Abstract
Objective
Perception of personal identity cannot be separated from the perception of the social context and one's social identity. Full involvement in group psychotherapy may require not only the awareness of personal impairment, but also social identification. The aim of the current study was to examine the association between social identification and symptom improvement in group-based psychotherapy.
Method
169 participants received 12 sessions of group-based cognitive behavioral therapy for social anxiety disorder. Social identification, the extent to which a person identifies with those who suffer from the same psychological problem as themselves and/or with those lacking psychopathology (non-sufferers), and clinical outcome were assessed at baseline, mid-and posttreatment, and 1, 3, and 6-months follow-up.
Results
At baseline, patients aspired for closeness with non-sufferers, and viewed themselves as distant from fellow sufferers and non-sufferers. After treatment, participants viewed not only themselves, but also other individuals with social anxiety, as closer to both non-sufferers and fellow sufferers. These ratings were related to clinical outcomes.
Conclusions
The increase in closeness to both sufferers and non-sufferers across treatment may reflect a movement towards a more tolerant, less dichotomous and rigid, separation of ill and healthy that occurs with successful social anxiety treatment.
Keywords: Social identification, Stigma, Personality, Cognitive behavioral therapy, Social anxiety disorder, Predictor
Psychological disorders not only cause significant personal impairment (Schneier et al., 1994), they also pose a potential threat to one's identity. Social identity refers to one's construal of self through the lens of group membership (Turner & Onorato, 1999). According to social identity theory, the tendency to divide the social world into two categories, the ingroup (i.e., the group with which one identifies) or outgroup (i.e., any group other than the one with which one identifies) is an attempt to enhance one's self-esteem. This tendency is only successful if the ingroup members perceive their group as superior to competing groups (Tajfel & Turner,1986). Consistent with stigma against mental disorders, membership in a group of individuals suffering from psychopathology may be perceived as belonging to an inferior group. Despite intensive efforts in public health education over the past decades, attitude surveys reflect an increase in such prejudice against mental disorders (Jorm & Oh, 2009; Link, Yang, Phelan, & Collins, 2004; Phelan, Link, Stueve, & Pescosolido, 2000; Schomerus et al., 2012). Individuals with mental illnesses are thus confronted on one hand, with a dual challenge of clinical symptoms and personal suffering and on the other, the potential of inclusion in a publically stigmatized group, the mentally ill. Consequently, self-stigmatization, or the acceptance of the legitimacy of negative social attitudes towards an ingroup, is common in patients with a mental disorder (Alonso et al., 2009; Corrigan & Watson, 2002; Hinshaw & Stier, 2008; Rüsch, Angermeyer, & Corrigan, 2005; Watson, Corrigan, Larson, & Sells, 2007).
One way to cope with stigma-related threat is to view oneself as dissimilar and refuse to identify with the devalued social group (Allport, 1954; Quinn & Chaudoir, 2009; Smart & Wegner, 2000). While it is easier to distance oneself from the devalued group when group membership is not obvious and can be hidden, “concealable stigma”, (Goffman,1986; Clair, Beatty, & MacLean, 2005), denial of a devalued identity has also been shown to be associated with aggravated distress (Barreto, Ellemers, & Banal, 2006; Crocker, Major, & Steele, 1998; Jacoby, Snape, & Baker, 2005; Smart & Wegner, 1999) and reduced treatment compliance (Fung, Tsang, & Corrigan, 2008; Sirey et al., 2001). Furthermore, strong accentuation of the dichotomy between “normal” and “abnormal” may increase perceived illness stigma in individuals who identify themselves as “mentally ill.” Identification with a devalued group may only be empowering if individuals believe that the distinctions between their devalued group and a more valued outgroup is small and the perceived status differences between groups (and the legitimacy of socially constructed differences) are questionable (Campbell & Jovchelovitch,2000). Thus, the subjective “distance” of the self to the ingroup and to a relevant outgroup may be highly relevant to treatment progress, particularly in group-based therapy. Because the perception of personal identity cannot be separated from the perception of the social context and one's social identity (Mischel & Shoda, 1995; Mendoza-Denton, Ayduk, Mischel, Shoda, & Testa, 2001; Onorato & Turner, 2004), psychotherapy engagement may not only require awareness of personal impairment, but also acceptance of this social identification (Petersen, van den Berg, Janssens, & Van den Bergh, 2011).
Notably, identification with groups is not completely stable and can change over time as a person accumulates new information, moves to new contexts, and adds more positively valenced content to the group identity (Quinn & Chaudoir, 2009). Therefore, it is reasonable to hypothesize that group identification can change over the course of therapy, and such change could relate to progress during treatment. In support of this notion, a recent study on substance abuse found that identity transition (change in identification from a “user identity” to a “recovery identity”) accounted for a substantial amount of variance in post-treatment drinking behavior change, even when controlling for traditional factors (e.g., session attendance, substance use severity/duration) (Dingle, Stark, Cruwys, & Best, 2015).
Identification with a low status group as one's ingroup has been shown to reduce self-stigmatization and lead to empowerment (Rosenthal & Crisp, 2006), including in mental disorders (Crabtree, Haslam, Postmes, & Haslam, 2010; Rüsch, Lieb, Bohus, & Corrigan, 2006). Similarly, Cruwys et al. (2014) found that members of a group-based CBT program for depression who more strongly identified with other group members showed superior improvements compared to those who did not. A robust body of research examining the impact of connectedness and social identification on mental and physical health, indicates that group identification is advantageous in general. For example, Sani, Madhok, Norbury, Dugard, and Wakefield (2015) showed that the greater the number of groups an individual identifies with, the lower their level of depression (Sani et al., 2015). Likewise, stronger national identification is linked to lower rates of posttraumatic stress disorder for individuals living in a region with ongoing violence and conflict (Muldoon & Downes, 2007). Further evidence comes from Wakefield, Bickley, and Sani (2013) who demonstrated that higher degrees of subjective group identification (i.e., one's sense of belonging to a group) was associated with decreased depression and anxiety, as well as increased life satisfaction in multiple sclerosis (MS) patients. Moreover, change in perceived norms in young women undergoing a body acceptance group program (e.g., members arguing against distorted weight ideals), indicated greater identification with the other members of the group and mediated reductions in disordered eating (Cruwys, Haslam, Fox, & McMahon, 2015). Taken together, these studies indicate that social/ group identification could be an important, yet largely neglected, factor influencing therapeutic change.
The aim of the current study was to examine group identification as a time-varying predictor of symptom improvement in patients undergoing 12-sessions of group CBT for social anxiety disorder (SAD). We hypothesized that increases in identification with the ingroup and a reduction of accentuation between the categories “health” and “disease” would be associated with therapeutic success, although the direction of this relation is unclear at this time. To assess social identification we used an adapted version the Overlap of Self, Ingroup, and Outgroup (OSIO) scale, a validated measure used in social psychology (Schubert & Otten, 2002).
1. Methods
1.1. Participants
The sample consisted of 169 outpatients with a diagnosis of social anxiety disorder (SAD). The sample was part of a larger study examining the efficacy of d-cycloserine as an augmentation strategy of cognitive behavioral therapy for SAD (Hofmann et al., 2013). Patients were primarily white (61.5%), male (56.8%), and single (66.9%), with the majority having a college degree. The mean age was 32.6 years (SD = 10.36) (see Hofmann et al., 2013 for more details). Inclusion criteria were current DSM-IV diagnostic criteria for generalized SAD (First, Spitzer, Gibbon, & Williams, 1996; DiNardo, Brown, & Barlow, 1994),1 a score 60 or higher on the Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987), age 18–65, and agreement not to initiate concurrent psychotherapy or psychotropic medication. Exclusion criteria included: 1) major medical or cognitive illness, 2) drug abuse/dependence, eating disorder or PTSD diagnosis, clinically significant suicidal ideation or behavior in past 6 months, and 3) pregnancy, lactation, or not using medically accepted forms of contraception when of childbearing age. The study was approved by institutional review boards and written informed consent was obtained from all participants.
1.2. Study design and treatment
Eligible participants at three sites (Boston University, Massachusetts General Hospital, and SMU) received identical 12-session CBT protocols. Patients were randomized to receive either 50 mg of DCS (N = 87) or an identical looking placebo pill (N = 82) during sessions 3–7. The protocol and timing (12 weekly 2.5-h sessions) followed Heimberg's cognitive behavioral group therapy approach (Heimberg & Becker, 2002), with modified emphasis on exposure strategies (Hofmann, 2007). Session 1 educated patients about the nature and treatment of SAD. Session 2 introduced patients to cognitive restructuring. Session 3–7 focused on exposure therapy where patients were led through repeated and prolonged confrontation of feared situations. Session 8–12 combined the use of cognitive restructuring strategies with exposure practice. Each treatment group was led by two therapists and was comprised of 4–6 patients. In-depth training and close monitoring through supervision meetings ensured treatment adherence.
1.3. Measures
Primary outcome variables were assessed throughout the treatment phase (at baseline, sessions 2–8, 10, and 12), at post-treatment (week 13), and at follow-up (1, 3, and 6 months). Secondary measures (including our social identification measures) were assessed at baseline, mid-treatment, post-treatment, and at all three follow-ups.
The Liebowitz Social Anxiety Scale (LSAS, Liebowitz, 1987), which served as the primary outcome measure in this study, is a 24-item clinician-administered symptom severity measure for SAD. Baseline social anxiety severity was assessed using the Social Phobic Disorders Severity Form (SPD-SC, Liebowitz et al., 1992). Baseline depressive symptom severity was assessed using the Montgomery–Åsberg Depression Rating Scale (MADRS, Montgomery & Asberg, 1979). All scales demonstrate good psychometric properties. These three measures were administered by independent evalua-tors, blind to treatment condition and patients' scores on the self-administered measures, at the respective assessment time points.
The Social Identification Scale for Psychiatric Disorders (SIS-P)
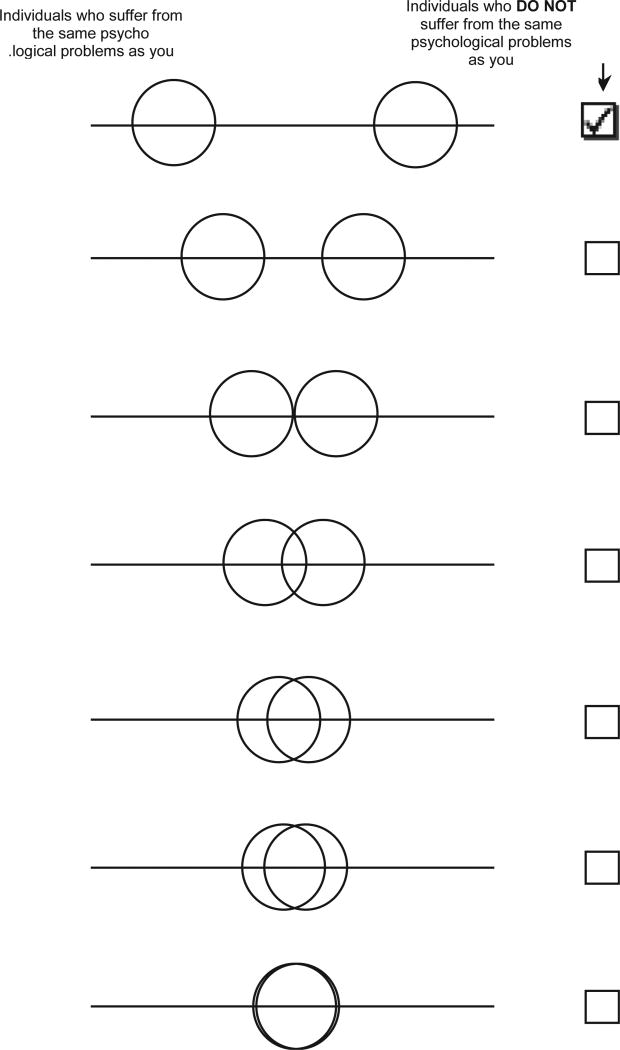
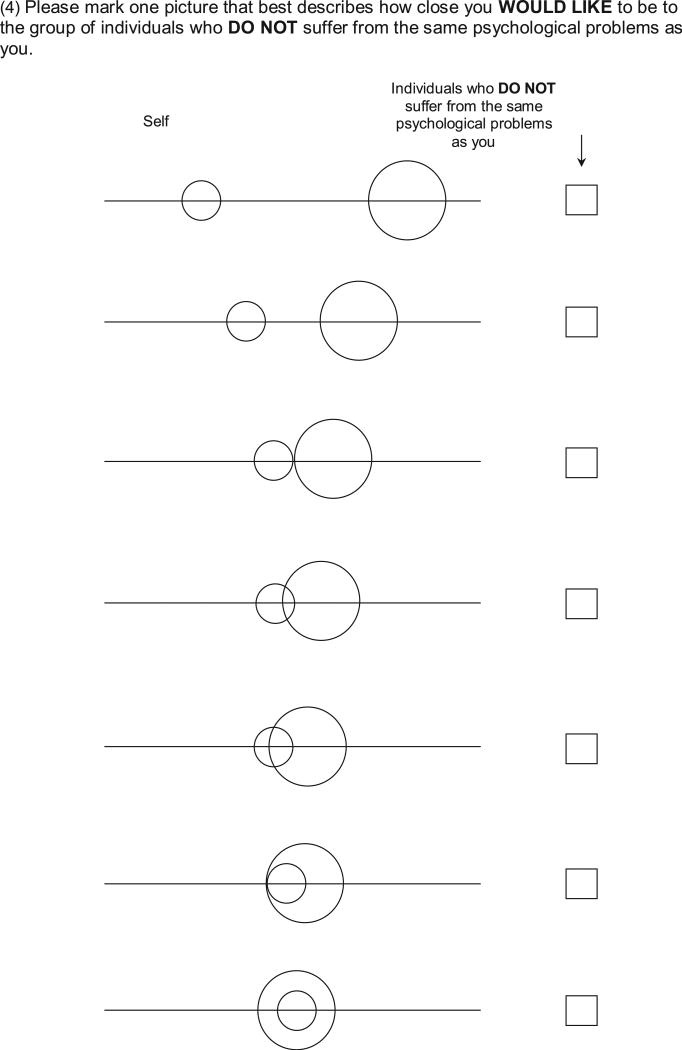
We assessed identification with the ingroup and the outgroup using the four-item SIS-P, a measure developed for the current study. The SIS-P contains four items and is a modified version of the Overlap of Self, Ingroup, and Outgroup Scale (OSIO, Schubert & Otten, 2002). The OSIO has demonstrated convergent validity with traditional self-report measures of perceived group differences across three samples (Schubert & Otten, 2002). In another sample, Schubert and Otten (2002) demonstrated that participants properly interpreted the OSIO items. For each item on the SIS-P, the participant selects one of seven graphical diagrams. Each diagram consists of two circles centered on a horizontal line. In the first diagram the circles are far apart. They become closer together in each successive diagram until they overlap completely in diagram seven (see Fig. 1). For our analyses, we assigned a value of 1 if the participant selected the first diagram, 2 if they selected the 2nd diagram, and so on to a value of 7 for the last diagram. The SIS-P instructions were as follows:
Fig. 1.
SIS-P example item.
On the following pages you find 4 groups of diagrams.
-
-
The big circles in the diagrams represent group members who either suffer from the same psychological problems or not.
-
-
Small circles represent you.
-
-
The closer the circles the closer related you perceive the group members or your relation to these members.
Please choose one picture per group of diagrams that best represents the closeness of the two groups or your closeness to one of the two groups (see Fig. 1 as an example).
Example: If you would choose the first diagram, this would mean that for you these two groups are not very close to each other.
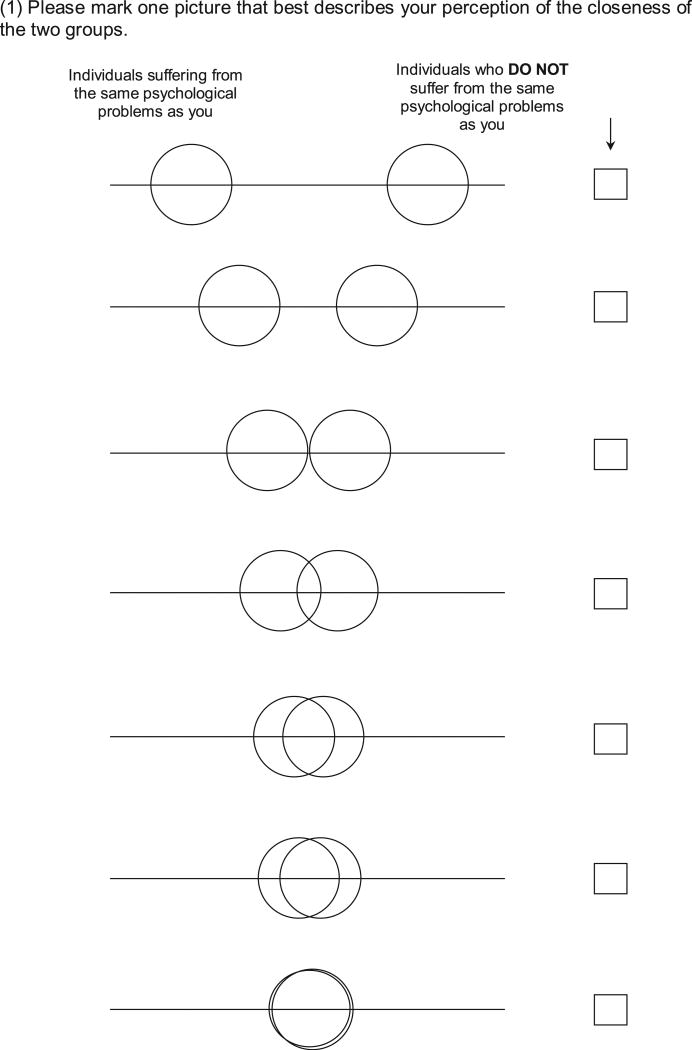
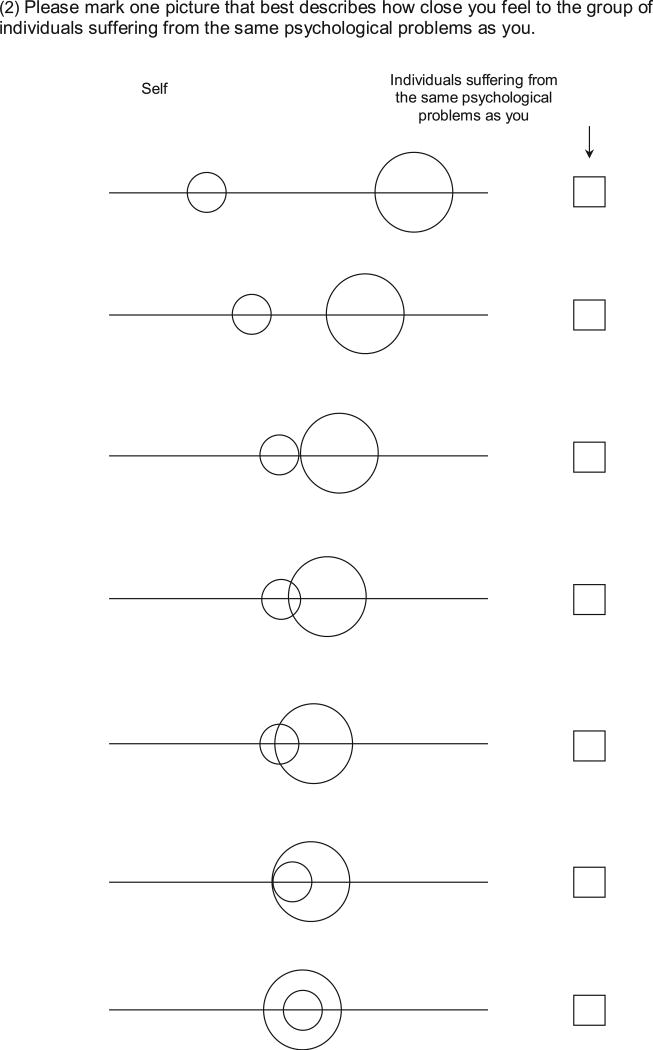
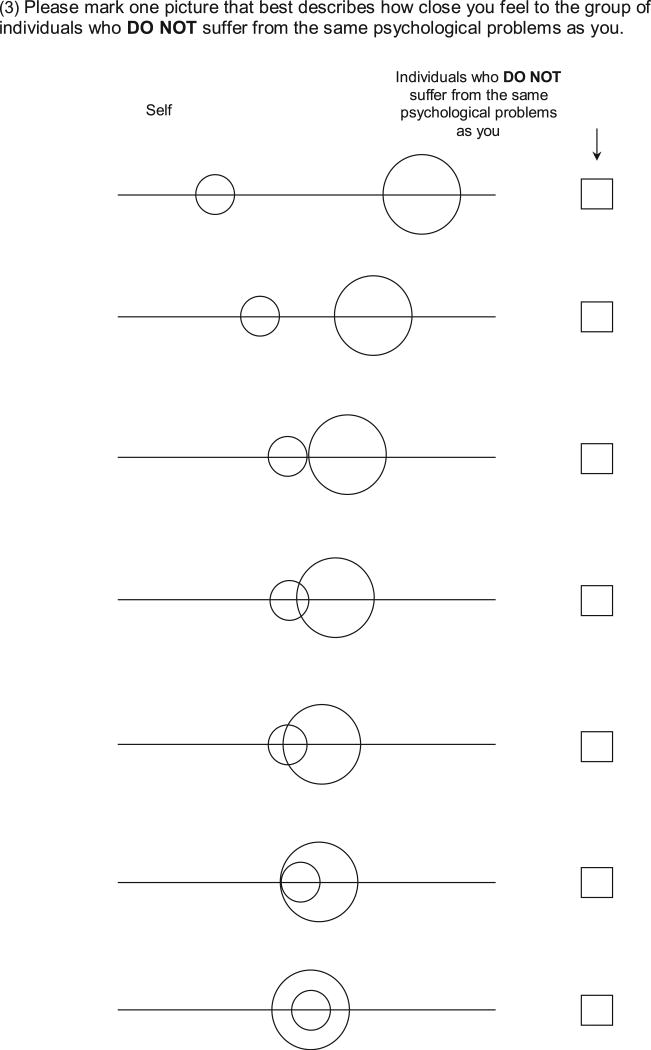
The four items (see Appendix) symbolized the following relations: 1) Perceived closeness of Ingroup and Outgroup (relation between individuals suffering from the same psychological problems (ingroup or sufferers]) compared to individuals who do not suffer from the same psychological problems [outgroup or non-sufferers]), 2) Ingroup Identification (self in relation to ingroup), 3) Outgroup Identification (self in relation the outgroup), and 4) Desired Outgroup identification (ideal closeness of self to outgroup). We denote the different items by their question number SIS-P-(1–4).
NEO-Five-Factor Inventory (NEO-FFI; Costa & McCrae, 1992)
The NEO-FFI is a valid, reliable, and widely used 60-item measure of the Five-Factor model (FFM) of personality: agreeableness, conscientiousness, extraversion, neuroticism, and openness. Decadesofresearch have established strong links between the FFM in general, and particularly neuroticism, with nearly all forms of psychopathology (Clark, Watson, & Mineka, 1994; Kotov, Gamez, Schmidt, & Watson, 2010; Malouff, Thorsteinsson, & Schutte, 2005; McCrae, 1991). In addition, FFM traits have been shown to predict treatment outcome for depressive disorders (Bagby et al., 1995, 2008). They also moderated treatment outcome in this study, as reported in Smits et al. (2013). The NEO-FFI was included to determine if SIS-P was related to treatment outcome over and above any relations it may have with the NEO. The NEO-FFI was administered only at baseline.
2. Analytical approach
Analyses were conducted using multilevel models (MLM). This analytical approach allows the inclusion of all subjects regardless of missing data, thereby improving power and generalizability. It also allows nesting of repeated assessments within subjects. The growth curve of the outcome measures changed markedly from the treatment phase to the follow-up phase; therefore, the growth curve for the analyses was modeled as “piecewise” (Singer & Willett, 2003), allowing growth curve parameters (e. g., slope of change over time) to change from the treatment phase to the follow-up phase. We employed maximum likelihood estimation and an unstructured covariance matrix for the errors of the repeated measures. All models included the following control variables: treatment condition (DCS vs. pill placebo), sex, age, race, and cohabitation status.
These piecewise growth curve models were used to examine the change in the four social identification scales over time and to test the relation between social identification and outcome over time. To investigate the relation between identification and outcome, each measure of social identification was added as a time-varying predictor (TVP) of change in LSAS over time. Recent research shows that TVPs conflate between-subjects and within-subjects relations between TVPs (i.e., social identification) and outcome (i.e., LSAS) (Wang & Maxwell, 2015). Following Wang and Maxwell, we disaggregated the between- and within-subjects effects of each social identification measure by forming two predictors for each of the four social identification scales. Those two predictors for each scale were: 1) the participant's mean level of the scale across time (which comprised the “between-subjects” component of the scale), and 2) the participant's deviation score at each time point from their mean level on that scale, coded as the difference between one's score at a time point and one's mean level on the scale (the “within-subjects” component of the scale).
In order to determine the unique effect of each indicator of social identification while controlling for the others we included all four identification scales as predictors of LSAS in one MLM model. Hence, in addition to the predictors for the piecewise growth curve model mentioned above, we included the mean and deviation scores for all four social identification measures, plus their interactions with the slopes of over time (these latter terms examined whether the identification measures moderated the slopes of change in LSAS over time). As this was not a randomized experiment with respect to the social identification measures, people with different levels of social identification may have differed on a number of other variables. To control for some of these differences, we included a number of covariates: treatment condition (DCS vs. pill placebo), sex, age, race, cohabitation, having comorbid psychiatric diagnoses, baseline depressive symptoms, initial severity, neuroticism, extraversion, openness, agreeableness, and conscientiousness (all centered at their respective means). We also included treatment grouping as a level 3 clustering variable in the MLM analyses to account for the fact that participants were treated in groups.
Follow-up analyses were conducted to test whether the relation between social identification and LSAS differed by treatment condition. Nonsignificant interactions were dropped from all models. Because no generally accepted measure for effect size currently exists in MLM analyses, we used the t to Cohen's d effect size transformation to estimate the effect size for all significant effects.
Note that we had up to 6 assessments for each subject, which yielded a total of 880 data points for the MLM analyses. Thus, although we had quite a few predictors in the MLM models, power analyses, conducted using the MLM power analysis program PinT 2.12 (Snijders & Bosker,1993), indicated greater than 0.95 power to detect a medium effect size for the social identification predictors. Since we had no a priori reason to believe that receiving DCS vs. Placebo would impact the effect of social identification on CBT outcome, the DCS treatment × social identification interaction was explored in supplementary exploratory analyses only.
3. Results
This study is a secondary analysis of data from a larger investigation (Hofmann et al., 2013). The major outcome results from this study, including change in LSAS as a result of treatment, are reported in Hofmann et al. (2013). As reported in the outcome study, there were no significant differences between treatment conditions on demographics or on the baseline levels of the primary study variables. See Table 1 for descriptive information about the sample on our psychological variables.
Table 1.
Descriptive statistics: Clinical and personality characteristics, identification.
| Pretreatment | Midtreatment | Posttreatment | 1FU | 3FU | 6FU | |
|---|---|---|---|---|---|---|
| Clinical Characteristics at Baseline | ||||||
| CGI-Severity | 5.29 (0.84) | |||||
| MADRS | 12.53 (8.69) | |||||
| Neuroticism | 32.17 (7.19) | – | – | – | – | |
| Extraversion | 19.08 (6.81) | – | – | – | – | – |
| Openness | 30.01 (6.04) | – | – | – | – | – |
| Agreeableness | 30.10 (6.22) | – | – | – | – | – |
| Conscientiousness | 27.23 (8.42) | – | – | – | – | |
| Changes in Social Anxiety Severity and Social Identification | ||||||
| LSAS | 81.65 (16.08) | 53.10 (18.52) | 39.76 (19.96) | 39.35 (20.21) | 39.87 (21.20) | 40.36 (22.16) |
| SIS-P-1 | 2.38 (1.36) | 2.98 (1.48) | 3.31 (1.47) | 3.16 (1.48) | 3.09 (1.44) | 3.19 (1.50) |
| SIS-P-2 | 3.67 (1.62) | 4.28 (1.37) | 4.63 (1.27) | 4.44 (1.39) | 4.14 (1.35) | 4.35 (1.27) |
| SIS-P-3 | 2.09 (1.29) | 2.73 (1.40) | 3.17 (1.41) | 3.13 (1.53) | 3.10 (1.60) | 3.18 (1.54) |
| SIS-P-4 | 5.44 (1.60) | 5.03 (1.64) | 5.19 (1.42) | 5.11 (1.44) | 5.22 (1.47) | 5.20 (1.47) |
Note. LSAS = Liebowitz Social Anxiety Disorder Scale; CGI = Clinical Global Impression; MADRS = Montgomery Asberg Depression Rating Scale; SIS-P = Social-Identification Scale for Psychiatric Disorders [SIS-P-1: ingroup-outgroup, SIS-P-2: self-ingroup, SIS-P-3: self-outgroup, SIS-P-4: aspired self-outgroup].
3.1. Correlations
Bivariate correlations among the study variables at baseline are presented in Table 2. As can be seen, the SIS-P scales were largely independent from social anxiety, depression, and the FFM, highlighting our hypothesis that this may be a new construct that has yet to be explored in social anxiety. The strongest associations were small in magnitude with the greatest being r = .26. The individual SIS-P scales were only modestly correlated with each other (rs ≤ 0.19) except for the strong relation between SIS-P-1 (perceived closeness of the ingroup and outgroup) and SIS-P-3 (identification with the outgroup), r = 0.63.
Table 2.
Correlation of the clinical and personality measures at baseline.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.LSAS | ||||||||||||
| 2.CGI-Severity | 0.78b | |||||||||||
| 3.MADRS | 0.30b | 0.26b | ||||||||||
| 4.SIS-P-1 | −.12 | −.15a | −.24b | |||||||||
| 5.SIS-P-2 | −0.04 | 0.03 | −0.01 | 0.16a | ||||||||
| 6.SIS-P-3 | −0.18 | −0.16a | −0.22b | 0.63b | 0.19a | |||||||
| 7.SIS-P-4 | 0.10 | 0.06 | −0.03 | 0.01 | 0.19a | 0.02 | ||||||
| 8.Neuroticism | 0.36b | 0.34b | 0.53b | −0.26b | 0.02 | −0.24b | 0.10 | |||||
| 9.Extraversion | −0.34b | −0.33b | −0.30b | 0.18a | −0.04 | 0.22b | −0.01 | −0.39 | ||||
| 10.Openness | −0.10 | −0.13 | −0.05 | −0.03 | 0.04 | −0.03 | −0.13 | 0.12 | 0.03 | |||
| 11.Agreeableness | −0.15a | −0.20b | −0.27b | 0.17a | −0.02 | 0.18a | −0.03 | −0.17a | 0.17a | 0.07 | ||
| 12.Conscientiousness | 0.30b | 0.26b | −0.39b | 0.07 | −0.05 | 0.03 | −0.09 | −0.43b | 0.42a | −0.03 | 0.28b |
Note. LSAS = Liebowitz Social Anxiety Disorder Scale; CGI = Clinical Global Impression; MADRS = Montgomery Asberg Depression Rating Scale, SIS-P=Social-Identification Scale for Psychiatric Disorders [SIS-P-1: ingroup-outgroup, SIS-P-2: self-ingroup, SIS-P-3: self-outgroup, SIS-P-4: aspired self-outgroup].
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
3.2. Change in social identif2ication and relation to outcome
Below we report the results for each SIS-P scale. For each of these scales (see Appendix), we first report the change in the scale over time (from four piecewise growth curve models, one for each scale), and then report the relation of the scale to LSAS (from the single MLM model which included all four identification scales as simultaneous, disaggregated predictors of LSAS).
3.2.1.Perceived closeness of ingroup and outgroup
The first item (SIS-P-1) instructed patients to mark the picture that best describes the perceived closeness between individuals suffering from the same psychological problems as themselves (ingroup) and individuals who did not suffer from the same problems (outgroup). As previously noted, participants received a score of 1 if they selected the first picture (indicating no overlap), to 7 if they selected the 7th picture (complete overlap). At pretreatment, patients on average chose a picture that depicted no overlap between the ingroup and outgroup (mean (SD): 2.38 (1.36), see Appendix for the visualization of the scores). The piecewise growth model for SIS-P-1 showed that the slope of change during the treatment phase was significant, b = 0.07, t(250) = 7.82, p < 0.001, d = 0.99, with ingroup-outgroup overlap increasing over time. Patients chose partly overlapping circles at post (M = 3.31 [1.47]). This slope of change during treatment did not vary by DCS treatment group. Also, ingroup-outgroup overlap did not change during the follow-up period, b = 0.00, t(355) = −0.22, p=.83.
The MLM analysis of the relation between social identification and LSAS indicated that deviations from a person's mean level of ingroup-outgroup differentiation were marginally related to LSAS, within individuals over time. When individuals reported relatively higher levels of closeness between ingroup and outgroup (higher than their average level), they were marginally more likely to report lower social anxiety severity (LSAS), b = −0.61, t(413) = −1.82, p = 0.069, d = 0.18. Mean level of perceived closeness between ingroup and outgroup (between-subjects) was not significantly related to LSAS.
3.2.2. Ingroup Identification
The second item (SIS-P-2) asked patients to mark the picture that best describes their perceived closeness to individuals suffering from the same psychological problems as them (ingroup). Average scores at pretreatment indicated only a slight overlap between self and other sufferers (M = 3.67 (1.62)), but there was a significant increase in self-ingroup overlap over time during treatment, b = 0.06, t(152) = 5.76, p < 0.001, d = 0.93. Participants reported greater overlap at posttreatment (M = 4.63 (1.27)). The increase in perceived overlap did not differ by treatment group. On the other hand, there was a slight but significant decrease in perceived self-ingroup overlap during follow-up, b = −0.01, t(136) = −2.18, p=.031, d = 0.37, which also did not differ by treatment group.
Analyses of the relation between self-ingroup overlap and LSAS indicated that individuals who, on average, perceived themselves as closer to individuals suffering from the same psychological problems had lower levels of social anxiety severity, b = −2.04, t(162) = −2.94, p = 0.004, d = 0.46.
3.2.3. Outgroup identification
The third item asked patients to indicate the perceived closeness between them and non-sufferers (outgroup). Similar to the ingroup-outgroup comparison (SIS-P-1), at baseline patients indicated a substantial distance between themselves and individuals who did not suffer from the same psychological problem (M = 2.09 (1.29)), but perceived themselves to be significantly closer to the outgroup at posttreatment (M = 3.17 (1.41); b = 0.08, t(154) = 8.37, p < 0.001, d = 1.35), regardless of DCS treatment condition. There was no significant change during follow-up.
Analysis of the relation between this social identification scale and LSAS showed that both the between- and within-subjects effects of the self-outgroup scale were significantly related to LSAS. Individuals who, on average, viewed themselves as closer to non-sufferers had lower LSAS scores, b = −2.44, t(162) = −2.27, p = 0.024, d = 0.36. In addition, when participants reported higher than their average perceived closeness between self and outgroup, they also reported lower social anxiety severity, b = −0.87, t(515) = −2.30, p = 0.022, d = 0.20.
3.2.4. Desired Outgroup identification
The fourth item asked the patient to indicate their desired closeness to individuals who do not suffer from the same psychological problems as they (outgroup). At baseline, patients chose pictures of almost fully overlapping circles (M = 5.44 (1.60)). Our growth curve model showed that there was a slight, marginally significant decrease in this desired overlap by posttreatment (M = 5.19 (1.42); b = −0.02, t(153) = −1.81, p = 0.072, d = 0.29). This change did not differ by DCS treatment group, and was not significant during follow-up.
Analysis of the relation between SIS-P-4 and LSAS showed that participants who had higher mean levels of desired overlap between themselves and others who did not suffer from social anxiety had higher of social anxiety symptoms, b = 1.66, t(153) = 2.57, p < 0.011, d = 0.42).
3.3. Exploratory analyses
Baseline levels of the SIS-P items were not predictors of rate of improvement in LSAS over the course of the study (p = 0.151; p = 0.072; p = 0.623; and p = 0.156, respectively, for the four SIS-P items). Furthermore, treatment condition (DCS vs. pill placebo) did not moderate the relation between LSAS and any of the social identification scales. We attempted to use the available data to determine whether there was evidence supporting the notion that changes in social identification was a cause of changes in social anxiety, or vice versa. Unfortunately, since the present study is a secondary analysis of data from a larger investigation, the data collection was not optimally designed to investigate the causal interplay between social identification and social anxiety in that social identification was assessed only at weeks 0, 8, 13, 17, 25, 37. Thus, the time lag between assessments was very long, and the likelihood that social identification at an earlier time (e.g., week 8) would predict LSAS at the next assessment many weeks later (e.g., at week 13), or vice versa, was low. Despite this limitation, we followed the approach suggested by Hamaker, Kuiper, and Grasman (2015) to perform a series of longitudinal cross lag panel analyses to determine if earlier levels of the social identification variables would predict later levels of social anxiety, controlling for earlier levels of social anxiety and vice versa. We used the disaggregated versions of each time-varying predictor, as is necessary for accurate assessment of the cross lag effect (Hamaker et al., 2015). Not surprisingly, given the long time lags between assessments, these cross lag analyses provided little support for quasi-causality in either direction. Further, examining only the treatment phase of the study (during which social identification and social anxiety did change, and hence might have changed each other), we found no significant cross lag relations in either direction.
4. Discussion
The aim of this investigation was to examine the relation between social identification and social anxiety severity in patients receiving group cognitive behavioral therapy for social anxiety disorder. The findings indicate that patients' social identification with regard to ingroup (sufferers) and outgroup (non-sufferers) changed over time. At pretreatment, patients indicated little identification with the ingroup or the outgroup, and little overlap between those groups. Patients did, however, express a desire to be close to non-sufferers. After treatment, patients viewed themselves as being closer to both sufferers (the ingroup) and non-sufferers (the outgroup), and they perceived sufferers to be more similar to non-sufferers. They also indicated a marginally significant decrease in their desire to “be like” non-sufferers.
Additionally, we found a relation between social identification and social anxiety severity. Greater perceived closeness between the self and the ingroup, and the self and the outgroup, was associated with lower social anxiety severity, as was lower perceived overlap between the ingroup and the outgroup (marginally) and lower desire to be like the outgroup. Note that these results do not imply that social identification actually caused social anxiety. It is likewise possible that changes in social anxiety drove the changes in social identification. For example, lesser symptoms of social anxiety may have led patients to logically perceive that they were closer to non-sufferers. We attempted to assess whether there was evidence for a specific direction of causality (changes in social identity causing changes in social anxiety versus changes in social anxiety causing changes in social identity) by performing longitudinal cross-lag panel analyses. However, these analyses showed no significant cross-lag paths, and hence provided no support for causality in either direction. The lack of cross-lag paths in both directions may suggest that the lags were too long in our cross-lag analyses, since they ranged from 5 weeks to 12 weeks. It may not be surprising that social identification, or social anxiety, at mid-treatment would not be highly related to social anxiety, or social identification, at posttreatment, given that therapy was ongoing during this time and both of these variables were changing throughout this time. Hence, further research is needed to determine if identification causes social anxiety, or vice versa, or whether they each impact each other.
Given the lack of temporal precedence, we can only speculate how change in social identification might have led to clinical improvement, or vice versa. Core to SAD is a profound fear of being negatively judged or devalued and ultimately rejected by others. Preoccupation with being exposed as incompetent, boring, or weak in turn leads to intense efforts to hide one's true “personality” and feelings (e.g., Heimberg et al., 2014). Such maladaptive efforts can range from subtle avoidance behaviors (e.g., averting gaze) to complete social withdrawal. One explanation for the observed associations is that reductions in social anxiety led to changes in social identity. That is, sufferers who rated themselves as closer to non-sufferers were in fact veridically closer to non-sufferers in terms of their presentations and experience. A central aim of CBT for SAD is to achieve symptom reduction by demonstrating to sufferers that the likelihood and severity of negative social consequences is less than anticipated. This is best achieved through systematic and repeated engagement with perceived social threats and a resulting violation of an expected outcome. Such engagements can easily be facilitated in group treatment settings, as was the case in the present intervention, in which group members debate critical topics or give speeches. Related to social identification, an example of misappraisal could be the idea of being perceived as weak and damaged when experiencing anxiety or nervousness in social situations. Consequently, a client may not only adopt a view that they are weak and damaged, but also view others with similar concerns in the same way. The systematic challenge of appraisals could have a normalizing impact on the sufferer's social identity and also reduce the perceived gap between self, sufferers, and non-sufferers. Viewing self/sufferers as closer to non-sufferers, as observed over the course of treatment in this study, could be an outcome of such processing. Also worth considering are expectation effects: given that CBT strives to “normalize” social fears, clients likely expect to belong to the ingroup by the end of treatment.
Taking a social psychology perspective, the observed findings could also be interpreted in the context of the well-documented impact of social identity and stigma on well-being. Mental illness has been conceptualized as a concealable stigma (Goffman, 1963). Based on the preoccupation model of secrecy (Lane & Wegner, 1995), efforts to hide aspects of one's devalued identity may spur obsessive preoccupations similar to the effects of thought suppression (e.g., Wegner, 1992). Individuals with social anxiety disorder are particularly vulnerable to social status salience. In our study, patients who perceived greater similarities between themselves and other sufferers also experienced greater symptom reductions, as compared to those who saw themselves as more distal to other social anxiety sufferers. Such seemingly contradictory phenomena may reflect what Crabtree and colleagues (2010) describe as the “both threatening and remedial” effects of identification with mental health support groups. In this model, the benefits of identification with a stigmatized group are characterized by a bi-phasic response: an initial sense of mutual belonging and acceptance (“I am, like you, a person suffering from social anxiety”), followed by the joint desire for normative change (“We support each other in changing norms/ social identifications that are maladaptive.”). As such, individuals who express openness and acceptance towards other members at treatment onset may not only feel more accepted (and less scrutinized by objective or subjective social judgement), but also receive greater social support. Greater closeness towards other sufferers may not only facilitate reductions in perceived bias but additionally indicate a greater ability to shift negative self-focus towards a positive focus on ingroup members. Reduction in self-focused attention has been associated with greater symptom reduction in prior studies (e.g., Hofmann, 2000; Bögels, 2006). On the other hand, individuals who hold stigmatizing views against themselves and others are more likely to be subjected to, or perceive, social alienation, and thus have less opportunity to correct their misappraisals. Treatment progress may be dampened in groups with a predominance of members who refuse/ deny a shared identity. Therefore shifts in identification may indicate stronger group cohesiveness. The impact of changes in group cohesiveness on treatment adherence (e.g., dropout, regular attendance, homework completion) and engagement (e.g., group participation, joint goals, constructive feedback) awaits further exploration.
A more tolerant, less dichotomous and rigid, separation of ill and healthy could be associated with an improved sense of perceived personal control (e.g., Lebowitz & Ahn, 2015), In a recent series of studies using unselected community samples, Greenaway et al. (2015) found robust positive associations between group identification and perceived personal control. They theorized an upward spiral of well-being, whereby feelings of control increase as individuals identify with groups, which in turn allows individuals to increase the quantity and quality of their social connections. As such, positive group identification (sense of belonging) and identity transition (drive for normative change), particularly when treatment is administered in a group setting, seems highly relevant to the improvement of the individual. It may facilitate cohesiveness and willingness to work as a team (e.g., Ellemers, De Gilder, & Haslam, 2004).
Taken together, the finding that social identity changed over the course of CBT is notable given that social identity is not a direct focus of CBT. This may suggest that social identification in the context of mental illness is not stable, but can change over time. As noted above, several factors may account for this finding, including the intervention itself, social group interactions, or both. Notably, studies based on the “social cure” tradition posit that a sense of belonging to a group in and of itself is protective and associated with improved social support, well-being, and health behaviors (Dingle et al., 2015; Jetten, Haslam, & Halam, 2012). However, since the present study did not include an attention control group, it remains unclear the degree to which changes in identity and changes in symptoms are due to the treatment or would have occurred in a similar fashion independently. While we cannot disaggregate the effects of group participation or sense of belong-ingness overall, CBT, even when administered in a group context, focuses predominately on symptom reduction. Social context is rarely addressed; rather, control over external situations or events is facilitated though control of one's inner experiences (thoughts, feelings) and actions. Results in the present study suggest that therapy did lead to change in social identity in some, which was positively related to therapeutic success. The exploration of targeted strategies aimed at reducing dichotomous perceptions of social identification and identity transition warrant further research.
Although this research on social identification points to a potentially important construct related to mental illness, a number of limitations deserve mention. First, the SIS-P was created for the current study based on the OSIO (Schubert & Otten, 2002), a widely used measure of identification. As such, the psychometric properties of the SIS-P are not well established. Notwithstanding, the current study provides some evidence of discriminant validity from the NEO-FFI as it was only weakly correlated with the NEO-FFI (see Table 2), and it was related to outcome over and above the NEO-FFI scales. If the current results can be replicated and yield results comparable to other established measures of social identification (e.g., Doosje, Ellemers, & Spears, 1995), then further exploration of the relation of social identification with other psychological disorders is warranted. Second, because the SIS-P was based a pictorial measure of social identification (Schubert & Otten, 2002), it is not possible to assess the relevance of distinct components of social identification for therapy success, such as sense of belonging to an ingroup, positive (or negative) emotional valence of social identity, or perceived group cohesion. Third, only a single item was used to assess each domain, and the SIS-P did not go through a rigorous iterative development process necessary for developing optimal measures. Fourth, since all participants in the study received CBT, it is not possible to know whether it was CBT that caused the changes in social identification over time, or whether these changes would have occurred naturally, without the intervention. Fifth, our cross lag analyses were unable to confirm that changes in social identification actually caused changes in social anxiety, or vice versa, possibly because the lags between assessments were too long. Finally, it is possible that the current results may underestimate the influence of patients' social perception of the self and others on treatment outcome, compared to what might be found with a more rigorously developed measure. Among the advantages of using pictorial scales is that differences in literacy are less influential than when using ratings on verbal scales, and comparisons between patients from different cultural and educational backgrounds may be more valid (Aaron, Aron, & Smollan, 1992; Li, 2002).
Despite these limitations, this study provide valuable insights into the relation of patients' social perception of the self and others and clinical improvement in the context of mental health intervention research. Social identification with others suffering from the same psychological issues, with non-sufferers, and perceiving more overlap between sufferers and non-sufferers, appear to be associated with treatment success.
Acknowledgments
This report was supported by grants R01MH075889 (to Mark Pollack, M.D.) and R01MH078308 (to Stefan Hofmann, Ph.D.) from the National Institute of Mental Health. Time dedicated to this paper was in part supported by a grant from the National Institutes of Health (NIMH K23 MH096029-01A1, to Luana Marques, Ph.D. and NIBIB 1U01EB021952-01 to Alicia Meuret, Ph.D.).
Appendix.
SIS-P
Instructions
On the following pages you find 4 groups of diagrams.
-
-
The big circles in the diagrams represent group members who either suffer from the same psychological problems or not.
-
-
Small circles represent you.
-
-
The closer the circles the closer related you perceive the group members or your relation to these members.
Please choose one picture per group of diagrams that best represent the closeness of the two groups or your closeness to one of the two groups.
Example: If you would choose the first diagram, this would mean that for you these two groups are not very close to each other.
Footnotes
Integrity and reliability of diagnoses was ensured by certification training and weekly supervision and feedback based on approximately 20% of the audio recorded assessment interviews (see Hofmann et al., 2013 for more details).
Conflicts of interest
None of the authors have any actual or potential conflict of interest related to the findings of this study.
References
- Aaron A, Aron EN, Smollan D. Inclusion of other in the self scale and the structure of interpersonal closeness. Journal of Personality and Social Psychology. 1992;63:596–612. [Google Scholar]
- Allport G. The nature of prejudice. Reading, MA: Addison-Wesley; 1954. [Google Scholar]
- Alonso J, Buron A, Rojas-Farreras S, de Graf R, Haro JM, de Girolamo G, ESEMeD/MHEDEA 2000 Investigators Perceived stigma among individuals with common mental disorders. Journal of Affective Disorders. 2009;118(1–3):180–186. doi: 10.1016/j.jad.2009.02.006. http://dx.doi.org/10.1016/j.jad.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Joffe RT, James DA, Parker DA, Kalemba V, Harkness KL. Major depression and the five-factor model of personality. Journal of Personality Disorders. 1995;9(3):224–234. http://dx.doi.org/10.1521/pedi.1995.9.3.224. [Google Scholar]
- Bagby RM, Quilty LC, Segal ZV, McBride CC, Kennedy SH, Costa PT. Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. Canadian Journal of Psychiatry. Revue Canadienne de Psy-chiatrie. 2008;53(6):361–370. doi: 10.1177/070674370805300605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreto M, Ellemers N, Banal S. Working undercover: performance-related self-confidence among members of contextually devalued groups who try to pass. European Journal of Social Psychology. 2006;36(3):337–352. http://dx.doi.org/10.1002/ejsp.314. [Google Scholar]
- Bögels SM. Task concentration training versus applied relaxation, in combination with cognitive therapy, for social phobia patients with fear of blushing, trembling, and sweating. Behavior Research and Therapy. 2006;44(8):1199–1210. doi: 10.1016/j.brat.2005.08.010. http://dx.doi.org/10.1016/j.brat.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Campbell C, Jovchelovitch S. Health, community and development: towards a social psychology of participation. Journal of Community & Applied Social Psychology. 2000;10(4):255–270. http://dx.doi.org/10.1002/1099-1298(200007/08)10, 4<255::aid-casp582>3.0.co;2-m. [Google Scholar]
- Clair JA, Beatty J, MacLean TL. Out of sight but not out of mind: managing invisible social identities in the workplace. Academy of Management Review. 2005;30(1):78–95. http://dx.doi.org/10.5465/amr.2005.15281431. [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. http://dx.doi.org/10.1037/0021-843x.103.1.103. [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002;9:35–53. http://dx.doi.org/10.1093/clipsy.9.1.35. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI): Professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Crabtree JW, Haslam SA, Postmes T, Haslam C. Mental health support groups, stigma, and self-esteem: positive and negative implications of group identification. Journal of Social Issues. 2010;66:553–569. http://dx.doi.org/10.1111/j.1540-4560.2010.01662.x. [Google Scholar]
- Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social Psychology. 4. Vol. 2. Boston,MA: McGraw-Hill; 1998. pp. 504–553. [Google Scholar]
- Cruwys T, Haslam SA, Dingle GA, Jetten J, Hornsey MJ, Chong EMD, Oei TPS. Feeling connected again: interventions that increase social identification reduce depression symptoms in community and clinical settings. Journal of Affective Disorders. 2014;159:139–146. doi: 10.1016/j.jad.2014.02.019. http://dx.doi.org/10.1016/j.jad.2014.02.019. [DOI] [PubMed] [Google Scholar]
- Cruwys T, Haslam SA, Fox NE, McMahon H. “That's not what we do”: evidence that normative change is a mechanism of action in group interventions. Behaviour Research and Therapy. 2015;65:11–17. doi: 10.1016/j.brat.2014.12.003. http://dx.doi.org/10.1016/j.brat.2014.12.003. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety disorders interview schedule for DSM-IV: Lifetime version (ADIS-IV-L) San Antonio, TX: The Psychological Corporation; 1994. [Google Scholar]
- Dingle GA, Stark C, Cruwys T, Best D. Breaking good: breaking ties with social groups may be good for recovery from substance misuse. British Journal of Social Psychology. 2015;54:236–254. doi: 10.1111/bjso.12081. http://dx.doi.org/10.1111/bjso.12081. [DOI] [PubMed] [Google Scholar]
- Doosje B, Ellemers N, Spears R. Perceived intragroup variability as a function of group status and identification. Journal of Experimental Social Psychology. 1995;31:410–436. http://dx.doi.org/10.1006/jesp.1995.1018. [Google Scholar]
- Ellemers N, van den Heuvel H, de Gilder D, Maass A, Bonvini A. The underrepresentation of women in science: differential commitment or the queen bee syndrome? The British Journal of Social Psychology. 2004;43(3):315–338. doi: 10.1348/0144666042037999. http://dx.doi.org/10.1348/0144666042037999. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis-I disorders, clinician version. Washington, D.C.: American Psychiatric Press, Inc.; 1996. [Google Scholar]
- Fung KM, Tsang HW, Corrigan PW. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatric Rehabilitation Journal. 2008;32(2):95–104. doi: 10.2975/32.2.2008.95.104. http://dx.doi.org/10.2975/32.2.2008.95.104. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Prentice-Hall; 1963. [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon and Schuster; 1986. [Google Scholar]
- Greenaway KH, Haslam SA, Cruwys T, Branscombe NR, Ysseldyk R, Heldreth C. From “we” to “me”: group identification enhances perceived personal control with consequences for health and well-being. Journal of Personality and Social Psychology. 2015 doi: 10.1037/pspi0000019. http://dx.doi.org/10.1037/pspi0000019 [Epub ahead of print] [DOI] [PubMed]
- Hamaker EL, Kuiper RM, Grasman RPPP. A critique of the cross-lagged panel model. Psychological Methods. 2015;20:102–116. doi: 10.1037/a0038889. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York, NY: Guilford Press; 2002. [Google Scholar]
- Heimberg RG, Hofmann SG, Liebowitz MR, Schneier FR, Smits JA, Stein MB, Craske MG. Social anxiety disorder in DSM-5. Depression and Anxiety. 2014;31(6):472–479. doi: 10.1002/da.22231. http://dx.doi.org/10.1002/da.22231. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Stier A. Stigma as related to mental disorders. Annual Review of Clinical Psychology. 2008;4:367–393. doi: 10.1146/annurev.clinpsy.4.022007.141245. http://dx.doi.org/10.1146/annurev.clinpsy.4.022007.141245. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Self-focused attention before and after treatment of social phobia. Behavior Research and Therapy. 2000;38:717–725. doi: 10.1016/s0005-7967(99)00105-9. http://dx.doi.org/10.1016/s0005-7967(99)00105-9. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cognitive Behaviour Therapy. 2007;36:195–209. doi: 10.1080/16506070701421313. http://dx.doi.org/10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Smits JA, Rosenfield D, Simon N, Otto MW, Meuret AE, Pollack MH. D-Cycloserine as an augmentation strategy with cognitive-behavioral therapy for social anxiety disorder. American Journal of Psychiatry. 2013;170:751–758. doi: 10.1176/appi.ajp.2013.12070974. http://dx.doi.org/10.1176/appi.ajp.2013.12070974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. The Lancet. Neurology. 2005;4:171–178. doi: 10.1016/S1474-4422(05)01014-8. http://dx.doi.org/10.1016/S1474-4422(05)01014-8. [DOI] [PubMed] [Google Scholar]
- Jetten J, Haslam C, Haslam SA. The social cure: Identity, health and well-being. London: Psychology Press; 2012. [Google Scholar]
- Jorm AF, Oh E. Desire for social distance from people with mental disorders. The Australian and New Zealand Journal of Psychiatry. 2009;43:183–200. doi: 10.1080/00048670802653349. http://dx.doi.org/10.1080/00048670802653349. [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. http://dx.doi.org/10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Lane JD, Wegner DM. The cognitive consequences of secrecy. Journal of Personality and Social Psychology. 1995;69:237–253. http://dx.doi.org/10.1037/0022-3514.69.2.237. [Google Scholar]
- Lebowitz MS, Ahn W. Emphasizing Malleability in the biology of depression: durable effects on perceived agency and prognostic pessimism. Behaviour Research and Therapy. 2015;71:125–130. doi: 10.1016/j.brat.2015.06.005. http://dx.doi.org/10.1016/j.brat.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li HZ. Culture, gender and self-close-other (s) connectedness in Canadian and Chinese samples. European Journal of Social Psychology. 2002;32:93–104. http://dx.doi.org/10.1002/ejsp.63. [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of PharmacoPsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR, Schneier F, Campeas R, Hollander E, Hatterer J, Fyer A, Klein DF. Phenelzine vs atenolol in social phobia. A placebo-controlled comparison. Archives of General Psychiatry. 1992;49:290–300. doi: 10.1001/archpsyc.49.4.290. [DOI] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophrenia Bulletin. 2004;30:511–541. doi: 10.1093/oxfordjournals.schbul.a007098. http://dx.doi.org/10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, Schutte NS. The relationship between the five-factor model of personality and symptoms of clinical disorders: a meta-analysis. Journal of Psychopathology and Behavioral Assessment. 2005;27:101–114. http://dx.doi.org/10.1007/s10862-005-5384-y. [Google Scholar]
- McCrae RR. The five-factor model and its assessment in clinical settings. Journal of Personality Assessment. 1991;57:399–414. doi: 10.1207/s15327752jpa5703_2. http://dx.doi.org/10.1207/s15327752jpa5703_2. [DOI] [PubMed] [Google Scholar]
- Mendoza-Denton R, Ayduk O, Mischel W, Shoda Y, Testa A. Person X situation interactionism in self-encoding (I am… when….): implications for affect regulation and social information processing. Journal of Personality and Social Psychology. 2001;80:533–544. http://dx.doi.org/10.1037/0022-3514.80.4.533. [PubMed] [Google Scholar]
- Mischel W, Shoda Y. A cognitive-affective system theory of personality: reconceptualizing situations, dispositions, dynamics, and invariance in personality structure. Psychological Review. 1995;102:246–268. doi: 10.1037/0033-295x.102.2.246. http://dx.doi.org/10.1037/0033-295X.102.2.246. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. The British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. http://dx.doi.org/10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Muldoon OT, Downes C. Social identification and post-traumatic stress symptoms in post-conflict Northern Ireland. British Journal of Psychiatry. 2007;191:146–159. doi: 10.1192/bjp.bp.106.022038. [DOI] [PubMed] [Google Scholar]
- Onorato RS, Turner JC. Fluidity in the self-concept: the shift from personal to social identity. European Journal of Social Psychology. 2004;34:257–278. http://dx.doi.org/10.1002/ejsp.195. [Google Scholar]
- Petersen S, van den Berg RA, Janssens T, Van den Bergh O. Illness and symptom perception: a theoretical approach towards an integrative measurement model. Clinical Psychology Review. 2011;31:428–439. doi: 10.1016/j.cpr.2010.11.002. http://dx.doi.org/10.1016/j.cpr.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? Journal of Health and Social behavior. 2000;41:188–207. http://dx.doi.org/10.2307/2676305. [Google Scholar]
- Quinn DM, Chaudoir SR. Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology. 2009;97:634–651. doi: 10.1037/a0015815. http://dx.doi.org/10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal HE, Crisp RJ. Reducing stereotype threat by blurring intergroup boundaries. Personality and Social Psychology Bulletin. 2006;32:501–511. doi: 10.1177/0146167205281009. http://dx.doi.org/10.1177/0146167205281009. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. European Psychiatry. 2005;20:529–539. doi: 10.1016/j.eurpsy.2005.04.004. http://dx.doi.org/10.1016/j.eurpsy.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Lieb K, Bohus M, Corrigan PW. Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatric Services. 2006;57:399–402. doi: 10.1176/appi.ps.57.3.399. http://dx.doi.org/10.1176/appi.ps.57.3.399. [DOI] [PubMed] [Google Scholar]
- Sani F, Madhok V, Norbury M, Dugard P, Wakefield JR. Greater number of group identifications is associated with lower odds of being depressed: evidence from a Scottish community sample. Social Psychiatry and Psychiatric Epidemiology. 2015;50:1–9. doi: 10.1007/s00127-015-1076-4. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, Liebowitz MR. Functional impairment in social phobia. The Journal of Clinical Psychiatry. 1994;55:322–331. [PubMed] [Google Scholar]
- Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica. 2012;125:440–452. doi: 10.1111/j.1600-0447.2012.01826.x. http://dx.doi.org/10.1111/j.1600-0447.2012.01826.x. [DOI] [PubMed] [Google Scholar]
- Schubert T, Otten S. Overlap of self, ingroup, and outgroup: pictorial measures of self-identification. Self and Identity. 2002;1:535–576. http://dx.doi.org/10.1080/152988602760328012. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis. New York: Oxford University Press; 2003. [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery: perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services. 2001;52:1615–1620. doi: 10.1176/appi.ps.52.12.1615. http://dx.doi.org/10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- Smart L, Wegner DM. Covering up what can't be seen: concealable stigma and mental control. Journal of Personality and Social Psychology. 1999;77:474–486. doi: 10.1037//0022-3514.77.3.474. http://dx.doi.org/10.1037/0022-3514.77.3.474. [DOI] [PubMed] [Google Scholar]
- Smart L, Wegner DM. The hidden costs of hidden stigma. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. New York: Guilford Press; 2000. pp. 220–242. [Google Scholar]
- Smits JA, Hofmann SG, Rosenfield D, DeBoer LB, Costa PT, Simon NM, Pollack MH. D-cycloserine augmentation of cognitive behavioral group therapy of social anxiety disorder: prognostic and prescriptive variables. Journal of Consulting and Clinical Psychology. 2013;81:1100–1112. doi: 10.1037/a0034120. http://dx.doi.org/10.1037/a0034120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders TA, Bosker RJ. Standard errors and sample sizes for two-level research. Journal of Educational Statistics. 1993;18:237–259. http://dx.doi.org/10.2307/1165134. [Google Scholar]
- Tajfel H, Turner JC. The social identity theory of intergroup behaviour. In: Worchel S, Austin WG, editors. Psychology of intergroup relations. 2. Chicago: Nelson-Hall; 1986. pp. 7–24. [Google Scholar]
- Turner JC, Onorato RS. Social identity, personality, and the self-concept: a self-identification perspective. In: Tyler TR, Kramer RM, John OP, editors. The psychology of the social self. Mahwah, NJ: Lawrence Erlbaum; 1999. pp. 11–46. [Google Scholar]
- Wakefield JRH, Bickley S, Sani F. The effects of identification with a support group on the mental health of people with multiple sclerosis. Journal of Psychosomatic Research. 2013;74:420–426. doi: 10.1016/j.jpsychores.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Wang L, Maxwell SE. On disaggregating between-person and within-person effects in longitudinal data using multilevel models. Psychological Methods. 2015;20:63–83. doi: 10.1037/met0000030. [DOI] [PubMed] [Google Scholar]
- Watson AC, Corrigan P, Larson JE, Sells M. Self-stigma in people with mental illness. Schizophrenia Bulletin. 2007;33:1312–1318. doi: 10.1093/schbul/sbl076. http://dx.doi.org/10.1093/schbul/sbl076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegner DM. You can't always think what you want: problems in the suppression of unwanted thoughts. In: Zanna M, editor. Advances in experimental social Psychology. Vol. 25. San Diego, CA: Academic Press; 1992. pp. 193–225. [Google Scholar]