Abstract
Background:
Rheumatoid arthritis is a chronic autoimmune disease characterized by synovial tissue inflammation and destruction of articular components which if not controlled properly, can cause disability in patients. For this reason, evaluation of disease activity and its control is very important. In recent years using sonography is promising for the evaluation of disease activity. This study aimed to compare “clinical examination” and “ultrasonography” methods in the detection of disease activity in patients with rheumatoid arthritis.
Materials and Methods:
This cross-sectional study was conducted during 2015 in Al-Zahra Hospital of Isfahan. Based on the American College of Rheumatology 2010 criteria, ninety patients with rheumatoid arthritis who diagnosed by rheumatologist entered into the study. All patients, collaborator by radiologists were subjected to sonography of specific joints structures using two methods, i.e., high-resolution ultrasonography and power Doppler.
Results:
A total of 2520 joints from ninety patients were examined by physical examination and ultrasonography that 244 joints (9.7%) in physical examination and 348 joints (13.4%) in ultrasonography were involved and the difference between the two groups was statistically significant (P < 0.001).
Conclusion:
Probably, ultrasonography can diagnose joint involvement better than physical examination in patients with Rheumatoid arthritis.
Keywords: Rheumatoid arthritis, synovitis, ultrasonography
INTRODUCTION
Rheumatoid arthritis is a chronic autoimmune disease characterized by synovial tissue inflammation and destruction of articular components which if not controlled properly, can cause disability in patients. Community-based studies have shown that mortality in patients with rheumatoid arthritis in developing countries is more than developed countries.[1] According to the World Health Organization statistics about the burden of the disease, years of lost due to disability, years of potential life lost and daily adjusted life year for rheumatoid arthritis are 4488, 48.1, and 4636 years, respectively.[1] In a large cohort study of 17,085 patients, annual medical costs in patients with rheumatoid arthritis were more than 5900 dollars and lifetime medical costs were more than 93,000 dollars.[2]
Management of rheumatoid arthritis such as the determination of treatment decisions depends on a number of factors. Although the level of disease activity is of paramount importance, the disease duration, acknowledgement of poor prognostic factors (e.g., seropositivity for rheumatoid factor [RF] and/or anti-cyclic citrullinated peptide [anti-CCP], erosions, and extra-articular disease), and the level of patient's disability as well as self-reported impact of disease have to be taken into account.[3]
The most important way to prevent these debilitating complications and costs is properly control of the disease. Generally, rheumatoid arthritis activity is evaluated by clinical and laboratory parameters such as erythrocytes sedimentation rate (ESR) and C-reactive protein (CRP). Furthermore conventionally, the degree of disease activity has been evaluated by measuring subjective clinical variables, laboratory measures, and radiographic findings.[2,4,5] However, clinical evaluation of joint pain and swelling have not been sufficiently reliable,[3] and conventional plain radiography depicts indirect signs of cartilage loss and bone erosions due to previous destructive synovial inflammatory activity.[6] In recent years, ultrasonography has been shown to be highly effective in assessing joint abnormalities, like bone destruction and inflammation in finger joints[7] and also the results of joint evaluation in many studies have been in favor of ultrasonography compared with a physical exam.[3,5,6,7] High-frequency ultrasonography (US) has greatly improved musculoskeletal imaging in rheumatology.[6] Several studies have revealed that the high-frequency US is accurate for detecting joint effusion[7,8,9,10,11,12] and synovitis,[8,9,10,11,12] compared with magnetic resonance imaging (MRI) and direct arthroscopic visualization. US is more sensitive and reproducible than clinical evaluation in assessing joint inflammation. This study was aimed to compare physical examination and ultrasonography for detection of joints involvement in patients with rheumatoid arthritis.
MATERIALS AND METHODS
This study is a cross-sectional study which has been conducted during the year 2015 in the Al-Zahra Hospital affiliated to Isfahan University of Medical Sciences. The subjects in this study were ninety patients with rheumatoid arthritis who were selected based on the American College of Rheumatology 2010 and EULAR criteria and referred to the rheumatology outpatient clinic.[2] Patients with a history of joints involvement of crystalline disease, history of intra-articular injection, history of isotope synovectomy, joint surgery, infectious arthritis, and history of joint replacement surgery were excluded from this study. According to “sample size formula for correlation studies” and based on 95% of the confidence interval, 80% of power, and 30% correlation between joint involvement in physical examination and ultrasonography, ninety patients was estimated for the study.[10] These patients were selected using random sampling method from the list of patients who had recorded in rheumatology clinic. After entering the clinic, at first, demographic data and history of the disease were asked and entered to collection data form. Then, RF (by agglutination tests) and the anti-CCP antibody (recognizes arginine residues modified by peptidylarginine deiminase. Anti-CCP belongs to the family of antifilaggrin autoantibodies, accompanied by the anti-keratin antibody and the antiperinuclear factor) was measured for all patients and then each patient was examined by a rheumatologist. In this study, only 28 joints which are used in Disease Activity Score (DAS-28) tool were evaluated by examination and ultrasonography.[8]
Twenty-eight joints in each patients included 10 proximal interphalangeal (PIP) joints, 10 metacarpophalangeal (MCP) joints, 2 wrist joints, 2 elbow joints, 2 shoulder joints, and 2 knee joints were studied.
Individual characteristics (age, sex, medications, disease duration, DAS-28) with the result of the examinations and laboratory tests (including ESR, CRP, RF, and anti-CCP) were recorded in a questionnaire. Before completing the questionnaire and performing ultrasound, explanation about the scheme was given to each patients and informed consent form was completed and signed by the patients. After completing the examination, the patients were referred to the radiology department to have joint ultrasound by radiologist collaborator. It should be noted that the radiologist was not aware of the clinical examination results.
Each patient information collected includes the following: Age, marital status, duration of disease, medications, RF, anti-CCP, duration of morning stiffness (in minutes), Visual Analog Scale Patient (VAS-P), the clinical examination findings include tenderness and swelling of joints (intensity from 0 to 3), ultrasound findings include effusion, synovitis, and power Doppler (intensity from 0 to 3).[3,7]
For ease of comparison of ultrasound and examination results, any joint or joints group were examined separately. For example, ultrasound and examination results of PIP joints were compared and therefore were divided into 6 categories including interphalangeal, MCP, wrist, elbow, shoulder, and knee joints.
Joints involvement were examined separately for each patient based on DAS-28, included tender joint count (TJC), swollen joint count (SJC), swollen joint index, ultrasound joint effusion count, ultrasound joint synovitis count (US-JSC), and ultrasound power Doppler joint count. The activity of the disease such as clinical symptoms was measured using DAS-28.
Finally, collected data were entered into computer and analyzed using SPSS software version 18 (IBM corporation, 2015 Armonk, New York, USA). The Chi-square, Kappa agreement, and spearman correlation test were used for data analysis.
RESULTS
In this study, ninety patients who referred to rheumatology clinic of Al-Zahra Hospital were studied. Seventy-seven (85.6%) were female and 13 (14.4%) were male. The mean age was 49.8 ± 8.8 years (range: 25–72). The mean of disease duration was 10.2 ± 4.9 years. Morning stiffness was 46.6 ± 18.2 min as average. The mean VAS-P in these patients was 45 ± 10 (in millimeter). Used medications among the patients included methotrexate 69 (76.7%), hydroxychloroquine 46 (51.1%), prednisone 86 (95.6%), leflunomide 28 (31.1%), sulfasalazine 32 (35.6%), and biologic agents 15 (16.7%).
RF and anti-CCP were positive in 69 (77%) and 60 (66.7%) of cases, respectively.
In this study, no relationship between TJC with VAS-P, ESR, and CRP were seen respectively (P = 0.17, P = 0.1 and P = 0.06).
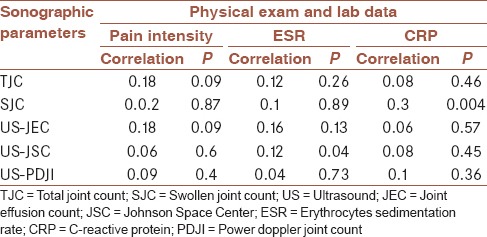
The sonographic finding showed that a number of joints involvement are not related to pain intensity, but the involvement of US-JSC was related to ESR (P = 0.04) and involvement of SJC is related to CRP (P = 0.004) [Table 1].
Table 1.
Correlation between pain intensity and inflammatory markers with sonographic findings
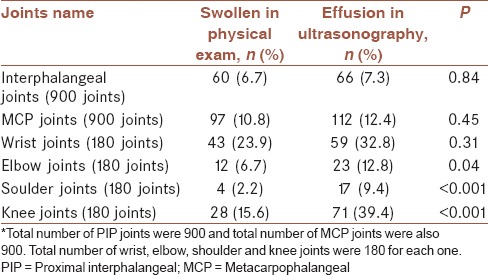
Comparison of the results of clinical examination and ultrasound findings showed that among 2520 studied joints, 244 (9.7%) swollen joints were detected in the physical examination, but 348 joints (13.8%) with effusion were detected by ultrasonography. According to Table 2, the frequency of joints involvement in elbow, shoulder, and knee was different in physical examination and ultrasonography (P < 0.001).
Table 2.
Agreement of clinical examination and ultrasonography in joints effusion*
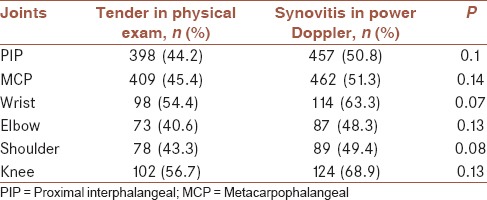
Frequency distribution of tender joints (in the physical examination) and synovitis in US and power Doppler are shown in Tables 3 and 4. According to these tables, the frequency distribution of tender joints and synovitis were not statistically different in physical examination, ultrasonography and power Doppler (P > 0.05).
Table 3.
Comparison of tender joint in physical exam and synovitis in ultrasonography*
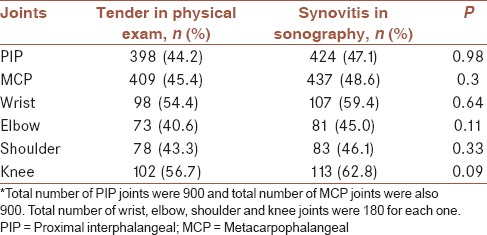
Table 4.
Comparison of tender joint in physical exam and positive results in power Doppler sonography
DISCUSSION
The overall objective of this study was to compare two methods of physical examination and ultrasound in joint involvement in patients with rheumatoid arthritis who were admitted to the outpatient clinic of Al-Zahra Hospital. In this study, ninety patients referred to the rheumatology clinic of Al-Zahra Hospital were evaluated by clinical examination and ultrasound and then the results were reviewed and analyzed.
In this study, the use of ultrasound was more powerful to find a joint effusion than clinical examination in large joints and ultrasound can detect more joint effusion. Of other items that were examined in this study was comparison of tenderness in the diagnosis of synovitis despite positive findings on ultrasound and power Doppler.
CONCLUSION
According to our study, physical examination findings are not different with ultrasonography and power Doppler for joints tenderness when physical exam and hyperemia in power doppler sonography were compared. These findings are consistent with previous studies by Naredo et al. which had reported similar findings.[5] In a study conducted by Filer et al., extended ultrasound joint evaluation significantly increased detection of joint involvement in all regions and outcome groups. Grayscale and power Doppler scanning of MCP joints, wrists, and metatarsophalangeal joints provide the optimum minimal ultrasound data to improve on clinical predictive models for RA.[11] In the study of Kane, ultrasonography is more sensitive than clinical examination in the detection of suprapatellar bursitis, knee effusion, and Baker's cyst in RA. PE underestimates knee inflammation in RA. This has implications for the use of PE as a component of standardized DAS-28 and in guiding knee joint aspiration.[12] Furthermore, Macin reported that power Doppler ultrasonography was reliable for assessing inflammatory activity in the MCP joints of RA patients, using dynamic MRI as the standard.[13]
Suggestions
According to the results of this study, ultrasound in the evaluation of joint effusion in patients with rheumatoid arthritis is more sensitive than clinical examination in large joints and also it is safe, affordable and available.
According to the study, the following is recommended for future research: Comparison of ultrasound and clinical examination in patients with rheumatoid arthritis that remained to be done in terms of clinical complete remission.
Comparison of ultrasound with MRI which is the most sensitive method.
Conducting a study to compare clinical examination and ultrasound to examine all joints.
Financial support and sponsorship
This study was supported by Isfahan University of Medical Sciences. This design was registered in research faculty of the medical school of Isfahan by code 394677.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Symmons D, Mathers C, Pfleger B. Global burden of disease. 2000. [Last accessed on 2015 Jun 14]. Available from: www.who.int/health info .
- 2.Firestein GS, Budd RC. Kelley's Text Book of Rheumatology. 9th. Philadelphia: Elsevier Sounders Pub; 2013. pp. 1059–137. [Google Scholar]
- 3.Xiao H, Liu M, Tan L, Liao X, Li Y, Gao J, et al. Value of ultrasonography for diagnosis of synovitis associated with rheumatoid arthritis. Int J Rheum Dis. 2014;17:767–75. doi: 10.1111/1756-185X.12390. [DOI] [PubMed] [Google Scholar]
- 4.Szkudlarek M, Klarlund M, Narvestad E, Court-Payen M, Strandberg C, Jensen KE, et al. Ultrasonography of the metacarpophalangeal and proximal interphalangeal joints in rheumatoid arthritis: A comparison with magnetic resonance imaging, conventional radiography and clinical examination. Arthritis Res Ther. 2006;8:R52. doi: 10.1186/ar1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naredo E, Bonilla G, Gamero F, Uson J, Carmona L, Laffon A. Assessment of inflammatory activity in rheumatoid arthritis: A comparative study of clinical evaluation with grey scale and power Doppler ultrasonography. Ann Rheum Dis. 2005;64:375–81. doi: 10.1136/ard.2004.023929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backhaus M, Balint PV, Benis S, Berner-Hammer H, David Bong J, Antonio Bouffard, et al. Essential Applications of Musculoskeletal Ultrasound In Rheumatology, Saunders. 2010:155–61. [Google Scholar]
- 7.Bounty N, Morel M, Flipo R, Demondion X, Ctten A. Early Rheumatoid arthritis: A review of MRI and sonographic findings. AJR. 2007;189:1502–9. doi: 10.2214/AJR.07.2548. [DOI] [PubMed] [Google Scholar]
- 8.Backhaus M, Burmester GR. Guide lines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60:641–9. doi: 10.1136/ard.60.7.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt WA. Ultrasound in rheumatology. Int J Rheum Dis. 2014;17:711–5. doi: 10.1111/1756-185X.12545. [DOI] [PubMed] [Google Scholar]
- 10.Chehrei A. 1st. Tehran: Tchehr Corp; 2005. Determining of Sample Size in Medical Studies; p. 39. [Google Scholar]
- 11.Filer A, de Pablo P, Allen G, Nightingale P, Jordan A, Jobanputra P, et al. Utility of ultrasound joint counts in the prediction of rheumatoid arthritis in patients with very early synovitis. Ann Rheum Dis. 2011;70:500–7. doi: 10.1136/ard.2010.131573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kane D, Balint PV, Sturrock RD. Ultrasonography is superior to clinical examination in the detection and localization of knee joint effusion in rheumatoid arthritis. J Rheumatol. 2003;30:966–71. [PubMed] [Google Scholar]
- 13.Szkudlarek M, Court-Payen M, Strandberg C, Klarlund M, Klausen T, Ostergaard M. Power Doppler ultrasonography for assessment of synovitis in the metacarpophalangeal joints of patients with rheumatoid arthritis: A comparison with dynamic magnetic resonance imaging. Arthritis Rheum. 2001;44:2018–23. doi: 10.1002/1529-0131(200109)44:9<2018::AID-ART350>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]


