Abstract
The expression of Programmed cell Death Ligand 1 (PD-L1) is observed in many malignant tumors and is associated with poor prognosis including Gastric Cancer (GC). The relationship between PD-L1 expression and prognosis, however, is controversial in GC. This paper purports to use a meta-analysis to investigate the relationship between PD-L1 expression and prognosis in GC. For this study, the following databases were searched for articles published from June 2003 until February 2017: PubMed, EBSCO, Web of Science and Cochrane Library. The baseline information extracted were: authors, year of publication, country where the study was performed, study design, sample size, follow-up time, baseline characteristics of the study population, pathologic data, overall survival (OS). A total of 15 eligible studies covering 3291 patients were selected for a meta-analysis based on specified inclusion and exclusion criteria. The analysis showed that the expression level of PD-L1 was associated with the overall survival in GC (Hazard Ratio, HR = 1.46, 95%CI = 1.08–1.98, P = 0.01, random-effect). In addition to the above, subgroup analysis showed that GC patients with deeper tumor infiltration, positive lymph-node metastasis, positive venous invasion, Epstein-Barr virus infection positive (EBV+), Microsatellite Instability (MSI) are more likely to expression PD-L1. The results of this meta-analysis suggest that GC patients, specifically EBV+ and MSI, may be prime candidates for PD-1 directed therapy. These findings support anti-PD-L1/PD-1 antibodies as a kind of immunotherapy which is promising for GC.
Introduction
Worldwide, gastric cancer (GC) is the fourth most common malignant disease in males (fifth in females) and the third leading cause of cancer mortality in males (fifth in females), especially in Eastern Asia (particularly in Korea, Mongolia, Japan, and China), Central and Eastern Europe, and South America, and lowest in Northern America and most parts of Africa[1]. Developing immunotherapeutic strategies has become a hot area of focus in the treatment of GC. However, the therapeutic efficacy of all immune-checkpoint blockers is not satisfied[2–5]. To date, no phase III clinical trials on the immune-checkpoint blockers have been conducted on GC patients.
Recently, some clinical trials have indicated that monoclonal antibodies that target PD-1 or its receptor PD-L1 prevent the inhibitory effects of PD-1/PD-L1 pathway and enhance T cell functions, leading to impressive outcomes in patients with cancers[6–9]. However, from[10], ‘the predictive effects of PD-L1 in response to PD-1/PD-L1 antibodies in GC are not conclusive and the indication of PD-L1 expression in tumors remains controversial and needs to be further investigated’.
Through a meta-analysis, this review focuses on PD-L1 expression and its association with clinical outcomes in GC. Furthermore, this research attempts to show that the potential of PD-L1 positive patient to obtain optimum treatment benefit, appears promising. It might pinpoint patients most likely to strongly benefit from the inhibition of PD-L1/PD-1 as monotherapy compared to those that may most likely require a different or combinatorial approach in GC.
Materials and methods
Search strategy
Studies indexed, from June 2003 until February 2017 were systematically searched in the following databases: PubMed, EBSCO, Web of Science and Cochrane Library. The search terms used were: (“stomach neoplasms” OR “gastric cancer” OR “advanced gastric cancer” OR “gastric carcinoma” OR “stomach cancers”) AND (“PD-1” OR “PD-L1” OR “programmed death 1” OR “programmed death ligand 1” OR “programmed cell death ligand 1” OR “programmed death 1 ligand 1” OR“B7-H1”). Additionally, the reference lists of the selected articles were manually reviewed to obtain other potentially relevant articles. Selected publications were all in the English language.
Selection criteria
From the potentially relevant articles obtained above, those that indicated correlation between prognosis (including OS and/or clinical significance) and PD-1/PD-L1 in GC were selected.
Inclusion criteria
For inclusion in this meta-analysis:
Articles were limited to those dealing human subjects only.
All patients with GC would have been diagnosed by pathological evidence.
Expressions of PD-L1 would have been detected by Immunohistochemical (IHC) Assay from gastric carcinoma specimens.
All patients had been followed up and results reported.
Exclusion criteria
The following criteria were used to exclude irrelevant papers:
The literature was not the original article (such as meta-analysis, review), or a literature duplication.
The object of this study was cellular-based or animal-based.
The study also covered other malignancies, or the study did not include the analysis of expressions of PD-L1 in subgroups.
Data extraction and quality assessment
Data from each included study was independently extracted. The following baseline information was used: authors, year of publication, country where the study was performed, study design, sample size, follow-up time, cut-off criteria for overexpression (the definition of positive PD-L1), baseline characteristics of the study population, pathologic data, overall survival (OS).
This meta-analysis was conducted in accordance with the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement[11–13]. The quality of the included studies was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOS) checklist, independently by our team authors. This quality-assessment tool focuses on 8 items categorized in three groups (selection, comparability and outcome) with a maximum number of 9 stars. The articles achieving six or more stars were considered high quality[14].
Statistical analysis
Hazard ratios (HR) including 95% Confidence interval (CI) were used to assess the association between PD-L1 expression level and OS in GC. An observed HR > 1 implied a worse prognostic significance for the group with elevated PD-L1 expression. Conversely, HR < 1 implied a worse prognostic significance for the group with decreased PD-L1 expression. Revman 5.3 Software (RevMan, The Cochrane Collaboration) was used to evaluate heterogeneity between studies by Cochrane Q-test and P-values. Estimates of HR were weighted and pooled using the Mantel-Haenszel random effect model. The Stata 12.0 Software (Stata, College Station) was used to evaluate the sensitivity and publication bias of the studies. Publication bias was evaluated by Begg’s and Egger’s test, P < 0.05 was considered statistically significant. Begg’s and Egger’s test of publication bias was not performed on analysis subgroup with less than 5 studies because of low sensitivity of qualitative and quantitative tests[15].
Results
Description of trials included in the meta-analysis
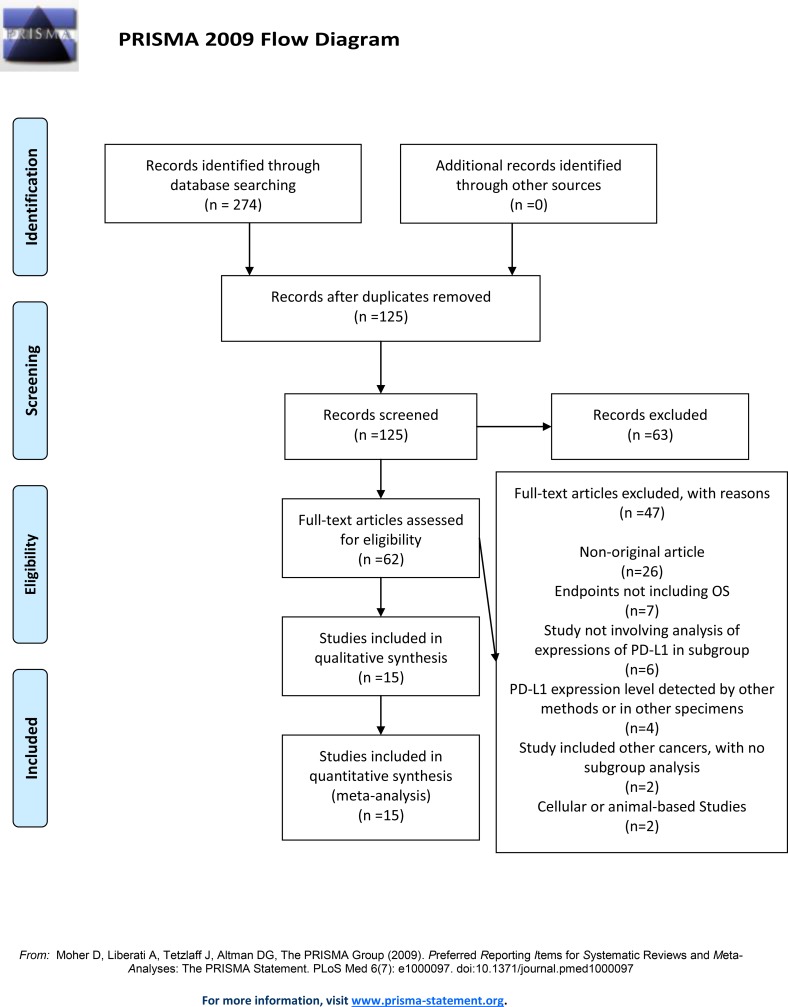
The search strategy originally generated 274 relevant clinical studies in English. Of these, 149 were eliminated because of repetition, 63 were excluded based on evaluation of their title or abstract. The remaining 62 articles were scrutinized by a full-text review. Based on the inclusion and exclusion criteria, 15 studies were selected for this meta-analysis. The detailed search and study selection process is shown in Fig 1.
Fig 1. Flow chart of study selection.
Study and patient characteristics
The 15 studies published between 2006 until 2016, included 3291 patients at baseline, with a maximum sample size of 451 and a minimum sample size of 96 participants. The majority of the studies were reported in Asia, 7 in China, 4 in Japan, 3 in South Korea, and 1 in Germany. The defining criterion for PD-L1 positive was that PD-L1 expression was observed in tumor cells by IHC. The discrepancies in the percentage of the PD-L1 positive expression patients were due to the variation in the cut-off values with the maximum ratio at 69.40% and the minimum at 14.32%. 1925(58.49%) patients did not undergo radiation or chemotherapy before surgery in 8 studies, others did not report. The characteristics of the included studies have been shown in Table 1.
Table 1. Characteristics of studies included in the meta-analysis.
| Author, year | Country |
No. |
Stage |
Follow-up, months | PD-L1 (%) | Cut off for positive | Location within tumor cells^ | Preoperative Chemoradiotherapy# | Surgery | Postoperative adjuvant Chemotherapy No. | Quality Assessment* |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Boger et al.[16], 2016 | Germany |
451 | I-IV | >20 | 23.73% | >1% | cytoplasmic | NOT | 401 patients received R0 resection and 50 received R1/R2 resection | NA | 8 |
| Chang et al.[17], 2016 | Korea |
451 | NA | >60 | 69.40% | NA | cytoplasmic |
NA | Gastric resection | NA | 7 |
| Dai et al.[18], 2016 | China |
398 | I-IV | >61 | 14.32% | >5% | cytoplasmic |
NOT | Gastric resection | 275 | 6 |
| Eto et al.[19], 2016 | Japan |
105 | II-III | >34 | 24.76% | >50% | cytoplasmic and nuclear |
NA | Gastric resection | 73 | 8 |
| Geng et al.[20], 2015 | China |
100 | I-IV | >60 | 65.00% | >50% | cytoplasmic and nuclear |
NA | Gastric resection | NA | 7 |
| Hou et al.[21], 2014 | China |
111 | I-IV | NA | 63.06% | >10% | NA | NOT | Gastric resection | NA | 7 |
| Kang et al.[22], 2016 | Korea |
234 | I-III | >65 | 15.38% | >10% | cytoplasmic |
NA | Gastric resection | 86 | 7 |
| Kawazoe et al.[23], 2016 | Japan |
383 | III-IV | >75 | 24.80% | >1% | cytoplasmic |
NOT | Gastric resection | 261 | 8 |
| Kim et al.[24], 2014 | Korea |
243 | I-III | >74 | 43.62% | >10% | cytoplasmic |
NA | Gastric resection | 89 | 8 |
| Li et al.[25], 2016 | China | 137 | I-IV | >17 | 40.88% | >5% | cytoplasmic | NA | Gastric resection | NA | 7 |
| Qing et al.[26], 2015 | China |
107 | NA | >42 | 50.47% | >10% | NA | NOT | Gastric resection | NA | 6 |
| Saito et al.[27], 2016 | Japan |
96 | NA | NA | 34.38% | >5% | cytoplasmic |
NA | Gastric resection | NA | 6 |
| Tamura et al.[28], 2015 | Japan |
241 | I-IV | >60 | 53.11% | >50% | NA | NOT | Gastric resection | 65 | 8 |
| Wu et al.[29], 2006 | China |
102 | NA | >42 | 42.16% | NA | cytoplasmic and nuclear |
NOT | Gastric resection | NA | 7 |
| Zhang et al.[30], 2015 | China |
132 | II-III | >66 | 50.76% | NA | cytoplasmic |
NOT | 40 patients received D1 resection and 92 patients received D2 resection | 63 | 7 |
^: PD-L1 expression location within the tumor cell as observed by the study
NA: Not available
NOT: No patients underwent pre-operative chemoradiotherapy
*: Quality Assessment based on Newcastle-Ottawa Scale
Prognosis
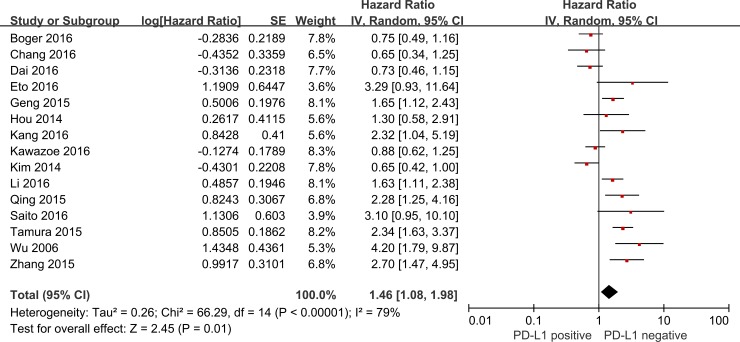
A total of 15 studies reported that the expression level of PD-L1 was related to OS. 11 studies indicated that PD-L1 overexpression was associated with poor prognosis of GC, conversely, 3 studies reported that PD-L1 overexpression was associated with better prognosis, and there was no indicated associations 1 study. Analysis showed that the expression level of PD-L1was associated with the OS in GC (HR = 1.46, 95%CI = 1.08–1.98, P = 0.01, random-effect) (Fig 2).
Fig 2. Forest plot describing the association between PD-L1 positive and HR of patients with GC.
Correlation of PD-L1 expression with clinicopathological characteristics
As shown in Table 2, a meta-analysis was performed to evaluate the relationship between the PD-L1 expression and clinicopathological characteristics in GC. Results demonstrated that the PD-L1 overexpression was significantly related to depth of infiltration (T-stage), lymph-node metastasis (N-stage), venous invasion, Epstein-Barr virus (EBV) infection, MSI-status. On the contrary, there was no clear relationship with sex, age, tumor site, tumor size, tumor differentiation, Lauren-Classification, TNM stage, lymphatic invasion, neural invasion (S1 Fig). Exploratory subgrouping was performed as per the ethnicity, stages of cancer, location within the tumor cells, pre operative chemoradiotherapy and post surgery adjuvant chemoradiotherapy, follow-up time of more than 5 years and also the PD-L1 positive cut-off value (S2 Fig). The analysis suggested that for the following exploratory subgroup: Asian, stages II-III, cut-off value of more than 50% and also the cytoplasmic and nuclear PD-L1 expression location within the tumor cell, the P values demonstrated a positive association with the OS in GC (Table 3).
Table 2. Correlation of PD-L1 expression with clinicopathological characteristics and Begg’s and Egger’s test in subgroup analysis.
| Subgroup analysis | No. of studies | No. of patients | Experimental group: positive/total | Control group: positive/total | OR | 95% CI | P value | Heterogeneity (I2) |
Begg's test (P value) |
Egger's test (P value) |
|---|---|---|---|---|---|---|---|---|---|---|
|
Gender |
14 | 2958 | Male 681/2073 (32.85%) |
Female 282/885 (31.86%) |
1.15 | 0.96–1.38 | 0.12 | 0% | 0.511 | 0.572 |
| Age1 | 4 | 707 | <60years 79/302 (26.16%) |
≥60years 140/405 (34.57%) |
0.74 | 0.49–1.11 | 0.15 | 18% | - | - |
| Age2 | 2 | 938 | <65years 237/515 (46.02%) |
≥65years 187/423 (44.21%) |
0.65 | 0.39–1.08 | 0.10 | 63% | - | - |
| Age3 | 2 | 484 | <70years 154/327 (47.09%) |
≥70years 80/157(50.96%) |
0.94 | 0.60–1.48 | 0.80 | 22% | - | - |
| Tumor site | 10 | 2060 | Proximal tumor 358/1106 (32.37%) |
Distal tumor 316/954(33.12%) |
1.05 | 0.74–1.47 | 0.79 | 59% | 0.858 | 0.882 |
| Tumor size | 5 | 509 | <5cm 142/287 (49.48%) |
≥5cm 130/222(58.56%) |
0.67 | 0.42–1.05 | 0.08 | 36% | 1.000 | 0.991 |
| Tumor differentiation | 12 | 2709 | well and moderately differentiation 437/1107 (39.48%) |
poorly differentiation 639/1602(39.89%) |
0.93 | 0.52–1.65 | 0.80 | 89% | 0.304 | 0.632 |
| Lauren Classification | 4 | 1101 | Intestinal 175/622 (28.14%) |
Diffuse 90/479(18.79%) |
1.58 | 0.54–4.64 | 0.40 | 90% | - | - |
| Depth of infiltration | 10 | 2438 | T1/T2 stage 291/858 (33.92%) |
T3/T4 stage 657/1580(41.58%) |
0.47 | 0.24–0.93 | 0.03 | 89% | 0.592 | 0.756 |
| Lymph-node metastasis | 12 | 2633 | N- 338/948(35.65%) |
N+ 708/1685(42.02%) |
0.54 | 0.31–0.95 | 0.03 | 86% | 0.193 | 0.939 |
| TNM stage | 9 | 1926 | I/IIstage 306/852(35.92%) |
III/IV stage 380/1074(35.38%) |
0.72 | 0.40–1.28 | 0.26 | 85% | 0.602 | 0.450 |
| Lymphatic invasion | 7 | 1857 | lymphatic invasion- 342/864(39.58%) |
lymphatic invasion+ 411/993(41.39%) |
0.66 | 0.32–1.36 | 0.26 | 88% | 0.072 | 0.050 |
| Venous invasion | 6 | 1623 | Venous invasion- 507/974(52.05%) |
Venous invasion+ 210/649(32.36%) |
0.52 | 0.36–0.74 | 0.0003 | 5% | 0.707 | 0.806 |
| Neural invasion | 4 | 1326 | Neural invasion- 337/853(39.51%) |
Neural invasion+ 175/473(37.00%) |
0.74 | 0.25–2.20 | 0.58 | 92% | - | - |
| E-B virus infection | 4 | 1307 | E-B virus + 94/171(54.97%) |
E-B virus– 223/1136(19.63) |
15.50 | 4.17–57.62 | <0.0001 | 77% | - | - |
| MSI-status | 2 | 937 | MSI 36/61(59.02%) |
MSS 176/876(20.09%) |
6.09 | 2.44–15.25 | 0.0001 | 62% | - | - |
Table 3. Exploratory subgrouping analysis of heterogeneity.
| No. of studies | HR | 95% CI | P value | Heterogeneity (I2) | ||
|---|---|---|---|---|---|---|
| Asian | 14 | 1.54 | 1.13–2.11 | 0.007 | 78% | |
| Stages | I-IV | 6 | 1.30 | 0.87–1.94 | 0.20 | 80% |
| II-III | 2 | 2.80 | 1.62–4.84 | 0.0002 | 0% | |
| I-III | 2 | 1.17 | 0.34–4.07 | 0.80 | 87% | |
| Follow-up more than 5 years | 8 | 1.24 | 0.82–1.88 | 0.30 | 84% | |
| Cut-off value | >1% | 2 | 0.83 | 0.63–1.08 | 0.17 | 0% |
| >5% | 3 | 1.36 | 0.66–2.78 | 0.40 | 79% | |
| >10% | 4 | 1.41 | 0.70–2.85 | 0.34 | 80% | |
| >50% | 3 | 2.03 | 1.53–2.71 | <0.00001 | 11% | |
| Location within tumor cells | cytoplasmic | 9 | 1.12 | 0.79–1.60 | 0.52 | 76% |
| cytoplasmic and nuclear | 3 | 2.50 | 1.28–4.90 | 0.007 | 55% | |
| No preoperative Chemoradiotherapy | 8 | 1.51 | 0.97–2.35 | 0.07 | 84% | |
| Postoperative adjuvant Chemotherapy | 7 | 1.42 | 0.86–2.33 | 0.17 | 85% | |
Publication bias and sensitivity analysis
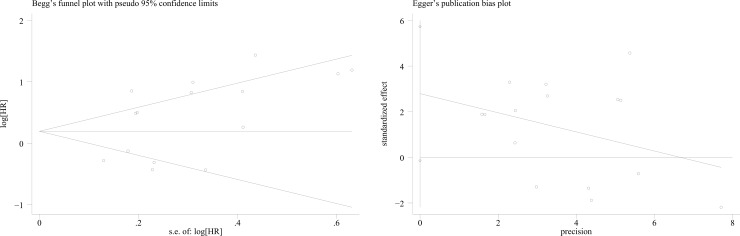
Begg’s and Egger’s test was used to evaluate the publication bias, respectively. In this meta-analysis, Begg’s and Egger’s test indicated no publication bias among included articles regarding the HR and OS (Begg’s test: P = 0.276 and Egger’s test P = 0.061) (Fig 3). There was no publication bias in subgroups analysis, as indicated by all the P values being greater than 0.05 (Table 2 and S3 Fig). Stata12.0 software was used to perform sensitivity analysis to assess whether the individual studies do not affect the overall results. The results indicated that individual study had little influence on the final results, and demonstrated that the analysis was relatively stable and credible (S4 Fig).
Fig 3. Begg’s and Egger’s funnel plot with 95% CI for OS publication bias testing.
Discussion
Based on the theory of The Cancer-Immunity Cycle, T cells have been the major focus of efforts to therapeutically manipulate endogenous anti-tumor immunity. However, for various reasons (factors in the tumor microenvironment might suppress effector T (Teff) cells that are produced), the activated Teff cells can’t specifically recognize and bind to cancer cells, T cells therefore cannot kill their target cancer cells. In other words, some molecules, namely factors, may act to modulate activated anti-tumor T cell, such as PD-L1[31].
PD-L1(B7-H1) is a B7-family member that has been ascribed as regulating T cell functions through the engagement with PD-1, a CD28family member receptor[32, 33]. Recent clinical trials have shown that anti-PD-L1/PD-1 antibodies produced both durable tumor regression and prolonged disease stabilization in patients with non-small-cell lung cancer[7], melanoma[6], renal-cell cancer[8], and pancreatic cancer[9]. Chen et al.[31] described the anti-cancer mechanism as when the antibodies block the PD-L1/PD-1 interaction, Teff cells can restore their anti-cancer function. Blank et al.[34] have demonstrated that blocking PD-L1 can improve immune functions of tumor-specific Teff cells when interacting with their target tumor cells in vitro.
However, the relationship between PD-L1 expression and prognosis is still subject to much controversy in GC. Boger et al.[16] reported that patients with PD-L1 positive tumor cells had a significantly improved prognosis, conversely, Chang et al.[17] showed that high PD-L1 expression was a significant adverse prognostic factor. In addition, Kawazoe et al.[23] indicated that PD-L1 was not a prognostic factor.
Recently, a few meta-analyses have shown a correlation between PD-L1 and prognosis in GC; Wu et al.[35], Xu et al.[36], and Liu et al.[37] demonstrated that PD-L1 overexpression was a worse prognostic factor in GC. However, their analyses covered small number of studies (3, 5 and 8 studies respectively) and also lacked further subgroup analysis. Zhang et al.[38] reported that PD-L1 positive was a risk factor for OS but it did not analyze the association between PD-L1 positive and Lauren-Classification, lymphatic, venous, neural invasion. To point out, sample patients are more from the East Asian community. Results may not apply in general to all human types, as it is known that reactions to medicine are not the same in general. In our study, the relation between the PD-L1 expression and a specific molecular subgroup such as E-B virus infection GC and MSI were analyzed.
Consistently with the experimental results of Ma et al.[39] and Derks et al.[40], this meta-analysis also demonstrated that EBV+ Gastric Cancer and MSI tend to show positive PD-L1 expression. The results of this meta-analysis, covering 3291 patients, showed that PD-L1 overexpression is a significant adverse prognostic factor. This finding fits the theory of the Cancer-Immunity Cycl[31]. In this theory, dead cancer cells release antigens, which are then captured by dendritic cells(DCs) which in turn process and present them. The latter prime and activate the Teff cells responses against the cancer-specific antigens. The activated Teff cells, then, traffic to and infiltrate the tumor bed, specifically recognize and bind to cancer cells and kill their target cancer cell. In cancer patients, the Cancer-Immunity Cycle does not perform optimally, one of the reasons (or most importantly) may be that some immune rheostat factors (such as PD-L1/PD-1) in the tumor microenvironment might be suppressing those Teff cells that are produced. Our findings concur with results of several clinic trials about anti-PD-L1/PD-1 antibodies, which supported the importance of the PD-L1/PD-1 pathway in GC, and demonstrated that anti-PD-L1/PD-1 antibodies can be safely given to patients and provided sustained anti-cancer activity.
As mentioned by[41]: ‘Regulatory T (Treg) cells are the main mediators of peripheral tolerance. They actively suppress Teff cells and inhibit immune-mediated tissue damage’. Treg cells can be divided into naturally occurring Treg (nTreg) and induced Treg(iTreg) cells[42]. PD-L1 is highly expressed on T reg cells and can make iTreg cells express some molecules (such as CD25, CTLA-4), which can potentially suppress Teff cells, owing to: [(1) PD-L1 can induce the development of functional fork head box p3+ (Foxp3+) iTreg cells, (2)PD-L1 enhances and maintains Foxp3 expression on iTreg cell and augments suppression at low Treg/T eff cell ratios. In addition, the TGF-βcan synergize the phenomenon.] Increased PD-L1 expression by tumor cells may induce and maintain iTreg cells in the periphery, thereby increasing the suppression of anti-tumor T cell responses and allowing tumor progression[43].
In effect, this research paper tries to evaluate the association between the PD-L1 overexpression and the clinical pathological features. From this meta-analysis, gastric cancer patients with deeper tumor infiltration, positive lymph-node metastasis, positive venous invasion, E-B virus infection positive, MSI are more likely to express PD-L1. The results of subgroup analysis tend to support the idea that patients with positive PD-L1 have unfavorable prognosis.
A recent study[44] aiming to perform a comprehensive molecular profiling found that key driver genes were enriched in a specific molecular subgroup: [(1) Epstein-Barr Virus positive (EBV+) GC, (2) Microsatellite Instability (MSI), (3) Chromosomal Instability (CIN) or (4) Genomically stable (GS) tumors]. EBV+ GC and MSI GC have rich lymphocytic infiltration in tumor stroma and thus can be classified as gastric carcinoma with prominent lymphoid stroma (medullary carcinoma). The lymphoid stroma in these tumors has high number of CD8 T cells, capable of mounting a robust antitumor inflammatory response. Besides, the positive PD-L1 expression was associated with a concomitant, significant increase in the number of CD8 T cells at tumor invasive front[39].
Beyond the differential presence of PD-L1+ cells in EBV+ and EBV- GC, Derks et al.[40] observed a difference in infiltration pattern of PD-L1 positive immune cells; while PD-L1+ immune cells were able to infiltrate the center of EBV+ and MSI GC, in EBV- and MSS GC PD-L1+ immune cells stayed mainly at the invasive margin. Further analysis showed that compared to EBV- GC, EBV+ GCs indeed have strong enrichment of IFN-γ response genes. The combination of PD-L1 positivity and enrichment for an IFN-γ signature in EBV+ GCs suggests the potential for PD-L1 expression and activation of the PD-1 pathway to be a critical mechanism in these tumors to control an antecedent cytotoxic anti-tumor immune response, which increases the likelihood of response to PD-1 blockade in this GC subtype. Interestingly, besides EBV+ GCs, MSI GCs have high IFN-γ response gene expression, perhaps reflecting the large lymphocyte infiltrate that is typical for mismatch-repair deficient cancers with a high mutational load.
To the best of our knowledge, it is the first meta-analysis to investigate the association between PD-L1 expression and E-B virus infection and MSI in GC. This study shows that the expression level of PD-L1 is higher in EBV+ GC and MSI than in EBV- GC and Microsatellite stability (MSS). The result suggests that specifically EBV+ GC and MSI may be prime candidates for PD-1directed therapy.
Limitations
The limitations of this study should be stressed on. The heterogeneity among included studies cannot be ignored. We were unable to control for factors such as environmental conditions, racial differences, socioeconomic situation, postoperative treatment, follow-up, all of which are known to influence the OS. Besides, these studies have used a number of monoclonal and polyclonal PD-L1 antibodies for immunohistochemistry and a variety of different scoring schemes/criteria to define positive PD-L1 expression. For example, Eto et al.[19] and Geng et al.[20] reported that when the percentage of PD-L1positivecancer cells was greater than 50%, which was the definition of PD-L1 positive, while, Kawazoe et al.[23] and Boger et al.[16] considered that PD-L1-positive cases on tumor cells were defined by the presence of at least 1% of tumor cells with membrane staining. The different ratio of the patient with PD-L1 overexpression ranged from 14%[18] to 69%[17].
Publication bias is another possible reason, wherein studies showing that PD-L1 was not a prognostic factor could be less likely to be published than studies showing that PD-L1 was a prognostic factor. Then the included studies were only English researches, no other languages. Beyond publication bias, the patients covered in this study were strictly from the countries where the studies were made. The conclusion would hence apply to those countries only unless the study is extended to other countries representatively. Perhaps the racial and social factors were also at play here as it has also been observed in other fields other than medicine. Their effects could have been cofounded with those being measured here. More representative samples of patient studies could be needed for stronger conclusion. Also, grey literature was not accounted for in this study as only studies published in the English language were chosen[45, 46].
Conclusion
This meta-analysis was to firstly evaluate the association between the PD-L1 expression and a specific molecular subgroup (EBV+ and MSI) in GC. Furthermore, gastric cancer patient with EBV+ and MSI tend to show PD-L1 expression, which demonstrated that specifically EBV+ GC and MSI may be prime candidates for PD-L1 directed therapy. However, further large-scale and comprehensive researches are needed to support our results and conclusion.
Supporting information
(A) sex, (B) age, (C) tumor site, (D) tumor size, (E) tumor differentiation, (F) Lauren Classification, (G) depth of infiltration,(H) lymph-node metastasis, (I) TNM stage, (J) lymphatic invasion, (K) venous invasion, (L) neural invasion, (M) E-B virus infection, (N)MSI-status.
(TIF)
(A) Asian, (B-1) stages I-IV, (B-2) stages II-III, (B-3) stages I-III, (C) follow-up more than 5 years, (D-1) cut-off value >1%, (D-2) cut-off value >5%, (D-3) cut-off value >10%, (D-4) cut-off value >50%, (E-1) location within tumor cells were cytoplasmic, (E-2) location within tumor cells were cytoplasmic and nuclear, (F) no patients underwent pre-operative chemoradiotherapy, (G) patients underwent postoperative adjuvant Chemotherapy.
(TIF)
(A) sex, (B) tumor site, (C) tumor size, (D) tumor differentiation, (E) depth of infiltration, (F) lymph-node metastasis, (G) TNM stage, (H) lymphatic invasion, (I) venous invasion.
(TIF)
(A) sex, (B) tumor site, (C) tumor size, (D) tumor differentiation, (E) depth of infiltration, (F) lymph-node metastasis, (G) TNM stage, (H) lymphatic invasion, (I) venous invasion,(J)OS.
(TIF)
(DOC)
Data Availability
All relevant data are included within the paper.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA: a cancer journal for clinicians. 2015;65(2):87–108. doi: 10.3322/caac.21262 . [DOI] [PubMed] [Google Scholar]
- 2.Fuchs CS, Tomasek J, Yong CJ, Dumitru F, Passalacqua R, Goswami C, et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet (London, England). 2014;383(9911):31–9. Epub 2013/10/08. doi: 10.1016/s0140-6736(13)61719-5 . [DOI] [PubMed] [Google Scholar]
- 3.Lordick F, Kang YK, Chung HC, Salman P, Oh SC, Bodoky G, et al. Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. The Lancet Oncology. 2013;14(6):490–9. Epub 2013/04/19. doi: 10.1016/S1470-2045(13)70102-5 . [DOI] [PubMed] [Google Scholar]
- 4.Van Cutsem E, de Haas S, Kang YK, Ohtsu A, Tebbutt NC, Ming Xu J, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a biomarker evaluation from the AVAGAST randomized phase III trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2012;30(17):2119–27. doi: 10.1200/JCO.2011.39.9824 . [DOI] [PubMed] [Google Scholar]
- 5.Waddell T, Chau I, Cunningham D, Gonzalez D, Okines AF, Okines C, et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. The Lancet Oncology. 2013;14(6):481–9. Epub 2013/04/19. doi: 10.1016/S1470-2045(13)70096-2 ; PubMed Central PMCID: PMCPmc3669518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. The New England journal of medicine. 2015;372(26):2521–32. doi: 10.1056/NEJMoa1503093 . [DOI] [PubMed] [Google Scholar]
- 7.Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet (London, England). 2016. Epub 2016/12/17. doi: 10.1016/s0140-6736(16)32517-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choueiri TK, Fishman MN, Escudier B, McDermott DF, Drake CG, Kluger H, et al. Immunomodulatory Activity of Nivolumab in Metastatic Renal Cell Carcinoma. Clinical cancer research: an official journal of the American Association for Cancer Research. 2016. Epub 2016/11/01. doi: 10.1158/1078-0432.ccr-15-2839 ; PubMed Central PMCID: PMCPmc5106340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mace TA, Shakya R, Pitarresi JR, Swanson B, McQuinn CW, Loftus S, et al. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2016. Epub 2016/11/01. doi: 10.1136/gutjnl-2016-311585 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu X, Yang Z, Latchoumanin O, Qiao L. Antagonizing programmed death-1 and programmed death ligand-1 as a therapeutic approach for gastric cancer. Therapeutic advances in gastroenterology. 2016;9(6):853–60. Epub 2016/11/03. doi: 10.1177/1756283X16658251 ; PubMed Central PMCID: PMCPmc5076768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England). 2010;8(5):336–41. Epub 2010/02/23. doi: 10.1016/j.ijsu.2010.02.007 . [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4:1 Epub 2015/01/03. doi: 10.1186/2046-4053-4-1 ; PubMed Central PMCID: PMCPmc4320440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283(15):2008–12. Epub 2000/05/02. . [DOI] [PubMed] [Google Scholar]
- 14.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European journal of epidemiology. 2010;25(9):603–5. Epub 2010/07/24. doi: 10.1007/s10654-010-9491-z . [DOI] [PubMed] [Google Scholar]
- 15.Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2007;176(8):1091–6. Epub 2007/04/11. doi: 10.1503/cmaj.060410 ; PubMed Central PMCID: PMCPmc1839799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boger C, Behrens HM, Mathiak M, Kruger S, Kalthoff H, Rocken C. PD-L1 is an independent prognostic predictor in gastric cancer of Western patients. Oncotarget. 2016;7(17):24269–83. Epub 2016/03/25. doi: 10.18632/oncotarget.8169 ; PubMed Central PMCID: PMCPmc5029700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang H, Jung WY, Kang Y, Lee H, Kim A, Kim HK, et al. Programmed death-ligand 1 expression in gastric adenocarcinoma is a poor prognostic factor in a high CD8+ tumor infiltrating lymphocytes group. Oncotarget. 2016;7(49):80426–34. Epub 2016/10/16. doi: 10.18632/oncotarget.12603 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai C, Geng R, Wang C, Wong A, Qing M, Hu J, et al. Concordance of immune checkpoints within tumor immune contexture and their prognostic significance in gastric cancer. Molecular oncology. 2016;10(10):1551–8. doi: 10.1016/j.molonc.2016.09.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eto S, Yoshikawa K, Nishi M, Higashijima J, Tokunaga T, Nakao T, et al. Programmed cell death protein 1 expression is an independent prognostic factor in gastric cancer after curative resection. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2016;19(2):466–71. doi: 10.1007/s10120-015-0519-7 . [DOI] [PubMed] [Google Scholar]
- 20.Geng Y, Wang H, Lu C, Li Q, Xu B, Jiang J, et al. Expression of costimulatory molecules B7-H1, B7-H4 and Foxp3+ Tregs in gastric cancer and its clinical significance. International journal of clinical oncology. 2015;20(2):273–81. doi: 10.1007/s10147-014-0701-7 . [DOI] [PubMed] [Google Scholar]
- 21.Hou J, Yu Z, Xiang R, Li C, Wang L, Chen S, et al. Correlation between infiltration of FOXP3+ regulatory T cells and expression of B7-H1 in the tumor tissues of gastric cancer. Experimental and molecular pathology. 2014;96(3):284–91. doi: 10.1016/j.yexmp.2014.03.005 . [DOI] [PubMed] [Google Scholar]
- 22.Kang HJ, Lee IS, Park YS, Ho WJ, Sohn D, Ahn JY, et al. Biomarkers of EBV-positive Gastric Cancers: Loss of PTEN Expression is Associated with Poor Prognosis and Nodal Metastasis. Annals of surgical oncology. 2016;23(11):3684–92. doi: 10.1245/s10434-016-5284-2 . [DOI] [PubMed] [Google Scholar]
- 23.Kawazoe A, Kuwata T, Kuboki Y, Shitara K, Nagatsuma AK, Aizawa M, et al. Clinicopathological features of programmed death ligand 1 expression with tumor-infiltrating lymphocyte, mismatch repair, and Epstein-Barr virus status in a large cohort of gastric cancer patients. 2016. doi: 10.1007/s10120-016-0631-3 . [DOI] [PubMed] [Google Scholar]
- 24.Kim JW, Nam KH, Ahn SH, Park do J, Kim HH, Kim SH, et al. Prognostic implications of immunosuppressive protein expression in tumors as well as immune cell infiltration within the tumor microenvironment in gastric cancer. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2016;19(1):42–52. doi: 10.1007/s10120-014-0440-5 . [DOI] [PubMed] [Google Scholar]
- 25.Li Z, Lai Y, Sun L, Zhang X, Liu R, Feng G, et al. PD-L1 expression is associated with massive lymphocyte infiltration and histology in gastric cancer. Human pathology. 2016;55:182–9. doi: 10.1016/j.humpath.2016.05.012 . [DOI] [PubMed] [Google Scholar]
- 26.Qing Y, Li Q, Ren T, Xia W, Peng Y, Liu GL, et al. Upregulation of PD-L1 and APE1 is associated with tumorigenesis and poor prognosis of gastric cancer. Drug design, development and therapy. 2015;9:901–9. doi: 10.2147/DDDT.S75152 ; PubMed Central PMCID: PMC4338255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saito R, Abe H, Kunita A, Yamashita H, Seto Y, Fukayama M. Overexpression and gene amplification of PD-L1 in cancer cells and PD-L1+ immune cells in Epstein-Barr virus-associated gastric cancer: the prognostic implications. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc. 2016. doi: 10.1038/modpathol.2016.202 . [DOI] [PubMed] [Google Scholar]
- 28.Tamura T, Ohira M, Tanaka H, Muguruma K, Toyokawa T, Kubo N, et al. Programmed Death-1 Ligand-1 (PDL1) Expression Is Associated with the Prognosis of Patients with Stage II/III Gastric Cancer. Anticancer research. 2015;35(10):5369–76. Epub 2015/09/27. . [PubMed] [Google Scholar]
- 29.Wu C, Zhu Y, Jiang J, Zhao J, Zhang XG, Xu N. Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in gastric carcinoma and its clinical significance. Acta histochemica. 2006;108(1):19–24. doi: 10.1016/j.acthis.2006.01.003 . [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Qiu M, Jin Y, Ji J, Li B, Wang X, et al. Programmed cell death ligand 1 (PD-L1) expression on gastric cancer and its relationship with clinicopathologic factors. International journal of clinical and experimental pathology. 2015;8(9):11084–91. Epub 2015/12/01. ; PubMed Central PMCID: PMCPmc4637642. [PMC free article] [PubMed] [Google Scholar]
- 31.Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10. Epub 2013/07/31. doi: 10.1016/j.immuni.2013.07.012 . [DOI] [PubMed] [Google Scholar]
- 32.Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annual review of immunology. 2008;26:677–704. Epub 2008/01/05. doi: 10.1146/annurev.immunol.26.021607.090331 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nature reviews Immunology. 2008;8(6):467–77. doi: 10.1038/nri2326 . [DOI] [PubMed] [Google Scholar]
- 34.Blank C, Kuball J, Voelkl S, Wiendl H, Becker B, Walter B, et al. Blockade of PD-L1 (B7-H1) augments human tumor-specific T cell responses in vitro. International journal of cancer. 2006;119(2):317–27. Epub 2006/02/17. doi: 10.1002/ijc.21775 . [DOI] [PubMed] [Google Scholar]
- 35.Wu P, Wu D, Li L, Chai Y, Huang J. PD-L1 and Survival in Solid Tumors: A Meta-Analysis. PloS one. 2015;10(6):e0131403 doi: 10.1371/journal.pone.0131403 ; PubMed Central PMCID: PMC4483169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu F, Feng G, Zhao H, Liu F, Xu L, Wang Q, et al. Clinicopathologic Significance and Prognostic Value of B7 Homolog 1 in Gastric Cancer: A Systematic Review and Meta-Analysis. Medicine. 2015;94(43):e1911 doi: 10.1097/MD.0000000000001911 ; PubMed Central PMCID: PMC4985428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu YX, Wang XS, Wang YF, Hu XC, Yan JQ, Zhang YL, et al. Prognostic significance of PD-L1 expression in patients with gastric cancer in East Asia: a meta-analysis. OncoTargets and therapy. 2016;9:2649–54. doi: 10.2147/OTT.S102616 ; PubMed Central PMCID: PMC4863684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang M, Dong Y, Liu H, Wang Y, Zhao S, Xuan Q, et al. The clinicopathological and prognostic significance of PD-L1 expression in gastric cancer: a meta-analysis of 10 studies with 1,901 patients. Scientific reports. 2016;6:37933 doi: 10.1038/srep37933 ; PubMed Central PMCID: PMC5124943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ma C, Patel K, Singhi AD, Ren B, Zhu B, Shaikh F, et al. Programmed Death-Ligand 1 Expression Is Common in Gastric Cancer Associated With Epstein-Barr Virus or Microsatellite Instability. The American journal of surgical pathology. 2016;40(11):1496–506. Epub 2016/10/19. doi: 10.1097/PAS.0000000000000698 . [DOI] [PubMed] [Google Scholar]
- 40.Derks S, Liao X, Chiaravalli AM, Xu X, Camargo MC, Solcia E, et al. Abundant PD-L1 expression in Epstein-Barr Virus-infected gastric cancers. Oncotarget. 2016;7(22):32925–32. Epub 2016/05/06. doi: 10.18632/oncotarget.9076 ; PubMed Central PMCID: PMCPmc5078063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133(5):775–87. Epub 2008/05/31. doi: 10.1016/j.cell.2008.05.009 . [DOI] [PubMed] [Google Scholar]
- 42.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nature immunology. 2003;4(4):330–6. doi: 10.1038/ni904 . [DOI] [PubMed] [Google Scholar]
- 43.Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK, et al. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. The Journal of experimental medicine. 2009;206(13):3015–29. Epub 2009/12/17. doi: 10.1084/jem.20090847 ; PubMed Central PMCID: PMCPmc2806460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bass AJ, Thorsson V, Shmulevich I, Reynolds SM, Miller M, Bernard B, et al. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513(7517):202–9. doi: 10.1038/nature13480 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burdett S, Stewart LA, Tierney JF. Publication bias and meta-analyses: a practical example. International journal of technology assessment in health care. 2003;19(1):129–34. Epub 2003/04/19. . [DOI] [PubMed] [Google Scholar]
- 46.Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC medical research methodology. 2017;17(1):64 Epub 2017/04/20. doi: 10.1186/s12874-017-0347-z ; PubMed Central PMCID: PMCPmc5395863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) sex, (B) age, (C) tumor site, (D) tumor size, (E) tumor differentiation, (F) Lauren Classification, (G) depth of infiltration,(H) lymph-node metastasis, (I) TNM stage, (J) lymphatic invasion, (K) venous invasion, (L) neural invasion, (M) E-B virus infection, (N)MSI-status.
(TIF)
(A) Asian, (B-1) stages I-IV, (B-2) stages II-III, (B-3) stages I-III, (C) follow-up more than 5 years, (D-1) cut-off value >1%, (D-2) cut-off value >5%, (D-3) cut-off value >10%, (D-4) cut-off value >50%, (E-1) location within tumor cells were cytoplasmic, (E-2) location within tumor cells were cytoplasmic and nuclear, (F) no patients underwent pre-operative chemoradiotherapy, (G) patients underwent postoperative adjuvant Chemotherapy.
(TIF)
(A) sex, (B) tumor site, (C) tumor size, (D) tumor differentiation, (E) depth of infiltration, (F) lymph-node metastasis, (G) TNM stage, (H) lymphatic invasion, (I) venous invasion.
(TIF)
(A) sex, (B) tumor site, (C) tumor size, (D) tumor differentiation, (E) depth of infiltration, (F) lymph-node metastasis, (G) TNM stage, (H) lymphatic invasion, (I) venous invasion,(J)OS.
(TIF)
(DOC)
Data Availability Statement
All relevant data are included within the paper.