Abstract
Nivolumab improves overall survival rates of patients with advanced or recurrent non‐small‐cell lung cancer (NSCLC). Among immune‐related adverse events caused by nivolumab, interstitial lung disease (ILD) is a clinically serious and potentially life‐threatening toxicity, for which appropriate treatment is needed immediately. However, ILD is sometimes difficult to distinguish from invasive lung adenocarcinoma using only computed tomography (CT) findings. A 71‐year‐old man was diagnosed with advanced lung adenocarcinoma. The patient developed dyspnoea after eight cycles of nivolumab, when chest CT indicated ILD classified with a cryptogenic organizing pneumonia (COP) pattern. Although immunosuppressive therapies improved the CT findings temporarily, dyspnoea was re‐exacerbated 2 months later. The CT findings helped in making the diagnosis of a combination of ILD and invasive lung cancer, confirmed by a transbronchial lung biopsy. In conclusion, nivolumab‐related ILD and cancer invasion may concur and aggressive biopsy should be considered if nivolumab‐related ILD is refractory to immunosuppressive therapy.
Keywords: chemotherapy, immunotherapy, interstitial lung disease, nivolumab, non‐small cell lung cancer
Introduction
Nivolumab, a fully human immunoglobulin G4 (IgG4) programmed cell death‐1 (PD‐1) immune‐checkpoint‐inhibitor (ICI) antibody, improves overall survival rates of patients with advanced or recurrent non‐squamous non‐small‐cell lung cancer (NSCLC) that progresses during chemotherapy 1. ICIs are associated with unique toxicities, termed immune‐related adverse events (irAEs) 2. Among the irAEs, interstitial lung disease (ILD) is a clinically serious and potentially life‐threatening toxicity, for which appropriate treatment is needed immediately. However, ILD is sometimes difficult to distinguish from invasive lung adenocarcinoma by only computed tomography (CT) findings 3. In this study, we report a case of lung adenocarcinoma that developed refractory ILD during treatment with nivolumab, diagnosed as a combination of ILD and invasive lung cancer.
Case Report
A 71‐year‐old man presented with a persistent cough for 3 months. Chest CT revealed a 25‐mm‐diameter mass in the right middle lobe of the lung and thickened interlobular septa around the mass. Transbronchial biopsy confirmed a diagnosis of lung adenocarcinoma harbouring minor mutations in epidermal growth factor receptors (EGFRs). Positron emission tomography–CT indicated metastases in mediastinal lymph nodes and malignant lymphangitis, confirming the diagnosis of stage IV (cT4N2M1a) based on the tumour‐node‐metastasis (TNM) staging system.
The patient underwent six cycles of carboplatin with a target area under the curve (AUC) of 5 mg/mL/min, 500 mg/m2 of pemetrexed on day 1 every 4 weeks, and folic acid and vitamin B12 supplements, followed by maintenance chemotherapy with 500 mg/m2 of pemetrexed. A chest CT acquired after six cycles of pemetrexed demonstrated tumour progression, but no findings that suggested ILD in the left upper lobe of the lung (Fig. 1A). Nivolumab, at a dose of 3 mg/kg, was administrated on day 1 every 2 weeks. After eight cycles of nivolumab, a chest CT showed the progression of primary tumour and new multifocal CT findings such as ground‐grass nodules (GGNs) and consolidation in all the lobes of the lung, causing cough and dyspnoea (Fig. 1B).
Figure 1.
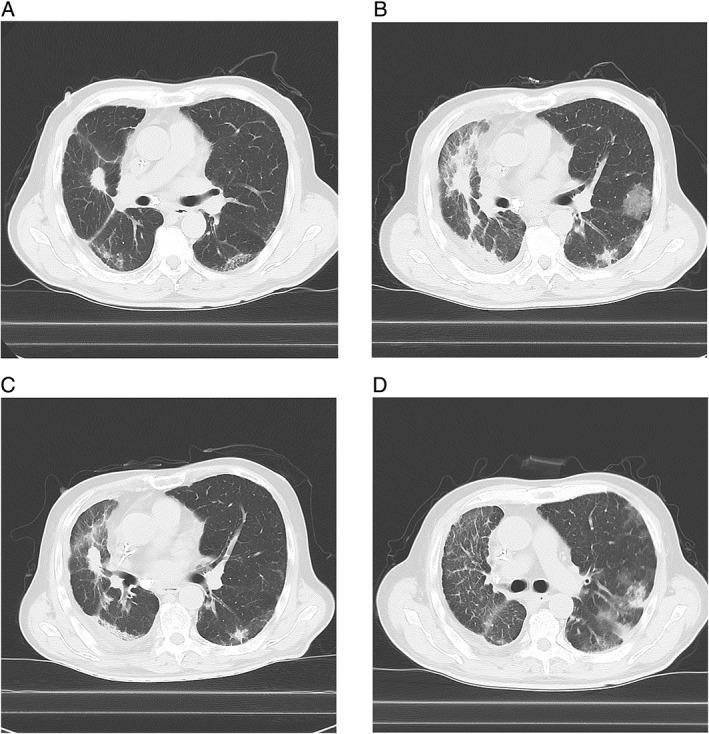
Chest computed tomography (CT) scans of the left upper lobe of the lung before and after initiating nivolumab. (A) No finding suggesting interstitial lung disease (ILD) before administration of nivolumab. (B) Appearance of the combination of ground‐grass nodule (GGN) and consolidation after eight cycles of nivolumab. (C) Improvement in CT findings after immunosuppressive treatment for 1 month; the GGN disappeared but the consolidation remained. (D) Re‐exacerbation of the combination of GGN and consolidation after tapering the dose of prednisolone to 30 mg daily.
Prednisolone at a dose of 60 mg (equivalent of 1 mg/kg) daily was initiated as treatment for nivolumab‐related pneumonitis, which did not improve the patient's dyspnoea. Cyclosporine A at a dose of 50 mg was added twice daily 2 weeks later, which improved the patient's dyspnoea and the CT findings (Fig. 1C). Disappearance of consolidation around the primary tumour indicated that the size of primary tumour had not changed after nivolumab therapy.
The dose of prednisolone was tapered to 30 mg daily after 2 months; however, dyspnoea worsened again (Fig. 1D). The patient was treated with injections of methylprednisolone at a dose of 1 g daily for 3 days and infliximab at a dose of 5 mg/kg. Along with the treatment, a transbronchial lung biopsy was performed at the left upper lobe of the lung. The tissue samples demonstrated atypical cells in the alveoli and sub‐epithelial tissue of the bronchus and fibrosis in the alveolar wall. The atypical cells were positive for thyroid transcription factor‐1 and napsin A, and negative for p63, which suggested the combination of ILD and invasive lung cancer (Fig. 2A–C). The patient's general condition worsened due to the progression of lung cancer and died 1 month after bronchoscopy.
Figure 2.

Histological images of tissue samples obtained by transbronchial lung biopsy. Atypical cells in sub‐epithelial tissue of bronchus and fibrosis in the alveolar wall (haematoxylin and eosin staining, 200×) (A). Immunohistochemical staining showing positivity for thyroid transcription factor‐1 (TTF‐1) (B) and napsin A (C).
Discussion
We reported a case of NSCLC in a patient who developed a combination of invasive lung cancer and nivolumab‐related ILD diagnosed by a transbronchial lung biopsy. Different distribution between the consolidation and GGNs suggested that the consolidation and GGNs arose from different aetiologies. For the following two reasons, however, we diagnosed both the consolidation and GGNs with nivolumab‐induced ILD based on the clinical course of the patient. First, disappearance of the CT findings after immunosuppressive therapies reduced the possibility of detecting infection and lymphangitis. Second, non‐shrinkage of the primary tumour after nivolumab reduced the possibility of the effect of nivolumab. Multifocal GGNs and consolidation could be classified as having a cryptogenic organizing pneumonia (COP) pattern, based on the American Thoracic Society/European Respiratory Society international multidisciplinary classifications of interstitial pneumonias. The COP pattern with multifocal distribution was reported to represent most of the CT findings in ICI‐related ILD patients 4. Furthermore, typical cases of ICI‐related ILD were sensitive to immunosuppressive treatments 4. In the present case, the lung disease newly developed during the treatment with nivolumab was typical for nivolumab‐related ILD, but was refractory to the treatment with corticosteroids and infliximab, unlike typical nivolumab‐related ILD.
This atypical outcome caused doubt in the diagnosis of ILD. Then, metastasis of lung cancer or invasion of lymphocytes into metastatic tumours was considered in the differential diagnosis of the lung disease. The CT findings in lung adenocarcinoma patients sometimes resembles that of interstitial pneumonia 3, especially that of the COP pattern. Among 564 patients with resected lung adenocarcinoma, CT findings of 13 patients were reported to represent organizing pneumonia (OP) 5. In cases of lung cancer mimicking the COP pattern, aggressive biopsy would be recommended to confirm the diagnosis. In the present case, transbronchial lung biopsy confirmed the diagnosis of the coexistence of pneumonitis and cancer invasion, which complicated the treatment of the lung disease. Immunosuppressive treatments might have suppressed the lymphocyte invasion induced by nivolumab.
In conclusion, ICI‐related pneumonitis is mainly represented by the COP pattern, which is sometimes difficult to distinguish from lung adenocarcinoma mimicking OP. Moreover, nivolumab‐related ILD and cancer invasion may concur. To offer the most appropriate treatment and to avoid losing the next opportunity for chemotherapy, aggressive biopsy should be considered in such situations.
Acknowledgments
This study was supported in part by a grant from the National Hospital Organization's fiduciary funds (for English editing and manuscript submission). I would like to thank Editage (http://www.editage.com) for their help with English language editing.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Kanai, O. , Nakatani, K. , Fujita, K. , Okamura, M. and Mio, T. (2017) Concurrence of nivolumab‐induced interstitial lung disease and cancer invasion. Respirology Case Reports, 5 (6), e00257. doi: 10.1002/rcr2.257.
Associate Editor: Kazuhisa Takahashi
References
- 1. Borghaei H, Paz‐Ares L, Horn L, et al. 2015. Nivolumab versus docetaxel in advanced nonsquamous non‐small‐cell lung cancer. N. Engl. J. Med. 373:1627–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Michot JM, Bigenwald C, Champiat S, et al. 2016. Immune‐related adverse events with immune checkpoint blockade: a comprehensive review. Eur. J. Cancer 54:139–148. [DOI] [PubMed] [Google Scholar]
- 3. Fujita K, Shim J, Nakatani K, et al. 2015. Patient with lung adenocarcinoma manifesting as an unusual migratory pulmonary infiltration. BMJ Case Rep. 10.1136/bcr-2015-211771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nishino M, Chambers ES, Chong CR, et al. 2016. Anti‐PD‐1 inhibitor‐related pneumonitis in non‐small cell lung cancer. Cancer Immunol. Res. 4:289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ichikawa T, Hattori A, Suzuki K, et al. 2016. Clinicopathological characteristics of lung cancer mimicking organizing pneumonia on computed tomography: a novel radiological entity of pulmonary malignancy. Jpn. J. Clin. Oncol. 46:681–686. [DOI] [PubMed] [Google Scholar]


