) | 33 (12.2) | 6 (6.8) | 11 (11.7) | |||
| Child is a girl | 211 (49.9) | 49 (47.1) | 58 (50.4) | .86 | 124 (45.8) | 35 (39.8) | 43 (45.7) | .6 | .11 |
| Mean maternal age, y | 26.2 ±5.6 | 25.9 ±5.3 | 26.1 ±5.4 | .92 | 26.3 ±5.5 | 27.0 ±5.7 | 25.2 ±5.0 | .07 | .8 |
| Maternal race | .27 | .14 | .03 | ||||||
| Black/African American | 400 (94.6) | 100 (96.2) | 105 (91.3) | 249 (91.9) | 75 (85.2) | 87 (92.5) | |||
| Other | 23 (5.4) | 4 (3.8) | 10 (8.7) | 22 (8.1) | 13 (14.8) | 7 (7.5) | |||
| Mother born in the US | 416 (98.4) | 103 (99.0) | 110 (95.6) | .16 | 260 (95.9) | 87 (98.9) | 93 (98.9) | .29 | .37 |
| Maternal education | .09 | .69 | < .01 | ||||||
| Some high school or less | 90 (21.3) | 28 (26.9) | 35 (30.4) | 42 (15.6) | 17 (19.5) | 16 (17.0) | |||
| Completed high school | 333 (78.7) | 76 (73.1) | 80 (69.6) | 227 (84.4) | 70 (80.5) | 78 (83.0) | |||
| Maternal marital status | .08 | .38 | .92 | ||||||
| Married | 46 (10.9) | 6 (5.8) | 6 (5.2) | 27 (10.0) | 8 (9.1) | 5 (5.3) | |||
| Not married | 377 (89.1) | 98 (94.2) | 109 (94.8) | 242 (90.0) | 80 (90.9) | 89 (94.7) | |||
| Mother is employed | 163 (38.5) | 48 (46.1) | 54 (47.0) | .14 | 113 (41.7) | 38 (43.2) | 50 (53.2) | .15 | .31 |
| Material hardships | |||||||||
| Food insecurity (yes vs no) | 98 (23.2) | 22 (21.1) | 23 (20.2) | .76 | 54 (19.9) | 25 (28.4) | 19 (20.2) | .23 | .79 |
| Housing insecurity (yes vs no) | 160 (39.7) | 29 (28.7) | 46 (41.1) | .1 | 100 (38.6) | 26 (30.6) | 37 (42.5) | .25 | .91 |
| Maternal health | |||||||||
| Depressive symptoms | 90 (21.3) | 33 (31.7) | 26 (22.6) | .08 | 48 (17.7) | 26 (29.6) | 16 (17.0) | .04 | .19 |
| Fair or poor physical health | 103 (24.5) | 27 (26.0) | 27 (23.5) | .91 | 62 (23.1) | 19 (21.6) | 21 (22.3) | .95 | .48 |
| Child’s health fair or poor (yes vs no) | 23 (5.5) | 9 (8.6) | 7 (6.1) | .48 | 22 (8.1) | 12 (13.6) | 4 (4.3) | .07 | .15 |
Six zip codes where the civil unrest occurred (21201, 21205, 21213, 21223, 21215, 21217).
χ2 and t test comparing residential proximity (proximal vs distal).
χ2 (or Fisher exact) and analysis of variance comparing periods (before, acute, and after).
We used piecewise logistic regression models to assess the pattern of changes in prevalence of maternal–child problems over time.19,20 Multivariable models tested whether the change (slope) differed between periods (before, acute, or after) by including interactions between continuous time (month) and categorical periods in proximal and distal neighborhoods separately. Significant interactions would indicate that change differs across periods. To test whether difference in prevalence over periods differed by residential proximity, we included a 3-way interaction among continuous time, categorical periods, and residence (proximal/distal) in the model.
Hypothesis 3.
We assessed differences in this subset’s characteristics by residential proximity via the χ2 statistic or the Fisher exact test for categorical variables or via the t test for continuous variables (Table 2). Logistic regression assessed maternal concerns about daily and community routines and safety by residential proximity to civil unrest, maternal psychological and physical health, material hardships, and child physical health. To assess whether concerns about daily and community routines and safety mediated relations between proximity and maternal–child health problems, we used the product-of-coefficients approach23 on the basis of a probit model for the mediation model with categorical dependent variable or moderator.
TABLE 2—
Characteristics of Subset by Residential Proximity to Civil Unrest: Children’s HealthWatch; Baltimore, MD; June 2015–October 2015
| Characteristic | Proximal (n = 74),a No. (%) or Mean ±SD, | Distal (n = 63), No. (%) or Mean ±SD | P |
| Child age groups, y | .29 | ||
| < 1 | 22 (29.7) | 25 (39.7) | |
| 1 to < 2 | 23 (31.1) | 11 (17.5) | |
| 2 to < 3 | 16 (21.6) | 16 (25.4) | |
| 3 to < 4 | 13 (17.6) | 11 (17.5) | |
| Child is a girl | 31 (41.9) | 23 (36.5) | .52 |
| Maternal age, yb | 27.0 ±6.0 | 26.2 ±6.3 | .49 |
| Maternal race | .25 | ||
| Black/African American | 68 (91.9) | 54 (85.7) | |
| Other | 6 (8.1) | 9 (14.3) | |
| Maternal country of birthc | ≥ .99 | ||
| US-born | 73 (98.7) | 63 (100.0) | |
| Maternal education | .3 | ||
| Some high school or less | 21 (28.4) | 13 (20.6) | |
| Completed high school | 53 (71.6) | 50 (79.4) | |
| Maternal marital status | .99 | ||
| Married | 7 (9.5) | 6 (9.5) | |
| Not married | 67 (90.5) | 57 (90.5) | |
| Mother is employed | 40 (54.1) | 31 (49.2) | .57 |
| Presence of material hardship | 35 (47.3) | 38 (60.3) | .13 |
| Fair or poor maternal physical health | 28 (37.8) | 19 (30.2) | .34 |
| Maternal depressive symptoms | 34 (46.0) | 22 (34.9) | .19 |
| Fair or poor child physical health | 8 (10.8) | 6 (9.5) | .8 |
| Reported concerns regarding | |||
| Daily or community routines | 57 (77.0) | 34 (54.0) | < .01 |
| Safety | 40 (54.1) | 28 (44.4) | .26 |
Six zip codes where the civil unrest occurred (21201, 21205, 21213, 21223, 21215, 21217).
t test.
Fisher exact test.
We conducted analyses using SAS version 9.3 (SAS Institute, Cary, NC) and Mplus 7.0.24 We used the 2-tailed test, and we considered a P level of less than or equal to .05 to be significant.
RESULTS
Mean maternal age was 26 years. Most mothers were African American (93%), were US-born (98%), had completed high school (79%), were not married (91%), were not employed (57%), were recruited from the emergency department (89%), and lived in neighborhoods proximal to the civil unrest (59%). Among children, 46% were younger than 1 year, 47% were girls, and 7% had fair or poor health. Among mothers, 22% reported 2 or more depressive symptoms, 24% had fair or poor health, 22% experienced food insecurity, 38% experienced housing insecurity, 84% received WIC and 80% SNAP benefits.
Periods
We defined 3 periods: before the civil unrest (January 2014 through March 2015), acute (during the civil unrest April–August 2015), and after the civil unrest (September–December 2015). Across all 3 civil unrest periods, we found no significant differences in sample characteristics for proximal or distal neighborhoods separately. Combining the 3 periods, mothers living in neighborhoods distal to the civil unrest were more likely to be high school graduates and less likely to be African American than were mothers living in proximal neighborhoods (Table 1), with no differences in children’s age or gender or maternal marital status, employment, or age.
Covariates included child’s age group, maternal race, age, marital status and education, which were variables associated with periods or proximity.
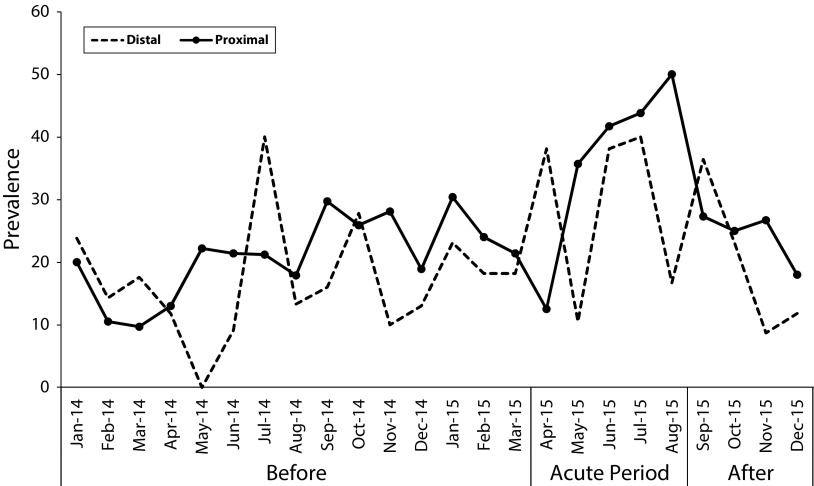
Trend Analyses
In proximal neighborhoods, the monthly depressive symptoms prevalence increased from a high of 30% before civil unrest to 50% during acute civil unrest (Figure 1).
FIGURE 1—
Monthly Prevalence of Maternal Depressive Symptoms by Residential Proximity: Children’s HealthWatch; Baltimore, MD; January 2014–December 2015
Prevalence differed in proximal neighborhoods on the basis of the Cochran-Armitage trend test (z = 1.96; P = .050), with no difference in depressive symptoms prevalence in distal neighborhoods (z = 0.56; P = .57). There were no significant differences in the prevalence of maternal fair or poor health, child fair or poor health, or material hardships over time on the basis of residential proximity (all P > .10). Our further analyses focused exclusively on maternal depressive symptoms.
Before the civil unrest, changes in maternal depressive symptoms did not differ by residential proximity. During the acute civil unrest, changes in depressive symptoms varied by residential proximity, as verified by the significant 3-way interaction among month, periods, and proximity (b = 0.53; 95% confidence interval [CI] = 0.01, 1.05; P = .045). In proximal neighborhoods, changes in depressive symptoms increased significantly during the acute civil unrest period compared with the period before civil unrest, as indicated by the significant 2-way interaction between period and proximity (b = 0.41; 95% CI = 0.03, 0.79; P = .03). In distal neighborhoods, changes in depressive symptoms during the acute civil unrest period did not differ from the previous period (b = −0.03; 95% CI = −0.41, 0.34; P > .86). The prevalence of depressive symptoms decreased significantly following the acute civil unrest period in distal neighborhoods compared with the period before the acute phase, as indicated by the 2-way interaction between period and proximity (b = −0.71; 95% CI = −1.26, −0.16; P = .01).
Characteristics of Sample Subset
Among the subset of mothers who completed the additional questionnaire following the unrest, mean maternal age was 27 years, most mothers were African American (89%), were US-born (99%), were not married (90%), experienced at least 1 type of material hardship (53%), were concerned about either daily and community routines or safety (76%), and were recruited from the emergency department (96%; Table 2).
Demographic variables did not differ by proximity.
Maternal Concerns
Although child gender was not significantly related to maternal concerns about daily and community routines (75% girls vs 60% boys; P = .06), we included it as a covariate. On the basis of logistic regression models, mothers in proximal neighborhoods were more likely to express concerns about daily and community routines (adjusted odds ratio [AOR] = 2.83; 95% CI = 1.34, 5.94; P < .01; 77% vs 54%) than were mothers in distal neighborhoods. Mothers with concerns regarding daily and community routines were more likely to report depressive symptoms (AOR = 2.33; 95% CI = 1.07, 5.05; P = .03) than were mothers without concerns. Proximity to unrest and maternal depressive symptoms were not related to safety concerns. Neither maternal–child physical health nor material hardships was associated with maternal concerns.
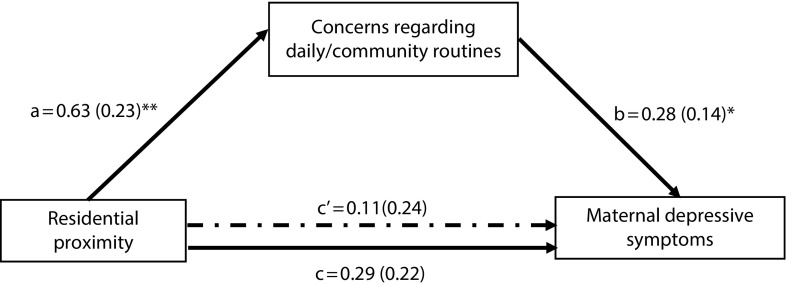
Mediation Analysis
On the basis of the probit model and adjusting for child gender, residential proximity was related to maternal concerns regarding daily and community activities (a = 0.63; SE = 0.23; P < .01), and maternal concerns were related to maternal depressive symptoms after adjusting for proximity and child gender (b = 0.28; SE = 0.14; P = .04).
The total effect between residential proximity and maternal depressive symptoms was not significant (c = 0.29; SE = 0.22; P = .19). Neither was the mediation effect (indirect) between proximity and maternal depressive symptoms via maternal concerns regarding daily and community activities (a × b = 0.18; SE = 0.11; P = .096; Sobel test; Figure 2). The mediating effect of safety concerns was not significant in the relation between residential proximity and maternal depressive symptoms (a × b = 0.04; SE = 0.05; P = .39).
FIGURE 2—
Path Model of Residential Proximity on Maternal Depressive Symptoms via Concerns Regarding Daily and Community Routines: Children’s HealthWatch; Baltimore, MD; June 2015–October 2015
Note. Indirect effect via maternal concerns is a × b = 0.18; SE = 0.11; P = .096 on the basis of the Sobel test and adjusted for child gender.
*P < .05; **P < .01.
DISCUSSION
This investigation yielded 3 primary findings regarding the impact of civil unrest on mothers. First, an acute reactive period of elevated maternal depressive symptoms occurred during the 5 months immediately surrounding the civil unrest (April–August 2015), followed by a return to rates comparable to those reported before the unrest. Second, residential proximity to civil unrest increased the likelihood of elevated rates of depressive symptoms. Third, maternal concerns regarding daily and community activities were elevated in proximal neighborhoods, but maternal concerns did not fully explain the relation between residential proximity and maternal depressive symptoms.
Maternal–Child Health
In a city with chronic community violence and racial segegation,11 patterns of maternal depressive symptoms varied by residential proximity to civil unrest, as predicted by stress accumulation theories,7 reaching 50% in proximal neighborhoods. Maternal depressive symptoms, even intermittent symptoms, can undermine maternal well-being and negatively affect parenting behaviors,25 thereby increasing children’s risk of negative socioemotional development related to difficulties in attention regulation, attachment, achievement, adaptive skills, and externalizing and internalizing behavior,26 especially early in life when young children are highly dependent on their mothers and sensitive to variations in interpersonal relationships.27
Stress and violence exposure can cause disruptions in the hypothalamic–pituitary–adrenal axis and brain morphology,28 potentially placing young children at risk for subsequent physical and mental health conditions. One possible explanation for the absence of child health findings in this investigation is our focus on physical health, rather than behavioral and socioemotional development.
Approximately 5 months after the acute civil unrest period, maternal depressive symptoms returned to previous levels in proximal neighborhoods and declined below previous levels in distal neighborhoods. The reason for the decline is unknown, particularly in the context of high rates of property and violent crimes and family disturbance calls throughout the city, but may relate to the positive response of the local government and institutions to restore order and safety, to enable families to return to routine community activities, to provide contacts of available services, and to initiate a mental health and trauma recovery plan.5
In addition, the end of the summer and the resumption of routines associated with school in September may have contributed to a return to previous levels. Although the decline in the prevalence of maternal depressive symptoms is a positive sign, having more than one fifth of mothers report depressive symptoms, along with one half reporting material hardships, signifies chronic conditions of stress for mothers that may undermine young children’s health and well-being.13,29
Maternal Concerns
More than three quarters of the mothers living in the zip codes proximal to the civil unrest expressed concerns regarding daily and community routines, suggesting that the civil unrest may have disrupted daily and community activities for mothers and children. Daily routines provide a sense of security and are important to young children’s development.30 Although maternal concerns were associated with maternal depressive symptoms, as predicted by theories of stress accumulation,7 and may have caused mothers to limit daily and community activities,31 the mediation analysis found that maternal concerns did not completely explain the relation between proximity and maternal depressive symptoms.
The nonsignificant finding may be attributed to the lack of power because of the limited sample size. Another possibility is our reliance on cross-sectional data, which may have clouded the temporal aspects of the relations among civil unrest with subsequent concerns and depressive symptoms.
Additional Findings
Civil unrest was not related to maternal and child physical health or to housing and food insecurity. One possible explanation is that the property destruction was directed against shops (especially pharmacies), not homes or individuals. Another possibility is that the local government and other organizations moved quickly to restore order and initiate services.5 A third possibility is that public assistance programs may have buffered families from hardships. Finally, the civil unrest may have disrupted children’s socioemotional development, including their attachment, emotional regulation, and attention. However, Children’s HealthWatch is designed to focus on children’s physical health, and we did not measure socioemotional development. Further investigations on the effect of community violence should examine children’s socioemotional development.
Approximately 50% of the mothers expressed concerns about safety, regardless of residential proximity to the civil unrest. This finding is generally consistent with a previous report from Baltimore,1 which found relatively low safety concerns in communities with high rates of violence.
Gender differences in socialization practices are common among African American families, as we observed.32 The elevated concern among mothers of daughters may represent their perceived vulnerability to civil unrest.
Limitations and Strengths
This study has several limitations. Information about maternal psychological and physical health, child physical health, and material hardships was mother reported and may be subject to over- or underreporting. We used a convenience sample, which may not represent the general population, as it included mother–child pairs who sought emergency medical care. Emergency departments are a safety net for low-income, uninsured families and are often used for nonurgent conditions.33
We assessed depressive symptoms through a validated screening tool,14 rather than considering other psychological symptoms, such as anxiety. The distal area represented multiple zip codes, with varying resources and many with very few families represented. Because of this pattern, we did not have the power to conduct multilevel modeling to examine participants within zip codes and therefore compared proximal versus distal zip codes.
Major strengths are the focus on mothers of very young children and systematic data collection over 2 years, including periods before, during, and after the unrest. This approach enabled us to isolate the acute civil unrest period and investigate changes in the prevalence of maternal–child health problems.
Conclusions
The aftermath of the civil unrest continued through 2016, as noted by increased rates of property and violent crimes (including murders) and family disturbance calls, the trials of the 6 indicted police officers (all acquitted), and findings of the US Justice Department34 that the Baltimore Police Department “engages in a pattern or practice of conduct that violates the Constitution or federal law,” including racial discrimination.
Civil unrest often reflects social injustice. Consequences to the communities extend far beyond physical destruction and disrupt the daily functioning of mothers and young children.
Public Health Implications
There is an urgent need for public health practitioners to develop policies and programs to ensure that mothers and children are protected from community violence and civil unrest. Multilevel strategies can reduce social injustice by providing basic resources for low-income communities and families, including safety and access to affordable housing, food, medications, and services. Strategies that engage community members in effective solutions to address their concerns can improve their perceptions of safety, leading to beneficial effects on parents’ interactions with their children.2
In response to civil unrest, public health responses are needed to work with the community, along with local, state, and federal agencies to restore safety, justice, and families’ ability to engage in routine daily and community activities. Setting up communication systems, including hotlines, may reduce anxiety and help families feel informed and connected to safe community resources and services10; however, community outreach may be necessary to ensure that families are aware of communication systems.5 Clinical recommendations following civil unrest include screening for maternal psychological symptoms and children’s behavioral and socioemotional development and providing parent–child nurturing programs that can mitigate negative mental health effects of civil unrest.35
ACKNOWLEDGMENTS
Data collection was supported in part by funding to Children’s HealthWatch, donors to which are listed at http://www.childrenshealthwatch.org.
Findings from this study were presented at the Pediatric Academic Societies 2017 Meeting; May 8, 2017; San Francisco, CA.
We acknowledge the contributions of Jonathan Gross, MPH, from the Baltimore City Health Department; Laurence S. Magder, PhD, from the Department of Epidemiology and Public Health, University of Maryland School of Medicine; and the Children’s HealthWatch team, especially Deborah A. Frank, MD, Mariana Chilton, PhD, Megan Sandel, MD, Eduardo Ochoa, MD, Diana Cutts, MD, Patrick H. Casey, MD, and Stephanie A. Ettinger De Cuba, MPH.
HUMAN PARTICIPANT PROTECTION
The Children’s HealthWatch study was approved by the University of Maryland Baltimore institutional review board.
Footnotes
REFERENCES
- 1.Johnson SL, Solomon BS, Shields WC, McDonald EM, McKenzie LB, Gielen AC. Neighborhood violence and its association with mothers’ health: assessing the relative importance of perceived safety and exposure to violence. J Urban Health. 2009;86(4):538–550. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maschi T, Perez RM, Tyson E. Exploring the relationship between exposure to violence, perceptions of neighborhood safety, and children’s adaptive functioning: clinical and community implications. J Hum Behav Soc Environ. 2010;20(6):744–761. [Google Scholar]
- 3.Mitchell SJ, Lewin A, Horn IB, Valentine D, Sanders-Phillips K, Joseph JG. How does violence exposure affect the psychological health and parenting of young African American mothers? Soc Sci Med. 2010;70(4):526–533. doi: 10.1016/j.socscimed.2009.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 5.Wen LS, Warren KE, Tay S, Khaldun JS, O’Neill DL, Farrow OD. Public health in the unrest: Baltimore’s preparedness and response after Freddie Gray’s death. Am J Public Health. 2015;105(10):1957–1959. doi: 10.2105/AJPH.2015.302838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drake B, Rank MR. The racial divide among American children in poverty: reassessing the importance of neighborhood. Child Youth Serv Rev. 2009;31(12):1264–1271. [Google Scholar]
- 7.Seo D, Tsou KA, Ansell EB, Potenza MN, Sinha R. Cumulative adversity sensitizes neural response to acute stress: association with health symptoms. Neuropsychopharmacology. 2014;39(3):670–680. doi: 10.1038/npp.2013.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 9.Farver JA, Frosch DL. L.A. stories: aggression in preschoolers’ spontaneous narratives after the riots of 1992. Child Dev. 1996;67(1):19–32. doi: 10.1111/j.1467-8624.1996.tb01716.x. [DOI] [PubMed] [Google Scholar]
- 10.Wen LS, Sharfstein JM. Unrest in Baltimore: the role of public health. JAMA. 2015;313(24):2425–2426. doi: 10.1001/jama.2015.5561. [DOI] [PubMed] [Google Scholar]
- 11.Massey DS, Tannen J. A research note on trends in Black hypersegregation. Demography. 2015;52(3):1025–1034. doi: 10.1007/s13524-015-0381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Census Bureau. QuickFacts: Baltimore City, Maryland. Available at: https://www.census.gov/quickfacts/table/PST045216/2404000. Accessed July 20, 2016.
- 13.Frank DA, Casey PH, Black MM et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics. 2010;125(5):e1115–e1123. doi: 10.1542/peds.2009-1078. [DOI] [PubMed] [Google Scholar]
- 14.Kemper KJ, Babonis TR. Screening for maternal depression in pediatric clinics. Am J Dis Child. 1992;146(7):876–878. doi: 10.1001/archpedi.1992.02160190108031. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey 1988–94. Atlanta, GA: 1994. [Google Scholar]
- 16.Monette S, Séguin L, Gauvin L, Nikiéma B. Validation of a measure of maternal perception of the child’s health status. Child Care Health Dev. 2007;33(4):472–481. doi: 10.1111/j.1365-2214.2006.00713.x. [DOI] [PubMed] [Google Scholar]
- 17.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 18.Cutts DB, Meyers AF, Black MM et al. US housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 20.Chou C, Yang D, Pentz MA, Hser Y. Piecewise growth curve modeling approach for longitudinal prevention study. Comput Stat Data Anal. 2004;46(2):213–225. [Google Scholar]
- 21.Harris EP. Baltimore riots: damage and incidents of violence. 2015. Available at: http://www.baltimoresun.com/news/maryland/bal-map-mondays-violence-20150427-htmlstory.html. Accessed September 22, 2016.
- 22.Chinni D. Zip codes map out impact of Baltimore unrest. 2015. Available at: http://blogs.wsj.com/washwire/2015/04/29/zip codes-spell-out-affect-of-baltimore-unrest. Accessed September 22, 2016.
- 23.MacKinnon DP. Introduction to Statistical Mediation Analysis. New York, NY: Taylor and Francis; 2008. [Google Scholar]
- 24.Muthén LK, Muthén BO. Mplus User’s Guide: Statistical Analysis with Latent Variables. 7th ed. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 25.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 26.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 27.Campbell SB, Brownell CA, Hungerford A, Spieker SI, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev Psychopathol. 2004;16(2):231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- 28.Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131(2):319–327. doi: 10.1542/peds.2012-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernández D, Jiang Y, Carrión D, Phillips D, Aratani Y. Housing hardship and energy insecurity among native-born and immigrant low-income families with children in the United States. J Child Poverty. 2016;22(2):77–92. doi: 10.1080/10796126.2016.1148672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zisberg A, Young HM, Schepp K, Zysberg L. A concept analysis of routine: relevance to nursing. J Adv Nurs. 2007;57(4):442–453. doi: 10.1111/j.1365-2648.2007.04103.x. [DOI] [PubMed] [Google Scholar]
- 31.Dias JJ, Whitaker RC. Black mothers’ perceptions about urban neighborhood safety and outdoor play for their preadolescent daughters. J Health Care Poor Underserved. 2013;24(1):206–219. doi: 10.1353/hpu.2013.0018. [DOI] [PubMed] [Google Scholar]
- 32.Mandara J, Varner F, Richman S. Do African American mothers really “love” their sons and “raise” their daughters? J Fam Psychol. 2010;24(1):41–50. doi: 10.1037/a0018072. [DOI] [PubMed] [Google Scholar]
- 33.Mortensen K, Song PH. Minding the gap: a decomposition of emergency department use by Medicaid enrollees and the uninsured. Med Care. 2008;46(10):1099–1107. doi: 10.1097/MLR.0b013e318185c92d. [DOI] [PubMed] [Google Scholar]
- 34.US Department of Justice, Civil Rights Division. Investigation of the Baltimore City Police Department. 2016. Available at: https://www.justice.gov/opa/file/883366/download. Accessed October 4, 2016.
- 35.Furlong M, McGilloway S, Bywater T, Hutchings J, Smith SM, Donnelly M. Cochrane review: behavioural and cognitive-behavioural group-based parenting programmes for early onset conduct problems in children aged 3 to 12 years. Evid Based Child Health. 2013;8(2):318–692. doi: 10.1002/ebch.1905. [DOI] [PubMed] [Google Scholar]