Abstract
OBJECTIVE:
To determine the association between enrollment in patient-centered medical homes (PCMHs) and the receipt of preventive services among adolescents and young adults.
METHODS:
Retrospective cohort study including patients of Hennepin County aged 10 to 24 who had face-to-face or telephone encounters with health care providers between 2010 and 2014 at clinics with PCMHs at the Hennepin County Medical Center, Minnesota. Exposure was enrollment in PCMHs. Outcomes were receipt of (1) preventive visits; (2) prescriptions for influenza, meningococcal, and human papillomavirus vaccinations; (3) screening for sexually transmitted infections; (4) prescription of any contraceptive and long-acting reversible contraceptives; and (5) cervical cancer screening. Generalized mixed effect models in a propensity-score-matched sample were used for data analysis.
RESULTS:
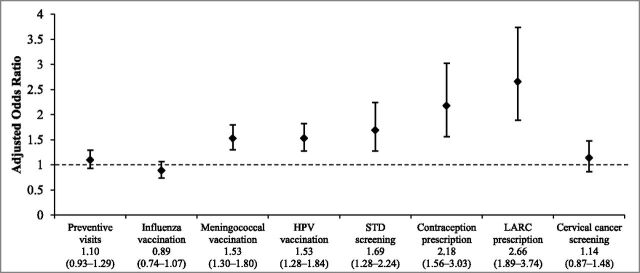
Overall, 21 704 patients were included. Most patients were female, US-born, Hispanic/Latino, with an average age of 20.8 years. Patients enrolled in PCMH (n = 729) were more likely to be Latino, students, and have health insurance (P < .001). Adjusted odds ratios (99% confidence intervals) comparing the receipt of preventive services of patients enrolled in PCMHs to youth who did not receive these services were as follows: (1) preventive visits 1.10 (0.93–1.29); (2) influenza 0.89 (0.74–1.07), meningococcal 1.53 (1.30–1.80), and human papillomavirus vaccinations 1.53 (1.28–1.84); (3) screening for sexually transmitted infections 1.69 (1.28–2.24); (4) prescription of any type of contraception 2.18 (1.56–3.03) and long-acting reversible contraceptives 2.66 (1.89–3.74); and (5) cervical cancer screening 1.14 (0.87–1.48).
CONCLUSIONS:
Overall, patients enrolled in PCMHs had higher odds of receiving multiple preventive services.
What’s Known on This Subject:
Not all adolescents and young adults receive recommended preventive services. Patient-centered medical homes aim to improve outcomes and experience and reduce costs. Adolescents and young adults receiving these services have achieved higher rates of preventive visits and immunizations.
What This Study Adds:
Adolescent and young adults enrolled in patient-centered medical homes are more likely to receive multiple preventive services including immunizations, screening for sexually transmitted infections, and contraception. Young adult, foreign-born, nonstudent, and insured patients benefited most consistently from these services.
One in 5 people in the United States is an adolescent or young adult.1 Behavioral patterns established in these years contribute to youths’ current and future health status.2 Because most adolescent morbidity is preventable, delivering preventive services is critical.
As summarized by Ozer and collaborators,3 high-quality preventive care for adolescents and young adults should encompass multiple areas, including physical growth and development, emotional and relational well-being, social and academic competence, sexuality and reproductive health, substance use and risk reduction, age-appropriate immunizations, and strategies to minimize preventable injuries. However, only 38% to 81% of adolescents, and even fewer young adults, received a preventive checkup in the previous 12 months.4,5 In addition, male, ethnic minority, low-income, and uninsured youth have lower rates of preventive services.4–14
The patient-centered medical home (PCMH), one of the most widespread approaches to health care delivery transformation, emphasizes improved access and continuity of care via primary care provider (PCP)-led teams. This system of care was developed as a strategy to achieve the Triple Aim: improve outcomes and experience and reduce costs.15 So far, PCMHs have been shown to reduce acute care use and improve health care outcomes in children.16–18 However, there is little evidence of their effects on preventive care services for adolescents and young adults.19 The aim of this study is to evaluate the effect of PCMH enrollment on receipt of multiple preventive services among youth aged 10 to 24. In addition, we explored whether the effects of PCMH enrollment differed by sociodemographic characteristics.
Methods
Study Design
We conducted a retrospective cohort study with patients aged 10 to 24 who were enrolled in the ambulatory clinics of Hennepin County Medical Center (HCMC) that have PCMHs that deliver services for adolescents and young adults between 2010 and 2014 (n = 28 649). Patients were excluded if they did not have any face-to-face or telephone encounters with health care providers (n = 3291, 11.5%), were not residents of Hennepin County (n = 5097, 17.8%), and if they did not release their clinical information for research (n = 87, 0.3%). The study’s protocol was approved by the Human Subjects Research Office of the Minneapolis Medical Research Foundation.
Setting
HCMC is a safety net hospital and large ambulatory clinic system in Minnesota, providing care for low-income, uninsured, and vulnerable persons.20 In 2015, >500 000 patients were served, of whom >70 000 (25%) did not have health insurance. In addition, whereas 86% of the entire state of Minnesota and 76% of Hennepin County residents are white,21 HCMC patients are 35% white, 32% African American/black, 19% Hispanic/Latino, and 12% other racial/ethnic status.
Exposure
The independent variable was PCMH enrollment. In the HCMC network, there are 14 primary care clinics with certified Health Care Homes (HCHs).22 In Minnesota, HCHs are PCMHs that are certified by the state based on clinic eligibility and 5 standards: (1) access/communication, (2) patient tracking and registry functions, (3) care coordination, (4) care plans, and (5) performance reporting and quality improvement.23 These HCH certification standards are at a level 3 of the National Committee for Quality Assurance recognition status (Minnesota Department of Health, unpublished data, 2016), which is the highest PCMH certification status.
Of the 14 HCMC HCHs, 9 provide care for adolescents and/or young adults. Other HCHs do not have young patients in their panel. Although each of those HCHs serves a different patient population based on its target population or location (eg, 1 HCH is focused on Latinos, and others are located in areas with high concentrations of patients from specific ethnicities), all focus their services in providing comprehensive care management to patients with high risk of future medical use. Eligibility for HCH services is determined according to health service utilization, number and type of chronic conditions, and sociodemographic characteristics. Most HCHs serving youth have care coordinators who use standard intake, monitoring, and follow-up protocols. Not all HCHs have the same resources (eg, some have a community health worker, social worker, nurse coordinator, school navigator, or parent educator) or practice the same intensity of care (eg, 1 HCH works with a single PCP, and other HCHs work with multiple PCPs; some HCHs have biweekly or monthly panel management meetings, but others do not have this practice). One HCH is focused on positive youth development and delivers adolescent-friendly services,24 and another HCH has implemented certain components of adolescent-friendly care. Patients were considered exposed to the PCMH services if they were enrolled in any of the HCHs serving adolescents and/or young adults between 2010 and 2014.
Outcomes
Outcomes of this study are receiving (1) preventive health care visits; (2) influenza, meningococcal, and human papillomavirus (HPV) vaccinations; (3) screening for sexually transmitted infections (STIs); (4) prescription for any artificial contraceptive method and long-acting reversible contraceptives (LARCs); and (5) screening for cervical cancer if the patient was 21 years or older. Because STI screening is recommended for sexually active women under 25 and high-risk males,3 this outcome included both men and women because Hennepin County has the highest rate of Chlamydia trachomatis infections in Minnesota.25
Age (at January 1, 2015) was a continuous variable except when conducting stratified analyses, when it was categorized as 10 to 18 and 19 to 24. Race was patient-reported, and coded as Hispanic/Latino, non-Hispanic black (African American or African), and other (all patients from racial groups with <10% in any group). Other covariates included being US-born (versus foreign-born), primary language (English or other), marital status (single or other), employment (student or other including full- or part-time workers, self-employed, unemployed, and others), and health insurance status. Because few PCMH patients had private insurance, this variable was categorized into insured and uninsured.
Data Extraction
All data were extracted from patients’ electronic medical records. For each calendar year between January 1, 2010, and December 31, 2014, all eligible patients were classified as either receiving or not receiving each preventive service. Information on preventive visits was extracted by using the International Classification of Disease, Ninth Edition codes V.20.2 and V.70.0. Vaccinations included influenza (each year’s annual flu vaccine); meningococcal (meningococcal polysaccharide vaccine [MPSV4] or any quadrivalent meningococcal conjugate [MCV4, MenACWY-D, and –CRM]); and HPV (at least 1 dose of bi-, tetra-, or nano-valent HPV vaccines). Patients were counted as receiving STI screening if providers ordered a urine sample to detect C trachomatis. Youth were classified as receiving contraceptive medications if they were prescribed any type of hormonal contraceptive (pills, patches, rings, or implants) or intrauterine device. LARCs included implants and intrauterine devices. Patients aged 21 or older were classified as receiving cervical cancer screening if providers ordered a Papanicoulau test or HPV DNA amplification test.
Statistical Analysis
Proportions and means (±SD) were calculated to describe patients and the clinical services they received. Demographic characteristics of patients enrolled in PCMHs were compared with patients not enrolled in these programs by using χ2 and t tests for categorical and continuous outcomes, respectively.
The effects of PCMH enrollment status on the receipt of each preventive service were estimated by using mixed-effect logistic regressions. Two levels were considered in all analyses, where times of follow-up (2010–2014) were nested within patients. Unadjusted and adjusted odds ratios and 99% confidence intervals were calculated for each outcome. Unadjusted models did not include covariates, and adjusted models used propensity score matching to adjust for potential selection bias due to different probabilities of enrollment in PCMHs. The propensity score was estimated after regressing PCMH enrollment status on all covariates.26 Propensity scores ranged between 0.002 and 0.794, and patients enrolled in PCMHs were matched to patients not receiving these services based on the propensity score within a 0.1 caliper. Analyses evaluating contraceptive prescriptions and cervical cancer screening were limited to female patients, with cervical cancer screening analysis further restricted to patients 21 years or older.
To explore whether the effect of PCMHs on preventive services differed by demographic characteristics, we also tested interaction terms between PCMH enrollment status and demographic characteristics 1 at a time, by using propensity score matched mixed-effect logistic regression models. For interactions with P values <.01, we conducted stratified (subgroup) analyses for the different categories of each variable (eg, full models run separately for male and female patients), estimating adjusted odds ratios and 99% confidence intervals for the effect of PCMH in each group.
To determine the robustness of findings, we also conducted 2 sets of sensitivity analyses: first by using regression adjustment and the second by using 1:1 matching on all demographic characteristics. All analyses were conducted using Stata 14 (StataCorp, College Station, TX), and resulting P values <.01 were considered statistically significant.
Results
Patients
A total of 21 704 HCMC patients aged 10 to 24 were included in this study. Of them, 729 were enrolled in the 9 PCMHs serving adolescents and young adults at HCMC network (3.4%). Table 1 summarizes demographic characteristics of patients according to PCMH enrollment status. Most patients were female (55.7%), US born (68.8%), Latino (42.9%) or African American (32.4%), with an average age of 20.8 years and with public (47.6%) or no health insurance (41.8%). We observed demographic heterogeneity in patients enrolled in the different PCMHs according to age, gender, race/ethnicity, employment, and health insurance status. On average, PCMH patients were younger, more likely to be Latino or African American, and more likely to have public health insurance, compared with non-PCMH patients. Propensity score matching allowed successful balance between groups (Supplemental Table 4).
TABLE 1.
Sociodemographic Characteristics of Patients Enrolled and Not Enrolled in PCMHs
| Enrolled in PCMHs (n = 729) | Not Enrolled in PCMHs (n = 20 975) | P | |
|---|---|---|---|
| Gender, female | 434 (59.5) | 11 658 (55.6) | .035 |
| Age, y, mean (SD) | 19.0 (5.0) | 20.8 (5.2) | <.001 |
| Race | <.001 | ||
| Hispanic/Latino | 467 (64.1) | 8862 (42.3) | |
| Non-Hispanic black | 189 (25.9) | 6841 (32.6) | |
| Non-Hispanic white | 29 (4.0) | 3185 (15.2) | |
| Other | 44 (6.0) | 2087 (10.0) | |
| Country of birth, US | 471 (64.6) | 14 463 (68.8) | .108 |
| Primary language, English | 377 (51.7) | 14 381 (68.6) | <.001 |
| Marital status, single | 695 (95.3) | 19 265 (91.9) | .001 |
| Employment status, student | 405 (55.6) | 9741 (46.4) | <.001 |
| Health insurance status, insured | <.001 | ||
| Public insurance | 422 (57.9) | 9904 (47.2) | |
| Private insurance | 25 (3.4) | 2274 (10.8) | |
| No insurance | 282 (38.7) | 8797 (41.9) |
Values are n (%), unless otherwise noted.
Effect of PCMH Status on Receipt of Preventive Services
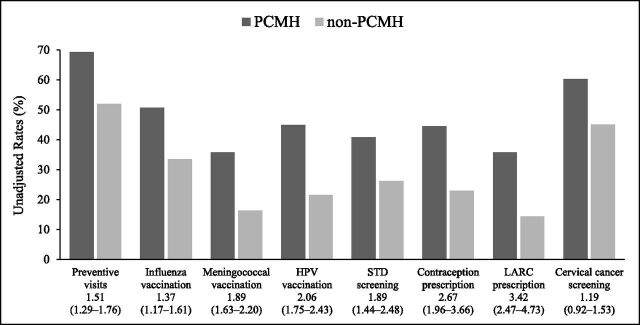
Overall, youth patients enrolled in PCMHs were more likely to receive most preventive services compared with patients not enrolled in these programs (Fig 1). As we observed heterogeneity in PCMH patient composition, we also noticed variability in the outcomes achieved according to the PCMH in which patients were enrolled. After controlling for demographic differences between groups, the effect of PCMHs on most outcomes remained significant (Fig 2).
FIGURE 1.
Unadjusted rates, odds ratios, and 99% confidence intervals comparing the receipt of preventive services between 2010 and 2014 among patients enrolled and not enrolled in PCMHs. Analyses evaluating contraceptive prescriptions and cervical cancer screening were conducted only among female patients. The analysis of cervical cancer screening was also restricted to patients 21 years or older.
FIGURE 2.
Adjusted odds ratios and 99% confidence intervals comparing the receipt of preventive services among patients enrolled and not enrolled in PCMHs. Analyses evaluating contraceptive prescriptions and cervical cancer screening were conducted only among female patients. The analysis of cervical cancer screening was also restricted to patients aged 21 years or older. Mixed effects logistic regression models used propensity score matching.
Results by Patient Demographics
Table 2 presents adjusted odd ratios of the effect of PCMHs on outcomes in demographic subgroup analyses, shown for all combinations that had significant interaction terms in overall models. Gender only had a significant interaction for meningococcal vaccinations. Among females, PCMH enrollees were more likely to receive meningococcal vaccinations than non-PCMH enrollees, but PCMH had no effects among males. Among adolescents, PCMH enrollees had lower odds of preventive visits and flu shots but higher odds STI screening and contraception prescriptions. For young adults, PCMH enrollment (versus nonenrollment) meant higher odds of almost all preventive services. Hispanic/Latino PCMH enrollees had higher odds of preventive visits, but lower odds of flu shots, versus non-PCMH patients; however, PCMH showed no significant effects for other racial/ethnic groups. Among those who were foreign born, PCMH enrollees had higher odds than non-PCMH patients for receiving most services, but PCMH had no significant effects for US-born patients. Among students, PCMH enrollees had lower odds of preventive visits and immunizations, but among nonstudents, PCMH enrollees were more likely to receive preventive visits and flu, meningococcal, and HPV vaccinations. Finally, insured patients in PCMHs had higher odds of most preventive services, whereas PCMH benefits for uninsured patients were limited to meningococcal vaccination and contraception and LARC prescriptions. There were no significant interactions between PCMH enrollment and sociodemographics on cervical cancer screening.
TABLE 2.
Stratified Adjusted Odd Ratios (99% CI) of PCMH Effects on Outcomes That Had Statistically Significant Interactions
| Preventive Visits | Influenza Vaccination | Meningococcal Vaccination | HPV Vaccination | STI Screening | Contraception Prescription | LARC Prescription | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | — | — | 1.00 (0.75–1.33) | — | — | — | — |
| Female | — | — | 1.98 (1.62–2.42)a | — | — | — | — |
| Age category, y | |||||||
| 10–18 | 0.63 (0.51–0.79)a | 0.60 (0.47–0.78)a | 1.00 (0.83–1.22) | 1.08 (0.90–1.32) | 3.78 (2.05–6.96)a | 5.16 (2.65–10.06)a | 5.96 (2.71–13.07)a |
| 19–24 | 1.88 (1.53–2.31)a | 1.37 (1.08–1.73)a | 8.63 (6.35–11.74)a | 3.82 (2.79–5.25)a | 1.25 (0.95–1.64) | 1.53 (1.07–2.17)a | 1.95 (1.35–2.81)a |
| Race | |||||||
| Hispanic/Latino | 1.24 (1.03–1.49)a | 0.72 (0.60–0.87)a | — | — | — | — | — |
| Non-Hispanic black | 0.72 (0.50–1.02) | 1.51 (0.99–2.29) | — | — | — | — | — |
| Other | 0.71 (0.42–1.20) | 1.41 (0.75–2.64) | — | — | — | — | — |
| Country of birth | |||||||
| United States | 0.84 (0.67–1.04) | — | 1.16 (0.93–1.45) | 1.12 (0.89–1.42) | 1.44 (0.98–2.14) | 1.24 (0.75–2.07) | 1.69 (0.92–3.09) |
| Other | 1.80 (1.43–2.27)a | — | 2.77 (2.18–3.53)a | 3.09 (2.27–4.19)a | 1.72 (1.20–2.47)a | 2.89 (1.90–4.40)a | 3.06 (2.08–4.49)a |
| Employment status | |||||||
| Student | 0.65 (0.52–0.82)a | 0.59 (0.45–0.76)a | 1.02 (0.84–1.24) | 1.06 (0.87–1.30) | — | — | — |
| Other | 1.89 (1.54–2.38)a | 1.43 (1.13–1.83)a | 7.52 (5.60–10.11)a | 3.80 (2.76–5.24)a | — | — | — |
| Health insurance status | |||||||
| Insured | 1.86 (1.49–2.33)a | — | 2.33 (1.77–3.07)a | 2.71 (1.94–3.78)a | 2.40 (1.77–3.27)a | 2.81 (1.74–4.54)a | 3.17 (1.93–5.20)a |
| Uninsured | 0.86 (0.70–1.07) | — | 1.29 (1.05–1.57)a | 1.23 (0.99–1.54) | 1.26 (0.95–1.66) | 1.67 (1.07–2.59)a | 2.09 (1.32–3.33)a |
Analyses evaluating contraceptive prescriptions were conducted only among female patients. Mixed-effects logistic regression models used propensity score matching. Results are not reported for interactions that were not statistically significant.
Statistically significant comparing patients enrolled in PCMHs with patients not enrolled in these services within each strata.
Sensitivity Analyses
Results using propensity score matching, regression adjustment, and 1:1 matching were similar (Table 3). Propensity score matching tended to estimate more conservative effect estimates than the regression adjustment and 1:1 matching.
TABLE 3.
Adjusted Odds Ratios (99% Confidence Intervals) Comparing the Receipt of Preventive Services Among Patients Enrolled in PCMHs and Not Enrolled in These Programs Using Propensity Score Matching, Regression Adjustment, and 1:1 Matching on Patient Demographics
| Outcome | Propensity Score Matching | Regression Adjustmenta | 1:1 Matching |
|---|---|---|---|
| Preventive visits | 1.10 (0.93–1.29) | 1.28 (1.10–1.49) | 1.40 (0.80–2.44) |
| Influenza vaccinationb | 0.89 (0.74–1.07) | 1.11 (0.94–1.31) | 1.04 (0.54–2.00) |
| Meningococcal vaccinationb | 1.53 (1.30–1.80) | 1.74 (1.46–2.08) | 1.88 (1.08–3.28) |
| HPV vaccinationb | 1.53 (1.28–1.84) | 1.77 (1.49–2.10) | 2.54 (1.36–4.73) |
| STI screeningb | 1.69 (1.28–2.24) | 2.07 (1.66–2.56) | 2.30 (0.91–5.84) |
| Contraception prescriptionb | 2.18 (1.56–3.03) | 3.39 (2.50–4.61) | 5.00 (1.54–16.20) |
| LARC prescriptionb | 2.66 (1.89–3.74) | 3.96 (2.86–5.49) | 7.83 (2.15–28.51) |
| Cervical cancer screeningb | 1.14 (0.87–1.48) | 1.20 (0.93–1.56) | 0.69 (0.22–2.17) |
Analyses evaluating contraceptive prescriptions and cervical cancer screening were conducted only among female patients. The analysis of cervical cancer screening was also restricted to patients aged 21 y or older.
Mixed effect regression models were adjusted for patient’s gender, age, race, country of birth, primary language spoken at home, marital, employment, and health insurance status.
These items had consistent findings across analytical methods.
Discussion
In this study, we identified that patients enrolled in PCMHs had greater overall likelihood of receiving preventive care compared with adolescents and young adults not receiving these services. In addition, we found dissimilar effects according to the patient’s sociodemographics.
Our findings support the usefulness of PCMHs as a health care strategy to increase the receipt of multiple preventive services in a health system that provides care to adolescents and young adults at risk for preventive care disparities.4–14 Overall, patients enrolled in PCMHs were more likely to be Hispanic/Latino and speak a language other than English, compared with patients not receiving these services. This means HCMC is giving access to comprehensive health care management services to patients who have been less likely to enroll in PCMHs.19 An example of these efforts is the Aqui Para Ti (Here For You) HCH,24 which is focused on the healthy youth development of Latino patients and contributed a large proportion of PCMH patients to this study. Second, although the rates of preventive services in this population were lower than in previous studies,4–13 we observed that patients enrolled in PCMHs were more likely to receive preventive care after matching them on their likelihood of PCMH enrollment. Because vulnerable youth have greater mental, sexual, behavioral, and physical health risks,27,28 they have a greater need for preventive health services but also have lower chances of receiving them.4–14 PCMHs may offer particular benefit to underserved youth, even though getting access to this model of care remains a problem in this age group; only ∼3% of the adolescents and young adults receiving care at HCMC received PCMH services.
Our results from interactions and subgroup analyses indicate that some patients receive most benefit from PCMHs. Such findings suggest multiple explanations: first, young adults, foreign-born, nonstudents, and insured patients are most in need of services and derive the most direct benefit; second, youth in these groups respond most favorably with the delivery of health care provided in these settings; and third, PCMHs focused on specific populations are more effective than others (eg, HCH targeting healthy youth versus HCHs including patients with chronic conditions). In the first case, PCMHs are simply a response to particular needs. In the latter, certain patient groups either respond to or receive better experience or delivery of care in PCMHs. If PCMHs are serving some youth better than others, it is an area for further attention. Alternatively, if some groups respond better to a PCMH model of care or if differences in PCMH implementation relate to outcomes, then work is needed to identify the characteristics of effective health care teams and strategies that improve care delivery across sites, as the level of PCMH implementation has been associated with the receipt of preventive services in nonpediatric patients.29
Important limitations of the current study include differential levels of exposure, residual confounding, receiving services outside the HCMC network, including multiple comparisons, and not assessing the degree of adolescent-friendliness of HCMC clinics. First, although we identified the PCMH enrollment status of the included participants, we could not measure the length of time patients were exposed to the services of the different programs. These different lengths of exposure might underestimate the magnitude of the identified associations because patients with brief exposures were classified as being fully exposed, which might not have been accurate according to the length of membership in the PCMH.30 Second, although we estimated average treatment effects by using propensity score matching, which produce valid and more reliable effect estimates than other methods,26 we were not able to incorporate into the analysis measures of patient complexity,31,32 or other confounders such as level of education, income, or having special health care needs (eg, chronic conditions). In addition, during adolescence and young adulthood, marital, employment, and health insurance status change over time, and because we only had access to patients’ status on these variables at the time of data extraction, we could not consider them as time-varying covariates. We believe that the residual confounding might have made us overestimate the PCMH effects. Additional overestimation of PCMH effects could arise from differential measurement of the outcomes because patients might have received some of the preventive services outside the HCMC network (eg, influenza vaccinations), especially those patients who did not receive the PCMH services. Moreover, although patients could also have been nested within PCPs and specific primary care clinics,33 these 3- or 4-level models were not conducted because many of patients did not identify a PCP (n = 8355, 38.4%) or received care at multiple facilities of the HCMC (n = 8480, 39.1%). We think that effect overestimation might be counterbalanced with the potential underestimation of effects due to the lack of consideration of length of exposure and the use of 99% confidence intervals. Fourth, in this study we focused on 8 outcomes and reported ∼20 analyses for each of them (including main effects, interactions, and stratified analyses). This means that by chance, ∼8 of the statistically significant associations could have been wrong with an α of 0.05.34 To minimize this issue, we decided to use P < .01 as the marginal level for statistical significance and conducted sensitivity analyses that reported a pattern of consistent findings across multiple preventive services. Finally, we did not assess the degree that PCMHs or clinics offered adolescent-friendly care,35 which could have affected the study’s results. Future studies need to confirm our findings, especially the subgroup analyses.
This study presents a comprehensive evaluation of the benefits of PCMHs related to increasing the receipt of preventive services. These findings support the need to expand this model of care to benefit more low-income adolescents and young adults as a strategy to reduce health inequities. The Affordable Care Act has provided funding to increase access to PCMHs,36 which has increased receipt of preventive services.37 Although the $35.7 million investment to support implementation of this model of care is important, these funds will not reach everyone. Local, state, and federal policies need to fund the implementation of coordinated team-based services, especially at locations that serve low-income, minority, and uninsured patients, who are least likely to receive preventive and therapeutic care.4–14 In addition, these policies need to address the needs of those youth who are not covered by the Affordable Care Act, including undocumented immigrants with no access to care. Shifting part of the Emergency Medical Assistance Program to support preventive care among youth could support this goal. Although cost reductions are possible, they might be limited to more complex patients,38 and it remains to be seen whether reductions or cost offsets can be attained among adolescents and young adults.
Conclusions
Overall, youth enrolled in PCMHs had greater likelihood of receiving multiple preventive services compared with adolescents and young adults who were not enrolled in these programs. This finding highlights the value of this model of care at addressing not only the specific needs of patients but also improving their preventive care.
Supplementary Material
Acknowledgments
Diego Garcia-Huidobro had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank Kristen Godfrey Walters, HCMC’s Community Care Coordination Manager, for supporting this research project, and Mark A. Caldwell, Senior Research Analyst at the Minnesota Department of Health, and Kathleen Conboy, Senior Nurse Planner at the Minnesota Department of Health, for developing the crosswalk between National Committee for Quality Assurance PCMH and Minnesota’s HCH standards.
Glossary
- HCH
Health Care Home
- HCMC
Hennepin County Medical Center
- HPV
human papillomavirus
- LARC
long-acting reversible contraceptive
- PCMH
patient-centered medical home
- PCP
primary care provider
- STI
sexually transmitted infection
Footnotes
Dr Garcia-Huidobro conceptualized and designed the study, contributed to the acquisition of the data, analyzed and interpreted the findings, and drafted the initial manuscript; Dr Shippee supervised the data analyses, drafted parts of the manuscript, and critically reviewed and revised the manuscript; Dr Joseph-DiCaprio and Mrs O’Brien contributed to the interpretation of the findings and critically reviewed the manuscript; Dr Svetaz conceptualized and designed the study, contributed to the acquisition of the data and interpretation of the findings, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FUNDING: Research reported in this article was supported by the Eliminating Health Disparities Initiative of the Minnesota Department of Health (principal investigator: Svetaz) and by the National Research Service Award in Primary Medical Care (grant T32HP22239), Bureau of Health Professions, Health Resources and Services Administration, Department of Health and Human Services (principal investigator: Borowsky). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding institutions.
References
- 1.US Census Bureau . 2013 population estimates: annual estimates of the resident population for selected age groups by sex for the United States, states, counties, and Puerto Rico commonwealth and municipalities . Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed April 12, 2016
- 2.National Research Council and Institute of Medicine, Committee on Adolescent Health Care Services and Models of Care for Treatment, Prevention, and Healthy Development . In: Lawrence RS, Gootman JA, Sim LJ, eds. Adolescent Health Services: Missing Opportunities. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 3.Ozer EM, Urquhart JT, Brindis CD, Park MJ, Irwin CE Jr. Young adult preventive health care guidelines: there but can’t be found. Arch Pediatr Adolesc Med. 2012;166(3):240–247 [DOI] [PubMed] [Google Scholar]
- 4.Irwin CE Jr, Adams SH, Park MJ, Newacheck PW. Preventive care for adolescents: few get visits and fewer get services. Pediatrics. 2009;123(4):e565–e572 [DOI] [PubMed] [Google Scholar]
- 5.Adams SH, Park MJ, Irwin CE Jr. Adolescent and young adult preventive care: comparing national survey rates. Am J Prev Med. 2015;49(2):238–247 [DOI] [PubMed] [Google Scholar]
- 6.Hoover KW, Leichliter JS, Torrone EA, Loosier PS, Gift TL, Tao G; Centers for Disease Control and Prevention (CDC) . Chlamydia screening among females aged 15–21 years—multiple data sources, United States, 1999–2010. MMWR Suppl. 2014;63(2):80–88 [PubMed] [Google Scholar]
- 7.Ozer EM, Zahnd EG, Adams SH, et al. Are adolescents being screened for emotional distress in primary care? J Adolesc Health. 2009;44(6):520–527 [DOI] [PubMed] [Google Scholar]
- 8.Lau JS, Adams SH, Irwin CE Jr, Ozer EM. Receipt of preventive health services in young adults. J Adolesc Health. 2013;52(1):42–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–385 [DOI] [PubMed] [Google Scholar]
- 10.Rand CM, Auinger P, Klein JD, Weitzman M. Preventive counseling at adolescent ambulatory visits. J Adolesc Health. 2005;37(2):87–93 [DOI] [PubMed] [Google Scholar]
- 11.Ma J, Wang Y, Stafford RSUS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36(5):441. [DOI] [PubMed] [Google Scholar]
- 12.Jamal A, Dube SR, Babb SD, Malarcher AM; Centers for Disease Control and Prevention (CDC) . Tobacco use screening and cessation assistance during physician office visits among persons aged 11–21 years—National Ambulatory Medical Care Survey, United States, 2004–2010. MMWR Suppl. 2014;63(2):71–79 [PubMed] [Google Scholar]
- 13.George MG, Tong X, Wigington C, Gillespie C, Hong Y; Centers for Disease Control and Prevention (CDC) . Hypertension screening in children and adolescents—National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, and Medical Expenditure Panel Survey, United States, 2007–2010. MMWR Suppl. 2014;63(2):47–53 [PubMed] [Google Scholar]
- 14.Elster A, Jarosik J, VanGeest J, Fleming M. Racial and ethnic disparities in health care for adolescents: a systematic review of the literature. Arch Pediatr Adolesc Med. 2003;157(9):867–874 [DOI] [PubMed] [Google Scholar]
- 15.DeVries A, Li CH, Sridhar G, Hummel JR, Breidbart S, Barron JJ. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18(9):534–544 [PubMed] [Google Scholar]
- 16.Homer CJ, Klatka K, Romm D, et al. A review of the evidence for the medical home for children with special health care needs. Pediatrics. 2008;122(4):e922–e937 [DOI] [PubMed] [Google Scholar]
- 17.Raphael JL, Zhang Y, Liu H, Tapia CD, Giardino AP. Association of medical home care and disparities in emergency care utilization among children with special health care needs. Acad Pediatr. 2009;9(4):242–248 [DOI] [PubMed] [Google Scholar]
- 18.Cooley WC, McAllister JW, Sherrieb K, Kuhlthau K. Improved outcomes associated with medical home implementation in pediatric primary care. Pediatrics. 2009;124(1):358–364 [DOI] [PubMed] [Google Scholar]
- 19.Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604–611 [DOI] [PubMed] [Google Scholar]
- 20.Hennepin County Medical Center . About Hennepin County Medical Center. Available at: http://hcmc.org/aboutus/index.htm. Accessed April 12, 2016
- 21.US Census Bureau . State & county QuickFacts: Hennepin County, Minnesota. Available at: http://quickfacts.census.gov/qfd/states/27/27053.html. Accessed April 12, 2016
- 22.Minnesota Department of Health . Certified Healthcare Homes. Available at: http://www.health.state.mn.us/healthreform/homes/documents/certhch.pdf. Accessed April 12, 2016
- 23.Minnesota Department of Health . Health Care Homes: certification & recertification. Available at: http://www.health.state.mn.us/healthreform/homes/certification/certification/certassess.html. Accessed April 12, 2016
- 24.Svetaz MV, Garcia-Huidobro D, Hurtado GA, et al. Can a healthy youth development clinic serving Latino families be youth friendly and family oriented? A mixed-methods evaluation. Int J Adolesc Med Health. 2016;28(1):61–68 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention . Chlamydia—reported cases and rates of reported cases in counties and independent cities ranked by number of reported cases, United States, 2014. Available at: http://www.cdc.gov/STI/stats14/tables/9.htm. Accessed April 12, 2016
- 26.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8 pt 2):757–763 [DOI] [PubMed] [Google Scholar]
- 27.Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–1652 [DOI] [PubMed] [Google Scholar]
- 28.Markovitz AR, Alexander JA, Lantz PM, Paustian ML. Patient-centered medical home implementation and use of preventive services: the role of practice socioeconomic context. JAMA Intern Med. 2015;175(4):598–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dosemeci M, Wacholder S, Lubin JH. Does nondifferential misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol. 1990;132(4):746–748 [DOI] [PubMed] [Google Scholar]
- 30.Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012;65(10):1041–1051 [DOI] [PubMed] [Google Scholar]
- 31.Grembowski D, Schaefer J, Johnson KE, et al. ; AHRQ MCC Research Network . A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care. 2014;52(suppl 3):S7–S14 [DOI] [PubMed] [Google Scholar]
- 32.Killip S, Mahfoud Z, Pearce K. What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Ann Fam Med. 2004;2(3):204–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bender R, Lange S. Adjusting for multiple testing—when and how? J Clin Epidemiol. 2001;54(4):343–349 [DOI] [PubMed] [Google Scholar]
- 34.Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health. 2013;52(6):670–681 [DOI] [PubMed] [Google Scholar]
- 35.US Department of Health and Human Services . The Affordable Care Act supports patient-centered medical homes in health centers. 2016. Available at: http://www.hhs.gov/news/press/2014pres/08/20140826a.html. Accessed April 12, 2016
- 36.Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE Jr. Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatr. 2014;168(12):1101–1106 [DOI] [PubMed] [Google Scholar]
- 37.Tebb KP, Sedlander E, Bausch S, Brindis CD. Opportunities and challenges for adolescent health under the Affordable Care Act. Matern Child Health J. 2015;19(10):2089–2093 [DOI] [PubMed] [Google Scholar]
- 38.Flottemesch TJ, Anderson LH, Solberg LI, Fontaine P, Asche SE. Patient-centered medical home cost reductions limited to complex patients. Am J Manag Care. 2012;18(11):677–686 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.