Abstract
Background
Blockade of the renin–angiotensin–aldosterone system is a cornerstone in cardiovascular disease prevention and hypertension treatment. The relevance of ambulatory blood pressure monitoring (ABPM) has been widely confirmed for both increasing the accuracy of blood pressure (BP) measurements, particularly in pharmacological trials, and focusing on 24 h BP prognostic parameters. The aim of this study was to assess the effects of canrenone addition on ambulatory BP in uncontrolled hypertensive patients already treated with the highest tolerated dose of angiotensin-converting enzyme (ACE) inhibitors or angiotensin II type 1 receptor (AT1R) antagonists plus hydrochlorothiazide (HCT).
Methods
ABPM was performed at baseline and after 3 months of combination therapy in 158 outpatients with stage 1 or 2 hypertension who were randomized to add canrenone (50 or 100 mg) to the pre-existing therapy with ACE inhibitors or AT1R antagonists plus HCT. Twenty-four-hour systolic and diastolic BPs were considered normalized when the values were <130 and <80 mmHg, respectively.
Results
The addition of canrenone was associated with a reduction in systolic and diastolic BPs (24 h and daytime and nighttime; P<0.001), mean arterial pressures (P<0.001), and pulse pressures (P<0.01). The Δ 24 h systolic/diastolic BPs were −13.5±11.2/−8±8 mmHg and −16.1±13.5/−11.2±8.3 mmHg (50 and 100 mg/day, respectively). In the 50 mg arm, the 24 h systolic and diastolic BPs were normalized in 67.5% and 74% of the patients, respectively, and in 61.6% and 68.5% of the patients in the 100 mg arm, respectively (P<0.05; P= not significant for 50 vs 100 mg). The percentage of patients whose nocturnal decrease was >10% with respect to diurnal values did not change during combination therapy.
Conclusion
Canrenone addition to ACE inhibitors or AT1R antagonists plus HCT was associated with a significant reduction of 24 h BP and to an increased number of patients meeting 24 h ABPM targets in a clinical setting of uncontrolled stage 1 or 2 hypertension.
Keywords: ambulatory blood pressure, canrenone, RAAS, ACE inhibitors, AT1R antagonist
Introduction
Atherosclerosis, from initial endothelial lesions to overt cardiovascular events, recognizes hypertension as one of the major risk factors.1–3 However, only a small number of patients are treated in order to achieve blood pressure (BP) goals, and treatment of hypertension is far from optimal even in high vascular risk populations.4
The activation of a number of inflammatory mediators and pathways, among which the angiotensin system has a relevant role, contributes to endothelial dysfunction and damage.5–12 Moreover, it is known that patients at increased cardiovascular risk have an upregulation of angiotensin II type 1 receptors (AT1Rs) in immune cells crucial for the mechanisms leading to inflammation/atherosclerosis.10–12 Aldosterone, in addition to its effects on volume and BP regulation, has a number of extrarenal actions that contribute to the pathogenesis of cardiovascular disease.13 Although no definite role for these drugs in cardiovascular mortality has been documented, the introduction of mineralocorticoid receptor antagonists seems to be associated with potentially impressive outcomes in human cardiovascular protection.14–16 Therefore, blocking the renin–angiotensin–aldosterone system (RAAS) is a cornerstone in cardiovascular prevention and in the treatment of hypertension, including the anti- remodeling effects of the blockade.17,18 For this purpose, among treatment options in clinical settings, angiotensin-converting enzyme (ACE) inhibitors or AT1R antagonists are the first choice, with the mineralocorticoid receptor antagonists and renin inhibitors constituting the other possible interventionary drugs for RAAS.
Several studies point to aldosterone as relevant for BP, and besides its obvious role in primary hyperaldosteronism, higher circulating aldosterone levels are associated with higher BP values and are related to future development of drug-resistant hypertension and hypertension in non-hypertensive individuals.17,19–21 However, aldosterone receptor antagonists are associated with potential side effects such as glomerular filtration rate (GFR) reduction and hyperkalemia, and little is known about office visit BP changes when these drugs are added on top of the angiotensin system blockade.16,22,23 Moreover, the effects of canrenone added to the pre-existing blockade of the system on ambulatory BP monitoring (ABPM) parameters are unknown. Therefore, we sought to assess the effects of canrenone addition (50 or 100 mg), an aldosterone receptor antagonist, to the existing therapy, which included the highest tolerated dose of ACE inhibitors or AT1R antagonists plus hydrochlorothiazide (HCT) on 24 h ambulatory BP in uncontrolled hypertensive patients.
Methods
Patients
One hundred and seventy-eight consecutive outpatients had been included in the ESCAPE-IT trial (NCT02687178). These patients had hypertension that was not controlled by pre-existing treatment (either the maximum tolerated dose of ACE inhibitors or AT1R antagonists plus HCT) and were randomly assigned to be treated for 3 months with canrenone (50 or 100 mg/day) in addition to their existing treatment. One hundred and fifty-eight of those consecutive patients were submitted to 24 h ABPM (80 patients in the 50 mg arm and 78 patients in the 100 mg arm) and were evaluated in this study. The detailed study design has been described previously.24 This study presents a secondary analysis focused on ABPM. Besides ABPM, all patients had a complete clinical evaluation, office visit BP measurements, and routine laboratory examinations at baseline (pre-study canrenone addition) and 3 months after canrenone addition. One hundred and fifty patients completed the ABPM study with the two recordings (77 patients in the 50 mg canrenone arm and 73 in the 100 mg arm). In five patients, the quality of the recordings was not good (see later) even when the recordings were repeated either at baseline or at the 3-month evaluation, and three patients refused consent to repeat the ABPM.
Uncontrolled hypertension was defined as persistence of office BP values ≥140 mmHg for systolic BP and/or ≥90 mmHg for diastolic BP despite ongoing treatment. In all the patients, the persistence of high BP was confirmed by the 24 h values of ABPM (see later).
The study inclusion and exclusion criteria have been already described.24 Briefly, inclusion criteria included several parameters: 1) office BP values ≥140/90 mmHg; 2) undergoing ongoing therapy with maximal tolerated dose for at least 2 months of ACE inhibitors or AT1R antagonists plus HCT 25 mg/day; 3) both sexes; 4) age >45 and <75 years; 5) grade 1 or 2 hypertension; 6) body mass index (BMI) ≤35 kg/m2; and 7) giving informed consent to the study.
We excluded patients with the following characteristics: 1) office BP ≥180 mmHg for systolic and/or ≥110 mmHg for diastolic BP; 2) patients receiving any other antihypertensive drugs or cortisones; 3) acute clinical events occurring within 3 months before the study (after clinical evaluation of potential interferences); 4) previous myocardial infarction or ischemic/hemorrhagic stroke (1 year from study enrollment); 5) active cancer, diabetes, and/or alcohol or drug abuse; 6) actual or potential pregnancy and/or breastfeeding; 7) pre-existing conditions, including HIV infection, chronic hepatitis, hepatic cirrhosis, chronic heart failure, previous mastectomy or ovariectomy, and/or nephrotic syndrome; 8) known hypersensitivity to canrenone or its metabolites; 9) previous inclusion in other clinical studies (within 3 months before the study); and 10) denial of the study informed consent. Moreover, patients were excluded after laboratory examination evaluation if hyperkalemia (K+ >5 mEq/L), hyponatremia (Na+ <135 mEq/L), serum creatinine >1.5 mg/dL, hyperuricemia >10 mg/dL, and GFR calculated with modification of diet in renal disease formula <45 mL/min/1.73 m2 were present.25,26
Besides standard laboratory evaluations, the homeostasis model assessment of insulin resistance index (HOMA-IR) was calculated.27
Of the 158 patients, 39 (25%) received ACE inhibitors plus HCT, whereas 119 received AT1R antagonists plus HCT. Patients who were treated with statins or antiplatelet/anticoagulant drugs did not modify their treatment throughout the study.
Our study complied with the Declaration of Helsinki, and all the patients gave their informed consent to the study, which had been approved by the Ethics Committee (EC Gallarate-Va) and by the local Ethics Committee at each study site.
ABPM
All the enrolled patients underwent 24 h ABPM before the addition of canrenone to their existing treatment and again after 3 months of combination treatment. The 24 h noninvasive ABPM was performed by means of a Spacelabe 902017 (Spacelabs Healthcare, Edinburgh, UK) set to take one measurement every 15 min during the day (07:00 to 22:00 h) and every 20 min at night (22:00 to 07:00 h). When the quality of the ambulatory tracing was not sufficient (valid measures <80%), the patients underwent repeat monitoring on the following day. Reading and editing of the data were performed by a computerized program. Mean values of 24 h BP (mean arterial, systolic, diastolic, and pulse pressures) and heart rates were recorded. Pressures measured during the daytime and nighttime periods were considered in subsequent analysis together with the nocturnal reduction in BP percentage (< or >10%) that was calculated using the formula: ([diurnal value - nocturnal value]/diurnal value) ×100%. Uncontrolled BP values according to ABPM were 24 h systolic BP ≥130 mmHg and/or 24 h diastolic BP ≥80 mmHg. Moreover, for diurnal and nocturnal BPs, increased values were considered ≥135/85 and ≥120/70 mmHg, respectively.25
Statistical analysis
Descriptive statistics of continuous variables were reported as mean ± standard deviation (SD); categorical descriptive variables were reported as absolute rates and percentages.
The analysis of the efficacy and safety variables for both canrenone doses (50 and 100 mg) was carried out using the Student’s t-test for paired data in order to compare the values measured at the final visit with the values measured at the baseline visit. The chi-square test was used in case of categorical data. The analysis of the difference in efficacy and safety between doses of canrenone was carried out using one-way analysis of variance (ANOVA). Fisher’s exact test was used in cases of categorical data. A two-sided P<0.05 was indicated for statistical significance.
Results
In patients enrolled in the canrenone 50 mg group, the sex distribution was 50 males and 30 females with a mean age of 57.1±8.9 years and a BMI of 27.5±3.5 kg/m2; the patients in the canrenone 100 mg group consisted of 48 males and 30 females with a mean age of 57.6±9.2 years and a BMI of 27.4±3.6 kg/m2. Clinical and laboratory characteristics of the patients enrolled in the two dose regimen arms are shown in Table 1. At the 3-month combination treatment evaluation, both office systolic and diastolic and pulse pressure evaluation were significantly reduced (P<0.001) following the addition of 50 or 100 mg canrenone, whereas heart rate was similar at the two visits. A modest, but significant, increase in K+ was observed with both canrenone doses, and although GFR was unchanged following both doses, a modest increase in serum creatinine was noted during 100 mg treatment.
Table 1.
Clinical and laboratory characteristics at baseline and after 3 months of combination treatment
| Canrenone 50 mg
|
Canrenone 100 mg
|
|||
|---|---|---|---|---|
| Baseline | 3 months | Baseline | 3 months | |
| Patients (N) | 80 | 77 | 78 | 73 |
| Office SBP (mmHg) | 153.9±9 | 133.6±12.5*** | 154.8±9.4 | 131.2±12.8*** |
| Office DBP (mmHg) | 92.9±8.5 | 82.3±9.2*** | 94.8±7.6 | 82.4±7.8*** |
| Office PP (mmHg) | 60.9±12.4 | 51.3±10.8*** | 60±10.6 | 48.8±10.8*** |
| Clinical HR (beats/min) | 72.8±7.5 | 70.7±8.4 | 72.7±9.7 | 72.2±8.7 |
| Blood glucose (mg/dL) | 93.8±12.6 | 96.1±24.0 | 94.9±15.4 | 97.01±18.3 |
| HOMA-IR index | 2.61±1.89 | 3.11±2.09* | 2.63±2.02 | 2.67±1.69 |
| LDL-c (mg/dL) | 128.4±37.2 | 124.3±38.6 | 125.8±35.4 | 128.4±37.1 |
| Creatinine (mg/dL) | 0.92±0.19 | 0.94±0.18 | 0.87±0.18 | 0.92±0.22* |
| GFR (mL/min/1.73 m2) | 84.0±15.7 | 83.3±16.9 | 87.2±19.4 | 81.8±17.3 |
| Uricemia (mg/dL) | 5.82±1.64 | 5.58±1.55 | 5.33±1.62 | 5.59±1.58 |
| Na+ (mEq/L) | 141.5±2.6 | 141.2±3.3 | 141.7±2.7 | 141.2±3.7 |
| K+ (mEq/L) | 4.25±0.43 | 4.49±0.45* | 4.33±0.74 | 4.66±0.41* |
Notes: Data are reported as mean ± SD.
P<0.05 vs baseline values;
P<0.001 vs baseline values.
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure; HR, heart rate; HOMA-IR, homeostasis model assessment of insulin resistance index; LDL-c, low-density lipoprotein cholesterol; GFR, glomerular filtration rate; SD, standard deviation.
ABPM
The systolic and diastolic BPs (24 h, daytime, and nighttime) and mean arterial and pulse pressures were significantly reduced when canrenone was added to the pre-existing therapy (P<0.001; P<0.01 for nighttime pulse pressure; Table 2). Heart rate did not change during the second ambulatory recording.
Table 2.
ABPM results at baseline and after 3 months of combination treatment
| Canrenone 50 mg
|
Canrenone 100 mg
|
|||
|---|---|---|---|---|
| Baseline | 3 months | Baseline | 3 months | |
| Patients (N) | 80 | 77 | 78 | 73 |
| 24 h SBP (mmHg) | 138.8±10.2 | 125.6±9.9*** | 142.4±11.9 | 126.9±10.3*** |
| 24 h DBP (mmHg) | 84.6±8.6 | 76.6±7.9*** | 88.4±8.9 | 77.5±7.8*** |
| 24 h MAP (mmHg) | 103.5±7.9 | 93.7±7.7*** | 107.4±9.1 | 95.0±7.5*** |
| 24 h PP (mmHg) | 54.1±9.2 | 48.9±8*** | 53.8±9.3 | 49.3±9.8*** |
| 24 h HR (beats/min) | 72.4±9.6 | 72.7±7.1 | 73.4±8.6 | 75.2±9 |
| Daytime SBP (mmHg) | 142.7±10.4 | 129±10*** | 146.2±11.5 | 130.4±10.5*** |
| Daytime DBP (mmHg) | 88.2±8.9 | 79.8±8.1*** | 91.9±9.2 | 81±8.4*** |
| Daytime MAP (mmHg) | 107.1±8.2 | 96.9±7.9*** | 110.9±8.9 | 98.5±7.9*** |
| Daytime PP (mmHg) | 54.5±9.7 | 49.2±8.4*** | 54.3±9.4 | 49.4±9.9*** |
| Daytime HR (beats/min) | 75.3±10.2 | 75.6±8 | 76.4±9.2 | 78.3±10 |
| Nighttime SBP (mmHg) | 128.8±11.2 | 116.7±11.4*** | 131.8±14.9 | 118.4±11.8*** |
| Nighttime DBP (mmHg) | 75.6±9.1 | 68.6±8.8*** | 79.1±10.5 | 69.2±8.2*** |
| Nighttime MAP (mmHg) | 94.3±8.7 | 85.6±8.7*** | 97.8±11.3 | 86.8±8.6*** |
| Nighttime PP (mmHg) | 53.1±8.6 | 48±7.4*** | 52.7±9.7 | 49.3±9.9** |
| Nighttime HR (beats/min) | 65.2±9.4 | 65.5±7.2 | 65.4±7.9 | 67.6±8.3 |
Notes: Data are reported as mean ± SD.
P<0.01 vs baseline values;
P<0.001 vs baseline values.
Abbreviations: ABPM, ambulatory blood pressure monitoring; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; HR, heart rate; SD, standard deviation.
The degree of reduction in BP occurred in steady pattern: 1) Δ 24 h systolic BP at 50 mg/day was −13.5±11.2 mmHg; 100 mg/day was −16.1±13.5 mmHg (P= ns for 50 mg treatment vs 100 mg); 2) Δ 24 h diastolic BP at 50 mg/day was −8±8 mmHg; 100 mg/day was −11.2±8.4 mmHg (P<0.05 between the two doses); and 3) Δ 24 h mean arterial pressure at 50 mg/day was −9.9±8.4 mmHg; 100 mg/day was −12.8±9.4 mmHg (P<0.05 between the two doses).
Moreover, after considering the previously described thresholds for defining elevated 24 h BPs (described in the “Methods” section) at ABPM, it was observed that a significant number of patients in the 50 mg arm whose 24 h BP was not controlled by the pre-existing therapy achieved a normalized 24 h systolic or diastolic BP (P<0.05 for both BPs, normalized vs non-normalized) and in the 100 mg arm (P<0.05) (P= ns for 50 mg vs 100 mg) as shown in Figure 1. Twenty-four-hour BP was ≤130 mmHg for systolic and ≤80 mmHg for diastolic BP (both BPs after normalization) in 61% of patients after 50 mg canrenone addition and in 47.9% after 100 mg addition (Figure 2).
Figure 1.
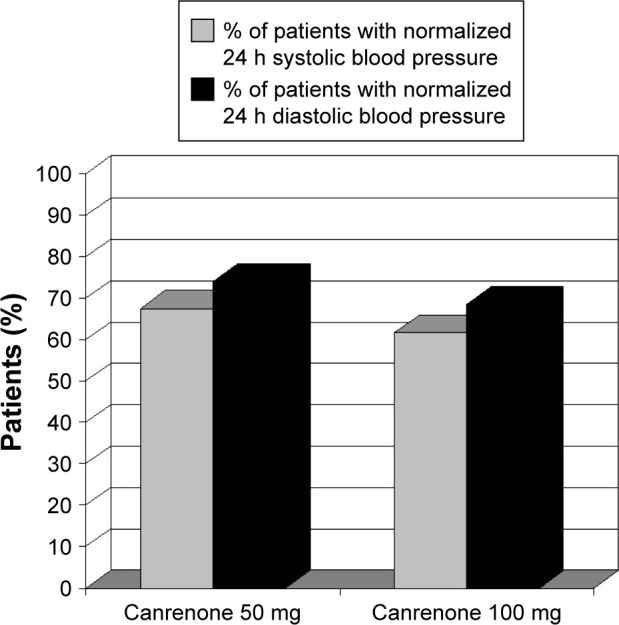
After the addition of canrenone, previously uncontrolled BPs (ie, 24 h systolic BP ≥130 mmHg; diastolic BP ≥80 mmHg) were normalized in 67.5% and 74% of the patients treated with 50 mg/day (systolic and diastolic BPs, respectively) and in 61.6% and 68.5% of the patients treated with 100 mg/day (P<0.05 for both BPs, normalized vs non-normalized).
Note: No statistically significant difference was found between the normalization of BPs at the two dosages (P= ns for 50 mg vs 100 mg).
Abbreviations: BP, blood pressure; ns, not significant.
Figure 2.
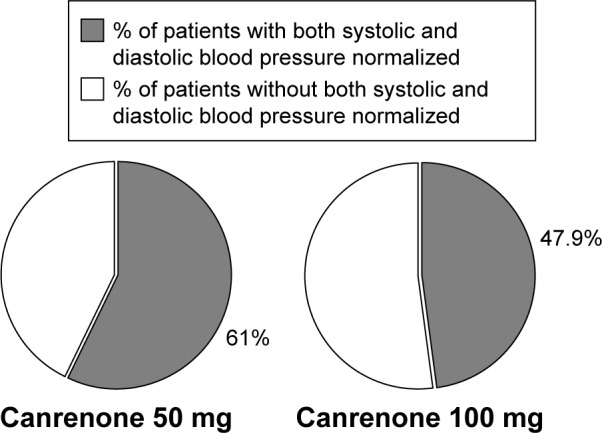
Twenty-four-hour BP was <130 mmHg for systolic and <80 mmHg for diastolic BP (ie, both BPs normalized) in 61% of patients after addition of 50 mg canrenone and in 47.9% of patients after addition of 100 mg.
Abbreviation: BP, blood pressure.
At baseline, in the 50 mg group, 47.5% of patients had a >10% nocturnal fall of systolic BP and 77.5% of diastolic BP; in the 100 mg group, 52.6% had >10% systolic and 76.9% diastolic BP reduction. After 3 months of combination therapy, 45.5% of patients treated with 50 mg canrenone had a reduced nocturnal systolic BP >10% of diurnal values and 76.6% of patients had a diastolic BP reduction >10%. In the 100 mg treated patients, 39.7% and 68.5% of patients had reduced nocturnal systolic and diastolic BPs, respectively, which were >10% with respect to diurnal values. When comparing baseline and 3-month treatments, no significant differences were found in nocturnal BP decrease, with either the 50 or 100 mg treatment.
Discussion
In the clinical setting, adding canrenone (50 or 100 mg) to the existing therapy, which included the highest tolerated dose of ACE inhibitor or AT1R antagonists plus HCT, resulted in a reduction in BP as assessed by 24 h BP monitoring. ABPM targets for 24 h systolic and diastolic BP were achieved in 67.5% and 74% of previously uncontrolled hypertensive patients in the 50 mg arm, respectively (P<0.05 for both BPs), and in 61.6% and 68.5% of patients in the 100 mg treatment arm, respectively (P<0.05).
To our knowledge, this is the first study describing BP reduction during ABPM upon canrenone addition (as for inclusion criteria) to agents blocking the vascular effects of angiotensin II in hypertensive stage 1 or 2 patients.
It is well known that the accuracy of BP measurements is higher if arterial pressure is monitored over time, preferably by ABPM.28,29 Moreover, the relevance of ABPM has been indicated in pharmacological trials.30 In our study, we evaluated the ambulatory 24 h ABPM to confirm BP, and therefore, we used the ABPM targets to identify uncontrolled and controlled patients before and throughout the study, thus giving reliable results for BP measurements.
Previously, spironolactone and eplerenone, either as add-on pre-existing therapy or as monotherapy, have been described to reduce BP in patients with essential hypertension, metabolic syndrome, those with refractory hyper-tensions undergoing dialysis, and patients with resistant hypertension.22,31–39 Moreover, spironolactone (if tolerated) was used as an intensified pharmacological treatment (control group) to compare the effect of renal denervation in patients with true resistant hypertension; this treatment yielded similar BP reductions.40
Our results show that canrenone was effective in reducing BP in patients already being treated with drugs able to block ACE or AT1R. Office visit systolic and diastolic BPs were significantly reduced after the addition of canrenone at the two doses. During ABPM, the Δ 24 h systolic BP at 50 mg/day was −13.5±11.2 mmHg, and at 100 mg/day, it was −16.1±13.5 mmHg. The Δ 24 h diastolic BP at 50 mg/day was −8±8 mmHg and at 100 mg/day was −11.2±8.3 mmHg. Although the degree of reduction was significantly higher for diastolic and mean BP in the 100 mg treated patients (P<0.05 between the two doses), no differences were found for systolic 24 h BP reduction, and interestingly, the number of patients achieving 24 h BP normalization was similar during the two treatment regimens.
A diminished nocturnal BP decrease has been associated with poor cardiovascular outcome.41 In our study, when comparing baseline and the 3-month treatments, no significant differences were found in nocturnal BP decrease as indicated by the number of patients with a nocturnal BP reduction >10% with respect to diurnal values with either the 50 or 100 mg treatment. Our patient’s selection, including those already treated with drugs interfering with AT1R transduction signals and in stage 1 or 2 hypertension, may possibly have influenced this parameter.
Peripheral pulse pressure is a marker of aging-associated arterial stiffening, and relationships associating pulse pressure, arterial stiffness, and renal function are observed mainly in patients 60 years of age or older.42,43 It has been recently confirmed in a large cohort of high-risk subjects that pulse pressure is associated with multiple adverse cardiovascular outcomes, and this value provides prognostic utility beyond that of mean arterial pressure.44 In our patients, pulse pressure was significantly reduced for 24 h, daytime, and nighttime values (P<0.001; P<0.01 for nocturnal BP during 100 mg treatment). These data, in conjunction with the preserved GFR after canrenone addition, may indicate a protective vascular effect.
Canrenone has been related to improved diastolic cardiac function in essential hypertensive patients and patients with mild systolic heart failure and metabolic syndrome; mineralocorticoid receptor antagonists have been described to ameliorate diastolic function and markers of cardiac fibrosis in patients with diastolic dysfunction and heart failure with preserved ejection fraction.45–47 In our study, the patients using statins did not modify their treatment throughout the study. It is well known that additive preventive effects on atherosclerosis can be obtained by combination therapy of anti-RAAS and lipid-lowering agents and that using these two classes of drugs can influence the inflammatory/fibrous environment and atrial fibrillation.48–50
As already reported for the whole population, we did not observe clinically relevant side effects in the group of patients undergoing ABPM, and in particular, no threatening hypotension episodes were seen during the 24 h BP monitoring.24 This may be due in part to patient selection, including those patients who were already tolerant of ACE or AT1R blockade in terms of renal perfusion. As expected based on previously published literature, an increase in serum K was observed in conjunction with a non-clinically relevant increase in serum creatinine at the higher doses.23 However, no patient had to stop the mineralocorticoid receptor antagonist because of severe hyperkalemia or incident renal failure, and GFR did not decrease during combination treatment.
Our study investigated the 3-month effects of canrenone addition to the existing maximal tolerated therapy with ACE inhibitors or AT1R plus HCT. Therefore, our results do not show the effects of mineralocorticoid receptor antagonists used as first-line antihypertensive therapy and may not apply to longer follow-up periods. Moreover, we acknowledge that we did not measure the serum levels of the selected drugs.
Conclusion
In a clinical setting of stage 1 or 2 hypertension, dual RAAS blockade obtained by adding canrenone to the maximal tolerated dose of ACE inhibitors or AT1R antagonists plus HCT was associated with a reduction in 24 h, daytime, and nighttime systolic and diastolic BPs and pulse pressures as demonstrated during ABPM. ABPM targets for 24 h systolic and diastolic BPs were achieved in a high percentage of previously uncontrolled hypertensive patients in both the 50 and 100 mg treatment arms in the absence of hypotensive episodes during both daytime and nighttime periods and/or other clinically relevant side effects.
Acknowledgments
The study was supported by THERABEL GiEnne Pharma, Italy. The sponsor provided financial support for the research and had no role in study design, collection, analysis, interpretation of data, in writing the report, or in the decision to submit the article for publication.
Footnotes
Disclosure
Massimo Vanasia is employed by Direzione Medica THERABEL GiEnne Pharma, Italy. The other authors report no conflicts of interest in this work.
References
- 1.Freis ED. Hypertension and atherosclerosis. Am J Med. 1969;46(5):735–740. doi: 10.1016/0002-9343(69)90024-2. [DOI] [PubMed] [Google Scholar]
- 2.Congiu T, Schembri L, Tozzi M, et al. Scanning electron microscopy examination of endothelium morphology in human carotid plaques. Micron. 2010;41(5):532–536. doi: 10.1016/j.micron.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Piepoli MF, Hoes AW, Agewall S, et al. European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016 2016 May 23; doi: 10.1093/eurheartj/ehw106. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016;23(6):636–648. doi: 10.1177/2047487315569401. [DOI] [PubMed] [Google Scholar]
- 5.Falcone C, Bozzini S, Guasti L, et al. Soluble RAGE plasma levels in patients with coronary artery disease and peripheral artery disease. Sci World J. 2013;2013:584504. doi: 10.1155/2013/584504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guasti L, Maresca AM, Schembri L, et al. Relationship between regulatory T cells subsets and lipid profile in dyslipidemic patients: a longitudinal study during atorvastatin treatment. BMC Cardiovasc Disord. 2016;16:26. doi: 10.1186/s12872-016-0201-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guasti L, Marino F, Cosentino M, et al. Cytokine production from peripheral blood mononuclear cells and polymorphonuclear leukocytes in patients studied for suspected obstructive sleep apnea. Sleep Breath. 2011;15(1):3–11. doi: 10.1007/s11325-009-0315-x. [DOI] [PubMed] [Google Scholar]
- 8.Marino F, Guasti L, Cosentino M, et al. Thyroid hormone and thyrotropin regulate intracellular free calcium concentrations in human polymorphonuclear leukocytes: in vivo and in vitro studies. Int J Immunopathol Pharmacol. 2006;19(1):149–160. [PubMed] [Google Scholar]
- 9.Patarroyo Aponte MM, Francis GS. Effect of angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists in atherosclerosis prevention. Curr Cardiol Rep. 2012;14(4):433–442. doi: 10.1007/s11886-012-0275-9. [DOI] [PubMed] [Google Scholar]
- 10.Marino F, Guasti L, Cosentino M, et al. Angiotensin II type 1 receptor expression in polymorphonuclear leukocytes from high-risk subjects: changes after treatment with simvastatin. J Cardiovasc Pharmacol. 2007;49(5):299–305. doi: 10.1097/FJC.0b013e31803d35ce. [DOI] [PubMed] [Google Scholar]
- 11.Marino F, Maresca AM, Cosentino M, et al. Angiotensin II type 1 and type 2 receptor expression in circulating monocytes of diabetic and hypercholesterolemic patients over 3-month rosuvastatin treatment. Cardiovasc Diabetol. 2012;11:153. doi: 10.1186/1475-2840-11-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marino F, Guasti L, Tozzi M, et al. Angiotensin type 1 receptor expression and interleukin-8 production in polymorphonuclear leukocytes of patients with peripheral arterial disease. J Cardiovasc Pharmacol. 2009;54(6):520–525. doi: 10.1097/FJC.0b013e3181bfadfd. [DOI] [PubMed] [Google Scholar]
- 13.Ferrario CM, Schiffrin EL. Role of mineralocorticoid receptor antagonists in cardiovascular disease. Circ Res. 2015;116(1):206–213. doi: 10.1161/CIRCRESAHA.116.302706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng KP, Arnold J, Sharif A, et al. Cardiovascular actions of mineralocorticoid receptor antagonists in patients with chronic kidney disease: a systematic review and meta-analysis of randomized trials. J Renin Angiotensin Aldosterone Syst. 2015;16(3):599–613. doi: 10.1177/1470320315575849. [DOI] [PubMed] [Google Scholar]
- 15.Briet M, Schiffrin EL. Vascular actions of aldosterone. J Vasc Res. 2013;50(2):89–99. doi: 10.1159/000345243. [DOI] [PubMed] [Google Scholar]
- 16.McGraw AP, McCurley A, Preston IR, Jaffe IZ. Mineralocorticoid receptors in vascular disease: connecting molecular pathways to clinical implications. Curr Atheroscler Rep. 2013;15(7):340. doi: 10.1007/s11883-013-0340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Te Riet L, van Esch JH, Roks AJ, van den Meiracker AH, Danser AH. Hypertension: renin-angiotensin-aldosterone system alterations. Circ Res. 2015;116(6):960–975. doi: 10.1161/CIRCRESAHA.116.303587. [DOI] [PubMed] [Google Scholar]
- 18.Grandi AM, Solbiati F, Laurita E, et al. Effects of dual blockade of renin-angiotensin system on concentric left ventricular hypertrophy in essential hypertension: a randomized, controlled pilot study. Am J Hypertens. 2008;21(2):231–237. doi: 10.1038/ajh.2007.47. [DOI] [PubMed] [Google Scholar]
- 19.Sartori M, Calò LA, Mascagna V, et al. Aldosterone and refractory hypertension: a prospective cohort study. Am J Hypertens. 2006;19(4):373–379. doi: 10.1016/j.amjhyper.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Vasan RS, Evans JC, Larson MG, et al. Serum aldosterone and the incidence of hypertension in nonhypertensive persons. N Engl J Med. 2004;351(1):33–41. doi: 10.1056/NEJMoa033263. [DOI] [PubMed] [Google Scholar]
- 21.Vongpatanasin W. Resistant hypertension: a review of diagnosis and management. JAMA. 2014;311(21):2216–2224. doi: 10.1001/jama.2014.5180. [DOI] [PubMed] [Google Scholar]
- 22.Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159–166. doi: 10.1038/jhh.2014.64. [DOI] [PubMed] [Google Scholar]
- 23.Esteras R, Perez-Gomez MV, Rodriguez-Osorio L, Ortiz A, Fernandez-Fernandez B. Combination use of medicines from two classes of renin-angiotensin system blocking agents: risk of hyperkalemia, hypotension, and impaired renal function. Ther Adv Drug Saf. 2015;6(4):166–176. doi: 10.1177/2042098615589905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Derosa G, Maffioli P, D’Avino M, et al. Efficacy and safety of two dosages of Canrenone as add-on therapy in hypertensive patients taking ace-inhibitors or angiotensin II receptor blockers and hydrochlorothiazide at maximum dosage in a randomized clinical trial: the ESCAPE-IT trial. Cardiovasc Ther. 2017;35(1):47–54. doi: 10.1111/1755-5922.12235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.ESH/ESC Task Force for the Management of Arterial Hypertension 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31(10):1925–1938. doi: 10.1097/HJH.0b013e328364ca4c. [DOI] [PubMed] [Google Scholar]
- 26.Klahr S, Levey AS, Beck GJ, et al. For the Modification of Diet in Renal Disease Study Group: the effects of dietary protein restriction and bloodpressure control on the progression of chronic renal disease. N Engl J Med. 1994;330:877–884. doi: 10.1056/NEJM199403313301301. [DOI] [PubMed] [Google Scholar]
- 27.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien E. Why is it that we continue to deny patients ambulatory blood pressure monitoring? Hypertension. 2016;67(3):484–487. doi: 10.1161/HYPERTENSIONAHA.115.06777. [DOI] [PubMed] [Google Scholar]
- 29.Siu AL. U.S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163(10):778–786. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 30.Bakris GL, Lindholm LH, Black HR, et al. Divergent results using clinic and ambulatory blood pressures: report of adarusentan-resistant hypertension trial. Hypertension. 2010;56(5):824–830. doi: 10.1161/HYPERTENSIONAHA.110.156976. [DOI] [PubMed] [Google Scholar]
- 31.Ni X, Zhang J, Zhang P, et al. Effects of spironolactone on dialysis patients with refractory hypertension: a randomized controlled study. J Clin Hypertens (Greenwich) 2014;16(9):658–663. doi: 10.1111/jch.12374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White WB, Carr AA, Krause S, Jordan R, Roniker B, Oigman W. Assessment of the novel selective aldosterone blocker eplerenone using ambulatory and clinical blood pressure in patients with systemic hypertension. Am J Cardiol. 2003;92(1):38–42. doi: 10.1016/s0002-9149(03)00461-2. [DOI] [PubMed] [Google Scholar]
- 33.Václavík J, Sedlák R, Plachy M, et al. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension. 2011;57(6):1069–1075. doi: 10.1161/HYPERTENSIONAHA.111.169961. [DOI] [PubMed] [Google Scholar]
- 34.Flack JM, Oparil S, Pratt JH, et al. Efficacy and tolerability of eplerenone and losartan in hypertensive black and white patients. J Am Coll Cardiol. 2003;41(7):1148–1155. doi: 10.1016/s0735-1097(03)00054-8. [DOI] [PubMed] [Google Scholar]
- 35.de Souza F, Muxfeldt E, Fiszman R, Salles G. Efficacy of spironolactone therapy in patients with true resistant hypertension. Hypertension. 2010;55(1):147–152. doi: 10.1161/HYPERTENSIONAHA.109.140988. [DOI] [PubMed] [Google Scholar]
- 36.Suzuki H, Shuto H, Shuto C, et al. Eplerenone, an aldosterone blocker, is more effective in reducing blood pressure in patients with, than without, metabolic syndrome. Ther Adv Cardiovasc Dis. 2012;6(4):141–147. doi: 10.1177/1753944712452191. [DOI] [PubMed] [Google Scholar]
- 37.Bomback AS, Muskala P, Bald E, Chwatko G, Nowicki M. Low-dose spironolactone, added to long-term ACE inhibitor therapy, reduces blood pressure and urinary albumin excretion in obese patients with hypertensive target organ damage. Clin Nephrol. 2009;72(6):449–456. doi: 10.5414/cnp72449. [DOI] [PubMed] [Google Scholar]
- 38.Pelliccia F, Rosano G, Patti G, Volterrani M, Greco C, Gaudio C. Efficacy and safety of mineralocorticoid receptors in mild to moderate arterial hypertension. Int J Cardiol. 2015;200:8–11. doi: 10.1016/j.ijcard.2014.10.150. [DOI] [PubMed] [Google Scholar]
- 39.Pelliccia F, Patti G, Rosano G, Greco C, Gaudio C. Efficacy and safety of eplerenone in the management of mild to moderate arterial hypertension: systematic review and meta-analysis. Int J Cardiol. 2014;177(1):219–228. doi: 10.1016/j.ijcard.2014.09.091. [DOI] [PubMed] [Google Scholar]
- 40.Rosa J, Widimský P, Toušek P, et al. Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the Prague-15 study. Hypertension. 2015;65(2):407–413. doi: 10.1161/HYPERTENSIONAHA.114.04019. [DOI] [PubMed] [Google Scholar]
- 41.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31(9):1731–1768. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 42.Safar ME, Plante GE, Mimran A. Arterial stiffness, pulse pressure, and the kidney. Am J Hypertens. 2015;28(5):561–569. doi: 10.1093/ajh/hpu206. [DOI] [PubMed] [Google Scholar]
- 43.Wang Y, Hu Y, Li Y, et al. Association of renal function with the ambulatory arterial stiffness index and pulse pressure in hypertensive patients. Hypertens Res. 2012;35(2):201–206. doi: 10.1038/hr.2011.167. [DOI] [PubMed] [Google Scholar]
- 44.Selvaraj S, Steg PG, Elbez Y, et al. Pulse pressure and risk for cardiovascular events in patients with atherothrombosis: from the REACH Registry. J Am Coll Cardiol. 2016;67(4):392–403. doi: 10.1016/j.jacc.2015.10.084. [DOI] [PubMed] [Google Scholar]
- 45.Grandi AM, Imperiale D, Santillo R, et al. Aldosterone antagonist improves diastolic function in essential hypertension. Hypertension. 2002;40(5):647–652. doi: 10.1161/01.hyp.0000036399.80194.d8. [DOI] [PubMed] [Google Scholar]
- 46.de Simone G, Chinali M, Mureddu GF, et al. Effect of canrenone on left ventricular mechanics in patients with mild systolic heart failure and metabolic syndrome: the AREA-in-CHF study. Nutr Metab Cardiovasc Dis. 2011;21(10):783–791. doi: 10.1016/j.numecd.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 47.Pandey A, Garg S, Matulevicius SA, et al. Effect of mineralocorticoid receptor antagonists on cardiac structure and function in patients with diastolic dysfunction and heart failure with preserved ejection fraction: a meta-analysis and systematic review. J Am Heart Assoc. 2015;4(10):e002137. doi: 10.1161/JAHA.115.002137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koh KK, Han SH, Oh PC, Shin EK, Quon MJ. Combination therapy for treatment or prevention of atherosclerosis: focus on the lipid-RAAS interaction. Atherosclerosis. 2010;209(2):307–313. doi: 10.1016/j.atherosclerosis.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chaugai S, Sherpa LY, Sepehry AA, Arima H, Wang DW. Effect of RAAS blockers on adverse clinical outcomes in high CVD risk subjects with atrial fibrillation: a meta-analysis and systematic review of randomized controlled trials. Medicine (Baltimore) 2016;95(26):e4059. doi: 10.1097/MD.0000000000004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dentali F, Gianni M, Squizzato A, et al. Use of statins and recurrence of atrial fibrillation after catheter ablation or electrical cardioversion. A systematic review and meta analysis. Thromb Haemost. 2011;106:363–370. doi: 10.1160/TH10-10-0660. [DOI] [PubMed] [Google Scholar]


