Abstract
Background:
Only a few studies have carried out to evaluate the association of depression and anxiety with metabolic syndrome (MetS). The aim of this study was to investigate whether the depression and anxiety are associated with MetS and its different components.
Materials and Methods:
This cross-sectional study forms part of the prospective Isfahan Cohort Study. A total of 470 participants were chosen. Anxiety and depression symptoms were measured using hospital anxiety and depression scale (HADS). The MetS was diagnosed according to the American Heart Association and National Heart, Lung, and Blood Institute. One-way analysis of variance and binary logistic regression were used.
Results:
The mean age of participants was 55.7 ± 9.3. The prevalence of MetS in female participants with symptoms of depression (P < 0.0001), concurrent anxiety and depression (P = 0.004), anxiety (P < 0.0001), and asymptomatic individuals (P = 0.001) was significantly different when compared to male participants. Moreover, the analysis showed that having anxiety symptoms is in a negative relationship with MetS (odds ratio [OR] = 0.31; 95% confidence interval [CI] = 0.12–0.78). In addition, with each 10-year increase in age, the probability of MetS will decrease 40% (OR = 0.59; 95%Cl = 0.53–0.72). Body mass index (OR = 1.29; 95%CI = 1.21–1.37), and gender (higher age for women) (OR = 0.34; 95%CI = 0.11–0.98) had positive relationship with MetS.
Conclusion:
The study findings revealed that the prevalence of MetS in patients with anxiety was lower than the healthy subjects, while no significant association was found between depression, concurrent depression, an anxiety with MetS.
Keywords: Anxiety, depression, Iran, metabolic syndrome
INTRODUCTION
Metabolic syndrome (MetS) refers to a chronic, progressive, and clustering of multiple metabolic risk factors that directly increases the risk of cardiovascular disease (CVD) mortality (two or threefold), type 2 diabetes mellitus and all-causes mortality.[1,2,3,4] Indeed, the components of MetS are abdominal obesity, dyslipidemia, hypertension, impaired glucose tolerance, and insulin resistance.[5] In a recent study, findings from the Midlife in the United States National Sample showed the prevalence of MetS was 36.6%.[6] MetS prevalence in Iran and throughout the world is substantially increased during recent years from 10% to 63.2% and <10% to 84%, respectively.[7,8,9] In another study, it is interesting to note that prevalence of anxiety in patients with MetS was approximately 60%.[10] These discrepancies depend on the region, MetS definitions, methodology (longitudinal vs. cross-sectional), and composition (sex, age, race, and ethnicity) of the population studied.
Depression and anxiety are the leading causes of disability worldwide. Toward this end, depression is anticipated as the second cause of important diseases in the near future.[11] Nowadays, depressive and anxiety disorders are becoming increasingly common in the general population. In a population-based study, the 1-year prevalence rates of anxiety and mood disorders were approximately 18% and 10%, respectively.[12,13] Moreover, accumulating evidence indicates that individuals with depression and anxiety symptoms might be having interference effects which can lead to MetS.[10] Although MetS is extensively studied, existing evidence about its association with anxiety and depression on the large population is scarce, also, these studies yielded conflicting findings. A few studies have addressed the association of MetS with anxiety[14] while some authors suggested a weak or failed to find an association among those with anxiety and a current MetS condition.[10,15,16,17,18] Furthermore, several studies revealed the positive relationship between MetS and depression,[10,19,20] however, others declared no association.[15,16]
In the direction of inconsistent findings, low evidence, and few population-based studies, the aim of this study was to investigate the association of depression and anxiety with MetS and its different components in a large nationally representative population-based cohort study.
MATERIALS AND METHODS
Subjects
This cross-sectional study forms part of the prospective Isfahan Cohort Study (ICS). ICS is a community-based cohort study among 6504 individuals aged ≥35 years for detecting mortality, morbidity, and risk factors of cardinal CVDs, and also to prevent and control CVDs.[21,22] We used the data of the postintervention phase that was conducted in 2007. There were 1520 participants available in Isfahan city (rural and urban), 599 (39.4%) participants suffered from MetS. Fifteen participants had died for the last follow-up and 470 (30.9%) attended the examinations. Inclusion criteria were as follows: participating in ICS from 2001 with ATP III criteria for Mets.[23] Furthermore, exclusion criteria were as follows: (1) Participants dissatisfaction; (2) participants who had died; (3) no data on depression, anxiety; (4) no data of more than two components of MetS; (5) left the region; (6) no overnight fasting for 8 h; and (7) history of pregnancy. Written informed consents were obtained from all participants.
Measurements
Blood pressure was taken during supine rest with 15-min intervals using an automatic sphygmomanometer, three blood pressure readings were obtained, and the average of three readings was used. Body mass index (BMI) was calculated as weight divided by height in square meters (kg/m2). Waist circumference (WC) was measured by tape, horizontally 1 cm above the navel, on light clothing.[24] Blood samples were drawn after overnight fasting with standard venipuncture techniques, high-density lipoprotein (HDL) cholesterol, triglycerides, and fasting blood sugar (FBS) levels were determined using standard laboratory techniques.
Measurement of metabolic factors
The MetS was diagnosed according to the American Heart Association and National Heart, Lung, and Blood Institute's update of the National Cholesterol Education Program-Adult Treatment Panel III definition.[1] With this definition, the MetS is defined by the coexistence of three or more of the following characteristics: (1) WC ≥102 cm (40 inch) in men and 88 cm (35 inch) in women; (2) HDL <1.03 mmol/L (40 mg/dl) in men and 1.30 mmol/L (50 mg/dl) in women; (3) triglycerides ≥1.69 mmol/L (150 mg/dl); (4) blood pressure >130/85 mmHg; and (5) FBS ≥5.6 mmol/L (100 mg/dl).
Psychiatric evaluations
Anxiety and depression symptoms were measured using hospital anxiety and depression scale (HADS),[25] which is designed to detect adverse anxiety and depressive states in out-patient populations during the preceding 2 weeks. HADS is a self-report questionnaire comprising 14 four-point scale, two 7-item subscales of HADS-anxiety (HADS-A) and HADS-depression (HADS-D). Each item is answered by the patient on a four-point (0–3) response category. Hence, scores are ranged from 0 to 21 for anxiety, and 0–21 for depression.[26] The normal rate is below 8 while 8–10 indicates mild symptoms, 11–14; moderate, and 15–21 points to a severe state of depression or anxiety (using these cut-offs, we recognized four groups: anxiety only (HADS-A ≥8, HADS-D <8), depression only (HADS-A <8, HADS-D ≥8), anxiety and depression (both HADS-A and HADS-D ≥8), and a reference control group (both HADS-A and HADS-D <8). Previous studies have been revealed good internal consistency and psychometric properties for both anxiety and depression with sensitivity and specificity about 0.80.
Statistical analysis
Sample characteristics of participants were summarized; continuous variables were reported as a mean ± standard deviation, and categorical variables as numbers (percentages). The differences in mean levels of each MetS components among four groups (only depression, only anxiety, both depression and anxiety, and none of the depression and anxiety) were analyzed using one-way analysis of variance with post hoc Tukey tests. Binary logistic regression was used to explore the association of anxiety and depression with the MetS and its individual components, and in this analysis, the MetS and its components were considered dependent variable. As potential confounding factors affecting the metabolic abnormalities, we used age, gender, smoking, BMI, and age-gender interaction. Results of logistic regression analysis were presented as adjusted odds ratios (ORs) with 95% confidence intervals (CIs). The values of P < 0.05 were considered statistically significant. The statistical analyses were undertaken using the Statistical Program for Social Sciences software system version 18.0 (SPSS Inc., Chicago, IL) for Windows.
RESULTS
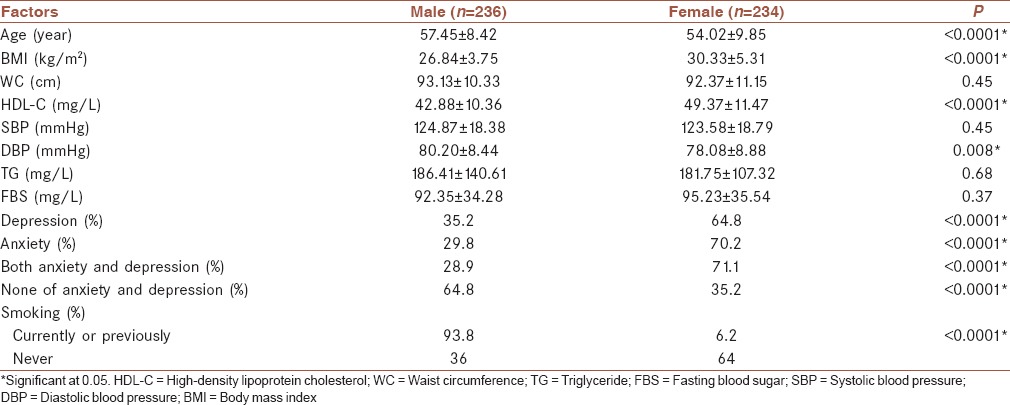
Demographic and clinical characteristics of participants divided by gender are presented in Table 1. Of the 470 participants, 236 (50.2%) were men and 234 (49.8%) were women. The mean age of participants was 55.7 ± 9.3. There was a significant difference between men and women considering the mean age and BMI (for both P < 0.0001). The prevalence of anxiety symptoms was statistically different among men and women (P <0.0001). The prevalence of depression symptoms (P <0.0001) and concurrent depression and anxiety (P <0.0001) was higher in women than men [Table 1].
Table 1.
Demographic and clinical characteristics by gender
The prevalence of MetS based on gender, smoking, and HADS categories is shown in Figure 1. Of all participants, 167 (35.5%) had MetS. The prevalence of MetS among women and men was estimated (47.5% and 23.5%, respectively) (P <0.0001) [Figure 1].
Figure 1.
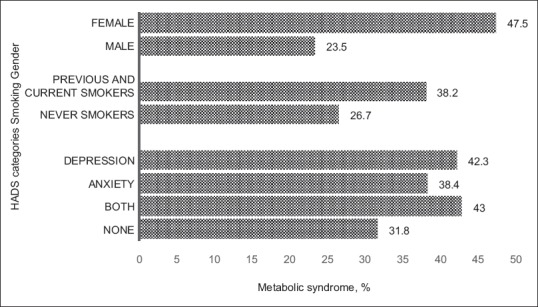
Prevalence of metabolic syndrome
Based on the HADS scores, about 50.5% of participants did not report anxiety and depression disorders, 24.5% of them reported symptoms of anxiety and depression disorders, 17% reported symptoms of depression, and 8% reported symptoms of anxiety.
In the univariate analysis, the prevalence of MetS in women with symptoms of depression (P < 0.0001), concurrent anxiety and depression (P = 0.004), anxiety (P < 0.0001), and asymptomatic individuals (P = 0.001) was significantly different from male participants.
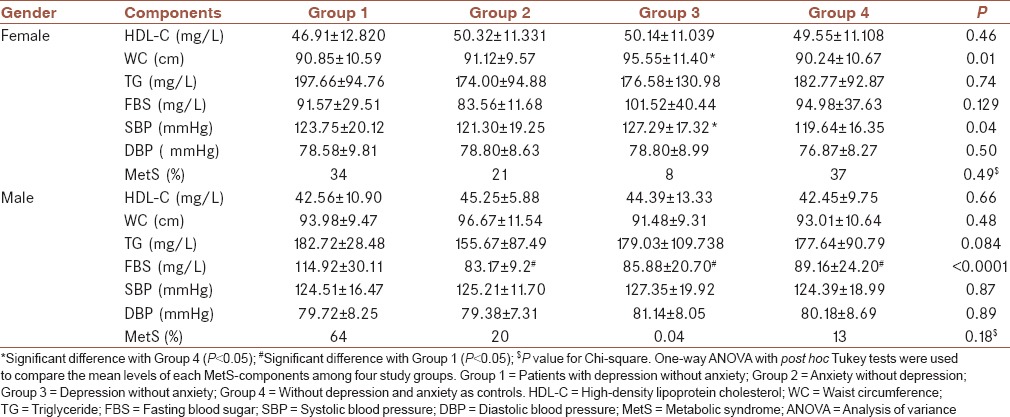
Comparison of mean levels of MetS components with HADS levels is presented in Table 2. In women, univariate analysis demonstrated that WC (P = 0.01) and systolic blood pressure (P = 0.05) in patients with concurrent depression and anxiety symptoms were significantly higher than other groups. A significant difference of FBS was observed between those men with depression symptoms and other groups (P < 0.0001). Moreover, the post hoc Tukey test revealed that only the differences of SBP and WC between the subjects with concurrent depression and anxiety versus patients without depression and anxiety (P = 0.026 and P = 0.008, respectively), were significant in women. However, only the differences of FBS between depressive patients versus patients with anxiety (P = 0.022), depressive patients versus patients with concurrent depression and anxiety (P = 0.002), and depressive patients versus patients without depression and anxiety (P < 0.0001) were significant in male [Table 2].
Table 2.
Comparison of mean levels of metabolic syndrome components with Hospital Anxiety and Depression Scale levels
Association of MetS and its components with depression and anxiety are shown in Table 3. In women, the univariate analysis indicated that having anxiety symptoms is in a negative relationship with MetS (OR = 0.33; 95%Cl = 0.14–0.74). In addition, with each 10-year increase in age, the probability of MetS will decrease 40% (OR = 0.59; 95%Cl = 0.53–0.72). On the other hand, BMI and gender (higher age for women) had a positive relationship with MetS.
Table 3.
Adjusted association of metabolic syndrome and its components with depression and anxiety
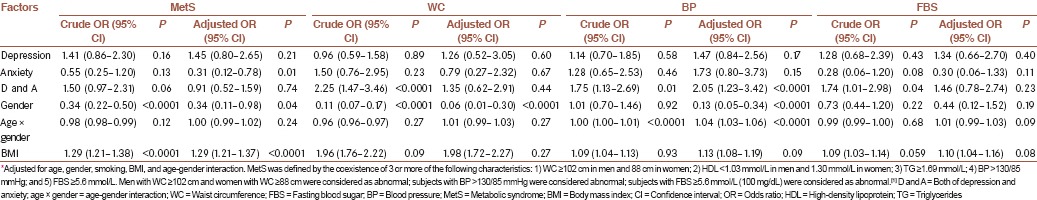
Results revealed that having none of depression, anxiety, and concurrent depression and anxiety symptoms had a significant relationship with WC. Meanwhile, age (OR = 0.25; 95%CI = 0.18–0.35), gender, aging in women (OR = 4.33; 95%CI = 2.56–7.31), and BMI had a significant relationship with WC.
According to the obtained results, aging in women (OR = 2.17; 95%CI = 1.59–3.09) and being male (OR = 0.02; 95%CI = 0.001–0.1) contributed to increase and decrease the likelihood of hypertension, respectively. However, other factors had no significant relationship with blood pressure.
In addition, FBS was not affected by depression, anxiety, and concurrent depression and anxiety. BMI is a risk factor for higher than expected FBS while aging contributed to the reduction of this probability (OR = 0.65; 95%CI = 0.50–0.84) (adjusted R2 = 0.21) [Table 3].
DISCUSSION
In the current community-based study, the relationship of the presence of depression, anxiety, and concurrent depression and anxiety with MetS was assessed in a large nationally representative population-based cohort study. Based on the study results, the presence of anxiety symptoms contributed to decreasing the likelihood of MetS. In the univariate analysis, depression had a positive relationship with MetS. However, no significant relationship was observed between anxiety and MetS. These findings were in contrast to Räikkönen et al. study on women.[27] Meanwhile, there are various studies which are incongruent with results of these two studies.[18]
It could be concluded that lack of relationship between anxiety and other components of MetS could be a reason for the fact that the relationship between MetS and anxiety is not through components of MetS, and probably, biological process can verify the relationship between psychological disorders and MetS.[18]
Several studies revealed that depression and MetS have a mutual relationship with each other[17,28,29] which is in contrary with the current results. As a result, we assessed this relationship for men and women separately, and there was no significant relationship. The present findings were in contrast to the study of Muhtz et al.[17,30] These discrepancies can be due to various methods used in these studies to measure depression symptoms or different definitions for MetS. Each of these disorders may be effective as a distal determinant through the effect of weight and amount of received calorie on MetS.
To justify the recent findings, another point is self-reported tool was used in our study and cultural context of Iranian to overstate their pain and discomfort,[31] While biological relationships are not affected by the severity of symptoms. On the other hand, epidemiological studies demonstrated that higher-degree of depression has a more intense association with MetS.[32] Therefore, this difference can be due to lower severity of depression symptoms among participants of the current study.
Although, results of the univariate analysis demonstrated a positive relationship between having anxiety, depression, and concurrent anxiety and depression with WC, like other studies,[33,34] this effect was not observed in the final model. It seems that BMI and gender confound this effect since this effect in univariate analysis and without the presence of BMI and gender was considered as a predictive variable.
Although this study was conducted on a community-based Iranian adult, cross-sectional nature of data did not allow assessing the relationship between anxiety and MetS. Furthermore, while the sample size of the current study was not small, but according to the small proportion of participants who had concurrent depression and anxiety symptoms, the statistical power of multivariate analysis of findings of this part may not be adequate. Meanwhile, consistency of other results of the current study with international documents can be used to justify the accuracy of other findings. Another limitation of this study was using the self-reported tool to determine the level of depression and anxiety. Therefore, more studies based on a diagnosis of psychological disorders instead of self-reported tools are needed.
CONCLUSION
The present study revealed that the prevalence of MetS in patients with anxiety was lower than the healthy subjects, while no significant association was found between depression, concurrent depression, an anxiety with MetS. The study findings do not make us needless for further investigations, so we suggest such studies with the possibility of neural nutritional disorders with the context of anxiety and depression, and using a diagnostic method for psychological disorders instead of self-reported methods should be considered.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–72. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 3.Miettola J, Niskanen LK, Viinamäki H, Sintonen H, Kumpusalo E. Metabolic syndrome is associated with impaired health-related quality of life: Lapinlahti 2005 study. Qual Life Res. 2008;17:1055–62. doi: 10.1007/s11136-008-9386-6. [DOI] [PubMed] [Google Scholar]
- 4.Kahl KG, Schweiger U, Correll C, Müller C, Busch ML, Bauer M, et al. Depression, anxiety disorders, and metabolic syndrome in a population at risk for type 2 diabetes mellitus. Brain Behav. 2015;5:e00306. doi: 10.1002/brb3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. American Heart Association; National Heart, Lung, and Blood Institute; American Heart Association. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 6.Boylan JM, Ryff CD. Psychological well-being and metabolic syndrome: Findings from the midlife in the United States national sample. Psychosom Med. 2015;77:548–58. doi: 10.1097/PSY.0000000000000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelishadi R, Gharipour M, Sadri GH, Tavasoli AA, Amani A. Cardiovascular disease risk factors, metabolic syndrome and obesity in an Iranian population. East Mediterr Health J. 2008;14:1070–9. [PubMed] [Google Scholar]
- 8.Zabetian A, Hadaegh F, Azizi F. Prevalence of metabolic syndrome in Iranian adult population, concordance between the IDF with the ATPIII and the WHO definitions. Diabetes Res Clin Pract. 2007;77:251–7. doi: 10.1016/j.diabres.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein Sadri G, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: An emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131:90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 10.Skilton MR, Moulin P, Terra JL, Bonnet F. Associations between anxiety, depression, and the metabolic syndrome. Biol Psychiatry. 2007;62:1251–7. doi: 10.1016/j.biopsych.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Ghanei Gheshlagh R, Parizad N, Sayehmiri K. The relationship between depression and metabolic syndrome: Systematic review and meta-analysis study. Iran Red Crescent Med J. 2016;18:e26523. doi: 10.5812/ircmj.26523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 13.Butnoriene J, Bunevicius A, Saudargiene A, Nemeroff CB, Norkus A, Ciceniene V, et al. Metabolic syndrome, major depression, generalized anxiety disorder, and ten-year all-cause and cardiovascular mortality in middle aged and elderly patients. Int J Cardiol. 2015;190:360–6. doi: 10.1016/j.ijcard.2015.04.122. [DOI] [PubMed] [Google Scholar]
- 14.Carroll D, Phillips AC, Thomas GN, Gale CR, Deary I, Batty GD. Generalized anxiety disorder is associated with metabolic syndrome in the Vietnam experience study. Biol Psychiatry. 2009;66:91–3. doi: 10.1016/j.biopsych.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Hildrum B, Mykletun A, Midthjell K, Ismail K, Dahl AA. No association of depression and anxiety with the metabolic syndrome: The Norwegian HUNT study. Acta Psychiatr Scand. 2009;120:14–22. doi: 10.1111/j.1600-0447.2008.01315.x. [DOI] [PubMed] [Google Scholar]
- 16.Herva A, Räsänen P, Miettunen J, Timonen M, Läksy K, Veijola J, et al. Co-occurrence of metabolic syndrome with depression and anxiety in young adults: The Northern Finland 1966 Birth Cohort Study. Psychosom Med. 2006;68:213–6. doi: 10.1097/01.psy.0000203172.02305.ea. [DOI] [PubMed] [Google Scholar]
- 17.Takeuchi T, Nakao M, Nomura K, Inoue M, Tsurugano S, Shinozaki Y, et al. Association of the metabolic syndrome with depression and anxiety in Japanese men: A 1-year cohort study. Diabetes Metab Res Rev. 2009;25:762–7. doi: 10.1002/dmrr.1041. [DOI] [PubMed] [Google Scholar]
- 18.Goldbacher EM, Matthews KA. Are psychological characteristics related to risk of the metabolic syndrome? A review of the literature. Ann Behav Med. 2007;34:240–52. doi: 10.1007/BF02874549. [DOI] [PubMed] [Google Scholar]
- 19.McCaffery JM, Niaura R, Todaro JF, Swan GE, Carmelli D. Depressive symptoms and metabolic risk in adult male twins enrolled in the National Heart, Lung, and Blood Institute twin study. Psychosom Med. 2003;65:490–7. doi: 10.1097/01.psy.0000041545.52924.82. [DOI] [PubMed] [Google Scholar]
- 20.Rhee SJ, Kim EY, Kim SH, Lee HJ, Kim B, Ha K, et al. Subjective depressive symptoms and metabolic syndrome among the general population. Prog Neuropsychopharmacol Biol Psychiatry. 2014;54:223–30. doi: 10.1016/j.pnpbp.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Mohammadifard N, Sarafzadgan N, Sadri G, Malek AH, Shahrokhi S, Tolooie H, et al. Isfahan Healthy Heart Program: A Comprehensive Integrated Community-Based Program for Cardiovascular Disease Prevention and Control. Design, Methods and Initial Experience 2000-2001. 2002 [Google Scholar]
- 22.Sarrafzadegan N, Baghaei A, Sadri G, Kelishadi R, Malekafzali H, Boshtam M, et al. Isfahan healthy heart program: Evaluation of comprehensive, community-based interventions for non-communicable disease prevention. Prev Control. 2006;2:73–84. [Google Scholar]
- 23.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 24.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 26.Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Räikkönen K, Matthews KA, Kuller LH. The relationship between psychological risk attributes and the metabolic syndrome in healthy women: Antecedent or consequence? Metabolism. 2002;51:1573–7. doi: 10.1053/meta.2002.36301. [DOI] [PubMed] [Google Scholar]
- 28.Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30:1–10. doi: 10.1016/j.psyneuen.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Toker S, Shirom A, Melamed S. Depression and the metabolic syndrome: Gender-dependent associations. Depress Anxiety. 2008;25:661–9. doi: 10.1002/da.20379. [DOI] [PubMed] [Google Scholar]
- 30.Muhtz C, Zyriax BC, Klähn T, Windler E, Otte C. Depressive symptoms and metabolic risk: Effects of cortisol and gender. Psychoneuroendocrinology. 2009;34:1004–11. doi: 10.1016/j.psyneuen.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Lotfi MH, Aminian AH, Ghomizadea A, Zarea S. Prevalence of depression amongst students of Shaheed Sadoughi university of medical sciences, Yazd, Iran. Iran J Psychiatry Behav Sci. 2010;4:51–5. [Google Scholar]
- 32.Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, et al. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–80. doi: 10.2337/dc11-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hach I, Ruhl UE, Klotsche J, Klose M, Jacobi F. Associations between waist circumference and depressive disorders. J Affect Disord. 2006;92:305–8. doi: 10.1016/j.jad.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 34.Ho RC, Niti M, Kua EH, Ng TP. Body mass index, waist circumference, waist-hip ratio and depressive symptoms in Chinese elderly: A population-based study. Int J Geriatr Psychiatry. 2008;23:401–8. doi: 10.1002/gps.1893. [DOI] [PubMed] [Google Scholar]


