Abstract
Background
Failure to address social determinants of health (SDH) may contribute to the problem of readmissions in high-risk individuals. Comprehensive shared care plans (CSCP) may improve care continuity and health outcomes by communicating SDH risk factors across settings.
Purpose
The purpose of this study to evaluate the state of knowledge for integrating SDH into a CSCP. Our scoping review of the literature considered 13,886 articles, of which seven met inclusion criteria.
Results
Identified themes were: integrate health and social sectors; interoperability; standardizing ontologies and interventions; process implementation; professional tribalism; and patient centeredness.
Discussion
There is an emerging interest in bridging the gap between health and social service sectors. Standardized ontologies and theoretical definitions need to be developed to facilitate communication, indexing, and data retrieval.
Conclusions
We identified a gap in the literature that indicates that foundational work will be required to guide the development of a CSCP that includes SDH that can be shared across settings. The lack of studies published in the United States suggests that this is a critical area for future research and funding.
Keywords: Social determinants of health, Patient care planning, Interdisciplinary communication, Health information exchange, Coordinated care
Introduction
In 2016, representatives from the U.S. Department of Health and Human Services outlined a vision for the future of multidisciplinary shared care planning, recognizing that poor individual health outcomes may evolve from social inequities; thereby, cascading into public socioeconomic burdens (Baker et al., 2016). The proposed comprehensive shared care plan (CSCP) aims to use health information technology (HIT) to align key stakeholders via the interoperable exchange of meaningful, timely, and actionable patient care information that can be shared between providers and settings. Perhaps most importantly, the national vision for a CSCP is one that is holistic, places the individual at the center of care, and includes information about community-based needs and services over time (Baker et al., 2016). Social determinants of health (SDH), defined as the conditions in which a person is born, lives, grows, works, and ages, include factors such as socioeconomic status, neighborhood environment, and education (World Health Organization, 2016). Thus, unmet social needs have the potential to influence the overall wellness of individuals and their communities.
For instance, there is a wide body of literature that indicates that those individuals living with low socioeconomic status have more chronic illness, receive less preventative care, and die earlier than more advantaged income groups (Chen, Weider, Konopka, & Danis, 2014). Recognizing that HIT may facilitate the collection of SDH information to improve practice and policy, Chen et al. (2014) recommended routinely assessing and recording socioeconomic status into the electronic health record. Prioritizing a comprehensive approach to health care that includes routine screening and early identification of the entirety of an individual’s social context would enable the multidisciplinary team to incorporate tailored interventions into the CSCP, thereby synchronizing care and ideally improving overall individual and population-level health outcomes.
The importance of social determinants in keeping people healthy is not a new topic. Within the social sciences, seminal work by Evans and Stoddard in their book, Why are some people healthy and others not? (Evans, Barer, & Marmor, 1994), clearly articulates that health was not something that was produced by the health care system but that the context of people’s lives played a significant role in how healthy they are. This concept has been reinforced by decades of research on health disparities. Although the health care system acknowledges this impact at the population level, it rarely becomes an important part of the interprofessional conversation about how to manage an individual’s chronic illness. An example of how this work influenced nurse anthropologists is in a model that examined the impact of social factors on the health of frail elders in cultural communities in the rural United States and Philippines (Hewner, 2001).
Recent calls to include SDH into routine health assessments and to incorporate deficits in social factors as part of a plan of care that moves with the individual across health care settings have been proposed. The assumption is that this is a practice that is well accepted and that all we need to do is figure out how to add this information to an interprofessional care plan as discrete data so that it can be incorporated in all health care settings. The authors observed that although SDH and care planning have been discussed in the literature for decades, it is not clear that a body of evidence exists that demonstrates how to best incorporate SDH into multidisciplinary care planning at the practice level.
Method
The purpose of this scoping review is to rapidly evaluate the current state of knowledge of including information about social factors that affect health and recovery into a multidisciplinary care plan and to identify where there may be gaps in the literature to guide future research priorities. Our first step was to look for the evidence to support the assumption that health professionals know how to incorporate SDH into a care plan as people transition between settings. The method include five stages (a) identifying the research question, (b) identifying relevant studies, (c) study selection, (d) charting the data, and (e) collating, summarizing, and reporting the results (Arksey & O’Malley, 2005).
Stage 1: Identifying the Research Question
Our choice to use a scoping review was guided by the research question: What is the state of the science of incorporating SDH into a CSCP for individuals at risk for hospitalization?
Stage 2: Identifying Relevant Studies
S.H. and S.S.S. worked closely with a health sciences librarian to identify keywords and develop a rigorous search strategy for this scoping review (Table 1). Identifying appropriate search terms was challenging because of the fact that the term social determinants of health was not explicitly indexed as a Medical Subject Heading term until 2014 (National Library of Medicine (PubMed), 2016). Moreover, there is no consensus on the definition of shared care planning (Gu et al., 2015). To address this issue, we elected to cast a broad net and seek studies that focused on care planning in a general sense. We assumed that evidence of incorporating SDH information into the CSCP would become evident as we conducted our review.
Table 1.
Search Strategy Key Terms
| Longitudinal care planning |
| “LCP” |
| Shared care plans |
| Personalized care plans |
| Patient care planning |
| Continuity of patient care |
| Cooperative behaviour |
| Interdisciplinary communication |
| Patient care team |
| Meaningful use |
| Patient-centered care |
| Organization and administration |
| Health information exchange |
| Delivery of health care |
| System integration |
| Coordinated care |
| Multidisciplinary |
An a priori protocol of inclusion and exclusion criteria was created to guide the identification of relevant studies. The following inclusion criteria were established: Population: Adults 18 years and older who were at risk for hospitalization. Intervention: Any study that incorporated SDH information into a multidisciplinary care plan. Outcome: There were no limitations placed on study outcomes. Design: Any published study with a level of evidence on the hierarchy between systematic review (level I) and expert opinion (level VII) was considered (Polit & Beck, 2012). We limited our studies to those published in English, and we did not limit by date of publication.
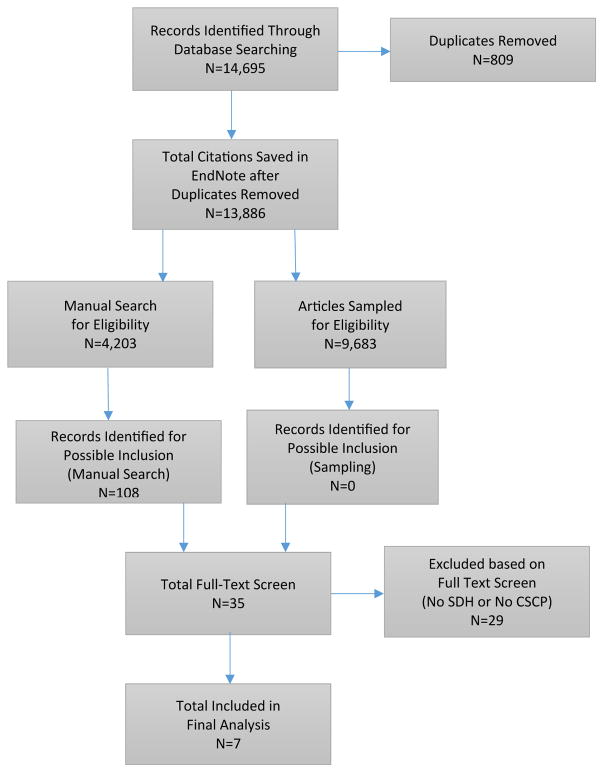
In total, 14,695 articles were identified and imported from PubMed (n = 10,734), Medline/CINAHL (n = 3,839), and Web of Science (n = 122) into an EndNote X7 file, and 13,886 articles remained after removing duplicates (n = 809) (Figure 1). In addition, the authors used a snowball technique to identify potentially relevant articles based on ancestral searches of references lists, manually sorting through journals of interest, and by other means such as personal networking and conference attendance. We continued to monitor these sources throughout the review process that ranged from November 9, 2015 through September 10, 2016 and did not discover any additional articles for review that were not in our original file.
Figure 1.
Prisma diagram of study protocol.
Stages 3 and 4: Study Selection and Charting the Data
Identifying a large number of studies is a common challenge when conducting a scoping review. Therefore, it was necessary to develop a data reduction strategy. Various methods have been used in the past for pragmatic reasons such as limiting included studies to a single language to avoid the need for translation services (Arksey & O’Malley, 2005; Pham et al., 2014). Our approach was as follows: (a) manually extract known relevant studies; (b) search the original database for relevant articles using the EndNote search functionality; (c) search the original database for irrelevant articles using the EndNote search functionality to reduce the data set; and (d) sample remaining articles in the database for validation. Studies were selected if they met inclusion criteria as described in stage 2.
Step A: Articles previously known to the authors with potential relevance were extracted for a full-text screening. Steps B and C: The search function in EndNote was set to “any field” to filter the remaining database for articles that were more likely to meet inclusion criteria using terms such as a keyword or specific author name. For example, the author “Rigby” was searched based on known relevant work, and the identified references underwent a title and abstract screen (S.S.S.). Likewise, keywords that were unlikely to yield relevant studies (such as the word child) were searched, and those articles also underwent a title and abstract screen. This process was repeated until the database appeared to be saturated.
Articles identified as potentially meeting inclusion criteria were independently screened by two reviewers (S.H. and F.M.) for eligibility and placed into a keep folder in EndNote (n = 108). Differences in selected articles were discussed or arbitrated by the third reviewer (S.S.S.). About 35 articles meeting inclusion criteria received full-text screening and had data extracted into a matrix (S.H., S.S.S., and F.M.) (Garrard, 2011). About seven articles were included in the final analysis (S.S.S. and S.H.) (Figure 1).
A quality acceptance sampling plan (International Organization for Standardization (ISO), 1999) was applied in step D to the remaining 9,683 studies to validate that all relevant articles had been extracted from the primary data set (S.C. and S.S.S.). This method is typically used in manufacturing operations and quality assurance processes to determine the acceptability of a lot of material or components. The ISO sampling approaches are based on the idea of identifying defects in each item inspected. Our process looked for two types of defects: defect 1—identification of new exclusion criteria or keywords that had not yet been previously identified and applied and defect 2—identification of new themes that had not yet been identified in the current set of reviewed articles. For this step, we defined the threshold of maximum allowable defects, known as the acceptance quality limit, to be 1% (α = 0.05; β = 0.10). Therefore, if we identified more than four of 200 of sampled articles from the remaining 9,683 studies to be relevant, then we would have rejected our premise and determined that there were remaining articles in the database to review. We set the threshold at six of 200 sampled articles. Our sampling plan revealed that there were zero unidentified themes noted; therefore, we determined that our search efforts had reached saturation and that it would be appropriate to proceed.
Results
Stage 5: Collating, Summarizing, and Reporting the Results
Seven articles ranging in date from 1996 to 2015 were deemed to meet the inclusion criteria for our scoping review of the literature (Table 2). The following themes were identified: integrate health and social services, interoperability, standardizing ontologies and interventions, process implementation, professional tribalism (not respecting the values of other professions), and patient centeredness. For example, in 1996, Boydell and McAllister (1996) sought to bring national leaders from 14 countries within across the European Union (EU) together in Belfast, Ireland, to elicit a consensus for the development of a prototype for the integration of health and social care needs to promote aging in place (Boydell & McAllister, 1996). The workgroup members recommended that care planning be patient centered and supported by a modular open-architecture health information system that enables the collection, aggregation, and dissemination of relevant social status information including population needs and outcomes. The leaders recommended that SDH assessment information should include client-identified goals, mental health needs, perceived well-being, and be appropriate for use across cultures. A model, the EPIC Assessment System, was developed based on the recommendations.
Table 2.
Data Extraction of Key Information for Synthesis and Quality Appraisal
| Author, Title, Journal | Year | Purpose | Design | Population | Setting | Results | Limitations |
|---|---|---|---|---|---|---|---|
| Boydell, L., & McAllister, B., European prototype for integrated care (EPIC), International Journal of Health Care Quality Assurance | 1996 | To develop a prototype Information system for integrated care between health and social care professionals | Survey of national leaders followed by a national conference of medical association & specialist associations, and range of experts in care of the elderly for consensus seeking | Multidisciplinary leaders throughout the EU (14 countries) | Conference held in Belfast, Ireland, in 1993 | Consensus: Information needs to be standardized, instrument to be short, valid, & reliable, crosscultural, assessments to be staged, and in addition to health information, instrument needs to include mental status and perceived well-being with client-identified goals (patient centered). Open-source modular EPIC-EASY tool developed |
Article more than 20 years old; quality of evidence is low (expert opinion only); focus on elderly only; few SDH included; potential for informing CSCP assessment element development only; unable to locate recent related studies |
| Self, R., Rigby, A., Leggett, C., & Paxton, R., Clinical decision support tool: A rational needs-based approach to making clinical decisions, Journal of Mental Health | 2008 | To develop and validate an interoperable CDS tool of care packages for standardizing mental health and other social care planning needs across disciplines and care settings | Sought multidisciplinary professional consensus; participatory action research; workshops; statistical and data science methods for clustering (wards, k-means, & dendrogram); expert panels | Three clinical managers; 3 psychiatrists; 2 clinical psychologists; 12 nurses; 3 social workers; and 3 occupational therapists | United Kingdom (England) | Identification and standardization of 13 clinically meaningful clusters of shared needs & intervention items by MH characteristics. A shared vocabulary for needs, aims, and activities was agreed on for CSCP | Low level of evidence; care packages developed but not tested; no current studies related to CSCP found; lacks patient & caregiver perspectives, focus primarily on MH needs with less emphasis on other SDH |
| Rigby, M., Hill, P., Koch, S., & Keeling, D., Social Care informatics as an essential part of holistic health care: A call for action, International Journal of Medical Informatics | 2011 | To gather a crossdisciplinary consensus on how to use informatics to integrate person-centered holistic care needs (health & social care) | Exploratory workshop to find common ground on key issues | EU 15 countries, 23 participants (social work, medicine, nursing, law, ethics, informatics, psychology, health management, and policy professionals) | United Kingdom | Unanimous declaration for action using informatics for including social needs into health care needs: identifying information and communication needs for integrating health & social care; need for shared ontologies & standards; shared access to information; automated discovery of knowledge in systems; citizen empowerment | Low level of evidence (expert opinion only); high-level discussion identifying needs for the foundational development of a CSCP |
| Poulymenopoulou, M., Papakonstantinou, D., Malamateniou, F., & Vassilacopoulos, G., Using a patient-centered approach for health and social care integration, Studies in Health Technology & Informatics | 2012 | To propose a BPM framework for integrating and Redesigning Information sharing & process activities for health and social care Delivery | Conceptual framework using a case study | Prototype | Greece | System to be patient centered; multidisciplinary & interoperable. Four-stage model: process modeling, process redesign, service modeling, workflow modelling, & prototypes (BPEL) models | Theoretical, conceptual model. Remains untested |
| MacNaughton-Doucet, L., Determinants of health in discharge planning for seniors: Asking the right questions, Canadian Journal on Aging | 2013 | Proposes the use of an SDH framework for the development of a common language to support a multidisciplinary approach to bridging gaps during discharge planning | Conceptual framework using a case study | Not applicable | Canada | Recommendations for policy, practice, and research include enhancing policies for systematically incorporating SDH into discharge planning & evaluation of interdisciplinary team understanding Propose a framework for hospital discharge planning incorporating social determinants of health for CSCP |
Theoretical conceptual model. Remains untested. This article appears to have no subsequent citations |
| Atherton, I., Lynch, E., Williams, A., & Witham, M., Barriers and solutions to linking and using health and social care Data in Scotland, British Journal of Social Work | 2015 | To share the Scottish experience of integrating social and health data, to better understand how stakeholders want to use the data, and to map out a plan for forward progress | Group plenary sessions with themes extracted | Multidisciplinary experts from government, academia, nursing, and public health | Scotland | Key barriers included mapping trajectories in health and social care, refining identification of those at risk, evaluation of interventions (especially public health), improving data quality, and building integrated services. Solutions: improving communication between providers and users, improving communication, understanding content, clear guidance to system developers, improved engagement with the public | Low level of evidence (expert opinion only); high-level discussion identifying needs for the foundational development of a CSCP |
| Ramgard, M., Blomqvist, K., & Petersson, P., Developing health and social care planning in Collaboration, Journal of Interprofessional Care | 2015 | To identify barriers and opportunities for interprofessional collaboration for HSCPC for older persons living at home | Participatory action research; reflective dialogs; meetings recorded and transcribed for content analysis | 18 RNs, physical or Occupational therapists, social workers, senior managers, and general practitioners from 3 Municipalities | Sweden | High status professionals may be a barrier to interprofessional collaboration. Open communication flattened hierarchies and placed the person at the center of care. Recommendations were adopted by 2 municipalities | Low level of evidence (expert opinion only); local-level solution & likely unrealistic to implement on a large scale; SDH for older adults only; identifies barriers to CSCP but no solutions All participants were females |
Note. BPM, business process management; BPEL, business process execution language; CDS, Cancer Decision Support; CSCP, comprehensive shared care plan; EPIC-EASY, European prototype for integrated care-Epic Assessment System; EU, European Union; HSCPC, health and social care planning; MH, mental health; RNs, registered nurses; SDH, social determinants of health.
Similar consensus-seeking workgroups of multidisciplinary leaders in the field were assembled across Europe from 2011 to 2015 (Atherton, Lynch, Williams, & Witham, 2015; Ramgard, Blomqvist, & Petersson, 2015; Rigby, Hill, Koch, & Keeling, 2011). Rigby et al. (2011) brought together 23 participants from 15 countries within the EU for the identification of key issues for social care using informatics to improve the harmonization of social and health needs across settings. Multidisciplinary professionals included members from health care, social care, and informatics backgrounds. Key themes in this study also included using informatics for integrating social and health care needs. The stakeholders concluded that harmonization will require identifying needs for information and communication sharing, standardizing ontologies and standards, improving access to information, automated discovery of knowledge in databases, and citizen empowerment. These key themes were echoed in a similar study undertaken in Scotland (Atherton et al., 2015), which additionally pointed out that linked data may make it possible to better understand client populations, map trajectories of decline, and help identify risk groups but that there are many barriers to overcome such as obtaining consent for data sharing.
Ramgard et al. (2015) used participatory action research methods that brought together 18 individuals from three municipalities in Sweden. The participants included registered nurses, physical and occupational therapists, social workers, managers, and general practitioners. The authors identified interprofessional communication among high status professionals as a potential impediment to collaboration because of professional tribalism. These barriers also included organizational structures and geographical distance; uncertainty regarding knowledge and different value systems; and respecting other people’s knowledge and perspectives as key themes (Ramgard et al., 2015). The authors recommended a flattening of hierarchies and placing the care recipient at the center of planning to facilitate communication.
Among the included studies were two proposed theoretical frameworks (MacNaughton-Doucet, 2013; Poulymenopoulou, Papakonstantinou, Malamateniou, & Vassilacopoulos, 2012). Canadian nurse researcher, MacNaughton-Doucet, presented a framework to include SDH information into the discharge planning processes for the development of a CSCP (MacNaughton-Doucet, 2013). She recommends elevating staff education and the creation of the CSCP up to the organizational level to ensure that a systematic approach to incorporating SDH into the discharge planning process occurs. Poulymenopoulou et al. (2012) used a business process model of change to outline a four-stage approach to redesign care so that it is patient centered. The authors use a prototype case study to illustrate how an individual’s transfer from home by emergency personnel to the emergency department could be improved by using HIT to integrate longitudinal health and social care needs information. They proposed that a patient-centered, multidisciplinary, and interoperable information system could improve interactions between health care personnel, reduce errors and redundancies, and deliver targeted information to the right person at the right time. This approach effectively bridges the gap between the organization and the individual’s health and social context, “through the creation of a longitudinal health and social history that is available at any time and from any computer at any location” (Poulymenopoulou et al., 2012, p. 470).
Self, Rigby, Leggett, and Paxton (2008) used an innovative mixed-methods approach to develop and validate an interoperable clinical decision support tool for multidisciplinary providers that “…conveys professional understandings and assessments during care planning in a way that is accessible to people from a wide range of professional backgrounds, and service users and carers” (abstract) for individuals receiving mental health services in England. This study is an important step toward incorporating decision support into CSCPs to ensure that patient-centered interoperable systems are available to standardize social needs care planning across disciplines and care settings. The study combined the knowledge of three clinical managers, three psychiatrists, two clinical psychologists, 12 nurses, three social workers, and three occupational therapists via a participatory action research workshop. The workshop findings were combined with statistical and data science methods (k-means algorithm) to create 13 clinically meaningful clusters of aims, activities, and services that grouped patients together based on similar mental health characteristics and social support needs. These clusters were deemed to be clinically relevant and described in a shared language that was agreed on by the multidisciplinary participants. The identification and clustering of shared patient needs and care interventions make it possible to standardize approaches to care for use in a multidisciplinary interoperable system that can be shared across settings.
Discussion and Recommendations
Care transitions can be complicated by chronic comorbidities, low socioeconomic status, and advancing age. The results of this study support the recent recommendations set forth by the Department of Health and Human Services (Baker et al., 2016). However, the findings also illustrate the fact that the current state of the science of incorporating SDH into CSCP is only emerging. For example, we noted the lack of an agreed on definition for the most basic concepts of CSCP during our review, as care planning in this context was described as: shared care planning, longitudinal care planning, and multidisciplinary care planning, to name a few. Certainly, defining concepts is key to the foundation of any rigorous scientific inquiry and for future work in this area. Clearly, a rigorous concept analysis for shared care planning is urgently needed.
It is also clear from this review that there is an emerging interest in bridging the gap between health and social service sectors as evidenced by the fact that most of the included studies shared similar themes and were published very recently (between 2011 and 2015) and recent recommendations by the Centers for Medicare and Medicaid Services (CMS) for acute care hospitals to consider the social context and psychosocial needs of individuals during discharge planning (CMS, 2015). Moreover, we did not identify any relevant literature before 1996, which supports the notion that interoperable HIT is necessary for the feasible creation of actionable multidisciplinary CSCPs. In addition, we find it important to point out the fact that not a single study identified for this scoping review was conducted within the United States, which suggests that there are policy-driven initiatives within the EU and Canada to integrate social and health needs data that are not occurring similarly in the United States. The lack of studies within the United States is an important key finding of this scoping review and suggests that this is a critical area for future research and funding.
International experts appear to agree that CSCP needs to be patient centered and include social needs that tell the patient’s story (Boydell & McAllister, 1996; Poulymenopoulou et al., 2012; Varpio et al., 2015). Rapid technological innovation that includes increasing storage capacity, portable devices, and processing speeds make it possible for modern health records to be intelligent, dynamic, and shared seamlessly between providers and settings, in real time. However, workflows and interprofessional communication practices may serve as barriers to implementation that may be compounded by the challenges of integrating care between disparate and geographically distant health and social service sectors (Hagglund, Chen, & Koch, 2011; MacNaughton-Doucet, 2013; Poulymenopoulou et al., 2012; Ramgard et al., 2015).
Interoperability is fundamental for integrating SDH into CSCP processes. This will likely require policy-level involvement to delineate roles and responsibilities, provide guidance to systems developers, create inter-operability standards, establish reimbursement mechanisms, and promote the interlinking of health and social care networks. Baker et al. (2016) pointed out that the U.S. government may facilitate the alignment of key stakeholders by providing remunerative mechanisms to support the adoption of CSCPs such as accessing federal and state funding under the Health Information Technology for Economic and Clinical Health Act. Moreover, interoperability is dependent on the development of multidisciplinary care priorities, shared ontologies, and horizontal integration at the professional and systems levels that will ultimately require the flattening of hierarchies for the development of standardized care pathways that are meaningful to a variety of disciplines (Ramgard et al., 2015).
We have made every effort to ensure rigor in our study by adhering as closely as possible to accepted methodological processes of a scoping literature review. We have strived for methodological transparency by drawing on salient reporting standards established by systematic review methods, such as reporting our search terms, using multiple screeners, including a matrix of included studies, and by outlining our process using a PRISMA diagram. The primary limitation of our study is based on the massive volume of articles that were obtained by casting such a wide net. This occurred because of the fact that it is not currently possible to extract articles that are specific to social factors affecting health outcomes by using SDH as a keyword. Therefore, it was necessary to infer how SDH were incorporated into the CSCP using related words and concepts such as socioeconomic status or demographic information. We believe that our approach for sampling the remaining articles has a precedent, was rigorous, logical, and transparent. Moreover, we feel confident that the state of the science has been established with this review as evidenced by the fact that even the most recent articles that were included consistently demonstrate a low level of evidence primarily in the form of expert opinion. However, we recognize that it is quite possible that pertinent studies were not identified because of the lack of systematic indexing of SDH and established definitions for care planning, which makes it difficult to recognize similar themes.
Conclusion
We have identified a large gap in the literature for how to best incorporate SDH information into the CSCP. Future work should begin with the basics of scientific discovery, which evolve from fundamental processes such as the development of theoretical definitions of a CSCP. The creation of a theoretical framework will also be necessary to guide future studies for testing approaches to incorporate SDH into multidisciplinary care planning. Research that creates a shared nomenclature that is meaningful to all disciplines and that incorporates and tests the standardized assessment of SDH into CSCP will help elevate the level of evidence and establish a firm scientific foundation. Moreover, CSCP would ideally have a holistic focus and should include social and health information that transcends the life span, including the integration of information that ranges from childhood conditions that spill over into adulthood, to the inclusion of advance care planning preferences that outline the individual’s goals for care at the end of life.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We extend a heartfelt thank you to Sharon Murphy, Health Sciences Librarian, for your sage advice and unwavering guidance.
References
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. [Google Scholar]
- Atherton IM, Lynch E, Williams AJ, Witham MD. Barriers and solutions to linking and using health and social care data in Scotland. British Journal of Social Work. 2015;45(5):1614–1622. [Google Scholar]
- Baker A, Cronin K, Conway P, DeSalvo K, Rajkumar R, Press M. Making the comprehensive shared care plan a reality. 2016 Retrieved from http://catalyst.nejm.org/making-the-comprehensive-shared-care-plan-a-reality/
- Boydell L, McAllister B. European prototype for integrated care (EPIC) Computer Methods and Programs in Biomedicine. 1996;45(1–2):47–49. doi: 10.1016/0169-2607(94)90014-0. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) 80 FR 68125, revision to requirements for discharge planning for hospitals, critical access hospitals, and home health agencies. Code of Federal Regulations (C.F.R.) 2015 Retrieved from https://www.federalregister.gov/documents/2015/11/03/2015-27840/medicare-and-medicaid-programs-revisions-to-requirements-for-discharge-planning-for-hospitals.
- Chen C, Weider K, Konopka K, Danis M. Incorporation of socioeconomic status indicators into policies for the meaningful use of electronic health records. Journal of Health Care for the Poor & Underserved. 2014;25(1):1–16. doi: 10.1353/hpu.2014.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans RG, Barer ML, Marmor TR. Why are some people healthy and others not?: The determinants of health of populations. New York, NY: Aldine de Gruyter; 1994. [Google Scholar]
- Garrard J. Health sciences literature review made easy: The matrix method. 3. Sudbury, MA: Jones & Bartlett Learning, LLC; 2011. [Google Scholar]
- Gu Y, Warren J, Humphrey G, Bycroft J, McKinlay E, Doughty R, Tibby S. What is shared care planning? International Journal of Integrated Care. 2015;15(5):1–3. [Google Scholar]
- Hagglund M, Chen R, Koch S. Modeling shared care plans using CONTsys and openEHR to support shared homecare of the elderly. Journal of the American Medical Informatics Association. 2011;18(1):66–69. doi: 10.1136/jamia.2009.000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewner SJ. Postmenopausal function in context: Biocultural observations on Amish, neighboring non-Amish, and Ifugao household health. American Journal of Human Biology. 2001;13(4):521–530. doi: 10.1002/ajhb.1084. [DOI] [PubMed] [Google Scholar]
- International Organization for Standardization (ISO) Sampling procedures for inspection by attributes—Part 1: Sampling schemes indexed by acceptance quality limit (AQL) for lot-by-lot inspection. 1999 Retrieved from http://www.iso.org/iso/catalogue_detail.htm?csnumber=1141.
- MacNaughton-Doucet LJ. Determinants of health in discharge planning for seniors: Asking the right questions. Canadian Journal on Aging. 2013;32(3):307–315. doi: 10.1017/S0714980813000342. [DOI] [PubMed] [Google Scholar]
- National Library of Medicine (PubMed) MeSH: Social determinants of health. 2016 Retrieved from http://www.ncbi.nlm.nih.gov/mesh/?term=social+determinants+of+health.
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polit D, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. 9. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- Poulymenopoulou M, Papakonstantinou D, Malamateniou F, Vassilacopoulos G. Using a patient-centered approach for health and social care integration. Studies in Health Technology & Informatics. 2012;180:467–471. [PubMed] [Google Scholar]
- Ramgard M, Blomqvist K, Petersson P. Developing health and social care planning in collaboration. Journal of Interprofessional Care. 2015;29(4):354–358. doi: 10.3109/13561820.2014.1003635. [DOI] [PubMed] [Google Scholar]
- Rigby M, Hill P, Koch S, Keeling D. Social care informatics as an essential part of holistic health care: A call for action. International Journal of Medical Informatics. 2011;80(8):544–554. doi: 10.1016/j.ijmedinf.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Self R, Rigby A, Leggett C, Paxton R. Clinical decision support tool: A rational needs-based approach to making clinical decisions. Journal of Mental Health. 2008;17(1):33–48. [Google Scholar]
- Varpio L, Rashotte J, Day K, King J, Kuziemsky C, Parush A. The EHR and building the patient’s story: A qualitative investigation of how EHR use obstructs a vital clinical activity. International Journal of Medical Informatics. 2015;84(12):1019–1028. doi: 10.1016/j.ijmedinf.2015.09.004. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) What are social determinants of health? 2016 Retrieved from http://www.who.int/social_determinants/sdh_definition/en/