Abstract
Objective
To identify work-related predictors of breastfeeding duration among physicians.
Study design
Data on 238 children were obtained from 50 physicians, whose main affiliation was with Johns Hopkins University (Baltimore, MD), and 80 physicians, whose main affiliation was with University of Florida (Gainesville, FL). We used a mixed linear model to determine which variables were significant predictors of breastfeeding duration, when controlling for maternal demographics and taking into account the clustering of observations on study location and mothers.
Results
Although physicians intended to breastfeed 56% of the infants for at least 12 months and 97% of infants were breastfed at birth, only 34% continued to receive breastmilk at 12 months. Duration of lactation among physicians correlated with the following work-related factors: (1) not having to make up missed call/work that occurred as result of pregnancy or maternity leave; (2) longer length of maternity leave; (3) sufficiency of time at work for milk expression; and (4) perceived level of support for breastfeeding efforts at work from colleagues, program director, or chief residents.
Conclusion
Our findings support the importance of work-related factors in breastfeeding maintenance among physicians and suggest that a tailored intervention, providing time and institutional encouragement, might result in significant improvement in their breastfeeding duration.
Many health organizations recommend exclusive breastfeeding for the first 6 months of life, followed by continued breastfeeding for the first year and beyond.1,2 Exclusive breastfeeding is defined as infant not receiving any nutrition except human milk (with the exception of vitamins and medications). These recommendations are based on extensive evidence of health benefits for both breastfed infants and breastfeeding mothers.3 Human milk has been shown to protect infants against otitis media, gastroenteritis, hospitalization for lower respiratory tract infections, atopic dermatitis, sudden infant death syndrome, necrotizing enterocolitis, type 1 diabetes mellitus, and childhood asthma and obesity.4–8 Maternal benefits include reduced risk of diabetes mellitus and malignancy of breast and ovaries.3 With obesity and diabetes rates increasing, breastfeeding may be considered a cornerstone of preventive medicine. Furthermore, breastfeeding benefits extend beyond the mother and child dyad and include environmental, economic and healthcare cost savings.9–11 For example, some estimate that the United States (U.S.) would save $13 billion and prevent 911 deaths in one year if 90% of families’ infants could be breastfeed exclusively for 6 months.9
Despite excellent breastfeeding initiation rates, female physicians in the US, as a group, are at risk of premature breastfeeding cessation.12–16 Previous studies suggest that work-related factors not only influence physicians’ breastfeeding duration, but might have a stronger impact on their breastfeeding maintenance than do their intentions or education. 17, 18 Improving breastfeeding duration of female physicians requires identification of modifiable work-related and institutional factors that impact breastfeeding duration. To identify predictors of breastfeeding duration among physicians, we analyzed data from 2 observational studies. This study expands on prior research to determine modifiable predictors of breastfeeding duration among physicians. The main variable of interest was duration of breastfeeding, defined as the age (in months) that infant was completely weaned from breastmilk.
Methods
We conducted 2 cross-sectional survey studies at two academic institutions (Johns Hopkins University School of Medicine (JHU) and University of Florida College of Medicine (UF)) in the U.S., using a convenience sample of female physicians who volunteered to participate. 17, 18
Criteria for participation were identical for both studies and included being a female physician (Doctor of Medicine [MD] or Doctor of Osteopathic Medicine [DO]) and having at least one biological child. Eligible participants were included whether they were in training (e.g., resident or fellow) or had completed training (eg, faculty at academic site or community practice). Participants were included, regardless of their infants’ feeding methods (formula, breastmilk, or combination). Although recruitment efforts only focused on physicians affiliated with JHU and UF, we included physicians not affiliated with either institution if they contacted us to express interest in the study and were otherwise eligible to participate.
JHU Study
The institutional review board at JHU approved the protocol for this study.17 The initial questionnaire was developed in 2008 after review of instruments utilized in previous similar studies.12–15, 19 The questionnaire was piloted among 20 physicians who were not included in the subsequent studies. The final instrument contained 49 items and took approximately 15–30 minutes to complete. Participants were asked a series of questions regarding each of their children, including age, infant-feeding intention, whether or not the infant was breastfed, mother’s goal for breastfeeding duration when infant was born, age at which infant first received any nutrition other than breastmilk, age at which infant was weaned completely from breastmilk, as well as work-related factors and other enablers and obstacles of breastfeeding. To assess availability of time at work for milk expression, participants chose between “never,” “occasionally,” “sometimes,” “often,” and “always.” Similarly, availability of worksite lactation facilities was assessed by asking each participant their frequency of “access to appropriate place to express milk.” Participants also were asked to rate the support that they felt they received for their breastfeeding efforts while working from colleagues, attending physicians if applicable, and program director or chief. Participants could choose “always opposed my efforts,” “usually opposed my efforts,” “neither supportive nor oppositional,” “usually supportive,” and “always supportive.” When participants reported that they faced opposition of their breastfeeding efforts at work, they were asked to choose any of the following as reasons that might have influenced the opposition, “changes in the schedule,” “perceived special favors,” “lack of administrative support,” “more work for others,” or “other (please specify).”
Recruitment was initiated through an e-mail that contained information about the study and contact information for the principal investigator (PI). This e-mail was sent once to the head of the institution’s Women’s Task Force as well as residency program directors, with request for dissemination. The recruitment e-mail stated that the purpose of the study was to assess infant-feeding intentions and practices of physicians and possible obstacles and enablers that affect their breastfeeding success. The PI set up interviews with potential participants as they expressed interest in the study via e-mail or telephone. Fifty eligible interviews were conducted between February and August of 2009. Although every attempt was made to meet with all participants, only 29 interviews were performed in person. Due to time constraints and clinical responsibilities, 10 participants completed the interview on the phone. Eleven participants completed the paper questionnaire and were interviewed in person or on the phone afterwards to clarify and confirm their written responses. The PI conducted all the interviews (by phone and in person).
UF Study
The institutional review board at UF approved the protocol for this study.18 Further survey items and response scales were developed in 2009 and incorporated into the JHU questionnaire mainly to assess breastfeeding advocacy of participants. This modified instrument contained 53 items and took approximately 20–30 minutes to complete. The recruitment e-mail was sent once in 2009 to residency and fellowship program directors and once in 2010 to the institution’s listserv for housestaff and faculty. The PI set up interviews with potential participants as they responded to express interest in the study. All participants were interviewed in person between October 2009 and July 2011 by the PI.
Statistical Analyses
Data from the 2 institutional studies were merged using REDCap electronic data capture tools hosted at UF.20 The primary outcomes were predictors of breastfeeding duration. We used the R statistical software package (V.2.15.0; R Foundation for Statistical Computing, Vienna, Austria, 2012) to generate means, standard deviations and frequencies of demographic variables in the data set and to conduct univariate tests. We used the infant as the unit of analysis for calculation of rates because infant-feeding practices of some multiparous participants varied with different offspring. All comparisons were performed at a 95% confidence level.
We created a series of models, each with breastfeeding duration as the outcome variable. We transformed maternal specialty to a dichotomous variable by assigning it as surgical if associated mainly with procedures, and labeled all other specialties as non-surgical (Table I). Variables in the following categories were included as primary predictors: maternal demographics (e.g. age at the time of study, stage of career at the time of study, number of biological children, location (JHU or UF), specialty (surgical or nonsurgical), and marital status), breastfeeding education (medical school and residency), child-related information (e.g. birth year, age at the time of mother’s participation in the study, maternal stage of career at the time of childbirth, breastfeeding duration goal, and maternal reasons for decision to breastfeed), and maternal work-related factors (eg, duration of maternity leave, duration of paid leave, maternity leave makeup, reasons for return to work, availability of worksite lactation facilities, availability of time at work for milk expression or breastfeeding, and support from colleagues).
In subsequent multivariate analysis, we used a mixed linear model to determine which survey responses were significant predictors of breastfeeding duration when controlling for maternal demographics (eg, maternal age, career stage, number of biological children, specialty, marital status, breastfeeding education, and birth year of child) and taking into account the clustering of observations on study location and mothers. We modeled the mother as a repeated factor, used an exchangeable working covariance structure, and excluded subjects still being breastfed at the time of the study. We considered any variable with a p value < 0.05 a significant predictor of duration of breastfeeding.
Results
One hundred and thirty interviews were included in this analysis. Eighty participants (61.5%) were recruited at UF or affiliated institutions and 50 (38.5%) at JHU or affiliated institutions (Table II). The participants’ ages ranged from 26 to 60 years at the time of the study, with a mean age of 37.6 years (Table II). Thirty seven (28.5%) participants were in training, and 93 (71.5%) had completed training. Only 21.5% (n = 28) of participants reported receiving breastfeeding education in medical school and 19.2% (n =25) received breastfeeding education in residency. Additional demographics are characterized in Table II. Participants’ specialties are described in Table I. Eighty-five (65.4%) participants were in non-surgical fields and 45 (34.6%) in surgical fields.
The 130 participants included in the study had a total of 238 children, ranging in age from 6 weeks to 28 years old. One-hundred-and-sixty-nine (71%) of the children were born in or after 2003, the year that the 80-hour work week was implemented, and 69 (29%) were born before 2003 (19). At the time of the study, 2 participants had not returned to work yet. Participants reported returning to work full-time after childbirth in 194 (81.5%) cases.
Breastfeeding Intentions and Behavior
Intention to breastfeed was 100% as all 130 participants reported planning to breastfeed during all 238 pregnancies. The 2 most frequent reasons cited for breastfeeding intention were infant health (98%; n= 226) and bonding (84%; n = 150). In 215 pregnancies (90.3%), participants expressed numerical goals for breastfeeding duration, ranging from 1 to 24 months, and in 134 cases (56.3%) planned to breastfeed for at least 12 months. In 23 pregnancies, participants either reported not having a goal regarding the length of breastfeeding or stated that they had hoped to breastfeed until return to work or as long as possible.
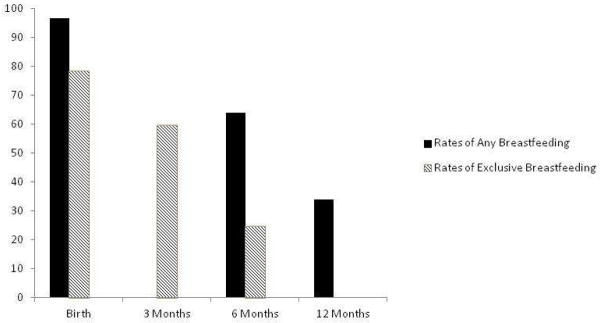
Immediately after birth, 186 children (78.2%) were breastfed exclusively, 44 (18.5%) received a combination of human milk and formula, and 8 (3.4%) received formula only. Participants reported that 3 infants did not receive human milk because of maternal health issues, 2 due to infant health issues, and 3 because of lack of breastmilk. One hundred and forty two infants (59.7%) continued to receive breastmilk exclusively at 3 months and 59 (24.8%) at 6 months (Figure). The mean duration of exclusive breastfeeding was 3.49 months (standard deviation of 2.43, range of 0–13 months).
Figure 1.
Breastfeeding Rates of Physicians in our Studies
The mean duration of breastfeeding was 9.91 months (standard deviation of 6.34, range of 0–36). One hundred and fifty two infants (63.9%) continued to receive some human milk at 6 months, and 81 (34.0%) at 12 months (Figure). Participants continued to breastfeed 212 of the infants (89.1%) after return to work and reported expressing milk at work in 202 (84.9%) cases. Thirty participants were breastfeeding at the time of study.
Predictors of Breastfeeding Duration
Potentially modifiable work-related factors that were associated with breastfeeding duration consisted of: (1) no requirement to make up missed work or call that occurred as a result of pregnancy or maternity leave; (2) longer duration of maternity leave; (3) availability of time at work to express milk or breastfeed; and (4) participant’s perception of level of enhanced support for her breastfeeding efforts at work from her colleagues and program director or chief (Table III). Mean duration of breastfeeding for participants who reported having to make up missed call or work was 8 months, compared with 10.1 months for participants who reported not having to make up missed call or work (p=0.043). One week increase in total maternity leave (paid and unpaid) was associated with 0.14 month increase in breastfeeding duration (r=0.16, p=0.022).
Each increase in score in reported availability of time at work for milk expression (e.g. occasionally compared with never) was associated with a 1.1-month increase in breastfeeding duration (r=0.29, p <0.0001). Although attending physician’s support initially had a statistically significant association with breastfeeding duration (r = 0.17, p = 0.028), the correlation was not significant in the multivariate analysis. Each unit increase in reported collegial support (eg always supportive compared with usually supportive) was associated with 1.3-month increase in breastfeeding duration (r = 0.19, p = 0.011) and each unit increase in reported support from chief residents or program director was associated with 1.1-month increase in breastfeeding duration (p=0.010) in the multivariate analysis.
Maternal demographics (maternal age, career stage, number of biological children, specialty, marital status, breastfeeding education, and birth year of child) were not significant predictors of breastfeeding duration (all p-values>0.25). Similarly, maternal reasons for return to work did not have statistically significant association with breastfeeding duration. There was a strong correlation between breastfeeding duration and maternal goal for breastfeeding duration (p<0.0001). Each month increase in reported maternal goal to breastfeed was associated with a 0.86-month increase in actual breastfeeding duration (Table III). Citing inadequate time or inadequate milk supply as reasons for complete breastfeeding cessation was associated with shorter breastfeeding duration (Table III). Participants who reported that they encountered non-support at work due to perceived special favors by their colleagues had an average 3.5 month decrease in breastfeeding duration compared with participants who did not report perceived special favors by their colleagues (p = 0.037). The other reasons for work-site non-support did not have a statistically significant association with duration of breastfeeding.
Discussion
Maternal postpartum employment has been cited as a major obstacle to exclusive breastfeeding and breastfeeding continuation in the general population.21–26 Availability of worksite lactation facilities, support from coworkers and supervisors, and length of maternity leave have been associated with breastfeeding success in working women, and inflexible work schedules have been associated with breastfeeding cessation.27–36 Based on previous literature, we expected similar associations among physicians.12–14, 17 However, we did not find a statistically significant correlation between availability of worksite lactation facilities and breastfeeding duration of physicians. From our qualitative data, we believe that physicians often overcome the barrier of space at work for milk expression by creatively using unconventional locations, such as unused patient rooms, on-call rooms, or recovery rooms.17, 18
The work-related variables that showed significant associations with breastfeeding duration might reflect the flexibility of a physician’s work schedule as well as the level of overall support in her immediate work environment. To date, randomized trials have not been conducted that evaluate the effectiveness of workplace interventions in promoting breastfeeding among women returning to paid work after childbirth. As women now make up almost one-half of the American workforce and more mothers of infants are participating in the workforce,37 scientific evaluation of the effectiveness of workplace interventions in promoting breastfeeding among working women is an important next step in developing evidence-based and cost-effective health policy change to improve their breastfeeding continuation and exclusive breastfeeding rates.
Protected time at work might be easier and more cost-effective to modify than other potential work-related factors, such as length of maternity leave. Our results support further study to determine whether protected time at workplace for milk expression and breastfeeding as well as other programs to promote breastfeeding duration among physicians returning to work will increase the frequency and duration of their breastfeeding.
As our studies were cross-sectional, the associations we have reported do not imply causality. Recall bias is possible because we relied on participants’ memories of previous breastfeeding behavior. Although maternal recall is thought to be a valid and reliable estimate of breastfeeding initiation and duration, validity and reliability of maternal recall for breastfeeding intention are not clear. 38, 39 Another potential limitation is institutional bias, as the individual studies were conducted mainly in 2 academic medical centers. Although this allowed for detailed, in-depth analyses with extensive one-on-one interviews, our findings might not be applicable to all physicians in the U.S. Issues of time and change of practice also might affect our results as the enablers and obstacles older women included in our study reported might be different that those younger women are currently facing. Other potential limitations are recruitment bias suggested by the high percentage of participants from the specialty of Internal Medicine, and selection bias, which could result in over-representation of actual breastfeeding rates among physicians.
Our findings emphasize the discrepancy between physician mothers’ breastfeeding duration goal and their actual breastfeeding duration. Furthermore, our results support the importance of work-related factors in breastfeeding maintenance among female physicians and suggest that a tailored intervention, providing time and institutional encouragement, might result in significant extension of their duration of breastfeeding.
These findings have important implications for future prospective and interventional research, involving a larger and more diverse sample from various healthcare settings to determine whether significant differences exist in infant-feeding intentions and behavior of physicians in different healthcare settings, specialties, and those in training versus physicians in practice. Cause and effect relationships between maternal work-related factors and breastfeeding behavior would also best be assessed prospectively.
Table 1.
Specialties of Physician Mothers Included in the Study (n=130)
| Specialty | Number | Percentage (%) |
|---|---|---|
| Surgical | ||
| Anesthesiology | 8 | 6.2 |
| Ear, nose & throat | 1 | 0.8 |
| General surgery and subspecialties | 6 | 4.6 |
| Medicine/interventional cardiology | 8 | 6.2 |
| Medicine/gastroenterology | 7 | 5.4 |
| Medicine/pulmonary and critical care | 1 | 0.8 |
| Obstetrics gynecology | 6 | 4.6 |
| Ophthalmology | 1 | 0.8 |
| Pediatrics/gastroenterology | 1 | 0.8 |
| Pediatrics/pulmonary | 1 | 0.8 |
| Radiology | 4 | 3.1 |
| Urology | 1 | 0.8 |
| Total surgical | 45 | 34.6 |
| Non-surgical | ||
| Dermatology | 1 | 0.8 |
| Family medicine | 4 | 3.1 |
| * General internal medicine and subspecialties | 55 | 42.3 |
| Internal medicine/pediatrics | 1 | 0.8 |
| Neurology | 4 | 3.1 |
| Pathology | 2 | 1.5 |
| * Pediatrics and other pediatric subspecialties | 13 | 10.0 |
| Physical medicine and rehab | 1 | 0.8 |
| Psychiatry | 3 | 2.3 |
| Radiation oncology | 1 | 0.8 |
| Total non-surgical | 85 | 65.4 |
Procedure-based subspecialties, such as gastroenterology, interventional cardiology, and pulmonary in internal medicine and pediatrics were categorized as “surgical,” and other subspecialties (e.g., endocrinology) were categorized as “non-surgical.”
Table 2.
Maternal Demographics (n = 130)
| Category | Number (%) |
|---|---|
| Age (years) at time of study | |
| Mean +/− standard deviation | 37.55 ± 6.67 |
| Median [Range] | 36.5 [26–60] |
| Mode | 39 |
| Study location | |
| Johns Hopkins University School of Medicine | 50 (38.5%) |
| University of Florida College of Medicine | 80 (61.5%) |
| Career stage at time of study | |
| In training (residency or fellowship) | 37 (28.5%) |
| Had completed training | 93 (71.5%) |
| Specialty (surgical or non-surgical) | |
| Surgical | 45 (35.4%) |
| Non-surgical | 85 (64.6%) |
| Marital Status at time of Study | |
| Married | 121 (93.1%) |
| Other | 9 (6.9%) |
| Number of biological children | |
| 1 | 47 (36.2%) |
| 2 | 63 (48.5%) |
| 3 | 15 (11.5%) |
| 4 | 5 (3.8%) |
| Age of children (months) | |
| Mean +/− standard deviation | 73.24 ± 48.00 |
| Median [Range] | 48.0 [1.5–336.0] |
| Mode | 60 |
| Maternal stage of career at childbirth | |
| Before medical school | 6 (3%) |
| During medical school | 16 (5%) |
| During residency | 62 (29%) |
| During fellowship | 41 (15%) |
| After completion of training | 104 (43%) |
| Other stages of medical training | 9 (5%) |
| Infant-feeding Intentions | |
| Maternal intention to breastfeed each infant | 238 (100%) |
| Maternal intention to breastfeed infant for at least 12 months | 134 (56.3%) |
| Breastfeeding education during medical school | |
| Yes | 28 (21.5%) |
| No | 102 (78.5%) |
| Breastfeeding education during residency | |
| Yes | 25 (19.2%) |
| No | 105 (80.8%) |
Table 3.
Significant Predictors of Breastfeeding Duration (BFD) (Controlling for Maternal Demographics)
| Variables | Estimated effect on BFD (in months) | 95% CI (for the effect) | P-value |
|---|---|---|---|
| General variables | |||
| Maternal BFD goal | 0.86 increase in BFD for each 1 month increase in BFD goal | (0.642, 1.08) | <0.001 |
| Infant feeding method at birth | <0.001 | ||
| Exclusive BF | 8.2 increase in BFD compared to formula only | (4.17, 12.10) | <0.001 |
| Combination (BF & formula) | 3.0 increase in BFD compared to formula only | (0.951, 4.95) | 0.003 |
| Infant-feeding method consistency | 2.5 increase in BFD if reported consistent infant feeding method during 30 days postpartum | (0.589, 4.37) | 0.011 |
| Work-related variables | |||
| Maternity leave | 0.14 increase in BFD for each week increase in total maternity leave (paid and unpaid) | (0.042, 0.233) | 0.005 |
| Maternity leave make-up | 3.6 increase in BFD if mother did not report requirement to make up missed call or work | (0.690, 6.54) | 0.016 |
| Collegial support of Milk Expression at Work (MW) | 1.3 increase in BFD for each unit increase in score on this question | (0.366, 2.25) | 0.007 |
| Program director or chief’s support of MW | 1.1 increase in BFD for each unit increase in score on this question | (0.263, 1.90) | 0.010 |
| Reported “perceived special favors” influenced collegial non-support of MW | 3.5 decrease in BFD if answered “yes” | (−6.77, −0.145) | 0.041 |
| Weaning-related variables | |||
| BF weaning due to infant health | 6.6 increase in BFD if answered “no” | (1.57, 11.7) | 0.011 |
| BF weaning due to infant lack of interest in BF | 2.17 decrease in BFD if answered “yes” | (−4.16, −0.200) | 0.031 |
| BF weaning for inadequate time | 2.9 increase in BFD if answered “no” | (0.616, 5.12) | 0.013 |
| BF weaning for inadequate milk | 3.3 increase in BFD if answered “no” | (1.32, 5.29) | 0.001 |
| BF weaning due to other reason* | 3.4 increase in BFD if answered “yes” | (1.70, 5.01) | <0.001 |
Mothers were asked the reason for breastfeeding cessation for each of their children. The choices were “Mother not interested in breastfeeding,” “Mother not comfortable with breastfeeding,” “Lack of adequate milk supply,” “Too stressful,” “Lack of time,” Maternal health,” “Infant health,” “Infant not interested in breastfeeding,” and “Other.” Reporting “other” reasons for breastfeeding cessation than those listed was associated with a 3.3-month increase in breastfeeding duration.
Acknowledgments
Supported by Clinical and Translational Science Institute, National Institutes of Health (1UL1RR029890).
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Academy of Pediatrics Breastfeeding and the use of human milk. Work Group on Breastfeeding. Pediatrics. 1997;100:1035–9. doi: 10.1542/peds.100.6.1035. [DOI] [PubMed] [Google Scholar]
- 2.World Health organization (WHO) Global strategy on infant and young child feeding. Geneva: WHO; 2001. [Google Scholar]
- 3.Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007;153:1–186. [PMC free article] [PubMed] [Google Scholar]
- 4.Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, Schanler RJ, et al. American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 5.Grummer-Shawn LM, Mei Z. Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics. 2004;113:e81–6. doi: 10.1542/peds.113.2.e81. [DOI] [PubMed] [Google Scholar]
- 6.Scariati PD, Grummer-Strawn LM, Fein SB. A longitudinal analysis of infant mortality and the extent of breastfeeding in the United States. Pediatrics. 1997;99:E5. doi: 10.1542/peds.99.6.e5. [DOI] [PubMed] [Google Scholar]
- 7.Bonati M, Campi R. Breastfeeding and infant illness. Am J Public Health. 2000;90:1478–9. doi: 10.2105/ajph.90.9.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oddy WH. Breastfeeding protects against illness and infection in infants and children: a review of the evidence. Breastfeed Rev. 2001;9:11–18. [PubMed] [Google Scholar]
- 9.Bartick M, Reinhold A. The Burden of Suboptimal Breastfeeding in the United States: A Pediatric Cost Analysis. Pediatrics. 2010;125:e1048–56. doi: 10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- 10.Riordan JM. The cost of not breastfeeding: a commentary. J Hum Lact. 1997;13:93–7. doi: 10.1177/089033449701300202. [DOI] [PubMed] [Google Scholar]
- 11.Wright AL. The rise of breastfeeding in the United States. Pediatr Clin North Am. 2001;48:1–12. doi: 10.1016/s0031-3955(05)70282-0. [DOI] [PubMed] [Google Scholar]
- 12.Miller N, Miller D, Chism M. Breastfeeding practices among resident physicians. Pediatrics. 1996;98:434–7. [PubMed] [Google Scholar]
- 13.Arthur CR, Saenz RB, Replogle WH. The employment-related breastfeeding decisions of physician mothers. J Miss State Med Assoc. 2003;44:383–7. [PubMed] [Google Scholar]
- 14.Arthur CR, Saenz RB, Replogle WH. Personal breast-feeding behaviors of female physicians in Mississippi. South Med J. 2003;96:130–5. doi: 10.1097/01.SMJ.0000051268.43410.45. [DOI] [PubMed] [Google Scholar]
- 15.Kacmar JE, Taylor JS, Nothnagle M, Stumpff J. Breastfeeding practices of resident physicians in Rhode Island. Med Health R I. 2006;89:230–1. [PubMed] [Google Scholar]
- 16.Sattari M, Levine D, Serwint JR. Physician mothers: an unlikely high risk group-call for action. Breastfeed Med. 2010;5:35–9. doi: 10.1089/bfm.2008.0132. [DOI] [PubMed] [Google Scholar]
- 17.Sattari M, Levine D, Bertram A, Serwint JR. Breastfeeding Intentions of Female Physicians. Breastfeed Med. 2010;5:297–302. doi: 10.1089/bfm.2009.0090. [DOI] [PubMed] [Google Scholar]
- 18.Sattari M, Levine D, Neal D, Serwint JR. Personal Breastfeeding Behavior of Physician Mothers Is Associated with Their Clinical Breastfeeding Advocacy. Breastfeed Med. 2013;8:31–7. doi: 10.1089/bfm.2011.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freed GL, Clark SJ, Sorenson J, Lohr J, Cefalo R, Curtis P. National assessment of physicians’ breastfeeding knowledge, attitudes, training, and experience. JAMA. 1995;273:472–6. doi: 10.1001/jama.1995.03520300046035. [DOI] [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hawkin SS, Griffiths LJ, Dezateux C, Law C. The Millennium Cohort Study Child Health Group. The Impact of maternal employment on breast-feeding duration in the UK Millennium cohort study. Public Health Nutr. 2007;10:891–6. doi: 10.1017/S1368980007226096. [DOI] [PubMed] [Google Scholar]
- 22.McKinley NM, Hyde JS. Personal Attitudes or Structural Factors? A Contextual Analysis of Breastfeeding Duration. Psycho Women Quart. 2004;28:388–399. [Google Scholar]
- 23.Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, Lieu TA. Clinician support and psychological risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112:108–115. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 24.Ryan AS, Zhou W, Arensberg MB. The effect of employment status on breastfeeding in the United States. Women health Issues. 2006;16:243–51. doi: 10.1016/j.whi.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Cooking AR, Donath SM, Amir LH. Maternal employment and breastfeeding: results from the longitudinal study of Australian children. Acta Paediatr. 2008;97:620–3. doi: 10.1111/j.1651-2227.2008.00740.x. [DOI] [PubMed] [Google Scholar]
- 26.Meek JY. Breastfeeding in the workplace. Pediatr Clin North Am. 2001;48:461–74. doi: 10.1016/s0031-3955(08)70038-5. [DOI] [PubMed] [Google Scholar]
- 27.Lewallwen LP, Dick MJ, Flowers J, Powell W, Zickefoose KT, Wall YG, Price ZMl. Breastfeeding support and early cessation. J Obstet Gynecol Neonatal Nurs. 2006;35:166–72. doi: 10.1111/j.1552-6909.2006.00031.x. [DOI] [PubMed] [Google Scholar]
- 28.Guendelman S, Kosa JL, Pearl M, Graham S, Goodman J, Kharrazi M. Juggling Work and breastfeeding: Effects of maternity Leave and occupational Characteristics. Pediatrics. 2009;123:e38–46. doi: 10.1542/peds.2008-2244. [DOI] [PubMed] [Google Scholar]
- 29.Visness CM, Kennedy KI. Maternal employment and breastfeeding: findings from the 1988 National Maternal and Infant Health Survey. Am J Public Health. 1997;87:945–50. doi: 10.2105/ajph.87.6.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacknowitz A. The role of workplace characteristics in breastfeeding practices. Women Health. 2008;47:87–111. doi: 10.1080/03630240802092357. [DOI] [PubMed] [Google Scholar]
- 31.Ortiz J, McGilligan K, Kelly P. Duration of breast milk expression among working mothers enrolled in an employer-sponsored lactation program. Pediatr Nurs. 2004;30:111–9. [PubMed] [Google Scholar]
- 32.Johnston ML, Esposito N. Barriers and facilitators for breastfeeding among working women in the United States. J Obstet Gynecol Neonatal Nurs. 2007;36:9–20. doi: 10.1111/j.1552-6909.2006.00109.x. [DOI] [PubMed] [Google Scholar]
- 33.Borwn CA, Poag D, Kasprzycki C. Exploring large employers’ and small employers’ knowledge, attitudes, and practices on breastfeeding support in the workplace. J Hum Lact. 2001;17:39–46. doi: 10.1177/089033440101700108. [DOI] [PubMed] [Google Scholar]
- 34.Kimbro RT. On-the-job moms: work and breastfeeding initiation and duration for a sample of low-income women. Matern Child Health J. 2006;10:19–26. doi: 10.1007/s10995-005-0058-7. [DOI] [PubMed] [Google Scholar]
- 35.Fein SB, Roe BE. The effect of work status on initiation and duration of breastfeeding. Am J Public Health. 1998;88:1042–6. doi: 10.2105/ajph.88.7.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roe B, Whittington LA, Fein SB, Teisl MF. Is there competition between breastfeeding and maternal employment? Demography. 1999;36:157–71. [PubMed] [Google Scholar]
- 37. [Accessed January 17, 2013];Women in the Labor Force in 2010 Fact Sheet. http://www.dol.gov/wb/factsheets/Qf-laborforce-10.htm.
- 38.Launer LJ, Forman MR, Hundt GL, et al. Matenral recall of infant feeding events is accurate. J Epidemiol Community Health. 1992;46:203–206. doi: 10.1136/jech.46.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li R, Scanlon KS, Serudla MK. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev. 2005;63:103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]