Abstract
Problem Identification
Arab American women are an ethnic minority and immigrant population in the United States with unique and nuanced sociocultural factors that influence preventive health behaviors. The aims of this article are to evaluate and synthesize the existing evidence on cervical cancer screening behaviors, as well as determine factors that influence these behaviors, among Arab American women.
Literature Search
Extensive literature searches were performed using PubMed, CINAHL®, Scopus, Embase, and Cochrane databases; articles published through October 2015 were sought.
Data Evaluation
Of 17 articles, 14 explicitly identified Arab and/or Muslim women and cervical cancer screening in either the title or the abstract; the remaining three focused on cancer attitudes and behaviors in Arab Americans in general but measured cervical cancer screening. Eleven articles reported different aspects of one intervention. Because of methodologic heterogeneity, the current authors synthesized results narratively.
Synthesis
Key factors influencing cervical cancer screening were identified as the following: knowledge of cervical cancer screening and prevention; attitudes and beliefs; healthcare setting; education, marital status, income, and social support; and immigration and acculturation.
Conclusions
Cervical cancer screening rates among Arab American women are comparable to other ethnic minorities and lower than non-Hispanic White women. Findings are inconsistent regarding factors influencing cervical cancer screening behaviors in this underrepresented group.
Implications for Research
Significant need exists for more research to better understand cervical cancer prevention behaviors in this group to inform culturally relevant interventions. Healthcare providers play a crucial role in increasing cervical cancer screening awareness and recommendations for Arab American women.
Keywords: Arab American women, cervical cancer screening, Pap test, integrative review
Cervical cancer, the only cancer that is almost entirely preventable or curable if detected early, affects women, mainly those aged 30–50 years, in their most productive years (Moyer, 2012). In the United States, rates for new cervical cancer cases have fallen by about 1% each year during the past 10 years (Howlader et al., 2015). However, death rates (2.3 per 100,000) have not changed significantly from 2002–2012, and racial and ethnic minorities experience disproportionately greater mortality (4 per 100,000 for Black women; 3.5 per 100,000 for American Indian or Alaska Native women; 2.7 per 100,000 for Hispanic women) (Howlader et al., 2015). In addition, cervical cancer survivors have reported poor quality of life because of side effects related to the disease and its treatment (including sexual, urinary, and psychological effects); many have also experienced pregnancy complications (Frederiksen, Njor, Lynge, & Rebolj, 2015; Kyrgiou et al., 2006; Pfaendler, Wenzel, Mechanic, & Penner, 2015; Vermeer, Bakker, Kenter, Stiggelbout, & ter Kuile, 2015; White, 2015).
Advances in cervical cancer screening (regular Papanicolaou [Pap] and human papillomavirus [HPV] DNA testing) have led to significant decreases in cervical cancer rates compared to other types of cancer. Strong evidence supports the benefits of early detection in substantially reducing cervical cancer incidence and mortality (Katki et al., 2011; Markowitz et al., 2013; Moscicki, 2008; Paavonen et al., 2009; Vesco et al., 2011). Despite the effectiveness of these screening strategies, significant racial and ethnic disparities in cervical cancer screening and detection still exist. These disparities are related to multiple intersecting factors—such as race, ethnicity, culture, socioeconomic and immigration status, religion, and nativity (country of citizenship at birth)—that may influence an individual’s ability to receive preventive care (Glick, Clarke, Blanchard, & Whitaker, 2012; Johnson, Mues, Mayne, & Kiblawi, 2008; Pierce Campbell, Menezes, Paskett, & Giuliano, 2012; Seeff & McKenna, 2003; Swan et al., 2010). This integrative review focuses on Arab American women, whose highest reported rate of cervical cancer screening (87%) falls below the Healthy People 2020 target of 93% (Dallo & Kindratt, 2015).
Arab Americans are a growing ethnic minority in the United States, with a growth rate of more than 72% from 2000–2010; an estimated 3.5 million individuals can trace their roots to one of the 22 Arab countries (Arab American Institute, n.d.). Arab Americans’ health and health behaviors are understudied, in part because this population is classified as White by the U.S. government. This categorization not only renders them invisible as an ethnic minority (Ajrouch & Jamal, 2007; Naber, 2000), but also leads to a lack of research being conducted with this population. Initially, Arab immigrants actively pursued the White racial classification to easily assimilate into the mainstream; however, this classification also imposed an invisibility that subsequently had a significant impact on the lives of Arab Americans (Jamal & Naber, 2008). The events of and after September 11, 2001, increased visibility of Arabs in the United States, reinforced stereotypes, and amplified discrimination (Jamal & Naber, 2008) and health disparities in this ethnic minority group (El-Sayed, Tracy, Scarborough, & Galea, 2011; Inhorn & Fakih, 2006). Arab American women are vulnerable in terms of health behaviors because they are situated at the intersection of race, ethnicity, culture, socioeconomic and immigration status, religion, and nativity. Their invisibility within the White racial category deters the explication of how these factors relate to their health behaviors. Unless research studies specifically target Arab American women, no data are available regarding their health behaviors. A systematic review found only 34 articles addressing health and health behaviors among Arab Americans in the United States (El-Sayed & Galea, 2009). This paucity of research underscores the need for additional investigations, particularly given the increased incidence of discrimination and poor mental and physical health outcomes among Arab American women (Abu-Ras & Abu-Bader, 2008, 2009; Hassouneh & Kulwicki, 2007).
Despite some scholarly work that has become available in the past two decades about Arab Americans, a significant lack of knowledge exists about preventive health behaviors (e.g., cervical cancer screening) in this population. Therefore, the purpose of this integrative review is to evaluate and synthesize the existing evidence on cervical cancer screening behaviors and factors that influence these behaviors among Arab American women. Ultimately, this knowledge can be used to inform interventions to promote cervical cancer screening.
Literature Search
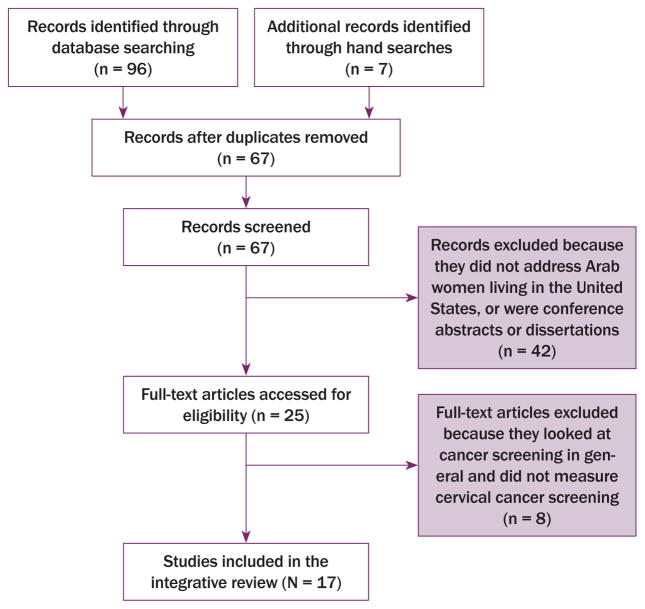
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline was followed in performing this integrative review (Liberati et al., 2009). PubMed, CINAHL®, Scopus, Embase, and Cochrane databases were used to search for relevant articles published through October 2015. The search terms Arab American women, Arab women, or Arab were used in combination with cervical cancer screening, cervical cancer, cancer screening, Pap smear, Pap test, Papanicolaou test, HPV, or human papillomavirus. One hundred and three articles were identified from the database and ancestry searches (search of references in relevant articles). After duplicates (full duplication) were removed, 67 article abstracts were screened. Inclusion criteria were as follows: (a) included Arab and/or Arab American women, (b) conducted in the United States, (c) measured one or more types of cervical cancer screening as a variable, and (d) used the English language. Conference abstracts and dissertations were excluded. Two of the current authors independently reviewed the articles to determine relevance for inclusion. All study designs were examined, including qualitative, quantitative, mixed methods, secondary data analyses, and intervention development. The term Arab American women is used in this article as an inclusive term to refer to Arab women who do not identity as Arab American for various reasons (e.g., personal identity or preference, citizenship) but are living in the United States and to Arab American women who identify as such. Therefore, it refers to both Arab and Arab American women.
Data Evaluation
Integrative reviews are comprehensive and allow for the inclusion of a wide range of publications that can differ in purpose, design, and sample, among other factors. Although inclusion of multiple methodologic approaches and designs in an integrative review can complicate the analysis, heterogeneity of the designs and sampling frame can increase the depth and breadth of the conclusions (Whittemore, 2005). Because of the methodologic heterogeneity, the authors synthesized the results narratively and did not perform a meta-analysis.
A rating system was used to score the findings in addressing the aims of the research. The rating system employed, a two-point scale that assessed the relevance of data (1 for low and 2 for high), followed the system suggested by Whittemore and Knafl (2005) and assisted the authors in analyzing the findings. Studies that scored low were not excluded, but they contributed less to the analytic process and the results (Whittemore & Knafl, 2005). Two of the current authors independently rated the articles for data relevance; scoring discrepancies were discussed until agreement was reached. Nine articles scored high on data relevance, and eight scored low. Articles also scored low when the overall sample included Arab American women, but a separate analysis for the subsample of Arab American women was not provided. One example is a study that investigated Muslim women in the United States (Padela, Peek, Johnson-Agbakwu, Hosseinian, & Curlin, 2014) but did not provide separate findings on Arab American Muslim women. Sixteen studies were evaluated as level III for strength of evidence based on the Johns Hopkins Nursing Evidence-Based Practice Rating Scale (New-house, Dearholt, Poe, Pugh, & White, 2005), with one study evaluated as level I (Gauss, Mabiso, & Williams, 2013). Because of the heterogeneity of the studies used in this integrative review, the two aforementioned approaches were used to evaluate the strength and relevance of data (Whittemore & Knafl, 2005).
Data Synthesis
General Study Characteristics
The authors’ search resulted in the identification of 17 relevant articles that met the inclusion criteria. Figure 1 is a flowchart reporting the search and screening results. Of the 17 studies, 14 explicitly identified Arab and/or Muslim women and cervical cancer screening in either the title or abstract; the remaining three described cancer attitudes and behaviors in Arab Americans in general and had cervical cancer screening as a measured variable. The authors did not find any studies investigating HPV infection and vaccination among Arab American women. Eleven articles reported on different aspects of one intervention, the Kin KeeperSM Cancer Prevention Intervention, which was developed and implemented among Black, Latina, and Arab women in Michigan (Detroit and Dearborn) from 2009–2015. Studies were also conducted in Chicago, New York, the San Francisco Bay Area, and a community in southwestern Pennsylvania, whereas two were secondary data analyses using the National Health Interview Survey (NHIS) and Michigan Special Cancer Behavioral Risk Factor Survey (SCBRFS). Methodologic approaches were varied, consisting of three qualitative designs (interviews and focus groups); 11 quantitative designs (cross-sectional; randomized, controlled trials; longitudinal; and secondary data analysis); and three multi-method approaches to describe the development and evaluation of an intervention and the psychometric testing of a cervical cancer literacy tool. The location, purpose, participants, design, findings, limitations, and data relevance score of included studies are summarized in Table 1.
FIGURE 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Flow Diagram of Articles Considered for Inclusion
TABLE 1.
Summary of Studies Included in the Integrative Review (N = 17)
| Study (Location) | Purpose, Participants, and Design | Findings | Limitations |
|---|---|---|---|
| Qualitative studies | |||
| Matin & LeBaron, 2004a (San Francisco Bay Area) |
|
|
The target population was Muslim women (Indian, Afghan, Pakistani, Palestinian, Egyptian, or Yemeni immigrants), with few participants of Arab origin. Results were not reported separately for Arab women, and the sample size was small. |
| Shah et al., 2008a (New York) |
|
|
Cervical cancer screening was not the main outcome of the study, and the sample size was small. All women identified as Muslim. |
| Quantitative studies | |||
| Dallo & Kindratt, 2015b (United States) |
|
|
Secondary data analysis occurred, and the sample size of Arab Americans compared to non-Arab Americans was small. Cervical cancer screening was not the main out-come of the study. |
| Darwish-Yassine & Wing, 2005a (Michigan) |
|
|
Cervical cancer screening was not the main outcome of the study, and sample size was not provided for Arab American women (only percentages). |
| Padela et al., 2014a (Chicago) |
|
|
The target population was Muslim women, with a small sample of Arabs. Results were not reported separately by ethnicity and for Arab women. |
| Salman, 2012b (southwestern Pennsylvania) |
|
|
The sample size was small, and the target population was Arab Muslim women recruited from a community in southwestern Pennsylvania. Non-English–speaking women were excluded. |
| Kin KeeperSM Cancer Prevention Intervention studies (qualitative) | |||
| Mousa et al., 2010a (Detroit, Michigan) |
|
|
The study is an evaluation of an intervention targeting ethnic minority women, including Arab Americans. The data were not presented separately for the Arab community health workers. The sample size was small. |
| Kin Keeper Cancer Prevention Intervention studies (quantitative) | |||
| Gauss et al., 2013b (Detroit, Michigan) |
|
|
A single-item measure was used to assess pain perceptions of the Pap test. Findings are limited to underserved Arab women in Detroit, Michigan. |
| Roman et al., 2014b (Detroit, Michigan) |
|
|
This study used a some-what new approach (the additive approach to incorporate co-occurring risk factors: competing priorities, health risks, health literacy, and system risks). Findings are limited to underserved Arab women in Detroit, Michigan. |
| Talley & Williams, 2015b (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. |
| Williams et al., 2013b (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. Only baseline data are presented, and evaluating the long-term effectiveness of the intervention is not possible. |
| Williams et al., 2014b (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. |
| Williams et al., 2015b (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. |
| Zambrana et al., 2015b (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. Only baseline data are presented, and evaluating the long-term effectiveness of the intervention is not possible. |
| Kin Keeper Cancer Prevention Intervention studies (mixed- and multi-methods studies) | |||
| Ford et al., 2014a (Detroit, Michigan) |
|
|
The study is an evaluation of the fidelity of an intervention targeting ethnic minority women, including Arab Americans. The data were not presented separately for the Arab participants and community health workers. Findings are limited to underserved Arab women in Detroit, Michigan. |
| Williams et al., 2009a (Detroit, Michigan) |
|
|
Data were not presented separately for the Arab sample. The sample size for Arab community health workers was small. Findings are limited to underserved Arab women in Detroit, Michigan. |
| Williams & Templin, 2013a (Detroit, Michigan) |
|
|
Findings are limited to underserved Arab women in Detroit, Michigan. |
The data relevance score (based on Whittemore & Knafl, 2005) was low.
The data relevance score (based on Whittemore & Knafl, 2005) was high.
C-CLAT—Cervical Cancer Literacy Assessment Tool; CI—confidence interval; OR—odds ratio; Pap—Papanicolaou
Cervical Cancer Screening Rates
Only six studies reported cervical cancer screening rates, ranging from 7%–84%; two of these did not report a separate rate for Arab American women. Dallo and Kindratt’s (2015) secondary data analysis of the 2000–2011 NHIS data compared cancer screening behaviors of U.S.-born and foreign-born (European and Arab countries) non-Hispanic White women. After adjusting for age, foreign-born Arab American women were significantly less likely (84%) to receive a Pap test in their lifetime than European (87%) and U.S. (95%) women (p ≤ 0.00). A secondary data analysis of the Michigan SCBRFS reported that, among women aged 50 years or older, 77% of Arab American women had received a Pap test in the past three years, compared to 87% of the general population in Michigan, 86% of American Indians, 85% of African Americans, and 77% of Hispanics; significance levels were not provided by the authors (Darwish-Yassine & Wing, 2005). In another study, Arab American women aged 21 years or older were significantly more likely (71%) to have received a Pap test in the past three years than Latina women (68%) but less likely than Black women (83%; p < 0.01) (Williams et al., 2013). In a focus group study with 25 participants in 3 groups, the majority (no specified rate) of Arab American women had previously been screened for cervical cancer, but few had received testing at the recommended interval (Shah, Ayash, Pharaon, & Gany, 2008). The lowest cervical cancer screening rate (50%) was reported in a small sample of Arab American women (Salman, 2012). Rates of ever receiving cervical cancer screening were similar in other studies (84% in Padela et al., 2014; 80% in Williams et al., 2013).
Factors Associated With Cervical Cancer Screening
In the following sections, various factors that influence cervical cancer screening are described, synthesized from the studies reviewed: knowledge of cervical cancer screening and prevention; attitudes and beliefs; healthcare providers and setting; education, marital status, income, and social support; and nativity, immigration, and acculturation. Lastly, the Kin Keeper model is reviewed.
Knowledge of cervical cancer screening and prevention
The conceptual and operational definitions of knowledge about cervical cancer screening included not only this knowledge, but also awareness of and health literacy about cancer screening. Knowledge was operationalized in several ways, ranging from specific questions related to the purpose of a Pap test to more detailed literacy assessment tools, such as the Cervical Cancer Literacy Assessment Tool (C-CLAT). The majority of Arab American women understood that the purpose of a Pap test is to detect cervical cancer cells early (Salman, 2012; Shah et al., 2008). Overall, Arab American women had an above-average cervical cancer literacy score using the C-CLAT in terms of their awareness, knowledge and screening, and prevention and control of cervical cancer (X̄ = 10, SD = 3), similar to Black and Latina women (Talley & Williams, 2015); however, only a small number of Arab American women were able to answer more than 75% of the 16 questions correctly (Williams, Talley, & Smith, 2014; Zambrana et al., 2015).
Higher health literacy risk—defined by Roman et al. (2014) as low cervical cancer literacy, no knowledge of own family cancer history, and an education of less than 12 years—was associated with reduced odds of receiving a Pap test in the past three years; however, the relationship was not significant (odds ratio [OR] = 0.9, 95% confidence interval [CI] [0.67, 1.17]). No other studies investigated the relationship between having cervical cancer screening knowledge or literacy and receiving cervical cancer screening.
Attitudes and beliefs
Different aspects of attitudes and beliefs toward cervical cancer screening were addressed in several studies. These factors, which relate to sociocultural and religious issues, as well as to Pap test pain perception, influence cervical cancer screening among Arab American women.
From sociocultural and religious perspectives, tensions exist related to conflict between religious and sociocultural values in Arab and Muslim societies concerning bodily privacy, modesty, and virginity, as well as the guidelines that recommend a Pap test starting at age 21 years, regardless of sexual activity (Matin & LeBaron, 2004; Salman, 2012). One participant in a study said, “I would want to be assured as much as possible that my hymen wouldn’t be broken. That’s the underlying fear for a lot of us” (Matin & LeBaron, 2004). Embarrassment and modesty were reported as barriers to receiving a Pap test. Women expressed comfort in wearing their Islamic and cultural clothing during the test and strongly preferred a female provider (Salman, 2012). Despite sociocultural and religious concerns about cervical cancer screening, modesty and religiosity were not associated with cervical cancer screening rates among Muslim women (Arab and non-Arab); however, people’s interpretation of events in their lives as a punishment from God was negatively associated with cervical cancer screening rates (p < 0.05) (Padela et al., 2014).
Fatalism, the degree to which a person believes that health outcomes are inescapable and controlled by God, has also been reported to influence preventive health behaviors (Padela et al., 2014; Shah et al., 2008). Among Muslim women (Arab and non-Arab), higher fatalism scores (using three fatalism measures) were associated with lower cervical cancer screening rates (p < 0.05), but, when adjusting for sociodemographic variables, the association was not significant (Padela et al., 2014). Participants in the focus groups also expressed fatalistic thoughts about cancer, such as “God only knows,” “I think cancer is from God. It has no reasons,” and “We do the best we can; the rest is up to God” (Shah et al., 2008, p. 434).
Perceptions of pain during Pap test procedures were reported in only one study in which 24% of Arab American women perceived the procedure to be very painful (Gauss et al., 2013). In addition, women who perceived the Pap test to be very painful were 50% less likely to make an appointment for their first Pap test (OR = 0.58, 95% CI [0.14, 0.94]). The Kin Keeper model, an educational intervention that focused on increasing knowledge of cervical cancer screening and prevention, was successful in decreasing perceptions that the Pap test is very painful (by 4% immediately postintervention and by 15% 12 months postintervention) (Gauss et al., 2013).
Healthcare providers and setting
The role of the healthcare provider and the setting influenced whether Arab American women received cervical cancer screening. Having a primary care provider increased the odds of receiving a Pap test among Muslim women (Arab and non-Arab; OR = 11.1, 95% CI [5, 24.4]) (Padela et al., 2014). Similarly, the lack of a healthcare provider’s recommendations for a Pap test decreased the odds for receiving it (OR = 0.26, 95% CI [0.12, 0.54]). When asked about their healthcare provider’s recommendation for cervical cancer screening, more than half of the Arab American women in one study reported that, in the past three years, their healthcare provider had not recommended that they receive a Pap test (Roman et al., 2014).
Gender and religious affiliation of the healthcare provider seemed to be salient factors for women to obtain a Pap test. If given the choice, Arab American women would prefer that a female provider perform the Pap test (Salman, 2012). In addition, Muslim American women expressed preference for a Muslim provider who would better understand their sociocultural and religious perspectives (Matin & LeBaron, 2004). Perceived religious discrimination in the healthcare setting was negatively associated with receiving a Pap test among Muslim women (Arab and non-Arab; OR = 0.81, 95% CI [0.7, 0.95]) (Padela et al., 2014).
Education, marital status, income, and social support
Results were mixed regarding the associations among level of education, marital status, income, and cervical cancer screening. One study reported higher odds of receiving cervical cancer screening with increased educational attainment (OR = 3.5, 95% CI [1.1, 11.4]) (Padela et al., 2014). No significant relationships between level of education and receiving a Pap test were reported in the other studies (Roman et al., 2014; Salman, 2012).
Being single was significantly associated with reduced odds of receiving a Pap test (OR = 0.1, 95% CI [0.02, 0.39]) in one study (Roman et al., 2014) but not significantly associated in another (Padela et al., 2014). During one-on-one interviews and focus group sessions, single Muslim women (Arab and non-Arab) reported their preference for not receiving cervical cancer screening and gynecologic care, identifying marital status as crucial to when gynecologic care would be needed and appropriate (Matin & LeBaron, 2004).
Household income was not significantly associated with cervical cancer screening (Padela et al., 2014; Salman, 2012); however, lack of health insurance and having to pay extra costs for a Pap test were considered to be economic concerns and were negatively related to receiving cervical cancer screening (p < 0.00) (Salman, 2012). Arab American women who knew another woman from the Arab community who had received cervical cancer screening were also more likely to get a Pap test (p = 0.00) and had a greater motivation to get screened (Salman, 2012). Family cohesion and communication, family-reported health status, and presence of different generations in the household were not associated with cervical cancer literacy among Arab American women; however, Arab American women living in families with large age differences had significantly higher cervical cancer literacy (p = 0.02) (Zambrana et al., 2015).
Nativity, immigration, and acculturation
Disparities in cervical cancer screening existed by nativity status (referring to native- or foreign-born status); foreign-born Arab American women were less likely to report receiving a Pap test than European- and U.S.-born non-Hispanic White women (p < 0.00) (Dallo & Kindratt, 2015). Length of stay in the United States and an understanding of English were positively associated with cervical cancer screening. Arab American women who had lived in the United States for 10 years or longer were more likely to have received a Pap test in the past two years compared to those who had lived in the United States for fewer than 10 years (p < 0.004) (Padela et al., 2014; Salman, 2012). Women who understood and spoke English very well were more likely to have received a Pap test in the past two years compared to women who did not understand (p = 0.62) or speak (p = 0.13) English very well (Salman, 2012).
The Kin Keeper Cancer Prevention Intervention
The Kin Keeper model was developed using a community-based participatory approach in a diverse sample of underserved ethnic and racial minority women (African Americans, Latinas, and Arabs). The aim of the intervention is to promote breast and cervical cancer screening, and it focuses on the strong kinship ties between female family members and engaged community health workers (Ford et al., 2014; Mousa et al., 2010; Williams, Mabiso, Jackson, Lawshe, & Maurer, 2009). Overall, Arab women’s cervical cancer literacy and screening rates are similar to those of Black and Latina women in the United States. In addition, an Arabic version of the C-CLAT was developed and psychometrically evaluated during the development of the Kin Keeper model. The internal consistency of the C-CLAT among Arab American women was 0.6, which was lower than among Black and Latina women (0.73 and 0.76, respectively) (Williams & Templin, 2013).
Studies of the Kin Keeper model provide a better understanding of the challenges faced in the retention of hard-to-reach populations, such as Arab American women, in longitudinal studies. To date, no published studies have reported the postintervention follow-up results of the Kin Keeper model in relation to cervical cancer literacy and screening rates among Arab American women.
Discussion
The aims of this review were to assess and synthesize the existing evidence on cervical cancer screening behaviors among Arab American women. Even when focused on what can be construed as a homogeneous sample, the heterogeneity of study findings demonstrates the multiple nuanced factors that are involved in understanding cervical cancer screening in this group. Eleven of 17 studies reported data on different aspects of the Kin Keeper intervention using the same sample, and three studies investigated cancer screening attitudes and practices in general. As a result, a firm conclusion can be drawn: Significant need exists for additional research to better understand cervical cancer screening attitudes, beliefs, and behaviors among Arab American women.
Many complex factors can influence ethnic minority women’s decision regarding cervical cancer screening. Failure to receive cervical cancer screening is attributable to multiple interrelated reasons, including personal factors (e.g., fear of pain, embarrassment, threat to virginity, anxiety, inadequate knowledge, lack of time, misperception of risk), cultural factors (e.g., provider gender, acculturation, meaning of preventive medicine), religious factors, and systemic factors (e.g., lack of insurance, poverty, immigration status, geographic isolation, lack of providers, length of stay in the United States) (Daley et al., 2011; Johnson et al., 2008; Lee & Carvallo, 2014).
Marital status plays a considerable role in explaining the wide range of screening prevalence in Arab American women. Despite the lack of consistent evidence associating marital status and Pap test uptake, a trend of lower uptake exists among unmarried Arab American women. The studies that reported low screening rates had either a very small sample of single women (Matin & LeBaron, 2004) or a small sample of single women (Salman, 2012). Conversely, the majority of Arab women who reported higher cervical cancer screening rates were married (Dallo & Kindratt, 2015; Williams et al., 2013). This trend is supported by the fact that female premarital virginity and bodily privacy are very important in most Arab societies and reflect respect, modesty, and good reputation (Abboud, Jemmott, & Sommers, 2015; Akl, 2014; Ilkkaracan, 2008). Virginity is mostly defined by the presence and appearance of a hymen; a Pap test could be considered a cause of loss of virginity and an invasion of bodily privacy. To maintain virginity, single Arab American women might engage in sexual activity other than vaginal–penile intercourse (e.g., anal intercourse) (Abboud et al., 2015) and are at risk for sexually transmitted infections that can be shared by skin-to-skin contact, such as HPV (Moscicki, 2005). Single Arab women who engage in behaviors that suggest sexual engagement, such as gynecologic examinations, cervical cancer screening, or HPV vaccination, may be stigmatized, which interferes with their access to sexual and reproductive health care. In addition, single Arab women are not expected to seek reproductive and sexual health care and consider cervical cancer screening to be unimportant or unnecessary before marriage. Regardless of sexual activity or marital status, and because sexually transmitted infections are not the only cause of cervical cancer, routine cervical cancer screening is necessary for early detection of precancerous cells and for substantial reduction of cancer incidence and mortality (Moyer, 2012). More research is needed to understand the relationship between cervical cancer screening behaviors and marital status among Arab American women to design interventions to increase screening in single Arab American women. Other studies among Asian and Latina women have also identified that perceptions of cervical cancer screening are deeply rooted in sociocultural norms, such as modesty, gender relations, and culturally defined morality (Daley et al., 2011; Tung, Nguyen, & Tran, 2008; Watts et al., 2009). The current authors did not find any published studies reporting HPV vaccination attitudes and behaviors among Arab American women. Three effective HPV vaccines (bivalent, quadrivalent, and 9-valent vaccines) exist, and strong evidence supports the benefits of these vaccines in substantially reducing HPV infection and cervical cancer incidence (Kash et al., 2015; Moscicki, 2008; Petrosky et al., 2015; Thaxton & Waxman, 2015).
That the studies reviewed did not necessarily target Arab women impedes firm conclusions. Arabs are defined as individuals who descend from one of the 22 Arab countries. Realizing that not all Arabs are Muslim is important (the majority [91%] of Arabs are Muslim, but millions of Arabs are Christian, and thousands are Jewish or atheistic); in addition, not all Muslims are Arabs (80% of Muslims live in non-Arabic speaking countries, like Indonesia, Pakistan, India, and Iran) (Pew Research Center, 2009). In this review, two studies focused on Muslim women in the United States had small subsamples of Arab Muslim women, and data on these women were not presented separately (Matin & LeBaron, 2004; Padela et al., 2014). Salman (2012) and Shah et al. (2008) targeted samples of Arab Muslim women; these two samples excluded Arab women who did not identify as Muslim. Although Muslims are the majority in the Arab world, in the United States, Arab Americans are mostly Christians (Arab American National Museum, 2015; Samhan, 2014).
The Kin Keeper studies targeted underserved Arab American women in Dearborn, Michigan. The findings of these studies do not adequately represent the socioeconomic background of other Arab women in the United States. Although Michigan has the highest concentrated population of Arabs in the country, this population includes a disproportionate number of Arab Americans with lower education levels and income compared to Arab Americans living in other states, such as New York or California (Arab American Institute, n.d.; Read, Amick, & Donato, 2005). Most of the studies reviewed do not adequately represent the diversity among Arab American women, necessitating more research, with special attention paid to representation of the diverse religions, countries of origin, and socioeconomic backgrounds.
Acculturation is a complex concept that is hard to measure. Only two studies measured this concept and its association with cervical cancer screening. Padela et al. (2014) measured acculturation as number of years living in the United States, whereas Salman (2012) measured it in terms of years living in the United States and proficiency in the English language. In addition, nativity status plays a significant role in the acculturation process and in health disparities across several races and ethnicities (Dallo, Booza, & Nguyen, 2015; Echeverria & Carrasquillo, 2006; Singh & Hiatt, 2006). Among Arab American women, being foreign-born is associated with having significantly lower odds of receiving a Pap test, even after controlling for demographic and socioeconomic factors (Dallo & Kindratt, 2015). Other studies conducted among His-panics reported that foreign-born status and having lived in the United States for fewer than five years are barriers to receiving cervical cancer screening (Goel et al., 2003; Rodríguez, Ward, & Pérez-Stable, 2005; Watts et al., 2009). The acculturation experience is dynamic and multifaceted, and it cannot be reduced to number of years, English proficiency, or nativity; other indicators—such as residential area (ethnic enclave versus nonethnic enclave), socioeconomic factors, opportunities for upward mobility, social capital, influence of familial and interpersonal relations and values, and discrimination—can provide a better socioecologic understanding of the acculturation process and health behaviors of immigrants in the United States (Lopez-Class, Castro, & Ramirez, 2011; Unger & Schwartz, 2012; Viruell-Fuentes, Miranda, & Abdulrahim, 2012). The findings of this review and other studies suggest the need for healthcare providers to take into consideration the unique and nuanced needs of immigrant populations.
Limitations
Several limitations were identified in these studies. The sample sizes of Arab women were small, and results were sometimes not reported separately for Arab women. In addition, the 11 studies reporting on the Kin Keeper intervention were limited to Arab women from Detroit, Michigan. Also, this review is based on the small number of studies available to date.
Implications for Nursing
Despite limitations, the results of these studies have substantial implications for healthcare providers. Arab Americans are a fast-growing ethnic minority in the United States. In addition, nurses must care for multinational and multiethnic populations because of the effects of migration. These factors contribute and are in addition to the challenges and obstacles that inhibit individuals from obtaining health care that is free of stereotyping and discrimination. The findings of this integrative review offer nurses an initial understanding of the complex and intersecting factors (e.g., gender, education, ethnicity, religion, immigration, education) that influence sexual and reproductive health among Arab American women.
From this review of the existing literature, the authors determined that cervical cancer screening rates among Arab American women were similar to the screening rates of other ethnic minorities and lower than those of non-Hispanic White women in the United States. Even with mixed results regarding the factors influencing cervical cancer screening behaviors, nurses are encouraged to offer additional attention to Arab American women through health education and cervical cancer screening recommendations because few studies have reported that cervical cancer literacy and healthcare provider recommendations for cervical cancer screening increase the rates of Pap testing in this population. In addition, despite evidence supporting HPV vaccination efficacy, no studies were found investigating HPV vaccination attitudes and behaviors, which offers another opportunity for nurses to initiate conversation about HPV infection and vaccination among young Arab American women. Nurses play a key role in protecting against and detecting cervical cancer through Pap testing and HPV vaccination; as such, nurses have important communication opportunities for creating awareness among women. Through comprehensive and culturally informed care, nurses can identify and address several factors (e.g., perceived barriers, lack of knowledge, socioeconomic and immigration factors) that can hinder a woman’s ability to receive cervical cancer screening.
More research is needed to address the barriers to and facilitators of cervical cancer screening among Arab American women, as well as HPV knowledge and vaccination rates. Qualitative and quantitative research must be conducted to understand the complex socioecologic factors in cervical cancer screening and prevention among Arab American women. A socioecologic approach will help to examine and understand the multiple levels of influence on health behaviors, including individual, community, environmental, and policy levels (Sallis & Owen, 2015). This understanding will help to design multilevel and culturally relevant programs similar to the Kin Keeper model but reaching more than underserved women in one geographic area. Future research needs to focus on more representative samples of Arab women in the United States with respect to country of origin, religion, immigration, and socioeconomic background.
At the policy level, given the rapidly changing and complex healthcare guidelines relating to cervical cancer screening and prevention, healthcare settings need to have formal guidelines and strategies that meet the educational and training needs of healthcare providers to be able to provide current and evidence-based care to women from diverse backgrounds. To eradicate cervical cancer, policymakers need to shift funding streams into cancer prevention, community outreach, and continuing education and training for healthcare providers.
Conclusion
The findings from the studies reviewed support the idea that Arab American women’s health behaviors in terms of cervical cancer screening differ from those of non-Hispanic White women in the United States and are more comparable to those of other ethnic minorities. These findings add to the already existing discourse on the importance of separating Arab Americans from the “White” category in the U.S. Census. A separate category for individuals of Arab or Middle Eastern ancestry will assist in reaching Arabs throughout the country.
Knowledge Translation.
A lack of consistent research findings precludes firm conclusions about cervical cancer screening behaviors among Arab American women and the factors associated with these behaviors.
Additional research is needed to inform culturally relevant interventions and programs to increase cervical cancer screening rates in this population.
Healthcare providers should be knowledgeable about complex factors that influence cervical cancer screening among Arab American women to promote cancer prevention and treatment.
Acknowledgments
Abboud was supported by a Ruth L. Kirschstein NRSA Institutional PostDoctoral Fellowship (T32NR007100; principal investigator Sommers) at the School of Nursing at the University of Pennsylvania throughout the conceptualization and completion of this article.
Footnotes
Abboud, Brawner, and Sommers contributed to the conceptualization and design. Abboud, De Penning, and Sommers completed the data collection. Abboud, Brawner, Menon, Glanz, and Sommers provided the analysis. All of the authors contributed to the manuscript preparation.
References
- Abboud S, Jemmott LS, Sommers MS. “We are Arabs:” The embodiment of virginity through Arab and Arab American women’s lived experiences. Sexuality and Culture. 2015;19:715–736. doi: 10.1007/s12119-015-9286-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Ras W, Abu-Bader SH. The impact of the September 11, 2001, attacks on the well-being of Arab Americans in New York City. Journal of Muslim Mental Health. 2008;3:217–239. doi: 10.1080/15564900802487634. [DOI] [Google Scholar]
- Abu-Ras W, Abu-Bader SH. Risk factors for depression and posttraumatic stress disorder (PTSD): The case of Arab and Muslim Americans post-9/11. Journal of Immigrant and Refugee Studies. 2009;7:393–418. doi: 10.1080/15562940903379068. [DOI] [Google Scholar]
- Ajrouch KJ, Jamal A. Assimilating to a white identity: The case of Arab Americans. International Migration Review. 2007;41:860–879. doi: 10.1111/j.1747-7379.2007.00103.x. [DOI] [Google Scholar]
- Akl AA. Doctoral dissertation. 2014. Multimodal expressions of young Arab Muslim American women. Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3670665) [Google Scholar]
- Arab American Institute. Demographics. n.d Retrieved from http://www.aaiusa.org/demographics.
- Arab American National Museum. Arab Americans: An integral part of American society. 2015 Retrieved from http://www.arabamericanmuseum.org/umages/pdfs/resource_booklets/AANM-ArabAmericansBooklet-web.pdf.
- Daley E, Alio A, Anstey EH, Chandler R, Dyer K, Helmy H. Examining barriers to cervical cancer screening and treatment in Florida through a socio-ecological lens. Journal of Community Health. 2011;36:121–131. doi: 10.1007/s10900-010-9289-7. [DOI] [PubMed] [Google Scholar]
- Dallo FJ, Booza J, Nguyen ND. Functional limitations and nativity status among older Arab, Asian, Black, Hispanic, and White Americans. Journal of Immigrant and Minority Health. 2015;17:535–542. doi: 10.1007/s10903-013-9943-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallo FJ, Kindratt TB. Disparities in vaccinations and cancer screening among U.S.- and foreign-born Arab and European American non-Hispanic white women. Women’s Health Issues. 2015;25:56–62. doi: 10.1016/j.whi.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Darwish-Yassine M, Wing D. Cancer epidemiology in Arab Americans and Arabs outside the Middle East. Ethnicity and Disease. 2005;15(Suppl 1):S1-5–8. [PubMed] [Google Scholar]
- Echeverria SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Medical Care. 2006;44:788–792. doi: 10.1097/01.mlr.0000215863.24214.41. [DOI] [PubMed] [Google Scholar]
- El-Sayed AM, Galea S. The health of Arab-Americans living in the United States: A systematic review of the literature. BMC Public Health. 2009;9:272. doi: 10.1186/1471-2458-9-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sayed AM, Tracy M, Scarborough P, Galea S. Ethnic inequalities in mortality: The case of Arab-Americans. PLOS ONE. 2011;6:e29185. doi: 10.1371/journal.pone.0029185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford S, Meghea C, Estes T, Hamade H, Lockett M, Williams KP. Assessing the fidelity of the Kin KeeperSM prevention intervention in African American, Latina and Arab women. Health Education Research. 2014;29:158–165. doi: 10.1093/her/cyt100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederiksen ME, Njor S, Lynge E, Rebolj M. Psychological effects of diagnosis and treatment of cervical intraepithelial neoplasia: A systematic review. Sexually Transmitted Infections. 2015;91:248–256. doi: 10.1136/sextrans-2014-051754. [DOI] [PubMed] [Google Scholar]
- Gauss JW, Mabiso A, Williams KP. Pap screening goals and perceptions of pain among black, Latina, and Arab women: Steps toward breaking down psychological barriers. Journal of Cancer Education. 2013;28:367–374. doi: 10.1007/s13187-012-0441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick SB, Clarke AR, Blanchard A, Whitaker AK. Cervical cancer screening, diagnosis and treatment interventions for racial and ethnic minorities: A systematic review. Journal of General Internal Medicine. 2012;27:1016–1032. doi: 10.1007/s11606-012-2052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel MS, Wee CC, McCarthy EP, Davis RB, Ngo-Metzger Q, Phillips RS. Racial and ethnic disparities in cancer screening: The importance of foreign birth as a barrier to care. Journal of General Internal Medicine. 2003;18:1028–1035. doi: 10.1111/j.1525-1497.2003.20807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassouneh DM, Kulwicki A. Mental health, discrimination, and trauma in Arab Muslim women living in the U.S.: A pilot study. Mental Health, Religion and Culture. 2007;10:257–262. doi: 10.1080/13694670600630556. [DOI] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, … Cronin KA. SEER cancer statistics review, 1975–2012. 2015 Retrieved from http://seer.cancer.gov/archive/csr/1975_2012.
- Ilkkaracan P, editor. Deconstructing sexuality in the Middle East: Challenges and discourses. Hampshire, England: Ashgate Publishing Limited; 2008. [Google Scholar]
- Inhorn MC, Fakih MH. Arab Americans, African Americans, and infertility: Barriers to reproduction and medical care. Fertility and Sterility. 2006;85:844–852. doi: 10.1016/j.fertnstert.2005.10.029. [DOI] [PubMed] [Google Scholar]
- Jamal A, Naber N, editors. Race and Arab Americans before and after 9/11: From invisible citizens to visible subjects. Syracuse, NY: Syracuse University Press; 2008. [Google Scholar]
- Johnson CE, Mues KE, Mayne SL, Kiblawi AN. Cervical cancer screening among immigrants and ethnic minorities: A systematic review using the health belief model. Journal of Lower Genital Tract Disease. 2008;12:232–241. doi: 10.1097/LGT.0b013e31815d8d88. [DOI] [PubMed] [Google Scholar]
- Kash N, Lee MA, Kollipara R, Downing C, Guidry J, Tyring SK. Safety and efficacy data on vaccines and immunization to human papillomavirus. Journal of Clinical Medicine. 2015;4:614–633. doi: 10.3390/jcm4040614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katki HA, Kinney WK, Fetterman B, Lorey T, Poitras NE, Cheung L, … Castle PE. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: A population-based study in routine clinical practice. Lancet Oncology. 2011;12:663–672. doi: 10.1016/S1470-2045(11)70145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: Systematic review and meta-analysis. Lancet. 2006;367:489–498. doi: 10.1016/S0140-6736(06)68181-6. [DOI] [PubMed] [Google Scholar]
- Lee J, Carvallo M. Socioecological perspectives on cervical cancer and cervical cancer screening among Asian American women. Journal of Community Health. 2014;39:863–871. doi: 10.1007/s10900-014-9887-x. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, … Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine. 2009;151:W-65–W-94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- Lopez-Class M, Castro FG, Ramirez AG. Conceptions of acculturation: A review and statement of critical issues. Social Science and Medicine. 2011;72:1555–1562. doi: 10.1016/j.socscimed.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Markowitz LE, Hariri S, Lin C, Dunne EF, Steinau M, McQuillan G, Unger ER. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. Journal of Infectious Diseases. 2013;208:385–393. doi: 10.1093/infdis/jit192. [DOI] [PubMed] [Google Scholar]
- Matin M, LeBaron S. Attitudes toward cervical cancer screening among Muslim women: A pilot study. Women and Health. 2004;39:63–77. doi: 10.1300/j013v39n03_05. [DOI] [PubMed] [Google Scholar]
- Moscicki AB. Impact of HPV infection in adolescent populations. Journal of Adolescent Health. 2005;37(Suppl):S3–S9. doi: 10.1016/j.jadohealth.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Moscicki AB. HPV vaccines: Today and in the future. Journal of Adolescent Health. 2008;43(Suppl):S26–S40. doi: 10.1016/j.jadohealth.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousa SM, Brooks E, Dietrich M, Henderson A, McLean C, Patricia Williams K. Community health workers speak out about the Kin KeeperSM model. Journal of Cancer Education. 2010;25:236–241. doi: 10.1007/s13187-010-0049-2. [DOI] [PubMed] [Google Scholar]
- Moyer VA. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2012;156:880–891. doi: 10.7326/0003-4819-156-12-201206190-00424. [DOI] [PubMed] [Google Scholar]
- Naber N. Ambiguous insiders: An investigation of Arab American invisibility. Ethnic and Racial Studies. 2000;23:37–61. doi: 10.1080/014198700329123. [DOI] [Google Scholar]
- Newhouse R, Dearholt S, Poe S, Pugh LC, White K. The Johns Hopkins Nursing Evidence-Based Practice Rating Scale. Baltimore, MD: The Johns Hopkins Hospital, Johns Hopkins University School of Nursing; 2005. [Google Scholar]
- Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, … Dubin G. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and pre-cancer caused by oncogenic HPV types (PATRICIA): Final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301–314. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- Padela AI, Peek M, Johnson-Agbakwu CE, Hosseinian Z, Curlin F. Associations between religion-related factors and cervical cancer screening among Muslims in greater Chicago. Journal of Lower Genital Tract Disease. 2014;18:326–332. doi: 10.1097/LGT.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosky E, Bocchini JA, Jr, Hariri S, Chesson H, Curtis CR, Saraiya M, … Markowitz LE. Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. Morbidity and Mortality Weekly Report. 2015;64:300–304. [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. Mapping the global Muslim population. 2009 Oct 7; Retrieved from http://www.pewforum.org/2009/10/07/mapping-the-global-muslim-population.
- Pfaendler KS, Wenzel L, Mechanic MB, Penner KR. Cervical cancer survivorship: Long-term quality of life and social support. Clinical Therapeutics. 2015;37:39–48. doi: 10.1016/j.clinthera.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce Campbell CM, Menezes LJ, Paskett ED, Giuliano AR. Prevention of invasive cervical cancer in the United States: Past, present, and future. Cancer Epidemiology, Biomarkers and Prevention. 2012;21:1402–1408. doi: 10.1158/1055-9965.EPI-11-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JG, Amick B, Donato KM. Arab immigrants: A new case for ethnicity and health? Social Science and Medicine. 2005;61:77–82. doi: 10.1016/j.socscimed.2004.11.054. [DOI] [PubMed] [Google Scholar]
- Rodríguez MA, Ward LM, Pérez-Stable EJ. Breast and cervical cancer screening: Impact of health insurance status, ethnicity, and nativity of Latinas. Annals of Family Medicine. 2005;3:235–241. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman L, Meghea C, Ford S, Penner L, Hamade H, Estes T, Williams KP. Individual, provider, and system risk factors for breast and cervical cancer screening among underserved Black, Latina, and Arab women. Journal of Women’s Health. 2014;23:57–64. doi: 10.1089/jwh.2013.4397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Owen N. Ecological models of health behaviors. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior: Theory, research, and Practice. 5. San Francisco, CA: John Wiley and Sons; 2015. pp. 43–64. [Google Scholar]
- Salman KF. Health beliefs and practices related to cancer screening among Arab Muslim women in an urban community. Health Care for Women International. 2012;33:45–74. doi: 10.1080/07399332.2011.610536. [DOI] [PubMed] [Google Scholar]
- Samhan HH. Intra-ethnic diversity and religion. In: Nassar-McMillan SC, Ajrouch KJ, Hakim-Larson J, editors. Biopsychosocial perspectives on Arab Americans. Culture, development, and health. New York, NY: Springer; 2014. pp. 45–65. [Google Scholar]
- Seeff LC, McKenna MT. Cervical cancer mortality among foreign-born women living in the United States, 1985 to 1996. Cancer Detection and Prevention. 2003;27:203–208. doi: 10.1016/S0361-090X(03)00062-X. [DOI] [PubMed] [Google Scholar]
- Shah SM, Ayash C, Pharaon NA, Gany FM. Arab American immigrants in New York: Health care and cancer knowledge, attitudes, and beliefs. Journal of Immigrant and Minority Health. 2008;10:429–436. doi: 10.1007/s10903-007-9106-2. [DOI] [PubMed] [Google Scholar]
- Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. International Journal of Epidemiology. 2006;35:903–919. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- Swan J, Breen N, Graubard BI, McNeel TS, Blackman D, Tangka FK, Ballard-Barbash R. Data and trends in cancer screening in the United States: Results from the 2005 National Health Interview Survey. Cancer. 2010;116:4872–4881. doi: 10.1002/cncr.25215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley CH, Williams KP. Impact of age and comorbidity on cervical and breast cancer literacy of African Americans, Latina, and Arab women. Nursing Clinics of North America. 2015;50:545–563. doi: 10.1016/j.cnur.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaxton L, Waxman AG. Cervical cancer prevention: Immunization and screening 2015. Medical Clinics of North America. 2015;99:469–477. doi: 10.1016/j.mcna.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Tung WC, Nguyen DH, Tran DN. Applying the trans-theoretical model to cervical cancer screening in Vietnamese-American women. International Nursing Review. 2008;55:73–80. doi: 10.1111/j.1466-7657.2007.00602.x. [DOI] [PubMed] [Google Scholar]
- Unger JB, Schwartz SJ. Conceptual considerations in studies of cultural influences on health behaviors. Preventive Medicine. 2012;55:353–355. doi: 10.1016/j.ypmed.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeer WM, Bakker RM, Kenter GG, Stiggelbout AM, ter Kuile MM. Cervical cancer survivors’ and partners’ experiences with sexual dysfunction and psychosexual support. Supportive Care in Cancer. 2016;24:1679–1687. doi: 10.1007/s00520-015-2925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesco KK, Whitlock EP, Eder M, Lin J, Burda BU, Senger CA, … Zuber S. Screening for cervical cancer: A systematic evidence review for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Evidence Synthesis No. 86. [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Social Science and Medicine. 2012;75:2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Watts L, Joseph N, Velazquez A, Gonzalez M, Munro E, Muzikansky A, … Del Carmen MG. Understanding barriers to cervical cancer screening among Hispanic women. American Journal of Obstetrics and Gynecology. 2009;201:199. doi: 10.1016/jjog.2009.05.014. [DOI] [PubMed] [Google Scholar]
- White ID. Sexual difficulties after pelvic radiotherapy: Improving clinical management. Clinical Oncology. 2015;27:647–655. doi: 10.1016/j.clon.2015.06.018. [DOI] [PubMed] [Google Scholar]
- Whittemore R. Combining evidence in nursing research: Methods and implications. Nursing Research. 2005;54:56–62. doi: 10.1097/00006199-200501000-00008. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Knafl K. The integrative review: Updated methodology. Journal of Advanced Nursing. 2005;52:546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- Williams KP, Ford S, Meghea C. Cultural connections: The key to retention of Black, Latina, and Arab women in the Kin Keeper(SM) Cancer Prevention Intervention studies. Journal of Cancer Education. 2015;31:522–528. doi: 10.1007/s13187-015-0857-5. [DOI] [PubMed] [Google Scholar]
- Williams KP, Mabiso A, Jackson TL, Lawshe DC, Maurer J. Breast cancer and cervical cancer control program enrollees inform the Kin Keeper curriculum. Journal of Cancer Education. 2009;24:257–260. doi: 10.1080/08858190902972939. [DOI] [PubMed] [Google Scholar]
- Williams KP, Roman L, Meghea CI, Penner L, Hammad A, Gardiner J. Kin KeeperSM: Design and baseline characteristics of a community-based randomized controlled trial promoting cancer screening in Black, Latina, and Arab women. Contemporary Clinical Trials. 2013;34:312–319. doi: 10.1016/j.cct.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams KP, Talley CH, Smith D. Cervical cancer awareness among African-American, Latina, and Arab women. Journal of the National Black Nurses Association. 2014;25:31–38. [Google Scholar]
- Williams KP, Templin TN. Bringing the real world to psychometric evaluation of cervical cancer literacy assessments with Black, Latina, and Arab women in real-world settings. Journal of Cancer Education. 2013;28:738–743. doi: 10.1007/s13187-013-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrana RE, Meghea C, Talley C, Hammad A, Lockett M, Williams KP. Association between family communication and health literacy among underserved racial/ethnic women. Journal of Health Care for the Poor and Underserved. 2015;26:391–405. doi: 10.1353/hpu.2015.0034. [DOI] [PubMed] [Google Scholar]