Abstract
OSTEOTRANS MX® (Takiron Co., Ltd., Osaka, Japan) is a bioactive resorbable maxillofacial osteosynthetic material composed of an unsintered hydroxyapatite/poly-l-lactide composite, and its effective osteoconductive capacity has been previously documented. However, the mechanical strength of this plate system is unclear. Thus, the aim of this in vitro study was to assess its tensile and shear strength and evaluate the biomechanical intensity of different osteosynthesis plate designs after sagittal split ramus osteotomy by simulating masticatory forces in a clinical setting. For tensile and shear strength analyses, three mechanical strength measurement samples were prepared by fixing unsintered hydroxyapatite/poly-l-lactide composed plates to polycarbonate skeletal models. Regarding biomechanical loading evaluation, 12 mandibular replicas were used and divided into four groups for sagittal split ramus osteotomy fixation. Each sample was secured in a jig and subjected to vertical load on the first molar teeth. Regarding shear strength, the novel-shaped unsintered hydroxyapatite/poly-l-lactide plate had significantly high intensity. Upon biomechanical loading evaluation, this plate system also displayed significantly high stability in addition to bioactivity, with no observed plate fracture. Thus, we have clearly demonstrated the efficacy of this plate system using an in vitro model of bilateral sagittal split ramus osteotomy of the mandible.
Keywords: sagittal split ramus osteotomy, unsintered hydroxyapatite/poly-l-lactide composite plate, bioactive resorbable plate, biomechanical loading evaluation, tensile and shear strength evaluation
1. Introduction
The standard osteofixation in orthognathic surgery has been titanium osteosynthesis for many years [1,2]. Internal fixation devices have the benefits of securing the osteotomy segments, preventing displacement from muscular pull, shortening the healing period, obviating the need for maxillomandibular fixation, and preventing relapse [3]. Recently, a biologically inert resorbable plate system has been introduced to eliminate the need for a second operation for removing the fixation material. Although many previous reports have shown resorbable osteosynthesis to yield good clinical results, these platforms are not widely used due to their handling properties, intensity, and insecurity concerning their ability to maintain segments in the proper position [4].
Meanwhile, resorbable osteosynthesis technology is constantly evolving in its capacity to enhance bioresorbability and marked bioactive osteoconductivity, with new material compositions conferring different and improved in-situ behaviors. OSTEOTRANS MX® (Takiron Co., Ltd., Osaka, Japan), also called Super FIXSORB MX® in Japan, is a bioactive and totally resorbable maxillofacial osteosynthetic bone fixation material, which has been reported to exhibit clinical efficacy with relatively long-term results [5,6]. However, both the strength and stability of this plate system are still unclear. Thus, the aims of this in vitro study were to assess the physical strength of this bioactive resorbable plate system, as well as the biomechanical intensity of different osteosynthesis plate designs after sagittal split ramus osteotomy (SSRO) by simulating masticatory forces in a clinical setting.
2. Materials and Methods
2.1. Materials
Forged composites of unsintered hydroxyapatite/poly-l-lactide (u-HA/PLLA), prepared via the same means as OSTEOTRANS MX®, were processed by machining or milling treatments into various miniscrews and miniplates, which, respectively, contained 30 and 40 weight fractions of u-HA (raw hydroxyapatite, neither calcined nor sintered material) particles in composites (hereinafter referred to as u-HA 30 miniscrew and u-HA 40 miniplate).
2.2. Tensile and Shear Strength Evaluation
2.2.1. Sample Preparation
Mechanical strength measurement samples were prepared by fixing the plate with screws to the polycarbonate plate. The polycarbonate plates were fixed by different osteosynthesis methods using resorbable plate and screws to form the following groups:
a single u-HA/PLLA straight plate, fixing the plate on each side with two screws (total four screws)
double u-HA/PLLA straight plate, fixing the plate on each side with two screws (total eight screws)
one u-HA/PLLA ladder plate, fixing the plate on each side with two screws (total eight screws)
We used all plates (thickness: 1.4 mm) and screws (diameter: 2 mm; length: 8 mm). The fixed models were mounted on autographs across the chuck. This test was measured on the maximum stress and the stress at the time of 1-mm movement until the plate or screw was destroyed, and the load was applied at a test speed of 10 mm/min. Two types of strength tests (the tensile and shear strength test) were performed, each in triplicate.
2.2.2. Strength Tests
Tensile strength (St) was measured by the method illustrated in Figure 1A according to the Japanese Industrial Standard (JIS) K7113 [7]. The peak value of the profile attained by an Autograph AGS 2000 D (Shimadzu Co., Kyoto, Japan) was considered the St. The temperature and relative humidity were 23 °C and 50%, respectively.
Figure 1.
Mechanical strength models were prepared by fixing the plate with screws to the polycarbonate plate. (A). Tensile strength; (B). Shear strength.
Shear strength (Ssp) was measured by the method illustrated in Figure 1B according to JIS K7113. The peak value of the profile attained by the Autograph AGS 2000 D was considered the Ssp.
2.3. Biomechanical Loading Evaluation
2.3.1. Sample Preparation
This study involved 12 polyurethane replicas of human mandibles with bonelike consistency, with a medullar and a cortical portion (Code #8311, SYNBONE AG, Laudquart, Switzerland). SSRO mimicking the Dal Pont modification, as guided by a computer-controlled program, was performed in the mandible. The buccal cortex osteotomy of the mandible model was carried out towards the angle of the mandible from the second molars. Further bone models were prepared from bone defects so as to not be affected by bone interference [8] (Figure 2A). The bone segments were fixed by different commercially available osteosynthesis methods using a titanium miniplate/resorbable plate and monocortical screws. In all groups, bone fixation could be performed without plate bending; thus, the following groups were formed (Figure 2B):
-
(a)
a single conventional titanium straight plate (Synthes (Oberdorf, Switzerland) Compact Lock 2.0: 1.5 mm) with four screws (2.0 mm diameter × 6 mm long monocortical screws) was installed in each bone segment
-
(b)
a single u-HA/PLLA straight plate (OSTEOTRANS MX®; thickness: 1.4 mm) with four screws (2.0 mm diameter × 6 mm long monocortical screws) was installed in each bone segment
-
(c)
double u-HA/PLLA straight plates (OSTEOTRANS MX®; thickness: 1.4 mm), each with four screws (2.0 mm diameter × 6 mm long monocortical screws), were installed in each bone segment
-
(d)
one u-HA/PLLA ladder plate (OSTEOTRANS MX®; thickness: 1.4 mm) with eight screws (2.0 mm diameter × 6 mm long monocortical screws) was installed in each bone segment.
Figure 2.
(A) Sagittal split ramus osteotomy mimicking the Dal Pont modification, guided by a computer-controlled program, was performed in the mandible. The buccal cortex osteotomy of the mandible model was carried out towards the angle of the mandible from the second molars. An additional bone model was prepared from bone defects so as not to be affected by bone interference; (B) (a) Single conventional titanium plate; (b) Single u-HA/PLLA straight plate; (c) Double u-HA/PLLA straight plates; (d) u-HA/PLLA ladder plate.
2.3.2. Loading Test
After fixation, the specimens were mounted on a testing machine (AG-2kNXD, Shimazu, Japan), which was based on a biomechanical cantilever-bending model that simulates masticatory forces, and stabilized in the condylar and coronoid areas. An initial load was applied to standardize the test requirements, and the machine was then reset. A linear load in the mandibular first molar region was applied to the mandibles at a displacement speed of 10 mm/min. The resistance forces needed to displace the distal segment were transmitted from the load cell to a computer. During the maximum stress, it was difficult to compare the fixing condition for receiving the influence of such elongation of the plate and not only breakage of the plate. Therefore, we compared the amount of movement at the time of the load in the postoperative average occlusal force in reference to [9] (postoperative 1 week: 50 N; postoperative 1 month: 130 N) (Figure 3).
Figure 3.
A linear load in the mandibular first molar region was applied at a displacement speed of 10 mm/min. We compared the amount of movement at the time of the load in the postoperative average occlusal force (postoperative 1 week, about 50 N, and postoperative 1 month, about 130 N) to the reference.
2.4. Statistical Analysis
To compare the amount of movement based on the fixed material under certain conditions, we performed a Tukey–Kramer test. JMP 11.0 for Mac computers was the statistical software package used (SAS Institute Inc., Cary, NC, USA). p < 0.05 was considered statistically significant.
3. Results
3.1. Tensile and Shear Strength Evaluation
The results shown in Table 1 and Table 2 indicate that the u-HA/PLLA ladder plate group was significantly superior to other plate systems with regards to St and Ssp. In this study, all breakages were plates; there was no screw breakage.
Table 1.
Mean values and respective standard deviations for the tensile strength test for each group.
| Tensile Strength Evaluation | |||
|---|---|---|---|
| Stress at the Time of 1 mm Move (N) | |||
| Plate | Single u-HA/PLLA Plate | Double u-HA/PLLA Plate | u-HA/PLLA Ladder Plate |
| #1 | 152.3 | 300.4 | 335.5 |
| #2 | 161.5 | 302.8 | 342.2 |
| #3 | 149.9 | 294.5 | 341.4 |
| Ave. | 154.6 | 299.2 | 339.7 |
| S.D. | 6.1 | 4.3 | 3.7 |
| Maximum Stress (N) | |||
| Plate | Single u-HA/PLLA Plate | Double u-HA/PLLA Plate | u-HA/PLLA Ladder Plate |
| #1 | 198.3 | 394.7 | 459.1 |
| #2 | 190.8 | 443.7 | 446.4 |
| #3 | 202.6 | 428.5 | 464.4 |
| Ave. | 197.2 | 422.3 | 456.6 |
| S.D. | 6.0 | 25.1 | 9.3 |
Table 2.
Mean values and respective standard deviations for the shear strength test for each group.
| Shear Strength Evaluation | |||
|---|---|---|---|
| Stress at the Time of 1 mm Move (N) | |||
| Plate | Single u-HA/PLLA Plate | Double u-HA/PLLA Plate | u-HA/PLLA Ladder Plate |
| #1 | 22.4 | 46.9 | 110.2 |
| #2 | 20.6 | 50.1 | 115.1 |
| #3 | 21.1 | 48.6 | 111.8 |
| Ave. | 21.4 | 48.5 | 112.4 |
| S.D. | 1.0 | 1.6 | 2.5 |
| Maximum Stress (N) | |||
| Plate | Single u-HA/PLLA Plate | Double u-HA/PLLA Plate | u-HA/PLLA Ladder Plate |
| #1 | 63.8 | 126.8 | 187.2 |
| #2 | 63.3 | 123.3 | 174.7 |
| #3 | 63.0 | 91.5 | 171.3 |
| Ave. | 63.4 | 113.9 | 177.7 |
| S.D. | 0.4 | 19.4 | 8.4 |
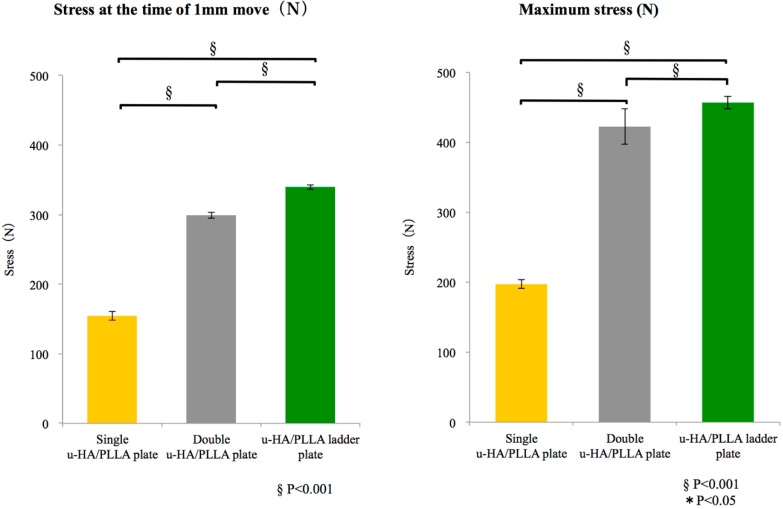
3.1.1. Tensile Strength
There was a significant difference among groups, as well as between the single u-HA/PLLA plate and double u-HA/PLLA plate groups and between the double u-HA/PLLA plate and u-HA/PLLA ladder plate groups. In particular, the u-HA/PLLA ladder plate group was significant regarding stress at the time of 1-mm movement and the maximum stress (Figure 4).
Figure 4.
Mean values and respective standard deviations for the tensile strength test for each group. Left graph shows the maximum stress, and the right graph shows the stress during 1-mm movement in tensile strength.
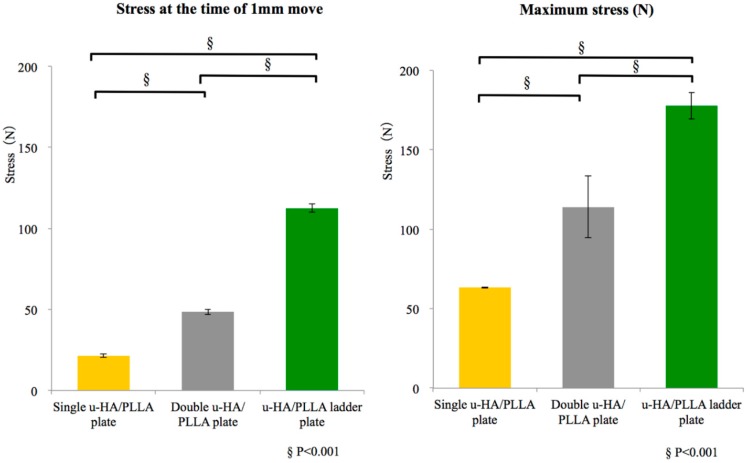
3.1.2. Shear Strength
The comparison among groups showed a significant difference between the u-HA/PLLA ladder plate and single and double u-HA/PLLA plate groups regarding stress at the time of 1-mm movement and the maximum stress. The u-HA/PLLA ladder plate group had a significantly higher mechanical strength than any other group (Figure 5).
Figure 5.
Mean values and respective standard deviations for the shear strength test for each group. Left graph shows the maximum stress, and the right graph shows the stress during 1-mm movement in shear strength.
3.2. Biomechanical Loading Evaluation
The titanium plate and single u-HA/PLLA straight plate groups deformed, and none of the plates were broken or fractured with a 50 N load. With a 130 N load, all plates in the single u-HA/PLLA group were broken. However, only one sample in the double u-HA/PLLA group fractured upon the 130 N load. The titanium plate group was accompanied by movement of large bone fragments due to the deformation of plates at 130 N load. Although the u-HA/PLLA ladder plate group moved bone fragments a little, none of the plates were broken. The single u-HA/PLLA plate group significantly moved more, compared to all the other osteosynthesis materials. This group could not be compared to the broken plates in the single and double u-HA/PLLA groups. On the other hand, the titanium plate group exhibited significantly greater movement than the u-HA/PLLA ladder plate group (Table 3, Figure 6).
Table 3.
Mean values and respective standard deviations for the amount of movement by adding load for each group.
| The Amount of Movement of 50N Load (mm) | ||||
| Plate | Single Titanium Plate | Single u-HA/PLLA Plate | Double u-HA/PLLA Plates | u-HA/PLLA Ladder Plate |
| #1 | 2.58 | 4.02 | 1.34 | 0.80 |
| #2 | 2.05 | 3.64 | 1.16 | 1.32 |
| #3 | 1.68 | 3.33 | 1.38 | 1.14 |
| Ave. | 2.10 | 3.66 | 1.29 | 1.09 |
| S.D. | 0.45 | 0.35 | 0.12 | 0.26 |
| The Amount of Movement of 130N Load (mm) | ||||
| Plate | Single Titanium Plate | Single u-HA/PLLA | Double u-HA/PLLA | u-HA/PLLA Ladder Plate |
| #1 | 7.39 | - | - | 3.33 |
| #2 | 6.67 | - | 6.21 | 3.57 |
| #3 | 7.87 | - | 5.61 | 3.49 |
| Ave. | 7.31 | - | - | 3.46 |
| S.D. | 0.60 | - | - | 0.12 |
Figure 6.
Mean values and respective standard deviations for the amount of movement by adding load for each group. Left graph shows the amount of movement with 50 N load, and the right graph shows the amount of movement with 130 N load.
4. Discussion
An overwhelming majority of orthognathic surgery patients ask for a resorbable osteosynthesis system [10,11,12]. However, a resorbable fixation plate is, on the whole, weaker than titanium and produces adverse effects in vitro [13]. Although multiple resorbable plates and screws are put in place to enhance strength, the resorbable osteosynthesis system might fracture as a result of the excessive occlusal force imposed by physical properties of the material. The rigidity and stability between fractured bone segments promoted by an osteosynthesis method are the primary factors in patient recovery, because if bone healing is not efficient, resorbable osteosynthesis methods may cause serious impairments to treatment [14]. Therefore, there is an increased interest in developing a more adequate osteosynthesis method that is bioactive with minimal morbidity.
OSTEOTRANS MX®, the bioactive and resorbable osteoconductive plate system used in this study, is made from a composite of uncalcined u-HA/PLLA. Use of this resorbable plate system obviates the need for a second surgery to remove the plate. Moreover, it has been clinically applied in various maxillofacial surgeries, such as those for trauma, fractures [15,16], and reconstruction [17]. Resorbable plates have been previously made from PLLA alone. However, PLLA osteosynthetic devices have several disadvantages, including lower dynamic strength, an inability to fuse with bone, and long resorption and replacement times [18,19,20,21]. OSTEOTRANS MX® was designed to overcome these problems, and the u-HA/PLLA composite material was developed by adding particulate resorbable uncalcined and unsintered HA to PLLA as aforementioned. Shikinami et al. [22] reported that HA crystals can bind directly to bone in vivo. In addition, it has been reported that the plates directly bonded to bone clearly displayed the effective osteoconductivity of the u-HA/PLLA plate system in maxillofacial regions [15,16]. Its early osteoconductive bioactivity can be advantageous for early functional improvement after orthognathic surgery. Because of its bioactive, osteoconductive, as well as bioresorbable properties, the u-HA/PLLA composite fixation system has immense potential and clinically advantageous and may broaden its applicability in various aspects of orthognathic surgery as a feasible next generation material.
Regarding tensile stress, both the maximum stress and the stress at the time of 1-mm movement of the double u-HA/PLLA and u-HA/PLLA ladder plate groups were significantly higher than the single u-HA/PLLA plate group. Although the number of screws across the osteotomy line was the same for the two groups, there were only two screws along the tensile direction for the single u-HA/PLLA plate group. On the other hand, because four screws fixed the double u-HA/PLLA and u-HA/PLLA ladder plate groups, these results suggested high tensile strength without stress concentration to the screw hole periphery. For shear stress, both the maximum stress and the stress at the time of 1-mm movement in the u-HA/PLLA ladder plate group was significantly higher than in the single and double u-HA/PLLA plate groups. In the shear test, the plate tends to rotate about the screw hole. Since the u-HA/PLLA ladder plate was connected at a right angle, this resulted in interference with respect to rotational movement. In addition to the vertical connection in the u-HA/PLLA ladder plate, this plate system demonstrated higher stress possibly due to 3-dimentional stress distribution functional, together with preventing rotational movement via the distal screw fixation. In this study, we further confirmed the stability of the 3-dimentional plating system was sufficient in the u-HA/PLLA ladder plate group, consistent with that in similar experimental studies on biomechanics of titanium plate systems [23,24,25]. Furthermore, with regard to operability, because the distal screw is not vertically fixed, the consistency of the plate itself can be utilized. Therefore, it is unnecessary to bend plates, which could be fixed in close contact with bone fragments. This is an excellent system that combines strength and practicality.
Many biomechanical tests have been performed to evaluate the various fixation methods used for SSRO. To simulate clinical conditions, fresh sheep mandibles [26,27], synthetic polyurethane jaw models [23], and finite element models [24] have been utilized to determine the best human mandible fixation technique. However, according to past literature, the ideal material for biomechanical loading tests is human mandibular bone [25]. Since it is difficult to obtain this material due to legal and ethical reasons, such in vitro alternative models are controversial, as they cannot exactly reproduce the function of the human bone [28]. In our study, synthetic jaw models were used because they are easy to obtain, inexpensive, allow for standardization [28,29], and are amenable in evaluating the mechanical characteristics of fixation materials prior to their application in humans [27].
In this study, the biomechanical test was performed using a two-point model, which has been utilized in numerous studies for comparing the different osteosynthesis systems [23,25,27]. Since the weakness of this model may be that it does not accurately simulate the masticatory muscles, it has been previously suggested to use a three-point mechanical test [26]. However, Ribeiro-Junior et al. [30] believed that both two- and three-point models were poor substitutes for evaluating the fixation systems used in mandibular sagittal osteotomies due to their inability to truly reflect human mandibular function. Nevertheless, our experiments were performed using a two-point model, and we used the bilateral mandibular model to approximate the human condition without a hemimandibular model.
Currently, the trend for fixation after an SSRO is to use titanium miniplates with monocortical screws [31,32]. During the fracture healing period, premature failure of the plates must be prevented. The loads transmitted through the plates should not exceed the limit of strength of the material [33]. Bending of the bone plate for SSRO surgery, particularly in a resorbable plate system, has not been widely demonstrated. In our study, one of the experimental resorbable plates did not withstand a 50 N load. On the other hand, fixation of two plates had higher strength, compared to a one plate fixation. In previous biomechanical investigations, the parallel position of the two plates confers enhanced strength for SSRO fixation [34]. The double miniplates as a scheme of a two-point fixation largely enhance stability and decrease latent failure since stress is distributed over the two plates [31,32]. However, in the double resorbable plate fixation, large bone fragmental movement caused plate fractures in one sample without sufficient strength for a 130 N load, although the other two samples bore the movement. In addition, the u-HA/PLLA ladder plate showed a much higher strength than the titanium plate and double resorbable plate fixation. For the u-HA/PLLA ladder plate, its two arms hold the two fixation sites via a double step, similar to that in the 3-dimensional plating system. This allows a double miniplate-like action through a single construct with stress distributed over two fixation sites. In addition to the vertical connection in the u-HA/PLLA ladder plate, as shown by our shear test results, this plate system had higher stress due to preventing rotational movement via distal screw fixation. We have shown that such a plate system is a biomechanically effective plate structure for SSRO surgery.
This study will significantly contribute to the understanding of the biomechanical actions involved in chewing, loading, and movement by simulating masticatory forces with different prototypes. It will also help in understanding the kinematics associated with osteosynthesis in a clinical setting. Although this study revealed that the novel-shaped u-HA/PLLA ladder plate system could exert stability immediately after the SSRO osteotomy, all the osteosynthesis systems showed the unstable conditions of biomechanical intensity. This could be the first step in understanding the behavior of these osteosynthesis devices. In future research, it would be necessary to monitor the clinical stability of various osteosynthetic fixation systems including bioresorbable systems because these devices can change biomechanical properties and intensity with the interaction of the surrounding tissues and the process of bioresorbability.
In addition, since an effective method for reproducing mandibular function is yet to be developed, we should not assume that the biomechanical results observed in this study would elicit an immediate change in the current application of osteosynthesis methods. Here, it should be noted that the complex oromandibular interactions between the mandible and adjacent musculatures are taken into consideration. However, we believe that the findings of the present study could support and stimulate an active discussion about future clinical applications in orthognathic surgery.
5. Conclusions
The u-HA/PLLA ladder plate system significantly optimized the resistance and stability of plate fixation in vitro as compared with a single plate fixing standard SSRO. Due to its bioactive, osteoconductive, as well as bioresorbable properties, this u-HA/PLLA composite fixation system has much potential to be widely and safely applied as a next generation material in orthognathic surgery.
Acknowledgments
We declare no financial support from Takiron Co, Ltd., Osaka, Japan. Some analyses, such as tensile and shear strength and biomechanical loading evaluations, were done at the Takiron Medical Institute, Kobe, Japan.
Abbreviations
| u-HA | unsintered hydroxyapatite; |
| PLLA | poly-l-lactide-acid; |
| SSRO | sagittal split ramus osteotomy |
Author Contributions
Shintaro Sukegawa participated in the design of the study and experiments, acquisition of data, and drafted the manuscript. Takahiro Kanno performed and coordinated the study and contributed to the drafting of the manuscript. Yoshiki Manabe analyzed the data. Kenichi Matsumoto, Yuka Sukegawa-Takahashi, and Masanori Masui collected the data. Yoshihiko Furuki conceived the study and participated in its design. All authors approved the final version of the manuscript prior to submission.
Conflicts of Interest
The authors declare no competing interests.
References
- 1.Buijs G.J., van Bakelen N.B., Jansma J., de Visscher J.G.A.M., Hoppenreijs T.J.M., Bergsma J.E., Stegenga B., Bos R.R.M. A randomized clinical trial of biodegradable and titanium fixation systems in maxillofacial surgery. J. Dent. Res. 2012;91:299–304. doi: 10.1177/0022034511434353. [DOI] [PubMed] [Google Scholar]
- 2.Van Bakelen N.B., Buijs G.J., Jansma J., de Visscher J.G.A.M., Hoppenreijs T.J.M., Bergsma J.E., Stegenga B., Bos R.R.M. Decision-making considerations in application of biodegradable fixation systems in maxillofacial surgery—A retrospective cohort study. J. Craniomaxillofac. Surg. 2014;42:417–422. doi: 10.1016/j.jcms.2013.05.032. [DOI] [PubMed] [Google Scholar]
- 3.Erkmen E., Simşek B., Yücel E., Kurt A. Three-dimensional finite element analysis used to compare methods of fixation after sagittal split ramus osteotomy: Setback surgery-posterior loading. Br. J. Oral Maxillofac. Surg. 2005;43:97–104. doi: 10.1016/j.bjoms.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Al-Moraissi E.A., Ellis E. Biodegradable and Titanium Osteosynthesis Provide Similar Stability for Orthognathic Surgery. J. Oral Maxillofac. Surg. 2015;73:1795–1808. doi: 10.1016/j.joms.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 5.Shikinami Y., Matsusue Y., Nakamura T. The complete process of bioresorption and bone replacement using devices made of forged composites of raw hydroxyapatite particles/poly l-lactide (F-u-HA/PLLA) Biomaterials. 2005;26:5542–5551. doi: 10.1016/j.biomaterials.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Sukegawa S., Kanno T., Kawai H., Shibata A., Takahashi Y., Nagatsuka H., Furuki Y. Long-Term Bioresorption of Bone Fixation Devices Made from Composites of Unsintered Hydroxyapatite Particles and Poly-l-Lactide. J. Hard Tissue Biol. 2015;24:219–224. doi: 10.2485/jhtb.24.219. [DOI] [Google Scholar]
- 7.Oe M. Comparison of Mechanical Stiffness of Titanium and Biodegradable Osteofixation Systems. J. Jpn. Soc. Plastic Reconstr Surg. 2013;33:219–227. [Google Scholar]
- 8.Nakakuki K., Kurohara K., Arikawa K., Harada K. Biomechanical Loading Evaluation of Unsintered Hydroxyapatite/poly-l-lactic Acid Plate in Bilateral Sagittal Split Ramus Osteotomy. Jpn. J. Jaw Deform. 2014;24:211–217. doi: 10.5927/jjjd.24.211. [DOI] [Google Scholar]
- 9.Harada K., Watanabe M., Ohkura K., Enomoto S. Measure of bite force and occlusal contact area before and after bilateral sagittal split ramus osteotomy of the mandible using a new pressure-sensitive device: A preliminary report. J. Oral Maxillofac. Surg. 2000;58:370–373. doi: 10.1016/S0278-2391(00)90913-3. [DOI] [PubMed] [Google Scholar]
- 10.Kiely K.D., Wendfeldt K.S., Johnson B.E., Haskell B.S., Edwards R.C. One-year postoperative stability of LeFort I osteotomies with biodegradable fixation: A retrospective analysis of skeletal relapse. Am. J. Orthod. Dentofacial Orthop. 2006;130:310–316. doi: 10.1016/j.ajodo.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 11.Turvey T.A., Bell R.B., Tejera T.J., Proffit W.R. The use of self-reinforced biodegradable bone plates and screws in orthognathic surgery. J. Oral Maxillofac. Surg. 2002;60:59–65. doi: 10.1053/joms.2002.28274. [DOI] [PubMed] [Google Scholar]
- 12.Turvey T.A., Bell R.B., Phillips C., Proffit W.R. Self-Reinforced Biodegradable Screw Fixation Compared With Titanium Screw Fixation in Mandibular Advancement. J. Oral Maxillofac. Surg. 2006;64:40–46. doi: 10.1016/j.joms.2005.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahn Y.-S., Kim S.-G., Baik S.-M., Kim B.-O., Kim H.-K., Moon S.-Y., Lim S.-H., Kim Y.-K., Yun P.-Y., Son J.-S. Comparative study between resorbable and nonresorbable plates in orthognathic surgery. J. Oral Maxillofac. Surg. 2010;68:287–292. doi: 10.1016/j.joms.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Yamashita Y., Mizuashi K., Shigematsu M., Goto M. Masticatory function and neurosensory disturbance after mandibular correction by bilateral sagittal split ramus osteotomy: A comparison between miniplate and bicortical screw rigid internal fixation. Int. J. Oral Maxillofac. Surg. 2007;36:118–122. doi: 10.1016/j.ijom.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Sukegawa S., Kanno T., Katase N., Shibata A., Takahashi Y., Furuki Y. Clinical Evaluation of an Unsintered Hydroxyapatite/Poly-L-Lactide Osteoconductive Composite Device for the Internal Fixation of Maxillofacial Fractures. J. Craniofac. Surg. 2016;27:1391–1397. doi: 10.1097/SCS.0000000000002828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanno T., Tatsumi H., Karino M., Yoshino A., Koike T., Ide T., Sekine J. Applicability of an Unsintered Hydroxyapatite Particles/Poly-L-Lactide Composite Sheet with Tack Fixation for Orbital Fracture Reconstruction. J. Hard Tissue Biol. 2016;25:329–334. doi: 10.2485/jhtb.25.329. [DOI] [Google Scholar]
- 17.Sukegawa S., Kanno T., Hotaka K., Akane S., Matsumoto K., Sukegawa-Takahashi Y., Sakaida K., Nagatsuka H., Furuki Y. Surgical Treatment and Dental Implant Rehabilitation after the Resection of an Osseous Dysplasia. J. Hard Tissue Biol. 2016;25:437–441. doi: 10.2485/jhtb.25.437. [DOI] [Google Scholar]
- 18.Matsusue Y., Yamamuro T., Yoshii S., Oka M., Ikada Y., Hyon S., Shikinami Y. Biodegradable screw fixation of rabbit tibia proximal osteotomies. J. Appl. Biomater. 1991;2:1–12. doi: 10.1002/jab.770020102. [DOI] [PubMed] [Google Scholar]
- 19.Matsusue Y., Nakamura T., Iida H., Shimizu K. A long-term clinical study on drawn poly-L-lactide implants in orthopaedic surgery. J. Long. Term. Eff. Med. Implants. 1997;7:119–137. [PubMed] [Google Scholar]
- 20.Bergsma J.E., de Bruijn W.C., Rozema F.R., Bos R.R., Boering G. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials. 1995;16:25–31. doi: 10.1016/0142-9612(95)91092-D. [DOI] [PubMed] [Google Scholar]
- 21.Landes C.A., Ballon A., Tran A., Ghanaati S., Sader R. Segmental stability in orthognathic surgery: Hydroxyapatite/Poly-l-lactide osteoconductive composite versus titanium miniplate osteosyntheses. J. Craniomaxillofac. Surg. 2014;42:930–942. doi: 10.1016/j.jcms.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Shikinami Y., Hata K., Okuno M. Ultra-high-strength resorbable implants made from bioactive ceramic particles/polylactide composites. Bioceramics. 1996;9:391–394. [Google Scholar]
- 23.Van Sickels J.E., Peterson G.P., Holms S., Haug R.H. An in vitro comparison of an adjustable bone fixation system. J. Oral Maxillofac. Surg. 2005;63:1620–1625. doi: 10.1016/j.joms.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 24.Lee J.-Y., Lee J.-W., Pang K.-M., Kim H.-E., Kim S.-M., Lee J.-H. Biomechanical evaluation of magnesium-based resorbable metallic screw system in a bilateral sagittal split ramus osteotomy model using three-dimensional finite element analysis. J. Oral Maxillofac. Surg. 2014;72:402.e1–402.e13. doi: 10.1016/j.joms.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Tharanon W. Comparison between the rigidity of bicortical screws and a miniplate for fixation of a mandibular setback after a simulated bilateral sagittal split osteotomy. J. Oral Maxillofac. Surg. 1998;56:1055–1058. doi: 10.1016/S0278-2391(98)90255-5. [DOI] [PubMed] [Google Scholar]
- 26.Ozden B., Alkan A., Arici S., Erdem E. In vitro comparison of biomechanical characteristics of sagittal split osteotomy fixation techniques. Int. J. Oral Maxillofac. Surg. 2006;35:837–841. doi: 10.1016/j.ijom.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Olivera L.B., Sant’ Ana E., Manzato A.J., Guerra F.L.B., Arnett G.W. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: A study in sheep mandibles. J. Appl. Oral Sci. 2012;20:419–426. doi: 10.1590/S1678-77572012000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bredbenner T.L., Haug R.H. Substitutes for human cadaveric bone in maxillofacial rigid fixation research. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000;90:574–580. doi: 10.1067/moe.2000.111025. [DOI] [PubMed] [Google Scholar]
- 29.Sener I., Arıcı S., Bereket C., Tek M. In vitro biomechanical evaluation of modified plating techniques for bilateral sagittal split ramus osteotomy in mandibular advancement. J. Craniofac. Surg. 2012;23:1573–1576. doi: 10.1097/SCS.0b013e31826100ec. [DOI] [PubMed] [Google Scholar]
- 30.Ribeiro-Junior P.D., Magro-Filho O., Shastri K.A., Papageorge M.B. In vitro biomechanical evaluation of the use of conventional and locking miniplate/screw systems for sagittal split ramus osteotomy. J. Oral Maxillofac. Surg. 2010;68:724–730. doi: 10.1016/j.joms.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 31.Ueki K., Hashiba Y., Marukawa K., Alam S., Nakagawa K., Yamamoto E. Skeletal stability after mandibular setback surgery: Bicortical fixation using a 2.0-mm locking plate system versus monocortical fixation using a nonlocking plate system. J. Oral Maxillofac. Surg. 2008;66:900–904. doi: 10.1016/j.joms.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 32.Erkmen E., Simşek B., Yücel E., Kurt A. Comparison of different fixation methods following sagittal split ramus osteotomies using three-dimensional finite elements analysis. Part 1: Advancement surgery-posterior loading. Int. J. Oral Maxillofac. Surg. 2005;34:551–558. doi: 10.1016/j.ijom.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Tams J., Otten B., van Loon J.P., Bos R.R. A computer study of fracture mobility and strain on biodegradable plates used for fixation of mandibular fractures. J. Oral Maxillofac. Surg. 1999;57:973–981. doi: 10.1016/S0278-2391(99)90020-4. [DOI] [PubMed] [Google Scholar]
- 34.Aymach Z., Nei H., Kawamura H., Bell W. Biomechanical evaluation of a T-shaped miniplate fixation of a modified sagittal split ramus osteotomy with buccal step, a new technique for mandibular orthognathic surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011;111:58–63. doi: 10.1016/j.tripleo.2010.03.028. [DOI] [PubMed] [Google Scholar]