Abstract
Study Design
Systematic review.
Objective
The aim of this study was to review the techniques, indications, and outcomes of minimally invasive surgery (MIS) and separation surgery with subsequent radiosurgery in the treatment of patients with metastatic spine disease.
Summary of Background Data
The utilization of MIS techniques in patients with spine metastases is a growing area within spinal oncology. Separation surgery represents a novel paradigm where radiosurgery provides long-term control after tumor is surgically separated from the neural elements.
Methods
PubMed, Embase, and CINAHL databases were systematically queried for literature reporting MIS techniques or separation surgery in patients with metastatic spine disease. PRISMA guidelines were followed.
Results
Of the initial 983 articles found, 29 met inclusion criteria. Twenty-five articles discussed MIS techniques and were grouped according to the primary objective: percutaneous stabilization (8), tubular retractors (4), mini-open approach (8), and thoracoscopy/endoscopy (5). The remaining 4 studies reported separation surgery. Indications were similar across all studies and included patients with instability, refractory pain, or neurologic compromise. Intraoperative variables, outcomes, and complications were similar in MIS studies compared to traditional approaches, and some MIS studies showed a statistically significant improvement in outcomes. Studies of mini-open techniques had the strongest evidence for superiority.
Conclusions
Low-quality evidence currently exists for MIS techniques and separation surgery in the treatment of metastatic spine disease. Given the early promising results, the next iteration of research should include higher-quality studies with sufficient power, and will be able to provide higher-level evidence on the outcomes of MIS approaches and separation surgery.
Keywords: endoscopy, epidural spinal cord compression, metastatic spinal cord compression, minimally invasive surgery, mini-open, pathologic fracture, percutaneous instrumentation, separation surgery, spinal metastases, stereotactic radiosurgery, thoracoscopy, tubular retractor, VATS, video-assisted thoracoscopic surgery
Stabilization of the spinal column and decompression of the spinal cord constitute primary surgical goals in patients with spinal metastases. Decreasing the invasiveness of surgery has potential to reduce hospitalization duration, rehabilitation requirements, and risk of complications. As a result, minimally invasive surgery (MIS) has been increasingly practiced for spinal metastases and has been shown to decrease operative morbidity. MIS techniques include kyphoplasty/vertebroplasty,1–7 percutaneous fixation,8–11 tubular retractors,12–14 mini-open procedures,15,16 and thoracoscopy/endoscopy.17,18
Although MIS techniques aim to decrease the extent of the approach, integration of stereotactic radiosurgery (SRS) or stereotactic body radiotherapy (SBRT) has lead to a decrease in the amount of tumor removal required. Delivery of potentially ablative SRS doses largely obviates the need to maximize tumor excision. However, as the most common pattern of failure is within the epidural space in close proximity to the spinal cord, the goal of “separation surgery” is to excise the epidural tumor and provide circumferential decompression of the spinal cord, thereby ensuring optimal tumor radiation dosing and maximizing the efficacy of SRS.
The goal of the current systematic review is to discuss recent MIS techniques for patients with metastatic spine disease and review the indications, principles, and outcomes of patients undergoing separation surgery and subsequent radiotherapy. These two objectives will be addressed through the following questions:
Question #1: What are the indications, options, and outcomes for MIS in the treatment of patients with spinal metastases?
Question #2: What are the indications and outcomes for separation surgery in the treatment of patients with spinal metastases?
Materials and Methods
Electronic Literature Search
A comprehensive and systematic review of the literature was conducted using PubMed, Embase, and CINAHL databases in combination with a review of eligible article bibliographies. The MEDLINE search terms included the MeSH terms and keywords for the following terms: “minimally invasive spine spinal tumor” OR “percutaneous instrumentation” OR “mini-open spine surgery” OR “minimal access spine surgery” OR “spine thoracoscopy” OR “spine endoscopy” OR “separation surgery” OR “spine oncology” OR “spine metastases.”
Data Extraction
Given the two similar but disparate research questions, data extraction was divided by question. For question 1, several mean or median operative variables were collected from each study: operative technique, operative time (OT), estimated blood loss (EBL), length of stay (LOS), and complication rate (CR). For question 2, local recurrence (LR) and overall survival (OS) were collected. Follow-up, indications, and neurologic outcomes were collected for all articles.
Study Eligibility
A set of a priori inclusion and exclusion criteria was determined for each research objective. For both questions, the following inclusion criteria were used: published between 1950 and 2016, English or translated into the English language, patients 18 years or older, randomized or non-randomized controlled trials, cohort studies, case-control studies, or case series. For both questions, the following exclusion criteria were imposed: review or editorial, primary/intradural tumors, no surgical intervention, laboratory studies, or cases series of less than five patients.
For the first question involving MIS techniques, it was decided a priori to exclude studies of kyphoplasty/vertebroplasty. This area has been extensively studied with several recent comprehensive reviews.3,19,20 With respect to the second question, studies with specific mention of separation surgery were included, as described in earlier reviews.21,22 Given the significant overlap between MIS techniques, reports were grouped according to the primary technique of interest. Studies of less than five metastatic tumor patients were excluded from the initial search,23–25 as were those with significant patient overlap.26,27
The abstracts of all articles that matched the search terms and inclusion/exclusion criteria were evaluated by a reviewer (SLZ), and full-text versions of all relevant articles were obtained. These articles were studied for information relevant to the research questions, and their reference lists were closely searched for additional articles that may have been overlooked in the original search. Any disagreement on article inclusion was handled by a consensus between two additional reviewers (IL and DMS). After finalizing the included studies, data were extracted from each article by a single reviewer (SLZ) and confirmed by the two additional reviewers (IL and DMS). GRADE guidelines were used for evaluation of evidence quality, recommendation formulation, and recommendation strength as seen in Box 1.28,29 Observational publications included were all initially classified as low quality of evidence.
Box 1. How to Use and Interpret GRADE Recommendations.
| Strength of Recommendation | Interpretation |
|---|---|
| Strong | Can be confidently applied to all or almost all patients. |
| Clinicians apply an intervention in all or almost all circumstances without a thorough review of the evidence and factors, and with an informing, but not necessarily detailed, discussion with the patient. | |
| Weak | Can be applied to most patients, but not all patients. |
| Clinicians consider fundamental variables such as the quality of evidence, risk, and benefit of the intervention, their experience, cost-effectiveness, and most importantly, patient preferences, thus, often resulting in a shared decision-making process with the patient. |
Statistical Analysis
Given the limited number of articles and study heterogeneity, medians and ranges were used to summarize all numerical data points. All descriptive statistical analyses were performed in Microsoft Excel (Microsoft Corp, Redmond, WA) version 14.6.1 and STATA version 14 (StataCorp LP, College Station, TX).
Results
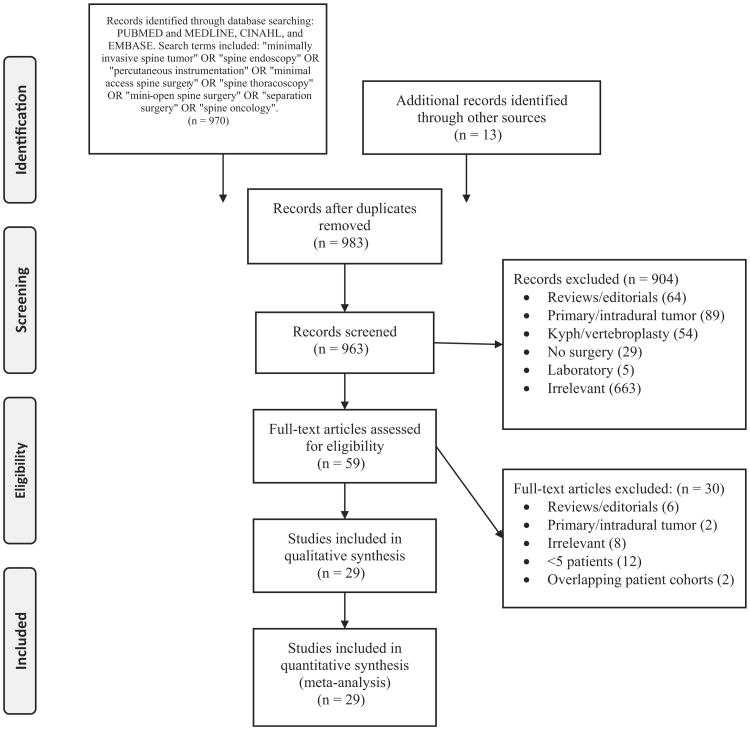
A total of 29 articles met the a priori inclusion criteria. Search results are summarized Figure 1. Twenty-five articles pertained to MIS surgical techniques and are summarized in Supplemental Digital Content, Table 1, http://links.lww.com/BRS/B215.8,9,22,24–28 Four articles reported outcomes after separation surgery and are summarized in Supplemental Digital Content, Table 2, http://links.lww.com/BRS/B215.
Figure 1.
Flow chart of included studies.
Question #1: What are the MIS indications and options in the treatment of patients with spinal metastases?
1.1 Percutaneous stabilization
Indications, OT/EBL/ LOS, complications, outcomes
Eight studies including 278 patients focused exclusively on percutaneous stabilization, with an additional seven articles that focused on other MIS techniques. The one nonpedicle screw study reported the placement of iliac screws in five patients with lumbosacral disease.30 Indications for stabilization ranged from spinal cord compression requiring an extensive resection and long fusion to a single unstable vertebral body requiring a short-segment fusion only. Instability alone was a surgical indication regardless of radiation sensitivity, often determined by an unstable or indeterminate spinal instability neoplastic score (SINS) score and refractory pain.31 The median average OT (range) was 154 minutes (72–413) among the six studies that reported this measure. Median EBL and LOS (range) were 128 cc (73–1400) and 7.6 days (5.2–12.6), among seven and five studies, respectively. The median complication rate was 9% (0%–18%) in seven studies. Complications were rare and included hardware failure, infection, and the need for additional decompression. One study reported two significant complications: medial screw placement causing complete paraplegia and cement extravasation causing a transient ASIA C injury that fully recovered to ASIA E after reoperation.11 Several studies reported expeditious time to radiation treatment.30 All studies reported significant improvement in pain most often measured with VAS scores, and in some cases improvement in kyphosis and scoliosis (Supplemental Digital Content, Table 3, http://links.lww.com/BRS/B215).
1.2 Tubular retractors
Indications, OT/EBL/LOS, complications, outcomes
Tubular retractors were the focus of 4 studies in 33 patients, with an additional 3 articles using tubular or table-mounted retractors that focused on other MIS techniques. Indications for tubular retractor use were primarily for decompression purposes, which included the posterior elements only, a unilateral transpedicular partial corpectomy,12,14 or a bilateral transpedicular, complete corpectomy.13 Only 2/4 studies reported mean OT (134 and 170 minutes); median EBL (range) was 335cc (50–400) across the 3 studies. LOS was reported in 2 studies at 6 and 7 days. Complication rate was reported in 3 studies, with 2 reporting 0% and the remaining study reporting a single urinary tract infection (UTI) as the only complication. All studies reported improvement in neurologic status with ASIA and Frankel grade, in addition to improvement in pain and functional outcome measured with the Oswestry disability index (ODI) (Supplemental Digital Content, Table 4, http://links.lww.com/BRS/B215).
1.3 Mini-open
Indications, OT/EBL/LOS, complications, outcomes
A total of eight studies focused principally on the mini-open approach in 232 patients, with an additional 3 articles that focused on other MIS techniques. Indications included MESCC with neurologic deficit and/or intractable pain. Interestingly, one study mentioned that the time of surgery dictated the choice of mini-open—scheduled cases during elective hours had the necessary staff and equipment for a mini-open case, whereas emergent cases at night or on the weekend were relegated to an open approach.15 Median OT was 132 minutes (75–452), and median EBL was 291 cc (68–1058) and median LOS was 6 days (2.9–7.2). The median complication rate was 7.3% (0%–29%), and included infection, dural tear, and UTI. A femoral fracture was seen during an early study of lateral surgery.33 Four studies directly compared the mini-open approach to a standard open decompression and fusion.15,16,33,34 Using one study as an example, the results overwhelmingly favored the mini-open group with decreased EBL (916.7 vs. 1697cc P = 0.019) and LOS (7.4 vs. 11.4, P = 0.001).15 Postoperative pain levels and need for opioids were also decreased in the mini-open group, and a trend of decreased perioperative complications was seen in the mini-open group, though this did not reach statistical significance.15 Quality of life was also found to be higher in the mini-open group in one study that assessed patient-reported outcome metrics.16
1.4 Thoracoscopy/endoscopy
Indications, OT/EBL/ LOS, complications, outcomes
Five studies of 32 patients were identified that used thoracoscopic/endoscopic techniques. Specific indications included patients with thoracic metastatic lesions and/or anterior disease that required direct anterior decompression, in addition to being judged unsuitable for an open thoracotomy. The indication to use an endoscope for a posterolateral decompression was to adequately visualize the spinal cord during the final stages of a corpectomy.35 Median OT was 306 minutes (258–360) and median EBL was 1050 cc (610–1120). Median LOS was 6.5 days (6.3–8.1) with a median complication rate of 11% (0%–14%). Complications ranged from intercostal neuralgia to atelectasis and prolonged requirement for chest tube. The complication rates were similar to those of open surgery and other MIS techniques.
Question #2: What are the indications for separation surgery in the treatment of patients with spinal metastases?
Indications
Indications for separation surgery were determined by the NOMS decision framework, which include the algorithm of neurologic, oncologic, mechanical, and systemic principles.36 The primary indications were radioresistant tumors or previously irradiated tumors causing high-grade MESCC.37,38
Complications/neurologic outcomes/survival
Four studies were identified that reported separation surgery in 286 patients. Three studies examined standard surgical intervention before radiotherapy, whereas one recent study evaluated laser interstitial thermotherapy (LITT).39 Three studies had long-term follow-up, except the LITT study that reported perioperative outcomes with a short median follow-up time of 4.7 months. The mean local failure rate was 17.1% with a mean time to local recurrence of 13.6 months. One study reported 1-year OS rates of 78% in patients with systemic therapy post-radiosurgery compared to 56% in patients without systemic therapy (P = 0.02).
In terms of multivariable predictors of LC and OS, delivery of high-dose per fraction radiosurgery (SRS) provided significantly better LC compared to low-dose hypofractionated SRS. Patients who received 24 to 30 Gy in three fractions had 1-year LC of 96%, and patients with single-fraction treatment of 24 Gy had 1-year LC of 91%, compared to 1-year LC of only 77% after lower-dose per fraction dosing.37 Additionally, an SRS dose of 18 to 26 gy in one to two fractions and postop epidural Bilsky grade of 0/1 versus 1/2 predicted improved LC, and systemic therapy post-SRS predicted improved OS.40 Of note, the study of LITT in 11 patients included quality of life and pain scores. The mean VAS pain score decreased from 6.2 to 2.8 at 60 days (P = 0.01), and the VAS quality of life measure remained stable from 60% preoperatively to 70% at 60 days (P = 0.31). Complications were minimal in all four studies and included hardware failure in a selected group of patients, only some of which required reoperation.37,39–41 Of note, some patients developed toxicity because of SRS, which included GI, GU, and musculoskeletal manifestations.40
Discussion
Among patients with metastatic spine disease, high complication rates and prolonged hospitalizations may negate any benefits of surgery.42,43 MIS approaches for the treatment of spinal metastases have grown significantly in recent years. The same goals of decompression, stabilization, and tumor control can be accomplished through smaller corridors that minimize iatrogenic pain and surgical morbidity.42,44 The goal of this systematic review was to describe MIS techniques, indications, and outcomes after separation surgery in patients harboring spinal metastases.
MIS Surgical Techniques
Stabilization
As mentioned, MIS stabilization indications range from isolated instability with or without debilitating pain to an adjunct in a larger decompressive operation. In the case of weakened bone secondary to tumor infiltration or osteoporosis, pedicle screw cement augmentation is recommended, as screw pullout or pedicle fracture in a short construct can be potentially catastrophic.52,53 Radiation can be started within 1 week of surgery, and sometimes 2 to 3 days.54 Outcomes were excellent as measured by pain, neurologic status, and complications; however, significant complications can still occur.11 Percutaneous screw placement is perhaps the workhorse of MIS for patients with spine metastases and was the most common technique utilized.
Decompression
Across all decompressive techniques, similar rates of neurologic improvement were seen, thus providing evidence that the same surgical goals can be accomplished through the use of tubular retractors, mini-open approaches, and thoracoscopic/endoscopic assistance. This was best portrayed in studies directly comparing the mini-open and traditional open approach.15,16,33,34 All four studies showed improvement among intraoperative, perioperative, and postoperative outcomes, with some statistically significant trends. Even PRO metrics showed superior improvements in quality and function in the mini-open group. Though direct comparison studies were not available for tubular retractor and thoracoscopic/ endoscopic approaches, similar positive results were reported.
Efforts
Given the evidence for successful outcomes, MIS options should be pursued in high-risk patients, such as those with low performance status or complex oncological comorbidities. Less invasive options may provide otherwise nonoperative patients a surgical option to treat their pain and/or neurologic deficit in the remaining months of life. However, surgeons must be cautioned that sometimes MIS options can require more time because of the necessary imaging technology; thus, open approaches may still be required in certain circumstances.
Evidence
The low-quality data presented support the continued application and exploration of MIS techniques. Except for comparative studies addressing the mini-open technique, the remaining studies are largely feasibility reports, although they do report favorable outcomes with respect to perioperative measures and wound complications. Similar and sometimes improved outcomes of pain, neurologic, and tumor control were seen with a low risk of complications. Mini-open has the strongest supporting evidence among MIS techniques.
Separation Surgery
Indications
Integration of radiosurgery in the treatment of spinal metastatic tumors, with evidence for long-term tumor control, has lead to a shift in surgical goals and the advent of separation surgery.55–57 Effective SRS requires adequate dose delivery to the tumor with minimal risk of toxicity to the spinal cord; hence, the need for separation between the two structures, which can be provided by separation surgery. The current recommendations for patients with high-grade MESCC by the Spine Oncology Study Group (SOSG) are to undergo surgical decompression followed by RT.58 Additionally, SOSG recommendations for radioresistant tumors are to undergo radiosurgery.58 The indications across all four studies of separation surgery were similar and included patients with high-grade MESCC, pathologic fracture, or mechanical instability.41 More invasive techniques that carry morbidity such as staged procedures, thoracotomy or retroperitoneal approaches, or corpectomies with anterior column reconstruction are rarely required. In addition to decreased LOS, EBL, LOS, and CR, the decreased morbidity may lead to improve LC and OS rates. Though the data to prove superiority of separation surgery to traditional techniques do not yet exist, long-term results in the current four studies are promising.
Outcomes
Two of four studies reported improved pain, and one study reported improved or stable neurologic function. In terms of predictors of LC and OS, significant predictors were higher dose-per-fraction SRS, adequate spinal cord decompression measured using postoperative Bilsky grade, and systemic therapy post-SRS.37,40 Complications were minimal, but examples of radiation toxicity were seen. Given the high doses and quick time to SRS, certain toxicities must be monitored and further explored.40 A criticism of separation surgery is the anterior column reconstruction required after tumor debulking is not adequately provided. This theoretical concern was addressed in a large study of 318 patients undergoing separation surgery.26 Amankulor et al26 reportednine cases of hardware failure (2.8%) that each presented with pain requiring reoperation. Risk factors for failure included iatrogenic chest wall destabilization after rib resection, construct lengths spanning six segments, and women. Overall, separation surgery with posterior-only stabilization was deemed safe given the low percentage of hardware failures that occurred.
Evidence
Low-quality data support the use of separation surgery in patients with MESCC followed by radiosurgery owing to the small number of studies available. Though the current studies of separation surgery report neurologic, survival, and recurrence outcomes that are comparable to previous approaches, studies directly comparing the outcomes of separation surgery to techniques such as vertebrectomy are lacking. The benefit of this approach may be realized through careful attention to complication profiles of the techniques and to patient-reported outcome measure metrics, where patients report improved functional status and overall satisfaction.
Limitations
Given the growing area of novel techniques, most studies are exploratory with low sample sizes. The overall quality of evidence was low, except for mini-open techniques. An additional confounder is publication bias. Newer techniques will be published more often than older ones, and this may falsely represent existing practice. The heterogeneity of studies across many different populations is also a limitation of any systematic review. Moreover, certain studies were missing vital information pertinent to data points evaluating MIS techniques and separation surgery. In addition, a bias may exist toward larger, more specialized centers with the means to invest in novel surgical technology, and these results may not apply to smaller, less specialized surgical settings.
Question #1: What are the indications, options, and outcomes for MIS in the treatment of patients with spinal metastases?
MIS provides safe and effective stabilization and decompression in patients with spinal metastases. Patients with mechanical instability benefit from percutaneous stabilization techniques using spinal instrumentation and cement. Patients with spinal cord compression benefit from MIS access using mini-open approach, tubular retractors, or thoracoscopy/endoscopy.
Strength of Recommendation: Strong
Quality of Evidence: Low
Question #2: What are the indications and outcomes for separation surgery in the treatment of patients with spinal metastases?
Separation surgery in conjunction with postoperative radiosurgery provides safe and effective tumor control. Patients with high-grade MESCC secondary to radioresistant tumors benefit from separation surgery followed by radiosurgery.
Strength of Recommendation: Strong
Quality of Evidence: Low
Supplementary Material
Key Points.
Current techniques for MIS in spinal metastases include percutaneous instrumentation, tubular retractors, mini-open approaches, and thoracoscopy/endoscopy.
Separation surgery is a novel treatment paradigm that includes surgical separation of tumor from the neural elements, with long-term tumor control achieved through radiosurgery.
MIS techniques and separation surgery provide effective and safe surgical options for patients with spinal metastases.
Acknowledgments
AOSpine International funds were received in support of this work.
Relevant financial activities outside the submitted work: board membership, grants.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
Supplemental digital content is available for this article. Direct URL citations appearing in the printed text are provided in the HTML and PDF version of this article on the journal's Web site (www.spinejournal.com).
References
- 1.Dalbayrak S, Onen MR, Yilmaz M, et al. Clinical and radiographic results of balloon kyphoplasty for treatment of vertebral body metastases and multiple myelomas. J Clin Neurosci. 2010;17:219–24. doi: 10.1016/j.jocn.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Qian Z, Sun Z, Yang H, et al. Kyphoplasty for the treatment of malignant vertebral compression fractures caused by metastases. J Clin Neurosci. 2011;18:763–7. doi: 10.1016/j.jocn.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 3.Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011;12:225–35. doi: 10.1016/S1470-2045(11)70008-0. [DOI] [PubMed] [Google Scholar]
- 4.Zheng L, Chen Z, Sun M, et al. A preliminary study of the safety and efficacy of radiofrequency ablation with percutaneous kyphoplasty for thoracolumbar vertebral metastatic tumor treatment. Med Sci Monit. 2014;20:556–63. doi: 10.12659/MSM.889742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tseng YY, Lo YL, Chen LH, et al. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of pain induced by metastatic spine tumor. Surg Neurol. 2008;70(suppl 1):S1:78–83. doi: 10.1016/j.surneu.2008.08.078. discussion S1:-4. [DOI] [PubMed] [Google Scholar]
- 6.Tseng YY, Yang ST, Tu PH, et al. Minimally invasive vertebroplasty in the treatment of pain induced by spinal metastatic tumor. Minim Invasive Neurosurg. 2008;51:280–4. doi: 10.1055/s-0028-1082328. [DOI] [PubMed] [Google Scholar]
- 7.Weitao Y, Qiqing C, Songtao G, et al. Open vertebroplasty in the treatment of spinal metastatic disease. Clin Neurol Neurosurg. 2012;114:307–12. doi: 10.1016/j.clineuro.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 8.Gerszten PC, Monaco EA., 3rd Complete percutaneous treatment of vertebral body tumors causing spinal canal compromise using a transpedicular cavitation, cement augmentation, and radiosurgical technique. Neurosurg Focus. 2009;27:E9. doi: 10.3171/2009.9.FOCUS09184. [DOI] [PubMed] [Google Scholar]
- 9.Rao PJ, Thayaparan GK, Fairhall JM, et al. Minimally invasive percutaneous fixation techniques for metastatic spinal disease. Orthop Surg. 2014;6:187–95. doi: 10.1111/os.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mendel E, Bourekas E, Gerszten P, et al. Percutaneous techniques in the treatment of spine tumors: what are the diagnostic and therapeutic indications and outcomes? Spine (Phila Pa 1976) 2009;34:S93–100. doi: 10.1097/BRS.0b013e3181b77895. [DOI] [PubMed] [Google Scholar]
- 11.Versteeg AL, Verlaan JJ, de Baat P, et al. Complications after percutaneous pedicle screw fixation for the treatment of unstable spinal metastases. Ann Surg Oncol. 2016;23:2343–9. doi: 10.1245/s10434-016-5156-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harel R, Doron O, Knoller N. Minimally invasive spine metastatic tumor resection and stabilization: new technology yield improved outcome. Biomed Res Int. 2015;2015:948373. doi: 10.1155/2015/948373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Massicotte E, Foote M, Reddy R, et al. Minimal access spine surgery (MASS) for decompression and stabilization performed as an out-patient procedure for metastatic spinal tumours followed by spine stereotactic body radiotherapy (SBRT): first report of technique and preliminary outcomes. Technol Cancer Res Treat. 2012;11:15–25. doi: 10.7785/tcrt.2012.500230. [DOI] [PubMed] [Google Scholar]
- 14.Deutsch H, Boco T, Lobel J. Minimally invasive transpedicular vertebrectomy for metastatic disease to the thoracic spine. J Spinal Disord Tech. 2008;21:101–5. doi: 10.1097/BSD.0b013e31805fea01. [DOI] [PubMed] [Google Scholar]
- 15.Lau D, Chou D. Posterior thoracic corpectomy with cage reconstruction for metastatic spinal tumors: comparing the mini-open approach to the open approach. J Neurosurg Spine. 2015;23:217–27. doi: 10.3171/2014.12.SPINE14543. [DOI] [PubMed] [Google Scholar]
- 16.Miscusi M, Polli FM, Forcato S, et al. Comparison of minimally invasive surgery with standard open surgery for vertebral thoracic metastases causing acute myelopathy in patients with short- or mid-term life expectancy: surgical technique and early clinical results. J Neurosurg Spine. 2015;22:518–25. doi: 10.3171/2014.10.SPINE131201. [DOI] [PubMed] [Google Scholar]
- 17.Kan P, Schmidt MH. Minimally invasive thoracoscopic approach for anterior decompression and stabilization of metastatic spine disease. Neurosurg Focus. 2008;25:E8. doi: 10.3171/FOC/2008/25/8/E8. [DOI] [PubMed] [Google Scholar]
- 18.Kan P, Schmidt MH. Minimally invasive thoracoscopic resection of paraspinal neurogenic tumors: technical case report. Neurosurgery. 2008;63 doi: 10.1227/01.neu.0000335011.30252.c4. ONSE54; discussion ONSE. [DOI] [PubMed] [Google Scholar]
- 19.De la Garza-Ramos R, Benvenutti-Regato M, Caro-Osorio E. Vertebroplasty and kyphoplasty for cervical spine metastases: a systematic review and meta-analysis. Int J Spine Surg. 2016;10:7. doi: 10.14444/3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroeder JE, Ecker E, Skelly AC, et al. Cement augmentation in spinal tumors: a systematic review comparing vertebroplasty and kyphoplasty. Evid Based Spine Care J. 2011;2:35–43. doi: 10.1055/s-0031-1274755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bilsky MH, Laufer I, Matros E, et al. Advanced lung cancer: aggressive surgical therapy vertebral body involvement. Thorac Surg Clin. 2014;24:423–31. doi: 10.1016/j.thorsurg.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Fisher C, Batke J. Editorial: separation surgery. J Neurosurg Spine. 2013;18:205–6. doi: 10.3171/2012.10.SPINE12743. [DOI] [PubMed] [Google Scholar]
- 23.Nzokou A, Weil AG, Shedid D. Minimally invasive removal of thoracic and lumbar spinal tumors using a nonexpandable tubular retractor. J Neurosurg Spine. 2013;19:708–15. doi: 10.3171/2013.9.SPINE121061. [DOI] [PubMed] [Google Scholar]
- 24.Tamburrelli FC, Scaramuzzo L, Genitiempo M, et al. Minimally invasive treatment of the thoracic spine disease: completely percutaneous and hybrid approaches. Minim Invasive Surg. 2013;2013:508920. doi: 10.1155/2013/508920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muhlbauer M, Pfisterer W, Eyb R, et al. Minimally invasive retroperitoneal approach for lumbar corpectomy and anterior reconstruction. Technical note. J Neurosurg. 2000;93:161–7. doi: 10.3171/spi.2000.93.1.0161. [DOI] [PubMed] [Google Scholar]
- 26.Amankulor NM, Xu R, Iorgulescu JB, et al. The incidence and patterns of hardware failure after separation surgery in patients with spinal metastatic tumors. Spine J. 2014;14:1850–9. doi: 10.1016/j.spinee.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 27.Moulding HD, Elder JB, Lis E, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine. 2010;13:87–93. doi: 10.3171/2010.3.SPINE09639. [DOI] [PubMed] [Google Scholar]
- 28.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 29.Neumann I, Santesso N, Akl EA, et al. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016;72:45–55. doi: 10.1016/j.jclinepi.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 30.Liu G, Hasan MY, Wong HK. Minimally invasive iliac screw fixation in treating painful metastatic lumbosacral deformity: a technique description and clinical results. Eur Spine J. 2016:1–9. doi: 10.1007/s00586-016-4387-6. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 31.Moussazadeh N, Rubin DG, McLaughlin L, et al. Short-segment percutaneous pedicle screw fixation with cement augmentation for tumor-induced spinal instability. Spine J. 2015;15:1609–17. doi: 10.1016/j.spinee.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 32.Zairi F, Arikat A, Allaoui M, et al. Minimally invasive decompression and stabilization for the management of thoracolumbar spine metastasis. J Neurosurg Spine. 2012;17:19–23. doi: 10.3171/2012.4.SPINE111108. [DOI] [PubMed] [Google Scholar]
- 33.Huang TJ, Hsu RW, Li YY, et al. Minimal access spinal surgery (MASS) in treating thoracic spine metastasis. Spine (Phila Pa 1976) 2006;31:1860–3. doi: 10.1097/01.brs.0000225995.56028.46. [DOI] [PubMed] [Google Scholar]
- 34.Fang T, Dong J, Zhou X, et al. Comparison of mini-open anterior corpectomy and posterior total en bloc spondylectomy for solitary metastases of the thoracolumbar spine. Journal of neurosurgery Spine. 2012;17:271–9. doi: 10.3171/2012.7.SPINE111086. [DOI] [PubMed] [Google Scholar]
- 35.McLain RF. Spinal cord decompression: an endoscopically assisted approach for metastatic tumors. Spinal Cord. 2001;39:482–7. doi: 10.1038/sj.sc.3101194. [DOI] [PubMed] [Google Scholar]
- 36.Laufer I, Rubin DG, Lis E, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013;18:744–51. doi: 10.1634/theoncologist.2012-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laufer I, Iorgulescu JB, Chapman T, et al. Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radio-surgery: outcome analysis in 186 patients. J Neurosurg Spine. 2013;18:207–14. doi: 10.3171/2012.11.SPINE12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moussazadeh N, Laufer I, Yamada Y, et al. Separation surgery for spinal metastases: effect of spinal radiosurgery on surgical treatment goals. Cancer Control. 2014;21:168–74. doi: 10.1177/107327481402100210. [DOI] [PubMed] [Google Scholar]
- 39.Tatsui CE, Stafford RJ, Li J, et al. Utilization of laser interstitial thermotherapy guided by real-time thermal MRI as an alternative to separation surgery in the management of spinal metastasis. J Neurosurg Spine. 2015;23:1–12. doi: 10.3171/2015.2.SPINE141185. [DOI] [PubMed] [Google Scholar]
- 40.Al-Omair A, Masucci L, Masson-Cote L, et al. Surgical resection of epidural disease improves local control following postoperative spine stereotactic body radiotherapy. Neuro-oncology. 2013;15:1413–9. doi: 10.1093/neuonc/not101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bate BG, Khan NR, Kimball BY, et al. Stereotactic radiosurgery for spinal metastases with or without separation surgery. J Neurosurg Spine. 2015;22:409–15. doi: 10.3171/2014.10.SPINE14252. [DOI] [PubMed] [Google Scholar]
- 42.Gerszten PC. Spine metastases: from radiotherapy, surgery, to radiosurgery. Neurosurgery. 2014;61(Suppl 1):16–25. doi: 10.1227/NEU.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 43.Vitaz TW, Oishi M, Welch WC, et al. Rotational and transpositional flaps for the treatment of spinal wound dehiscence and infections in patient populations with degenerative and oncological disease. J Neurosurg. 2004;100:46–51. doi: 10.3171/spi.2004.100.1.0046. [DOI] [PubMed] [Google Scholar]
- 44.Singh K, Samartzis D, Vaccaro AR, et al. Current concepts in the management of metastatic spinal disease. The role of minimally-invasive approaches. J Bone Joint Surg Br. 2006;88:434–42. doi: 10.1302/0301-620X.88B4.17282. [DOI] [PubMed] [Google Scholar]
- 45.Jansson KA, Bauer HC. Survival, complications and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J. 2006;15:196–202. doi: 10.1007/s00586-004-0870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Itshayek E, Yamada J, Bilsky M, et al. Timing of surgery and radiotherapy in the management of metastatic spine disease: a systematic review. Int J Oncol. 2010;36:533–44. [PubMed] [Google Scholar]
- 47.Sundaresan N, Digiacinto GV, Hughes JE, et al. Treatment of neoplastic spinal cord compression: results of a prospective study. Neurosurgery. 1991;29:645–50. doi: 10.1097/00006123-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 48.Ghogawala Z, Mansfield FL, Borges LF. Spinal radiation before surgical decompression adversely affects outcomes of surgery for symptomatic metastatic spinal cord compression. Spine (Phila Pa 1976) 2001;26:818–24. doi: 10.1097/00007632-200104010-00025. [DOI] [PubMed] [Google Scholar]
- 49.Sundaresan N, Rothman A, Manhart K, et al. Surgery for solitary metastases of the spine: rationale and results of treatment. Spine (Phila Pa 1976) 2002;27:1802–6. doi: 10.1097/00007632-200208150-00021. [DOI] [PubMed] [Google Scholar]
- 50.McPhee IB, Williams RP, Swanson CE. Factors influencing wound healing after surgery for metastatic disease of the spine. Spine (Phila Pa 1976) 1998;23:726–32. doi: 10.1097/00007632-199803150-00015. [DOI] [PubMed] [Google Scholar]
- 51.Keam J, Bilsky MH, Laufer I, et al. No association between excessive wound complications and preoperative high-dose, hypofractionated, image-guided radiation therapy for spine metastasis. Journal of neurosurgery Spine. 2014;20:411–20. doi: 10.3171/2013.12.SPINE12811. [DOI] [PubMed] [Google Scholar]
- 52.Sawakami K, Yamazaki A, Ishikawa S, et al. Polymethylmethacrylate augmentation of pedicle screws increases the initial fixation in osteoporotic spine patients. J Spinal Disord Tech. 2012;25:E28–35. doi: 10.1097/BSD.0b013e318228bbed. [DOI] [PubMed] [Google Scholar]
- 53.Burval DJ, McLain RF, Milks R, et al. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976) 2007;32:1077–83. doi: 10.1097/01.brs.0000261566.38422.40. [DOI] [PubMed] [Google Scholar]
- 54.Disa JJ, Smith AW, Bilsky MH. Management of radiated reoperative wounds of the cervicothoracic spine: the role of the trapezius turnover flap. Ann Plast Surg. 2001;47:394–7. doi: 10.1097/00000637-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Chang EL, Shiu AS, Mendel E, et al. Phase I/II study of stereotactic body radiotherapy for spinal metastasis and its pattern of failure. J Neurosurg Spine. 2007;7:151–60. doi: 10.3171/SPI-07/08/151. [DOI] [PubMed] [Google Scholar]
- 56.Moussazadeh N, Lis E, Katsoulakis E, et al. Five-year outcomes of high-dose single-fraction spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2015;93:361–7. doi: 10.1016/j.ijrobp.2015.05.035. [DOI] [PubMed] [Google Scholar]
- 57.Ghia AJ, Chang EL, Bishop AJ, et al. Single-fraction versus multi-fraction spinal stereotactic radiosurgery for spinal metastases from renal cell carcinoma: secondary analysis of Phase I/II trials. J Neurosurg Spine. 2016;24:829–36. doi: 10.3171/2015.8.SPINE15844. [DOI] [PubMed] [Google Scholar]
- 58.Bilsky MH, Laufer I, Burch S. Shifting paradigms in the treatment of metastatic spine disease. Spine (Phila Pa 1976) 2009;34:S101–7. doi: 10.1097/BRS.0b013e3181bac4b2. [DOI] [PubMed] [Google Scholar]
- 59.Kwan MK, Lee CK, Chan CY. Minimally invasive spinal stabilization using fluoroscopic-guided percutaneous screws as a form of palliative surgery in patients with spinal metastasis. Asian Spine J. 2016;10:99–110. doi: 10.4184/asj.2016.10.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moussazadeh N, Laufer I, Werner T, et al. Sacroplasty for cancer-associated insufficiency fractures. Neurosurgery. 2015;76:446–50. doi: 10.1227/NEU.0000000000000658. discussion 50. [DOI] [PubMed] [Google Scholar]
- 61.Park HY, Lee SH, Park SJ, et al. Minimally invasive option using percutaneous pedicle screw for instability of metastasis involving thoracolumbar and lumbar spine: a case series in a single center. J Korean Neurosurg Soc. 2015;57:100–7. doi: 10.3340/jkns.2015.57.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zairi F, Vielliard MH, Bouras A, et al. Long-segment percutaneous screw fixation for thoracolumbar spine metastases: a single centre experience. J Neurosurg Sci. 2015 doi: 10.23736/S0390-5616.16.03417-2. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 63.Dabravolski D, Lahm A, Esser J, et al. Tumours and metastases of the spine: cavity/coblation surgery and vertebroplasty/kyphoplasty. Orthopade. 2015;44:806–19. doi: 10.1007/s00132-015-3138-4. [DOI] [PubMed] [Google Scholar]
- 64.Dabravolski D, Lahm A, Kasch R, et al. Minimally invasive treatment of tumours and metastases in the spine by plasma field therapy (cavity coblation) and vertebro-/kyphoplasty with and without additional dorsal percutaneous instrumentation. Z Orthop Unfall. 2014;152:489–97. doi: 10.1055/s-0034-1382936. [DOI] [PubMed] [Google Scholar]
- 65.Tancioni F, Navarria P, Pessina F, et al. Early surgical experience with minimally invasive percutaneous approach for patients with metastatic epidural spinal cord compression (MESCC) to poor prognoses. Ann Surg Oncol. 2012;19:294–300. doi: 10.1245/s10434-011-1894-x. [DOI] [PubMed] [Google Scholar]
- 66.Uribe JS, Dakwar E, Le TV, et al. Minimally invasive surgery treatment for thoracic spine tumor removal: a mini-open, lateral approach. Spine (Phila Pa 1976) 2010;35:S347–54. doi: 10.1097/BRS.0b013e3182022d0f. [DOI] [PubMed] [Google Scholar]
- 67.Payer M, Sottas C. Mini-open anterior approach for corpectomy in the thoracolumbar spine. Surg Neurol. 2008;69:25–31. doi: 10.1016/j.surneu.2007.01.075. [DOI] [PubMed] [Google Scholar]
- 68.Huang TJ, Hsu RW, Liu HP, et al. Video-assisted thoracoscopic treatment of spinal lesions in the thoracolumbar junction. Surg Endosc. 1997;11:1189–93. doi: 10.1007/s004649900566. [DOI] [PubMed] [Google Scholar]
- 69.Dickman CA, Rosenthal D, Karahalios DG, et al. Thoracic vertebrectomy and reconstruction using a microsurgical thoracoscopic approach. Neurosurgery. 1996;38:279–93. doi: 10.1097/00006123-199602000-00010. [DOI] [PubMed] [Google Scholar]
- 70.McAfee PC, Regan JR, Fedder IL, et al. Anterior thoracic corpectomy for spinal cord decompression performed endoscopically. Surg Laparosc Endosc. 1995;5:339–48. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.