Abstract
IMPORTANCE
US health care spending has continued to increase, and now accounts for more than 17% of the US economy. Despite the size and growth of this spending, little is known about how spending on each condition varies by age and across time.
OBJECTIVE
To systematically and comprehensively estimate US spending on personal health care and public health, according to condition, age and sex group, and type of care.
DESIGN AND SETTING
Government budgets, insurance claims, facility surveys, household surveys, and official US records from 1996 through 2013 were collected and combined. In total, 183 sources of data were used to estimate spending for 155 conditions (including cancer, which was disaggregated into 29 conditions). For each record, spending was extracted, along with the age and sex of the patient, and the type of care. Spending was adjusted to reflect the health condition treated, rather than the primary diagnosis.
EXPOSURES
Encounter with US health care system.
MAIN OUTCOMES AND MEASURES
National spending estimates stratified by condition, age and sex group, and type of care.
RESULTS
From 1996 through 2013, $30.1 trillion of personal health care spending was disaggregated by 155 conditions, age and sex group, and type of care. Among these 155 conditions, diabetes had the highest health care spending in 2013, with an estimated $101.4 billion (uncertainty interval [UI], $96.7 billion–$106.5 billion) in spending, including 57.6% (UI, 53.8%–62.1%) spent on pharmaceuticals and 23.5% (UI, 21.7%–25.7%) spent on ambulatory care. Ischemic heart disease accounted for the second-highest amount of health care spending in 2013, with estimated spending of $88.1 billion (UI, $82.7 billion–$92.9 billion), and low back and neck pain accounted for the third-highest amount, with estimated health care spending of $87.6 billion (UI, $67.5 billion–$94.1 billion). The conditions with the highest spending levels varied by age, sex, type of care, and year. Personal health care spending increased for 143 of the 155 conditions from 1996 through 2013. Spending on low back and neck pain and on diabetes increased the most over the 18 years, by an estimated $57.2 billion (UI, $47.4 billion–$64.4 billion) and $64.4 billion (UI, $57.8 billion–$70.7 billion), respectively. From 1996 through 2013, spending on emergency care and retail pharmaceuticals increased at the fastest rates (6.4% [UI, 6.4%–6.4%] and 5.6% [UI, 5.6%–5.6%] annual growth rate, respectively), which were higher than annual rates for spending on inpatient care (2.8% [UI, 2.8%–2.8%] and nursing facility care (2.5% [UI, 2.5%–2.5%]).
CONCLUSIONS AND RELEVANCE
Modeled estimates of US spending on personal health care and public health showed substantial increases from 1996 through 2013; with spending on diabetes, ischemic heart disease, and low back and neck pain accounting for the highest amounts of spending by disease category. The rate of change in annual spending varied considerably among different conditions and types of care. This information may have implications for efforts to control US health care spending.
Health care spending in the United States is greater than in any other country in the world.1 According to official US estimates, spending on health care reached $2.9 trillion in 2014, amounting to more than 17% of the US economy and more than $9110 per person.2 Between 2013 and 2014 alone, spending on health care increased 5.3%.2
Despite the resources spent on health care, much remains unknown about how much is spent for each condition, or how spending on these conditions differs across ages and time. Understanding how health care spending varies can help health system researchers and policy makers identify which conditions, age and sex groups, and types of care are driving spending increases. In particular, this information can be used to identify where new technologies and processes may yield a potential return on investment.
The objective of this study was to systematically and comprehensively estimate US spending on personal health care and public health, according to condition (ie, disease or health category), age and sex group, and type of care.
Methods
Conceptual Framework
This project received review and approval from the University of Washington institutional review board, and because data was used from a deidentified database, informed consent was waived. The strategy of this research was to use nationally representative data containing information about patient interactions with the health care system to estimate spending by condition, age and sex group, and type of health care. Data were scaled to reflect the official US government estimate of personal health care spending for each type of care for each year of the study. These official estimates, reported in the National Health Expenditure Accounts (NHEA), disaggregate total health spending into personal health spending, government public health activities, investment, and 2 administrative cost categories associated with public health insurance such as Medicare and Medicaid. Personal health spending, which composed 89.5% of total health spending in 2013, was the focus of this study and was defined in the NHEA as “the total amount spent to treat individuals with specific medical conditions.”3 In addition to estimating personal health care spending, this study also made preliminary estimates disaggregating federally funded public health spending.
The NHEA divided total personal health care spending into 10 mutually exclusive types of care, which included hospital care, physician and clinical services, nursing facility care, and prescribed retail pharmaceutical spending, among others. These types of care are not routinely ascribed to specific health conditions.2 To better align the NHEA personal health spending accounts with health system encounter data, spending fractions from the Medical Expenditure Panel Survey4 and methods described by Roehrig5 were used to group these 10 categories into 6 types of personal health care: inpatient care, ambulatory care, emergency department care, nursing facility care, and dental care, along with spending on prescribed retail pharmaceuticals. Ambulatory care included health care in urgent care facilities, and prescribed retail pharmaceuticals only included prescribed medicine that was purchased in a retail setting, rather than that provided during an inpatient or ambulatory care visit. Spending on physicians was included in inpatient, ambulatory, emergency department care, and nursing facility care, depending on the type of care provided. Together, health care spending incurred in these 6 types of care constituted between 84.0% and 85.2% of annual personal health care spending from 1996 through 2013.2 Across all 18 years of this study, personal health care spending that fell outside of the 6 types of care tracked was on over-the-counter pharmaceuticals (6.6%), nondurable and durable medical devices (5.1%), and home health (3.6%). A detailed Supplement provides additional information about all the methods used for this analysis.
Spending on the 6 types of personal health care was then disaggregated across 155 mutually exclusive and collectively exhaustive conditions and 38 age and sex groups. Each sex was divided into 19 5-year age groups, with the exception of the group aged 0 to 4 years, which was split into 2 categories (<1 year and 1–4 years) for more granular analysis. Of the 155 conditions, 140 were based on the disease categories used in the Global Burden of Disease (GBD) 2013 study.6 The remaining 15 conditions were associated with substantial health care spending but were not underlying conditions of health burden, and were thus excluded from the GBD or included as a part of other underlying conditions. Examples of these additional categories include well visits, routine dental visits, pregnancy and postpartum care, septicemia, renal failure, and treatment of 4 major risk factors—hypertension, hyperlipidemia, obesity, and tobacco use. For these 4 risk factors, spending on the treatment of the risk factor was reported separately, whereas spending on the treatment of diseases the risk factor may have caused were allocated to the actual disease. For example, spending on statins for hyperlipidemia was considered spending on the treatment of each risk factor, and spending on treatment of ischemic heart disease (IHD) reported spending for the treatment of the disease. Spending on these 4 risk factors was reported separately because of the large amount of spending associated with these risk factors and the ability to estimate this spending in the underlying health system encounter data. Spending on treatment of other risk factors, such as dietary risks or high fasting glucose, was allocated to the conditions resulting from these risks. All 155 conditions of health care spending and the major spending in each category is shown in eTables 8.1, 9.1, and 10.1 of the Supplement. More information about the framework of this study is included in section 1 of the Supplement.
Data
For the 6 types of personal health care tracked in this study, encounter-level microdata were used to determine the amount of resources spent on each condition and age and sex group for each year. An encounter was defined as an interaction with the medical system, such as an inpatient or nursing care facility admission; an emergency department, dental, or ambulatory care visit; or the purchase of a prescribed pharmaceutical.7 Health care spending, patient age and sex, type of care, and patient diagnoses were extracted from insurance claims, facility surveys, and household surveys. In addition, sample weights were used to make the studies nationally representative. Table 1 reports all microdata sources used for this study. Together, these sources included more than 163 million health system encounters.
Table 1.
Health System Encounter and Claims Data Sources Used to Disaggregate Spending by Condition, Age and Sex Groups, and Type of Care
| Microdata Source | Years | Observations | Metrica | Mean Patient-Weighted Metricb |
|---|---|---|---|---|
| Ambulatory Care | ||||
| MEPS | 1996–2013 | 2 680 505 | Spending ($US billions) | 302.68 |
| Visits (thousands) | 1 601 515.67 | |||
| NAMCS/NHAMCS | 1996–2011 | 955 958 | Visits (thousands) | 98 469.18 |
| MarketScanc | 2000, 2010, 2012 | 1 134 628 128 | Treated prevalence | NA |
| Inpatient Care | ||||
| NIS | 1996–2012 | 128 223 548 | Spending ($US billions) | 781.50 |
| Bed days (thousands) | 167 161.94 | |||
| MarketScanc | 2000, 2010, 2012 | 65 679 028 | Treated prevalence | NA |
| Emergency Department Care | ||||
| MEPS | 1996–2013 | 89 462 | Spending ($US billions) | 30.47 |
| Visits (thousands) | 45 457.97 | |||
| NHAMCS | 1996–2011 | 464 279 | Visits (thousands) | 82 089.07 |
| MarketScanc | 2000, 2010, 2012 | 77 566 041 | Treated prevalence | NA |
| Nursing Facility Care | ||||
| Medicare Claims Datad | 1999–2001, 2002, 2004, 2006, 2008, 2010, 2012 | 25 449 729 | Spending ($US billions) | 30.44 |
| Bed days (thousands) | 68 451.04 | |||
| NNHS | 1997, 1999, 2004 | 23 428 | Spending ($US billions) | 50.50 |
| Bed days (thousands) | 403 564.31 | |||
| MarketScanc | 2000, 2010, 2012 | 7 735 120 | Treated prevalence | NA |
| MCBS | 1999–2011 | 12 608 021 | ||
| Dental Care | ||||
| MEPS | 1996–2013 | 488 922 | Spending ($US billions) | 69.46 |
| Visits (thousands) | 278 481.55 | |||
| Prescribed Retail Pharmaceuticals | ||||
| MEPS | 1996–2013 | 4 908 359 | Spending ($US billions) | 189.37 |
| Visits (thousands) | 2 748 649.75 | |||
Abbreviations: MCBS, Medicare Current Beneficiaries Survey; MEPS, Medical Expenditure Panel Survey; NA, not applicable; NAMCS, National Ambulatory Medical Care Survey; NHAMCS, National Hospital Ambulatory Medical Care Survey; NIS, National Inpatient Sample; NNHS, National Nursing Home Survey.
Metric indicates what each data source was used to estimate or model.
Mean patient-weighted metric is the average across time for the measurement of each metric. This measurement was adjusted to be nationally representative using the provided survey patient-weights.
MarketScan was developed by Truven Health Analytics.
Medicare Claims Data refers to the Limited Data Set from the Center for Medicare & Medicaid Services.
The Medical Expenditure Panel Survey began in 1996.4 The Medical Expenditure Panel Survey was used as an input into the ambulatory, dental, emergency department, and prescribed retail pharmaceutical spending estimates. Because of the importance of the Medical Expenditure Panel Survey to this analysis, this study made annual estimates extending back to 1996 but not before. More information about the data sources used for this study is included in section 2 of the Supplement.
Identifying the Condition of Health Care Spending
In these microdata, households, physicians, or health system administrators reported a primary diagnosis using International Classification of Diseases, Ninth Revision (ICD-9) coding. In the rare case that the primary diagnosis was not identified and more than 1 diagnosis was reported, the diagnosis listed first was assumed the primary diagnosis unless an injury diagnosis was included. With the exception of injuries occurring within a medical facility, injury codes, such as “fall” and “street or highway accident,” were prioritized over other diagnoses. This was done because many data sources report injuries separately from other diagnoses and it was unclear which diagnosis was the primary.
ICD-9 diagnoses were grouped to form 155 conditions using methods described in the GBD study.6 ICD-9 diagnoses related to the nature of an injury (rather than the condition) or diagnoses providing imprecise information, such as “certain early complications of trauma” and “care involving use of rehabilitation procedures,” were proportionally redistributed to 1 of the 155 condition categories using methods developed for the GBD.6,8 More information about how encounters were stratified by condition is included in section 3 of the Supplement.
Estimating Spending
Spending on encounters with the same primary diagnosis, age and sex group, year, and type of health care were aggregated. Sampling weights were used to ensure that the estimates remained nationally representative.
On average, comorbidities make health care more complicated and more expensive.9–11 Attributing all of the resources used in a health care encounter to the primary diagnosis biases the estimates.7 To account for the presence of comorbidities, a previously developed regression-based method was used to adjust health care spending. As a consequence, conditions that are often accompanied by costly comorbidities decreased after comorbidity adjustment, whereas conditions often considered comorbidities increased after adjustment. Thus, the adjusted spending estimates reflect the spending attributed to each condition, rather than the spending attributed to primary diagnoses. More information about adjusting the spending estimates for the presence of comorbidities is included in section 5 of the Supplement.
The spending estimates for each type of care were scaled to reflect the adjusted annual health care spending reported by the NHEA. This procedure is common, as no single data source offers a census of spending in all health care settings.12,13 This scaling procedure assumed that the spending captured in data used for this study was representative of spending in the total population. Spending was adjusted for inflation before any modeling, and all estimates are reported in 2015 US dollars. More information about scaling these estimates to reflect the NHEA type of care total is included in section 5 of the Supplement.
Addressing Data Nonrepresentativeness
Several data limitations made additional adjustments necessary. First, health care charges, rather than spending, were reported in the National Inpatient Sample, which was used to measure inpatient care spending.14 Because actual spending is generally a fraction of the charge, charge data were adjusted to reflect actual spending using a previously developed regression-based adjustment.15 This adjustment was stratified by condition, primary payer, and year because the average amount paid per $1 charged varied systematically across these dimensions. This adjustment allowed high-quality inpatient charge data to be used and is described in section 5 of the Supplement.
Second, to address concerns related to small sample sizes and undersampled rare conditions, a Bayesian hierarchical model was applied. For all types of care except prescribed retail pharmaceuticals and emergency department care, 2 or 3 data sources were combined to generate spending estimates with complete time and age trends, and to leverage the strength of each data source. A large number of models were considered for this process. The final model was selected because of its flexibility, responsiveness to patterns in the raw data, and ability to combine disparate data to produce a single estimate. The model was employed independently for each condition, sex, and type of care combination. More information about this modeling is included in section 4 of the Supplement.
The third adjustment addressed the fact that ambulatory and inpatient care data sources used for this study underestimate spending at specialty mental health and substance abuse facilities.4,14 To address this problem, spending on these types of care was split into portions that reflect mental health spending and substance abuse spending, and spending was scaled to an appropriate total reported by the US Substance Abuse and Mental Health Services Administration.16 This adjustment ensured that the total spending on mental health and substance abuse in these settings was commensurate with official US records. More information about this adjustment is included in section 5 of the Supplement.
Fourth, nursing facility care data were adjusted to account for differences in short-term and long-term stays. US Medicare reimburses nursing facilities for up to 100 days of care after a qualifying hospital event. To incorporate the best data available, Medicare data were used to measure spending for these short-term nursing facility stays, and 2 other sources of nationally representative data were used to estimate spending for nursing facility stays longer than 100 days.17–19 Spending on short-term and long-term nursing facility stays were added together and formed the total amount of spending in nursing facility care. This adjustment ensured the best data available were used to measure spending in nursing facilities, and ensured that disparate patterns of health care spending in short-term and long-term nursing facility care were considered. More information about this adjustment is included in section 5 of the Supplement.
Quantifying Uncertainty for Personal Health Care Spending
For all types of care, uncertainty intervals (UIs) were calculated by bootstrapping the underlying encounter-level data 1000 times. The entire estimation process was completed for each bootstrap sample independently, and 1000 estimates were generated for each condition, age and sex group, year, and type of care. The estimates reported in this article are the mean of these 1000 estimates. A UI was constructed using the 2.5th and 97.5th percentiles. Bootstrapping methods assume that the empirical distribution of errors in the sample data approximates the population’s distribution. This may not be true for our most disaggregated estimates. Furthermore, bootstrapping methods capture only some types of uncertainty and do not reflect the uncertainty associated with some modeling and process decisions. Because of these limitations, the reported UIs should not be considered precise. Furthermore, the UIs have not been derived analytically or been calibrated to reflect a specific degree of uncertainty. The UIs are included to reflect relative uncertainty across the disparate set of measurements. More information about generating UIs for personal health spending estimates is included in section 6 of the Supplement.
Estimating Federal Public Health Care Spending
In addition to the 6 types of personal health care spending, this study also generated preliminary estimates disaggregating federally funded public health spending by condition, age and sex group, and year from 1996 through 2013. Encounter-level data did not exist for public health spending. Instead, federal public health program budget data were extracted from the 4 primary federal agencies providing public health funding: the Health Resources and Services Administration, the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and the US Food and Drug Administration. For each of these agencies, individual programs were mapped to the associated conditions. Spending estimates were extracted from audited appropriations reports. A series of linear regressions was used to fill in program spending when not available. Population estimates and program-specific information were used to disaggregate program spending across age and sex groups. Because the NHEA does not include resources transferred to state and local public health offices in its estimate of federal public health spending, disaggregated public health spending estimates were not scaled. More information about how public health spending was estimated is included in section 7 of the Supplement. All data manipulation and statistical analyses were completed using Stata (StataCorp), version 13.1; R (R Foundation), version 3.3.1; Python (Python Software Foundation), version 3.5.1; and PyMC2,20 version 2.3.6.21,22
Results
Conditions Leading to the Most Personal Health Care Spending in 2013
Among the aggregated condition categories (Table 2), cardiovascular disease, which includes IHD and cerebrovascular disease but excludes spending on the treatment of hyperlipidemia and hypertension, was the largest category of spending, with an estimated $231.1 billion (UI, $218.5 billion–$240.7 billion) spent in 2013. Of this spending, 57.3% (UI, 52.6%–60.9%) was in an inpatient setting, whereas 65.2% (UI, 61.3%–68.2%) was for patients 65 years and older. Diabetes, urogenital, blood, and endocrine diseases made up the second-largest category with an estimated $224.5 billion (UI, $216.4 billion–$233.5 billion), and the spending was spread relatively evenly across ambulatory care, prescribed retail pharmaceuticals, and inpatient care. Of the aggregated conditions, spending on the risk factors (the treatment of hypertension, hyperlipidemia, and obesity, and tobacco cessation) and musculoskeletal disorders were estimated to increase the fastest, with estimated rates of 6.6% (UI, 5.9%–7.3%) and 5.4% (UI, 4.7%–6.0%), respectively.
Table 2.
Personal Health Care Spending in the United States by Aggregated Condition Category for 2013a
| Rankb | Aggregated Condition Category | 2013 Spending (Billions of Dollars), $ | Annualized Rate of Change, 1996–2013, % | 2013 Spending by Type of Care, %
|
2013 Spending by Age, %
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ambulatory Care | Inpatient Care | Pharmaceuticals | Emergency Care | Nursing Facility Care | <20 Years | ≥65 Years | ||||
| 1 | Cardiovascular diseases | 231.1 | 1.2 | 18.4 | 57.3 | 6.2 | 2.7 | 15.3 | 0.9 | 65.2 |
|
| ||||||||||
| 2 | Diabetes, urogenital, blood, and endocrine diseases | 224.5 | 5.1 | 31.5 | 23.0 | 31.0 | 4.2 | 10.3 | 3.5 | 42.6 |
|
| ||||||||||
| 3 | Other noncommunicable diseases | 191.7 | 3.1 | 43.0 | 11.3 | 6.5 | 2.8 | 3.2 | 15.3 | 32.9 |
|
| ||||||||||
| 4 | Mental and substance abuse disorders | 187.8 | 3.7 | 52.1 | 19.0 | 20.9 | 1.6 | 6.5 | 19.8 | 12.8 |
|
| ||||||||||
| 5 | Musculoskeletal disorders | 183.5 | 5.4 | 47.7 | 37.0 | 6.2 | 3.3 | 5.9 | 1.9 | 40.0 |
|
| ||||||||||
| 6 | Injuries | 168.0 | 3.3 | 34.5 | 33.7 | 0.7 | 25.1 | 6.1 | 14.1 | 27.5 |
|
| ||||||||||
| 7 | Communicable, maternal, neonatal, and nutritional disorders | 164.9 | 3.7 | 21.7 | 58.1 | 2.1 | 6.2 | 11.8 | 23.8 | 36.6 |
|
| ||||||||||
| 8 | Well care | 155.5 | 2.9 | 28.7 | 36.5 | 3.0 | 0.5 | 0.1 | 37.7 | 5.1 |
|
| ||||||||||
| 9 | Treatment of risk factors | 140.8 | 6.6 | 35.6 | 3.5 | 53.6 | 1.1 | 6.2 | 0.6 | 50.0 |
|
| ||||||||||
| 10 | Chronic respiratory diseases | 132.1 | 3.7 | 31.1 | 26.7 | 28.4 | 4.7 | 9.0 | 14.5 | 39.0 |
|
| ||||||||||
| 11 | Neoplasms | 115.4 | 2.5 | 42.0 | 51.2 | 1.0 | 1.2 | 4.6 | 3.0 | 46.3 |
|
| ||||||||||
| 12 | Neurological disorders | 101.3 | 4.0 | 26.3 | 15.0 | 12.3 | 3.5 | 43.0 | 2.4 | 58.8 |
|
| ||||||||||
| 13 | Digestive diseases | 99.4 | 2.9 | 20.6 | 60.8 | 5.5 | 6.4 | 6.7 | 6.0 | 39.3 |
|
| ||||||||||
| 14 | Cirrhosis | 4.2 | 5.1 | 7.8 | 88.5 | 0.0 | 0.0 | 3.6 | 1.3 | 19.6 |
|
| ||||||||||
| All conditions | 2100.1 | 3.5 | 33.6 | 33.2 | 13.7 | 4.9 | 9.3 | 11.1 | 37.9 | |
Reported in 2015 US dollars. Uncertainty intervals are reported in the Supplement.
Ranked from highest spending to lowest spending.
In 2013, among all 155 conditions, the 20 top conditions accounted for an estimated 57.6% (UI, 56.9%–58.3%) of personal health care spending, which totaled $1.2 trillion (Table 3). More resources were estimated to be spent on diabetes than any other condition, with an estimated $101.4 billion (UI, $96.7 billion–$106.5 billion) spent in 2013. Prescribed retail pharmaceutical spending accounted for an estimated 57.6% (UI, 53.8%–62.1%) of total diabetes health care spending, whereas an estimated 87.1% (UI, 83.0%–91.6%) of spending on diabetes was incurred by those 45 years and older. IHD was estimated to account for the second-highest amount of health care spending, at $88.1 billion (UI, $82.7 billion–$92.9 billion). Most IHD spending occurred in inpatient care settings (56.5% [UI, 51.7%–60.6%]) and was accounted for by those 65 years or older (61.2% [UI, 57.0%–64.8%]). Spending on IHD excludes spending on the treatment of hypertension and hyperlipidemia, both of which contribute to IHD and for which treatment often requires substantial spending on prescribed retail pharmaceuticals. Spending on the treatment of these 2 risk factors in 2013 was estimated to be $83.9 billion (UI, $80.2 billion–$88.8 billion) and $51.8 billion (UI, $48.9 billion–$54.6 billion), respectively. Low back and neck pain was estimated to be the third-largest condition of health care spending, at $87.6 billion (UI, $67.5 billion–$94.1 billion), with the majority of this spending (60.5% [UI, 49.3%–63.8%]) in ambulatory care. Because cancer was disaggregated into 29 conditions, none were among the top 20 conditions with the highest spending. Estimates reported in this article can be interactively explored at http://vizhub.healthdata.org/dex/ (Interactive).
Table 3.
Personal Health Care Spending in the United States by Condition for 2013
| Ranka | Condition | Assigned Aggregated Condition Category |
2013 Spending (Billions of Dollars), $ |
Annualized Rate of Change, 1996–2013, % |
2013 Spending by Type of Care, %
|
2013 Spending by Age, %
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ambulatory Care |
Inpatient Care |
Pharmaceuticals | Emergency Care |
Nursing Facility Care |
<20 Years | ≥65 Years | |||||
| All conditions | 2100.1 | 3.5 | 33.6 | 33.2 | 13.7 | 4.9 | 9.3 | 11.1 | 37.9 | ||
|
| |||||||||||
| 1 | Diabetes mellitus | Diabetes, urogenital, blood, and endocrine diseases | 101.4 | 6.1 | 23.5 | 9.5 | 57.6 | 0.4 | 9.1 | 1.7 | 42.8 |
|
| |||||||||||
| 2 | Ischemic heart disease | Cardiovascular diseases | 88.1 | 0.2 | 23.9 | 56.5 | 11.3 | 0.9 | 7.3 | 0.2 | 61.2 |
|
| |||||||||||
| 3 | Low back and neck pain | Musculoskeletal disorders | 87.6 | 6.5 | 60.5 | 28.8 | 4.1 | 4.2 | 2.5 | 2.0 | 28.8 |
|
| |||||||||||
| 4 | Treatment of hypertension | Treatment of risk factors | 83.9 | 5.1 | 45.8 | 1.3 | 41.2 | 1.8 | 9.9 | 0.7 | 53.4 |
|
| |||||||||||
| 5 | Falls | Injuries | 76.3 | 3.0 | 29.7 | 34.3 | 0.6 | 22.7 | 12.7 | 10.3 | 48.2 |
|
| |||||||||||
| 6 | Depressive disorders | Mental and substance abuse disorders | 71.1 | 3.4 | 53.1 | 11.6 | 32.1 | 0.5 | 2.8 | 7.1 | 13.3 |
|
| |||||||||||
| 7 | Oral disordersb | Other noncommunicable diseases | 66.4 | 2.9 | 1.0 | 1.5 | 0.4 | 1.2 | 0.1 | 13.1 | 20.7 |
|
| |||||||||||
| 8 | Sense organ diseasesc | Other noncommunicable diseases | 59.0 | 2.8 | 85.4 | 2.3 | 8.6 | 2.1 | 1.6 | 9.0 | 54.0 |
|
| |||||||||||
| 9 | Skin and subcutaneous diseasesd | Other noncommunicable diseases | 55.7 | 3.5 | 52.0 | 20.7 | 12.6 | 6.0 | 8.6 | 14.4 | 29.8 |
|
| |||||||||||
| 10 | Pregnancy and postpartum caree | Well care | 55.6 | 2.9 | 47.6 | 50.5 | 0.6 | 1.3 | 0.0 | 6.4 | 0.0 |
|
| |||||||||||
| 11 | Urinary diseases and male infertilityf | Diabetes, urogenital, blood, and endocrine diseases | 54.9 | 4.8 | 37.0 | 21.9 | 9.5 | 13.4 | 18.3 | 4.5 | 51.1 |
|
| |||||||||||
| 12 | COPD (chronic bronchitis, emphysema) | Chronic respiratory diseases | 53.8 | 2.5 | 19.2 | 34.8 | 18.9 | 6.1 | 21.1 | 3.5 | 64.5 |
|
| |||||||||||
| 13 | Treatment of hyperlipidemia | Treatment of risk factors | 51.8 | 10.3 | 20.9 | 0 | 78.5 | 0 | 0.6 | 0.4 | 48.8 |
|
| |||||||||||
| 14 | Well dental (general examination and cleaning, x-rays, orthodontia) | Well care | 48.7 | 2.7 | 0 | 0 | 0 | 0 | 0 | 37.4 | 12.8 |
|
| |||||||||||
| 15 | Osteoarthritis | Musculoskeletal disorders | 47.9 | 5.9 | 23.5 | 63.8 | 5.8 | 0.1 | 6.9 | 0 | 60.1 |
|
| |||||||||||
| 16 | Other musculoskeletal disordersg | Musculoskeletal disorders | 44.9 | 3.8 | 49.4 | 25.4 | 9.2 | 5.0 | 11.0 | 3.7 | 40.6 |
|
| |||||||||||
| 17 | Cerebrovascular disease | Cardiovascular diseases | 43.8 | 1.1 | 5.2 | 54.0 | 2.6 | 1.4 | 36.7 | 2.3 | 70.8 |
|
| |||||||||||
| 18 | Other neurological disordersh | Neurological disorders | 43.7 | 7.3 | 50.9 | 12.1 | 15.8 | 5.2 | 16.0 | 2.5 | 38.4 |
|
| |||||||||||
| 19 | Other digestive diseasesi | Digestive diseases | 38.8 | 3.3 | 39.0 | 36.2 | 12.5 | 7.7 | 4.6 | 5.2 | 35.8 |
|
| |||||||||||
| 20 | Lower respiratory tract infections | Communicable, maternal, neonatal, and nutritional disorders | 37.1 | 3.1 | 12.5 | 48.6 | 1.5 | 6.3 | 31.1 | 16.6 | 56.0 |
|
| |||||||||||
| 21 | Alzheimer disease and other dementias | Neurological disorders | 36.7 | 1.9 | 1.9 | 5.1 | 4.5 | 0.2 | 88.4 | 0 | 97.4 |
|
| |||||||||||
| 22 | Other chronic respiratory diseasesj | Chronic respiratory diseases | 34.7 | 3.2 | 68.4 | 3.1 | 25.1 | 2.9 | 0.5 | 23.4 | 12.4 |
|
| |||||||||||
| 23 | Septicemia | Communicable, maternal, neonatal, and nutritional disorders | 33.9 | 8.9 | 0 | 96.1 | 0 | 0 | 3.9 | 2.0 | 64.9 |
|
| |||||||||||
| 24 | Asthma | Chronic respiratory diseases | 32.5 | 5.4 | 21.6 | 13.8 | 57.5 | 6.0 | 1.1 | 27.8 | 19.8 |
|
| |||||||||||
| 25 | Exposure to mechanical forcesk | Injuries | 30.0 | 3.5 | 47.2 | 7.3 | 1.0 | 44.3 | 0.2 | 26.2 | 6.9 |
|
| |||||||||||
| 26 | Anxiety disorders | Mental and substance abuse disorders | 29.7 | 5.0 | 71.4 | 3.9 | 19.7 | 2.5 | 2.6 | 11.3 | 8.4 |
|
| |||||||||||
| 27 | Heart failure | Cardiovascular diseases | 28.5 | 1.1 | 4.2 | 71.0 | 0.7 | 0.6 | 23.7 | 1.2 | 76.7 |
|
| |||||||||||
| 28 | Well newborn | Well care | 27.9 | 3.8 | 0 | 100.0 | 0 | 0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 29 | Atrial fibrillation and flutter | Cardiovascular diseases | 27.7 | 4.6 | 32.3 | 41.0 | 5.9 | 11.2 | 9.6 | 0 | 67.3 |
|
| |||||||||||
| 30 | Other cardiovascular and circulatory diseasesl | Cardiovascular diseases | 26.0 | 2.4 | 24.6 | 62.4 | 4.4 | 1.3 | 7.3 | 1.1 | 60.6 |
|
| |||||||||||
| 31 | Other unintentional injuries (overexertion, other accidents) | Injuries | 25.6 | 5.8 | 65.6 | 14.7 | 0.9 | 18.5 | 0.4 | 8.6 | 11.2 |
|
| |||||||||||
| 32 | Attention-deficit/hyperactivity disorder | Mental and substance abuse disorders | 23.2 | 5.9 | 62.6 | 0.6 | 36.8 | 0 | 0 | 88.7 | 0.6 |
|
| |||||||||||
| 33 | Road injuries (auto, cycle, motorcycle, and pedestrian) | Injuries | 20.0 | 2.1 | 12.6 | 67.3 | 0.2 | 18.0 | 1.8 | 15.2 | 13.8 |
|
| |||||||||||
| 34 | Gynecological diseasesm | Diabetes, urogenital, blood, and endocrine diseases | 19.8 | 1.4 | 68.3 | 19.6 | 4.0 | 7.0 | 1.1 | 2.9 | 8.8 |
|
| |||||||||||
| 35 | Endocrine, metabolic, blood, and immune disordersn | Diabetes, urogenital, blood, and endocrine diseases | 19.6 | 5.4 | 36.1 | 33.1 | 24.4 | 1.0 | 5.4 | 9.6 | 35.3 |
|
| |||||||||||
| 36 | Colon and rectum cancers | Neoplasms | 18.5 | 2.0 | 41.7 | 52.0 | 0.7 | 0.6 | 5.0 | 0.4 | 54.5 |
|
| |||||||||||
| 37 | Schizophrenia | Mental and substance abuse disorders | 17.6 | 2.0 | 10.1 | 54.3 | 1.6 | 0.5 | 33.6 | 1.6 | 30.6 |
|
| |||||||||||
| 38 | Well person | Well care | 15.4 | 1.7 | 98.0 | 0 | 2.0 | 0 | 0 | 55.5 | 9.0 |
|
| |||||||||||
| 39 | Gallbladder and biliary diseases | Digestive diseases | 15.2 | 2.7 | 20.6 | 71.9 | 0.1 | 4.2 | 3.2 | 2.4 | 36.0 |
|
| |||||||||||
| 40 | Upper respiratory tract infections | Communicable, maternal, neonatal, and nutritional disorders | 14.7 | 1.3 | 69.2 | 5.1 | 3.3 | 19.6 | 2.8 | 57.1 | 6.0 |
|
| |||||||||||
| 41 | Chronic kidney diseases | Diabetes, urogenital, blood, and endocrine diseases | 13.5 | 4.0 | 18.1 | 68.0 | 3.3 | 0 | 10.7 | 2.0 | 52.5 |
|
| |||||||||||
| 42 | Drug use disorderso | Mental and substance abuse disorders | 13.5 | 3.1 | 56.4 | 32.6 | 0.3 | 2.7 | 8.0 | 5.0 | 19.7 |
|
| |||||||||||
| 43 | Bipolar disorder | Mental and substance abuse disorders | 13.1 | 4.0 | 29.6 | 60.7 | 5.7 | 0.1 | 3.9 | 13.6 | 9.0 |
|
| |||||||||||
| 44 | Trachea, bronchus, and lung cancers | Neoplasms | 13.1 | 2.0 | 48.6 | 46.0 | 0.9 | 0.5 | 4.1 | 0.4 | 54.5 |
|
| |||||||||||
| 45 | Acute renal failure | Diabetes, urogenital, blood, and endocrine diseases | 12.7 | 8.0 | 27.0 | 63.8 | 0.4 | 0 | 8.8 | 3.7 | 62.1 |
|
| |||||||||||
| 46 | Breast cancer | Neoplasms | 12.1 | 1.0 | 71.1 | 23.5 | 2.7 | 0 | 2.7 | 0.2 | 30.5 |
|
| |||||||||||
| 47 | Other infectious diseasesp | Communicable, maternal, neonatal, and nutritional disorders | 12.1 | 2.8 | 52.5 | 13.0 | 6.6 | 14.0 | 13.9 | 48.4 | 16.1 |
|
| |||||||||||
| 48 | Other neoplasms | Neoplasms | 11.6 | 5.5 | 28.9 | 69.0 | 0.4 | 0 | 1.8 | 11.5 | 35.9 |
|
| |||||||||||
| 49 | Interstitial lung disease and pulmonary sarcoidosis | Chronic respiratory diseases | 10.9 | 9.2 | 0 | 99.2 | 0 | 0 | 0.8 | 0.8 | 55.3 |
|
| |||||||||||
| 50 | Congenital anomalies | Other noncommunicable diseases | 10.7 | 4.4 | 23.6 | 72.6 | 0.1 | 0 | 3.6 | 69.6 | 8.4 |
|
| |||||||||||
| 51 | Aortic aneurysm | Cardiovascular diseases | 9.5 | 3.0 | 17.2 | 60.9 | 3.0 | 12.4 | 6.5 | 1.5 | 54.5 |
|
| |||||||||||
| 52 | Pancreatitis | Digestive diseases | 9.5 | 1.9 | 0.4 | 78.4 | 0.6 | 3.3 | 17.3 | 4.3 | 48.7 |
|
| |||||||||||
| 53 | Alcohol use disorders (alcohol dependence and harmful use) | Mental and substance abuse disorders | 9.3 | 2.0 | 43.3 | 38.6 | 0 | 14.0 | 4.2 | 2.6 | 7.9 |
|
| |||||||||||
| 54 | Diarrheal diseases | Communicable, maternal, neonatal, and nutritional disorders | 9.2 | 4.1 | 24.2 | 50.5 | 4.3 | 11.4 | 9.6 | 18.9 | 44.8 |
|
| |||||||||||
| 55 | Otitis media | Communicable, maternal, neonatal, and nutritional disorders | 8.8 | −0.1 | 82.6 | 1.4 | 5.9 | 10.1 | 0.1 | 83.2 | 2.3 |
|
| |||||||||||
| 56 | Nonmelanoma skin cancer | Neoplasms | 8.2 | 7.1 | 96.8 | 2.5 | 0.3 | 0 | 0.5 | 0 | 73.6 |
|
| |||||||||||
| 57 | Paralytic ileus and intestinal obstruction | Digestive diseases | 8.0 | 3.3 | 0.4 | 91.9 | 0 | 0 | 7.6 | 3.3 | 60.0 |
|
| |||||||||||
| 58 | Appendicitis | Digestive diseases | 7.8 | 3.4 | 0.3 | 95.6 | 0 | 0 | 4.1 | 19.8 | 20.0 |
|
| |||||||||||
| 59 | Migraine | Neurological disorders | 7.3 | 5.1 | 35.0 | 9.9 | 39.3 | 15.8 | 0 | 4.8 | 2.9 |
|
| |||||||||||
| 60 | Inflammatory bowel disease | Digestive diseases | 6.8 | 3.3 | 17.9 | 53.8 | 5.5 | 16.3 | 6.5 | 13.3 | 26.7 |
|
| |||||||||||
| 61 | Peptic ulcer disease | Digestive diseases | 6.7 | 1.7 | 2.7 | 74.3 | 0.4 | 8.9 | 13.7 | 2.0 | 55.6 |
|
| |||||||||||
| 62 | Iron-deficiency anemia | Communicable, maternal, neonatal, and nutritional disorders | 6.5 | 8.1 | 28.4 | 46.3 | 1.9 | 0.3 | 23.1 | 2.4 | 67.0 |
|
| |||||||||||
| 63 | Peripartum death due to complications of a preexisting medical condition | Communicable, maternal, neonatal, and nutritional disorders | 6.4 | 6.8 | 8.1 | 87.7 | 0.4 | 3.8 | 0 | 10.0 | 0 |
|
| |||||||||||
| 64 | Brain and nervous system cancers | Neoplasms | 5.7 | 3.2 | 24.4 | 65.4 | 1.7 | 0 | 8.5 | 9.6 | 26.9 |
|
| |||||||||||
| 65 | Uterine cancer | Neoplasms | 5.6 | 1.2 | 25.1 | 71.6 | 0.6 | 1.3 | 1.4 | 0.2 | 16.2 |
|
| |||||||||||
| 66 | Prostate cancer | Neoplasms | 5.4 | 0.8 | 55.2 | 35.9 | 2.7 | 0.5 | 5.7 | 0.1 | 66.4 |
|
| |||||||||||
| 67 | Other maternal disorders (second-degree and third-degree vaginal tears) | Communicable, maternal, neonatal, and nutritional disorders | 5.2 | 0.7 | 4.7 | 92.4 | 0.2 | 2.7 | 0 | 9.3 | 0 |
|
| |||||||||||
| 68 | Interpersonal violence (rape and assault) | Injuries | 5.2 | 3.5 | 5.0 | 65.6 | 0.1 | 29.3 | 0.1 | 16.2 | 2.3 |
|
| |||||||||||
| 69 | Other mental and behavioral disorders (insomnia) | Mental and substance abuse disorders | 5.1 | 2.2 | 71.9 | 9.8 | 17.3 | 0 | 1.0 | 22.0 | 18.6 |
|
| |||||||||||
| 70 | Neglected tropical diseases and malariaq | Communicable, maternal, neonatal, and nutritional disorders | 5.1 | 9.9 | 1.0 | 88.7 | 0.5 | 0 | 9.8 | 4.9 | 42.2 |
|
| |||||||||||
| 71 | Family planning | Well care | 5.1 | 5.7 | 24.4 | 0.3 | 75.3 | 0 | 0 | 4.5 | 1.3 |
|
| |||||||||||
| 72 | Obesity (treatment of morbid obesity, including bariatric surgery) | Treatment of risk factors | 5.0 | 9.9 | 18.8 | 74.6 | 4.3 | 0 | 2.3 | 2.0 | 7.4 |
|
| |||||||||||
| 73 | Preterm birth complicationsr | Communicable, maternal, neonatal, and nutritional disorders | 4.9 | 3.1 | 6.0 | 93.8 | 0.1 | 0.2 | 0 | 100.0 | 0 |
|
| |||||||||||
| 74 | Parkinson disease | Neurological disorders | 4.9 | 0.3 | 6.8 | 37.3 | 5.4 | 0 | 50.5 | 0 | 84.1 |
|
| |||||||||||
| 75 | HIV/AIDS | Communicable, maternal, neonatal, and nutritional disorders | 4.8 | 2.4 | 12.6 | 74.4 | 6.8 | 0 | 6.2 | 2.8 | 13.1 |
|
| |||||||||||
| 76 | Multiple sclerosis | Neurological disorders | 4.4 | 2.0 | 11.0 | 46.1 | 13.1 | 0 | 29.8 | 2.8 | 40.8 |
|
| |||||||||||
| 77 | Epilepsy | Neurological disorders | 4.3 | 8.5 | 7.2 | 79.0 | 5.8 | 0.8 | 7.3 | 20.9 | 22.7 |
|
| |||||||||||
| 78 | Cirrhosis of the liver | Cirrhosis | 4.2 | 5.1 | 7.8 | 88.5 | 0 | 0 | 3.6 | 1.3 | 19.6 |
|
| |||||||||||
| 79 | Stomach cancer | Neoplasms | 3.9 | 2.3 | 20.6 | 60.9 | 0.2 | 0.2 | 18.1 | 0.3 | 69.7 |
|
| |||||||||||
| 80 | Leukemia | Neoplasms | 3.9 | 2.5 | 2.3 | 94.8 | 0 | 0 | 2.9 | 18.1 | 28.5 |
|
| |||||||||||
| 81 | Gastritis and duodenitis | Digestive diseases | 3.4 | 2.2 | 12.2 | 54.6 | 3.0 | 19.4 | 10.7 | 6.0 | 40.2 |
|
| |||||||||||
| 82 | Hypertensive disorders of pregnancy | Communicable, maternal, neonatal, and nutritional disorders | 3.0 | 6.4 | 1.2 | 98.8 | 0 | 0 | 0 | 9.1 | 0 |
|
| |||||||||||
| 83 | Kidney cancer | Neoplasms | 3.0 | 4.3 | 30.6 | 67.7 | 0.1 | 0 | 1.6 | 3.4 | 43.0 |
|
| |||||||||||
| 84 | Autistic spectrum disorders | Mental and substance abuse disorders | 3.0 | 17.6 | 95.6 | 2.1 | 2.4 | 0 | 0 | 97.3 | 0.2 |
|
| |||||||||||
| 85 | Non-Hodgkin lymphoma | Neoplasms | 2.9 | 2.2 | 20.1 | 76.5 | 0 | 0 | 3.5 | 2.8 | 52.9 |
|
| |||||||||||
| 86 | Self-harm | Injuries | 2.8 | 5.1 | 0 | 97.7 | 0 | 2.0 | 0.3 | 8.6 | 7.1 |
|
| |||||||||||
| 87 | Bladder cancer | Neoplasms | 2.8 | 2.7 | 50.7 | 45.6 | 0.1 | 0 | 3.5 | 0.1 | 74.0 |
|
| |||||||||||
| 88 | Pancreatic cancer | Neoplasms | 2.7 | 2.5 | 28.0 | 65.2 | 1.6 | 2.2 | 3.1 | 0.7 | 53.0 |
|
| |||||||||||
| 89 | Hemoglobinopathies and hemolytic anemias | Diabetes, urogenital, blood, and endocrine diseases | 2.6 | 4.3 | 1.2 | 97.3 | 0 | 0 | 1.6 | 19.9 | 19.4 |
|
| |||||||||||
| 90 | Peripheral vascular disease | Cardiovascular diseases | 2.5 | 1.8 | 38.0 | 37.1 | 1.2 | 0.3 | 23.4 | 0 | 68.3 |
|
| |||||||||||
| 91 | Liver cancer | Neoplasms | 2.4 | 6.1 | 6.6 | 61.1 | 3.5 | 12.5 | 16.3 | 12.2 | 48.3 |
|
| |||||||||||
| 92 | Rheumatoid arthritis | Musculoskeletal disorders | 2.4 | −0.7 | 33.6 | 21.2 | 29.3 | 0 | 15.9 | 2.8 | 38.3 |
|
| |||||||||||
| 93 | Counselling services (medical consultation) | Well care | 2.1 | 3.8 | 84.9 | 0.7 | 9.7 | 0 | 4.7 | 9.8 | 12.6 |
|
| |||||||||||
| 94 | Animal contact (snake and dog) | Injuries | 2.1 | 3.8 | 40.6 | 15.0 | 2.1 | 42.0 | 0.3 | 28.1 | 9.0 |
|
| |||||||||||
| 95 | Sexually transmitted diseases excluding HIV | Communicable, maternal, neonatal, and nutritional disorders | 2.1 | 0.9 | 8.2 | 72.4 | 0.9 | 7.3 | 11.2 | 6.8 | 30.6 |
|
| |||||||||||
| 96 | Cervical cancer | Neoplasms | 2.1 | −0.6 | 39.8 | 40.9 | 0.3 | 0.1 | 18.9 | 0.7 | 23.2 |
|
| |||||||||||
| 97 | Obstructed labor | Communicable, maternal, neonatal, and nutritional disorders | 2.1 | 3.9 | 0.2 | 93.2 | 0.1 | 0 | 6.5 | 3.6 | 43.3 |
|
| |||||||||||
| 98 | Complications of abortion (miscarriage included) | Communicable, maternal, neonatal, and nutritional disorders | 2.0 | 3.8 | 30.8 | 43.6 | 0.4 | 25.3 | 0 | 5.7 | 0 |
|
| |||||||||||
| 99 | Rheumatic heart disease | Cardiovascular diseases | 1.9 | 0.3 | 0 | 97.2 | 0 | 0 | 2.8 | 0.6 | 71.3 |
|
| |||||||||||
| 100 | Cardiomyopathy and myocarditis | Cardiovascular diseases | 1.8 | 2.9 | 4.1 | 89.1 | 0.6 | 0 | 6.2 | 5.2 | 29.3 |
|
| |||||||||||
| 101 | Inguinal or femoral hernia | Digestive diseases | 1.8 | 2.1 | 15.7 | 80.9 | 0 | 0 | 3.4 | 2.5 | 57.1 |
|
| |||||||||||
| 102 | Ovarian cancer | Neoplasms | 1.5 | 1.5 | 26.2 | 69.8 | 0.3 | 0 | 3.6 | 0.7 | 37.9 |
|
| |||||||||||
| 103 | Fire, heat, and hot substances (including burns) | Injuries | 1.4 | 0.2 | 3.7 | 83.7 | 0.1 | 9.9 | 2.7 | 22.0 | 19.8 |
|
| |||||||||||
| 104 | Collective violence and legal intervention | Injuries | 1.3 | 2.2 | 0 | 99.6 | 0 | 0.4 | 0 | 13.9 | 16.1 |
|
| |||||||||||
| 105 | Vascular intestinal disorders | Digestive diseases | 1.3 | 2.4 | 0 | 95.8 | 0 | 0 | 4.2 | 0.9 | 63.5 |
|
| |||||||||||
| 106 | Malignant skin melanoma | Neoplasms | 1.3 | 2.5 | 71.6 | 26.5 | 0.3 | 0.0 | 1.6 | 1.0 | 29.6 |
|
| |||||||||||
| 107 | Foreign body (eye and airway obstruction) | Injuries | 1.2 | 2.1 | 21.1 | 40.3 | 0.4 | 37.6 | 0.7 | 26.7 | 16.8 |
|
| |||||||||||
| 108 | Gallbladder and biliary tract cancer | Neoplasms | 1.2 | 1.6 | 25.9 | 67.0 | 1.4 | 3.3 | 2.5 | 0.5 | 59.7 |
|
| |||||||||||
| 109 | Mouth cancer | Neoplasms | 1.2 | 1.2 | 30.4 | 65.3 | 0.2 | 0 | 4.0 | 0.7 | 40.4 |
|
| |||||||||||
| 110 | Other pharynx cancer | Neoplasms | 1.2 | 3.8 | 28.1 | 24.5 | 1.6 | 44.0 | 1.8 | 5.0 | 20.6 |
|
| |||||||||||
| 111 | Maternal hemorrhage (antepartum and postpartum hemorrhage) | Communicable, maternal, neonatal, and nutritional disorders | 1.1 | 4.2 | 1.8 | 73.3 | 0 | 24.9 | 0.0 | 6.8 | 0 |
|
| |||||||||||
| 112 | Varicella | Communicable, maternal, neonatal, and nutritional disorders | 1.0 | 2.9 | 36.1 | 30.9 | 10.0 | 1.4 | 21.6 | 6.4 | 58.7 |
|
| |||||||||||
| 113 | Meningitis | Communicable, maternal, neonatal, and nutritional disorders | 0.9 | 0.8 | 2.2 | 95.1 | 0.1 | 0 | 2.5 | 24.9 | 20.0 |
|
| |||||||||||
| 114 | Multiple myeloma | Neoplasms | 0.9 | 2.9 | 0 | 94.9 | 0 | 0 | 5.1 | 0 | 45.3 |
|
| |||||||||||
| 115 | Other nutritional deficiencies | Communicable, maternal, neonatal, and nutritional disorders | 0.9 | 2.0 | 28.0 | 12.8 | 15.0 | 0 | 44.2 | 10.5 | 53.7 |
|
| |||||||||||
| 116 | Poisonings | Injuries | 0.9 | 2.7 | 0.5 | 84.1 | 0 | 9.7 | 5.7 | 12.2 | 34.5 |
|
| |||||||||||
| 117 | Eating disorders (anorexia, bulimia) | Mental and substance abuse disorders | 0.9 | 0.4 | 2.7 | 85.7 | 0.2 | 10.9 | 0.5 | 35.2 | 0 |
|
| |||||||||||
| 118 | Mesothelioma | Neoplasms | 0.9 | 2.9 | 11.2 | 74.8 | 0.2 | 0.9 | 12.9 | 0.6 | 54.1 |
|
| |||||||||||
| 119 | Conduct disorder | Mental and substance abuse disorders | 0.8 | 0.9 | 66.6 | 32.8 | 0.6 | 0 | 0 | 95.7 | 0 |
|
| |||||||||||
| 120 | Nasopharynx cancer | Neoplasms | 0.8 | 3.9 | 43.7 | 21.9 | 5.5 | 26.2 | 2.6 | 10.0 | 22.6 |
|
| |||||||||||
| 121 | Other transport injuriess | Injuries | 0.8 | 1.8 | 26.8 | 62.2 | 0.3 | 8.5 | 2.3 | 22.3 | 10.7 |
|
| |||||||||||
| 122 | Larynx cancer | Neoplasms | 0.8 | 1.5 | 20.1 | 71.1 | 0.1 | 0 | 8.6 | 0.5 | 52.1 |
|
| |||||||||||
| 123 | Gout | Musculoskeletal disorders | 0.7 | 4.3 | 25.2 | 27.1 | 27.7 | 12.3 | 7.7 | 0.9 | 43.6 |
|
| |||||||||||
| 124 | Donor (organ donation) | Well care | 0.7 | 9.6 | 0 | 99.9 | 0 | 0 | 0.1 | 2.9 | 1.5 |
|
| |||||||||||
| 125 | Idiopathic intellectual disability | Mental and substance abuse disorders | 0.7 | −1.2 | 2.5 | 0.6 | 0.6 | 0 | 96.4 | 8.0 | 52.2 |
|
| |||||||||||
| 126 | Esophageal cancer | Neoplasms | 0.7 | 1.3 | 0 | 91.5 | 0 | 2.6 | 5.9 | 0.9 | 51.3 |
|
| |||||||||||
| 127 | Endocarditis | Cardiovascular diseases | 0.6 | −0.4 | 0 | 89.4 | 0 | 0 | 10.7 | 2.8 | 40.9 |
|
| |||||||||||
| 128 | Thyroid cancer | Neoplasms | 0.6 | 3.1 | 15.9 | 81.1 | 0.9 | 0 | 2.2 | 1.2 | 36.1 |
|
| |||||||||||
| 129 | Hypertensive heart disease | Cardiovascular diseases | 0.5 | −5.8 | 0 | 89.0 | 0 | 0 | 11.0 | 0.1 | 65.3 |
|
| |||||||||||
| 130 | Other neonatal disorders (feeding problems, temperature regulation) | Communicable, maternal, neonatal, and nutritional disorders | 0.4 | 6.5 | 4.5 | 89.4 | 0.1 | 6.0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 131 | Protein-energy malnutrition (nutritional marasmus) | Communicable, maternal, neonatal, and nutritional disorders | 0.4 | 0.2 | 0 | 54.5 | 0 | 0 | 45.2 | 13.3 | 53.4 |
|
| |||||||||||
| 132 | Neonatal encephalopathy (birth asphyxia and birth trauma) | Communicable, maternal, neonatal, and nutritional disorders | 0.4 | 3.1 | 0.1 | 100.0 | 0 | 0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 133 | Hemolytic disease in fetus and newborn and other neonatal jaundicet | Communicable, maternal, neonatal, and nutritional disorders | 0.3 | 2.6 | 6.0 | 93.0 | 0 | 1.0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 134 | Encephalitis | Communicable, maternal, neonatal, and nutritional disorders | 0.3 | 6.3 | 0 | 94.7 | 0 | 0 | 5.3 | 14.7 | 26.1 |
|
| |||||||||||
| 135 | Tuberculosis | Communicable, maternal, neonatal, and nutritional disorders | 0.3 | −0.5 | 2.1 | 84.1 | 0 | 0 | 13.8 | 10.1 | 27.6 |
|
| |||||||||||
| 136 | Whooping cough | Communicable, maternal, neonatal, and nutritional disorders | 0.3 | 2.7 | 2.6 | 96.6 | 0.5 | 0 | 0.4 | 31.1 | 0 |
|
| |||||||||||
| 137 | Hepatitis | Communicable, maternal, neonatal, and nutritional disorders | 0.3 | 3.2 | 36.2 | 62.7 | 0 | 0 | 1.1 | 1.3 | 16.7 |
|
| |||||||||||
| 138 | Sepsis and other infectious disorders of the newborn baby | Communicable, maternal, neonatal, and nutritional disorders | 0.2 | 4.2 | 0 | 100.0 | 0 | 0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 139 | Hodgkin lymphoma | Neoplasms | 0.2 | 1.1 | 0 | 97.6 | 0 | 0 | 2.4 | 12.9 | 14.4 |
|
| |||||||||||
| 140 | Pneumoconiosis | Chronic respiratory diseases | 0.2 | 3.2 | 0 | 98.0 | 0 | 0 | 2.0 | 0.1 | 72.3 |
|
| |||||||||||
| 141 | Exposure to forces of natureu | Injuries | 0.2 | 5.3 | 0.3 | 96.3 | 0 | 1.3 | 2.1 | 4.8 | 39.4 |
|
| |||||||||||
| 142 | Drowning | Injuries | 0.1 | −0.3 | 10.9 | 85.6 | 0 | 3.5 | 0 | 28.9 | 45.3 |
|
| |||||||||||
| 143 | Iodine deficiency (iodine hypothyroidism) | Communicable, maternal, neonatal, and nutritional disorders | 0.1 | −0.8 | 0 | 11.3 | 16.2 | 0 | 72.5 | 14.6 | 51.8 |
|
| |||||||||||
| 144 | Tobacco (tobacco use disorder, cessation) | Treatment of risk factors | 0.1 | 5.3 | 12.1 | 85.3 | 0 | 0.1 | 2.5 | 3.7 | 18.5 |
|
| |||||||||||
| 145 | Maternal sepsis and other pregnancy related infectionv | Communicable, maternal, neonatal, and nutritional disorders | 0.1 | 4.4 | 0 | 99.9 | 0 | 0 | 0.1 | 14.0 | 0 |
|
| |||||||||||
| 146 | Tension-type headache | Neurological disorders | 0.1 | 5.4 | 25.8 | 73.5 | 0 | 0 | 0.7 | 3.6 | 17.8 |
|
| |||||||||||
| 147 | Testicular cancer | Neoplasms | 0.1 | 2.8 | 19.2 | 77.9 | 0 | 2.1 | 0.7 | 9.0 | 3.3 |
|
| |||||||||||
| 148 | Intestinal infectious diseasesw | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | 0.8 | 0 | 90.0 | 0 | 0 | 10.1 | 25.8 | 26.1 |
|
| |||||||||||
| 149 | Vitamin A deficiency | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | 14.7 | 0 | 100.0 | 0 | 0 | 0 | 100.0 | 0 |
|
| |||||||||||
| 150 | Social services (services for family members) | Well care | <0.1 | −0.2 | 75.0 | 16.4 | 0 | 0 | 8.6 | 11.8 | 30.7 |
|
| |||||||||||
| 151 | Diphtheria | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | −0.1 | 53.5 | 29.3 | 15.5 | 0 | 1.7 | 57.9 | 0 |
|
| |||||||||||
| 152 | Acute glomerulonephritis | Diabetes, urogenital, blood, and endocrine diseases | <0.1 | 1.8 | 0 | 93.5 | 0 | 0 | 6.5 | 30.5 | 36.0 |
|
| |||||||||||
| 153 | Measles | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | −1.6 | 1.5 | 90.0 | 2.7 | 0 | 5.8 | 5.2 | 0 |
|
| |||||||||||
| 154 | Leprosy | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | 1.0 | 0 | 3.6 | 1.2 | 0 | 95.2 | 1.4 | 91.3 |
|
| |||||||||||
| 155 | Tetanus | Communicable, maternal, neonatal, and nutritional disorders | <0.1 | −1.3 | 0 | 82.5 | 0 | 0 | 17.5 | 36.4 | 20.3 |
Abbreviations: COPD, chronic obstructive pulmonary disease.
Ranked from largest spending to smallest spending. Reported in 2015 US dollars. eTables 9.1 and 9.2 in the Supplement include all conditions, all types of care, and uncertainty intervals for all estimates.
Oral surgery and dental caries, including fillings, crowns, extraction, and dentures.
Cataracts, vision correction, adult hearing loss, and macular degeneration.
Cellulitis, sebaceous cyst, acne, and eczema.
Normal pregnancy, including cesarean delivery.
Urinary tract infection and cyst of kidney.
Disorders of joints, muscular, and connective tissue.
Pain syndromes and muscular dystrophy.
Diseases of the esophagus and diverticulitis of the colon.
Sleep apnea, allergic rhinitis, and chronic sinusitis.
Falling object, striking other object, cuts, and being crushed.
Paroxysmal tachycardia, and unspecified dysrhythmias.
Menopausal and postmenopausal disorders and endometriosis.
Other diseases of thyroid and von Willebrand disease.
Cocaine, opioid, and amphetamines and cannabis dependence.
Viral and chlamydial infection and streptococcal infection.
Lyme disease, rabies, cysticercosis, and dengue.
Respiratory distress and extreme neonatal immaturity.
Riding animals and vehicles other than automobiles (buses, planes, trains).
Jaundice and hemolytic disease.
Excessive cold or heat, hurricanes, tornados, and earthquakes.
Major puerperal infection.
Escherichia coli, giardiasis, and typhoid fever.
Personal Health Care Spending by Condition, Age and Sex Group, and Type of Care in 2013
Figure 1 illustrates health care spending by condition, age group, and type of care. Spending among working-age adults (ages 20–44 years and 45–64 years), which totaled an estimated $1070.1 billion (UI, $1062.8 billion–$1077.3 billion) in 2013, was attributed to many conditions and types of care. Among persons 65 years or older, an estimated $796.5 billion (UI, $788.9 billion–$802.7 billion) was spent in 2013, 21.7% (UI, 21.4%–21.9%) of which occurred in nursing facility care. The smallest amount of health care spending was for persons under age 20 years, and was estimated at $233.5 billion (UI, $226.9 billion–$239.8 billion), which accounted for 11.1% (UI, 10.8%–11.4%) of total personal health care spending in 2013. Ambulatory and inpatient health care were the types of care with the most spending in 2013, each accounting for more than 33% of personal health care spending.
Figure 1. Personal Health Care Spending in the United States by Age Group, Aggregated Condition Category, and Type of Health Care, 2013.
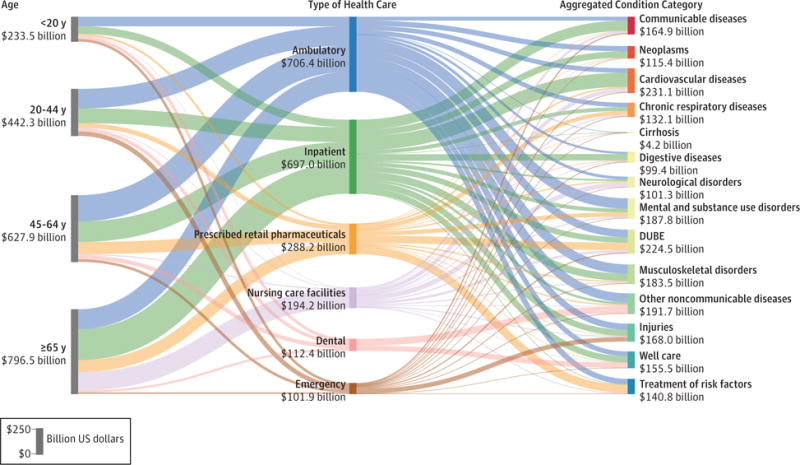
DUBE indicates diabetes, urogenital, blood, and endocrine diseases. Reported in 2015 US dollars. Each of the 3 columns sums to the $2.1 trillion of 2013 spending disaggregated in this study. The length of each bar reflects the relative share of the $2.1 trillion attributed to that age group, condition category, or type of care. Communicable diseases included nutrition and maternal disorders. Table 3 lists the aggregated condition category in which each condition was classified.
Personal Health Care Spending by Age and Sex
Figure 2 illustrates how health care spending was distributed across age and sex groups and conditions in 2013. Panel A shows that ages with the greatest spending were between 50 and 74 years. After this age, spending gradually declined as the size of the population began to decrease due to age-related mortality. Spending is highest for women 85 years and older. Life expectancy for older men is lower, resulting in less spending in the 85 years and older age group for men. Estimated spending differed the most between sexes at age 10 to 14 years, when males have health care spending associated with attention-deficit/hyperactivity disorder, and at age 20 to 44 years, when women have spending associated with pregnancy and postpartum care, family planning, and maternal conditions. Together these conditions were estimated to constitute 25.6% (UI, 24.3%–27.0%) of all health care spending for women from age 20 through 44 years in 2013. Excluding this spending, females spent 24.6% (UI, 21.9%–27.3%) more overall than males in 2013.
Figure 2. Personal Health Care Spending in the United States by Age, Sex, and Aggregated Condition Category, 2013.
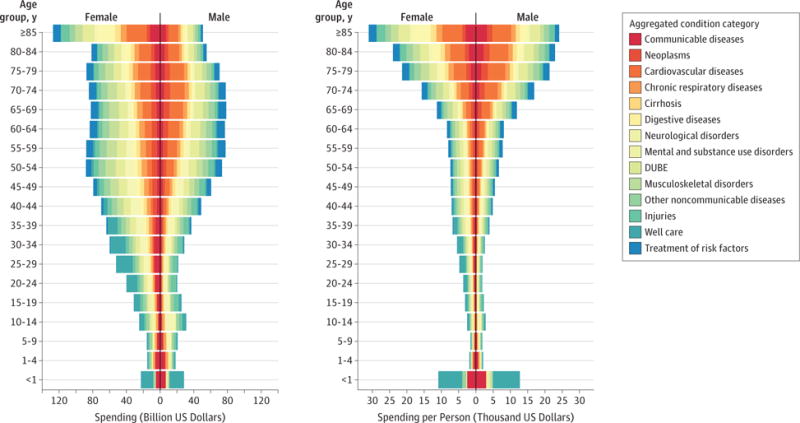
DUBE indicates diabetes, urogenital, blood, and endocrine diseases. Reported in 2015 US dollars. Panel A, illustrates health care spending by age, sex, and aggregated condition category. Panel B, illustrates health care spending per capita. Increases in spending along the x-axis show more spending.
Communicable diseases included nutrition and maternal disorders. Table 3 lists the aggregated condition category in which each condition was classified.
Panel B of Figure 2 shows that spending per person generally increases with age, with the exception of neonates and infants younger than 1 year. Modeled per-person spending on those younger than 1 year was greater than spending on any other age group younger than 70 years. When aggregating across all types of care, those 85 years or older spent more per person on health care than any other age group, although this pattern varied across the 6 types of personal health care and was driven by spending in nursing facilities. In all other types of care, spending per person decreased for the oldest age groups, a pattern that has been observed elsewhere.23 Although more was spent on females than males for every age group starting at age 15, spending per person in 2013 shows a different pattern. Estimated spending per person was greater among females than males for age 15 through 64 years and for age 75 years and older, whereas spending per person was greater among males than females for age 65 through 74 years and for younger than 15 years. Across all ages and conditions that were present for both sexes, the greatest absolute difference between female and male estimated spending per person was for IHD, for which males were estimated to spend more, and for depressive disorders and Alzheimer disease and other dementias, for which females were estimated to spend more.
Changes in US Personal Health Care Spending, 1996–2013
Between 1996 and 2013, health care spending was estimated to increase between 3% and 4% annually for most age groups. Annual growth was estimated to be highest for emergency care (6.4%) and prescribed retail pharmaceuticals (5.6%). Figure 3 and Figure 4 highlight the conditions with the greatest rates of annualized spending growth by condition. Growth rates vary across the age groups. Of conditions with at least $10 billion of spending in 1996, spending on attention-deficit/hyperactivity disorder was estimated to have increased the fastest for age 0 to 19 years (5.9% annually [UI, 3.5%–8.1%]), whereas spending on diabetes had the highest annual growth rates for those aged 20 to 44 years. In the older 2 age groups (45–64 years and ≥65 years), it was estimated that annual spending for hyperlipidemia increased faster than any other condition. Other conditions that had large rates of annualized increase were septicemia and low back and neck pain. Figure 5 shows total increase in spending and the 7 conditions with the largest absolute increase in spending. Diabetes increased $64.4 billion (UI, $57.8 billion–$70.7 billion) from 1996 through 2013. Spending on prescribed retail pharmaceuticals increased the most, especially from 2009 through 2013. Diabetes spending on ambulatory care also increased substantially.
Figure 3. 2013 Personal Health Care Spending in the United States and Annualized Growth Rates by Age Groups 0 to 19 Years and 20 to 44 Years, 1996–2013.
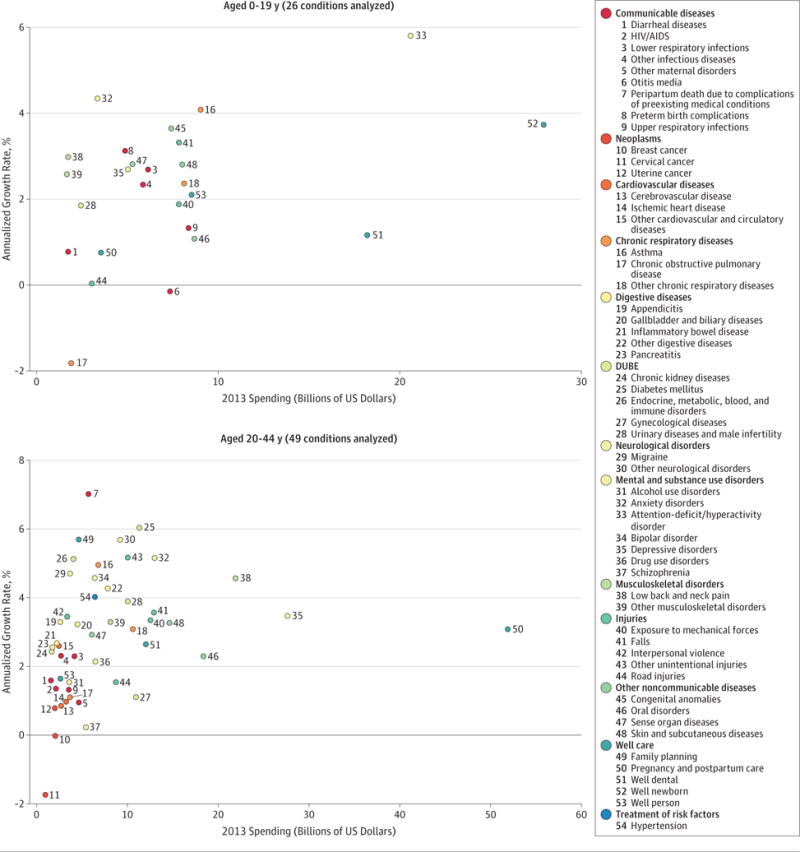
Each panel illustrates 2013 health care spending (reported in 2015 US dollars) and the annualized rate of change for each condition with at least $1 billion of health care spending, for each age group in 1996.
Figure 4. 2013 Personal Health Care Spending in the United States and Annualized Growth Rates by Age Groups 45 to 64 Years and 65 Years and Older, 1996–2013.
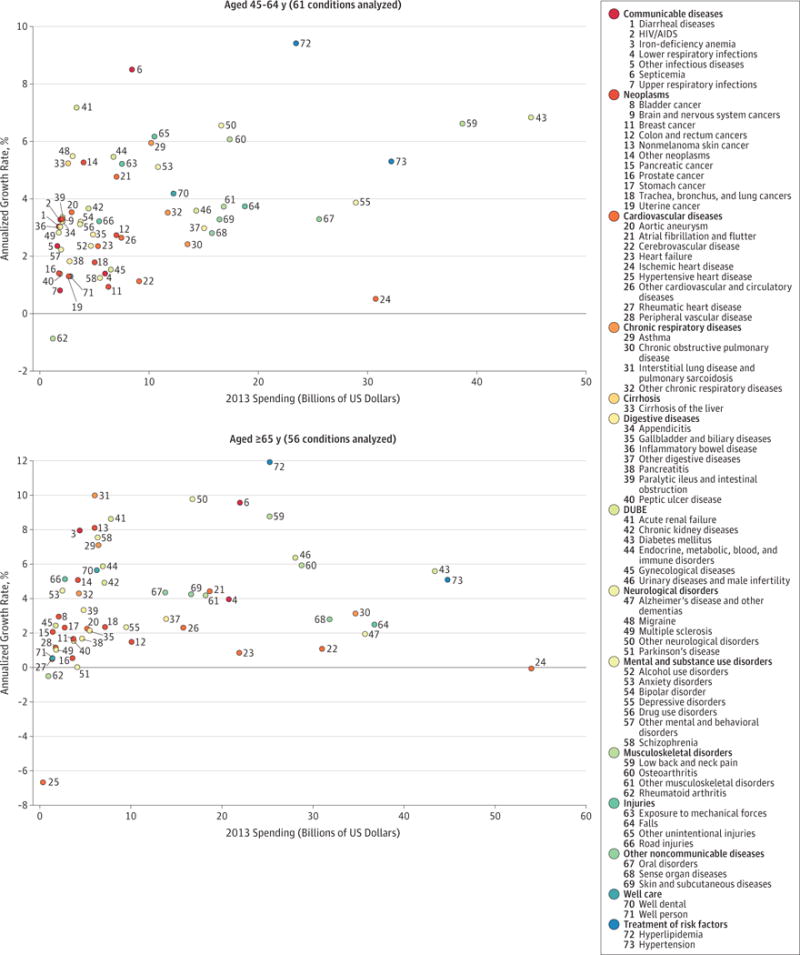
Each panel illustrates 2013 health care spending (reported in 2015 US dollars) and the annualized rate of change for each condition with at least $1 billion of health care spending, for each age group in 1996.
Figure 5. Personal Health Care Spending in the United States Across Time for All Conditions and the 7 Conditions With the Greatest Absolute Increases in Annual Spending From 1996–2013.
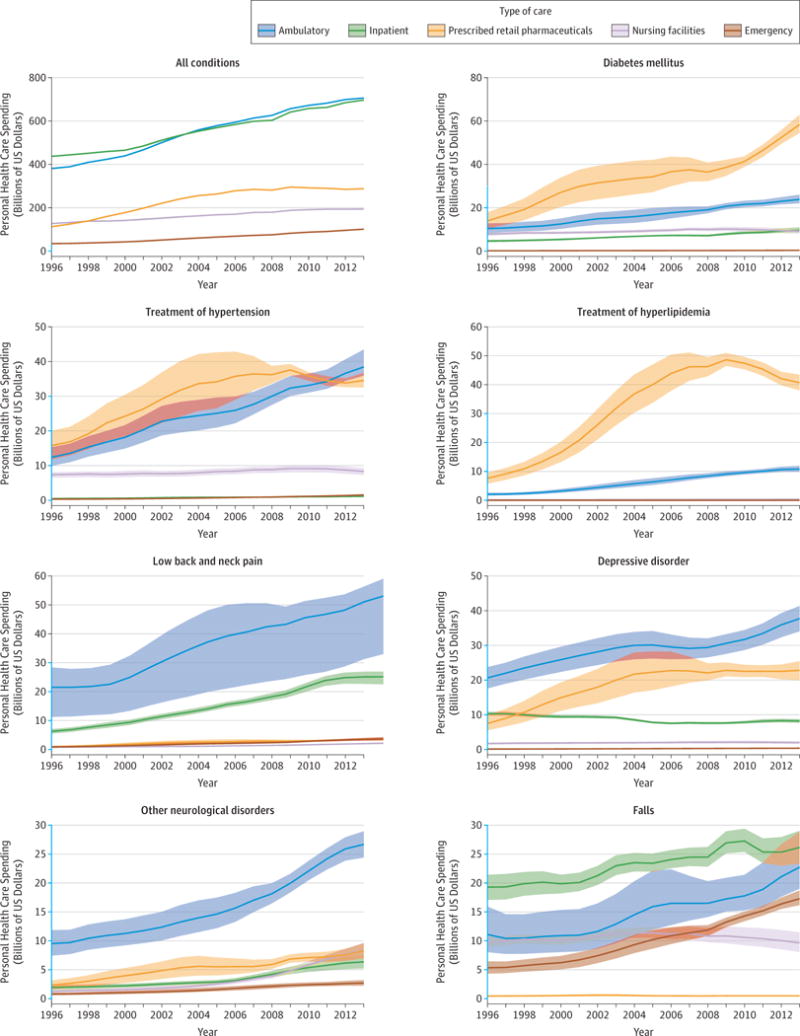
Reported in 2015 US dollars. Y-axis segments shown in blue indicate range from y = $0 billion to y = $30 billion. Shaded areas indicate uncertainty intervals.
Federal Government Public Health Spending
In 2013, 23.8% (UI, 20.6%–27.3%) of government public health spending was provided by the Health Resources and Services Administration, the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and the US Food and Drug Administration. Some of these resources were spent via federally run programs, whereas some of the spending was used to finance public health programs run by state and local governments. Table 4 reports estimated spending on the 20 conditions with the most public health spending. HIV/AIDS was estimated to be the condition in 2013 with the most federal public health spending, with an estimated $3.5 billion (UI, $3.3billion–$4.3billion) spent in 2013. The second-largest and third-largest conditions of federal public health spending in 2013 were estimated to be lower respiratory tract infections and diarrheal diseases, with an estimated $1.8 billion (UI, $1.2 billion–$2.1 billion) and $0.9 billion (UI, $0.7 billion–$1.0 billion) spent, respectively.
Table 4.
Largest 20 Public Health Spending Conditions for 2013 in the United Statesa
| Rankb | Condition | 2013 Spending (Billions of US Dollars), $ | Annualized Rate of Change (1996 to 2013), % |
|---|---|---|---|
| All causes | 76.63 | 2.69 | |
| 1 | HIV/AIDS | 3.52 | 4.97 |
| 2 | Lower respiratory tract infections | 1.78 | 15.68 |
| 3 | Diarrheal diseases | 0.93 | 14.11 |
| 4 | Other infectious diseases (viral and chlamydial infection and streptococcal infection) | 0.67 | 1.25 |
| 5 | Hepatitis | 0.60 | 6.77 |
| 6 | Preterm birth complications (respiratory distress and extreme immaturity) | 0.39 | −0.67 |
| 7 | Varicella | 0.35 | 14.98 |
| 8 | Tobacco (tobacco use disorder and cessation) | 0.34 | 9.58 |
| 9 | Family planning | 0.29 | 9.38 |
| 10 | Tetanus | 0.19 | 1.66 |
| 11 | Whooping cough | 0.19 | 1.66 |
| 12 | Diphtheria | 0.19 | 1.66 |
| 13 | Sexually transmitted diseases excluding HIV | 0.18 | 3.80 |
| 14 | Breast cancer | 0.18 | 30.01 |
| 15 | Meningitis | 0.17 | 6.00 |
| 16 | Low back and neck pain | 0.14 | 8.96 |
| 17 | Tuberculosis | 0.14 | 0.92 |
| 18 | Self-harm | 0.14 | 14.51 |
| 19 | Other neonatal disorders (feeding problems and temperature regulation) | 0.13 | 1.00 |
| 20 | Trachea, bronchus, and lung cancers | 0.13 | 7.39 |
| Top 20 causes | 10.64 | 5.59 |
Public health spending by condition in 2013 for 20 conditions with the largest spending in 2013. Reported in 2015 US dollars.
Ranked from largest spending to smallest spending. eTable 9.3 in the Supplement includes all conditions and uncertainty intervals for all estimates.
Discussion
This research estimated personal health care spending from 1996 through 2013 for 155 conditions, 6 types of health care, and 38 age and sex categories using a standardized set of methods that adjusted for data imperfections. In addition, federal public health spending from 4 US agencies was disaggregated by condition, age and sex group, and type of care. Across all age and sex groups and types of care, diabetes, IHD, and low back and neck pain accounted for the highest amounts of health care spending in 2013. Personal health care spending increased for 143 of the 155 conditions from 1996 through 2013. Spending on low back and neck pain and on diabetes increased the most over the 18 years. From 1996 through 2013, spending on emergency care and pharmaceuticals increased at the fastest rates, which were higher than annual rates for spending on inpatient care and nursing facility care.
Personal Health Care Conditions With Highest Spending
The conditions with highest health care spending in 2013 were a diverse group, with distinct patterns across age and sex, type of care, and time. Some of the top 20 conditions of health care spending in 2013 were chronic diseases with relatively high disease prevalence and health burden.6 These conditions included diabetes, IHD, chronic obstructive pulmonary disease, and cerebrovascular disease, all of which have an underlying health burden nearly exclusively attributable to modifiable risk factors. For example, diabetes was 100% attributed to behavioral or metabolic risk factors that included diet, obesity, high fasting plasma glucose, tobacco use, and low physical activity. Similarly, IHD, chronic obstructive pulmonary disease, and cerebrovascular disease each have more than 78% of their disease burden attributable to similar risks.24 Cancer was not included in the leading causes of spending because it was disaggregated into 29 conditions.
In addition to the chronic diseases mentioned above, a varied set of diseases, injuries, and risk factors composed the list of top 20 conditions causing health care spending. Many disorders related to pain were among these conditions, including low back and neck pain, osteoarthritis, other musculoskeletal disorders, and some neurological disorders associated with pain syndromes and muscular dystrophy. Unlike the 4 chronic conditions already mentioned, spending on these pain-related conditions was highest for working-age adults. Low back and neck pain, which also accounts for a sizable health burden in the United States, was the third-largest condition of spending in 2013 and one of the conditions for which spending increased the most from 1996 through 2013.6
The treatment of 2 risk factors, hypertension and hyperlipidemia, were also among the top 20 conditions incurring spending. Spending for these conditions has collectively increased at more than double the rate of total health spending, and together led to an estimated $135.7 billion (UI, $131.1 billion–$142.1 billion) in spending in 2013. Although a great deal of health burden is attributable to obesity and tobacco, the treatment of these 2 risk factors was not among the top 20 conditions of spending. Growth rates on spending for both of these risk factors were comparable with growth rates on spending for hypertension and hyperlipidemia, but these 2 risk factors had much less spending in 1996, and consequently continued to have much less spending in 2013.
Other disorders among the top 20 conditions accounting for health care spending were injuries resulting from falls and depressive disorders. Falls was the only injury on the top 20 list. Similarly, depressive disorders was the only mental health condition on the list, although when combined with other mental health and substance abuse conditions, this aggregated category became one of the largest aggregated categories of health care spending (Figure 1). There was also a large amount of health care spending for skin disorders, which included acne and eczema; sense disorders, which included vision correction and adult hearing loss; 2 conditions of spending related to dental care; and urinary diseases, which included male infertility, urinary tract infections, and cyst of the kidney. Health care spending on pregnancy and postpartum care was restricted to spending on healthy pregnancy, and excluded costs associated with maternal or neonatal complications, or well-newborn care. Pregnancy and postpartum care was the tenth-largest condition of spending. When combined with well-newborn care, this aggregated category was estimated to compose $83.5 billion (UI, $78.3 billion–$89.5 billion) of spending and accounted for the fifth-highest amount of US health care spending. Lower respiratory tract infection was the condition with the 20th-highest amount of spending, and Alzheimer disease had the 21st-highest amount. Although Alzheimer disease is often the focus of attention due to concerns about accelerated spending growth, this condition has had relatively minor growth (an estimated 1.9% [UI, 0.7%–3.2%]) from 1996 through 2013.
Conditions With the Highest Annual Increases in Personal Health Care Spending
In addition to highlighting conditions with large amounts of spending, this research also traced spending growth over time and identified the largest categories of spending growth. From 1996 through 2013, personal health care spending occurring in the 6 types of care tracked in this study increased by an estimated $933.5 billion. The conditions for which spending increased the most were diabetes, low back and neck pain, hypertension, and hyperlipidemia (Figure 5). Across all conditions, spending on prescribed retail pharmaceuticals increased at an annualized rate of 5.6% from 1996 through 2013. Of the 6 types of personal health care, only spending in emergency departments grew faster (6.4% annually), whereas the share of health care spending for inpatient hospitals and nursing facilities actually decreased. Although spending on prescribed retail pharmaceuticals and emergency department care increased at the fastest rates, the majority of the increase in spending occurred where spending was already concentrated—in ambulatory and inpatient care. Spending for these 2 types of care, which increased by an estimated $324.9 billion and $259.2 billion, respectively, from 1996 through 2013, remained higher than all other types of care.
Spending on Those 65 Years and Older
Because of the aging US population and political concerns about the financing of Medicare, there is increasing interest in health care spending on the oldest age groups. An estimated 37.9% (UI, 37.6%–38.2%) of personal health care spending was for those 65 years and older in 2013. Spending per person was greatest in the oldest age group, reaching an estimated $24 160 (UI, $23 149–$25 270) per man and $24 047 (UI, $23 551–$24 650) per woman. For those 65 years and older, 36.8% (UI, 36.2%–37.2%) of spending was in inpatient hospitals and 21.7% (UI, 21.4%–21.9%) was in nursing facility care, and the largest conditions of health care spending were estimated to be IHD, hypertension, and diabetes.
Comparing Personal Health Care Spending and Public Health Spending
In addition to estimating personal health spending, this study disaggregated public health spending from 4 federal agencies by condition and age and sex group. Prior to this research, studies of government public health programs were primarily focused on state and local programs. Disaggregating federal public health spending shows a focus on a variety of conditions and ages. Top conditions include infectious diseases like HIV/AIDS, lower respiratory tract infections, and diarrheal diseases. This list is different from the list in personal health care spending, where noncommunicable diseases comprise the majority of the spending. Although public health initiatives, such as screening, immunizations, health behavior interventions, and surveillance programs have been shown to be cost-effective, public health spending remains very small compared with personal health spending; in 2013, total government public health spending amounted to an estimated $77.9 billion, or about 2.8% of total health spending.
Comparison With Existing Literature
This research differs from cost of illness studies that measure spending for a single or small set of conditions, as this research used a comprehensive set of conditions and the total amount of spending attributed to these conditions reflects official US personal health spending estimates.25–27 Because of the comprehensive nature of this project, spending estimation was protected from the double counting that can occur in other cost-of-illness studies, in which the same spending may be attributed to multiple conditions.7
Although distinct from most cost-of-illness studies, this research was most similar to previous research by Thorpe and colleagues,5,12,28–30 who have each published work disaggregating health care spending by condition or age and sex groups. Previous research disaggregating spending by conditions showed that mental conditions and cardiovascular diseases accounted for the greatest amount of spending,5,12 and that spending on different conditions was changing at different rates from 2000 through 2010.29 Additionally, previous research disaggregating spending by age and sex groups showed that female spending per person was greater than male spending per person, and spending per person on those 65 years and older was 5 times as much as spending on those 18 years and younger.30 Although the condition list and age groups used in these other projects did not perfectly align with the mapping used in this study, the findings presented here are consistent with these previous findings. Results from this study estimated that in 2013 cardiovascular diseases and mental disorders were the largest aggregate condition categories accounting for health care spending, particularly when Alzheimer disease was included with other mental disorders as it was in these other studies. Similarly, this research confirms that spending per capita among persons 65 years and older was substantially more than spending on the other age groups, and particularly greater than that spent on children younger than 20 years. This study also shows that spending per person on males was generally less than spending on females.
However, the present study contains information and methodological improvements that were lacking in existing studies. The present study added to this literature by disaggregating spending at a more granular level. The condition categories used to disaggregate personal spending span 155 conditions, whereas previous studies used larger, more aggregated categories based on ICD-9 chapters. More importantly, the present study disaggregated personal health care spending simultaneously by condition, age and sex group, and type of care. Simultaneous disaggregation allows researchers and policy makers to focus more precisely on which conditions had increased spending, as well as on the ages and types of care where growth in health care spending is most acute. In addition to this more granular disaggregation, spending estimates for this study were adjusted to account for comorbidities.
Limitations
This research had 4 categories of limitations, all caused by imperfect data. The first category of limitations was technical and occurred because a high-quality census of US health care spending was not available. This problem manifests in several specific problems, all of which require modeling and at-time assumptions that may not be tenable. First, scaling of the estimates to reflect total US health care spending relied upon the assumption that the population-weighted data were representative of total national spending. As has been pointed out elsewhere, this scaling may be biased because some populations—such as incarcerated persons, those receiving care from Veterans Affairs facilities, or those serving on active military duty—were not represented in the raw data.31,32 These groups were estimated to together make up less than 3% of total health care spending.5 Second, health system encounters with exceedingly high health care spending, may not be captured fully in survey data.33 Third, imprecise ICD-9 codes that could not be directly mapped to a health condition required additional modeling and spending redistribution. Fourth, charge data were used for estimation of spending in inpatient care and nursing facility care. Inpatient care charges were adjusted using statistical methods and charge to payment ratios measured using an additional data source, but nursing facility care charges were assumed to reflect spending patterns. If the charge to payment ratios in nursing facility care vary by condition, this assumption will have biased the results. Fifth, this study made spending estimates at a very granular level. In some cases, a small number of cases were used as a basis for estimation.
In all of these cases, multiple data sources were leveraged and statistical smoothing was used to correct potential biases. Although these methods were applied consistently across all data sources and UIs were calculated for all estimates, a diverse set of assumptions and simplifications were necessary. In some cases, these assumptions may not be accurate and may bias the results. Statistical estimation and adjustments should never replace an effort to collect more specific, complete, and publicly available health care data. Given the size and complexity of the US health care system, additional resources are needed to improve patient-level resource tracking across time and types of care.
The second category of limitation was related to the quantification of uncertainty. This study relied on empirical bootstrapping to approximate UIs but these calculations depend on important assumptions that may not hold at the most granular reporting levels. Furthermore, these methods were not calibrated to reflect a precise range of confidence and do not account for all types of uncertainty. Thus, the reported UIs should be interpreted as relative measures of uncertainty, used to compare the uncertainty across the large set of spending estimates.
The third category of limitations was related to unavailable data. In particular, a critical mass of data did not provide information with spending stratified by geographic area, patient race, or socioeconomic status. In addition to this, the most granular GBD condition taxonomy was not used for this study, because at that level of granularity, the underlying data were too sparse to enable resource tracking. Similarly, these estimates extend only to 2013, rather than through the present because more recent data were not sufficiently available. From a policy perspective, these important demographic, socioeconomic, geographic, and epidemiological distinctions could motivate and inform necessary health system improvements, and warrant further research.
The fourth category of limitations was related to public health spending data availability. The fragmentation of the US public health system and lack of a comprehensive data source prevented a disaggregation of total government public health spending, and forced this study to focus exclusively on resources channeled through 4 federal agencies. These agencies make up only 23.8% (UI, 20.6%–27.3%) of total government public health spending. This research was included in this study as a valuable description to juxtapose the foci of public health spending and personal health spending and to highlight the need for ongoing research assessing public health spending.
Conclusions
Modeled estimates of US spending on personal health care and public health showed substantial increases from 1996 through 2013; with spending on diabetes, IHD, and low back and neck pain accounting for the highest amounts of spending by disease category. The rate of change in annual spending varied considerably among different conditions and types of care. This information may have implications for efforts to control US health care spending.
Supplementary Material
Acknowledgments
Funding/Support: This research was supported by grant P30AG047845 from the National Institute on Aging of the National Institutes of Health and by the Vitality Institute.
Role of the Funder/Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Dieleman had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Dieleman, Baral, Birger, Bui, Bulchis, Chapin, Horst, Joseph, Lavado, Lomsadze, DeCenso, Dicker, Flaxman, Templin, Tobias, Murray.
Acquisition, analysis, or interpretation of data: Dieleman, Baral, Birger, Bui, Bulchis, Hamavid, Horst, Johnson, Joseph, Lavado, Lomsadze, Reynolds, Squires, Campbell, DeCenso, Dicker, Flaxman, Gabert, Highfill, Naghavi, Nightingale, Templin, Tobias, Vos, Murray.
Drafting of the manuscript: Dieleman, Birger, Bui, Bulchis, Hamavid, Horst, Joseph, Lavado, Squires, Nightingale, Tobias.
Critical revision of the manuscript for important intellectual content: Dieleman, Baral, Birger, Bui, Bulchis, Chapin, Hamavid, Horst, Johnson, Joseph, Lomsadze, Reynolds, Squires, Campbell, DeCenso, Dicker, Flaxman, Gabert, Highfill, Naghavi, Templin, Tobias, Vos, Murray.
Statistical analysis: Dieleman, Baral, Birger, Bui, Hamavid, Horst, Johnson, Joseph, Lavado, Lomsadze, Reynolds, Squires, Campbell, DeCenso, Dicker, Flaxman, Gabert, Highfill, Naghavi, Templin. Obtained funding: Dieleman, Murray.
Administrative, technical, or material support: Dieleman, Bulchis, Chapin, Hamavid, Nightingale, Murray.
Supervision: Dieleman, Bulchis, Tobias, Murray.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Additional Contributions: We thank Herbie Duber, MD, Mike Hanlon, PhD, Annie Haakenstad, MA, Ann Bett-Madhaven, MLS, and Casey Graves, BA (all from the Institute for Health Metrics and Evaluation), for their assistance and feedback on the research. We also thank Charles Roehrig, PhD, and George Miller, PhD, (both from Altarum Institute); Abe Dunn, PhD, Bryn Whitmire, MS, and Lindsey Rittmueller, MS (all from US Bureau of Economic Analysis); Howard Bolnick, MBA, Jonathan Dugas, PhD, and Francois Millard, FIA (all from Vitality Institute); and David Cutler, PhD (Harvard University), for their feedback on the early draft of this article and its accompanying methods, appendix, and preliminary results. We also thank Kevin O’Rourke, MFA, and Adrienne Chew, ND (both from the Institute for Health Metrics and Evaluation), for their suggestions and edits. No compensation was provided for any assistance or feedback.
References
- 1.World Health Organization. The data repository. http://www.who.int/gho/database/en/. Accessed December 16, 2015.
- 2.Centers for Medicare & Medicaid Services. National health expenditure data: historical. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html. Accessed December 16, 2015.
- 3.National Health Expenditure Accounts. National Health Expenditure Accounts: methodology paper, 2014: definitions, sources, and methods. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/DSM-14.pdf. Accessed November 15, 2015.
- 4.Agency for Healthcare Research Quality. United States Medical Expenditure Panel Survey 1996–2013. https://meps.ahrq.gov/mepsweb/. Accessed November 15, 2016. [PubMed]
- 5.Roehrig C. Mental disorders top the list of the most costly conditions in the united states: $201 billion. Health Aff (Millwood) 2016;35(6):1130–1135. doi: 10.1377/hlthaff.2015.1659. [DOI] [PubMed] [Google Scholar]
- 6.Murray CJL, Barber RM, Foreman KJ, et al. GBD 2013 DALYs and HALE Collaborators Global,regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–2191. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen AB, Cutler DM. Challenges in building disease-based national health accounts. Med Care. 2009;47(7 suppl 1):S7–S13. doi: 10.1097/MLR.0b013e3181a23e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8(1):9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodgson TA, Cohen AJ. Medical care expenditures for diabetes, its chronic complications, and its comorbidities. Prev Med. 1999;29(3):173–186. doi: 10.1006/pmed.1999.0534. [DOI] [PubMed] [Google Scholar]
- 10.Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M. Multimorbidity’s many challenges. BMJ. 2007;334(7602):1016–1017. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 12.Roehrig C, Miller G, Lake C, Bryant J. National health spending by medical condition, 1996–2005. Health Aff (Millwood) 2009;28(2):w358–w367. doi: 10.1377/hlthaff.28.2.w358. [DOI] [PubMed] [Google Scholar]
- 13.Roehrig CS, Rousseau DM. The growth in cost per case explains far more of US health spending increases than rising disease prevalence. Health Aff (Millwood) 2011;30(9):1657–1663. doi: 10.1377/hlthaff.2010.0644. [DOI] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research Quality. United States Nationwide Inpatient Sample 1996–2013. https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed November 15, 2016.
- 15.Hamavid H, Birger M, Bulchis AG, et al. Assessing the complex and evolving relationship between charges and payments in US hospitals: 1996–2012. PLoS One. 2016;11(7):e0157912. doi: 10.1371/journal.pone.0157912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration. National Expenditures for Mental Health Services & Substance Abuse Treatment: 1986–2009. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. United States Medicare Skilled Nursing Facility Limited Data Set 1999–2016. https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/SkilledNursingFacilityMEDPARLDS.html. Accessed November 15, 2016.
- 18.Centers for Disease Control and Prevention. United States National Nursing Home Survey, 1997, 1999, 2004. http://www.cdc.gov/nchs/nnhs/. Accessed November 15, 2016.
- 19.Highfill T, Johnson D. Measuring nursing home price growth between 2000–2009. https://www.bea.gov/papers/pdf/Highfill%20Johnson_Nursing%20Homes%20MCE%20index.pdf. Accessed November 15, 2016.
- 20.National Center for Biotechnology Information. PyMC: Bayesian Stochastic Modelling in Python. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3097064/. Accessed November 28, 2016.
- 21.Foster JT. Bspline. https://github.com/johntfoster/bspline. Accessed June 11, 2016.
- 22.Patil A, Fonnesbeck C, Huard D, Salvatier J. PyMC2. https://github.com/pymc-devs/pymc. Accessed May 15, 2016.
- 23.Yamamoto DH. Health care costs—from birth to death. http://www.healthcostinstitute.org/files/Age-Curve-Study_0.pdf. Accessed November 15, 2016.
- 24.Feigin VL, Roth GA, Naghavi M, et al. Global Burden of Diseases, Injuries and Risk Factors Study 2013 and Stroke Experts Writing Group. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–924. doi: 10.1016/S1474-4422(16)30073-4. [DOI] [PubMed] [Google Scholar]
- 25.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 26.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2006–2014. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorpe KE, Florence CS, Joski P. Which medical conditions account for the rise in health care spending? Health Aff (Millwood) 2004 doi: 10.1377/hlthaff.w4.437. suppl web exclusives:W4-437–45. [DOI] [PubMed] [Google Scholar]
- 29.Dunn A, Rittmueller L, Whitmire B. Health care spending slowdown from 2000 to 2010 was driven by lower growth in cost per case, according to a new data source. Health Aff (Millwood) 2016;35(1):132–140. doi: 10.1377/hlthaff.2015.1109. [DOI] [PubMed] [Google Scholar]
- 30.Lassman D, Hartman M, Washington B, Andrews K, Catlin A. US health spending trends by age and gender: selected years 2002–10. Health Aff (Millwood) 2014;33(5):815–822. doi: 10.1377/hlthaff.2013.1224. [DOI] [PubMed] [Google Scholar]
- 31.Sing M, Banthin JS, Selden TM, Cowan CA, Keehan SP. Reconciling medical expenditure estimates from the MEPS and NHEA, 2002. Health Care Financ Rev. 2006;28(1):25–40. [PMC free article] [PubMed] [Google Scholar]
- 32.Aizcorbe A, Liebman E, Pack S, Cutler DM, Chernew ME, Rosen AB. Measuring health care costs of individuals with employer-sponsored health insurance in the US: a comparison of survey and claims data. Stat J IAOS. 2012;28(1–2):43–51. doi: 10.3233/SJI-2012-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernard D, Cowan C, Selden T, Cai L, Catlin A, Heffler S. Reconciling medical expenditure estimates from the MEPS and NHEA, 2007. Medicare Medicaid Res Rev. 2012;2(4):mmrr.002.04.a09. doi: 10.5600/mmrr.002.04.a09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


