Abstract
This study estimated the prevalence of maternal depressive symptoms and tested associations between maternal depressive symptoms and healthcare utilization and expenditures among United States publicly insured children with chronic health conditions (CCHC). A total of 6,060 publicly insured CCHC from the 2004–2009 Medical Expenditure Panel Surveys were analyzed using negative binomial models to compare healthcare utilization for CCHC of mothers with and without depressive symptoms. Annual healthcare expenditures for both groups were compared using a two-part model with a logistic regression and generalized linear model. The prevalence of depressive symptoms among mothers with CCHC was 19 %. There were no differences in annual healthcare utilization for CCHC of mothers with and without depressive symptoms. Maternal depressive symptoms were associated with greater odds of ED expenditures [odds ratio (OR) 1.26; 95 % CI 1.03–1.54] and lesser odds of dental expenditures (OR 0.81; 95 % CI 0.66–0.98) and total expenditures (OR 0.71; 95 % CI 0.51–0.98). Children of symptomatic mothers had lower predicted outpatient expenditures and higher predicted expenditures for total health, prescription medications, dental care; and office based, inpatient and ED visits. Mothers with CCHC were more likely to report depressive symptoms than were mothers with children without chronic health conditions. There were few differences in annual healthcare utilization and expenditures between CCHC of mothers with and without depressive symptoms. However, having a mother with depressive symptoms was associated with higher ED expenditures and higher predicted healthcare expenditures in a population of children who comprise over three-fourths of the top decile of Medicaid spending.
Keywords: Chronic health conditions, Maternal depressive symptoms, Healthcare utilization, Healthcare expenditures
Introduction
Childhood chronic health conditions, such as asthma, obesity, type I diabetes mellitus, and attention-deficit/hyperactivity disorder, have become increasingly common among children living in the United States (US) [1, 2]. Incongruences in the terms, definitions, and operationalizations of childhood chronic health conditions result in a wide range of estimates, which span from 3.49 to 35.3 % in children 17 years of age and younger belonging to the general population [3]. Children with chronic health conditions (CCHC) have increased healthcare utilization and expenditures compared to children without chronic health conditions [4–6]. Publicly insured CCHC receiving coverage through Medicaid and the Children's Health Insurance Program (CHIP) comprise over three-fourths of the top decile of Medicaid spending [7]. Children in the top decile of spending are more likely to be in worse health; have a chronic health condition and/or functional limitation; and disproportionately utilize emergency department (ED), hospital, and preventive care services [7].
Studies suggest that healthcare utilization and spending patterns are linked to the mother's mental health [8–12]. Distress associated with having a child with a chronic health condition can negatively affect the mother's mental health, as mothers with chronically ill children have been found to have elevated depressive symptomatology than mothers with healthy children [10, 13–16]. Maternal depressive symptoms, occurring most often in women of childbearing age [17], include cognitive, behavioral, and physical symptoms that accompany an unremitting sad mood. In one study, prevalence rates of depressive symptoms were found to range from 15.5 to 31 % in mothers of young children in a pediatric ED [8]. Maternal depressive symptoms adversely impact child health and developmental outcomes because the mother lacks the energy and focus necessary for attentive, supportive parenting [18, 19]. CCHC are particularly vulnerable to health effects of maternal depressive symptoms since management of a chronic condition requires reliable and accurate assessments and responses to the child's health needs [20, 21], which are often compromised among mothers with depressive symptoms. Mothers with depressive symptoms are more likely to have lower household incomes and greater percentages of children who are publicly insured or uninsured and experiencing poorer health [8, 9].
Growing evidence suggests that maternal depressive symptoms are associated with the child's health condition and healthcare utilization. Studies examining child healthcare practices have demonstrated that maternal depressive symptoms are related to suboptimal utilization of preventive care services (e.g., well-child visits and vaccinations) and increased utilization of acute care services (e.g., ED visits and hospitalizations) [8–12, 20, 22]. Despite more recent findings on utilization of healthcare services by mothers experiencing depressive symptoms, most studies did not use a nationally representative sample and were limited by their definition of chronic condition, as they mainly focused on specific health conditions. To our knowledge, no study, to date, has estimated the prevalence of depressive symptoms among mothers with CCHC receiving coverage through Medicaid or examined how maternal depressive symptoms affect the healthcare utilization and expenditures of this population. Therefore, the purpose of this study was to estimate the prevalence of maternal depressive symptoms and to assess the relationships between maternal depressive symptoms and healthcare utilization and expenditures in a nationally representative population of publicly insured CCHC.
Methods
Data Source and Sample
This study was a cross-sectional analysis of the 2004–2009 Medical Expenditure Panel Survey (MEPS). Developed by the Agency for Healthcare Research and Quality, the MEPS is comprised of several surveys designed to collect information on insurance coverage and healthcare utilization and expenditures. The MEPS database includes a subsample of households from the previous year's National Health Interview Survey conducted by the National Center for Health Statistics. A nationally representative sample of the US civilian non-institutionalized population is comprised of families who provide information about their demographics, health status, healthcare expenditures, and healthcare utilization, including dental and medical visits [23].
Within the MEPS database, we identified 6,060 publicly insured CCHC, where chronic condition was defined as a health condition that has lasted or is expected to last 12 months or longer and results in functional limitations and/or an ongoing need for medical care [24]. Children were identified as having a chronic health condition if they met one or more of the following conditions: (1) the caregiver reported that the child had a health condition that required ongoing medical care that had or was expected to last longer than 1 year; (2) the caregiver reported that the child had a functional limitation that had or was expected to last longer than 1 year; or (3) the child had a condition with an ICD-9 code that had been determined to meet the criteria for a chronic condition in previous studies [25, 26]. The self-reported measures were taken from the Household Component of the MEPS, and the ICD-9 codes were identified in the conditions file.
Dependent Variables
The dependent variables were healthcare utilization and healthcare expenditures. To measure healthcare utilization, we totaled the number of annual visits that the child made to each of the following settings: ED visits, inpatient admissions, preventive outpatient visits, acute outpatient visits, and dental visits. Preventive visits included visits for check-ups, immunizations, or well-child visits; all other visits were categorized as acute office based visits [27].
Annual healthcare expenditures were defined in the MEPS as the sum of direct payments for all care provided, including out-of-pocket payments and payments by private insurance, public insurance and other sources. Expenditure data were collected from parents about the care that their child received at each visit and the associated expenditures, including the source of payment and amount. Parents were asked for the total charge amount and the portion of payments made by the parent and by the insurers. Parents were also asked to provide documentation of the payment, such as a bill or receipt, if available. The expenditure data reported in the Household Component of the MEPS is corroborated with data collected from the Medical Provider Component, and the MEPS corrects any incorrect data reported in the Household Component and includes imputed expenditure data to address missing data [28].
The healthcare expenditures variable was the sum all of the expenditures associated with each healthcare setting and prescription medications. The total healthcare expenditures equaled the sum of all healthcare expenditures [28]. Inpatient expenditures included expenditures associated with both overnight and non-overnight stays and ED visits prior to admission. ED expenditures included both facility and physician expenditures. Dental care expenditures included all dental care expenses, including services rendered by general dentists, dental hygienists and all dental specialists. Prescription medication expenditures included expenditures for prescription purchases and medication refills in a given year. All expenditures were converted to 2009 dollars using the Medical Consumer Price Index.
Main Explanatory Variable
The main explanatory variable was a binary variable indicating whether or not the mother reported depressive symptoms, as determined by the Patient Health Questionnaire-2 (PHQ-2). The PHQ-2 is an abbreviated, self-administered form of the Primary Care Evaluation of Mental Disorders in which patients are asked two questions based on depressive symptoms. The PHQ-2 is used to screen for depressive symptoms and it is not equivalent to a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition diagnosis of depression. PHQ-2 scores range from 0 to 6, and a cutoff of 3 was used to indicate clinically significant depression.
Control Variables
We controlled for basic demographic variables that may be associated with maternal depressive symptoms and a childhood chronic health condition. Control variables included maternal and child age, child race and ethnicity (non-Hispanic White, non-Hispanic Black, non-Hispanic Other/multiracial and Hispanic), child gender, maternal education level (no high school, high school, at least 2 years of college), family income as a percentage of the federal poverty threshold (Poor/low-income (≤200), Middle/high-income >200), family size, and mother's marital status.
Because mothers with children with more severe health problems are more likely to report depressive symptoms [13], we controlled for three measures of the child's condition severity: (1) whether or not the child had a functional limitation; (2) child health status (excellent/good or fair/poor); and (3) maternal perception of child health. Maternal perception of child health was based on five questions from the Child Health Questionnaire, which asked for ratings of the child's health on a 5-point scale, ranging from “Definitely True” (1) to “Definitely False” (5). The five questions ask whether the: (1) child seems less healthy than other children; (2) child has never been seriously ill; (3) child usually catches whatever is going around; (4) mother expects child will have a healthy life; and 5) mother worries more than is usual about child's health. A score was constructed by summing the responses to the five questions to indicate maternal perception of child health (ranging from 5 to 25), with a low score indicating worse health. Items 2 and 4 were reverse scored to make the direction consistent. Based on the distribution of the score, we created a binary variable that indicated worse child health if the score was below 16.
Analysis
Negative binomial models were used to estimate the association between maternal depression and the number of visits for each category of utilization. Because a large number of children had no expenditures, a two-step approach was used to estimate the association between maternal depressive symptoms and health care expenditures. In the first step, we used a logistic regression model to predict having any healthcare expenditure. In the second step, we used a generalized linear model with a gamma distribution and log link, conditional on having any healthcare expenditure. We combined the models to calculate an incremental effect of maternal depressive symptoms, and an unconditional predicted healthcare expenditure for each child. The expenditure analysis was repeated for each type of healthcare expenditure separately, and for the total health expenditures. The data were analyzed using SAS 9.2 and Stata 12.0.
Results
Among the 23,730 publically insured children in our sample, we identified 6,060 (26 %) CCHC. Mothers with CCHC reported depressive symptoms at statistically significant higher prevalence than mothers with children without a chronic health condition: 19 % of mothers with CCHC reported depressive symptoms, while 13 % of mothers with children without a chronic health condition reported depressive symptoms. CCHC of mothers with depressive symptoms differed from CCHC of mothers without depressive symptoms (Table 1). CCHC of mothers with depressive symptoms were older, more likely to be non-Hispanic, and were in poorer health compared to children of mothers without depressive symptoms. Symptomatic mothers with CCHC were more likely to have less education, have a lower household income, have a larger family size and not be married compared to non-symptomatic mothers.
Table 1. Descriptive statistics for publicly insured children with a chronic health condition and their mothers (N = 6,060).
| Mother reported depressive symptoms (N = 1,151) Mean (SE)/proportion |
No reported depressive symptoms (N = 4,909) Mean (SE)/proportion |
p value | |
|---|---|---|---|
| Child age | 9.21 (0.24) | 8.06 (0.10) | 0.00 |
| Mother's age | 35.13 (0.46) | 34.32 (0.23) | 0.11 |
| Marital status (% married) | 0.35 | 0.48 | 0.00 |
| Family size | 4.12 (0.11) | 4.33 (0.05) | 0.06 |
| % Low-income (≤200 % FPL) | 0.88 | 0.80 | 0.00 |
| Education | 0.00 | ||
| No high school | 0.35 | 0.29 | |
| High school diploma | 0.57 | 0.57 | |
| College | 0.09 | 0.13 | |
| Race | 0.22 | ||
| White | 0.62 | 0.66 | |
| Black | 0.30 | 0.27 | |
| Other | 0.08 | 0.07 | |
| Ethnicity | |||
| Hispanic | 0.25 | 0.30 | 0.01 |
| Child's health status | |||
| Fair/poor | 0.14 | 0.07 | 0.00 |
| Child has functional limitation | 0.28 | 0.19 | 0.00 |
| Child poor health on health scale | 0.24 | 0.19 | 0.01 |
Values and SEs were survey weighted. P value indicates test for statistical significance of mothers reporting depressive symptoms to mothers who did not using t tests and Wald tests for variable constructs
Healthcare Utilization
The unadjusted number of ED visits was significantly higher for CCHC of mothers with depressive symptoms compared to CCHC of mothers without depressive symptoms (Table 2). Likewise, there was a trend toward a higher unadjusted number of office-based visits for CCHC of mothers with depressive symptoms than for CCHC of mothers without depressive symptoms. After adjusting for covariates, however, there were no significant differences in the number of visits between CCHC of mothers with depressive symptoms and CCHC of mothers without depressive symptoms.
Table 2. Number of visits and adjusted Incidence Rate Ratios (IRR) for each category for publicly insured children with a chronic health condition (N = 6,060).
| Mother reported depressive symptoms (N = 1,151) Mean (SE) |
No reported depressive symptoms (N = 4,909) Mean (SE) |
p value | IRR | 95 % CI | |
|---|---|---|---|---|---|
| ED visits | 0.35 (0.03) | 0.28 (0.01) | 0.02 | 1.13 | (0.96–1.33) |
| Acute office based visits | 3.67 (0.36) | 3.04 (0.18) | 0.09 | 1.04 | (0.87–1.25) |
| Preventive visits | 1.01 (0.07) | 1.03 (0.05) | 0.84 | 1.02 | (0.88–1.18) |
| Outpatient visits | 0.25 (0.05) | 0.25 (0.04) | 0.97 | 0.88 | (0.59–1.32) |
| Inpatient visits | 0.11 (0.02) | 0.08 (0.01) | 0.11 | 1.27 | (0.91–1.78) |
| Dental visits | 0.72 (0.05) | 0.77 (0.03) | 0.34 | 0.88 | (0.75–1.03) |
Means and SEs of number of visits were survey weighted. P value indicates test for statistical significance of mothers reporting depressive symptoms to mothers who did not using t tests
IRRs were calculated by taking the exponent of the coefficients of negative binomial models that were adjusted for the child's age, race and ethnicity, health status, presence of a functional limitation, health rating, maternal age, family size, family income and maternal education
Healthcare Expenditures
The unadjusted proportion of CCHC who had any ED expenditure was significantly higher for children of mothers with depressive symptoms than for children of mothers without depressive symptoms (Table 3). The unadjusted proportion of CCHC with any expenditures and dental expenditures were lower for children of mothers with depressive symptoms than for children of mothers without depressive symptoms, with marginal statistical significance. There were no significant differences in the unadjusted proportion of CCHC with any expenditures or amount of expenditures for those who had any for any other expenditure category.
Table 3. Unadjusted expenditures by category for publicly insured children with a chronic health condition (N = 6,060).
| Mother reported depressive symptoms (N = 1,151) Mean (SE)/proportion |
No reported depressive symptoms (N = 4,909) Mean (SE)/proportion |
p value | |
|---|---|---|---|
| Total | |||
| Any expenditure | 0.91 | 0.93 | 0.06 |
| Expenditure Amount | 3,927.37 (820.45) | 3,056.92 (489.67) | 0.36 |
| Emergency Department | |||
| Any expenditure | 0.23 | 0.18 | 0.01 |
| Expenditure Amount | 398.22 (37.91) | 513.70 (35.51) | 0.02 |
| Office based visit | |||
| Any expenditure | 0.78 | 0.81 | 0.18 |
| Expenditure amount | 698.59 (71.33) | 596.81 (38.08) | 0.19 |
| Inpatient hospital | |||
| Any expenditure | 0.23 | 0.22 | 0.47 |
| Expenditure amount | 21,060.67 (9,533.23) | 14,190.70 (256,035.00) | 0.49 |
| Outpatient | |||
| Any expenditure | 0.25 | 0.25 | 0.91 |
| Expenditure amount | 1,180.83 (346.73) | 1,039.10 (90.15) | 0.69 |
| Prescription medication | |||
| Any expenditure | 0.74 | 0.74 | 0.93 |
| Expenditure amount | 859.89 (62.50) | 740.15 (94.37) | 0.28 |
| Dental | |||
| Any expenditure | 0.37 | 0.40 | 0.10 |
| Expenditure amount | 364.00 (69.05) | 275.00 (17.19) | 0.21 |
Values and SEs were survey weighted. P value indicates test for statistical significance of mothers reporting depressive symptoms to mothers who did not using t tests
After adjusting for covariates, CCHC of mothers with depressive symptoms had lower odds of incurring any healthcare expenditure OR 0.71 (95 % CI 0.51–0.98) and any dental expenditure OR 0.81 (95 % CI 0.66–0.98) than CCHC of mothers without depressive symptoms (Table 4). However, CCHC of mothers with depressive symptoms were more likely to incur a healthcare expenditure in an ED OR 1.26 (95 % CI 1.03–1.54) than CCHC of mothers without depressive symptoms. Among CCHC who incurred any expenditure, no significant difference was observed in the amount of healthcare expenditures between the two groups for any type of care.
Table 4. Adjusted expenditures by category for publicly insured children with a chronic condition (N = 6,060).
| Any expenditure | Expenditure amount if any | Combined incremental effect | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| OR | 95 % CI | β | 95 % CI | IE ($) | 95 % CI | |
| Total expenditures | 0.71* | (0.51–0.98) | 0.12 | (−0.08–0.31) | 281.67* | (270.40–292.94) |
| ED expenditures | 1.26* | (1.03–1.54) | −0.18 | (−0.39–0.02) | 0.86* | (0.76–0.96) |
| Office visit expenditures | 0.85 | (0.67–1.09) | 0.14 | (−0.07–0.34) | 54.30* | (53.28–55.32) |
| Inpatient hospital | ||||||
| Expenditures | 1.07 | (0.85–1.34) | –0.07 | (−0.50–0.36) | −40.10* | (−41.35 to –38.80) |
| Outpatient expenditures | 0.95 | (0.76–1.20) | –0.09 | (−0.59–0.41) | –30.16* | (–30.62 to –29.71) |
| Prescription | ||||||
| Expenditures | 0.96 | (0.78–1.17) | 0.03 | (−0.15–0.21) | 12.42* | (11.97–12.86) |
| Dental expenditures | 0.81* | (0.66–0.98) | 0.16 | (−0.08–0.40) | 4.54* | (4.42–4.66) |
The combined incremental effect was calculated by combining both parts of the model with the formula IE = [Pr(y > 0lx = 1) -Pr(y >0|x = 0)] 9 E[y|y>0] + Pr(y>0) × (E[y|y>0, x = 1] – E[y|y>0, x = 0), where y is the expenditure, x is whether or not the mother reported depressive symptoms, Pr is the probability from the logit model and E[y] is the expected value of expenditures from the GLM model. The 95 % CI was estimated by bootstrapping for 1,000 repetitions
p <.05
Combining the probability of incurring any expenditure and the amount of expenditure for those who had any, we found that the combined incremental effect of having a mother with depressive symptoms was $282 (95 % CI 270–293) for total expenditure (Table 4). CCHC of mothers with depressive symptoms had higher unconditional predicted expenditures for total health expenditures, ED, office-based visits, prescription medications and dental care; and lower predicted expenditures for outpatient care (Fig. 1).
Fig. 1.
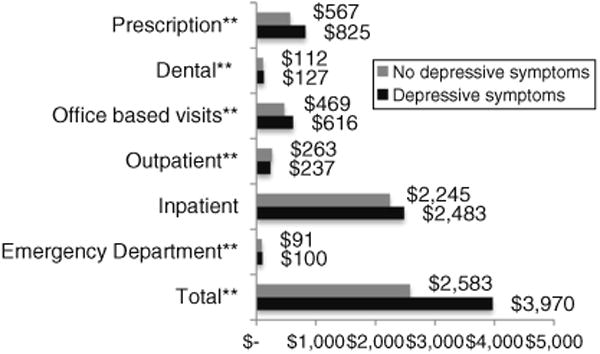
Unconditional predicted expenditures for children with mothers with and without depressive symptoms. Expenditures were calculated by multiplying the results of the two-part model (E[y|y > 0]*Probability (y > 0)). **p < .01, statistical difference between children with mothers reporting depressive symptoms compared to children with mothers reporting no symptoms. All results in 2009 US $
Discussion
Consistent with earlier studies [8, 9], we found that depressive symptoms among mothers caring for CCHC were more common than among mothers caring for children without chronic health conditions and that the presence of maternal depressive symptoms was associated with lower maternal education and household income, unmarried status, and poorer child health. There were few differences in annual healthcare utilization and expenditures between CCHC of mothers with and without depressive symptoms. However, having a mother with depressive symptoms was associated with higher ED expenditures, lower odds of a dental expenditure, and higher unconditional predicted healthcare expenditures in this high-cost publicly insured population.
While CCHC of mothers with depressive symptoms had lower odds of incurring any healthcare expenditure than CCHC of mothers without depressive symptoms, their unconditional predicted annual total expenditures were greater. Based on these expenditure patterns, we could speculate that mothers with depressive symptoms delay seeking care until the child symptoms are more severe or life threatening, which might increase health costs. These findings also could reflect the poorer health status of children of mothers with depressive symptoms compared to children of mothers without depressive symptoms.
Unlike others [8–10, 12], we found no effect on the number of annual visits to the ED by CCHC after controlling for other explanatory variables. However, we did find that CCHC of mothers with depressive symptoms were more likely to acquire healthcare expenditures related to ED use. That is, CCHC of mothers with depressive symptoms were more likely to have any ED expenditures despite no significant difference in the total number of ED visits. Further research should examine the reasons that CCHC with symptomatic mothers incur more costs with ED utilization than CCHC without symptomatic mothers.
We found that publicly insured CCHC of mothers with depressive symptoms were less likely to incur any dental expenditure compared to CCHC of mothers without depressive symptoms. One possible explanation is that publicly insured CCHC of mothers with depressive symptoms are not receiving routine dental care, which may contribute to the finding that dental care is the highest unmet need for children [29]. Among Medicaid recipients, only 1 in 5 children received preventive dental care despite being eligible [30]. Our findings indicate that CCHC of mothers with depressive symptoms are at higher risk for not receiving a dental visit than CCHC of mothers without depressive symptoms.
Results suggest that the maternal mental health status influences the child's utilization of healthcare services and thus, healthcare providers treating CCHC may need to incorporate a more integrated approach to care. Screening for and treating maternal depressive symptoms may be important when caring for CCHC. One study [31], in particular, found significant improvements in child health with treatment of maternal depressive symptoms. Moreover, both the American Academy of Pediatrics Task Force on the Family [32] and the Bright Futures practice guidelines for pediatric care providers [33] emphasize the need to support families by addressing maternal health conditions, such as depression. Other studies have reported reductions in healthcare expenditures following treatment of maternal depression [34]. Evidence has demonstrated that pediatric care providers can effectively manage maternal depression when working in conjunction with the mother's healthcare provider [35, 36]. In an effort to enhance child health and reduce healthcare expenditures associated with chronic health conditions, pediatric care providers must recognize the utility of evaluating and treating maternal depressive symptoms in pediatric healthcare settings.
While previous research has drawn attention to the important role of maternal depressive symptoms on child healthcare utilization, these studies have mainly assessed child healthcare utilization, with only one study examining healthcare use among children with chronic health conditions. Further, neither study examined the relationship between maternal depressive symptoms and healthcare utilization in children beyond 7 years of age. Our study breaks new ground by examining both spending patterns, linking maternal risk factors to these outcomes, and studying a wider age range of CCHC. These findings emphasize the need for pediatric care providers to recognize both the higher prevalence of depressive symptoms among mothers with CCHC, and the role maternal depressive symptoms may have in the utilization of healthcare services and spending patterns among CCHC.
There are a number of study limitations that should be considered in the interpretation of our results. First, mothers with publicly insured CCHC in worse health might be more likely to both report depressive symptoms and have higher healthcare expenditures, thus resulting in selection bias in our sample. We attempted to control for bias by including additional measures of the child's health and the mother's perception of the child's health in the model. Second, because this study is cross-sectional and observational, no causal inference can be made. Third, this study relies primarily on self-reported data of health status, which can result in an inaccurate reporting of health status and depressive symptoms. Self-report bias may have impacted the mother's willingness to disclose personal mental health information, as depression is often considered a stigmatizing condition.
Conclusion
This study focused on healthcare utilization and expenditures as an initial way to understand the effects of maternal depressive symptoms on publicly insured CCHC at the population level. The high prevalence of maternal depressive symptoms among CCHC and the expenditure patterns associated with dental and ED visits call attention to issues that should be concerning to pediatric care providers and healthcare policy makers. As a way to improve the health of CCHC, pediatric care providers should consider conducting routine screenings for maternal depressive symptoms during well-child visits. Future research should be directed toward the design and implementation of evidence-based practice standards for the treatment of maternal depressive symptoms in the context of creating an efficient and cost saving health system for publicly insured chronically ill children.
Acknowledgments
This work was supported by Grant 2T32 NR007091 from the National Institute of Nursing Research, NIH to the first author and Grant 2T32 NR008856 from the National Institute of Nursing Research, NIH to the second author.
Abbreviations
- CCHC
Children with chronic health conditions
- CHIP
Children's Health Insurance Program
- ED
Emergency Department
- MEPS
Medical Expenditure Panel Surveys
- PHQ-2
Patient Health Questionnaire-2
- US
United States
Footnotes
Conflict of interest: The authors have no conflicts of interest to disclose
References
- 1.Lipton RB. Incidence of diabetes in children and youth– tracking a moving target. JAMA. 2007;297(24):2760–2762. doi: 10.1001/jama.297.24.2760. [DOI] [PubMed] [Google Scholar]
- 2.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 3.van der Lee JH, Mokkink LB, Grootenhuis MA, Heymans HS, Offringa M. Definitions and measurement of chronic health conditions in childhood: a systematic review. JAMA. 2007;297(24):2741–2751. doi: 10.1001/jama.297.24.2741. [DOI] [PubMed] [Google Scholar]
- 4.Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114(1):79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- 5.Ireys HT, Anderson GF, Shaffer TJ, Neff JM. Expenditures for care of children with chronic illnesses enrolled in the Washington State Medicaid program, fiscal year 1993. Pediatrics. 1997;100(2 Pt 1):197–204. doi: 10.1542/peds.100.2.197. [DOI] [PubMed] [Google Scholar]
- 6.Liptak GS, Shone LP, Auinger P, Dick AW, Ryan SA, Szilagyi PG. Short-term persistence of high health care costs in a nationally representative sample of children. Pediatrics. 2006;118(4):e1001–e1009. doi: 10.1542/peds.2005-2264. [DOI] [PubMed] [Google Scholar]
- 7.Kenney GM, Ruhter J, Selden TM. Containing costs and improving care for children in Medicaid and CHIP. Health Affairs. 2009;28(6):w1025–w1036. doi: 10.1377/hlthaff.28.6.w1025. [DOI] [PubMed] [Google Scholar]
- 8.Flynn HA, Davis M, Marcus SM, Cunningham R, Blow FC. Rates of maternal depression in pediatric emergency department and relationship to child service utilization. General Hospital Psychiatry. 2004;26(4):316–322. doi: 10.1016/j.genhosppsych.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 10.Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Archives of Pediatrics and Adolescent Medicine. 2001;155(3):347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- 11.Logan JE, Riley AW, Barker LE. Parental mental and pain-related health and pediatric ambulatory care sensitive emergency department visits and hospitalizations. Health Services Research. 2008;43(2):656–674. doi: 10.1111/j.1475-6773.2007.00790.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sills MR, Shetterly S, Xu S, Magid D, Kempe A. Association between parental depression and children's health care use. Pediatrics. 2007;119(4):e829–e836. doi: 10.1542/peds.2006-2399. [DOI] [PubMed] [Google Scholar]
- 13.Leao LL, Zhang L, Sousa PL, et al. High prevalence of depression amongst mothers of children with asthma. Journal of Asthma. 2009;46(4):388–391. doi: 10.1080/02770900802444237. [DOI] [PubMed] [Google Scholar]
- 14.Jaser SS, Whittemore R, Ambrosino JM, Lindemann E, Grey M. Mediators of depressive symptoms in children with type 1 diabetes and their mothers. Journal of Pediatric Psychology. 2008;33(5):509–519. doi: 10.1093/jpepsy/jsm104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aydinok Y, Erermis S, Bukusoglu N, Yilmaz D, Solak U. Psychosocial implications of Thalassemia Major. Pediatrics International. 2005;47(1):84–89. doi: 10.1111/j.1442-200x.2004.02009.x. [DOI] [PubMed] [Google Scholar]
- 16.van Oers HA, Haverman L, Limperg PF, van Dijk-Lokkart EM, Maurice-Stam H, Grootenhuis MA. Anxiety and Depression in Mothers and Fathers of a Chronically Ill Child. Maternal and Child Health Journal. 2014 doi: 10.1007/s10995-014-1445-8. [DOI] [PubMed] [Google Scholar]
- 17.Desai HD, Jann MW. Major depression in women: A review of the literature. Journal of the American Pharmaceutical Association (Washington) 2000;40(4):525–537. [PubMed] [Google Scholar]
- 18.Gross D. Implications of maternal depression for the development of young children. Image: The Journal of Nursing Scholarship. 1989;21(2):103–107. doi: 10.1111/j.1547-5069.1989.tb00108.x. [DOI] [PubMed] [Google Scholar]
- 19.Hammen C. Depression runs in families. New York: Springer; 1991. [Google Scholar]
- 20.Holland ML, Yoo BK, Kitzman H, Chaudron L, Szilagyi PG, Temkin-Greener H. Mother-child interactions and the associations with child healthcare utilization in low-income urban families. Maternal and Child Health Journal. 2012;16(1):83–91. doi: 10.1007/s10995-010-0719-z. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy P, Freudigman K, Cicchetti D, Mayes L, Benitez JL, Salloum S, et al. The mother–child interaction and clinical judgment during acute pediatric illnesses. Journal of Pediatrics. 2000;136(6):809–817. [PubMed] [Google Scholar]
- 22.Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6):e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 23.Cohen J. Design and methods of the medical expenditure panel survey household component. Rockville, MD: Agency for Healthcare Policy and Research; 1997. [Google Scholar]
- 24.Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Affairs. 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 25.Murasko JE. An evaluation of the age-profile in the relationship between household income and the health of children in the United States. Journal of Health Economics. 2008;27(6):1489–1502. doi: 10.1016/j.jhealeco.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Burwell B, Crown W, Drabek J. Children with severe chronic conditions on Medicaid. US Department of Health and Human Services; 1997. http://aspe.hhs.gov/daltcp/reports/children.pdf. [Google Scholar]
- 27.Irwin CE, Jr, Adams SH, Park MJ, Newacheck PW. Preventive care for adolescents: Few get visits and fewer get services. Pediatrics. 2009;123(4):e565–e572. doi: 10.1542/peds.2008-2601. [DOI] [PubMed] [Google Scholar]
- 28.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. www.meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp.
- 29.Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The unmet health needs of America's children. Pediatrics. 2000;105(4 Pt 2):989–997. [PubMed] [Google Scholar]
- 30.Mouradian WE, Wehr E, Crall JJ. Disparities in children's oral health and access to dental care. JAMA. 2000;284(20):2625–2631. doi: 10.1001/jama.284.20.2625. [DOI] [PubMed] [Google Scholar]
- 31.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR*D-child report. JAMA. 2006;295(12):1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 32.Schor EL. Family pediatrics: Report of the task force on the family. Pediatrics. 2003;111(6 Pt 2):1541–1571. [PubMed] [Google Scholar]
- 33.Hagan JF, Shaw JS, Duncan PM. Bright futures: Guidelines for health supervision of infants, children, and adolescents. 3rd. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 34.Perry CD. Does treating maternal depression improve child health management? The case of pediatric asthma. Journal of Health Economics. 2008;27(1):157–173. doi: 10.1016/j.jhealeco.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 35.Olson AL, Dietrich AJ, Prazar G, Hurley J. Brief maternal depression screening at well-child visits. Pediatrics. 2006;118(1):207–216. doi: 10.1542/peds.2005-2346. [DOI] [PubMed] [Google Scholar]
- 36.Feinberg E, Smith MV, Morales MJ, Claussen AH, Smith DC, Perou R. Improving women's health during international periods: Developing an evidenced-based approach to addressing maternal depression in pediatric settings. Journal of Womens Health (Larchmt) 2006;15(6):692–703. doi: 10.1089/jwh.2006.15.692. [DOI] [PubMed] [Google Scholar]


