Abstract
Page kidney is a rarely seen phenomenon leading to secondary hypertension and encountered most frequently due to traumatic or nontraumatic subcapsular hematoma. Such a compression in kidneys causes hypoperfusion and microangiopathic ischemia and activates renin-angiotensin-aldosterone system leading to hypertension. In this presentation, we report a rare case of bilateral Page kidney presenting with hypertension attacks due to spontaneous subcapsular hematoma developing in different kidneys at different times.
Keywords: Page kidney, Computed tomography, Hypertension
Introduction
Page kidney is the rare condition in which there is external compression of the kidneys due to a subcapsular hematoma, tumor, lymphocele, or urinoma, which leads to hypertension because of the activation of the renin-angiotensin-aldosterone system [1], [2]. It has been reported in all age segments and patients in association with mostly subcapsular or perinephric hematoma due to traumatic or iatrogenic interventions including surgical complications such as ureteral surgery and postrenal biopsy [2].
Here, we report a case of bilateral Page kidney presenting with hypertensive attacks due to bilateral spontaneous subcapsular hematoma.
Case report
In June 2013, a 24-year-old male patient was admitted to our institute with complaints of right-flank pain and headache. On physical examination, right flank was found to be tender and blood pressure was 170/100 mm Hg. The patient did not present with high temperature, dysuria, other urological symptoms, or a history of trauma. Hypertension had not been diagnosed before the admission. Serum creatinine and potassium levels were 0.67 mg/dL and 3.9 mEq/L, respectively. Laboratory tests including a whole blood count and biochemical profile were normal.
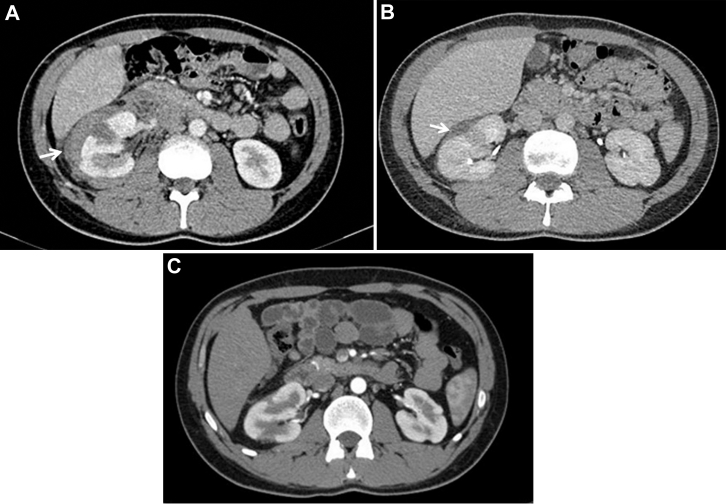
Doppler ultrasonography (US) did not show any findings supportive of renal artery stenosis. However, gray-scale US revealed a subcapsular hematoma on the right kidney. Computed tomography (CT) was also performed on this patient to detect any other additional pathology in the abdomen. CT confirmed the diagnosis of subcapsular hematoma on the right kidney and there was no other additional pathology. The subcapsular hematoma measured 23 mm in its thickest region with focal infarct regions in the right renal parenchyma due to pressure from the hematoma (Fig. 1A).
Fig. 1.
Axial intravenous contrast-enhanced CT images (June 2013). (A) Subcapsular hematoma encasing perirenal region of right kidney and focal infarct regions were observed (white arrow). (B) One-month later, reduced subcapsular hematoma thickness of right kidney was observed (white arrow). (C) Three months later, subcapsular hematoma resorbed completely.
The patient underwent extensive investigations, including measurements of plasma noradrenaline, adrenaline, dopamine, and normal 24-hour urinary vanillylmandelic acid, metanephrines, and catecholamines, all of which yielded results in the normal range. However, plasma renin levels were high at 8.45 ng/mL/h (normal range 0.2-2.8 ng/mL/h), with a plasma aldosterone concentration of 72.84 ng/dL. Prothrombin time, partial thromboplastin time, international normalized ratio, and platelet count were normal. The patient was prescribed antihypertensive treatment and followed up closely. A follow-up CT performed 1 month after the hospital discharge revealed that the subcapsular hematoma on the right kidney was resolving and now only measured 8 mm in its thickest region (Fig. 1B). Blood pressure was within the normal range. Another follow-up CT performed 3 months after the discharge revealed that the subcapsular hematoma has completely resolved (Fig. 1C).
After a span of 2 years in August 2015, the patient was readmitted to our institution, this time with the complaints of pain in the left flank region and nausea, with no history of trauma. Blood pressure was 160/100 mm Hg. CT scan showed a 20 mm subcapsular hematoma in the left kidney (Fig. 2). Antihypertensive treatment was again administered to the patient in the follow-up period.
Fig. 2.
Axial non–contrast-enhanced CT image (August 2015). Subcapsular hematoma encasing perirenal region of left kidney (white arrow).
Discussion
Page kidney was first demonstrated by wrapping canine kidneys in cellophane [3]. A similar compression arising from a hematoma is considered to cause renal hypoperfusion, activation of the renin-angiotensin-aldosterone system leading to salt and water retention and hypertension [2]. Several etiologies are responsible for causing Page kidney, the most frequent is blunt trauma leading to a subcapsular hematoma [4]. In addition, medical interventional procedures such as renal biopsy, extracorporeal shock wave lithotripsy, and percutaneous antegrade endopyelotomy also cause subcapsular hematoma leading to a Page kidney [5]. In addition, vehicle accidents and sports injuries were reported to lead to Page kidney cases in the literature [6]. Nontraumatic page kidney was reported in less number of cases in literature, and considered to develop because of other entities such as tumors, arteriovenous malformation, cystic rupture, subcapsular urinoma, pararenal lymphatic cyst, glomerulonephritis, vasculitis, and idiopathic [7], [8]. Our patient had neither the history of traumas nor known systemic diseases. Besides, all coagulative parameters were within normal limits. The subcapsular hematomas developed idiopathicly in the both kidneys of our patient at different times, and a complete resorption was formed between the attacks of high blood pressure.
For diagnosing a Page kidney, US is a noninvasive and replicable modality; however, this is dependent on the user's experience, and the technique may not detect tiny subcapsular hematomas. Renal Doppler US may be used in the evaluation of renal artery stenosis. Abdominal CT scans are more sensitive in recognizing active hemorrhages and tiny subcapsular hematomas. However, CT requires radiological expertise and exposes the patient to a high dose of radiations.
Antihypertensive drugs and regular follow-ups form the first line of treatment in Page kidneys. In situations where the treatment is unsuccessful, surgical procedures such as nephrectomy may be considered [8].
In conclusion, Page kidney is a rare cause of secondary hypertension. US and CT scan are easy and effective methods for the early diagnosis of this disorder.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Brotfain E., Koyfman L., Frenkel A., Smolikov A., Zlotnik A., Klein M. Traumatic page kidney induced hypertension in critical care: immediately resolved or long-term resistant problem. Case Rep Crit Care. 2013;2013:201424. doi: 10.1155/2013/201424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kenis I., Werner M., Nacasch N., Korzets Z. Recurrent non-traumatic page kidney. Isr Med Assoc J. 2012;14(7):452–453. [PubMed] [Google Scholar]
- 3.Gandhi V., Khosravi M., Burns A. Page kidney in a 17-year-old renal allograft. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr-2012-007653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diamond J.A. Hypertension due to perinephric compression: the “Page” kidney. Am J Hypertens. 2001;14(3):305. doi: 10.1016/s0895-7061(01)01286-9. [DOI] [PubMed] [Google Scholar]
- 5.Mufarrij P., Sandhu J.S., Coll D.M., Vaughan E.D., Jr. Page kidney as a complication of percutaneous antegrade endopyelotomy. Urology. 2005;65(3):592. doi: 10.1016/j.urology.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 6.Ozbek S., Kivrak A.S., Erol C., Koplay M. Non-traumatic Page kidney. BMJ Case Reports. 2013;2013 doi: 10.1136/bcr-2013-009135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smyth A., Collins C.S., Thorsteinsdottir B., Madsen B.E., Oliveira G.H., Kane G. Page kidney: etiology, renal function outcomes and risk for future hypertension. J Clin Hypertens (Greenwich) 2012;14(4):216–221. doi: 10.1111/j.1751-7176.2012.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.John J., Allen S., Perry M., Patel H.R., O'Brien T. Page kidney phenomenon presenting as acute renal failure after partial nephrectomy: a case report and review of the literature. Urol Int. 2008;80(4):440–443. doi: 10.1159/000132705. [DOI] [PubMed] [Google Scholar]