Abstract
Objective:
Cigarette smokers are more likely to consume alcohol at higher levels and experience poorer response to treatment for alcohol problems than are nonsmokers. One previous study in university students suggests that a potential reason for the high overlap between alcohol and tobacco use is that concurrent smoking is associated with overvaluation of alcohol, as reflected in elevated behavioral economic demand. The present study sought to extend these initial findings in a community sample with heavier levels of alcohol and tobacco use.
Method:
Participants were 111 non–treatment-seeking heavy drinkers (defined as 18+/14+ drinks per week for men/women) from a larger study on alcohol pharmacotherapy mechanisms. Forty-nine participants (44%) reported regular smoking (>5 cigarettes/day). Participants completed a hypothetical alcohol purchase task assessing alcohol consumption at escalating levels of price. Covariates included demographics, drinking quantity, alcohol use disorder severity, depression, and delay discounting.
Results:
In covariate-adjusted models, smokers reported significantly higher maximum alcohol expenditures (Omax) and breakpoint price (first price suppressing consumption to zero) compared with nonsmokers. Elevated alcohol demand correlated with drinking quantity and severity in the entire sample, but not with smoking frequency or nicotine dependence among smokers only.
Conclusions:
This study offers further evidence of increased reinforcing value of alcohol among smokers in a sample of heavy drinkers from the community. Clinical implications and potential mechanisms underlying this relationship are discussed.
Alcohol and tobacco use are highly overlapping in the general population. Individuals who consume alcohol regularly are more likely to smoke cigarettes than those who do not drink (Falk et al., 2006), and heavier drinkers tend to be heavier smokers (Shiftman & Balabanis, 1995). Alcohol use disorder (AUD) is also highly comorbid with nicotine use disorder (Grant et al., 2015), and the prevalence of smoking has been reported to be as high as 90% among the AUD treatment population (Batel et al., 1995). Finally, smokers with an AUD experience worse alcohol treatment outcomes than nonsmokers (Friend & Pagano, 2005; Hintz & Mann, 2007; Karam-Hage et al., 2005).
Experimental laboratory research has helped to explain the overlap between drinking and smoking, with studies pointing to cross-commodity craving, cue reactivity, elevated reinforcement, and alcohol priming as candidate mechanisms (Drobes, 2002; Erblich et al., 2009; Karch et al., 2008; King & Epstein, 2005; McKee et al., 2006; Peloquin et al., 2014; Rohsenow et al., 1997; Sayette et al., 2005). Additional research has emphasized shared genetic liability for alcohol and nicotine use disorders (for a review, see Tyndale, 2003). More recently, the concept of behavioral economic demand, defined as the quantitative relationship between consumption of a commodity and its cost (Bickel et al., 2014; MacKillop, 2016), has been applied to examine whether elevated value of alcohol and tobacco contributes to co-use of these substances. Tobacco use may contribute to greater incentive value of alcohol rewards among drinkers who also smoke cigarettes (McKee & Weinberger, 2013). To examine demand, studies often use alcohol purchase tasks (APTs) that measure self-reported alcohol consumption across a range of prices that can be plotted via an alcohol demand curve (Murphy & MacKillop, 2006). Demand curves yield several indices of reinforcing value, including intensity (consumption at zero cost), breakpoint (price that first suppresses demand to zero), Omax (maximum expenditure), Pmax (price corresponding to Omax), and elasticity (the proportionate slope of the demand curve).
In an initial application of demand to study concurrent smoking and drinking, Yurasek et al. (2013) assessed 207 university students who were heavy drinkers, one third of whom also smoked cigarettes, using an APT. After drinking quantity, alcohol problems, gender, and depressive symptoms were controlled for, smokers reported significantly greater maximum alcohol expenditure (Omax), greater maximum inelastic price (Pmax), and higher breakpoint compared with nonsmokers. Severity of nicotine dependence was positively correlated with elevated intensity, breakpoint, and Omax, and decreased elasticity. These findings suggest that the reinforcing value of alcohol is higher among smokers even after adjusting for relevant individual differences.
The present study sought to extend these initial findings in a community sample with higher rates of smoking and drinking than those reported by Yurasek et al. (2013). We also sought to control for the potential influence of other factors outside of those examined in the previous study, namely income, education level, and an individual’s degree of delayed reward discounting (Madden & Bickel, 2009). In the latter case, liability for addictive behavior is theorized to be greatest among individuals with high demand and greater preference for immediate rewards (i.e., steeper delay discounting; Bickel et al., 2014). Consequently, we tested the hypothesis that compared with nonsmokers, heavy drinking smokers would exhibit elevated alcohol demand above and beyond drinking level and other relevant factors.
Method
Participants
Adult heavy drinkers (N =111) were drawn from a larger study examining alcohol pharmacotherapy mechanisms (Miranda et al., 2016). For inclusion in the parent study, participants were required to be at least 18 years of age and report consuming at least 18 or 14 drinks per week for men and women, respectively. Participants who were currently seeking treatment for alcohol problems or had recently received treatment were excluded. Forty-nine participants were regular smokers (i.e., >5 cigarettes/day), and 62 were nonsmokers. Ten additional participants were excluded because they only reported occasional smoking (<5 cigarettes/day). These “chippers” are considered a distinct cohort compared with heavier smokers (Shiftman & Paty, 2006).
Measures
Alcohol demand.
An APT assessed hypothetical alcohol consumption (in standard drinks) at 24 ascending prices, from $0 (free) to $35 per drink (price intervals provided in Supplemental Table S1). (Three tables and one figure appear as online-only supplemental material accompanying this article on the journal’s website.) Participants were instructed to make choices based on a typical drinking situation, with no alcohol before completing the APT, no opportunity to drink elsewhere, and no opportunity to stockpile drinks. These prices and instructions are generally comparable to previously validated APT measures (MacKillop et al., 2010; Murphy & MacKillop, 2006).
Delay discounting.
Delay discounting was assessed using the Monetary Choice Questionnaire (MCQ; Kirby et al., 1999) comprising 27 dichotomous choices between smaller–sooner and larger–later monetary rewards (range: $25–$85). An overall discounting rate (k) was generated across all items.
Alcohol and smoking variables.
Weekly alcohol consumption over the last 90 days was assessed via a Timeline Followback (Sobell & Sobell, 1992). AUD severity was determined via the Structured Clinical Interview for DSM-IV (First et al., 2002). Severity was operationalized continuously as a symptom count from both the abuse and dependence modules. Participants rated their motivation to change drinking at baseline using a readiness ruler (0 = no thought of changing drinking to 10 = taking action to change drinking). Nicotine dependence was assessed using the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton et al., 1991), within which average number of cigarettes smoked per day was also reported.
Depression.
Self-reported depressive symptoms were assessed using the Beck Depression Inventory (Beck et al., 1996).
Demographics.
A self-report questionnaire assessed sex, age, race, education, and income.
Procedure
Data were collected during a baseline assessment before administration of any pharmacotherapy or other manipulations. Smokers were permitted to smoke as usual before the start of the session but were not permitted to smoke during the session itself. Participants completed study measures either using paper-and-pencil forms or via interview. The Brown University Institutional Review Board approved this study, and participants provided informed consent.
Data analysis
Consumption and expenditure values on the APT were plotted by price to generate alcohol demand curves. Observed demand indices included intensity, breakpoint, Omax, and Pmax (Murphy & MacKillop, 2006). Elasticity of demand was modeled via the exponentiated version of the Hursh and Silberberg (2008) equation developed by Koffarnus et al. (2015). The exponentiated model is advantageous because it considers all price intervals by allowing for zero consumption values (Koffarnus et al., 2015).
Outlying values (Zs > 3.29) for untransformed variables were recoded to one unit greater than the next nonoutlier value (Tabachnick & Fidell, 2001). Intensity, Pmax, elasticity, and MCQ-k were normalized using logarithmic transformations, and breakpoint and Omax were normalized using square root transformations. Group differences for demographic variables and alcohol use were evaluated using independent sample t-tests and chi-square tests. Differences in consumption on the APT at each price interval were first examined using independent samples t-tests. Next, at the level of demand indices, hierarchical linear regression models were used to examine the association between smoking status and elevated alcohol demand. Each demand index was included as the dependent variable in separate regression models. Smoking status (1 = smoker, 0 = nonsmoker) was entered in the first step, and covariates (sex, age, income, education, drinks/week, AUD severity, depression, and delay discounting) were added in the second step. Last, Pearson correlations were used to examine associations between study variables. Analyses were conducted in IBM SPSS Statistics for Windows, Version 23 (IBM Corp., Armonk, NY) and GraphPad Prism (GraphPad Software, Inc. La Jolla, CA).
Results
Descriptive statistics
The sample was 42% female and the mean age was 36.18 years (SD = 12.86; range 18–64). Descriptive statistics by group are in Supplemental Table S2. Compared with nonsmokers (n = 62), smokers (n = 49) reported significantly lower income and education and significantly more drinks per week, greater AUD severity score, and greater delay discounting rate (ps < .05). The groups did not significantly differ on age, sex, race, motivation to change drinking, or depression (ps > .14). Smokers reported smoking an average of 12.94 cigarettes per day (SD = 5.49) and a mean FTND score of 4.39 (SD = 2.00). The exponentiated model provided an excellent fit to the individual demand curves (median R2 = .93).
Continuous associations
Greater number of drinks per week was correlated with increased intensity (r = .49, p < .01), Omax (r = .28, p < .01), decreased elasticity (r = -.21, p < .01), and steeper delay discounting (r = .32, p < .01). Higher AUD severity was associated with elevated intensity (r = .43, p < .01) and Omax (r = .28, p < .01), and decreased elasticity (r = -.20, p < .05). The complete bivariate matrix is in Supplemental Table S3. In partial correlations controlling for drinks per week, the associations between AUD severity and intensity (rpart = .35, p < .001) and Omax (rpart = .20, p < .05) remained statistically significant. Among smokers, neither FTND scores nor cigarettes per day were significantly correlated with alcohol demand or delay discounting. The individual APT indices were significantly intercorrelated, albeit at differing magnitudes (rs =.24—.91, ps < .05). Of note, consistent with other studies (Acker et al., 2012; MacKillop et al., 2010; Skidmore et al., 2014), Omax and elasticity were highly correlated (r = .91), suggesting that these indices are capturing similar aspects of demand. However, for comprehensiveness, both variables were retained in the regression analyses.
Elevations in alcohol demand based on smoking status
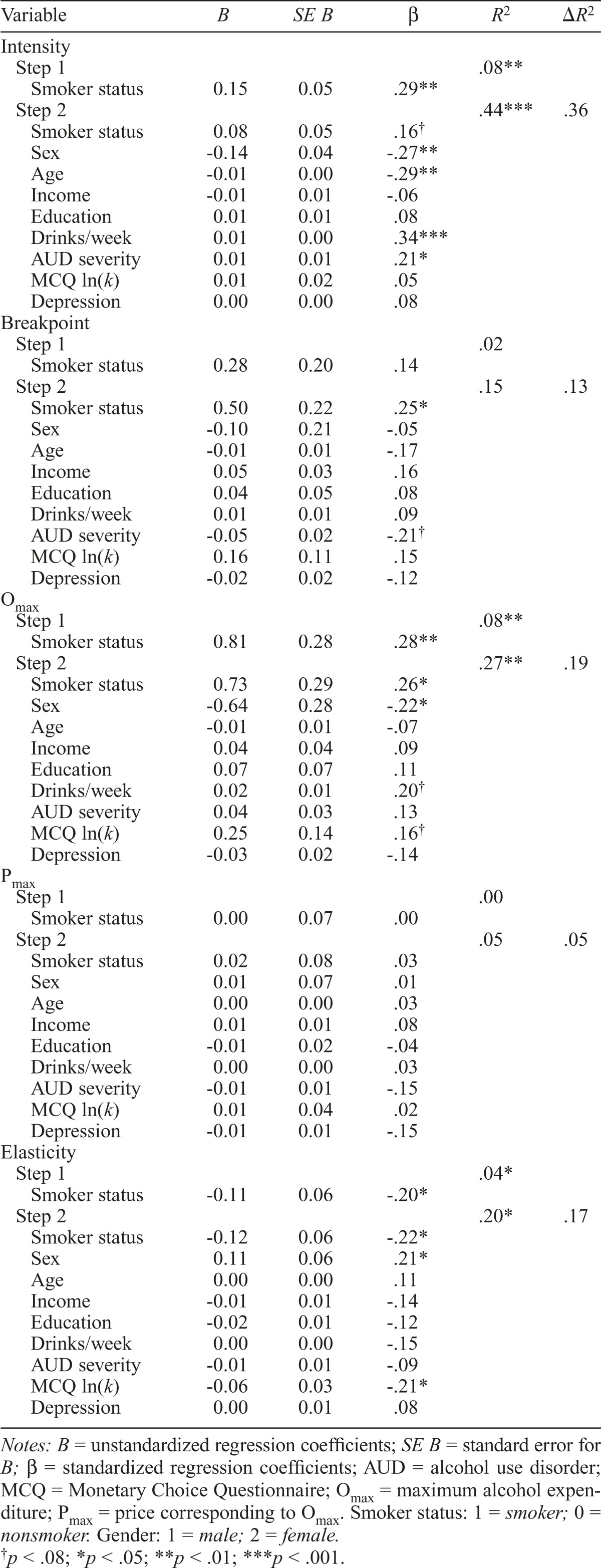
Smokers exhibited elevated alcohol consumption across the majority of price intervals (Supplemental Figure S1; price level comparisons presented in Supplemental Table S1). Results of the regression analyses are presented in Table 1. Before we controlled for covariates, being a smoker was significantly associated with higher intensity and Omax, and lower elasticity. After we added the individual difference variables, the relationship with intensity was no longer significant, but Omax and elasticity remained significant. Smoking status also predicted higher breakpoints in the covariate model. Smoking status was not associated with Pmax.
Table 1.
Hierarchical regression models predicting indices of alcohol demand
| Variable | B | SE B | β | R2 | ΔR2 |
| Intensity | |||||
| Step 1 | .88** | ||||
| Smoker status | 0.15 | 0.05 | 29** | ||
| Step 2 | .44*** | .36 | |||
| Smoker status | 0.08 | 0.05 | .16† | ||
| Sex | -0.14 | 0.04 | -.27** | ||
| Age | -0.01 | 0.00 | -.29** | ||
| Income | -0.01 | 0.01 | -.06 | ||
| Education | 0.01 | 0.01 | .08 | ||
| Drinks/week | 0.01 | 0.00 | .34*** | ||
| AUD severity | 0.01 | 0.01 | .21* | ||
| MCQ ln(k) | 0.01 | 0.02 | .05 | ||
| Depression | 0.00 | 0.00 | .08 | ||
| Breakpoint | |||||
| Step 1 | .02 | ||||
| Smoker status | 0.28 | 0.20 | .14 | ||
| Step 2 | .15 | .13 | |||
| Smoker status | 0.50 | 0.22 | .25* | ||
| Sex | -0.10 | 0.21 | -.05 | ||
| Age | -0.01 | 0.01 | -.17 | ||
| Income | 0.05 | 0.03 | .16 | ||
| Education | 0.04 | 0.05 | .08 | ||
| Drinks/week | 0.01 | 0.01 | .09 | ||
| AUD severity | -0.05 | 0.02 | -.21† | ||
| MCQ ln(k) | 0.16 | 0.11 | .15 | ||
| Depression | -0.02 | 0.02 | -.12 | ||
| Omax | |||||
| Step 1 | .08** | ||||
| Smoker status | 0.81 | 0.28 | .28** | ||
| Step 2 | .27** | .19 | |||
| Smoker status | 0.73 | 0.29 | .26* | ||
| Sex | -0.64 | 0.28 | -.22* | ||
| Age | -0.01 | 0.01 | -.07 | ||
| Income | 0.04 | 0.04 | .09 | ||
| Education | 0.07 | 0.07 | .11 | ||
| Drinks/week | 0.02 | 0.01 | .20† | ||
| AUD severity | 0.04 | 0.03 | .13 | ||
| MCQ ln(k) | 0.25 | 0.14 | .16† | ||
| Depression | -0.03 | 0.02 | -.14 | ||
| Pmax | |||||
| Step 1 | .00 | ||||
| Smoker status | 0.00 | 0.07 | .00 | ||
| Step 2 | .05 | .05 | |||
| Smoker status | 0.02 | 0.08 | .03 | ||
| Sex | 0.01 | 0.07 | .01 | ||
| Age | 0.00 | 0.00 | .03 | ||
| Income | 0.01 | 0.01 | .08 | ||
| Education | -0.01 | 0.02 | -.04 | ||
| Drinks/week | 0.00 | 0.00 | .03 | ||
| AUD severity | -0.01 | 0.01 | -.15 | ||
| MCQ ln(k) | 0.01 | 0.04 | .02 | ||
| Depression | -0.01 | 0.01 | -.15 | ||
| Elasticity | |||||
| Step 1 | .04* | ||||
| Smoker status | -0.11 | 0.06 | -.20* | ||
| Step 2 | .20* | .17 | |||
| Smoker status | -0.12 | 0.06 | -.22* | ||
| Sex | 0.11 | 0.06 | .21* | ||
| Age | 0.00 | 0.00 | .11 | ||
| Income | -0.01 | 0.01 | -.14 | ||
| Education | -0.02 | 0.01 | -.12 | ||
| Drinks/week | 0.00 | 0.00 | -.15 | ||
| AUD severity | -0.01 | 0.01 | -.09 | ||
| MCQ ln(k) | -0.06 | 0.03 | -.21* | ||
| Depression | 0.00 | 0.01 | .08 |
Notes: B = unstandardized regression coefficients; SE B = standard error for B; β = standardized regression coefficients; AUD = alcohol use disorder; MCQ = Monetary Choice Questionnaire; Omax = maximum alcohol expenditure; Pmax = price corresponding to Omax Smoker status: 1 = smoker; 0 = nonsmoker. Gender: 1 = male; 2 = female.
p < .08;
p < .05;
p < .01;
p < .001.
Discussion
This study examined demand for alcohol in a community sample of heavy drinking smokers and nonsmokers. Our results were generally consistent with the prior study in university students (Yurasek et al., 2013). Both studies found that being a smoker was associated with elevated breakpoint price and maximum expenditure (Omax) relative to being a nonsmoker. The present study also found significantly higher elasticity in smokers, but not the significant differences in Pmax that were found in the Yurasek et al. (2013) study. Of note, once chippers were excluded from the previous studies analyses, the differences in Pmax were also no longer statistically significant. Interestingly, both studies found that elevated alcohol demand was not universally elevated and appears to be specific to certain indices. Smokers tend to be willing to spend a greater amount of money on alcohol in total (Omax) and tolerate higher prices (breakpoint). Furthermore, although smokers also exhibit higher levels of intensity, in both cases, these differences were likely explained by higher drinking level or AUD severity. The lack of difference in Pmax is also not particularly unexpected, as previous studies have found this index to be less sensitive compared with other indices (Kiselica et al., 2016; Skidmore et al., 2014). Taken together, these two studies suggest that elevated alcohol demand among smokers may be more closely linked to expenditure and the impact of increasing price instead of solely due to elevated alcohol consumption.
This study makes several unique contributions to the literature. First, the consistency of the findings across studies is noteworthy given the differences in sample characteristics and methodologies. Participants in the present study were drawn from a community sample and were, on average, 15 years older and considerably heavier drinkers and smokers than were those the study by Yurasek et al. (2013). The fact that elevated demand is also observed in individuals with clinically meaningful levels of AUD severity has potential implications for treatment for alcohol problems. Screening for smoking status and level of alcohol demand at the beginning of AUD treatment may help identify individuals who may require more specialized interventions (MacKillop & Murphy, 2007; Murphy et al., 2015). Finally, this study also extends the literature by considering a number of individual difference factors that could explain elevated alcohol demand among smokers, including several variables not examined previously (i.e., income, education, and delay discounting). Of note, a number of other factors that were not considered here may also influence this relationship, including social or family characteristics or genetic liability.
Although smokers reported significantly higher alcohol demand compared with nonsmokers, prior research is somewhat ambiguous as to whether concurrent users of alcohol and tobacco may simply exhibit a general hypersensitivity to all rewards. On the one hand, nicotine administration selectively increases the amount that smokers are willing to work to obtain alcohol and the amount of alcohol consumed (e.g., Barrett et al., 2006), with comparable findings in animal models (e.g., Le et al., 2006). However, there is also evidence that nicotine increases the reinforcing value of non–alcohol-related stimuli (Attwood et al., 2012; Dawkins et al., 2006; Perkins et al., 2003). Finally, Chase et al. (2013) found that smokers did not exhibit a generalized elevation in demand across rewards (e.g., chocolate) but selectively exhibit elevations in cigarette demand. Future studies should examine demand for multiple types of drug and nondrug rewards in order to further evaluate generalized versus specific elevations in alcohol demand among smokers.
A number of limitations of this study should be considered. The design was cross-sectional and was not able to address the directionality of the relationship between smoking and drinking. The APT and MCQ were hypothetical, although there is empirical support for the validity of hypothetical behavioral economic measures (Amlung & MacKillop, 2015; Amlung et al., 2012; Johnson & Bickel, 2002; Madden et al., 2003). Although the data examined were collected at baseline, the participants were enrolled in a larger alcohol pharmacotherapy study and therefore may not be representative of all drinkers and smokers. Only a subset (44%) of the participants endorsed regular smoking, which may have constrained statistical power for the correla between behavioral economic and smoking variables. Finally, although no prohibition on smoking before the session was in place, data on acute nicotine withdrawal were not collected during the baseline session, so we were unable to address the possible influence of withdrawal symptoms.
In conclusion, this study provides additional evidence of elevated reinforcing value of alcohol in a community sample of heavy drinking smokers. Together with the study by Yurasek et al. (2013), these findings suggest that drinkers who also smoke cigarettes are less sensitive to price and other contingencies that typically influence alcohol consumption. Future research is needed to further evaluate the psychological and neurobiological mechanisms underlying elevated alcohol demand among smokers with the goal of reducing negative consequences from concurrent misuse of alcohol and nicotine and to improve treatment outcomes.
Footnotes
This study was funded by National Institutes of Health Grants AA07850, AA01723, AA019681, AA013526, DA027827, and K05019681. Michael Amlung’s role was partially supported by the Peter Boris Centre for Addictions Research. James MacKillop’s role was partially supported by the Peter Boris Chair in Addictions Research.
References
- Acker J., Amlung M., Stojek M., Murphy J. G., MacKillop J. Individual variation in behavioral economic indices of the relative value of alcohol: Incremental validity in relation to impulsivity, craving, and intellectual functioning. Journal of Experimental Psychopathology. 2012;3:423–436. doi:10.5127/jep.021411. [Google Scholar]
- Amlung M. T., Acker J., Stojek M. K., Murphy J. G., MacKillop J. Is talk “cheap”? An initial investigation of the equivalence of alcohol purchase task performance for hypothetical and actual rewards. Alcoholism: Clinical and Experimental Research. 2012;36:716–724. doi: 10.1111/j.1530-0277.2011.01656.x. doi:10.1111/j.1530-0277.2011.01656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M., MacKillop J. Further evidence of close correspondence for alcohol demand decision making for hypothetical and incen- tivized rewards. Behavioural Processes. 2015;113:187–191. doi: 10.1016/j.beproc.2015.02.012. doi:10.1016/j.beproc.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attwood A. S., Penton-Voak I. S., Goodwin C., Munafò M. R. Effects of acute nicotine and alcohol on the rating of attractiveness in social smokers and alcohol drinkers. Drug and Alcohol Dependence. 2012;125:43–48. doi: 10.1016/j.drugalcdep.2012.03.014. doi:10.1016/j.drugalcdep.2012.03.014. [DOI] [PubMed] [Google Scholar]
- Barrett S. P., Tichauer M., Leyton M., Pihl R. O. Nicotine increases alcohol self-administration in non-dependent male smokers. Drug and Alcohol Dependence. 2006;81:197–204. doi: 10.1016/j.drugalcdep.2005.06.009. doi:10.1016/j.drugalcdep.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Batel P., Pessione F., Maître C., Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90:977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. doi:10.1111/j.1360-0443.1995.tb03507.x. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., Brown G. K. San Antonio, TX: Psychological Corporation; 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- Bickel W. K., Johnson M. W., Koffarnus M. N., MacKillop J., Murphy J. G. The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology. 2014;10:641–677. doi: 10.1146/annurev-clinpsy-032813-153724. doi:10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase H. W., MacKillop J., Hogarth L. Isolating behavioural economic indices of demand in relation to nicotine dependence. Psychopharmacology. 2013;226:371–380. doi: 10.1007/s00213-012-2911-x. doi:10.1007/s00213-012-2911-x. [DOI] [PubMed] [Google Scholar]
- Dawkins L., Powell J. H., West R., Powell J., Pickering A. A double-blind placebo controlled experimental study of nicotine: I—Effects on incentive motivation. Psychopharmacology. 2006;189:355–367. doi: 10.1007/s00213-006-0588-8. doi:10.1007/s00213-006-0588-8. [DOI] [PubMed] [Google Scholar]
- Drobes D. J. Cue reactivity in alcohol and tobacco dependence. Alcoholism: Clinical and Experimental Research. 2002;26:1928–1929. doi: 10.1097/01.ALC.0000040983.23182.3A. doi:10.1111/j.1530-0277.2002.tb02506.x. [DOI] [PubMed] [Google Scholar]
- Erblich J., Montgomery G. H., Bovbjerg D. H. Script-guided imagery of social drinking induces both alcohol and cigarette craving in a sample of nicotine-dependent smokers. Addictive Behaviors. 2009;34:164–170. doi: 10.1016/j.addbeh.2008.10.007. doi:10.1016/j.addbeh.2008.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D. E., Yi H., Hiller-Sturmhöfel S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research & Health. 2006;29:162–171. [PMC free article] [PubMed] [Google Scholar]
- First M. G., Spitzer R. L., Gibbon M., Williams J. B. W. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. [Google Scholar]
- Friend K. B., Pagano M. E. Smoking cessation and alcohol consumption in individuals in treatment for alcohol use disorders. Journal of Addictive Diseases. 2005;24:61–75. doi: 10.1300/J069v24n02_06. doi:10.1300/J069v24n02_06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Saha T. D., Chou S. P., Jung J., Zhang H., Pickering R. P., Hasin D. S. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. doi:10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K. O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi:10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hintz T., Mann K. Long-term behavior in treated alcoholism: Evidence for beneficial carry-over effects of abstinence from smoking on alcohol use and vice versa. Addictive Behaviors. 2007;32:3093–3100. doi: 10.1016/j.addbeh.2007.06.006. doi:10.1016/j.addbeh.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Hursh S. R., Silberberg A. Economic demand and essential value. Psychological Review. 2008;115:186–198. doi: 10.1037/0033-295X.115.1.186. doi:10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Johnson M. W., Bickel W. K. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal for the Experimental Analysis of Behavior. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. doi:10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karam-Hage M., Pomerleau C. S., Pomerleau O. F., Brower K. J. Unaided smoking cessation among smokers in treatment for alcohol dependence. Addictive Behaviors. 2005;30:1247–1253. doi: 10.1016/j.addbeh.2004.12.003. doi:10.1016/j.addbeh.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Karch S., Jäger L., Karamatskos E., Graz C., Stammel A., Flatz W., Mulert C. Influence of trait anxiety on inhibitory control in alcohol-dependent patients: Simultaneous acquisition of ERPs and BOLD responses. Journal of Psychiatric Research. 2008;42:734–745. doi: 10.1016/j.jpsychires.2007.07.016. doi:10.1016/j.jpsychires.2007.07.016. [DOI] [PubMed] [Google Scholar]
- King A. C., Epstein A. M. Alcohol dose-dependent increases in smoking urge in light smokers. Alcoholism: Clinical and Experimental Research. 2005;29:547–552. doi: 10.1097/01.alc.0000158839.65251.fe. doi:10.1097/01.ALC.0000158839.65251.FE. [DOI] [PubMed] [Google Scholar]
- Kirby K. N., Petry N. M., Bickel W. K. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. doi:10.1037/0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Kiselica A. M., Webber T. A., Bornovalova M. A. Validity of the alcohol purchase task: A meta-analysis. Addiction. 2016;111:806–816. doi: 10.1111/add.13254. doi:10.1111/add.13254. [DOI] [PubMed] [Google Scholar]
- Koffarnus M. N., Franck C. T., Stein J. S., Bickel W. K. A modified exponential behavioral economic demand model to better describe consumption data. Experimental and Clinical Psychopharmacology. 2015;23:504–512. doi: 10.1037/pha0000045. doi:10.1037/pha0000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lệ A. D., Li Z., Funk D., Shram M., Li T. K., Shaham Y. Increased vulnerability to nicotine self-administration and relapse in alcohol-naive offspring of rats selectively bred for high alcohol intake. Journal of Neuroscience. 2006;26:1872–1879. doi: 10.1523/JNEUROSCI.4895-05.2006. doi:10.1523/JNEUROSCI.4895-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J. The behavioral economics and neuroeconomics of alcohol use disorders. Alcoholism: Clinical and Experimental Research. 2016;40:672–685. doi: 10.1111/acer.13004. doi:10.1111/acer.13004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J., Miranda R., Jr., Monti P. M., Ray L. A., Murphy J. G., Rohsenow D. J., McGeary J. E., Gwaltney C. J. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. Journal of Abnormal Psychology. 2010;119:106–114. doi: 10.1037/a0017513. doi:10.1037/a0017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J., Murphy J. G. A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug & Alco- hoi Dependence. 2007;89:227–233. doi: 10.1016/j.drugalcdep.2007.01.002. doi:10.1016/j.drugalcdep.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Madden G. J., Begotka A. M., Raiff B. R., Kastern L. L. Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. doi:10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden G. J., Bickel W. K. Washington, D.C.: American Psychological Association; 2009. Impulsivity: The behavioral and neurological science of discounting. [Google Scholar]
- McKee S. A., Krishnan-Sarin S., Shi J., Mase T., O’Malley S. S. Modeling the effect of alcohol on smoking lapse behavior. Psychopharmacology. 2006;189:201–210. doi: 10.1007/s00213-006-0551-8. doi:10.1007/s00213-006-0551-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Weinberger A. H. How can we use our knowledge of alcohol-tobacco interactions to reduce alcohol use? Annual Review of Clinical Psychology. 2013;9:649–674. doi: 10.1146/annurev-clinpsy-050212-185549. doi:10.1146/annurev-clinpsy-050212-185549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R., Jr., MacKillop J., Treloar H., Blanchard A., Tidey J. W., Swift R. M., Monti P. M. Biobehavioral mechanisms of topiramate’s effects on alcohol use: An investigation pairing laboratory and ecological momentary assessments. Addiction Biology. 2016;21:171–182. doi: 10.1111/adb.12192. doi:10.1111/adb.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J. G., Dennhardt A. A., Yurasek A. M., Skidmore J. R., Martens M. P., MacKillop J., McDevitt-Murphy M. E. Behavioral economic predictors of brief alcohol intervention outcomes. Journal of Consulting and Clinical Psychology. 2015;83:1033–1043. doi: 10.1037/ccp0000032. doi:10.1037/ccp0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J. G., MacKillop J. Relative reinforcing efficacy of alcohol among college student drinkers. Experimental & Clinical Psychopharmacology. 2006;14:219–227. doi: 10.1037/1064-1297.14.2.219. doi:10.1037/1064-1297.14.2.219. [DOI] [PubMed] [Google Scholar]
- Peloquin M. P. J., McGrath D. S., Telbis D., Barrett S. P. Alcohol and tobacco cue effects on craving in non-daily smokers. Experimental and Clinical Psychopharmacology. 2014;22:502–510. doi: 10.1037/a0038250. doi:10.1037/a0038250. [DOI] [PubMed] [Google Scholar]
- Perkins K. A., Ciccocioppo M., Jacobs L., Doyle T., Caggiula A. The subjective and reinforcing effects of visual and olfactory stimuli in alcohol drinking. Experimental and Clinical Psychopharmacology. 2003;11:269–275. doi: 10.1037/1064-1297.11.4.269. doi:10.1037/1064-1297.11.4.269. [DOI] [PubMed] [Google Scholar]
- Rohsenow D. J., Monti P. M., Colby S. M., Gulliver S. B., Sirota A. D., Niaura R. S., Abrams D. B. Effects of alcohol cues on smoking urges and topography among alcoholic men. Alcoholism: Clinical and Experimental Research. 1997;21:101–107. doi:10.1111/j.1530-0277.1997.tb03735.x. [PubMed] [Google Scholar]
- Sayette M. A., Martin C. S., Wertz J. M., Perrott M. A., Peters A. R. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychology of Addictive Behaviors. 2005;19:263–270. doi: 10.1037/0893-164X.19.3.263. doi:10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Balabanis M. Associations between alcohol and tobacco. In: Fertig J. B., Allen J. P., editors. Alcohol and tobacco: From basic science to clinical practice (NIH Publication No. 95-3931. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. pp. 17–36. [Google Scholar]
- Shiffman S., Paty J. Smoking patterns and dependence: Contrasting chippers and heavy smokers. Journal of Abnormal Psychology. 2006;115:509–523. doi: 10.1037/0021-843X.115.3.509. doi:10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- Skidmore J. R., Murphy J. G., Martens M. P. Behavioral economic measures of alcohol reward value as problem severity indicators in college students. Experimental and Clinical Psychopharmacology. 2014;22:198–210. doi: 10.1037/a0036490. doi:10.1037/a0036490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L. C., Sobell M. B. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R. Z., Allen J. P., editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Tabachnick B. G., Fidell L. S. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001. Using multivariate statistics. [Google Scholar]
- Tyndale R. F. Genetics of alcohol and tobacco use in humans. Annals of Medicine. 2003;35:94–121. doi: 10.1080/07853890310010014. doi:10.1080/07853890310010014. [DOI] [PubMed] [Google Scholar]
- Yurasek A. M., Murphy J. G., Clawson A. H., Dennhardt A. A., MacKillop J. Smokers report greater demand for alcohol on a behavioral economic purchase task. Journal of Studies on Alcohol and Drugs. 2013;74:626–634. doi: 10.15288/jsad.2013.74.626. doi:10.15288/jsad.2013.74.626. [DOI] [PMC free article] [PubMed] [Google Scholar]