Abstract
Neonatal Salter-Harris I fractures of the distal humerus are a rare injury. This injury can be easily mistaken for a posterior elbow dislocation, creating a delay in diagnosis. We present a case of a neonate with a distal humerus Salter-Harris I fracture secondary to trauma during delivery. The patient presented with pseudoparesis of the left arm following birth. Posterior displacement of the elbow was identified on radiographs. Ultrasound of the elbow was performed after a gentle closed reduction of the left elbow was unsuccessful. A transphyseal supracondylar distal humerus fracture was identified on ultrasound. The patient subsequently had an intraoperative left elbow arthrogram to assist in visualization of the supracondylar fracture during closed reduction and percutaneous pinning. At 2-month follow-up, the patient was neurologically intact with full passive range of motion and had normal alignment of the capitellar ossification center and distal humerus on follow-up radiographs.
Keywords: Supracondylar, Humerus, Salter-Harris, Fracture, Dislocation, Pediatric, Neonate, Trauma
Introduction
Neonatal trauma is a common entity, with an estimated prevalence of approximately 3 traumatic injuries per 100 births [1], [2]. Superficial soft tissue injuries such as scalp hematoma comprise most traumatic birth injuries. When birth trauma does involve the musculoskeletal system, injury most commonly occurs around the shoulder with clavicle fractures and brachial plexus injury comprising a majority of musculoskeletal related birth injuries [1], [2]. Neonatal supracondylar fractures as the result of trauma during delivery are very rare with only a few case reports and case series present in the literature [3]. Previous case reports of neonatal supracondylar fracture have focused on the clinical aspects of the injury with little discussion of the imaging findings of supracondylar fractures in this age group. This case report focuses on describing the imaging characteristics of neonatal supracondylar fractures in multiple imaging modalities: radiographs, ultrasound, and fluoroscopy.
Supracondylar fractures in a neonate can be easily missed due to the low incidence of this injury as well as the absence of distal humerus epiphyseal ossification at birth. It is important that radiologists are aware of this injury pattern and its imaging appearance in order to make the correct diagnosis in a timely manner and avoid delays in diagnosis.
Case report
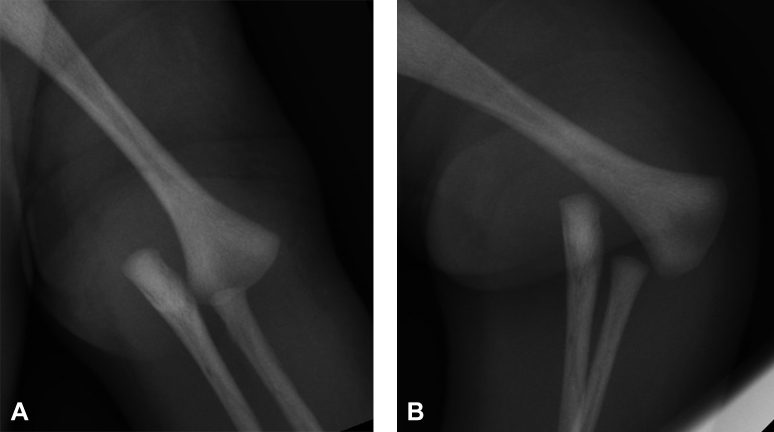
A 2-day-old baby girl presented with pseudoparesis of the left upper extremity. The patient was delivered at an outside institution with decreased motion of the left upper extremity appreciated shortly after delivery. Radiographs were obtained on the left upper extremity, which showed posteromedial dislocation of both the radius and ulna without visible fracture (Fig. 1). The patient was subsequently transferred to our institution for further evaluation and management of the injury.
Fig. 1.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Anterior-posterior (A) and lateral-oblique (B) radiographs of the left elbow demonstrate posteromedial dislocation of the elbow. No fracture is apparent on radiographs. There is no mineralization of the elbow ossification centers.
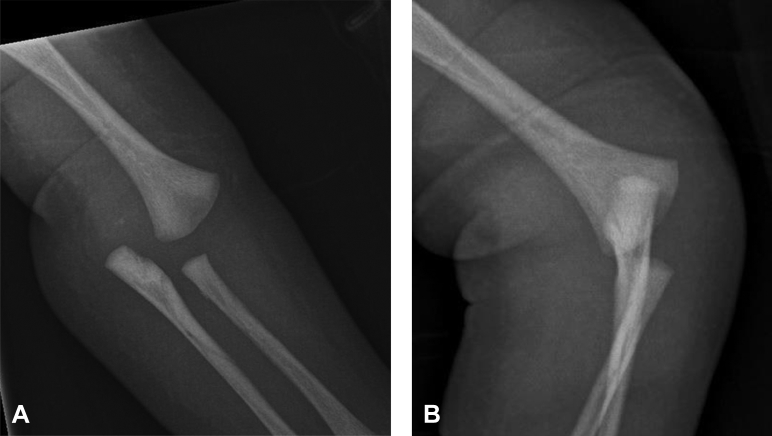
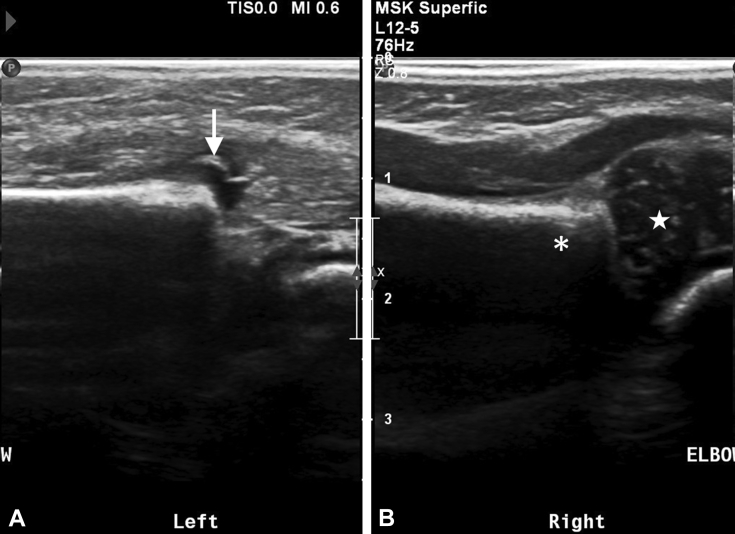
At our institution, a gentle closed reduction attempt of the elbow was attempted without success, and traction views of the elbow were obtained (Fig. 2). Because of the inability to reduce the fracture and posteromedial displacement of the elbow, an occult transphyseal fracture of the distal humerus was suspected. To avoid the need for sedation for an MRI or arthrogram, an ultrasound was ordered to confirm the diagnosis. An ultrasound was subsequently performed, which showed complete absence of the distal left humerus epiphysis from its expected position at the distal end of the humerus metadiaphysis on longitudinal ultrasound imaging (Fig. 3A) compared with normal positioning of the distal humerus epiphysis identified on the right (Fig. 3B). Transverse ultrasound demonstrated the left distal humerus epiphysis to be displaced posteromedial to the distal humerus metaphysis (Fig. 4). Findings were consistent with a posteriorly displaced Salter-Harris I (transphyseal) fracture of the distal humerus.
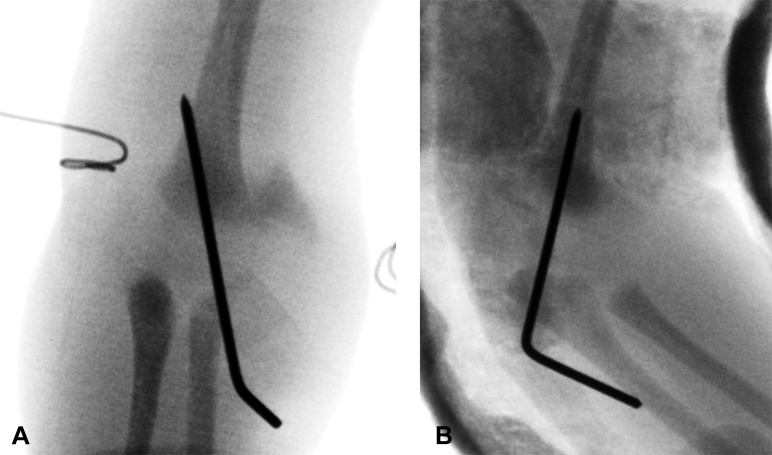
Fig. 2.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Anterior-posterior (A) and lateral-oblique (B) radiographs of the left elbow postattempted reduction demonstrate persistent posteromedial displacement of the elbow.
Fig. 3.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Comparison of longitudinal ultrasound images of the right and left elbows. (A) Longitudinal image of the left elbow demonstrates abrupt step-off at the distal humerus physis and absent epiphyseal cartilage with a small amount of joint fluid present along the anterior physeal line (arrow). (B) Longitudinal image of the right elbow demonstrates a normal physeal junction between the distal humerus metaphyseal bone (asterisks) and the unossified cartilage of the distal humerus epiphysis (star).
Fig. 4.
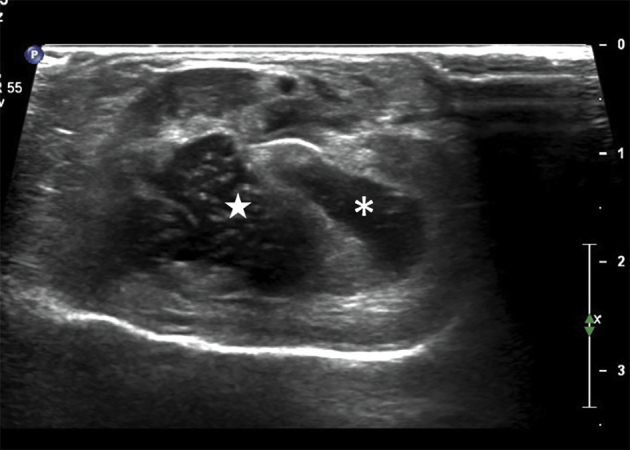
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Transverse ultrasound image of the left elbow shows the distal humerus epiphysis (star) displaced posterior and medial to the distal humerus metaphysis (asterisks).
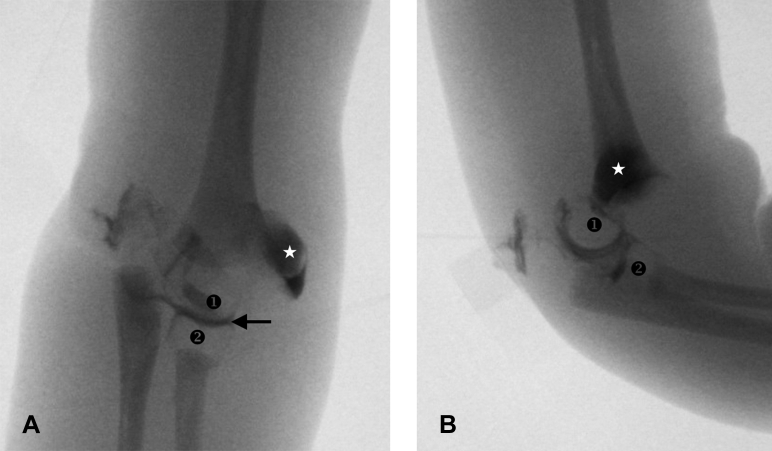
The patient was subsequently taken to surgery for closed reduction and percutaneous pinning of the left distal humerus fracture. Intraoperative left elbow arthrogram was performed to assist in identification of the unossified distal humerus epiphysis (Fig. 5). Arthrogram contrast both filled the joint and extended into the physeal fracture, outlining the displaced distal humerus epiphysis to allow visualization on fluoroscopy during reduction. The distal humerus physeal fracture was successfully reduced and fixated with a solitary laterally placed percutaneous pin (Fig. 6). At 2-month follow-up, the patient was neurologically intact with full passive range of motion and had normal alignment of the capitellar ossification center and distal humerus on follow-up radiographs (Fig. 7).
Fig. 5.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Anterior-posterior (A) and lateral (B) intraoperative elbow arthrogram images. Intraarticular contrast is present in the radiocapitellar joint (arrow) and outlines both the unossified distal humerus epiphysis (❶) and radial head (❷). Posteromedial displacement of the distal humerus epiphysis relative to the distal humerus metaphysis is readily visible. A large amount of intraarticular contrast has extravasated through a capsular defect into the medial elbow soft tissues (star).
Fig. 6.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Anterior-posterior (A) and lateral (B) intraoperative fluoroscopy images demonstrate anatomic alignment of the elbow postclosed reduction and percutaneous pinning using a single lateral pin.
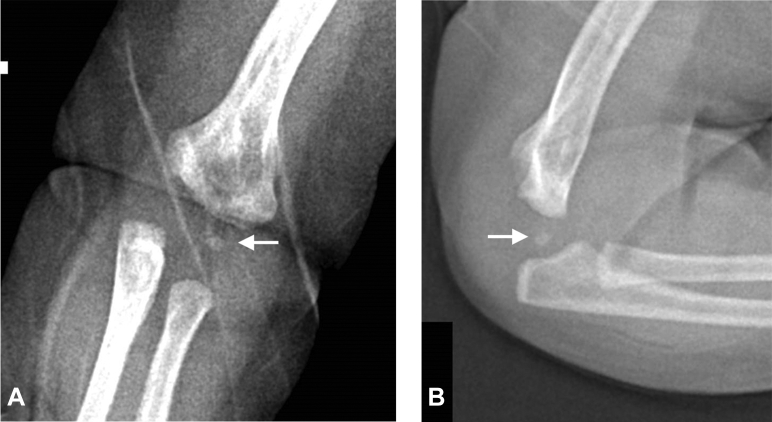
Fig. 7.
Two-day-old neonate with left Salter-Harris I distal humerus fracture. Anterior-posterior (A) and lateral (B) radiographs at 2-month follow-up show interval appearance of the capitellum ossification center (white arrows), which is in normal alignment with the distal humerus.
Discussion
Supracondylar fractures of the humerus are a common entity in children. Supracondylar fractures are the most common upper extremity fracture in children under 8 years of age with supracondylar fractures comprising over 50% of all elbow fractures in the pediatric population [4]. However, supracondylar fractures in neonates have been infrequently reported in the literature with only a few case reports and case series being described, most commonly in the setting of traumatic delivery or nonaccidental trauma [3].
Diagnosing transphyseal fractures can be challenging because of the absence of ossified epiphyseal cartilage. The first ossification center to form in the elbow is the capitellum, which typically does not appear until 6-12 months of age [5]. Until the capitellar ossification center appears, a distal humerus epiphyseal fracture can easily be mistaken for a pure posterior elbow dislocation on radiographs. However, elbow dislocation without fracture is rare in pediatric patients, particularly under the age of 10 years [6]. Also, elbow dislocations without fracture tend to displace posterolaterally, while supracondylar fractures tend to displace posteromedially [3]. Therefore, a supracondylar fracture should be suspected in any young pediatric patient presenting with posterior elbow displacement, particularly if the elbow joint is displaced posteromedially.
Radiographs and clinical examination may be sufficient for diagnosing neonate transphyseal fracture, even in the absence of epiphyseal ossification, although, typically an additional imaging modality is employed to assist in the diagnosis [3]. MRI, arthrography, and ultrasound have all been successfully utilized to diagnose neonate transphyseal fractures [7]. Arthrography is expensive and invasive and requires significant expertise in both performance and interpretation. MRI is expensive and time-consuming but is often preferred over arthrography for diagnosis due to MRI being less invasive and requiring less operator experience. MRI has been shown to be reliable for identifying radiographically occult fractures in multiple regions of the appendicular skeleton [8], [9]. Ultrasound is less expensive and more readily available than MRI and arthrography but requires significant expertise in performing and interpreting the examination, similar to arthrography, and is not typically considered a modality of choice for diagnosing bony injuries. However, ultrasound has been shown to be equivocal to diagnosing supracondylar humerus fractures in patients between 1 and 14 years of age [10].
On arthrography, contrast fills the elbow joint space and will extend into the physeal fracture line allowing the entire epiphysis to be outlined with contrast. The unossified distal humerus epiphysis will appear as a filling defect within the contrast with a contour similar to the contour of adult humeral condyles. On MRI, epiphyseal cartilage is low to intermediate signal on fluid-sensitive sequences and is easily distinguished from metaphyseal bone and adjacent soft tissues. Physeal fractures present as bright signal at the interface between the metaphysis and epiphysis on fluid-sensitive MR sequences, although completely displaced fractures will lack the high-signal line with diagnosis being made on the abnormal relationship between the metaphysis and epiphysis. On ultrasound, epiphyseal cartilage is hypoechoic with speckled hyperechoic foci, which is distinct from the markedly hyperechoic cortical bone of the metaphysis. Partially displaced physeal fractures can be identified by a hypoechoic line at the interface between the epiphysis and metaphysis, while diagnosis of completely displaced fractures again relies on recognizing an abnormal relationship between the epiphysis and metaphysis.
Because of the rarity of neonatal distal humeral fractures, there are no consensus guidelines for treatment. Both conservative and surgical managements of these fractures have been performed with generally good outcomes [3]. Decreased range of motion is the most common short-term complication of the fracture. Cubitus varus is the most common long-term complication with decreased range of motion and cubitus valgus also occurring as long-term complications [3].
Salter-Harris I fracture of the distal humerus is a rare but important diagnosis in the neonatal population. These fractures often have a similar presentation as pure elbow dislocations but can require different management. Therefore, it is important to consider a transphyseal (Salter-Harris I) humeral fracture in any neonate presenting with a posteriorly displaced elbow injury on radiographs.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Sauber-Schatz E.K., Markovic N., Weiss H.B., Bodnar L.M., Wilson J.W., Pearlman M.D. Descriptive epidemiology of birth trauma in the United States in 2003. Paediatr Perinat Epidemiol. 2010;24(2):116–124. doi: 10.1111/j.1365-3016.2009.01077.x. [DOI] [PubMed] [Google Scholar]
- 2.Moczygemba C.K., Paramsothy P., Meikle S., Kourtis A.P., Barfield W.D., Kuklina E. Route of delivery and neonatal birth trauma. Am J Obstet Gynecol. 2010;202(4):361.e1–361.e6. doi: 10.1016/j.ajog.2009.11.041. [DOI] [PubMed] [Google Scholar]
- 3.Ratti C., Guindani N., Riva G., Callegari L., Grassi F.A., Murena L. Transphyseal elbow fracture in newborn: review of literature. Musculoskelet Surg. 2015;99(S1):S99–S105. doi: 10.1007/s12306-015-0366-z. [DOI] [PubMed] [Google Scholar]
- 4.Landin L.A., Danielsson L.G. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57(4):309–312. doi: 10.3109/17453678608994398. [DOI] [PubMed] [Google Scholar]
- 5.Patel B., Reed M., Patel S. Gender-specific pattern differences of the ossification centers in the pediatric elbow. Pediatr Radiol. 2009;39:226–231. doi: 10.1007/s00247-008-1078-4. [DOI] [PubMed] [Google Scholar]
- 6.Little K.J. Elbow fractures and dislocations. Orthop Clin North Am. 2014;45:327–340. doi: 10.1016/j.ocl.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Jacobsen S., Hansson G., Nathorst-Westfelt J. Traumatic separation of the distal epiphysis of the humerus sustained at birth. J Bone Joint Surg Br. 2009;19(3):376–378. doi: 10.1302/0301-620X.91B6.22140. [DOI] [PubMed] [Google Scholar]
- 8.Gufler H., Schulze C.G., Wagner S., Baumbach L. MRI for occult physeal fracture detection in children and adolescents. Acta Radiol. 2013;54(4):467–472. doi: 10.1177/0284185113475606. [DOI] [PubMed] [Google Scholar]
- 9.Shi D.P., Zhu S.C., Li Y., Zheng J. Epiphyseal and physeal injury: comparison of conventional radiography and magnetic resonance imaging. Clin Imaging. 2009;33(5):379–383. doi: 10.1016/j.clinimag.2008.11.030. [DOI] [PubMed] [Google Scholar]
- 10.Eckert K., Janssen N., Ackermann O., Schweiger B., Radeloff E., Liedgens P. Ultrasound diagnosis of supracondylar fractures in children. Eur J Trauma Emerg Surg. 2014;40:159–168. doi: 10.1007/s00068-013-0306-2. [DOI] [PubMed] [Google Scholar]