Abstract
Objectives. To estimate obesity and overweight prevalence in American Indian and Alaska Native (AI/AN) children across genders, ages, and geographic regions in the Indian Health Service active clinical population.
Methods. We obtained data from the Indian Health Service National Data Warehouse. At least 184 000 AI/AN children aged 2 to 19 years had body mass index data for each year studied, 2006 to 2015. We calculated body mass index percentiles with the 2000 Centers for Disease Control and Prevention growth charts.
Results. In 2015, the prevalence of overweight and obesity in AI/AN children aged 2 to 19 years was 18.5% and 29.7%, respectively. Boys had higher obesity prevalence than girls (31.5% vs 27.9%). Children aged 12 to 19 years had a higher prevalence of overweight and obesity than younger children. The AI/AN children in our study had a higher prevalence of obesity than US children overall in the National Health and Nutrition Examination Survey. Results for 2006 through 2014 were similar.
Conclusions. The prevalence of overweight and obesity among AI/AN children in this population may have stabilized, while remaining higher than prevalence for US children overall.
Obesity has emerged as a marker of serious health risk for our nation’s children. Childhood obesity is associated with increased risk for later development of type 2 diabetes and other chronic diseases such as hypertension, coronary heart disease, and some forms of cancer.1,2 Obesity also increases the risk for social and emotional morbidity for children and adolescents.1 Furthermore, childhood obesity tends to persist into adulthood.1,2
According to previous studies, American Indian children experience higher prevalence of obesity and related health conditions, such as type 2 diabetes, compared with US children as a whole.1,3–8 However, previous estimates of obesity among American Indian/Alaska Native (AI/AN) children have relied upon limited regional studies, often with small sample sizes.1 The extent and severity of obesity among AI/AN children and youths have not been examined nationally.
Childhood obesity among low-income preschool-aged children in the United States may be decreasing, as indicated by Pediatric Nutrition Surveillance System data in several states9 and in nationally representative data of children aged 2 to 5 years from the National Health and Nutrition Examination Survey (NHANES) from 2003–2004 to 2013–2014.10 However, the latest studies drawing upon nationally representative data from NHANES have demonstrated no significant changes in childhood obesity prevalence for children aged 2 to 19 years in recent years, from 2005–2006 to 2013–2014.10,11 These findings suggest that overall childhood obesity prevalence may be plateauing, but is not decreasing.
To determine if similar trends are occurring in AI/AN children, we examined the prevalence of childhood obesity and overweight in the Indian Health Service (IHS) active clinical population in each year from 2006 to 2015. In addition, we estimated prevalence by age, sex, and geographic region.
METHODS
We used data collected each fiscal year (October 1 to September 30) from 2006 to 2015 at federally funded health care facilities that serve AI/AN people across all 12 IHS administrative areas. The facilities include federally operated IHS hospitals and clinics, as well as facilities operated directly by tribal governments through contracts or compacts with the IHS. We also included urban Indian health organizations that provide services to AI/AN people residing in 34 metropolitan areas. Together, these health care facilities serve about 2.2 million AI/AN people who belong to 567 federally recognized tribes in 36 states.
We obtained the data from the IHS National Data Warehouse (NDW), a central repository of registration and encounter-based patient data from IHS, tribal, and urban (I/T/U) Indian health facilities.12–15 As patients can receive services at multiple facilities, which submit data separately to the NDW, we identified unique patients according to the IHS standard unduplication process, which employs a probabilistic matching strategy to assign a unique identifier to each individual patient.15 This process allows patient information in the NDW to be linked across facilities within a fiscal year; however, it does not allow for data for individual patients to be linked across years.13 As such, the data were treated as cross-sectional, with each year treated independently of the others. This approach should result in conservative estimates of variability and confidence interval limits.16
Patients aged 2 to 19 years in the I/T/U clinical population with at least 1 outpatient primary care encounter for the relevant fiscal year were eligible to be included. We defined primary care encounters on the basis of clinic type and included general, pediatric, and family practice. Patients also had to be identified by sex and as AI/AN in the NDW. Data were available for AI/AN children from all 12 IHS administrative areas, and the distribution of AI/AN children across areas was similar to the overall distribution of AI/AN people of all ages across the areas.
Outcome Variable
We selected the most recent values of height and weight measured during the same outpatient encounter in each fiscal year for each eligible patient. We calculated body mass index (BMI) as weight in kilograms divided by height in meters squared, with age- and sex-specific BMI percentiles determined by using the 2000 Centers for Disease Control and Prevention (CDC) growth charts.17 Approximately one third of eligible patients in each fiscal year did not have any values for height and weight or did not have values for both during the same encounter. We excluded children if their BMI value was identified as being biologically implausible (extremely low or high), according to CDC definitions.18
We defined overweight and obesity on the basis of BMI percentiles. Overweight is presented in 2 different ways. First, we assigned children to distinct categories of overweight versus obesity, with overweight defined as BMI greater than or equal to the 85th and less than 95th percentile for age and sex (definition 2) and obesity as BMI greater than or equal to the 95th percentile for age and sex.19 Second, to facilitate comparisons with other recent studies, overweight is also defined as BMI greater than or equal to the 85th percentile (definition 1).
We defined class 2 obesity as BMI greater than or equal to 120% of the 95th percentile or BMI greater than or equal to 35, whichever is lower based on age and sex. We operationalized class 3 obesity as BMI greater than or equal to 140% of the 95th percentile or BMI greater than or equal to 40, whichever is lower based on age and sex.20
Other Variables
Other demographic variables obtained through the NDW included date of birth and sex. We calculated age as months of age at the time of selected height and weight for calculating BMI and converted to years of age by dividing by 12 and using the integer part of the result (e.g., we analyzed 10 years and 0 days to 10 years and 364 days as age of 10 years). We divided patients into age groups of 2 to 5, 6 to 11, and 12 to 19 years, consistent with other publications of obesity data on US children.
Because obesity prevalence varies regionally, we also examined trends by the following geographic regions: Alaska, California, Northwest, Southwest subregion 1, Southwest subregion 2, Southern Plains, Northern Plains, Great Lakes, and East (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). We created these geographic regions by renaming or combining IHS areas to preserve anonymity of specific tribes.
Statistical Analysis
The data analyses for this study were undertaken with SAS/BASE and SAS/STAT software, version 9.4 of the SAS System for Windows (2002–2012, SAS Institute Inc, Cary, NC).
We calculated descriptive statistics and confidence intervals, but we performed no statistical comparisons as there was substantial overlap in the children included over the fiscal years and no way to easily identify children from year to year. We adjusted analyses for clustering of patients within geographic areas by using survey analysis procedures in SAS.
RESULTS
At least 184 000 AI/AN children aged 2 to 19 years had BMI data for each year studied, 2006 to 2015. Results are presented for 2015 alone along with trends for 2006 through 2015.
Overweight and Obesity Prevalence in 2015
For 2015, 206 834 AI/AN children aged 2 to 19 years had BMI data in the NDW that met the criteria described in Methods and were included in the analysis. Table 1 summarizes overweight and obesity prevalence by age, sex, and region for 2015.
TABLE 1—
Distribution of Demographic Characteristics and Obesity in American Indian and Alaska Native Children: Fiscal Year 2015, United States
| Characteristic | Full Sample, No. (%) | Overweight Definition 1,a % (95% CI) | Overweight Definition 2,b % (95% CI) | Obesity,c % (95% CI) | Class 2 Obesity,d % (95% CI) | Class 3 Obesity,e % (95% CI) |
| Total no. | 206 834 | 99 729 | 38 352 | 61 377 | 24 794 | 8854 |
| Total prevalence | 48.2 (47.6, 48.9) | 18.5 (18.3, 18.8) | 29.7 (29.1, 30.3) | 12.0 (11.7, 12.3) | 4.3 (4.1, 4.5) | |
| Age, y | ||||||
| 2–5 | 54 380 (26.3) | 38.3 (37.4, 39.2) | 17.5 (17.1, 17.9) | 20.7 (20.1, 21.4) | 4.3 (4.1, 4.5) | 1.0 (0.9, 1.1) |
| 6–11 | 68 547 (33.1) | 49.6 (48.8, 50.4) | 17.9 (17.6, 18.2) | 31.7 (30.9, 32.4) | 13.0 (12.5, 13.5) | 4.4 (4.1, 4.6) |
| 12–19 | 83 907 (40.6) | 53.5 (52.8, 54.2) | 19.7 (19.4, 20.0) | 33.8 (33.2, 34.5) | 16.1 (15.7, 16.6) | 6.3 (6.0, 6.6) |
| Sex | ||||||
| Female | 105 723 (51.1) | 48.1 (47.4, 48.8) | 20.2 (19.9, 20.5) | 27.9 (27.3, 28.5) | 11.0 (10.7, 11.4) | 3.9 (3.7, 4.1) |
| Male | 101 111 (48.9) | 48.3 (47.6, 49.0) | 16.8 (16.5, 17.0) | 31.5 (30.9, 32.2) | 13.0 (12.6, 13.4) | 4.7 (4.5, 4.9) |
| IHS region | ||||||
| Alaska | 11 159 (5.4) | 46.8 (44.6, 49.1) | 20.8 (19.9, 21.7) | 26.0 (24.2, 27.8) | 8.9 (8.0, 9.8) | 3.1 (2.7, 3.4) |
| California | 12 745 (6.2) | 47.9 (46.5, 49.3) | 18.3 (17.6, 19.1) | 29.6 (28.4, 30.8) | 12.5 (11.7, 13.3) | 4.7 (4.1, 5.3) |
| Northwest | 11 628 (5.6) | 52.3 (50.5, 54.2) | 20.3 (19.5, 21.1) | 32.0 (30.4, 33.6) | 12.5 (11.6, 13.5) | 4.4 (3.9, 4.9) |
| Southwest subregion 1 | 40 905 (19.8) | 46.5 (45.5, 47.5) | 18.6 (18.1, 19.0) | 27.9 (27.1, 28.8) | 10.1 (9.6, 10.6) | 3.1 (2.8, 3.3) |
| Southwest subregion 2 | 31 007 (15.0) | 54.4 (52.9, 56.0) | 18.6 (18.1, 19.1) | 35.9 (34.3, 37.4) | 15.6 (14.5, 16.7) | 5.9 (5.2, 6.7) |
| Southern Plains | 48 534 (23.5) | 43.2 (42.1, 44.3) | 17.1 (16.8, 17.5) | 26.0 (25.1, 26.9) | 10.9 (10.4, 11.5) | 3.9 (3.7, 4.2) |
| Northern Plains | 33 953 (16.4) | 48.4 (47.0, 49.8) | 18.6 (18.2, 19.1) | 29.8 (28.6, 31.0) | 11.9 (11.2, 12.6) | 4.4 (4.0, 4.8) |
| Great Lakes | 9 839 (4.8) | 53.5 (50.4, 56.6) | 19.9 (19.1, 20.7) | 33.6 (30.9, 36.3) | 13.9 (12.5, 15.4) | 5.3 (4.5, 6.1) |
| East | 7 064 (3.4) | 53.3 (51.1, 55.5) | 19.4 (18.6, 20.2) | 33.9 (32.0, 35.9) | 14.7 (13.7, 15.7) | 5.4 (4.8, 6.1) |
Note. CI = confidence interval; IHS = Indian Health Service.
Overweight definition 1: body mass index (BMI, kg/m2) ≥ 85th percentile.
Overweight definition 2: BMI ≥ 85th but < 95th percentile.
Obesity: BMI ≥ 95th percentile, includes class 2 and class 3 obesity.
Class 2 obesity: BMI ≥ 120% of the 95th percentile or 35, includes class 3 obesity.
Class 3 obesity: BMI ≥ 140% of the 95th percentile or 40.
Overall, in AI/AN children aged 2 to 19 years, the prevalence of overweight (definition 2: BMI ≥ 85th but < 95th percentile) was 18.5% and obesity was 29.7%. Children aged 2 to 5 years were the smallest group, 26.3% of children included, and had the lowest prevalence of overweight (17.5%), obesity (20.7%), and classes 2 and 3 obesity (4.3% and 1.0%, respectively). Those aged 12 to 19 years represented the majority of children included, 40.6%, and had the highest prevalence of overweight (19.7%), obesity (33.8%), and classes 2 and 3 obesity (16.1% and 6.3%, respectively). In the middle age group, 6 to 11 years, prevalence was between the younger and older age groups for all BMI categories, with 17.9% overweight, 31.7% obese, 13.0% class 2 obese, and 4.4% class 3 obese.
Obesity and overweight in AI/AN children varied by year of age, with the highest obesity prevalence observed at 11 years of age (Figure 1). The distributions of children with BMI less than the 85th percentile and those with obesity underwent reciprocal changes with increasing age, while overweight remained relatively unchanged.
FIGURE 1—
Body Mass Index Category for American Indian and Alaska Native Children by Year of Age for Fiscal Year 2015, United States
Note. BMI = body mass index (defined as weight in kilograms divided by the square of height in meters).
Slightly more girls than boys were included in the analysis, 51.1% versus 48.9%. Whereas girls had a higher prevalence of overweight, 20.2%, versus 16.8% for boys, boys had higher prevalence of obesity than girls, 31.5%, versus 27.9%. Boys also had higher prevalence of classes 2 and 3 obesity than girls, 13.0% versus 11.0% and 4.7% versus 3.9%, respectively.
Among geographic regions, the Southern Plains had the lowest prevalence of both overweight (17.1%) and obesity (26.0%, equal to Alaska), respectively. The highest prevalence of overweight was seen in Alaska (20.8%), and the highest prevalence of obesity was seen in Southwest subregion 2 (35.9%). For class 2 obesity prevalence, Alaska was lowest (8.9%), and for class 3 obesity, Alaska and Southwest subregion 1 tied for lowest at 3.1%. Southwest subregion 2 was highest for both class 2 and 3 obesity (15.6% and 5.9%).
Overweight and Obesity Trends
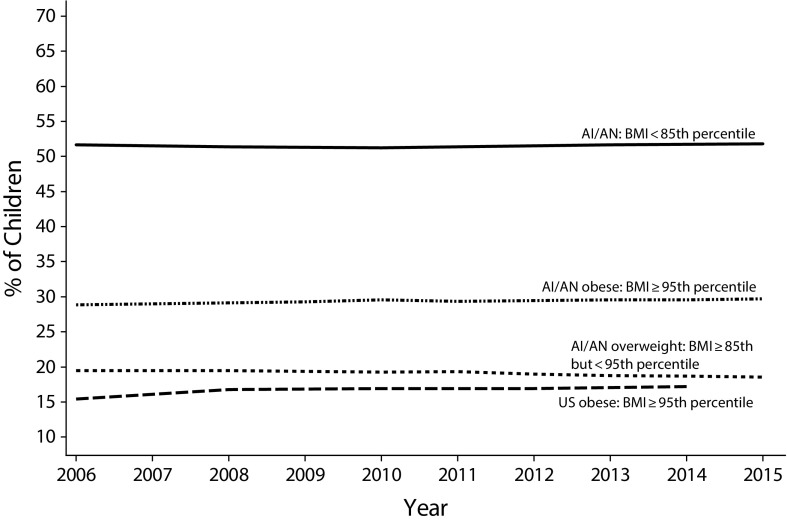
Figure 2 and Table A (available as a supplement to the online version of this article at http://www.ajph.org) present the prevalence of overweight (definition 2: BMI ≥ 85th but < 95th percentile) and obesity for AI/AN children overall by fiscal year from 2006 to 2015. In 2006, among all children aged 2 to 19 years, 19.5% were overweight and 28.9% were obese. The prevalence of overweight decreased slightly over the years to 18.5% in 2015, while obesity prevalence increased slightly to 29.7%, although the estimates for both were relatively stable. Figure 2 displays this stable linear trend over all years of the study. For both classes 2 and 3 obesity, prevalence increased slightly from 2006 to 2015, 11.0% to 12.0% for class 2 and 3.9% to 4.3% for class 3.
FIGURE 2—
Body Mass Index Categories Among American Indian and Alaska Native Children Aged 2 to 19 Years and US Obesity: 2006–2015
Notes. AI/AN = American Indian and Alaska Native; BMI = body mass index (kg/m2).
Table A (available as a supplement to the online version of this article at http://www.ajph.org) also provides prevalence estimates of overweight and obesity by age group, along with Figure 3. Children aged 12 to 19 years had the highest prevalence of overweight for all years of the study and obesity from 2011 to 2015, with those aged 6 to 11 years having higher obesity prevalence in some previous years. In children aged 2 to 5 years, there was a decrease in prevalence of overweight from 19.3% in 2006 to 17.5% in 2015. Overweight prevalence in the other 2 age groups was relatively stable: 18.6% in 2006 to 17.9% in 2015 for children aged 6 to 11 years and 20.2% in 2006 to 19.7% in 2015 for children aged 12 to 19 years. Children aged 2 to 5 years had the lowest prevalence of obesity for all years and a consistent decrease from 23.2% in 2010 to 20.7% in 2015. Among children aged 6 to 11 years, obesity prevalence was relatively steady across all years of the study (31.5% in 2006 and 31.7% in 2015), whereas we saw a slight increase in obesity in children aged 12 to 19 years, from 31.3% in 2006 to 33.8% in 2015.
FIGURE 3—
Prevalence of Overweight and Obesity Among American Indian and Alaska Native Children Aged 2 to 19 Years by Fiscal Year and Age Group: 2006–2015, United States
There was an increase in both classes of severe obesity for children aged 12 to 19 years, with class 2 rising from 14.2% in 2006 to 16.1% in 2015 and class 3 rising from 5.4% in 2006 to 6.3% in 2015. Prevalence of both classes of severe obesity among the younger age groups was lower than for those aged 12 to 19 years, and there was little change from 2006 to 2015.
Prevalence of overweight and obesity by geographic region was stable over all years of the study, with only small changes from year to year (data not shown).
DISCUSSION
We found that AI/AN children aged 2 to 19 years in this population consistently had a higher estimated prevalence of obesity than US children the same age included in NHANES (Figure 2). This finding is consistent with previous regional and tribal-specific studies.1,6 Although obesity prevalence was higher for AI/AN children than US children overall, we observed similar trends over time in prevalence of overweight and obesity in both groups.
The decrease in obesity prevalence we observed among AI/AN children aged 2 to 5 years from 2006 to 2015 is consistent with findings reported in national studies of children the same age. In particular, decreases in obesity prevalence have recently been reported among low-income preschool-aged children in 18 states between 2008 and 20119 according to data from the Pediatric Nutrition Surveillance System and among children aged 2 to 5 years in NHANES between 2003 and 2014.10
For school-aged children, the patterns we observed in AI/AN children were also similar to those in published studies for the general US population of children. In particular, analysis of data from NHANES showed no significant change in obesity prevalence between 2007–2008 and 2013–2014 for those aged 6 to 11 years, whereas a significant increase was seen for those aged 12 to 19 years between 1988–1994 and 2013–2014.10
As with total obesity, our estimates of severe obesity prevalence for AI/AN children were higher than those for US children overall. In particular, class 2 obesity prevalence among AI/AN children aged 2 to 19 years was nearly double the most recent estimate of US prevalence from NHANES reported by Skinner et al.11 (11.7% for AI/AN children in 2014 vs 6.2% for US children in 2013–2014). In our study, the prevalence of class 2 and 3 obesity increased slightly from 2006 to 2015. Similarly, Skinner et al. found significant increases in class 2 and 3 obesity among children in the United States from 1999 to 2014.11 Continued examination of class 2 and 3 obesity is warranted across all populations.
We found that AI/AN children have higher prevalence of obesity (BMI ≥ 95th percentile) than overweight (BMI ≥ 85th percentile but < 95th percentile), unlike US children overall, for whom studies have shown higher prevalence of overweight than obesity or similar prevalence for both.11,21
There are several issues to consider when one is comparing the results of this study to those for US children overall from NHANES and the Pediatric Nutrition Surveillance System. All 3 are based on direct measurement of children’s height and weight and use the same methods for calculating BMI and determining BMI percentiles. NHANES includes a nationally representative sample of children, but does not include sufficient numbers of AI/AN children to calculate valid estimates of BMI for this population. The Pediatric Nutrition Surveillance System includes a large number of children, including AI/AN children, but only those aged 2 to 4 years from low-income families who attend federally funded maternal and child health and nutrition programs. Our analysis is based on the largest number of AI/AN children reported in any study of childhood obesity and includes children of all ages from across the country. However, as our data only include AI/AN children in the IHS active clinical population, the results should not be generalized beyond the study population.
Disparities in Obesity Prevalence
The reasons for the higher obesity prevalence in AI/AN children, a relatively new phenomenon seen only in the past few generations,1,6 are not completely understood. Explanations often suggested include the fairly rapid transition from physically active subsistence and cultivation activities to a wage economy and sedentary lifestyles as traditional land bases have disappeared. Also, studies among Pima Indians have shown that in utero exposure to diabetes may mediate later obesity in the offspring through fetal adaptation to the hyperglycemic intrauterine environment.22
However, in light of recent research on the effects of stress and inadequate nutrition in utero and during early childhood on later obesity risk, the etiologies of obesity in AI/AN children almost certainly include the social determinants of health, particularly poverty. In the 2011 to 2013 American Community Survey, 29.2% of single-race AI/AN people were living in poverty in 2013, the highest rate of any racial group.23 Social injustice, trauma, stress, forced cultural change, and displacement leading to cultural disintegration have been cited as key contributors to obesity and other chronic illnesses among AI/AN people.24,25 In general populations, childhood trauma and stress have been shown to be linked to obesity and other chronic illnesses in adulthood.26,27 Indeed, many AI/AN people live in social and physical environments that place them at higher risk than many other US persons for exposure to traumatic events.25 Among children in a National Institute of Child Health and Human Development study, the experience of numerous negative life events in childhood increased risk for overweight by age 15 years.28 Another contributing factor to obesity in children living in lower-income households is food insecurity, which is the lack of dependable access to sufficient quantities of high-quality foods.29 Even before birth, stress and inadequate nutrition during pregnancy alter metabolic programming, increasing the risk for later obesity in the offspring.30
Classifying Childhood Overweight and Obesity
We used 2 definitions of childhood overweight in this study. One defined overweight inclusive of obesity (BMI ≥ 85th percentile for age and sex), which is used in other major studies10,11; the other distinguished between overweight and obesity (overweight = BMI ≥ 85th and < 95th percentile for age and sex). The latter definition was recommended by an Expert Committee in December 2007.31 Figure B (available as a supplement to the online version of this article at http://www.ajph.org) shows how AI/AN children fit into discrete BMI categories in fiscal year 2015, including overweight, obesity, and severe obesity. We think it is valuable to use an approach that assigns each child to a single BMI classification and recommend consistency in reporting to allow comparisons across studies.
Strengths and Limitations
The strengths of our study are sample size, which is substantially larger than any previous study of obesity in AI/AN children, and representation from tribes throughout the United States. In addition, these data are drawn from primary care visits for children that generally visit I/T/U facilities and are not limited to children at high risk for obesity or other medical conditions. Other studies have shown that data from electronic health records generate highly stable population estimates of BMI and obesity prevalence that are compatible with NHANES results.32
Our study has several limitations that need to be considered. Most importantly, the results cannot be generalized to all AI/AN children in the United States because there is a substantial but unknown number who do not receive care from I/T/U facilities and thus are not represented in the NDW. For fiscal year 2015, our analysis included 206 834 AI/AN children, whereas the US Census reports that there were approximately 1.97 million AI/AN children (AI/AN alone or in combination with other races) in the United States in 2013.33 However, as data on race are self-reported, many children counted by the Census as AI/AN may not meet the eligibility criteria to receive services at I/T/U facilities. In addition, some children who are eligible do not access services at these facilities.
Second, approximately one third of eligible patients in each fiscal year did not have any values for height and weight or did not have values for both during the same encounter. We excluded these children from all analyses, and it is unknown whether they are different from the included children in any way.
Third, this study is cross-sectional for each year and does not track children over time. As such, we are unable to evaluate the trajectory of BMI in AI/AN children as they age.
Finally, we performed no statistical tests as there was substantial overlap in the children included over the fiscal years and no way to link their data from year to year.
Conclusion and Public Health Implications
Obesity prevalence among AI/AN children in the IHS active clinical population is still high and higher than the general US population of children in NHANES. However, our data suggest that the overall prevalence of obesity among AI/AN children in this population may have stabilized in recent years.
To address the persistent disparity of higher obesity prevalence in AI/AN children, public health policy interventions aimed at childhood obesity should be inclusive of and culturally sensitive to AI/AN populations.
ACKNOWLEDGMENTS
K. Moore and S. Manson are supported by the Centers for American Indian and Alaska Native Health of the School of Public Health, University of Colorado Denver. K. Moore was funded by the Indian Health Service (HHSI236201300002C). S. Manson is funded by the National Institute of Diabetes, Digestive, and Kidney Diseases (1P30DK092923) and the Indian Health Service (HHSI242200400049C).
We would like to acknowledge Larry Layne, PhD, from the Indian Health Service Division of Epidemiology and Disease Prevention for his assistance with extracting data from the Indian Health Service National Data Warehouse and for preparing the map in Figure A (available as a supplement to the online version of this article at http://www.ajph.org).
HUMAN PARTICIPANT PROTECTION
The Indian Health Service determined this project to constitute public health practice and not research; therefore, no formal institutional review board approvals were required.
REFERENCES
- 1.Story M, Stevens J, Himes J et al. Obesity in American-Indian children: prevalence, consequences, and prevention. Prev Med. 2003;37(suppl 1):S3–S12. doi: 10.1016/j.ypmed.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Kelsey MM, Zaepfel A, Bjornstad P, Nadeau KJ. Age-related consequences of childhood obesity. Gerontology. 2014;60(3):222–228. doi: 10.1159/000356023. [DOI] [PubMed] [Google Scholar]
- 3.Story M, Evans M, Fabsitz R, Clay T, Holy Rock B, Broussard BA. The epidemic of obesity in American Indian communities and the need for childhood obesity-prevention programs. Am J Clin Nutr. 1999;69(4 suppl):747S–754S. doi: 10.1093/ajcn/69.4.747S. [DOI] [PubMed] [Google Scholar]
- 4.Acton KJ, Burrows NR, Moore K, Querec L, Geiss LS, Engelgau MM. Trends in diabetes prevalence among American Indian and Alaska native children, adolescents, and young adults. Am J Public Health. 2002;92(9):1485–1490. doi: 10.2105/ajph.92.9.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Obesity prevalence among low-income, preschool-aged children—United States, 1998–2008. MMWR Morb Mortal Wkly Rep. 2009;58(28):769–773. [PubMed] [Google Scholar]
- 6.Schell LM, Gallo MV. Overweight and obesity among North American Indian infants, children, and youth. Am J Hum Biol. 2012;24(3):302–313. doi: 10.1002/ajhb.22257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dabelea D, Mayer-Davis EJ, Saydah S et al. SEARCH for Diabetes in Youth Study Group. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pettitt DJ, Talton J, Dabelea D et al. SEARCH for Diabetes in Youth Study Group. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2014;37(2):402–408. doi: 10.2337/dc13-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Vital signs: obesity among low-income, preschool-aged children—United States, 2008–2011. MMWR Morb Mortal Wkly Rep. 2013;62(31):629–634. [PMC free article] [PubMed] [Google Scholar]
- 10.Ogden CL, Carroll MD, Lawman HG et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skinner AC, Perriin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity (Silver Spring) 2016;24(5):1116–1123. doi: 10.1002/oby.21497. [DOI] [PubMed] [Google Scholar]
- 12.Berger L, Correa O, Sims JG. Identifying polypharmacy among older adults using IHS national data warehouse data. IHS Prim Care Provid. 2010;35(10):238–241. [Google Scholar]
- 13.Ferucci ED, Johnston JM, Gaddy JR et al. Prevalence and incidence of systemic lupus erythematosus in a population-based registry of American Indian and Alaska Native people, 2007–2009. Arthritis Rheumatol. 2014;66(9):2494–2502. doi: 10.1002/art.38720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Indian Health Service. National Data Warehouse. Available at: http://www.ihs.gov/ndw. Accessed September 21, 2016.
- 15.Indian Health Service. Pictorial Userpop processing. Available at: https://www.ihs.gov/NDW/documents/WUPS/Pictorial_Userpop_Process_with_Text.pdf. Accessed September 21, 2016.
- 16.Sainani K. The importance of accounting for correlated observations. PM R. 2010;2(9):858–861. doi: 10.1016/j.pmrj.2010.07.482. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. CDC Growth Charts. Available at: http://www.cdc.gov/growthcharts/cdc_charts.htm. Accessed September 21, 2016.
- 18.Centers for Disease Control and Prevention. Cut-offs to define outliers in the 2000 CDC Growth Charts. Available at: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/biv-cutoffs.pdf. Accessed September 21, 2016.
- 19.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;(25):1–5. [PubMed] [Google Scholar]
- 20.Kelly AS, Barlow SE, Rao G et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–1712. doi: 10.1161/CIR.0b013e3182a5cfb3. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. 2011 Pediatric Nutrition Surveillance. Table 12D: Summary of trends in group and anemia indicators, children ages < 5 years. Available at: http://www.cdc.gov/pednss/pednss_tables/pdf/national_table12.pdf. Accessed April 13, 2015.
- 22.Pettitt DJ, Nelson RG, Saad MF, Bennett PH, Knowler WC. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care. 1993;16(1):310–314. doi: 10.2337/diacare.16.1.310. [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau. Facts for features: American Indian and Alaska Native heritage month: November 2014. Available at: http://www.census.gov/newsroom/facts-for-features/2014/cb14-ff26.html. Accessed September 21, 2016.
- 24.Joe JR, Young RS, editors. Diabetes as a Disease of Civilization: The Impact of Culture Change on Indigenous Peoples. New York, NY: Mouton de Gruyter; 1994. [Google Scholar]
- 25.Manson SM, Beals J, Klein SA, Croy CD AI-SUPERPFP Team. Social epidemiology of trauma among 2 American Indian reservation populations. Am J Public Health. 2005;95(5):851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 27.Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–e1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- 28.Lumeng JC, Wendorf K, Pesch MH et al. Overweight adolescents and life events in childhood. Pediatrics. 2013;132(6):e1506–e1512. doi: 10.1542/peds.2013-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ludwig DS, Blumenthal SJ, Willet WC. Opportunities to reduce childhood hunger and obesity: restructuring the Supplemental Nutrition Assistance Program (the food stamp program) JAMA. 2012;308(24):2567–2568. doi: 10.1001/jama.2012.45420. [DOI] [PubMed] [Google Scholar]
- 30.Entringer S, Buss C, Swanson JM et al. Fetal programming of body composition, obesity, and metabolic function: the role of intrauterine stress and stress biology. J Nutr Metab. 2012;(2012):632548. doi: 10.1155/2012/632548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barlow SE Expert Committee. Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 32.Bailey LC, Milov DE, Kelleher K et al. Multi-institutional sharing of electronic health record data to assess childhood obesity. PLoS One. 2013;8(6):e66192. doi: 10.1371/journal.pone.0066192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.US Census Bureau. Annual estimates of the resident population by sex, single year of age, race alone or in combination, and Hispanic origin for the United States: April 1, 2010 to July 1, 2013. Available at: http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed September 30, 2014.