Abstract
The objective of this study was to examine the relationship between nursing excellence and EHR adoption. Of 6,582 U.S. hospitals, 4,939 were eligible for the Medicare EHR Incentive Program and 6,419 were eligible for evaluation on the HIMSS Analytics EMRAM. Of 399 Magnet hospitals, 330 were eligible for the Medicare EHR Incentive Program and 393 were eligible for evaluation in the HIMSS Analytics EMRAM. MU attestation was defined as receipt of a Medicare EHR Incentive Program payment. EHR adoption was defined as Level 6 and/or 7 on the HIMSS Analytics EMRAM. Logistic regression showed that Magnet-designated hospitals were more likely than non-Magnet hospitals attest to MU (OR = 3.58, p < .001), and were more likely than non-Magnet hospitals to adopt EHRs (Level 6 only; OR = 3.68, p < .001); (Level 6 or 7; OR = 4.02, p < .001). This study suggested a positive relationship between Magnet Status and EHR use, which involves earning financial incentives for successful adoption. Continued investigation is needed to examine the relationships between the quality of nursing care, EHR utilization, financial implications, and patient outcomes.
Keywords: meaningful use, electronic health record, health information technology, nursing informatics, Magnet hospitals, HIMSS Analytics
INTRODUCTION
As a result of the American Recovery and Reinvestment Act (ARRA) of 2009, the Patient Protection and Affordable Care Act (PPACA) and other quality-of-care programs, the healthcare industry is experiencing a paradigm shift. Instead of volume-based delivery models, there is a movement toward a more data-driven, value-based approach.[1] This shift presents opportunities for professional nursing practice to support electronic health record (EHR) adoption and quality improvement efforts while simultaneously quantifying the profession’s contribution to patient care.
The Centers for Medicare and Medicaid Services (CMS) established the Electronic Health Records Incentive Program, also referred to as “Meaningful Use” (MU), in accordance with the ARRA.[2] Over a billion dollars have been invested by the United States government since 2009 to support the nationwide implementation, adoption, and meaningful use of EHR technology. Effective since 2015, Medicare and Medicaid reimbursement dollars are awarded to those who meet the established MU objectives,[3] while failure to meet established criteria results in financial penalties.[3,4] Demonstration of EHR MU and the subsequent qualification for CMS reimbursement occurs in three stages, the first of which began in 2011, and the third stage beginning in 2016.[5]
Successful attestation to MU is one metric of EHR adoption in the United States’ healthcare system; another is the Healthcare Information and Management Systems Society (HIMSS) Analytics’ Electronic Medical Record Adoption Model (EMRAM). The EMRAM ranks healthcare organizations on an eight-point scale, from zero to seven in ascending order, based on their level of electronic medical record (EMR) adoption.[6] The EMRAM is an independent, non-federal metric that is widely regarded as an industry standard for the evaluation of organizational EMR adoption. According to the HIMSS Analytics database, as of December 2013, only 3% of the 5,458 hospitals evaluated on the EMRAM achieved Level 7 and 13% achieved Level 6.[7]
Magnet status is a measure of quality in nursing care. The American Nurses Credentialing Center’s (ANCC’s) Magnet Recognition Program distinguishes hospitals that demonstrate nursing excellence, quality patient care, and innovations in professional practice.[8] The Magnet Recognition Program is guided by the Magnet Model, which offers a framework for both professional nursing practice and nursing research.[9] The model acknowledges Global Issues in Nursing and Health Care through five Core Models and their 14 respective Forces of Magnetism.[9] To attain Magnet recognition, hospitals must embody all components of the Magnet Model using established, quantifiable criteria. Among those criteria are: transformational nursing leadership, structural empowerment for all levels of nursing, and adoption of new innovations and demonstrated improvements to patient outcomes. To substantiate and support the attainment of Magnet Core Models, hospitals seeking Magnet status engage in an application process involving extensive data capture of nursing-sensitive indicators.[9]
Use of EHR technology is theorized to be related to the quality of nursing care. Numerous metrics of MU are either nursing-sensitive, or are dependent on nursing documentation. For example, nurses are directly involved in 11 of the 13 MU Stage I Core Objectives through their medication administration and reconciliation; admission and shift assessments; and patient teaching responsibilities. Despite the national attention EHR adoption has received, there is a gap in the current literature surrounding nursing’s impact on EHR adoption. The transition from paper to electronic records is challenging, and end-user resistance is a commonly reported reason for EHR implementation failures.[10] Nurses are the largest group of hospital clinicians and the largest group of EHR end-users,[11,12] yet the majority of the publications on EHR adoption, MU attestation, and HIT quality improvement initiatives have been written from a business, medical, or policy perspective. Also, there was limited research on Magnet organizations within the context of healthcare technology and EHR adoption.
The purpose of this study was to bridge the gap and explore the relationship between nursing excellence and EHR use. Successful EHR use was represented by two distinct measures to allow for the analysis of hospitals that are Magnet-designated but ineligible to participate in the CMS’ Medicare EHR Incentive Program due to their CMS classification. The HIMSS Analytics EMRAM does not exclude hospitals that specialize in long term, psychiatric, pediatric, rehabilitation, or cancer treatment. Therefore, every U.S. Magnet-designated hospital was able to be included in at least one analysis. Two research questions, with four hypotheses, guided the methods of this study:
- Are Magnet hospitals more likely to attest to Meaningful Use than non-Magnet hospitals?
- Hypothesis 1: Magnet hospitals are more likely than non-Magnet hospitals to receive Medicare reimbursement for Meaningful Use.
- Are Magnet hospitals more likely to have higher EHR adoption than non-Magnet hospitals?
- Hypothesis 2a: Magnet hospitals are more likely than non-Magnet hospitals to achieve HIMSS Analytics Level 6 or HIMSS Analytics Level 7.
- Hypothesis 2b: Magnet hospitals are more likely than non-Magnet hospitals to achieve HIMSS Analytics Level 7.
- Hypothesis 2c: Magnet hospitals are more likely than non-Magnet hospitals to achieve HIMSS Analytics Level 6.
METHODS AND MATERIALS
Design
This study was conducted using a non-experimental, quantitative design. The University of XXXX [Blinded for Review] Institutional Review Board reviewed the proposal for this study and granted a letter of Notification of Not Human Research Determination. The operational definition of nursing excellence was current Magnet recognition by the ANCC as of December 2013. Hospitals with current Magnet designation as of December 2013, hospitals awarded Magnet designation for the first time in 2013, and hospitals that were re-designated as Magnet organizations in 2013 were included in the analyses.
Theoretical framework
The theoretical support for this study is based on two conceptual frameworks, the Donabedian Quality Framework (DQF) and the ANCC’s Magnet Model. The DQF offers a framework for evaluating the quality of healthcare by examining the organizational conditions and characteristics that impact care delivery. The framework proposes that the organizational structures and processes involved in the delivery of healthcare influence the outcomes, or quality of the care that is delivered.[13] The Magnet Model describes the relationships that exist between the concepts of structure, process, and outcomes, by focusing on the nursing infrastructure that is created as a result of hospitals’ organizational structures and processes.[14]
Data collection
Study Samples
Two separate hospital data sets were used. The first data set was established to examine the relationship between Magnet recognition and MU attestation (H1). The inclusion and exclusion criteria for this data set focused on the Magnet hospitals’ eligibility to receive Medicare payments from the CMS for meeting MU criteria, so hospitals ineligible for EHR Incentive Program Medicare payments were excluded from the analysis of Hypothesis 1. Hospitals ineligible for Medicare EHR payments were those that were not considered Subsection (d) Hospitals paid under the Inpatient Prospective Payment System by the CMS Section 1886(d)(1)(B) of the Social Security Act. The Social Security Administration [15] defines Subsection (d) Hospitals as hospitals located within one of the 50 United States or the District of Columbia that are not one of the following types of facilities: 1) a rehabilitation hospital, 2) a psychiatric hospital, 3) a hospital whose inpatient population is predominantly under the age of 18, or 4) a hospital with an average inpatient stay that is greater than 25 days. Additionally, cancer-specialty hospitals were not eligible for the Medicare EHR incentive program.[16]
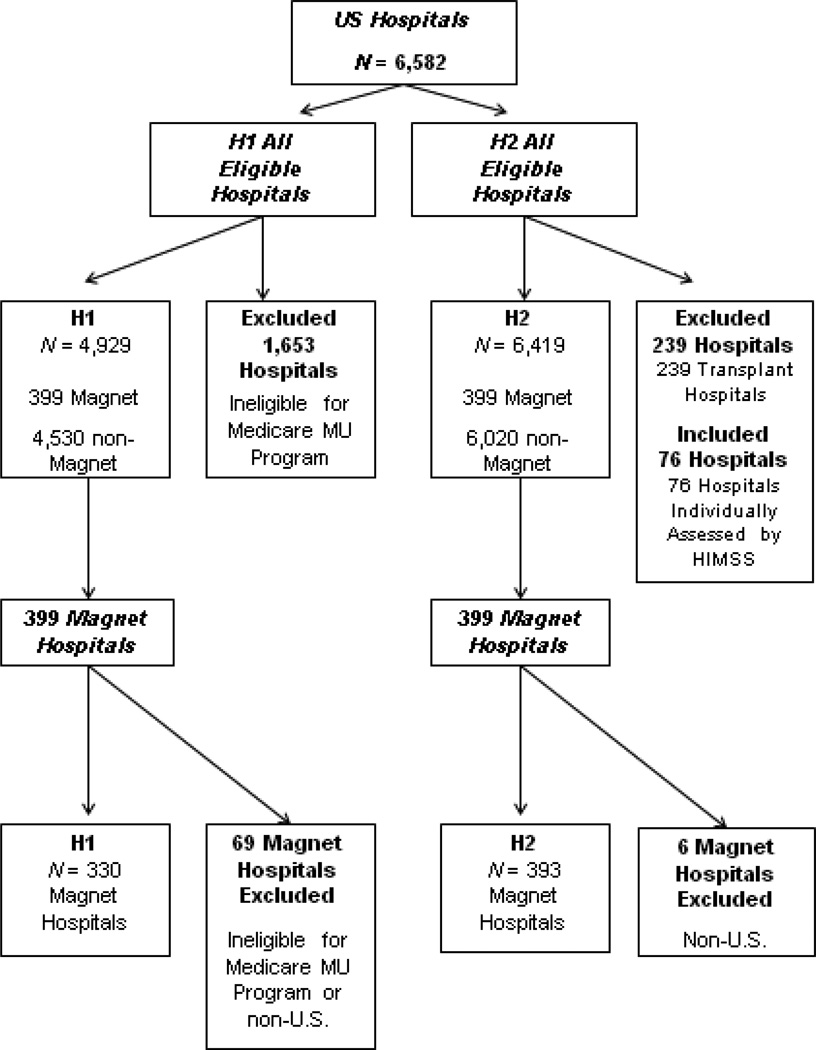
The second data set was developed to test Hypotheses 2a–c. The HIMSS Analytics EMRAM was not based on CMS eligibility; therefore, the facilities that were excluded from the first data set were included in these analyses (see Figure 1). These facilities represented the Medicare-ineligible hospitals as well as the hospitals whose CMS reporting structure could not be verified using public data files. Six international Magnet hospitals were excluded because the study’s population of interest was hospitals in the United States.
Figure 1.
Study Samples
Electronic Health Record Use
The study used two operational definitions of EHR use. The first was the receipt of Medicare reimbursement from the CMS for Meaningful Use attestation as of December 2013. The second was the achievement of Level 6 and/or 7 on the HIMSS Analytics EMRAM as of December 2013.
The first measure of EHR adoption was the receipt of at least one Medicare EHR Incentive Program payment from the CMS. As a national program, the Medicare EHR Incentive Program payment data is posted on the CMS.gov web site in comma separated value (CSV) file format and updated on a quarterly basis.[15] For this study, the CSV file “EH Recipients of Medicare EHR Incentive Program Payments” (EHRMIHRIPP) (as of December 2013) was downloaded into an Excel spreadsheet by the researcher from CMS.gov. This data set originally contained 5,190 entries that represented individual distributions of Medicare payments from May 2011 through December 2013; however, many hospitals appeared multiple times in the data set because they received more than one MU incentive payment between 2011 and 2013. For the purposes of this study, receipt of more than one Medicare MU payment represented a duplicate value. One thousand, six hundred and three such duplicate entries were removed from the data set before the CSV file was transferred into International Business Machines (IBM) Statistical Package for the Social Sciences (SPSS) Version 21. The criterion for duplication was the presence of identical provider National Provider Identifier (NPI) and CMS Certification Number (CCN) numbers. This resulted in 3,587 hospitals that had received at least one Medicare payment for successful Meaningful Use attestation between May 2011 and December 2013 (n = 3,587).
The second measure of EHR adoption in this study was the achievement of Level 6 and/or 7 on the HIMSS Analytics EMRAM. Hospitals that participated in the HIMSS Analytics Annual Study were eligible to receive their EMRAM score as a free service.[6] HIMSS Analytics data were retrieved from the HIMSS Analytics’ www.himssanalytics.org website and manually entered into three Excel spreadsheets by the researcher. The first spreadsheet contained 161 HIMSS Analytics Level 7 hospitals as of December 2013 (n = 161). The second spreadsheet contained 708 HIMSS Analytics Level 6 hospitals as of December 2013 (n = 708). The third spreadsheet was comprised of both Level 7 and Level 6 hospitals as of December 2013. The combined set contained 869 hospitals (n = 869).
There were 6,582 U.S. hospitals identified from the Health Resources and Services Administration’s Hospitals Health Systems Site Directory Report, the CMS General Hospital Information data set, and the CMS EHRMEHRIPP data set. To test Hypothesis 1, 1,653 of the initial 6,582 hospitals were excluded from the H1 analysis because they were ineligible for the Medicare EHR Incentive Program, resulting in a sample of 4,929 hospitals. To test Hypotheses 2a–c, 239 transplant hospitals with zero CMS-certified beds were excluded from the analyses. Seventy-six hospitals that were evaluated on the HIMSS Analytics EMRAM as individual facilities (as opposed to members of consolidated healthcare systems) were added to the analyses, which resulted in a sample of 6,419 out of a possible 6,582 U.S. hospitals. Figure 1 shows the study’s samples and exclusions.
Data analysis
Binary logistic regression analyses in IBM SPSS (IBM Corporation, Armonk, NY, USA). were used to test the study’s research questions. No patient data were analyzed. The data were retrieved from the official and publically accessible web sites for the CMS; the ANCC; and HIMSS Analytics.
RESULTS
CMS Meaningful Use
H1: Are Magnet hospitals are more likely than non-Magnet hospitals to receive Medicare reimbursement for Meaningful Use
Of the 330 Magnet hospitals, 297 (90%), and of the 4599 non-Magnet hospitals, 3290 (72%) received at least one Medicare payment from the CMS for Meaningful Use attestation between May 2011 and December 2013. The logistic regression model was statistically significant, χ2 = 63.61, p < .001. Magnet-recognized hospitals were more likely than non-Magnet hospitals to receive Medicare EHR payments for MU attestation, B = 1.28, SE = 0.19, p < .001, 95% CI [2.49, 5.16], OR = 3.58.
HIMSS Analytics EMRAM
Table 1 shows the percentage of Magnet versus non-Magnet hospitals that achieved Level 6 or 7; Level 7; or Level 6 on the HIMSS Analytics EMRAM as of December 2013.
Table 1.
Magnet Organizations and EHR Adoption (HIMSS Analytics Levels 6 and 7)
| Nursing Excellence | Achieved HIMSS Level 6 or 7 |
Achieved HIMSS Level 7 |
Achieved HIMSS Level 6 |
|---|---|---|---|
| Magnet (n = 393) | 36% (n = 140) | 19% (n = 27) | 29% (n = 113) |
| Non-Magnet (n = 6026) | 12% (n = 729) | 18% (n = 134) | 10% (n = 595) |
HIMSS Analytics Level 6 or HIMSS Analytics Level 7
The logistic regression model was statistically significant, χ2) = 132.67, p < .001. Magnet-recognized hospitals were more likely than non-Magnet hospitals to achieve Level 6 or 7 on the HIMSS Analytics EMRAM, B = 1.39, SE = 0.11, p < .001, 95% CI [3.23, 5.01], OR = 4.02.
HIMSS Analytics Level 7
The logistic regression model was not statistically significant, χ2 = .06, p = .802. Magnet-recognized hospitals were not more likely than non-Magnet hospitals to achieve Level 7 on the HIMSS Analytics EMRAM.
HIMSS Analytics Level 6
The logistic regression model was statistically significant, χ2 =100.61, p < .001. Magnet-recognized hospitals were more likely than non-Magnet hospitals to achieve Level 6 on the HIMSS Analytics EMRAM, B = 1.30, SE = 0.12, p < .001, 95% CI [2.91, 4.65], OR = 3.68.
DISCUSSION
This study examined the relationship between Magnet status and EHR use using four indicators of EHR use. Magnet-designated hospitals had a significantly greater likelihood than non-Magnet hospitals of receiving Medicare EHR incentive payments for MU attestation. The results of this study indicate that Magnet-recognized facilities have significantly greater likelihood than non-Magnet hospitals of achieving Level 6 or 7 on the HIMSS Analytics EMRAM. The results also indicate that Magnet-recognized facilities have significantly greater likelihood than non-Magnet hospitals of achieving Level 6 on the HIMSS Analytics EMRAM. However, there was no difference in EHR adoption between Magnet hospitals and non-Magnet hospitals, when EHR adoption was measured by the achievement of Level 7 on the EMRAM.
These findings are consistent with Kirkley et al. [17] and Lindgren et al. [18] that describe how the application of the Magnet Model can be directly translated into successful EHR adoption practices in hospital settings. Although scholars have begun to investigate associations between nursing excellence and EHR use, [19–22] this research is important to nursing practice because it is the first study that examined Magnet hospitals’ outcomes compared to non-Magnet hospitals with the multiple measures of EHR adoption, the CMS’ Medicare EHR Incentive Program and the HIMSS Analytics EMRAM. Currently there are minimal data about the characteristics of hospitals that have received EHR incentive payments, [23] and this analysis offers evidence that nursing excellence, as operationalized by Magnet recognition, is a hospital characteristic that is positively associated with MU attestation.
Although the EMRAM is a different approach to measuring EHR adoption from MU attestation, the positive correlation between Magnet status and achievement of HIMSS Level 6, or 6 and 7, is consistent with the finding that Magnet hospitals are more likely than non-Magnet hospitals to receive Medicare EHR incentive payments. The consistency across the three hypotheses which utilized two distinct measures of EHR adoption, and four methods of operationalization, provided additional support to the position that nursing excellence is a hospital characteristic that is positively associated with EHR adoption in the United States.
The additional cumulative capabilities that Level 7 contributes to the EMRAM over Level 6 include: continuity of care document transactions for the sharing of data, data warehousing, and continuity of data with emergency, ambulatory, and outpatient settings. [24] Health information exchange (HIE) is defined as the electronic sharing of clinical data across delivery settings. [25] The primary distinction between Level 7 and Level 6 focuses on an EMR’s ability to support HIE activities. HIE represents technical functionality, as opposed to a clinical process of care. Although the delivery of nursing care does contribute to HIE and nurses do benefit from data exchange, the cumulative capabilities specific Level 7 of the HIMSS Analytics EMRAM may not be directly related to nursing-sensitive outcomes. This offers a potential explanation for the failure to reject the null hypothesis for H2b, i.e., that nursing excellence alone does not lead to Level 7. However, it is possible that the small number of hospitals that have reached Level 7 in 2012 reduced statistical power to detect differences. Additionally, at the end of December 2013, there were only 161 hospitals in the U.S. that had reached Level 7. This figure represents less than 3% of the study’s sample, and this small sample size may have contributed to a restriction of range in the statistical analysis of the data. An increasing number of hospitals are achieving Level 7 on the HIMSS Analytics EMRAM every year; however, until there are more hospitals at Level 7, researchers might consider consolidating Levels 6 and 7 together as one variable. We recommend that this type of analysis be replicated after EHR adoption has increased in hospitals.
Understanding the associations between the quality of nursing care and hospitals’ ability to use EHRs may help to identify best practices that guide both EHR implementation and the achievement of nursing excellence. The current study represents introductory research intended to justify and stimulate further investigation of this rapidly-evolving discipline. This study also sought to establish a foundation for continuing research.
While many healthcare organizations work to meet the short-term goal of attesting to MU in order to avoid missing CMS payments and incurring potential penalties, continuing research needs to address several critical questions: 1) What is the nature of the relationship between nursing practice and the adoption of EHRs? 2) What are the common characteristics of hospitals that successfully adopt EHRs? 3) What are the common characteristics of hospitals that demonstrate nursing excellence? 4) Are there organizational characteristics that are consistent among hospitals that demonstrate nursing excellence and successfully adopt EHRs? 5) Is the successful adoption of EHR technology associated with measureable improvements to nursing-specific patient care? A recent study conducted by HIMSS Analytics and Healthgrades found that the performance of hospitals with high EMRAM levels was significantly better than hospitals that had low EMRAM levels for four patient outcomes, suggesting that there is a relationship between EMR use and patient outcomes. In this joint study, hospital performance was based on the number of patient mortalities. [26] Additional research that targets the outcomes of nursing care is warranted considering that nurses deliver majority of bedside care in the U.S. [27] and interact more with EHR technology than any other group of healthcare professionals. This study contributes original knowledge to the discipline of nursing informatics. Previous research primarily investigated topics such as acceptance of and/or resistance to EHR systems by nursing staff and changes in patient outcomes after the implementation of EHR technology, [28–36] while narrative articles described hospitals’ journeys from paper to electronic systems. [17,18] This study was unique in that it quantified the likelihood of Magnet hospitals adopting EHRs compared to non-Magnet hospitals.
The development of customized data sets to test the study’s hypotheses was advantageous because this study had a very specific focus; however, this also limited the ability to compare this study’s findings to other research projects that utilized different data sets for their samples. The sample used in Hypothesis 1 was slightly larger than the number of hospitals registered for the MU programs because it included all Medicare EHR-eligible hospitals. Thus, direct comparisons to other MU research studies whose sample included only registered, as opposed to eligible hospitals, cannot be made to the current study. The HIMSS Analytics data have a similar limitation because the sample used in this study is slightly larger than the number of hospitals in the HIMSS Analytics Database (that reflect data from 2013) because this study, by default of the larger sample, included some hospitals that were not in the 2013 HIMSS Analytics Database. Again, the researchers aimed to study all hospitals that could potentially receive a HIMSS Analytics EMRAM score and not only those that elected to participate in the survey.
Other limitations of this study were inherent to its research design. The use of data extracted from existing data sets limited the research questions that could be examined, and the researchers were not able to control the quality of the data collection. [37] This study utilized administrative data sets that were not specifically designed for nursing research, which could further constrain how the relationships between the variables were analyzed. [38] The data were cross-sectional in nature, which precludes any strict causal interpretations of these results.
CONCLUSION
United States hospitals must respond to the government’s imperatives to improve the quality of patient care through the use of HIT. There is tremendous potential for EHRs to revolutionize the healthcare delivery process, [39] yet numerous challenges to EHR implementation persist. Hospitals recognized for nursing excellence with Magnet designation have a greater likelihood of receiving Medicare EHR incentive payments and they are more likely to achieve higher levels of EHR use. Although the financial implications can only be speculated, this study provides direction regarding the importance of nursing excellence and adoption of EHRs. As the EHR revolution unfolds, continued investigation is needed to examine quality of nursing care, EHR utilization, financial implications, and patient outcomes.
Acknowledgments
Source Funding:
We have the following funding announcement to disclose: Support for this research was also received from the Center of Excellence for Health Disparities Research: El Centro, National Institute of Minority Health and Health Disparities grant 2P60MD002266 (Nilda P. Peragallo, Principle Investigator). The authors are solely responsible for this article’s content and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest:
There are no conflicts of interest.
Contributor Information
Christine Lippincott, University of Miami, School of Nursing and Health Studies, 5030 Brunson Dr., Coral Gables, FL 33146, United States.
Cynthia Foronda, University of Miami, School of Nursing and Health Studies, 5030 Brunson Dr., Coral Gables, FL 33146, United States, 9817Forondc@gmail.com, 414-732-4200, c.foronda@miami.edu, @CForondaPhDRN.
Martin Zdanowicz, University of Miami, School of Nursing and Health Studies, 5030 Brunson Dr., Coral Gables, FL 33146, United States.
Brian E. McCabe, University of Miami, School of Nursing and Health Studies, 5030 Brunson Dr., Coral Gables, FL 33146, United States.
Todd Ambrosia, Phillips Beth Israel School of Nursing, 776 Avenue of the Americas, Suite 4A, New York, NY 10001, United States.
References
- 1.Meaningful Use: Introduction. [Accessed March 21, 2015]; www.cdc.gov/ehrmeaningfuluse/introduction.html.
- 2.Jha AK, Burke MF, DesRoches C, et al. Progress toward Meaningful Use: Hospitals’ adoption of electronic health records. Am J Manag Care. 2011;17(Special Issue):SP117–SP124. [PubMed] [Google Scholar]
- 3.American Organization of Nurse Executives Position Paper: Nursing informatics executive leader. [Accessed March 21, 2015]; http://www.aone.org/resources/leadership%20tools/PDFs/AONE_Technology_Committee_CNIO_Position_Paper.pdf. [Google Scholar]
- 4.Medicare & Medicaid EHR Incentive Program: Meaningful Use Stage 1 Requirements Overview. [Accessed March 21, 2015]; http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Eligible_Hospital_Information.html.
- 5.Meaningful Use Definition and Objectives. [Accessed March 21, 2015]; http://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives.
- 6.Electronic Medical Record Adoption (EMRAM)℠. [Accessed March 21, 2015]; http://www.himssanalytics.org/emram/emram.aspx. [Google Scholar]
- 7.Healthcare Information and Management Systems Society Analytics. Current EMRAM℠ Scores. [Accessed March 14, 2104]; https://www.HIMSS Analyticsanalytics.org/emram/scoreTrends.aspx. [Google Scholar]
- 8.Klosek J. Exploring the barriers to the more widespread adoption of electronic health records. Notre Dame Journal of Law, Ethics, and Public Policy. 2011;25(2):429–445. [Google Scholar]
- 9.Choromanski L. Development of a nursing informatics governance committee. Comput Inform Nurs. 2011;29(2):69–72. doi: 10.1097/NCN.0b013e31820663d3. [DOI] [PubMed] [Google Scholar]
- 10.Harrington L. AONE creates new position paper: Nursing informatics executive leader. Nurse Leader. 2012;10(3):17–21. [Google Scholar]
- 11.ANCC Magnet Recognition Program. [Accessed March 21, 2015]; http://www.nursecredentialing.org/Magnet.aspx. [Google Scholar]
- 12.Magnet Model. [Accessed March 21, 2015]; http://www.nursecredentialing.org/Magnet/ProgramOverview/New-Magnet-Model. [Google Scholar]
- 13.Donabedian A. The definition of quality and approaches to its assessment [Vol. 1] Ann Arbor, MI: Health Administration Press; 1980. [Google Scholar]
- 14.American Nurses Credentialing Center. 2008 Magnet Recognition Program Application Manual. Silver Spring, MD: American Nurses Credentialing Center; 2008. [Google Scholar]
- 15.Recipients of Medicare EHR Incentive Program Payments. [Accessed March 21, 2015]; http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/DataAndReports.html.
- 16.Murphy K. How meaningful use eligibility affects non-meaningful users. [Accessed March 21, 2015];EHR Intelligence. 2013 Sep 9; http://ehrintelligence.com/2013/09/09/how-meaningful-use-eligibility-affects-non-meaningful-users/ [Google Scholar]
- 17.Kirkley D, Johnson AP, Anderson MA. Technology support of nursing excellence: The Magnet connection. Nurs Econ. 2004;22(2):94–98. [PubMed] [Google Scholar]
- 18.Lindgren CL, Elie LG, Vidal EC, et al. Transforming to a computerized system for nursing care: Organizational success within Magnet idealism. Comput Inform Nurs. 2010;28(2):74–78. doi: 10.1097/NCN.0b013e3181cd7f2d. [DOI] [PubMed] [Google Scholar]
- 19.Harrison RL, Lyerla F. Using nursing clinical decision support systems to achieve meaningful use. Comput Inform Nurs. 2012;30(7):380–385. doi: 10.1097/NCN.0b013e31823eb813. [DOI] [PubMed] [Google Scholar]
- 20.Harrison RL, Stalker SL, Henderson R, et al. (2013). Use of a clinical decision support system to improve hypoglycemic management. Medsurg Nurs. 2013;22(4):250–254. 263. [PubMed] [Google Scholar]
- 21.Simpson RL. Nurse informaticians critical to proving meaningful use. Nurs Adm Q. 2011;35(1):82–84. doi: 10.1097/NAQ.0b013e318203462a. [DOI] [PubMed] [Google Scholar]
- 22.Westra BL, Subramanian A, Hart CM, et al. Achieving “Meaningful use” of electronic medical records through the integration of the Nursing Management Minimum Data Set. J Nurs Adm. 2010;40(7/8):336–343. doi: 10.1097/NNA.0b013e3181e93994. [DOI] [PubMed] [Google Scholar]
- 23.Adler-Milstein J, Furukawa MF, King J, et al. Early results from the hospital electronic health record incentive programs. Am J Manag Care. 2013;19(7):e273–e284. [PubMed] [Google Scholar]
- 24.Maturity Models: Electronic Medical Record Adoption Model (EMRAM) [Accessed March 21, 2015]; http://www.himssanalytics.org/emram/ [Google Scholar]
- 25.Dullabh P, Adler-Milstein J, Hovey L, et al. Key challenges to enabling health information exchange and how states can help. [Accessed March 21, 2105];Final Report. 2014 https://healthit.gov/sites/default/files/state_hie_evaluation_stakeholder_discussions.pdf.
- 26.Beaudoin J. 2014 Ending debate on EMR effectiveness? [Accessed March 21, 2015]; http://www.healthcareitnews.com/news/ending-debate-emr-effectiveness?topic=06,08,19&mkt_tok=3RkMMJWWfF9wsRonuqnNZKXonjHpfsX56OklXrHr08Yy0EZ5VunJEUWy2YIJSdQ%2FcOedCQkZHblFnVUKSK2vULcNqKwP. [Google Scholar]
- 27.American Association of Colleges of Nursing. [Accessed March 21, 2015];Nursing Fact Sheet. http://www.aacn.nche.edu/media-relations/fact-sheets/nursing-fact-sheet. [Google Scholar]
- 28.Choi J, Boyle DK. Workgroup job satisfaction and patient falls in hospital units. J Nurs Adm. 2013;43(11):586–591. doi: 10.1097/01.NNA.0000434509.66749.7c. [DOI] [PubMed] [Google Scholar]
- 29.Everhart D, Schumacher JR, Duncan R, et al. Determinants of hospital fall trajectory groups: A longitudinal assessment of nurse staffing and organizational characteristics. Health Care Manage Rev. 2014;0(0) doi: 10.1097/HMR.0000000000000013. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He J, Dunton N, Staggs V. Unit-level time trends in inpatient fall rates of US hospitals. Medical Care. 2012;50(9):801–807. doi: 10.1097/MLR.0b013e31825a8b88. [DOI] [PubMed] [Google Scholar]
- 31.Hickey P, Gauvreau K, Connor J, et al. The relationship of nurse staffing, skill mix, and Magnet recognition to institutional volume and mortality for congenital heart surgery. J Nurs Adm. 2010;40(5):226–232. doi: 10.1097/NNA.0b013e3181da3f71. [DOI] [PubMed] [Google Scholar]
- 32.Kelley TF, Brandon DH, Docherty SL. Electronic nursing documentation as a strategy to improve quality of patient care. J Nurs Scholarsh. 2011;43(2):154–162. doi: 10.1111/j.1547-5069.2011.01397.x. [DOI] [PubMed] [Google Scholar]
- 33.Lake ET, Shang J, Klaus S, et al. Patient falls: Association with hospital Magnet status and nursing unit staffing. Res Nurs Health. 2010;33(5):413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McHugh MD, Kelly LA, Smith HL, et al. Lower mortality in Magnet hospitals. Medical Care. 2013;51(5):382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mills AC, Gillespie KN. Effect of Magnet hospital recognition on 2 patient outcomes. Journal of Nursing Care. 2013;28(1):17–23. doi: 10.1097/NCQ.0b013e318268a710. [DOI] [PubMed] [Google Scholar]
- 36.Rogers C. Improving processes to capture present-on-admission pressure ulcers. Adv Skin Wound Care. 2013;26(12):566–572. doi: 10.1097/01.ASW.0000437949.62301.6e. [DOI] [PubMed] [Google Scholar]
- 37.Hulley SB, Cummings SR, Browner WS, et al. Designing clinical research. 3rd. Philadelphia, PA: Lippincott Williams and Wilkins; 2007. [Google Scholar]
- 38.Waltz CF, Strickland OL, Lenz ER. Measurement in nursing and health care research. 4th. New York, NY: Springer; 2010. [Google Scholar]
- 39.Naser RJ. Electronic health record as a function of success: Implications for Meaningful Use. Doctoral dissertation. 2012 [Google Scholar]