Abstract
Depending on the planned catheter position for selective internal radioembolization, coil embolization of hepatic artery branches can be necessary to enable a selective and safe procedure. The anatomy of the hepatic arterial bed has been demonstrated to have a substantial number of anatomic variations, which turns coil embolization into a challenge if the feeder shows a reversed, “hairpin-like” turn immediately after its origin. Hepatointestinal collateral vessels originating from the periphery of the right hepatic artery often present with such a reversed course and can preclude patients from uncomplicated radioembolization if catheterization fails. The purpose of this report is to describe 2 potential solutions for successful coil embolization of reversed-curve hepatointestinal collateral vessels using either a regular 4 French RIM catheter or a novel steerable tip-deflecting microcatheter.
Keywords: Interventional radiology, Hepatointestinal anastomoses, Steerable microcatheter, Advanced embolization techniques, Radioembolization
Introduction
Selective internal radiotherapy is used increasingly for treatment of patients suffering from both metastasis and advanced hepatocellular carcinoma [1], [2]. Nontargeted embolization of intestinal arteries with even small amounts of yttrium-90 can lead to severe complications such as gastric or duodenal ulcer or pancreatitis [1], [3], [4]. Different strategies are used to prevent unintended radiation deposition. In uncomplicated cases, the catheter is placed distal to large hepatointestinal anastomoses, for example, the gastroduodenal or right gastric artery, in the central portion of the right or left liver artery, proximal to its branching. In patients with distal origin of hepatointestinal anastomoses, however, the desired catheter position is either too distal to treat the whole liver or unsafe due to potential reflux and nontargeted embolization. In these patients, coil embolization of the gastroduodenal or right gastric artery is required during radioembolization evaluation. Unfortunately, coiling can cause substantial hepatointestinal collateralization originating from the left or right peripheral hepatic artery bed and resulting in a substantial filling of duodenal, pancreatic, gastric, or cystic arteries. In a recent study, Schelhorn et al. [2] observed peripheral hepatointestinal collateral (HIC) in 7 of 64 patients (11%) after coiling of the gastroduodenal artery. In all cases, coil embolization of the HIC was not possible, making radioembolization more cumbersome and, in 3 patients, even impossible [2].
Catheterization of peripheral HICs can be challenging due to the small vessel diameter. In addition, HICs tend to present with sharp “hairpin-like” turns immediately after their origin from the hepatic artery. Even if placement of a microcatheter in the origin is feasible, lack of stability prevents further advancement of guidewire, catheter, or embolization coil. The purpose of this technical note is to describe 2 potential interventional approaches to overcome this limitation in patients with HIC precluding radioembolization.
Material and methods
This retrospective study was approved by the institutional review board, and written informed consent was obtained from each patient prior to the intervention. The study follows the ethical standards of the Declaration of Helsinki. Both patients underwent radioembolization based on a tumor board decision. During radioembolization evaluation, selective hepatic angiogram and biphasic C-Arm computed tomography (CACT; Artis Q, Siemens Healthcare, Forchheim, Germany) were conducted following our standard protocol to investigate the hepatic vasculature. Combined single-photon emission computed tomography/computed tomography (SPECT/CT) analysis was conducted after injection of 99-m technetium-labeled human serum albumin (99mTc-HAS, ROTOP Pharmaka AG, Dresden, Germany) in order to detect or rule out extrahepatic tracer deposition. In the 2 patients presented here, HIC vessels were detected during radioembolization evaluation, hindering uncomplicated central radioembolization. In both patients, the HIC presented as reversed curve–shaped small arteries arising from the proper hepatic artery. Both were successfully accessed and coil embolized using 2 different techniques to obtain stable catheter position.
Case 1: RIM catheter technique
In this 66-year-old male suffering from HCC and scheduled for radioembolization, an angiogram of the right hepatic artery in the assumed treatment position after coil embolization of the right gastric artery, the gastroduodenal artery, and a pancreatic artery showed a small reversed-curve HIC (Fig. 1A). Despite the use of different guidewires and microcatheters (Renegade STC 18 with Transend 0.014 guidewire, Boston Scientific, Marlborough, MA; Merit Maestro with Tenor 0.014 guidewire, Merit Medical Systems, UT; Boston Direxion 0.021, Boston Scientific; additional guidewires: Fathom-16 0.016 guidewire, Boston Scientific and ChoICE Floppy guidewire 0.014, Boston Scientific), a stable position for coil embolization could not be achieved. Access by the guidewire was feasible, but advancement of the microcatheter resulted in dislocation of the guidewire. There was a substantial portion of tumor supplied by numerous arterial branches originating proximal to the small tortuous artery, so a more distal catheter position was not an option. Thus, we decided to advance a RIM catheter (tempo 4, Cordis, Waterloo, Belgium) into the right hepatic artery. After placing the catheter distal to the HIC origin, retraction resulted in stable access of the ostium, enabling advancement of a hydrophilic microcatheter (Merit Maestro, Merit Medical Systems) into the HIC (Fig. 1B). After performing a selective angiogram demonstrating collateral flow into the region of the pancreatic head (Fig. 1C), occlusion was achieved by coil embolization (Fig. 1D) using pushable coils (VorteX, Boston Scientific; COILPusher-16 0.016, Boston Scientific). Contrast-enhanced CACT revealed no extrahepatic enhancement and subsequent combined SPECT/CT analysis after 99mTc-HSA tracer injection excluded extrahepatic uptake and the patient underwent uncomplicated radioembolization (Y90-TheraSphere, MDS Nordion, Ottawa, Ontario, Canada; Biocompatibles UK Ltd, Surrey, UK).
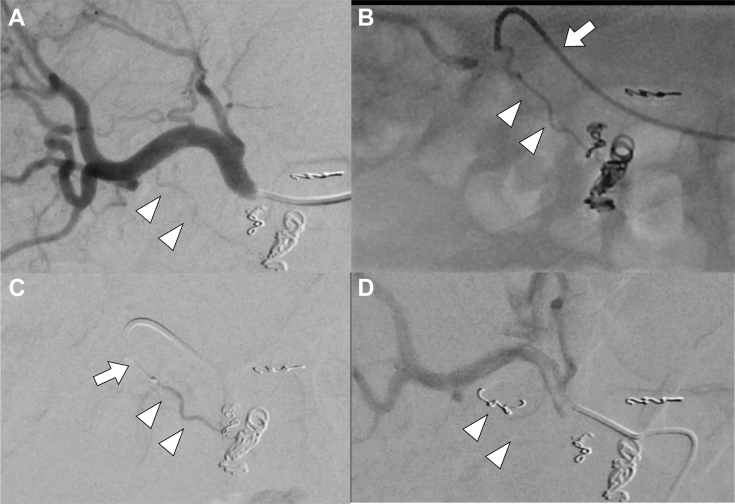
Fig. 1.
Angiographic (A, C, and D) and fluoroscopic (B) images of a 66-year-old male patient undergoing radioembolization evaluation. Initial angiogram (A) of the right hepatic artery shows a small reversed-curve hepatointestinal collateral vessels originating from the periphery of the right hepatic artery (arrowheads). Retraction of a configured standard catheter tip configuration (RIM) catheter (arrow; B) resulted in a stable access of the HIC orifice. Note the retrograde filling of gastroduodenal branches (arrowheads). Coaxial insertion of a microcatheter (arrow; C) in order to coil embolize the HIC (arrowheads). Occlusion of the HIC (D) was achieved by coil embolization (arrowheads). HIC, hepatointestinal collateral.
Case 2: steerable microcatheter technique
In this 59-year-old male suffering from bilobar multifocal HCC, the right gastric artery, the cystic artery, and the gastroduodenal artery were coil embolized in a first radioembolization evaluation session. A subsequent angiogram revealed a small HIC (Fig. 2B). Catheterization of the HIC origin in this first session with regular microcatheters (Renegade STC 18 with Transend 0.014 guidewire, Boston Scientific, Marlborough, MA; Merit Maestro with Tenor 0.014 guidewire, Merit Medical Systems, UT; Masters PARKWAY SOFT 1.98F with SION 0.014 guidewire, ASAHI Intecc, Pathumthani, Thailand) was not successful. Again, because a substantial portion of the tumor was supplied by arterial branches originating proximal to the HIC, a more distal catheter position was not feasible (Fig. 2A). Assuming the small HIC was not important, the patient underwent subsequent SPECT/CT. Unfortunately, extrahepatic tracer accumulation was detected (Figs. 3A and C), and radioembolization was determined to be contraindicated in this patient.
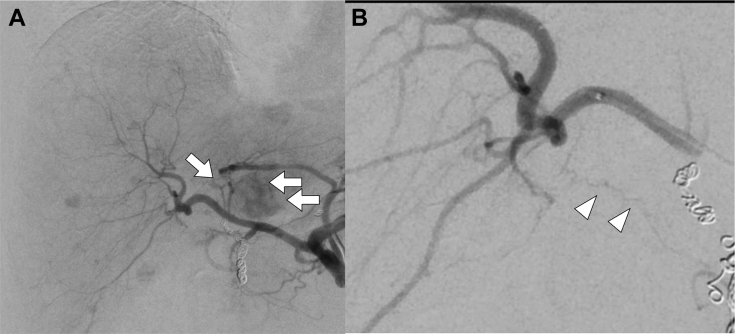
Fig. 2.
Angiographic images (A and B) of a 59-year-old male patient undergoing first radioembolization evaluation. Initial angiogram (A) of the common hepatic artery shows significant tumor blush and small arteries supplying the tumor originating from the right hepatic artery (arrows). Selective angiogram (B) of the distal right hepatic artery revealed a small reversed-curve hepatointestinal collateral vessels originating from the periphery of the right hepatic artery with retrograde filling of gastroduodenal branches (arrowheads).
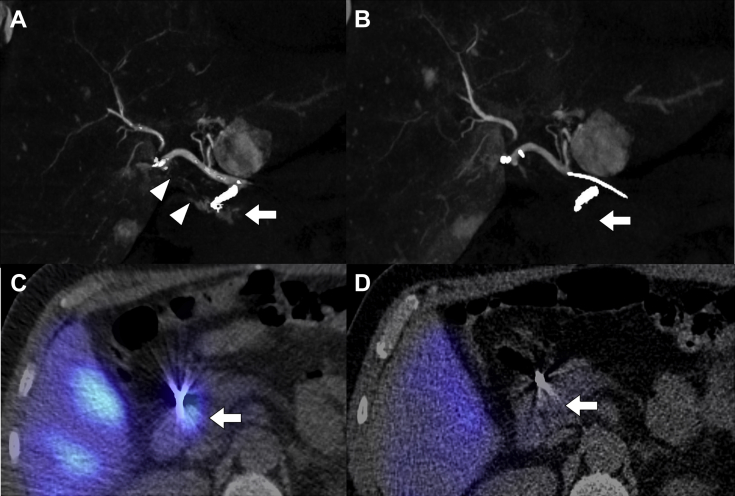
Fig. 3.
C-Arm CT (A and B) and corresponding SPECT/CT (C and D) images of a 59-year-old male patient comparing the first (A and C) and second (B and D) radioembolization evaluation. Pretreatment C-Arm CT (A and C) in the parenchymal phase and corresponding SPECT/CT of the first radioembolization evaluation showing enhancement of the duodenum (arrow; A and C) and the small reversed-curve HIC (arrowheads; A). C-Arm CT (B and D) in the parenchymal phase and corresponding SPECT/CT of the second radioembolization evaluation after occlusion of the HIC without extrahepatic contrast enhancement; neither in CACT (arrow; B) nor in corresponding SPECT/CT (arrow; D). CACT, C-Arm computed tomography; HIC, hepatointestinal collateral; SPECT/CT, single-photon emission computed tomography/computed tomography
Due to the introduction of a steerable microcatheter (SMC) (SwiftNINJA, Merit Medical Systems, UT), we recalled the patient for a second radioembolization evaluation 4 weeks later. In this second session, the known small tortuous hepatointestinal artery was still patent (Fig. 4A), and we decided to use the SMC. It is designed with a flexible catheter tip which can be inflected in 2 directions by the use of a wheel at the catheter hub. Access of the HIC was achieved by positioning the catheter tip near the origin and repeating inflection until the catheter tip hooked into the feeder. After successful entrance to the ostium (Fig. 4B), the microcatheter configuration was locked using the slider at the catheter hub and a guidewire was able to be advanced. Subsequently, to regain full flexibility of the microcatheter, the lock was released. Despite the stable guidewire position, the microcatheter could not be advanced more than approximately 3 mm into the HIC because the vessel diameter and the outer diameter of the microcatheter were of similar size. To perform coiling despite this, the microcatheter was locked again in an inflected configuration which provided increased catheter rigidity. In this state, we were able to advance a 2-mm pushable straight coil using a coil pusher (2 mm VorteX, Boston Scientific; COILPusher-16 0.016, Boston Scientific, Boston Scientific; Fig. 4C). Successful coil embolization was confirmed by CACT (Fig. 3B) and SPECT/CT (Fig. 3D), in which extrahepatic enhancement was excluded. Successful radioembolization (Y90-TheraSphere, MDS Nordion) was conducted 20 days later.
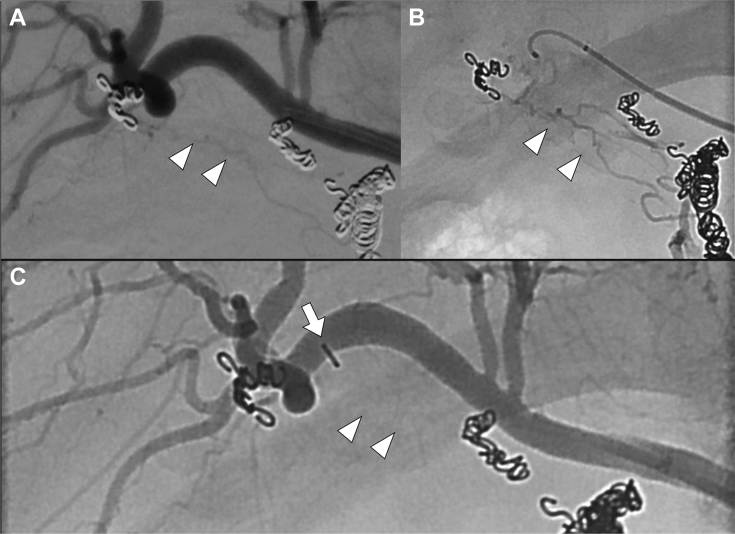
Fig. 4.
Angiographic (A and C) and fluoroscopic (B) images of a 59-year-old male patient undergoing second radioembolization evaluation. Initial angiogram (A) of the right hepatic artery shows the known small reversed-curve hepatointestinal collateral vessel originating from the periphery of the right hepatic artery is still patent (arrowheads). Positioning and stable access of the HIC orifice (B) with a steerable microcatheter and fluoroscopy of the small HIC (arrowheads); note the extensive retrograde filling of gastroduodenal branches. Occlusion of the HIC (arrowheads; C) was achieved with a small straight coil (arrow). HIC, hepatointestinal collateral.
With the 2 catheterization techniques described, occlusion of small tortuous HIC vessels with a diameter of less than 1 mm was achieved in both patients. In both cases, hepatointestinal shunting could be ruled out and radioembolization was performed in the planned positions without side effects. No adjustment of the planned microcatheter position was necessary.
Discussion
Catheterization and subsequent coil embolization can be challenging in small reversed-curve hepatointestinal arteries. Complete occlusion is crucial to prevent Y90 distribution into small gastrointestinal vessels, which has the potential to cause nonhealing gastrointestinal ulcers [1], [2], [5]. Schelhorn et al. [2] reported 28 patients with HICs of which 7 originated from the periphery of the hepatic arterial bed [2]. All of these were reported to be too small for catheterization and coil embolization [2]. In 4 patients, a more distal microcatheter position was achievable [2]. In 2 cases, repeated radioembolization evaluation revealed significant hepatointestinal shunting, and thus, radioembolization was considered unsafe and abandoned [2]. In the remaining case, surgical ligation of the HIC was conducted [2]. Considering all these cases, tortuous HICs originating from the periphery of the liver arteries have significant impact on the treatment decision. With the catheterization techniques described above, we demonstrate 2 different methods of successful coil embolization of small reversed-curve HICs.
The first technique relies on basic and low-cost materials. Configuration of the RIM catheter in this manner, however, requires a minimum diameter of the hepatic artery, and the technique has the potential to induce spasm or even to dissect the hepatic artery or the smaller HIC. Nevertheless, due to the lack of availability of other less traumatic techniques, we decided to use this approach.
Compared to the RIM catheter technique, the SMC enables a less traumatic placement of the catheter tip near the ostium of the HIC using inflection. Once the SMC is in place, it can be locked and gains rigidity enabling stable advancement of the guidewire even in a “hairpin-like” reversed-curve artery. Subsequently, the SMC can be released and advanced into the artery using the more rigid portion of the guidewire. If this attempt fails due to the tortuosity of the vessel as in our case, the rigidity of the SMC in locked state can be used to keep it inside the vessel ostium in order to place a coil in a central position. The SMC is more expensive than a regular microcatheter, so it is more often a “problem-solving” device than a “work horse” device. That said taking into account the numerous regular microcatheters that were used without success in our 2 cases, the appropriate use of a SMC can be even more cost-effective with regard to the total material costs. Nevertheless, advanced embolization techniques also depend on the technical skills and the experience of the performing interventional radiologist. In our case, the interventional radiologist had over 15 years of experience in interventional radiology and the presented techniques were the only successful approach.
The SMC represents a new device class and has the potential to expand the armamentarium of interventional radiology in oncology patients and might be of high value in this and numerous other endovascular interventions.
Teaching point
Catheterization of peripheral reversed-curve HICs can be challenging due to the small vessel diameter and the sharp-angled origins. The 2 represented approaches to catheterize these arteries can help to enable therapies like radioembolization. Interventional radiologists should be aware of technical developments like the new tip-deflection microcatehters. The presented techniques demonstrate the potential to expand the armamentarium of interventional radiology in oncology patients and might be of high value for performing radioembolization in a lobar but central and safe position, and numerous other types of endovascular interventions.
Footnotes
Competing Interests: F.K.W. received grants from Siemens Healthcare, DFG, Rebirth-Cluster of Excellence, BMBF, German Centre for Lung Research (DZL), and Promedicus Ltd., outside the submitted work. B.C.M. received grants from Siemens Healthcare, during the conduct of the study; and from Promedicus Ltd., outside the submitted work. The rest of the authors did not receive any competing interests.
Statement of informed consent and human rights: Our local ethics committee approved our protocol, and written informed consent was obtained from each study patient. The study follows the ethical standards of the Declaration of Helsinki.
References
- 1.Lewandowski R.J., Sato K.T., Atassi B., Ryu R.K., Nemcek A.A., Jr., Kulik L. Radioembolization with 90Y microspheres: angiographic and technical considerations. Cardiovasc Intervent Radiol. Springer-Verlag. 2007;30:571–592. doi: 10.1007/s00270-007-9064-z. [DOI] [PubMed] [Google Scholar]
- 2.Schelhorn J., Theysohn J., Ertle J., Schlaak J.F., Mueller S., Bockisch A. Selective internal radiation therapy of hepatic tumours: is coiling of the gastroduodenal artery always beneficial? Clin Radiol. 2014;69:e216–e222. doi: 10.1016/j.crad.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 3.Abdelmaksoud M.H.K., Hwang G.L., Louie J.D., Kothary N., Hofmann L.V., Kuo W.T. Development of new hepaticoenteric collateral pathways after hepatic arterial skeletonization in preparation for Yttrium-90 radioembolization. J Vasc Interv Radiol. 2010;21:1385–1395. doi: 10.1016/j.jvir.2010.04.030. Elsevier. [DOI] [PubMed] [Google Scholar]
- 4.Petroziello M.F., McCann J.W., Gonsalves C.F., Eschelman D.J., Anne P.R., Sato T. Side-branch embolization before 90Y radioembolization: rate of recanalization and new collateral development. Am J Roentgenol. 2012;197:W169–W174. doi: 10.2214/AJR.10.5600. [DOI] [PubMed] [Google Scholar]
- 5.Salem R., Lewandowski R.J., Sato K.T., Atassi B., Ryu R.K., Ibrahim S. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol. 2007;10:12–29. doi: 10.1053/j.tvir.2007.08.001. [DOI] [PubMed] [Google Scholar]