Abstract
Angiography and endovascular embolization play an important role in controlling acute arterial upper gastrointestinal hemorrhage, particularly when endoscopic intervention fails to do so. In our case, the patient presented with recurrent life-threatening bleed in spite of multiple prior endoscopic interventions and gastroduodenal artery embolization. Our teaching points focus on the role of angiography in acute upper gastrointestinal bleed and when to conduct empiric embolization, while reviewing the supraduodenal artery as an atypical but important potential culprit for refractory upper gastrointestinal bleed.
Keywords: Interventional radiology, Angiography, Endovascular embolization, UGIB
Introduction
The utilization of angiography has decreased in the setting of acute arterial upper gastrointestinal bleed (UGIB) due to the increased use of computed tomography angiography. However, angiography and transarterial embolization remain an important tool in controlling acute arterial UGIB, especially when endoscopic intervention fails to do so [1].
Case report
We report the case of an 86-year-old male, who presented with recurrent UGIB, including melena and bright red blood per rectum, status post recent endoscopic proximal duodenal ulcer clipping and subsequent angiography with gastroduodenal artery (GDA) embolization.
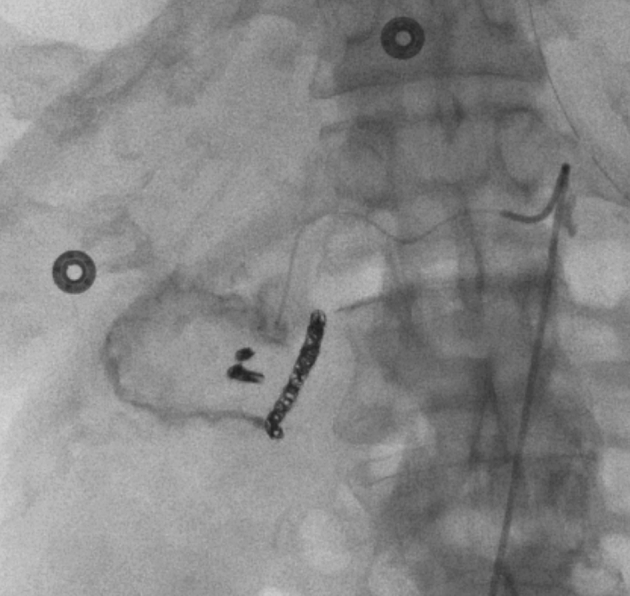
Initial digital subtraction angiography of the celiac trunk did not reveal any active extravasation (Fig. 1).
Fig. 1.

Digital subtraction angiography (DSA) of the celiac trunk showed the region of interest involving the proximal duodenum (circle), with endoscopically placed clips in the vicinity and previously coil-embolized GDA. GDA, gastroduodenal artery.
Next, digital subtraction angiography of the superior mesenteric artery was performed, without revealing any bleeding supplied by the inferior pancreaticoduodenal artery or the gastroduodenal arcade (Fig. 2).
Fig. 2.

DSA of the superior mesenteric artery (SMA) with previously embolized GDA showed no active bleeding. DSA, digital subtraction angiography; GDA, gastroduodenal artery.
The celiac trunk was then revisited, given that the territory’s proximity to the site of the UGIB identified by the endoscopic duodenal clips. The adjacent supraduodenal artery (SDA) was identified as the potential culprit for the bleed (Fig. 3). SDA usually supplies the proximal duodenum, and in our case, it wraps around the duodenal clips. This SDA also showed an aberrant origin, arising from the right gastric artery, which is less than 8% in all cases [2]. The SDA was selected by a microcatheter (Fig. 3) and empirically embolized with Embozene Microspheres (Boston Scientific, Marlborough, MA) (Fig. 4), in spite of the lack of obvious active extravasation. SDA angiography demonstrates hyperemia and delayed venous clearance suggestive of underlying vascular injury. Patient remained hemodynamically stable and did not require further blood transfusion in the immediate postprocedural period.
Fig. 3.
With the main catheter in the celiac trunk, SDA microcatheter superselective angiography demonstrated hyperemia and delayed venous clearance suggestive of underlying vascular injury. SDA, supraduodenal artery.
Fig. 4.
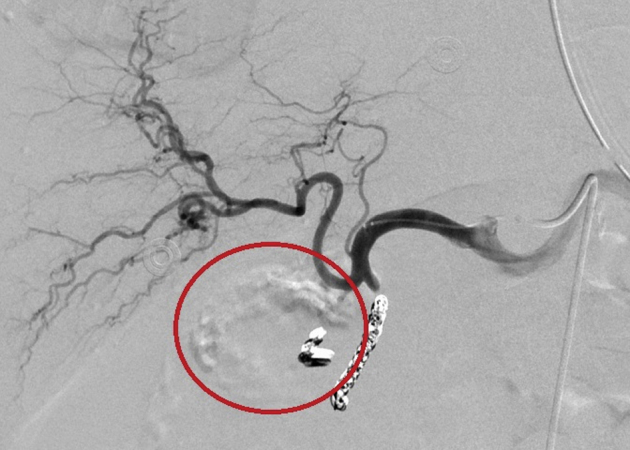
Postembolization using Embozene Microspheres: DSA of the common hepatic artery showed total stasis of the aberrant SDA. DSA, digital subtraction angiography; SDA, supraduodenal artery.
Discussion
Indications
The main indications for angiography in the setting of UGIB include the followings [3], [4], with our patient fitting in the second category.
-
•
Limited endoscopic visibility from vigorous bleeding
-
•
Bleeding not controlled by endoscopic therapy
-
•
Medical or anatomic reasons limiting endoscopic route, such as previous gastric bypass surgery
-
•
Qualified endoscopic operator not available
Empiric embolization
Empiric embolization may be pursued if prior endoscopy localizes the suspected bleeding site, and there is high suspicion for continued bleeding from that site. In our case, empiric embolization of the supraduodenal artery, which wrapped around the preexisting duodenal clips placed during prior endoscopy, was effective to control patient’s UGIB. Empiric embolization has been shown to be effective in controlling UGIB, particularly in refractory cases [3], [5]. Having the endoscopic clips as a target was of paramount importance to guide the prophylactic therapy in this case. While prophylactic GDA embolization is a common intervention in UGIB without angiographic evidence of bleeding, other duodenal branches may be the culprits and must be considered if GDA embolization has failed to control the bleeding, especially after ruling out retrograde bleeding via the pancreaticoduodenal arcade, which can be interrogated via SMA angiography.
Supraduodenal artery
As one of the arterial branches supplying the duodenum, the supraduodenal artery can be a potential culprit for UGIB. However, it has a variety of origins. The possible origins of the supraduodenal artery and the associated frequencies are listed as follows [2]: GDA, 26%; common or proper hepatic artery, 20%; left hepatic artery, 20%; right hepatic artery, 13%; cystic artery, 10%; and right gastric artery, 8%. In this case, the supraduodenal artery branches off an aberrant right gastric artery, which arises from the right hepatic artery. The anatomy of this case is reviewed in detail (Fig. 5).
Fig. 5.
DSA of celiac trunk (C) shows an aberrant origin of the right gastric artery (7), arising from the right hepatic artery (6), gives rise to an aberrant supraduodenal artery (8) supplying the proximal duodenum and wrapping around the duodenal clips (D). S, splenic artery; 1, left gastric artery; 2, accessory left hepatic artery arising from (1); 3, common hepatic artery; 4, coil-embolized GDA; 5, left hepatic artery, small in caliber due to (2); 9, right gastric artery proper; 10, middle hepatic artery; 11, right hepatic artery proper. GDA, gastroduodenal artery.
The patient remained hemodynamically stable since the last embolization of the aberrant SDA. Although SDA is an uncommon source for UGIB, knowing this variant is important clinically, especially in cases of refractory gastrointestinal bleed status post endoscopic intervention and GDA embolization.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Miller M., Smith S.P. Angiographic diagnosis and endovascular management of nonvariceal gastrointestinal hemorrhage. Gastroenterol Clin North Am. 2005;34(4):735–752. doi: 10.1016/j.gtc.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi H.F., Albanèse E.F. The supraduodenal artery. Surg Radiol Anat. 1989;11:37–40. doi: 10.1007/BF02102244. Image courtesy of David, Liu MD. [DOI] [PubMed] [Google Scholar]
- 3.Ramaswamy R.S., Choi H.W., Mouser H.C., Narsinh K.H., McCammack K.C., Treesit T. Role of interventional radiology in the management of acute gastrointestinal bleeding. World J Radiol. 2014;6(4):82–92. doi: 10.4329/wjr.v6.i4.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eriksson L., Ljungdahl M., Sundbom M., Nyman R. Transcatheter arterial embolization versus surgery in the treatment of upper gastrointestinal bleeding after therapeutic endoscopy failure. J Vasc Interv Radiol. 2008;19(10):1413–1418. doi: 10.1016/j.jvir.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Dixon S., Chan V., Shrivastava V., Anthony S., Uberoi R., Bratby M. Is there a role for empiric gastroduodenal artery embolization in the management of patients with active upper GI hemorrhage? Cardiovasc Intervent Radiol. 2013;36:970–977. doi: 10.1007/s00270-012-0511-0. [DOI] [PubMed] [Google Scholar]



